Effect of a Community-Based Program on Preschoolers’ Physical Activity and Nutrition in Chile
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Subjects
2.3. Intervention
- ▪
- Nutritional education: Kindergarten educators were trained through participatory workshops on healthy eating habits and the importance of fruit and vegetable consumption. Educational materials were also designed to support daily activities in the daycare centers [16]. The design of the Didactic Guides for Physical Activity and Nutrition was based on the curricula of preschool education. Didactic Guides contained 45–50 games to be played daily with the children, aiming to increase physical activity as well as incorporate healthy food habits knowledge. The educational training was directed to educators and technicians; motivational workshops were conducted with the parents. Nutritionists and physical activity teachers trained all participant educators for 2 months, during 3-day workshops, to favour the participation of all educators. They also visited each other three times a week at each intervention centre. An active and motivational strategy was designed for parents, Healthy Days, once a month, consisting of participative games, healthy snacks, and leaflets with information on growth, nutritional factors, and physical activity needs.
- ▪
- Promotion of physical activity: Age-appropriate, playful physical activities were developed to improve children’s levels of moderate-to-vigorous physical activity [24]. Daily exercise sessions and outdoor games were included. The specific PA strategies included:
- ▪
- Daily active play sessions lasting at least 60 min per day, broken into three to four 15–20-min blocks throughout the school day.
- ▪
- Integration of movement into learning activities, such as using dance, stretching, and action-based storytelling to reinforce educational content.
- ▪
- Reduction of prolonged sitting, ensuring that sedentary periods did not exceed 30 min at a time.
- ▪
- Outdoor free play sessions encouraging children to explore their environment and engage in self-directed physical activity.
- ▪
- Encouragement of home-based PA, with educators providing parents with recommendations for simple activities that could be done with minimal equipment.
- ▪
- Community participation: Community activities, such as “healthy days,” were organized to engage parents and promote the adoption of healthy habits at home [39].
- ▪
- Educative diagnostic
- ▪
- The design and validation of educative methodology
- ▪
- The design and validation of didactic material for educators in both nutrition and physical activity aspects was designed to facilitate their activities with children.
