Sport Intervention Programs (SIPs) to Improve Health and Social Inclusion in People with Intellectual Disabilities: A Systematic Review
Abstract
1. Introduction
Definition of Terms: From Physical Activity (PA) to Adapted Physical Activity (APA) and Sport Intervention Programs (SIPs)
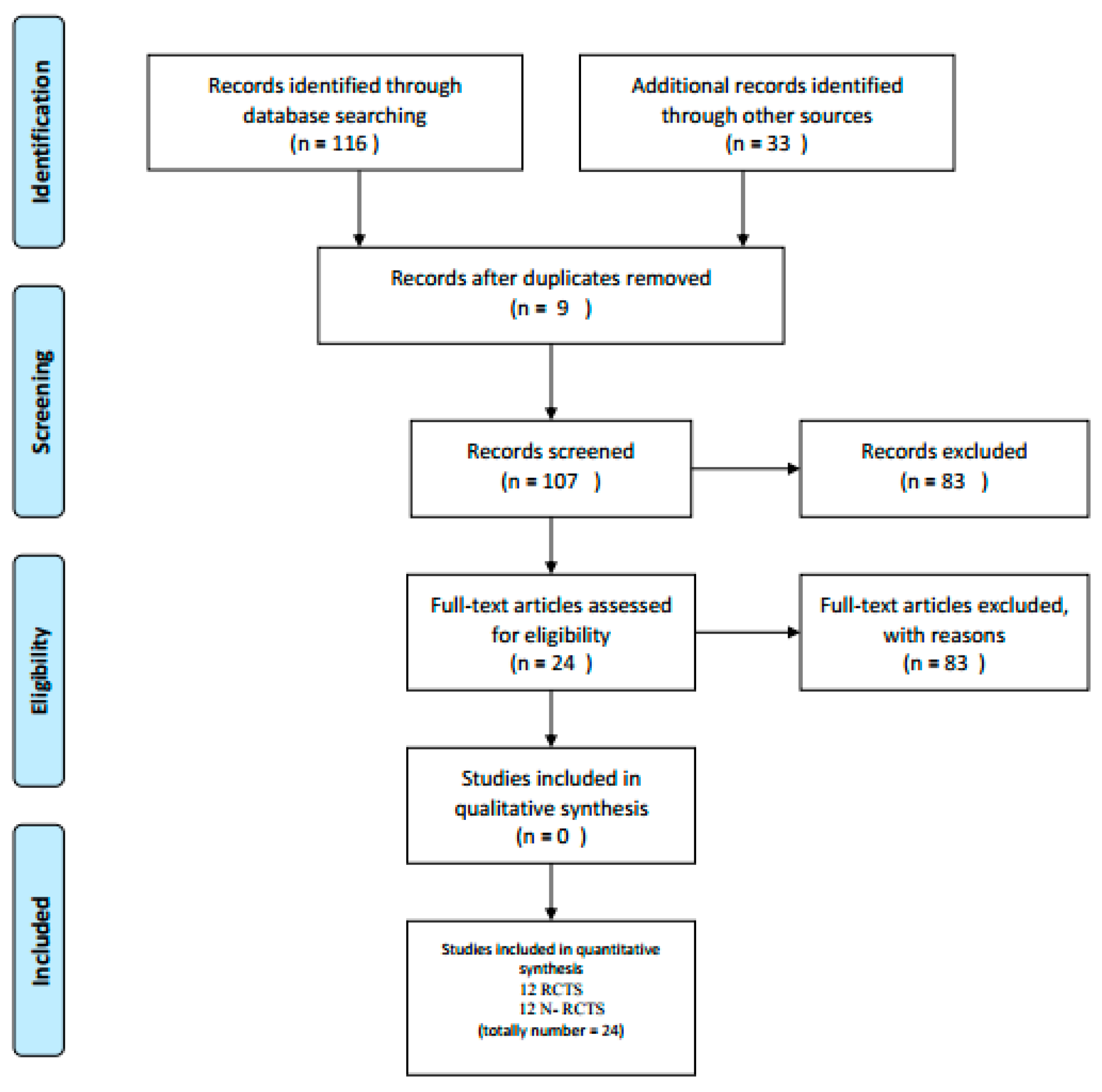
2. Materials and Methods
2.1. Participants
2.2. Procedure
- studies described SIPs in people with ID;
- cross-sectional, cohort, experimental, and quasi-experimental;
- peer-reviewed studies;
- people with ID aged between the ages of 6 and 60.
- studies were not published in the English language;
- studies were published before 1998;
- studies were not peer-reviewed;
- qualitative studies;
- grey literature, e.g., dissertations, conference abstracts, research reports, chapter(s) from a book, Ph.D. theses, reports on ID guidelines.
