Abstract
Background: Functional disability is a growing concern in aging populations with chronic health conditions, yet few studies have compared disability profiles across diagnostic categories using standardized tools. Objectives: This study aimed to characterize the functional profiles of adults with neurological, musculoskeletal, and chronic pain conditions using the World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) and to examine differences by age and sex. Methods: A total of 419 participants (median age = 73 years; 73% female) completed the 36-item WHODAS 2.0. Diagnoses were classified into three groups: neurological (n = 134), musculoskeletal (n = 230), and pain-related (n = 55). Domain-level scores were analyzed using non-parametric tests and Spearman correlations. Results: revealed that neurological conditions were associated with the highest disability levels, particularly in cognition, interpersonal relations, and participation. Musculoskeletal conditions showed greater impairments in mobility and self-care, while pain-related conditions demonstrated variable disability, especially in participation. Women reported higher disability scores in the neurologic group, with significant differences observed in the cognition domain among neurological cases (p = 0.048). Age was positively correlated with disability in self-care and mobility, especially in musculoskeletal conditions. Conclusions: These findings highlight the utility of WHODAS 2.0 in identifying domain-specific limitations across clinical populations. They support the need for individualized, diagnosis- and gender-sensitive rehabilitation strategies, and suggest that WHODAS 2.0 can inform targeted care planning and resource allocation in rehabilitation settings. Future research should incorporate longitudinal designs and explore contextual factors influencing functional outcomes.
1. Introduction
Functional disability is an increasing global public health challenge due to population aging and the rising burden of chronic non-communicable diseases. It involves difficulties performing basic daily activities that reduce autonomy, social participation, and well-being [1]. An estimated 15% of adults worldwide are affected, with 2–4% experiencing severe impairments [2], marking a notable increase compared to earlier estimates from the 1970s, which reflects improved measurement methods and the growing prevalence of chronic diseases [3]. Recent data suggest that 12.6% of adults globally experience functional difficulties, with variability across countries due to differences in measurement tools [4]. These limitations relate not only to medical outcomes but also to social exclusion, reduced quality of life, and increased healthcare use [5]. Recognizing this, the World Health Organization has redefined healthy aging as maintaining functional capacity to support well-being in older age, emphasizing that functional impairments are not inevitable consequences of aging but modifiable when detected early [6]. Thus, functional disability remains a core indicator for equitable health system planning [7].
Prevalence rates are consistently higher among women, older adults, and socioeconomically disadvantaged populations [2]. Multiple studies have identified age as a key determinant, with prevalence rising sharply in older age groups. Disability prevalence rises with age (e.g., from 22.4% at 60–64 years to 54.8% after age 80 [8], and is higher among women, partly due to socioeconomic disparities and caregiving roles [9]. Rural populations and those with lower income/education face additional barriers [10], highlighting structural inequalities.
With rising life expectancy, strategies such as early detection and person-centered rehabilitation are essential [11]. A biopsychosocial approach helps move beyond descriptive trends, acknowledging the interplay of biological, psychological, and social factors [12]. For example, chronic pain reflects not only tissue damage but also coping and social support [13].
The WHO’s ICF framework promotes a biopsychosocial understanding of disability, shifting focus from disease-centric models to one where functionality emerges from interactions between health conditions and context [14]. It guides rehabilitation strategies that foster adaptive changes, supported by neuroplasticity [15].
Evidence suggests that robust social networks and a supportive environment can buffer the impact of disease on functional ability, even in older adults facing multiple health challenges [16]. Therefore, incorporating the concept of functional aging into rehabilitation planning encourages a preventive, person-centered model that accounts for both biological vulnerabilities and protective social factors [6].
To support person-centered care and enable standardized assessments of functioning beyond diagnosis, the WHO Disability Assessment Schedule 2.0 (WHODAS 2.0) has become a key instrument in rehabilitation. Grounded in the International Classification of Functioning, Disability and Health (ICF), WHODAS 2.0 reflects the biopsychosocial model through six core domains: cognition, mobility, self-care, getting along, life activities, and social participation [17,18]. Available in 36- and 12-item versions, and adaptable to self-, interviewer-, or proxy-report, it assesses functioning over the last 30 days using a five-point Likert scale and provides both simple and complex scoring systems that translate into a 0–100 scale, where higher scores reflect greater disability [17,18].