2.4. Evaluation
2.5. Statistical Analysis
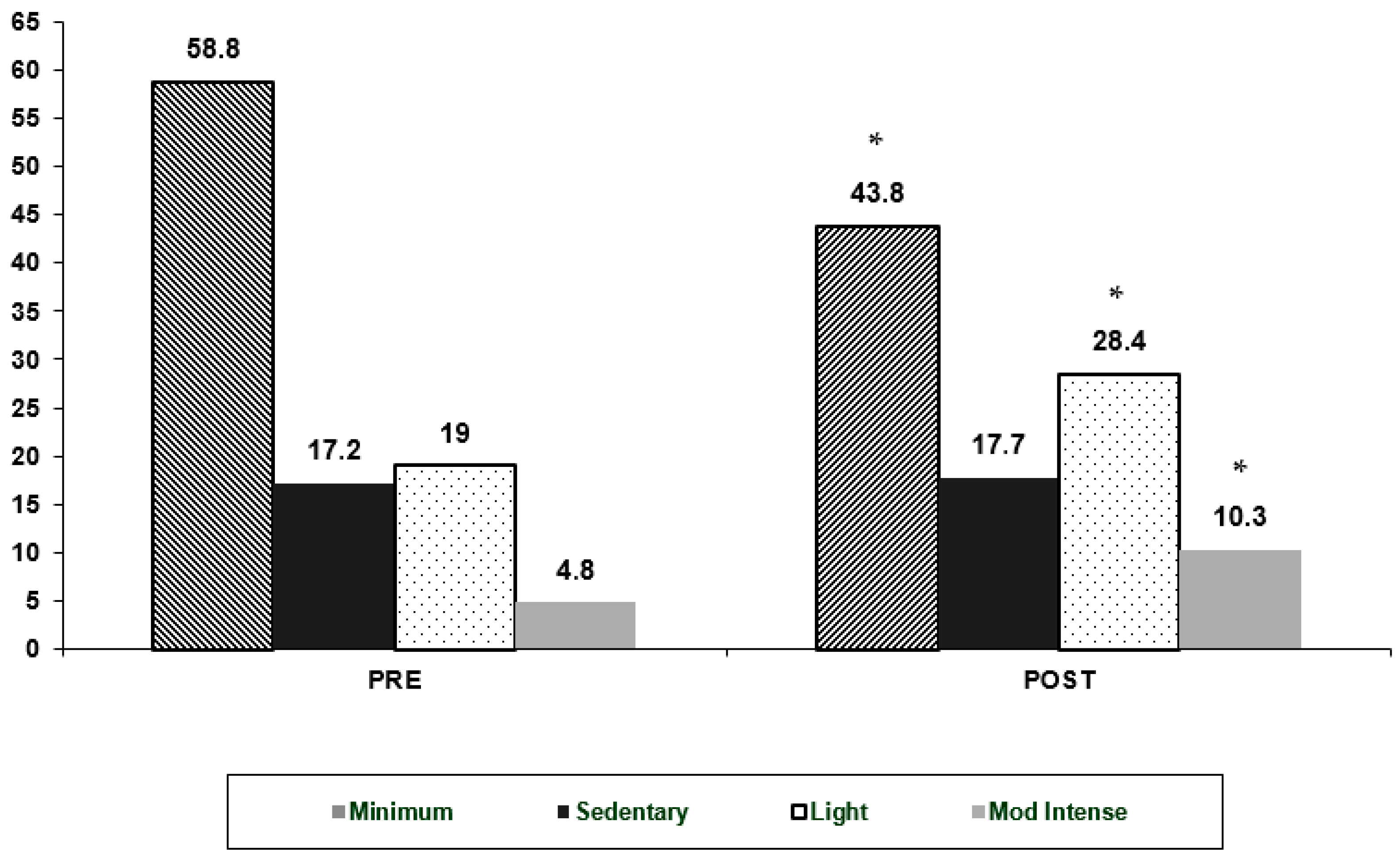
3. Results
4. Discussion
5. Future Research Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 6 March 2024).
- Monteiro, C.A.; Moubarac, J.-C.; Cannon, G.; Ng, S.W.; Popkin, B.M. Ultra-processed products are becoming dominant in the global food system. Obes. Rev. 2013, 14, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud (MINSAL). Encuesta Nacional de Salud 2016–2017; Gobierno de Chile: Santiago, Chile, 2017; Available online: https://epi.minsal.cl/encuesta-ens/ (accessed on 12 March 2024).
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Rivera, J.A.; de Cossío, T.G.; Pedraza, L.S.; Aburto, T.C.; Batis, C.; Popkin, B.M. Childhood and adolescent overweight and obesity in Latin America: A systematic review. Lancet Diabetes Endocrinol. 2014, 2, 321–332. [Google Scholar] [CrossRef] [PubMed]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Briefs 2017, 288, 1–8. [Google Scholar]
- Lobstein, T.; Jackson-Leach, R. Planning for the worst: Estimates of obesity and comorbidities in school-age children in 2025. Pediatr. Obes. 2016, 11, 321–325. [Google Scholar] [CrossRef]
- Tzioumis, E.; Adair, L.S. Childhood dual burden of under- and overnutrition in low- and middle-income countries: A critical review. Food Nutr. Bull. 2014, 35, 230–243. [Google Scholar] [CrossRef]
- Drewnowski, A.; Specter, S.E. Poverty and obesity: The role of energy density and energy costs. Am. J. Clin. Nutr. 2004, 79, 6–16. [Google Scholar] [CrossRef]
- Hawkes, C.; Jewell, J.; Allen, K. A food policy package for healthy diets and the prevention of obesity and diet-related non-communicable diseases: The NOURISHING framework. Obes. Rev. 2013, 14, 159–168. [Google Scholar] [CrossRef]
- Buscemi, J.; Odoms-Young, A.; Stolley, M.L.; Blumstein, L.; Schiffer, L.; Berbaum, M.L.; McCaffrey, J.; Montoya, A.M.; Braunschweig, C.; Fitzgibbon, M.L. Adaptation and dissemination of an evidence-based obesity prevention intervention: Design of a comparative effectiveness trial. Contemp. Clin. Trials 2014, 38, 355–360. [Google Scholar] [CrossRef]
- Towner, E.K.; Clifford, L.M.; McCullough, M.B.; Stough, C.O.; Stark, L.J. Treating obesity in preschoolers: A review and recommendations for addressing critical gaps. Pediatr. Clin. N. Am. 2016, 63, 481–510. [Google Scholar] [CrossRef]
- Ministerio de Salud (MINSAL). Ley de Etiquetado de Alimentos; Gobierno de Chile: Santiago, Chile, 2016; Available online: http://www.minsal.cl/reglamento-de-la-ley-de-etiquetado-de-alimentos-introduccion/ (accessed on 23 March 2024).