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ogg-Groenendaal, M.; Hermans, H.; Claessens, B. A systematic review on the effect of exercise interventions on challenging behavior for people with intellectual disabilities. Res. Dev. Disabil. 2014, 35, 1507–1517. [Google Scholar] [CrossRef] [PubMed]
- Mastebroek, M.; Naaldenberg, J.; Lagro-Janssen, A.L.; Van Schrojenstein Lantman de Valk, H. Health information exchange in general practice care for people with intellectual disabilities—A qualitative review of the literature. Res. Dev. Disabil. 2014, 35, 1978–1987. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, S.J.; McGrane, B.; Sanders, G.; Taylor, S.; Owen, M. A non-equivalent group pilot trial of a school-based physical activity and fitness intervention for 10–11 year oldenglish children: Born to move. BMC Public Health 2016, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- McGarty, A.M.; Downs, S.J.; Melville, C.A.; Harris, L. A systematic review and meta-analysis of interventions to increase physical activity in children and adolescents with intellectual disabilities. J. Intellect. Disabil. Res. 2017, 62, 312–329. [Google Scholar] [CrossRef] [PubMed]
- Alesi, M.; Battaglia, G.; Roccella, M.; Testa, D.; Palma, A.; Pepi, A. Improvement of gross motor and cognitive abilities by an exercise training program: Three case reports. Neuropsychiatr. Dis. Treat. 2014, 10, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Kahn, E.B.; Ramsey, L.T.; Brownson, R.C.; Heath, G.W.; Howze, E.H.; Powell, K.E.; Stone, E.J.; Rajab, M.W.; Corso, P. The effectiveness of interventions to increase physical activity a systematic review. Am. J. Prev. Med. 2002, 22, 72–107. [Google Scholar] [CrossRef]
- Bailey, R. Evaluating the relationship between physical education, sport and social inclusion. Educ. Res. Rev. 2005, 57, 71–90. [Google Scholar] [CrossRef]
- Allender, S.; Cowburn, G.; Foster, C. Understanding participation in sport and physical activity among children and adults: A review of qualitative studies. Health Educ. Res. Theory Pract. 2006, 21, 826–835. [Google Scholar] [CrossRef]
- Marcus, B.H.; Williams, D.M.; Dubbert, P.M.; Sallis, J.F.; King, A.C.; Yancey, A.K.; Franklin, B.A.; Buchner, D.; Daniels, S.R.; Claytor, R.P.; et al. Physical activity intervention studies: What we know and what we need to know a scientific statement from the american heart association council on nutrition, physical activity, and metabolism (subcommittee on physical activity); council on cardiovascular disease in the young; and the interdisciplinary working group on quality of care and outcomes research. Circulation 2006, 114, 273–2752. [Google Scholar] [CrossRef]
- Murphy, N.A.; Carbone, P.S.; Council on Children with Disabilities. Promoting the participation of children with disabilities in sports, recreation, and physical activities. Am. Acad. Ped. 2008, 121, 1057–1061. [Google Scholar] [CrossRef]
- Bodde, A.E.; Seo, D.C. A review of social and environmental barriers to physical activity for adults with intellectual disabilities. Disabil. Health J. 2009, 2, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Heath, G.W.; Parra, D.C.; Sarmiento, O.L.; Andersen, L.B.; Owen, N.; Goenka, S. Evidence-based intervention in physical activity: Lessons from around the world. Phys. Act. 2012, 3, 272–281. [Google Scholar] [CrossRef]
- Dairo, Y.M.; Collett, J.; Dawes, H.; Oskrochi, G.R. Physical activity levels in adults with intellectual disabilities: A systematic review. Prev. Med. Rep. 2016, 4, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Chow, B.C.; Wendy, Y.J.; Huang, W.Y.J.; Choi, P.H.N.; Pan, C.-Y. Design and methods of a multi-component physical activity program for adults with intellectual disabilities living in group homes. J. Exerc. Sci. Fit. 2016, 14, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Andriolo, R.B.; El Dib, R.P.; Ramos, L.; Atallah, Á.N.; da Silva, E.M.K. Aerobic exercise training programmes for improving physical and psychosocial health in adults with Down Syndrome. Cochrane Database Syst. Rev. 2011, 12. [Google Scholar] [CrossRef]
- Grondhuis, S.N.; Aman, M.G. Overweight and obesity in youth with developmental disabilities: A call to action. J. Intellect. Disabil. Res. 2014, 58, 787–799. [Google Scholar] [CrossRef]
- Bota, A.; Teodorescu, S.; Kiss, K.; Stoicoviciu, A. Fitness status in subjects with intellectual disabilities: A comparative studies. Proc. Soc. Behav. Sci. 2012, 46, 2078–2082. [Google Scholar] [CrossRef]
- Lina, J.D.; Lin, P.Y.; Lin, L.P.; Chang, Y.Y.; Ru Wu, S.; Wu, J.L. Physical activity and its determinants among adolescents with intellectual disabilities. Res. Dev. Disabil. 2009, 31, 263–269. [Google Scholar] [CrossRef]
- Rimmer, J.H.; Chen, M.D.; McCubbin, J.A.; Drum, C.; Peterson, J. Exercise intervention research on persons with disabilities: What we know and where we need to go. Am. J. Phys. Med. Rehabil. 2010, 89, 249–263. [Google Scholar] [CrossRef]
- Adams, D. Sports-Based intervention as a tool for social inclusion? Seameo sen icse. In Proceedings of the 2nd International Conference on Special Education: Access and Engagemen, Sarawak, Malaysia, 31 July–2 August 2017; Institute of Educational Leadership, University of Malaya: Sarawak, Malaysia, 2017. [Google Scholar]
- Howie, E.H.; Pate, R.R. Physical activity and academic achievement in children: A historical perspective. J. Sport Health Sci. 2012, 1, 160–169. [Google Scholar] [CrossRef]
- Simplican, S.C.; Leader, G.; Kosciulek, J.; Leahy, M. Defining social inclusion of people with intellectual and developmental disabilities: An ecological model of social networks and community participation. Res. Dev. Disabil. 2015, 38, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Rafferty, R.; Breslin, G.; Brennan, D.; Hassan, D. A systematic review of school-based physical activity interventions on children’s wellbeing. Int. Rev. Sport Exerc. Psychol. 2016, 9, 215–230. [Google Scholar] [CrossRef]
- Tercedor, P.; Villa-González, E.; Ávila-García, M.; Díaz-Piedra, C.; Martínez-Baena, A.; Soriano-Maldonado, A. A school-based physical activity promotion intervention in children: Rationale and study protocol for the previne project. BMC Public Health 2017, 17, 748. [Google Scholar] [CrossRef] [PubMed]
- D’isanto, T.; Di Tore, P.A. Physical activity and social inclusion at school: A paradigm change. J. Phys. Educ. Sport 2016, 16, 109–1102. [Google Scholar]
- Spieth, P.M.; Kubasch, A.S.; Penzlin, A.I.; Illigens, B.M.; Barlinn, K.; Siepmann, T. Randomized controlled trials—A matter of design. Neuropsych. Dis. Treat. 2016, 12, 1341–1349. [Google Scholar] [CrossRef]
- Raudenbush, S.W. On randomized experimentation in education: A commentary on deaton and cartwright, in honor of frederick mosteller. Soc. Sci. Med. 2018, 210, 63–66. [Google Scholar] [CrossRef] [PubMed]
- Funk, M. Physical Activity Interventions for Children with Down Syndrome: A Synthesis of the Research Literature. In Kinesiology Sport Studies, and Physical Education Synthesis Projects; 2017; Volume 32, Available online: https://digitalcommons.brockport.edu/pes_synthesis/32 (accessed on 30 December 2017).