WHODAS 2.0 has demonstrated strong psychometric properties across neurological, musculoskeletal, and chronic pain conditions, including high internal consistency, test–retest reliability, and sensitivity to change [18,19]. Its construct validity has been confirmed in populations with Parkinson’s disease, multiple sclerosis, and stroke, as well as in musculoskeletal disorders like osteoarthritis and chronic back pain [17,18]. In chronic pain syndromes such as fibromyalgia, it captures the interplay between physical discomfort, emotional burden, and social isolation [20]. Despite this versatility, most studies have analyzed single-diagnosis cohorts and have not fully exploited the instrument’s potential for cross-diagnostic, multifactorial disability profiling [17,18], particularly regarding the interaction of diagnosis with age, sex, and socioeconomic vulnerability.
Despite the widespread clinical adoption of WHODAS 2.0, several limitations in the literature restrict its utility for population-level and cross-diagnostic analyses. Although the instrument was designed to allow comparisons across diagnostic categories, most empirical studies have focused on single-diagnosis cohorts—such as individuals with Parkinson’s disease, chronic back pain, or musculoskeletal conditions—limiting the generalizability of their findings [18]. Additionally, few studies have explored domain-specific functional profiles across multiple health conditions while accounting for key demographic variables such as age, sex, and socioeconomic vulnerability [17]. This gap constrains our understanding of how chronic conditions intersect with social determinants to shape disability trajectories.
Moreover, few studies have conducted comprehensive multivariate analyses to examine how functional performance is shaped by the interaction of diagnostic group, age, gender, and other contextual factors [18,21]. The lack of integrative analyses hinders the design of truly individualized rehabilitation strategies that reflect the complex reality of patients with multimorbidity and diverse sociodemographic profiles.
Age-related differences are particularly underexplored at the domain level. Evidence suggests that middle-aged adults (50–64 years) may already experience significant declines in certain domains of functioning, which tend to worsen with age [22]. Similarly, while women consistently report higher levels of disability, there is insufficient data to determine whether this is due to biological differences, social roles, or disparities in access to services [23]. Addressing these analytical gaps is essential for advancing equity and precision in functional rehabilitation planning.
In response, this study aims to generate new insights into how diagnosis, age, and sex interact to shape functional disability across multiple domains. Using WHODAS 2.0 as a standardized assessment tool, it seeks to characterize the domain-specific functional profiles of adults living with neurological, musculoskeletal, and chronic pain conditions, considering age, sex, and diagnosis as key explanatory variables.
By moving beyond single-disease analyses and adopting a comparative, multivariable approach, the study intends to provide a more nuanced understanding of the interaction between clinical and demographic factors in shaping disability outcomes. This information is crucial for informing targeted rehabilitation strategies, tailoring interventions to individual needs, and improving health service planning in complex and heterogeneous populations. Ultimately, the study contributes to the development of evidence-based, equitable, and person-centered care models within diverse healthcare systems.
2. Materials and Methods
2.1. Study Design
This research followed an observational cross-sectional design based on a secondary analysis of clinical data from a rehabilitation center registry in Chile. This design was chosen to describe functional disability profiles at a single point in time across different chronic condition groups.
2.2. Participants
Participants were drawn from the clinical registry of a rehabilitation network and represented three major diagnostic categories: neurological disorders, musculoskeletal diseases, and chronic pain-related syndromes.
Inclusion criteria required participants to (1) be aged 18 years or older, (2) have a confirmed diagnosis within one of the three predefined chronic condition categories, and (3) have completed the full WHODAS 2.0 questionnaire as part of their functional assessment process. Only patients with complete demographic and diagnostic records were retained for analysis.
Exclusion criteria included (1) incomplete clinical data, particularly absence of key variables such as age, sex, or diagnosis; and (2) severe cognitive or communicative impairments that precluded reliable self-report or caregiver-assisted completion of WHODAS 2.0.
Participant selection was conducted retrospectively from institutional databases, applying non-probabilistic sampling of all eligible individuals assessed between 2022 and 2024. This full sample approach was chosen to ensure representation across conditions and enhance external validity by maximizing sample size within each diagnostic category.
2.3. Outcome Measures
The primary outcome assessed in this study was functional disability, defined as the degree of difficulty experienced by individuals in performing activities of daily living and participating in community and social life. Given the multidimensional nature of disability, a comprehensive evaluation approach was required to capture limitations across cognitive, physical, interpersonal, and occupational domains.
This study utilized the 36-item version of World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0), a standardized and validated instrument designed to measure functioning and disability independent of diagnosis and across diverse cultural contexts, across six core domains of functioning: cognition (understanding and communication), mobility (physical movement), self-care (personal hygiene, dressing, and eating), getting along with others (interpersonal interactions), life activities (domestic responsibilities and work/school engagement), and participation (involvement in society and community life).