- Bleiweiss-Sande, R.; Jiménez-Cruz, A.; Bacardí-Gascón, M.; Skelton, K.; Benjamin-Neelon, S. Interventions to prevent obesity in Latinx children globally: Protocol for a systematic review and meta-analysis. Syst. Rev. 2021, 10, 123. [Google Scholar] [CrossRef] [PubMed]
- Fitzgibbon, M.L.; Stolley, M.R.; Schiffer, L.A.; Braunschweig, C.L.; Gomez, S.L.; Van Horn, L.; Dyer, A.R. Hip-Hop to Health Jr. Obesity Prevention Effectiveness Trial: Postintervention results. Obesity 2011, 19, 994–1003. [Google Scholar] [CrossRef]
- Brown, T.; Moore, T.H.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019, 7, CD001871. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.L.; Ventura, A.K. Preventing childhood obesity: What works? Int. J. Obes. 2009, 33 (Suppl. 1), S74–S81. [Google Scholar] [CrossRef]
- Campbell, K.J.; Lioret, S.; McNaughton, S.A.; Crawford, D.A.; Salmon, J.; Ball, K.; McCallum, Z.; Gerner, B.E.; Spence, A.C.; Cameron, A.J.; et al. A parent-focused intervention to reduce infant obesity risk behaviors: A randomized trial. Pediatrics 2013, 131, 652–660. [Google Scholar] [CrossRef]
- Jelalian, E.; Evans, E.W. Behavioral intervention in the treatment of obesity in children and adolescents: Implications for Mexico. Nutr. Rev. 2017, 75, 79–84. [Google Scholar] [CrossRef]
- Matsudo, S.M.; Matsudo, V.R.; Araujo, T.L.; Andrade, D.R.; Andrade, E.L.; de Oliveira, L.C.; Braggion, G.F. The Agita São Paulo Program as a model for using physical activity to promote health. Rev Panam. Salud. Publica. 2003, 14, 265–272. [Google Scholar] [CrossRef]
- Hesketh, K.D.; Campbell, K.J. Interventions to prevent obesity in 0-5 year olds: An updated systematic review of the literature. Obesity 2010, 18 (Suppl. 1), S27–S35. [Google Scholar] [CrossRef]
- Sultana, M.; Nichols, M.; Moodie, M.; Allender, S.; Brown, V. A systematic review of economic evidence for community-based obesity prevention interventions in children. Obes. Rev. 2023, 24, e13592. [Google Scholar] [CrossRef]
- Sultana, M.; Nichols, M.; Jacobs, J.; Karacabeyli, D.; Allender, S.; Novotny, R.; Brown, V. The range of outcomes and outcome measurement instruments collected in multisectoral community-based obesity prevention interventions in children: A systematic review. Obes. Rev. 2024, 25, e13731. [Google Scholar] [CrossRef]
- Reilly, J.J.; Hughes, A.R.; Gillespie, J.; Malden, S.; Martin, A. Physical activity interventions in early life aimed at reducing later risk of obesity and related non-communicable diseases: A rapid review of systematic reviews. Obes. Rev. 2019, 20 (Suppl. 1), 61–73. [Google Scholar] [CrossRef] [PubMed]
- Lillquist, S.; Ruiz Barnecett, G.; Flexman, N.; Mikati, N. Recipes for health: A community-based nutrition and culinary intervention. Cureus 2022, 14, e32322. [Google Scholar] [CrossRef] [PubMed]
- Perry, M.; Mardin, K.; Chamberlin, G.; Busey, E.A.; Taillie, L.S.; Dillman Carpentier, F.R.; Popkin, B.M. National policies to limit food marketing and competitive food sales in schools: A global scoping review. Adv. Nutr. 2024, 15, 100254. [Google Scholar] [CrossRef] [PubMed]
- Bradford, L.E.; Okpalauwaekwe, U.; Waldner, C.L.; Bharadwaj, L.A. Drinking water quality in Indigenous communities in Canada and health outcomes: A scoping review. Int. J. Circumpolar. Health 2016, 75, 32336. [Google Scholar] [CrossRef]
- Barrett, M.; Spires, M.; Vogel, C. The Healthy Start scheme in England “is a lifeline for families but many are missing out”: A rapid qualitative analysis. BMC Med. 2024, 22, 177. [Google Scholar] [CrossRef]
- Neil-Sztramko, S.E.; Caldwell, H.; Dobbins, M. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2021, 9, CD007651. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Guidelines on Physical Activity and Sedentary Behavior. 2020. Available online: https://www.who.int (accessed on 22 September 2024).