- Verschuren, O.; Ketelaar, M.; Gorter, J.W.; Helders, P.J.M.; Uiterwaal, C.S.P.M.; Takken, T. Exercise training program in children and adolescents with cerebral palsy: A randomized controlled trial. Arch. Pediatr. Adolesc. Med. 2007, 161, 1075–1081. [Google Scholar] [CrossRef]
- Chu, C.H.; Pan, C.Y. The effect of peer- and sibling-assisted aquatic program on interaction behaviors and aquatic skills of children with autism spectrum disorders and their peers/siblings. Res. Autism Spect. Disor. 2012, 6, 1211–1223. [Google Scholar] [CrossRef]
- Inoue, C.; Forneris, T. The role of special olympics in promoting social inclusion: An examination of stakeholder perceptions. J. Sport Dev. 2015, 3, 23–34. [Google Scholar]
- Thorn, S.H.; Pittman, A.; Myers, R.E.; Slaughter, C. Increasing community integration and inclusion for people with intellectual disabilities. Res. Dev. Disabil. 2009, 30, 891–901. [Google Scholar] [CrossRef]
- Siperstein, G.N.; Glick, G.C.; Parker, R.C. Social inclusion of children with intellectual disabilities in a recreational setting. Intellect. Dev. Disabil. 2009, 47, 97–107. [Google Scholar] [CrossRef]
- Hall, S.A. The Social Inclusion of Young Adults with Intellectual Disabilities: A Phenomenology of Their Experiences. Ph.D. Thesis, University of Nebraska, Lincoln, NE, Canada, 2010; p. 18. Available online: http://digitalcommons.unl.edu/cehsedaddiss/18 (accessed on 30 December 2010).
- Grandisson, M.; Te´treault, S.; Freeman, A.R. Enabling integration in sports for adolescents with intellectual disabilities. J. Appl. Res. Intellec. Disabil. 2012, 25, 217–230. [Google Scholar] [CrossRef] [PubMed]
- McConkey, R.; Dowling, S.; Hassan, S.; Menke, S. Promoting social inclusion through Unified Sports for youth with intellectual disabilities: A five-nation study. J. Intellect. Disabil. Res. 2012, 57, 923–935. [Google Scholar] [CrossRef] [PubMed]
- Humphrey, N.; Lendrum, A.; Barlow, A.; Wigelsworth, M.; Squires, G. Achievement for all: Improving psychosocial outcomes for students with special educational needs and disabilities. Res. Dev. Disabil. 2013, 34, 1210–1225. [Google Scholar] [CrossRef] [PubMed]
- Lante, K.; Stancliffe, R.J.; Bauman, A.; Van der Ploeg, H.P.; Jan, S.; Davis, G.M. Embedding sustainable physical activities into the everyday lives of adults with intellectual disabilities: A randomised controlled trial. BMC Public Health 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Shields, N.; Synnot, A. Perceived barriers and facilitators toparticipation in physical activity for children with disability: A qualitative study. BMC Pediatr. 2016, 16, 1–10. [Google Scholar] [CrossRef]
- Slaman, J.; Roebroeck, M.E.; Van Meeteren, J.; van der Slot, W.M.; Reinders- Messelink, H.A.; Lindeman, E.; Stam, H.J.; van den Berg-Emons, R.J. 2 Move 16-24: Effectiveness of an intervention to stimulate physical activity and improve physical fitness of adolescents and young adults with spastic cerebral palsy; a randomized controlled trial. BMC Pediatr. 2010, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Alesi, M. Investigating Parental Beliefs Concerning Facilitators and Barriers to the Physical Activity in Down Syndrome and Typical Development. SAGE Open 2017, 7. [Google Scholar] [CrossRef]
- Koller, D.; Pouesard, M.L.; Rummens, J.A. Defining social inclusion for children with disabilities: A critical literature review. Child. Soc. 2018, 32, 1–13. [Google Scholar] [CrossRef]
- Lai, B.; Young, H.J.; Bickel, C.S.; Motl, R.W.; Rimmer, J.H. Current trends in exercise intervention research, rechnology, and behavioral change ctrategies for people with disabilities: A scoping review. Am. J. Phys. Med. Rehab. 2017, 96, 748–761. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A. The prisma statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epid. 2009, 62, 1–34. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for Systematic reviews and meta-analyses: The prisma statement. PLoS Med. 2009, 6. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kmet, L.; Lee, R.; Cook, L. Standard Quality Assessment Criteria for Evacuatig Primary Research Papers from a Variety of Felds, 2nd ed.; Alberta Heritage Foundation for Medical Research: Edmonton, AB, Canada, 2004. [Google Scholar]
- Abbott, J.H. The distinction between randomized clinical trials (RCTs) and preliminary feasibility and pilot studies: What they are and are not. J. Orthop. Sports. Phys. Ther. 2014, 44, 555–558. [Google Scholar] [CrossRef] [PubMed]
- Melville, C.A.; Mitchell, F.; Stalker, K.; Matthews, L.; McConnachie, A.; Murray, H.M.; Mutrie, N. Effectiveness of a walking programme to support adults with intellectual disabilities to increase physical activity: Walk well cluster-randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2015, 12. [Google Scholar] [CrossRef] [PubMed]