Each item is rated on a 5-point Likert scale ranging from 0 (“no difficulty”) to 4 (“extreme difficulty or cannot do”). The raw scores for each domain are summed, resulting in both domain-specific scores and a total score. The maximum total score is 144 points, with higher values indicating greater disability. For this study, the simple scoring method was applied, which allows direct summation of responses without item weighting, facilitating interpretation and analysis across subgroups.
WHODAS 2.0 has demonstrated strong psychometric properties. According to WHO field trials and validation studies, the 36-item version shows high internal consistency (Cronbach’s alpha > 0.90 for the total score; >0.80 for domains) and excellent test–retest reliability (ICC = 0.93–0.98) [17,18]. It also exhibits good construct and concurrent validity across general and clinical populations with chronic neurological, musculoskeletal, and pain-related conditions. Its alignment with the ICF framework further enhances conceptual and clinical relevance.
The choice of WHODAS 2.0 was based on its methodological and practical advantages. First, it is a cross-culturally validated tool, suitable for use in diverse clinical settings, including rehabilitation centers and outpatient services. Second, it permits comparison across diagnostic groups by focusing on functioning rather than disease-specific symptoms. This makes it ideal for studies involving heterogeneous populations with chronic conditions. Third, the availability of a 36-item version provides granular data at the domain level, which aligns with the objective of this study to examine differential patterns of functional disability in detail. Lastly, the instrument’s widespread use in global disability research enhances the generalizability and comparability of findings.
2.4. Statistical Analysis
All statistical analyses were conducted using GraphPad Prism version 9.5.1 and PAST 4.12b. Descriptive statistics, inferential tests, and graphical visualizations were performed in alignment with data distribution characteristics. The dataset was first reviewed for completeness, duplicates, and consistency. Each domain and total score were extracted and categorized by sex, diagnosis, and age group for comparative analysis.
The Shapiro–Wilk test was applied to assess the normality of distribution for all WHODAS 2.0 domain scores and the total score. A non-parametric analytical approach was pre-specified given the ordinal nature and non-normal distribution of WHODAS 2.0 scores, justifying the use of non-parametric statistical methods for both descriptive and inferential analyses. Descriptive statistics were expressed as medians and interquartile ranges (IQRs) for each domain and for the total score, stratified by diagnostic group, sex, and age range. Categorical data (e.g., sex distribution across diagnoses) were reported as absolute frequencies and percentages.
For inferential analysis, group comparisons were conducted using the Mann–Whitney U test for two-group comparisons (e.g., male vs. female within a diagnostic group) and the Kruskal–Wallis test with Dunn’s post hoc correction for multiple comparisons across more than two groups. Spearman’s rank correlation coefficient was used to explore associations between age and WHODAS domain scores, both at group level and within specific diagnoses (e.g., osteoarthritis, fibromyalgia).
The threshold for statistical significance was established at α = 0.05. All p-values are reported explicitly, and where multiple comparisons were performed, adjusted p-values were applied using Dunn’s method. Box plots and radar plots were generated to depict central tendency and variation across domains, diagnostic categories, and sex. Linear regression trend lines were plotted in cases where age was explored as a predictor of functional domain scores.
2.5. Ethical Considerations
This study was conducted in accordance with international ethical standards for research involving human subjects. The research protocol was reviewed and approved by the Institutional Ethics Committee of the Rehabilitation Center Club de Leones Cruz del Sur, under approval code CRCS_UID_010223, 1 February 2023, ensuring compliance with institutional and national guidelines for biomedical research.
All procedures followed the ethical principles outlined in the Declaration of Helsinki (last revision, 2013) and adhered to the guidelines issued by the Council for International Organizations of Medical Sciences (CIOMS) for the ethical conduct of research involving vulnerable populations.
Written informed consent was obtained from all participants prior to inclusion in the study. In cases where participants were unable to provide consent directly due to health or communication limitations, authorization was obtained from a legally authorized representative, in accordance with ethical protocols.
To ensure data confidentiality and participant privacy, all datasets were anonymized before analysis. Personal identifiers were removed, and each participant was assigned a coded identifier. Access to sensitive information was restricted to authorized personnel involved in the data handling and analysis process.
Participation in the study was entirely voluntary, and no financial compensation or material incentive was provided to participants. There were no foreseeable risks associated with participation, as all procedures were based on routine clinical assessments and secondary analysis of pre-existing data.