- Pérez-Escamilla, R.; Vilar-Compte, M.; Rhodes, E.; Sarmiento, O.L.; Corvalan, C.; Sturke, R.; Vorkoper, S. Implementation of childhood obesity prevention and control policies in the United States and Latin America: Lessons for cross-border research and practice. Obes. Rev. 2021, 22 (Suppl. 3), e13247. [Google Scholar] [CrossRef]
- Josyula, L.K.; Lyle, R.M. Barriers in the Implementation of a physical activity intervention in primary care settings: Lessons learned. Health Promot. Pract. 2013, 14, 81–87. [Google Scholar] [CrossRef]
- Villalobos Dintrans, P.; Rodriguez, L.; Clingham-David, J.; Pizarro, T. Implementing a food labeling and marketing law in Chile. Health Syst. Reform. 2020, 6, 1–8. [Google Scholar] [CrossRef]
- Skouteris, H.; McCabe, M.; Swinburn, B.; Newgreen, V.; Sacher, P.; Chadwick, P. Parental influence and obesity prevention in pre-schoolers: A systematic review of interventions. Obes. Rev. 2011, 12, 315–328. [Google Scholar] [CrossRef]
- Marshall, S.; Taki, S.; Laird, Y.; Love, P.; Wen, L.M.; Rissel, C. Cultural adaptations of obesity-related behavioral prevention interventions in early childhood: A systematic review. Obes. Rev. 2022, 23, e13402. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.D.; Fu, E.; Kobayashi, M.A. Prevention and management of childhood obesity and its psychological and health comorbidities. Annu. Rev. Clin. Psychol. 2020, 16, 351–378. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef]
- Sallis, J.F.; Owen, N.; Fisher, E.B. Ecological models of health behavior. In Health Behavior: Theory, Research, and Practice, 5th ed.; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; Jossey-Bass: San Francisco, CA, USA, 2015; pp. 43–64. [Google Scholar]
- Ayala, G.X.; Monge-Rojas, R.; King, A.C.; Hunter, R.; Berge, J.M. The social environment and childhood obesity: Implications for research and practice in the United States and countries in Latin America. Obes. Rev. 2021, 22 (Suppl. 3), e13246. [Google Scholar] [CrossRef] [PubMed]
- Lohman, T.G.; Boileau, R.A.; Slaughter, R.A. Body composition in children. In Human Body Composition; Lohman, T.G., Ed.; Human Kinetics: New York, NY, USA, 1984; pp. 29–57. [Google Scholar]
- WHO Multicentre Growth Reference Study Group. Reliability of anthropometric measurements in the WHO Multicentre Growth Reference Study. Acta. Paediatr. Suppl. 2006, 450, 38–46. [Google Scholar] [CrossRef]
- Schoeller, D.A. Hydrometry. In Human Body Composition; Roche, A., Heymsfield, S., Lohman, T.G., Eds.; Human Kinetics: New York, NY, USA, 1996; pp. 25–43. [Google Scholar]
- Going, S.B.; Levin, S.; Harrell, J.; Stewart, D.; Kushi, L.; Cornell, C.E.; Hunsberger, S.; Corbin, C.; Sallis, J. Physical activity assessment in American Indian schoolchildren in the Pathways study. Am. J. Clin. Nutr. 1999, 69, 788S–795S. [Google Scholar] [CrossRef]
- Grady, A.; Lorch, R.; Giles, L.; Lamont, H.; Anderson, A.; Pearson, N.; Romiti, M.; Lum, M.; Stuart, A.; Leigh, L.; et al. The impact of early childhood education and care-based interventions on child physical activity, anthropometrics, fundamental movement skills, cognitive functioning, and social-emotional wellbeing: A systematic review and meta-analysis. Obes. Rev. 2025, 26, e13852. [Google Scholar] [CrossRef]
- Arufe-Giráldez, V.; Pereira Loureiro, J.; Groba González, M.B.; Nieto Riveiro, L.; Canosa Domínguez, N.M.; Miranda-Duro, M.D.C.; Concheiro Moscoso, P.; Rodríguez-Padín, R.; Roibal Pravio, J.; Lagos Rodríguez, M.; et al. Multi-Context Strategies and Opportunities for Increasing Levels of Physical Activity in Children and Young People: A Literature Review. Children 2024, 11, 1475. [Google Scholar] [CrossRef]