- Elinder, L.S.; Bergström, H.; Hagberg, J.; Wihlman, U.; Hagströmer, M. Promoting a healthy diet and physical activity in adults with intellectual disabilities living in community residences: Design and evaluation of a cluster-randomized intervention. BMC Public Health 2010, 10, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, E.; Glidden, L.M. Changing attitudes toward disabilities through unified sports. Intellect. Dev. Disabil. 2014, 52, 367–378. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, F.; Melville, C.; Stalker, K.; Matthews, L.; McConnachie, A.; Murray, H.; Walker, A.; Mutrie, N. Walk well: A randomised controlled trial of a walking intervention for adults with intellectual disabilities: Study protocol. BMC Public Health 2013, 13, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Slaman, J.; Roebroeck, M.; Dallmijer, A.; Twisk, J.; Stam, H.; Van Den Berg-Emons, R.; Learn 2 Move Research Group. Can a lifestyle intervention programme improve physical behaviour among adolescents and young adults with spastic cerebral palsy? A randomized controlled trial. Dev. Child Neurol. 2014, 57, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Matthews, L.; Mitchell, F.; Stalker, K.; McConnachie, A.; Murray, H.; Melling, C.; Mutrie, N.; Melville, C. Process evaluation of the walk well study: A cluster-randomised controlled trial of a community based walking programme for adults with intellectual disabilities. BMC Public Health 2016, 16. [Google Scholar] [CrossRef] [PubMed]
- Blick, R.N.; Saad, A.E.; Goreczny, A.J.; Roman, K.; Sorensen, C.H. Effects of declared levels of physical activity on quality of life of individuals with intellectual disabilities. Res. Dev. Disabil. 2015, 37, 223–229. [Google Scholar] [CrossRef]
- Carmeli, E.; Zinger-Vaknin, T.; Morad, M.; Merrick, J. Can physical training have anaffecton well-being in adults with mild intellectual disability? Mech. Ageing Dev. 2005, 126, 299–304. [Google Scholar] [CrossRef]
- Carraro, A.; Gobbi, E. Effects of an exercise programme on anxiety in adults with intellectual disabilities. Res. Dev. Disabil. 2012, 33, 1221–1226. [Google Scholar] [CrossRef] [PubMed]
- Heller, T.; Hsieh, K.; Rimmer, J.H. Attitudinal and psychosocial outcomes of a fitness and health education program on adults with down syndrome. Am. J. Ment. Retard. 2004, 109, 175–185. [Google Scholar] [CrossRef]
- Fragala-Pinkham, M.; O’Neil, M.E.; Haley, S.M. Summative evaluation of a pilot aquatic exercise program for children with disabilities. Disabil. Health J. 2010, 3, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.Y. The efficacy of an aquatic program on physical fitness and aquatic skills in children with and without autism spectrum disorders. Res. Autism Spect. Disor. 2011, 5, 657–665. [Google Scholar] [CrossRef]
- Yanardag, M.; Erkan, M.; Yılmaz, I.; Arıcan, E.; Düzkantar, A. Teaching advance movement exploration skills in water to children with autism spectrum disorders. Res. Autism Spect. Dis. 2015, 9, 121–129. [Google Scholar] [CrossRef]
- Chen, M.D.; Tsai, H.Y.; Wang, C.C.; Wuang, Y.P. The effectiveness of racket-sport intervention on visual perception and executive functions in children with mild intellectual disabilities and borderline intellectual functioning. Neuropsychiatr. Dis. Treat. 2015, 11, 2287–2297. [Google Scholar] [CrossRef]
- Shields, N.; Taylor, N.F.; Dodd, K.J. Effects of a Community-Based Progressive Resistance Training Program on Muscle Performance and Physical Function in Adults With Down Syndrome: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2008, 89, 1215–1220. [Google Scholar] [CrossRef]
- Wely, L.V.; Becher, J.G.; Reinders-Messelink, H.R.; Lindeman, E.; Verschuren, O.; Verheijden, J.; Dallmeijer, A.J. Learn 2 move 7-12 years: A randomizedcontrolled trial on the effects of a physical activity stimulation program in children with cerebral palsy. BMC Pediatric 2010, 10, 1–10. [Google Scholar] [CrossRef]
- Ulrich, D.A.; Burghardt, A.R.; Lloyd, M.; Tiernan, C.; Hornyak, J.E. Physical Activity Benefits of Learning to Ride a Two-Wheel Bicycle for Children With Down Syndrome: A Randomized Trial. Phys. Ther. 2011, 10, 1463–1477. [Google Scholar] [CrossRef] [PubMed]
- Sackett, D.L. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest 1989, 95, 2S–4S. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability, and Healt: ICF; World Health Organization: Geneva, Switzerland, 2001; Available online: http://www.who.int/classifications/icf/en (accessed on 30 December 2017).