3. Results
3.1. Sample Characteristics and Overall WHODAS Scores
A total of 423 participants completed the WHODAS 2.0 assessment, of whom 419 were included in the final analysis after excluding four cases due to missing clinical data. The participants’ median age was 73 years (IQR: 64–80), and 306 (73%) were female, as shown in Table 1. Diagnoses were categorized into three groups: musculoskeletal (n = 230), neurological (n = 134), and pain-related conditions (n = 55). The highest median domain scores across the full sample were observed in mobility (D2: 2.40), life activities (D5: 2.00), and participation (D6: 1.88), while the lowest were in interpersonal relationships (D4: 0.80) and self-care (D3: 1.25). The total simple score had a median of 52.00 (IQR: 34.00–69.00). Shapiro–Wilk tests confirmed non-normal distributions for all variables (p < 0.05), supporting the use of non-parametric analyses.

Table 1.
Demographic characteristics for each subgroup of conditions. Age represented in means and standard deviation. Sex, represented with the number of female patients and the percentage of the subcategory.
3.2. Disability Profiles by Diagnostic Group
Median total scores varied across diagnostic categories, with the highest disability observed in neurological conditions (median = 59.00), followed by pain-related conditions (49.00) and musculoskeletal disorders (48.00) (Table 2).

Table 2.
WHODAS 2.0 scores by sex and total across all subcategories.
Domain-specific differences were also evident:
- -
- Neurological conditions showed the greatest overall disability, with the highest scores in mobility (D2: 2.50), life activities (D5: 2.06), and participation (D6: 2.00). Cognition (D1: 1.33) and self-care (D3: 1.75) were also notably affected.
- -
- Musculoskeletal disorders presented prominent difficulties in mobility (D2: 2.20) and life activities (D5: 1.75), with milder impairments in cognition (D1: 1.00) and participation (D6: 1.75).
- -
- Pain-related conditions had a more heterogeneous profile, with comparable scores in mobility (D2: 2.20) and participation (D6: 2.00), but lower disability in self-care (D3: 0.75) and cognition (D1: 1.17).
3.3. Neurological Subgroup Analysis
Within the neurological group (n = 134), the most frequent diagnoses were acquired brain injury (n = 47), Parkinson’s disease (n = 36), and polyneuropathy (n = 25). Across all domains, female participants consistently reported higher levels of disability than males. The median total simple score was 62.5 for women and 51.5 for men. A statistically significant sex difference was observed in the cognition domain (D1; p = 0.048). Detailed median domain scores by diagnosis and sex are presented in Table 2 and illustrated in Figure 1.
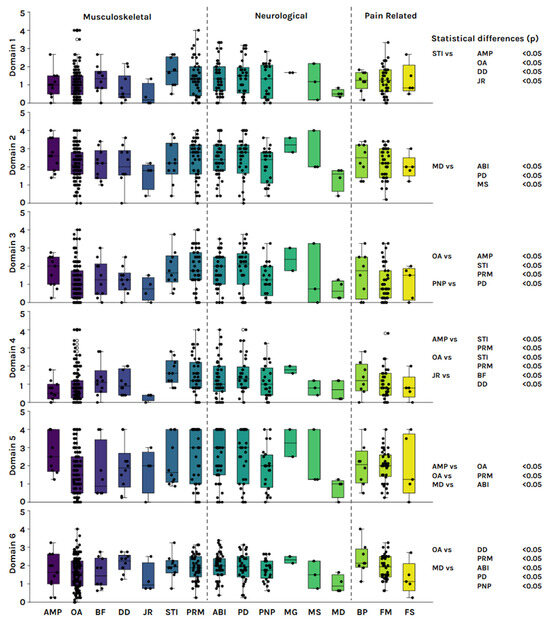
Figure 1.
Subcategory distribution of WHODAS 2.0 scores across all six domains. Mann–Whitney’s p value between subcategories expressed on the right side of the figure. AMP: amputee; OA: osteoarthritis; BF: bone fracture; DD: disc disease; JR: joint replacement; STI: soft tissue injuries; PRM: people with reduced mobility; ABI: acquire brain injury; PD: Parkinson’s disease; PNP: polyneuropathy; MG: Miastenia Gravis; MS: multiple sclerosis; MD: muscular dystrophy; FM: fibromyalgia; FS: frozen shoulder.
3.3.1. Acquired Brain Injury
Among the 47 individuals with acquired brain injury (ABI), 30 were female and 17 were male. The most pronounced intersex difference was observed in the life activities domain (D5), with a median score of 3.00 for women and 1.75 for men. While women showed higher scores across all WHODAS 2.0 domains, no statistically significant sex differences were identified in this subgroup.
3.3.2. Parkinson Disease
Among the 36 participants diagnosed with Parkinson’s disease (PD), 22 were women and 14 were men. The female subgroup presented a substantially higher total WHODAS 2.0 score (median = 68.00) compared to the male subgroup (median = 43.00). Although women exhibited consistently higher median scores across all domains, none of the sex-based differences reached statistical significance.
