A ‘Movement Screening Test’ of Functional Control Ability in Female Recreation Golfers and Non-Golfers over the Age of 80 Years: A Reliability Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Movement Screening Tests
2.4. Scoring System
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics
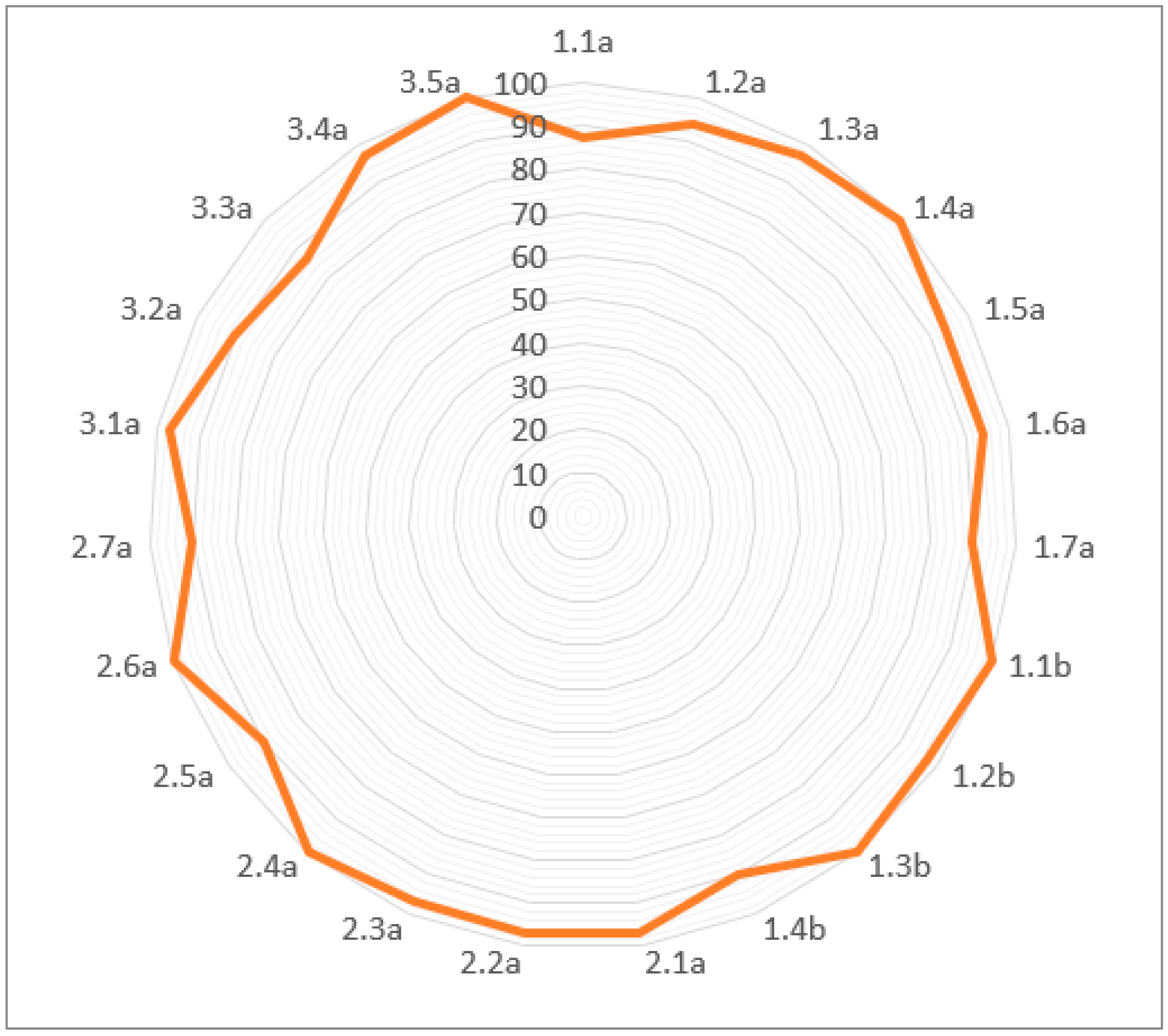
Percentage Agreements
3.2. Kappa Values
4. Discussion
Limitations and Future Recommendations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Movement Screen Test Instructions and Scoring System
| Test Details | Scoring Criteria |
|---|---|
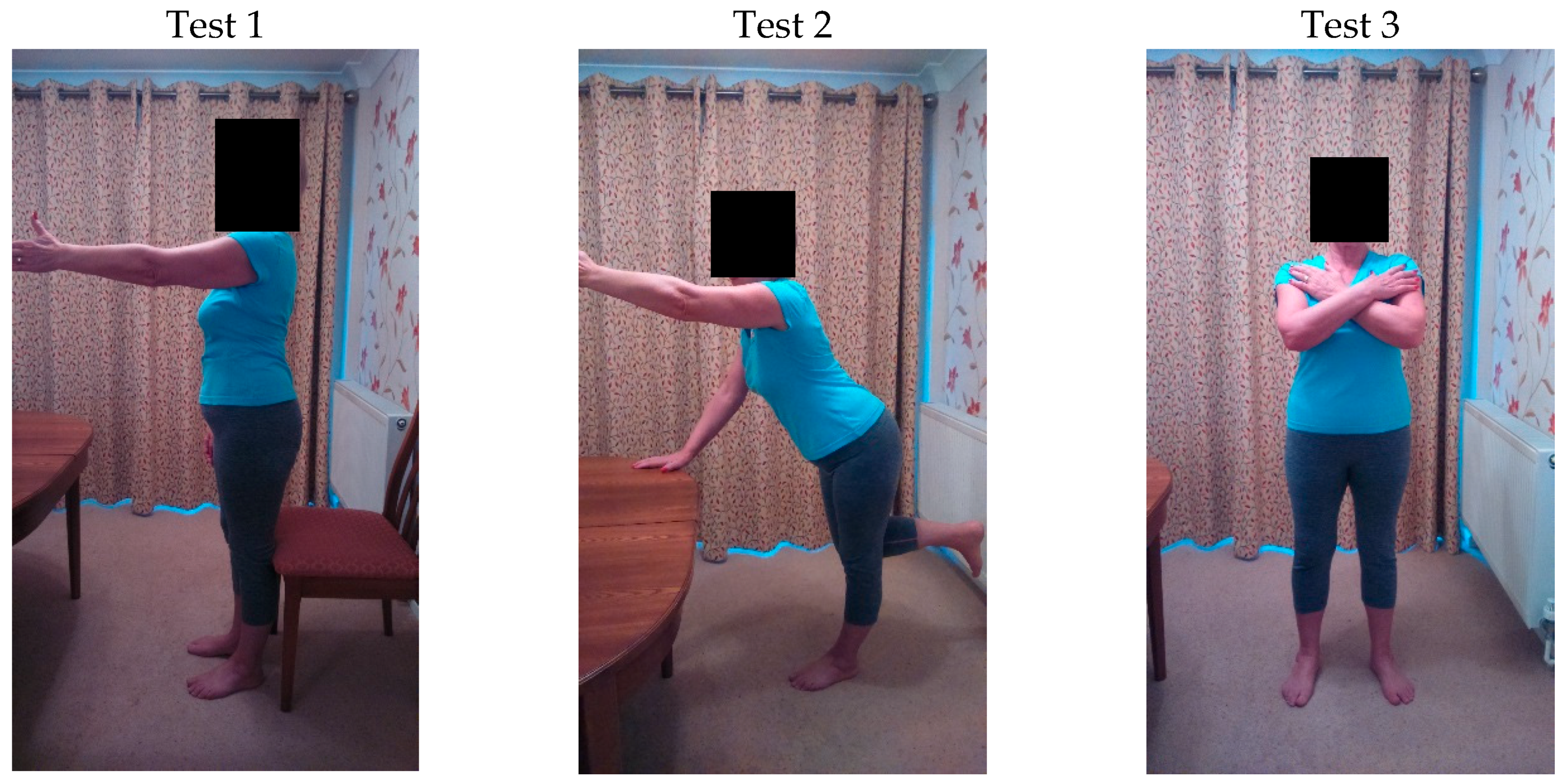
| Test 1a: Sit to stand with arm lift (Side View) Sitting with feet on the floor and spine straight, lean 30° forward at the hips. Then stand up keeping the knees out over the feet. Then, maintaining a neutral scapular position, lift the dominant arm to 90° shoulder flexion and lower back to the side. | 1: Can they keep the upper back straight and the collar bones up (the chest should not curl into flexion) during: the forward lean to a standing position? the horizontal arm lift and lower? 2: Can they keep the shoulders level and steady (prevent the shoulder hitching into elevation) during the horizontal arm lift? 3: Can they keep the shoulders level and steady (preventing the shoulder dropping down from the neutral position) during the arm lowering action? 4: Can they keep the thumb pointing towards the ceiling to control/prevent the shoulder from turning into medial rotation as the arm is lifted to horizontal? (the palm should be facing inwards) 5: Can they keep the low back straight (not rounding into flexion) during the forward trunk lean? 6: Can they keep the low back straight (not arching into extension) during: -the forward trunk lean? -the movement from sitting to standing? 