| Reference Title Country | Source Author Year | Study Population Age Sample Size | Aim of the Study | Intervention Program | Outcome Measures | Results and Discussion Main Issues | Quality Assessment |
|---|---|---|---|---|---|---|---|
| Effects of a Community-Based Progressive Resistance Training Program on Muscle Performance and Physical Function in Adults With Down syndrome: A Randomized Controlled Trial (USA) | Shields, Taylor & Dodd (2008) | Adults with Down syndrome (DS; N = 20) (13 men, 7 women; mean age: 26.9). Intervention group, N = 9; control group, N = 11. | To determine whether progressive resistance training improves muscle strength, muscle endurance, and physical functioning. | The intervention was organized in a supervised group progressive resistance training program with six exercises using weight machines. It was delivered twice a week for 10 weeks. All participants completed 2 to 3 sets of between 10 to 12 repetitions of each exercise until they reached fatigue. | Outcome measures were: aerobic and anaerobic capacity, agility, muscle strength, body mass index, self-perception, gross motor function, participation, and health-related quality of life (HRQOL). | The results suggest that strength training carried forward in a community setting is important for adults with DS. | 63.3% |
| LEARN 2 MOVE 7–12 years: A randomized controlled trial on the effects of a physical activitystimulation program in children with cerebral palsy (The Netherlands) | Van Wely et al. (2010) | Children with spastic cerebral palsy (CP; N = 50), aged between 7 and 12 years. | To verify the efficacy of an intervention to improve physical activity (PA) by lifestyle intervention and a fitness training program (LEARN 2 MOVE 7–12). | The intervention program consisted of a 6-month physical activity and active lifestyle stimulation program associated to a 4-month fitness training program. Assessment measures were collected before the start of the intervention (T0), after the 4-month fitness training program (T4), after the 6-month lifestyle intervention (T6), and after six months of follow-up (T12). | Primary outcome of this study was physical activity. Secondary outcome measures were fitness, capacity of mobility, social participation, and HRQOL. | The results suggest that it is important for the children to maintain an active lifestyle, especially if they have better levels of fitness and to continue more physical activities in their own environment. | 72.4% |
| Learn 2 Move 16–24: effectiveness of an intervention to stimulate physical activity and improve physical fitness of adolescents and young adults with spastic cerebral palsy; a randomized controlled trial (The Netherlands) | Slaman et al. (2010) | Adolescents and young adults with spastic CP (N = 60), aged between 16 and 24 years. | To verify the efficacy of an intervention to improve PA by lifestyle intervention and a fitness training program (LEARN 2 MOVE 16–24). | The intervention consisted of a 6-month program articulated in three parts: (1) counselling consisted of daily PA; (2) physical fitness training; (3) sports advice. | Outcome measures were: (1) accelerometry-based activity for measured PA level; (2) aerobic fitness; (3) neuromuscular fitness; and (4) body composition parameters determined by measuring body mass, height, waist circumference, fat mass, and lipid profile. | The results suggest that PA level can improve the fitness level of adolescents and young adults with CP by promoting a behavioral change toward a more active lifestyle. | 55.6% |
| Promoting a healthy diet and physical activity in adults with intellectual disabilities living in community residences: Design and evaluation of a cluster-randomized intervention (Sweden) | Schäfer Elinder et al. (2010) | Adults with mild-to-moderate intellectual disability (ID; N = 500) aged over 18 years. | To verify the validity of a health intervention to improve diet and PA in adult age. | The intervention program was organized in three parts in 12–15 months; (1) 10 health education sessions for residents in their homes; (2) meeting with a health ambassador among the staff in each residence and the formation of a network; (3) a study circle for staff. | Outcome measures: physical activity and health measures. | The results show that that people with ID are in need of professional care, but also have the basic right to autonomy and self-determination. | 46% |
| Aerobic exercise training programmes for improving physical and psychosocial health in adults with Down syndrome (Brazil) | Andriolo et al. (2011) | Adults with Down syndrome (N = 63) aged 18 years or above. | To verify the efficacy of aerobic exercise training programmed for physiological and psychosocial outcomes in adults with Down syndrome. | The intervention was an exercise training programme consisting of aerobic exercise with dynamic activities using large muscle groups. Moreover, additional instructions in health education or health awareness were given. The intervention was delivered at least three times each week for a minimum period of four weeks. | Outcome measures were: only standardized/validated scales or instruments. | No significant results were found for type of intervention (rowing vs. walking), for duration (10 vs. 16 weeks), or methods of monitoring intensity. | 59% |
| Physical Activity Benefits of Learning to Ride a Two-Wheel Bicycle for Children With Down Syndrome: A Randomized Trial (USA) | Ulrich et al. (2011) | Children with DS (N = 27) aged between 8 and 15 years. | To investigate the effectiveness of a riding 2-wheel bicycle intervention program to increase PA and health-related outcomes in people with DS. | The intervention was an exercise training programme consisting of a bicycle intervention. Assessment measures were collected in the month before the intervention (pre-intervention), at 7 weeks after the intervention, and at 12 months after the pre-intervention. | Outcome measures were: leg strength and balance, anthropometric parameters (height and weight), skinfolds, and physical activity (time spent in sedentary and moderate to vigorous activity). | The results suggest that the participants who learned to ride spent significantly less time in sedentary activity at 12 months after the preintervention measurement and more time in moderate-to-vigorous physical activity than participants in the control group. | 61.1% |
| Walk well: a randomised controlled trial of a walking intervention for adults with intellectual disabilities: study protocol (Scotland) | Mitchell et al. (2013) | Adults with ID (N = 40), aged over 18 years. | To evaluate the effectiveness of walking interventions (Walk Well intervention) impact on PA levels, health, and wellbeing in adults and older adults with ID. | The intervention consisted of three PA consultations and an individualized 12-week walking programme. Assessment measures were collected at baseline, post intervention (three months from baseline), and at follow-up (three months post intervention and six months from baseline). | The outcome measures were physical activities such as dance, swimming, and martial arts, and their improvement of participation, functioning, and health-related outcomes. | A significant increase was found in walking for participants who undertook the PA consultations and individualised walking programme. | 67% |