3.3.3. Polyneuropathies
In the polyneuropathy (PNP) subgroup (n = 25), 18 participants were female and 7 were male. A statistically significant sex difference was observed in the cognition domain (D1), with women reporting a median score of 2.00 compared to 0.17 in men (p = 0.007). Although women also exhibited higher scores in other domains, none of those differences were statistically significant.
3.4. Musculoskeletal Subgroup Analysis
The musculoskeletal group included 230 participants, of whom 171 were female and 59 were male. The median total WHODAS 2.0 score was 48.00 in women and 53.00 in men, a difference that did not reach statistical significance (p = 0.068). Detailed median scores by diagnosis and sex are presented in Table 2.
A multivariable correlation analysis revealed positive associations between age and several WHODAS domains, particularly in cognition (D1), mobility (D2), self-care (D3), and getting along (D4). The strongest correlation was observed between age and the self-care domain (D3), with a Spearman coefficient of ρ = 0.21 (p < 0.001).
When stratifying by diagnosis, this association was even more pronounced in participants with osteoarthritis (n = 130), where the correlation between age and self-care reached ρ = 0.25 (p < 0.001). No significant differences were observed between sexes in this correlation.
Domain-level scores varied across the different musculoskeletal diagnoses. Among People with Reduced Mobility (PRM, n = 47), higher disability scores were observed in mobility (D2), life activities (D5), and participation (D6). Individuals with amputation (n = 11) also showed elevated scores, particularly in self-care (D3) and life activities (D5). Lower levels of disability were reported in conditions such as joint replacement and bone fracture. Table 2 provides a detailed breakdown of domain scores and total scores by sex for each musculoskeletal diagnosis.
3.5. Pain-Related Subgroup Analysis
The pain-related group comprised 55 participants, including 42 individuals with fibromyalgia, 8 with back pain, and 5 with painful shoulder syndrome. Only three male participants were included in this group (one per diagnostic category), preventing meaningful statistical comparisons by sex.
The median total WHODAS 2.0 score for the group was 49.00. Domain-level scores showed functional variability across diagnoses, with the highest scores observed in participation (D6) and mobility (D2). Fibromyalgia was the most prevalent condition and demonstrated consistently moderate-to-high disability across all domains, whereas painful shoulder syndrome showed comparatively lower scores.
A multivariable correlation analysis revealed a significant negative association between age and participation (D6), with a Spearman coefficient of ρ = −0.35 (p < 0.001). This indicates that older participants reported lower disability in participation-related tasks. A similar trend was observed for the total WHODAS score, although it did not reach statistical significance. These findings may reflect the adoption of age-related coping strategies or lower perceived role expectations among older adults. Table 2 summarizes the median scores for each domain and the total score across the three diagnostic categories.
4. Discussion
This study aimed to characterize the functional profiles of adults with neurological, musculoskeletal, and chronic pain conditions using WHODAS 2.0, with special attention to differences by diagnosis, age, and sex. The results revealed that disability profiles differ substantially between clinical groups, with neurological conditions presenting the greatest overall disability, particularly in the domains of cognition, mobility, and participation. Musculoskeletal diseases showed greater limitations in mobility and self-care, while chronic pain conditions presented a more heterogeneous distribution, with a special impact on social participation. Higher levels of disability were also observed in women with neurological conditions and a positive correlation between age and functional impairment particularly in people with musculoskeletal diseases.
The analysis by functional domains revealed differentiated patterns according to diagnosis, which reflect both the pathophysiological impact of each condition and contextual and adaptive factors. In neurological conditions, higher scores in cognition, participation, and mobility are consistent with central nervous system impairments and progressive loss of executive skills, social interaction, and physical displacement, as documented in patients with Parkinson’s or acquired brain injuries [18,24]. In the musculoskeletal group, the limitations were concentrated in mobility and self-care, which can be explained by the presence of pain, joint stiffness, or cumulative motor impairment, especially in older adults with osteoarthritis. On the other hand, chronic pain conditions such as fibromyalgia showed a more variable profile, but with a notable affectation in participation, which could be linked to behavioral avoidance processes, fatigue, and emotional alterations [25]. In the musculoskeletal group, the limitations were concentrated in mobility and self-care, which can be explained by the presence of pain, joint stiffness, or cumulative motor impairment, especially in older adults with osteoarthritis. On the other hand, chronic pain conditions such as fibromyalgia showed a more variable profile, but with a notable affectation in participation, which could be linked to behavioral avoidance processes, fatigue, and emotional alterations.