7: Can they fully straighten at the hips when they stand up? (There should be a vertical line from the trunk through the legs. The trunk should not be leaning forwards or the hips pushed backwards) Total Score out of 7. |
| Test 1b: Sit to stand with arm lift (Front View) | 1: Can they keep the shoulders level and steady (control/prevent the shoulder blade hitching into elevation) during the horizontal arm lift? 2: Can they keep the shoulders level and steady (control/prevent the shoulder blade from dropping down from the neutral position) into depression during the arm lowering action? 3: Can they keep the thumb pointing towards the ceiling to control/prevent the shoulder from turning into medial rotation as the arm lifts to horizontal? (the palm should be facing inwards) 4: Can they keep the knees apart (over the feet, preventing the knees from collapsing in towards each other) during the sit-to-stand movement? Total Score out of 4. |
| Test 2: Trunk lean with knee bend and opposite arm lift. With hand support on a bench/table perform 45° forward trunk lean (independent hip flexion) + knee flexion to lift non-dominant foot off the floor and opposite arm lift to horizontal shoulder flexion. | 1: Can they control/prevent the head from dropping forward or lifting from their natural position during: -the trunk forward lean? -arm lifting and lowering? 2: Can they keep the shoulder and trunk steady on the weight-bearing arm? 3: Can they keep the non-weighting shoulder steady as the arm is lifted and reaches out? 4: Can they keep the thumb pointing towards the ceiling as the arm lifts to horizontal? (the palm should be facing inwards). 