| Can a lifestyle intervention programme improve physical behaviour among adolescents and young adults with spastic cerebral palsy? A randomized controlled trial (The Netherlands) | Slaman et al. (2014) | Adults with spastic CP (N = 57), aged between 16 and 25 years. | To evaluate the effectiveness of a lifestyle intervention programme on physical behavior in persons with CP. | The intervention consisted of a 6-month lifestyle programme consisting of fitness training and counselling on physical behaviour and sports participation. | Outcome measures of physical behaviours were objectively measured using ambulatory activity monitors. Self-reported PA was measured using the Physical Activity Scale for Individuals with Physical Disabilities. | The results suggest that the intervention did not affect the objectively measured PA during the intervention or at follow-up in adolescents and young adults with spastic CP. | 48.5% |
| Changing Attitudes Toward Disabilities Through Unified Sports (USA) | Sullivan et al. (2014) | Adults with ID (N = 16), aged between 17 and 21 years. | To examine the efficacy of a unified swimming program to: 1. result in more positive attitudes of persons without disabilities towards persons with ID; 2. Positively affect persons without disabilities; 3. Positively affect persons with ID. | The intervention consisted of four sessions over a 6-week program period involving swimming activities. | Outcome measures were related to the shared objective of arriving at a common outcome serving as a powerful force to motivate working together, creating cooperative interdependence, and facilitating positive attitude change. | The results suggest that on a revision attitudes inventory, the intervention group participants displayed significant increases in positive attitudes from pre- to post-test, whereas the control group participants did not. | 47.4% |
| Embedding sustainable physical activities into the everyday lives of adults with intellectual disabilities: A randomised controlled trial (Australia) | Lante et al. (2014) | Adults with ID (N = 90) aged between 18 and 55. Three groups: (1) a lifestyle physical activity group (N = 30); (2) a structured exercise group (N = 30); (3) a usual care control group (N = 30). | To compare two approaches to increase short-term (3-month) and long-term (9-month) PA outcomes in adults with ID: a lifestyle physical activity (light–moderate intensity, LMI) approach versus a structured exercise (moderate–vigorous intensity, MVI) approach. | The intervention (LMI—Lifestyle intervention physical activity or a structured MVI—Exercise group) consisted of a 12-week programme delivered by exercise specialists in the community with disability service staff, after which intervention continued for 6 months, delivered by disability service staff only. | Primary outcomes were aerobic fitness, 12-h energy expenditure, and proxy-reported everyday physical activity. Secondary outcomes were objectively assessed physical activity and sedentary behaviour, intervention compliance, functional walking capacity, participation in domestic activities, muscle strength, body composition, psychosocial outcomes, quality of life, and health care costs. | The results suggest the effectiveness and sustainability of the two approaches in increasing physical activity and exercise among adults with ID. | 56% |
| Effectiveness of a walking programme to support adults with intellectual disabilities to increase physical activity: Walk Well cluster-randomised controlled trial (Scotland) | Melville et al. (2015) | Adults with ID (N = 102) aged over 18 years. | To verify the efficacy of a behavior change programme to increase walking and reduce sedentary behaviors in adults with ID. | Walk Well was a 12-week intervention programme consisting of three face-to-face PA consultations based on behaviour change techniques, written resources for participants and carers, and an individualised, structured walking programme. | The primary outcome measure was the mean step count per day between baseline and 12 weeks, evaluated with accelerometers. Secondary outcome measures were percentage time per day spent sedentary and in moderate–vigorous physical activity (MVPA), body mass index (BMI), and subjective well being. | The results suggest that this is the first published trial of a walking program for adults with intellectual disabilities with a positive effect. | 51% |
| Process evaluation of the Walk Well study: a cluster-randomised controlled trial of a community based walking programme for adults with intellectual disabilities (Scotland) | Matthews et al. (2016) | Adults with ID (N = 102) aged over 18 years. | To evaluation the efficacy of a community-based walking intervention for adults with ID. | The Walk Well intervention of 12-week PA was a single-blind cluster-randomised controlled trial PA consultation-led walking intervention. The intervention group was delivered three PA consultations with a walking advisor at baseline, 6, and 12 weeks. | The outcome measures were change in daily step count at 12 weeks. Process evaluation used both qualitative interviews with stakeholders, quantifiable data collected during the intervention, and a qualitative interview with participants. | The results show that Walk Well was not effective in significantly increasing levels of physical activity. | 44% |
| Total: | 12 | papers |
| Reference Title and Country | Source Author Year | Study Population Age Sample Size | Aim of the Study | Intervention Program | Outcome Measures | Results and Discussion Main Issues | Quality Assessment |
|---|---|---|---|---|---|---|---|
| Attitudinal and Psychosocial Outcomes of a Fitness and Health Education Program on Adults With Down Syndrome (USA) | Heller et al. (2004) | Adults with Down syndrome (N = 53) aged 30 years and older. | To evaluate the effectiveness of a fitness and health education program to improve attitudinal and psychosocial outcomes in adults with Down syndrome. | The intervention program consisted of a 12-week, 3 days per week health promotion program lasting 2 h a day. In particular, a 1-h exercise class and 1-h health education component. | The outcome measures were attitudes towards exercise (cognitive–emotional barriers, outcomes expectations, and performance self-efficacy), and psychosocial well-being (community integration, depression, and life satisfaction). | The results suggest improved attitudes towards exercise, increased exercise self-efficacy, more positive expected outcomes, fewer cognitive–emotional barriers, higher life satisfaction, and lower depression. | 80.3% |