The functional differences according to sex and age observed in this study reinforce the importance of considering sociodemographic variables in rehabilitation planning. Women reported higher levels of disability in almost all domains, with statistically significant differences in the cognitive area within the neurological group. These findings are consistent with the literature that attributes these differences not only to biological factors, but also to the cumulative weight of structural inequalities, such as less access to specialized services, burden of caregiving roles, and greater exposure to chronic stress [9,26]. The functional differences according to sex and age observed in this study reinforce the importance of considering sociodemographic variables in rehabilitation planning. Women reported higher levels of disability in almost all domains, with statistically significant differences in the cognitive area within the neurological group. These findings are consistent with the literature that attributes these differences not only to biological factors, but also to the cumulative weight of structural inequalities, such as less access to specialized services, burden of caregiving roles, and greater exposure to chronic stress [11]. These associations reinforce the need to apply a life-course perspective in rehabilitation, anticipating functional impairment and promoting preventive strategies that consider both individual trajectories and social determinants of health.
From a clinical and programmatic perspective, the results of this study underscore the need to design differentiated interventions according to diagnosis, age, and gender. In people with neurological conditions, the simultaneous involvement of cognitive, motor, and participation domains suggests that rehabilitation programs should integrate physical and neurocognitive components, as well as strategies for social reintegration [18,27]. From a clinical and programmatic perspective, the results of this study underscore the need to design differentiated interventions according to diagnosis, age, and gender. In people with neurological conditions, the simultaneous involvement of cognitive, motor, and participation domains suggests that rehabilitation programs should integrate physical and neurocognitive components, as well as strategies for social reintegration [24,28]. For its part, in people with chronic pain, such as fibromyalgia, it is recommended to incorporate interdisciplinary interventions that address not only pain, but also emotional coping, fatigue, and functional self-perception [25]. In turn, the differences observed between women and men reinforce the need for gender-sensitive approaches, which consider inequalities in access to treatment, care responsibilities, and the stigma associated with certain conditions [9,26]. In turn, the differences observed between women and men reinforce the need for gender-sensitive approaches, which consider inequalities in access to treatment, care responsibilities, and the stigma associated with certain conditions [17,19].
The observed patterns can be interpreted through established theoretical frameworks. The biopsychosocial model supports the idea that disability arises from the interaction of physiological impairments, psychological resilience, and social–environmental context [12,14]. In neurological conditions, persistent impairments may reflect limited neuroplasticity or delayed access to specialized rehabilitation services [27]. Among older adults with musculoskeletal disorders, cumulative aging processes and limited mobility could lead to progressive loss of autonomy and increased participation restrictions, particularly in under-resourced contexts.
This study has certain limitations that must be considered when interpreting the results. First, the cross-sectional design prevents establishing causal relationships between the sociodemographic variables and the levels of functional disability observed. Second, the use of a single self-reporting tool such as WHODAS 2.0 could have introduced perception biases, particularly in people with cognitive impairments or low educational attainment, which could affect the accuracy of scores in some domains [17]. In addition, the study did not incorporate relevant contextual variables such as socioeconomic level, support networks, level of physical activity, or presence of comorbidities, which can significantly influence functionality, especially in older people [11]. Finally, although there was a diverse sample, the subgroup sizes were not homogeneous, which could limit the generalizability of the comparative analyses.
Future research should prioritize longitudinal cohort designs and robust multivariate analyses that incorporate contextual variables to better understand the complexity of functional disability across diverse populations. The integration of mixed methods—combining objective assessments (e.g., gait speed, grip strength, neuropsychological testing) with qualitative evaluations—would allow for a more comprehensive understanding of individual experiences and environmental influences. Additionally, the inclusion of social determinants such as income, housing, and social support would enhance the explanatory power of these studies. Advanced analytical strategies, including machine learning models, may further contribute by identifying predictive profiles of functional risk or recovery trajectories across various chronic health conditions.
Overall, the findings of this study reinforce the need to understand functional disability as a dynamic and multidimensional phenomenon, which requires differentiated approaches according to diagnosis, age, gender, and social context. Functional assessment through standardized tools such as WHODAS 2.0 makes it possible to identify critical domains of intervention, facilitating the design of more precise, equitable, and person-centered rehabilitation strategies. Adopting a view based on functional trajectories, beyond clinical diagnoses, represents a key step towards more inclusive and responsive health systems to human diversity. In this sense, the present study contributes to expanding the evidence base necessary to move towards personalized care models that promote autonomy, participation, and quality of life for people living with chronic conditions.