5: Can they keep the back straight and not let it round out into flexion during the forward lean? 6: Can they keep the back straight and not let it arch into extension? 7: Can they keep the pelvis from rotating (stay facing the front) during: -the foot lift? -the opposite arm lift? Total Score out of 7. |
| Test 3: Chest rotation with neutral head and pelvis. The range of upper body rotation should be 30° (using a line across the tips of the shoulders) towards the dominant side, without any head, pelvic, or leg movement Participants will perform a small knee bend and then rotate their trunk to 30° towards their dominant side. | 1: Can they keep the head facing forward and control/prevent the head from turning or rotating throughout the 30° of upper trunk rotation? 2: Can they keep their shoulders level and in a neutral mid position (prevent hitching into elevation) during trunk rotation? 3: Can they keep the pelvis facing the front and not allow it to rotate to follow the upper body (no rotation of the pelvis)? 4: Can they keep the knees apart and stationary during the chest turn? (no inward or outward movement of the knees across the line of the feet) 5: Can they keep the feet facing forward with the inside edges of the feet parallel and prevent the foot from turning in or out during the chest turn? Total Score out of 5. |
| Total of all test scores out of 23. | |
References
- World Health Organization World Health Day-Aging and Health. 2012. Available online: http://www.who.int/world-health-day/2012/toolkit/background/en/ (accessed on 16 November 2014).