| Can physical training have an effect on well-being in adults with mild intellectual disability? (Israel) | Carmeli et al. (2005) | Adults with ID (N = 22) aged between 54 and 66 years. | To investigate the effectiveness of physical training in adult people with ID, particularly strength and physical/psychological well-being. | The intervention was focused on the improvement of muscle strength, and general exercises. The training program for the two groups was performed 3 days a week during six consecutive months. The physical training program took place three times a week for six months. | The outcome measures were: self-efficacy, confidence, life satisfaction. | The results suggest positive effects of physical activity on mental health and psychological well-being for adults aged 60 years and older. Moreover, the results suggest the important role of physical training to enhance locomotor performance and perception of well-being among “older” adults with ID. | 66% |
| Physical activity and its determinants among adolescents with intellectual disabilities (Taiwan) | Lina et al. (2009) | Adolescents with ID (N = 351) aged between 16 and 18 years. | To describe the regular PA prevalence and examine its determinants among adolescents with ID in Taiwan. | The intervention program involved the people with ID that had regular physical activity habits. The physical activities included were walking, sports, and jogging at least exercise three times per week, 30 min per time. | The outcome measures were the physical education class in school, involving outdoor activities such as walking, jogging, sports, cycling, swimming, and dancing. | The results suggest the need to sustain sport motivation to participate in PA for people with ID in order to increase the positive effects of PA on this population. | 42.1% |
| Summative evaluation of a pilot aquatic exercise program for children with disabilities (USA) | Fragala-Pinkham et al. (2010) | Child participants with a variety of diagnoses (N = 16): autism spectrum disorders (ASDs; N = 6), cerebral palsyespastic diplegia (N = 1) and hemiplegia (N = 1), Down syndrome (N = 2), myelomeningocele with the lesion at the lumbar spine level (L4–5) (N = 1) and the sacral level (S1–2) (N = 1), developmental delay (N = 2), nonverbal learning disorder (N = 1), and oto-palatal-digital syndrome (N = 1). | To evaluate the efficacy of a pilot aquatic exercise program in children with disabilities. | The aquatic exercise consisted of a program warm-up (3–5 min), aerobic conditioning (20–30 min), strengthening exercises (5–10 min), and cool-down (3–5 min), 2 times per week for 14 weeks. The pool sessions lasted about 45 min. | The outcome measures were cardiorespiratory endurance, strength, functional mobility, and safety. | The results suggest that the children improved their swimming skills by increasing their PA levels during the program and maintaining this six months after the program ended. | 56.3% |
| The efficacy of an aquatic program on physical fitness and aquatic skills in children with and without autism spectrum disorders (Taiwan) | Pan (2011) | Children with ASD (N = 15) and their siblings (N = 15) aged between 7 and 12 years. | To evaluate, in children with ASD and their siblings without a disability, the effectiveness of an aquatic program on physical fitness and aquatic skills. | The intervention program was organized in 32 weeks, with 14 weeks aquatic program, 14 weeks control, and 4 weeks assessment and transition. In the first phase over 14 weeks, 14 children (group A: ASD, n = 7; siblings, n = 7) received the aquatic program, while 16 children (group B: ASD, n = 8; siblings, n = 8) did not. The second phase lasted 14 weeks. | Outcome measures were aquatic skills and physical fitness components. | The results suggest that aquatic skills and physical fitness increased following the aquatic program. Moreover, the results highlight the need to develop and implement intervention programs to enhance motor skills and physical fitness components for children with ASD and their siblings. | 47.1% |
| Effects of an exercise programme on anxiety in adults with intellectual disabilities (Italy) | Carraro et al. (2012) | Adults with mild ID (N = 18) and moderate ID (N = 9) aged between 31 and 49 years. | To evaluate the efficacy of a short-term exercise programme on anxiety states in adults with ID. | The intervention program was organized into two 1-h sessions per week over 12 consecutive weeks. There were three phases: an initial warm-up, a central phase in which the main topic was developed, and a cool-down including group discussion and individual comments circle time technique. | The outcomes measures were flexibility, muscular endurance and strength, cardiorespiratory health and functional independence, and functional and musculoskeletal health, such as walking capacity. | The results suggest the crucial role of exercise in people with ID as a strategy to promote mental health and wellbeing. | 77% |
| The effect of peer- and sibling-assisted aquatic program on interaction behaviors and aquatic skills of children with autism spectrum disorders and their peers/siblings (Taiwan) | Chu et al. (2012) | Children with ASD (N = 21) aged between 7 and 12 years old. | To evaluate the efficacy of an aquatic program in children with autism spectrum disorders (ASDs) to increase peer- and sibling-assisted learning on interaction behaviours and aquatic skills. | The intervention consisted of different times for each session. All participated in 16-week aquatic settings under three instructional conditions (teacher-directed, peer/sibling-assisted, and voluntary support). | The outcome measures were interaction behaviours and aquatic skills. | The results suggest that all children with ASD and their typical development (TD) peers/siblings significantly increased their aquatic skills after the program. The use of TD peer/sibling-assisted learning is a convenient instructional strategy. | 54.2% |
| Improvement of gross motor and cognitive abilities by an exercise training program: Three case reports (Italy) | Alesi et al. (2014) | Children with Down syndrome (N = 3) with chroological age of 10.3, 14.6, and 14 years, respectively and a mental age of less than 4 years. | To evaluate the effectiveness of an integrated exercise training program to improve motor and cognitive abilities in three children with Down syndrome. | The integrated exercise training program was distributed twice a week for a period of 2 months. This consisted of the following stages: a social interaction phase between child, coach, and parents (about 5 min) to enhance the motivation to participate; a warm-up period (~5 min); a central training period (~40 min) including two nursery rhyme games and several activities aimed at improving basic motor abilities such as running, jumping, throwing, and rolling; a cool-down period (~5 min); and a feedback phase (~5 min) to explore the child’s satisfaction level. | The outcome measures were chronological and mental age, body weight, height, gross motor skills, working memory, and attention skills. | The results suggest that in individuals with DS there is an important relation between motor and cognitive domains. For children and parents it is important to plan intervention programs based on the simultaneous involvement in order to promote an active lifestyle. | 77.2% |