5. Conclusions
This study provides evidence that functional disability in adults with chronic neurological, musculoskeletal, and pain-related conditions varies meaningfully across diagnostic groups, sex, and age. The use of WHODAS 2.0 enabled a multidimensional understanding of how these populations experience limitations in daily functioning, with neurological conditions and female sex being consistently associated with greater impairment.
These findings contribute to the field by reinforcing the utility of domain-based assessment tools in rehabilitation settings and highlighting the need for more tailored, person-centered approaches to functional evaluation and treatment planning. The analysis supports the relevance of incorporating demographic and diagnostic stratification into clinical decision-making processes.
For the populations affected, the results underscore the importance of accessible, individualized rehabilitation strategies that address both physical and cognitive barriers to autonomy. The study also supports the integration of gender-sensitive perspectives in rehabilitation programs to reduce disparities in functional outcomes.
Future research should build on these findings by employing longitudinal designs, incorporating objective functional metrics, and exploring contextual factors such as social support and access to care. This will allow for more predictive, equitable, and effective rehabilitation interventions across diverse patient populations.
Author Contributions
Conceptualization, P.B. and B.C.A.; methodology, P.B. and B.C.A.; software, P.B.; validation, P.B., B.C.A., and A.A.; formal analysis, P.B. and J.P.A.-G.; investigation, P.B. and B.C.A.; resources, A.A. and B.C.A.; data curation, J.P.A.-G. and P.B.; writing—original draft preparation, P.B. and J.P.A.-G.; writing—review and editing, J.C.M., F.C.-E., and C.C.; visualization, J.P.A.-G.; supervision, A.A. and B.C.A.; project administration, B.C.A.; funding acquisition, B.C.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Regional Government of Magallanes and the Chilean Antarctic through the Comprehensive Rehabilitation Program (Project BIP Code: 40000882-0). The funding body did not participate in the design of the study, data collection, analysis, interpretation of results, or writing of the manuscript.
Institutional Review Board Statement
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and was approved by the Institutional Review Board of the Rehabilitation Center Club de Leones Cruz del Sur (approval code: CRCS_UID_010223, 1 February 2023).
Informed Consent Statement
Written informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. Due to institutional policy and ethical restrictions, the datasets are not publicly available in order to protect patient confidentiality.
Acknowledgments
This study was made possible thanks to the support of the Comprehensive Rehabilitation Program, an initiative funded by the regional government of Magallanes and the Chilean Antarctic. The program provides interdisciplinary care to patients requiring physical, mental, or social rehabilitation in the cities of Punta Arenas, Puerto Natales, and Porvenir. The authors gratefully acknowledge the contributions of the clinical and administrative staff of the Corporación de Rehabilitación Club de Leones Cruz del Sur, whose collaboration was essential for the implementation and follow-up of standardized assessments. The contributions of data analysts, therapists, and support personnel not listed as authors are also acknowledged.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design, execution, interpretation, or writing of the study.
References
- World Health Organization. Disability and Health [Fact Sheet]; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/news-room/fact-sheets/detail/disability-and-health (accessed on 11 July 2025).
- Hartley, S.D. World Report on Disability (WHO); WHO and World Bank: Washington, DC, USA, 2011. [Google Scholar] [CrossRef]
- Coulter, A.; Entwistle, V.A.; Eccles, A.; Ryan, S.; Shepperd, S.; Perera, R. Personalised care planning for adults with chronic or long-term health conditions. Cochrane Database Syst. Rev. 2015, 2015, CD010523. [Google Scholar] [CrossRef] [PubMed]
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2021, 396, 2006–2017. [Google Scholar] [CrossRef] [PubMed]
- Netuveli, G.; Wiggins, R.D.; Hildon, Z.; Montgomery, S.M.; Blane, D. Functional limitation in long standing illness and quality of life: Evidence from a national survey. BMJ 2005, 331, 1382–1383. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) approach to healthy ageing. Maturitas 2020, 139, 6–11. [Google Scholar] [CrossRef]
- Stucki, G.; Cieza, A.; Melvin, J. The International Classification of Functioning, Disability and Health (ICF): A unifying model for the conceptual description of the rehabilitation strategy. J. Rehabil. Med. 2007, 39, 279–285. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef]
- Tareque, I.; Tiedt, A.D.; Islam, T.M.; Begum, S.; Saito, Y. Gender differences in functional disability and self-care among seniors in Bangladesh. BMC Geriatr. 2017, 17, 177. [Google Scholar] [CrossRef]
- Ipsen, C.; Hall, J.P.; Lui, J. Editorial: Rural disability and community participation. Front. Rehabil. Sci. 2022, 3, 1049578. [Google Scholar] [CrossRef]
- Beard, J.R.; Officer, A.; de Carvalho, I.A.; Sadana, R.; Pot, A.M.; Michel, J.-P.; Lloyd-Sherlock, P.; Epping-Jordan, J.E.; Peeters, G.M.E.E.; Mahanani, W.R.; et al. The World report on ageing and health: A policy framework for healthy ageing. Lancet 2016, 387, 2145–2154. [Google Scholar] [CrossRef]
- Engel, G.L. The Need for a New Medical Model: A Challenge for Biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef]
- Gatchel, R.J.; Peng, Y.B.; Peters, M.L.; Fuchs, P.N.; Turk, D.C. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol. Bull. 2007, 133, 581–624. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability and Health. 2001. Available online: https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health (accessed on 11 July 2025).