- Reinhardt, U. Does the aging of the population really drive the demand for health care? Health Aff. 2003, 22, 27–39. [Google Scholar] [CrossRef]
- Tian, Y.; Thompson, J.; Buck, D.; Sonola, L. Exploring the System Wide Costs of Falls in Older People in Torbay. 2013. Available online: http://www.kingsfund.org.uk/publications/exploring-system-wide-costs-falls-older-people-torbay (accessed on 18 November 2014).
- Todd, C.; Skelton, D. What are the Main Risk Factors for Falls among Older People and What are the Most Effective Interventions to Prevent these Falls? Health Evidence Network Report; WHO Regional Office for Europe: Copenhagen, Denmark, 2004; Available online: www.euro.who.int/document/E82552.pdf (accessed on 15 November 2014).
- Rubenstein, L.; Josephen, K. The epidemiology of falls and syncope. Clin. Geriatr. Med. 2002, 18, 141–158. [Google Scholar] [CrossRef]
- Petrella, J.; Kim, J.; Tuggle, S.; Hall, S.; Bamman, M. Age differences in knee extension power, contractile velocity, and fatigability. J. Appl. Physiol. 2005, 98, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Granacher, U.; Gruber, M.; Gollhofer, A. Force production capacity and functional reflex activity in young and elderly men. Aging Clin. Exp. Res. 2010, 22, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Era, P.; Sainio, P.; Koskinen, S.; Haavisto, P.; Vaara, M.; Aromaa, A. Postural balance in a random sample of 7979 subjects aged 30 years and over. Gerontology 2006, 52, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Amiridis, I.; Hatzitaki, V.; Arabatzi, F. Age-induced modifications of static postural control in humans. Neurosci. Lett. 2003, 30, 137–140. [Google Scholar] [CrossRef]
- Laughton, C.; Slavin, M.; Katdare, K.; Nolan, L.; Bean, J.F.; Kerrigan, D.C.; Phillips, E.; Lipsitz, L.A.; Collins, J.J. Aging, muscle activity, and balance control: Physiologic changes associated with balance impairment. Gait Posture 2003, 18, 101–108. [Google Scholar] [CrossRef]
- Crombie, I.; Irvine, L.; Williams, B.; McGinnis, A.; Slane, P.; Alder, E.; McMurdo, M. Why older people do not participate in leisure time physical activity: A survey of activity levels, beliefs and deterrents. Age Aging 2004, 33, 287–292. [Google Scholar] [CrossRef] [PubMed]
- British Heart Foundation. Interpreting the UK Physical Activity Guidelines for Older Adults (65+). Available online: http://www.bhfactive.org.uk/userfiles/Documents/frailerolderadults.pdf (accessed on 18 November 2014).