| Effects of declared levels of physical activity on quality of life of individuals with intellectual disabilities (USA) | Blick et al. (2015) | Participants with ID (N = 788) aged between 11 and 92 years. | To evaluate the impact of physical fitness on quality of life by comparing sedentary individuals with ID and individuals with ID who reported frequently exercising, as more than 12 times per month. | The intervention consisted of physical activity for individuals with physical disabilities. The participants were organized in three groups based on frequency of exercise participation: never exercises (n = 335, 42.5%), exercises 1–11 times per month (n = 237, 30.1%), and exercises more than 11 times per month (n = 216, 27.4%). | The outcome measures were employment, the quality of interpersonal relationships and inclusion in community activities, satisfaction with services received, and choice and control over daily activities. | The results suggest that the physical fitness enhanced the health and psychosocial well-being of individuals with ID who maintained a physically active lifestyle compared to individuals who did not report exercising. Individuals with a regular exercise habit had more frequent outings into the community than did their sedentary peers. | 47% |
| Teaching advance movement exploration skills in water to children with autism spectrum disorders (Turkey) | Yanardag et al. (2015) | Children with ASD (N = 3) with chronological age of 6 years. | To evaluate the effectiveness of the “most to least” Prompting (MLP) program to improve the learning processes of advance movement exploration skills in water for children with ASD. | The intervention consisted of MLP exercises to teach three different aquatic skills, essential for movement exploration in water and swimming, in a one-to-one training format over three sessions per week. | The outcome measures were physical activity’s stimulation of the improvement of physical fitness, motor performance, self-esteem, behaviour, and social outcomes. | The results suggest MLP was effective in teaching advance movement exploration skills in water to children with ASD. It is an important enjoyable intervention and an appealing setting to improve leisure skills and PA level for children with ASD. | 64% |
| The effectiveness of racket-sport intervention on visual perception and executive functions in children with mild intellectual disabilities and borderline intellectual functioning (Taiwan) | Chen et al. (2015) | Children with ID (N = 91) aged 6–12 years. | To evaluate the effects of table tennis training (TTT) versus standard occupational therapy (SOT) on visual perception and executive functions in school-age children with mild ID and borderline intellectual functioning (BIF). | The SOT and TTT programs were administered 60 min per session, three times a week, for 16 weeks. | The outcome measures were racket sports. In particular, the correlation between improved visual–perceptual and executive functions and school function. | The results suggest contributing to the treatment of cognitive/perceptual problems in children with mild ID and BIF with table tennis, which is a good alternative therapy. | 71.2% |
| Design and methods of a multi-component physical activity program for adults with intellectual disabilities living in group homes (Taiwan) | Chow et al. (2016) | Adults with ID (N = 62) aged between 18 and 55 years. | To evaluate the efficacy of intervention program PA levels in adults with ID living in group homes through multi-component physical activity (PA). | Thirty exercise sessions were run in groups over a 10-week period and three educational lessons were given to increase self-efficacy and social support for PA. In addition, staff training in exercise and advice concerning PA policies were provided to the caregivers working in the group homes. | The outcome measures were physical fitness variables, physical activity measures, and psychosocial variables. In particular, measurements were taken at baseline (week 0), post-intervention (week 11), and at the 10-week follow-up. | The results suggest that in adults with ID, it is important to promote active lifestyles. | 64% |
| Total: | 12 | papers. |
| Criteria | Yes (2) | Partial (1) | No (0) | NS |
|---|---|---|---|---|
| 1 Question/objective sufficiently described? | X | |||
| 2 Study design evident and appropriate? | X | |||
| 3 Method of subject/comparison group selection or source of information/input variables described and appropriate? | X | |||
| 4 Subject (and comparison group, if applicable) characteristics sufficiently described? | X | |||
| 5 If interventional and random allocation was possible, was it described? | X | |||
| 6 If interventional and blinding of investigators was possible, was it reported? | X | |||
| 7 If interventional and blinding of subjects was possible, was it reported? | X | |||
| 8 Outcome and (if applicable) exposure measure(s) well-defined and robust to measurement/misclassification bias? Means of assessment reported? | X | |||
| 9 Sample size appropriate? | X | |||
| 10 Analytic methods described/justified and appropriate? | X | |||
| 11 Some estimate of variance is reported for the main results? | X | |||
| 12 Controlled for confounding? | X | |||
| 13 Results reported in sufficient detail? | X | |||
| 14 Conclusions supported by the results? | X |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scifo, L.; Chicau Borrego, C.; Monteiro, D.; Matosic, D.; Feka, K.; Bianco, A.; Alesi, M. Sport Intervention Programs (SIPs) to Improve Health and Social Inclusion in People with Intellectual Disabilities: A Systematic Review. J. Funct. Morphol. Kinesiol. 2019, 4, 57. https://doi.org/10.3390/jfmk4030057
Scifo L, Chicau Borrego C, Monteiro D, Matosic D, Feka K, Bianco A, Alesi M. Sport Intervention Programs (SIPs) to Improve Health and Social Inclusion in People with Intellectual Disabilities: A Systematic Review. Journal of Functional Morphology and Kinesiology. 2019; 4(3):57. https://doi.org/10.3390/jfmk4030057
Chicago/Turabian StyleScifo, Lidia, Carla Chicau Borrego, Diogo Monteiro, Doris Matosic, Kaltrina Feka, Antonino Bianco, and Marianna Alesi. 2019. "Sport Intervention Programs (SIPs) to Improve Health and Social Inclusion in People with Intellectual Disabilities: A Systematic Review" Journal of Functional Morphology and Kinesiology 4, no. 3: 57. https://doi.org/10.3390/jfmk4030057
APA StyleScifo, L., Chicau Borrego, C., Monteiro, D., Matosic, D., Feka, K., Bianco, A., & Alesi, M. (2019). Sport Intervention Programs (SIPs) to Improve Health and Social Inclusion in People with Intellectual Disabilities: A Systematic Review. Journal of Functional Morphology and Kinesiology, 4(3), 57. https://doi.org/10.3390/jfmk4030057