- Kleim, J.A.; Jones, T.A. Principles of Experience-Dependent Neural Plasticity: Implications for Rehabilitation After Brain Damage. J. Speech Lang. Hear. Res. 2008, 51, S225–S239. [Google Scholar] [CrossRef] [PubMed]
- Cramm, J.M.; Nieboer, A.P. Social cohesion and belonging predict the well-being of community-dwelling older people. BMC Geriatr. 2015, 15, 30. [Google Scholar] [CrossRef]
- Üstün, T.B. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule WHODAS 2.0; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Federici, S.; Bracalenti, M.; Meloni, F.; Luciano, J.V. World Health Organization disability assessment schedule 2.0: An international systematic review. Disabil. Rehabil. 2017, 39, 2347–2380. [Google Scholar] [CrossRef]
- Chwastiak, L.A.; Von Korff, M. Disability in depression and back pain. J. Clin. Epidemiol. 2003, 56, 507–514. [Google Scholar] [CrossRef]
- Sozańska, A.; Sozański, B.; Łagowska-Sado, A.; Wilmowska-Pietruszyńska, A.; Wisniowska-Szurlej, A. Disability Assessment with WHODAS 2.0 of People with Fibromyalgia in Poland: A Cross Sectional-Study. Med. Sci. Monit. 2024, 30, e945450. [Google Scholar] [CrossRef]
- Garin, O.; Ayuso-Mateos, J.L.; Almansa, J.; Nieto, M.; Chatterji, S.; Vilagut, G.; Alonso, J.; Cieza, A.; Svetskova, O.; Burger, H.; et al. Validation of the “World Health Organization Disability Assessment Schedule, WHODAS-2” in patients with chronic diseases. Health Qual. Life Outcomes 2010, 8, 51. [Google Scholar] [CrossRef]
- Stineman, M.G.; Xie, D.; Pan, Q.; Kurichi, J.E.; Zhang, Z.; Saliba, D.; Henry-Sánchez, J.T.; Streim, J. All-Cause 1-, 5-, and 10-Year Mortality in Elderly People According to Activities of Daily Living Stage. J. Am. Geriatr. Soc. 2012, 60, 485–492. [Google Scholar] [CrossRef]
- Leveille, S.G.; Penninx, B.W.J.H.; Melzer, D.; Izmirlian, G.; Guralnik, J.M. Sex differences in the prevalence of mobility disability in old age: The dynamics of incidence, recovery, and mortality. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2000, 55, S41–S50. [Google Scholar] [CrossRef]
- Silva, C.; Coleta, I.; Silva, A.G.; Amaro, A.; Alvarelhao, J.; Queiros, A.; Rocha, N. Adaptation and validation of WHODAS 2.0 in patients with musculoskeletal pain. Rev. Saúde Pública 2013, 47, 752–758. [Google Scholar] [CrossRef]
- Wawrzyniak, K.M.; Finkelman, M.; Schatman, M.E.; Kulich, R.J.; Weed, V.F.; Myrta, E.; DiBenedetto, D.J. The World Health Organization Disability Assessment Schedule-2.0 (WHODAS 2.0) in a chronic pain population being considered for chronic opioid therapy. J. Pain Res. 2019, 12, 1855–1862. [Google Scholar] [CrossRef]
- Vlassoff, C. Gender differences in determinants and consequences of health and illness. J. Health Popul. Nutr. 2007, 25, 47–61. [Google Scholar] [PubMed]
- Pascual-Leone, A.; Amedi, A.; Fregni, F.; Merabet, L.B. The Plastic Human Brain Cortex. Annu. Rev. Neurosci. 2005, 28, 377–401. [Google Scholar] [CrossRef]
- Beaton, K.; Grimmer, K. Tools that assess functional decline: Systematic literature review update. Clin. Interv. Aging 2013, 2013, 485–494. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).