- Skelton, D.A.; Young, A.; Walker, A.; Hoinville, E. Physical Activity in Later Life: Further Analysis of the Allied Dunbar National Fitness Survey and the HEASAH; Health Education Authority, The Stationary Office: London, UK, 1999; pp. 40–58. [Google Scholar]
- Jones, J.; Rikli, R. Measuring functional fitness of older adults. J. Act. Aging 2002, 2, 24–30. [Google Scholar]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [PubMed]
- Berg, K.O.; Wood-Dauphinee, S.L.; Williams, J.I.; Gayton, D. Measuring balance in elderly: Preliminary development of an instrument. Physiother. Can. 1989, 41, 304–311. [Google Scholar] [CrossRef]
- Duncan, P.; Studenski, S.; Chandler, J.; Prescott, B. Functional Reach: Predictive validity in a sample of elderly male veterans. J. Gerontol. 1992, 47, M93–M98. [Google Scholar] [CrossRef] [PubMed]
- Dingenen, B.; Blandford, l.; Comerford, M.; Staes, F.; Mottram, S. The assessment of movement health in clinical practice: A multidimensional perspective. Phys. Ther. Sport 2018, 32, 282–292. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.; Merom, D.; Bull, F.C.; Buchner, D.M.; Fiatarone Singh, M.A. Updating the Evidence for Physical Activity: Summative Reviews of the Epidemiological Evidence, Prevalence, and Interventions to Promote “Active Aging”. Gerontologist 2016, 56, S268–S280. [Google Scholar] [CrossRef] [PubMed]
- McNeill, W.; Blandford, L. Movement Health. J. Bodyw. Mov. Ther. 2015, 19, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Comerford, M.J.; Mottram, S.L. Kinetic Control: The Management of Uncontrolled Movement, 1st ed.; Elsevier: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Mischiati, C.; Comerford, M.; Gosford, E.; Swart, J.; Ewings, S.; Botha, N.; Stokes, M.; Mottram, S.L. Intra and Inter-Rater Reliability of Screening for Movement Impairments: Movement Control Tests from the Foundation Matrix. J. Sports Sci. Med. 2015, 14, 427–440. [Google Scholar] [PubMed]
- Rowsome, K.; Comerford, M.; Mottram, S.; Samuel, D.; Stokes, M. Movement Control Testing of Older People in Community Settings: Description of a Screening Tool and Intra-Rater Reliability; Working Papers in the Health Sciences; University of Southampton: Southampton, UK, 2016; Volume 1, pp. 1–12. Available online: https://www.southampton.ac.uk/wphs/current_issue.page (accessed on 27 April 2018).
- Brach, J.S.; Van Swearingen, J.M.; Perera, S.; Wert, D.M.; Studenski, S. Motor learning versus standard walking exercise in older adults with subclinical gait dysfunction: A randomized clinical trial. J. Am. Geriatr. Soc. 2013, 61, 1879–1886. [Google Scholar] [CrossRef] [PubMed]
- Brach, J.S.; Lowry, K.; Perera, S.; Hornvak, V.; Wert, D.M.; Studenski, S.; Van Swearingen, J.M. Improving motor control in walking: A randomized clinical trial in older adults with subclinical walking difficulty. Arch. Phys. Med. Rehabil. 2015, 96, 388–394. [Google Scholar] [CrossRef] [PubMed]
- VanSwearingen, J.M.; Studenski, S.A. Aging, motor skill, and the energy cost of walking: Implications for the prevention and treatment of mobility decline in older persons. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 1429–1436. [Google Scholar] [CrossRef] [PubMed]
- Washburn, R.; MacAuley, E.; Katula, J.; Mihalko, S.L.; Boileau, R.A. The Physical Activity Scale for the Elderly (PASEP): Evidence for Validity. J. Clin. Epidemiol. 1999, 52, 643–651. [Google Scholar] [CrossRef]
- Cohen, J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960, 20, 37–46. [Google Scholar] [CrossRef]
- McHugh, M. Inter-Rater Reliability. The Kappa Statistic. Available online: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3900052/ (accessed on 1 October 2015).
- Fleiss, J. Reliability of Measurement in the Design and Analysis of Clinical Experiments; Wiley and Sons: New York, NY, USA, 2011; pp. 1–33. [Google Scholar]
- Steffen, T.; Hacker, T.; Mollinger, L. Age and Gender—Related test performance in community dwelling elderly people: Six minute walk test, Berg balance scale, Timed up and go test, and Gait speeds. Phys. Ther. 2002, 82, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Cicchetti, D.V.; Feinstein, A.R. High agreement but low kappa: II. Resolving the paradoxes. J. Clin. Epidemiol. 1990, 43, 551–558. [Google Scholar] [CrossRef]
- Chiu, A.; Yeung, S.; Lo, S. A comparison of four functional tests in discriminating fallers from non-fallers in older people. Disabil. Rehabil. 2003, 25, 45–50. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Golf (N = 21) | Non-Golf (N = 10) | Mean Difference (95% CI) | Significance |
|---|---|---|---|---|
| Age (Years) Range | 83 (3) 80–87 | 80.5 (1.25) 80–83 | N/A | p = 0.004 * |
| Height (m) Range | 1.58 ± 0.04 1.51–1.65 | 1.57 ± 0.05 1.46–1.66 | −0.01 (−0.05–0.02) | p = 0.38 |
| Weight (kg) Range | 62.3 ± 9.22 46.9–78.8 | 66.2 ± 12.7 53.4–93.8 | 3.87 (−4.34–12) | p = 0.34 |
| BMI (kg/m2) Range | 24.7 ± 3.56 18.8–31.9 | 26.8 ± 4.42 20.7–34 | 2.05 (−0.97–5.0) | p = 0.34 |
| Test | % Agreement | Kappa |
|---|---|---|
| 1.1a | 87 | 0.74 (0.50–0.97) |
| 1.2a | 94 | 0.71 (0.33–1.00) |
| 1.3a | 97 | 0.65 (0.02–1.00) |
| 1.4a | 100 | 1 (1.00–1.00) |
| 1.5a | 94 | 0.85 (0.65–1.00) |
| 1.6a | 94 | 0.81 (0.57–1.00) |
| 1.7a | 90 | 0.73 (0.45–1.00) |
| 1.1b | 100 | 1 (1.00–1.00) |
| 1.2b | 97 | 0.78 (0.37–1.00) |
| 1.3b | 100 | 1 (1.00–1.00) |
| 1.4b | 90 | 0.87 (0.69–1.00) |
| 2.1 | 97 | 0.87 (0.69–1.00) |
| 2.2 | 97 | 0.65 (0.02–1.00) |
| 2.3 | 97 | 0.65 (0.02–1.00) |
| 2.4 | 100 | 1 (1.00–1.00) |
| 2.5 | 90 | 0.73 (0.49–0.97) |
| 2.6 | 100 | NA |
| 2.7 | 90 | 0.66 (0.32–1.00) |
| 3.1 | 97 | 0.93 (0.81–1.00) |
| 3.2 | 90 | 0.67 (0.34–1.00) |
| 3.3 | 87 | 0.73 (0.49–0.97) |
| 3.4 | 97 | 0.47 (−0.12–1.00) |
| 3.5 | 100 | NA |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Webb, N.; Rowsome, K.; Ewings, S.; Comerford, M.; Stokes, M.; Mottram, S. A ‘Movement Screening Test’ of Functional Control Ability in Female Recreation Golfers and Non-Golfers over the Age of 80 Years: A Reliability Study. J. Funct. Morphol. Kinesiol. 2018, 3, 54. https://doi.org/10.3390/jfmk3040054
Webb N, Rowsome K, Ewings S, Comerford M, Stokes M, Mottram S. A ‘Movement Screening Test’ of Functional Control Ability in Female Recreation Golfers and Non-Golfers over the Age of 80 Years: A Reliability Study. Journal of Functional Morphology and Kinesiology. 2018; 3(4):54. https://doi.org/10.3390/jfmk3040054
Chicago/Turabian StyleWebb, Nicholas, Keira Rowsome, Sean Ewings, Mark Comerford, Maria Stokes, and Sarah Mottram. 2018. "A ‘Movement Screening Test’ of Functional Control Ability in Female Recreation Golfers and Non-Golfers over the Age of 80 Years: A Reliability Study" Journal of Functional Morphology and Kinesiology 3, no. 4: 54. https://doi.org/10.3390/jfmk3040054
APA StyleWebb, N., Rowsome, K., Ewings, S., Comerford, M., Stokes, M., & Mottram, S. (2018). A ‘Movement Screening Test’ of Functional Control Ability in Female Recreation Golfers and Non-Golfers over the Age of 80 Years: A Reliability Study. Journal of Functional Morphology and Kinesiology, 3(4), 54. https://doi.org/10.3390/jfmk3040054