- Heath, G.W.; Parra, D.C.; Sarmiento, O.L.; Andersen, L.B.; Owen, N.; Goenka, S.; Montes, F.; Brownson, R.C.; Lancet Physical Activity Series Working Group. Evidence-based intervention in physical activity: Lessons from around the world. Lancet 2012, 380, 272–281. [Google Scholar] [CrossRef]
- Park, K.H. Intervention for Severely Obese Children and Adolescents. J. Obes. Metab. Syndr. 2019, 28, 1–3. [Google Scholar] [CrossRef]
- Tayler, C.; Ishimine, K.; Cloney, D.; Cleveland, G.; Thorpe, K. The quality of early childhood education and care services in Australia. Aust. J. Early Child. 2019, 38, 203. [Google Scholar] [CrossRef]
- Niemeier, B.S.; Hektner, J.M.; Enger, K.B. Parent involvement in weight-related health interventions for children and adolescents: A systematic review and meta-analysis. Prev. Med. 2012, 55, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Wolfenden, L.; Nathan, N.K.; Sutherland, R.; Yoong, S.L.; Hodder, R.K.; Wyse, R.J.; Delaney, T.; Grady, A.; Fielding, A.; Tzelepis, F.; et al. Strategies for enhancing the implementation of school-based policies or practices targeting risk factors for chronic disease. Cochrane Database Syst. Rev. 2017, 11, CD011677. [Google Scholar] [CrossRef]
- Vážná, A.; Novák, J.M.; Daniš, R.; Sedlak, P. Adiposity and body fat distribution based on skinfold thicknesses and body circumferences in Czech preschool children, secular changes. PeerJ 2024, 12, e18695. [Google Scholar] [CrossRef]
- Sedlak, P.; Pařízková, J.; Procházková, L.; Cvrčková, L.; Dvořáková, H. Secular changes of adiposity in Czech children aged from 3 to 6 years: Latent obesity in preschool age. BioMed Res. Int. 2017, 2017, 2478461. [Google Scholar] [CrossRef]
- Bleich, S.N.; Segal, J.; Wu, Y.; Wilson, R.; Wang, Y. Systematic review of community-based childhood obesity prevention studies. Pediatrics 2013, 132, e201–e210. [Google Scholar] [CrossRef]
- Dube, L.; Addy, N.A.; Blouin, C.; Drager, N. From policy coherence to 21st century convergence: A whole-of-society paradigm of human and economic development. Ann. N. Y. Acad. Sci. 2014, 1331, 201–215. [Google Scholar] [CrossRef]
- Davison, K.K.; Birch, L.L. Childhood overweight: A contextual model and recommendations for future research. Obes. Rev. 2001, 2, 159–171. [Google Scholar] [CrossRef]
- Karnik, S.; Kanekar, A. Childhood obesity: A global public health crisis. Int. J. Prev. Med. 2012, 3, 1–7. Available online: https://www.ijpvmjournal.net (accessed on 25 October 2024).
- UNC Global Food Research Program. Front-of-Package (FOP) Food Labelling: Empowering Consumers to Make Healthy Choices. 2020. Available online: https://www.globalfoodresearchprogram.org/wp-content/uploads/2021/10/FOP_Factsheet_UNCGFRP.pdf (accessed on 29 December 2024).
- King, A.C.; Perez-Escamilla, R.; Vorkoper, S.; Anand, N.; Rivera, J. Childhood obesity prevention across borders: The promise of U.S.–Latin American research collaboration. Obes. Rev. 2021, 22, e13238. [Google Scholar] [CrossRef]
- Bertomeu-Gonzalez, V.; Sanchez-Ferrer, F.; Quesada, J.A.; Nso-Roca, A.P.; Lopez-Pineda, A.; Ruiz-Nodar, J.M. Prevalence of childhood obesity in Spain and its relation with socioeconomic status and health behaviors: Population-based cross-sectional study. Med. Clin. 2024, 163, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Zuluaga, N.A.; Osorno, A.; Lozano, A.; Villada, O. Clinical and metabolic effect of a multidisciplinary intervention through a comprehensive care program for children and adolescents with obesity. Biomedica 2020, 40, 166–184. [Google Scholar] [CrossRef] [PubMed]
- Latomme, J.; Cardon, G.; De Bourdeaudhuij, I.; Iotova, V.; Koletzko, B.; Socha, P.; Moreno, L.; Androutsos, O.; Manios, Y.; De Craemer, M.; et al. Effect and process evaluation of a kindergarten-based, family-involved intervention with a randomized cluster design on sedentary behaviour in 4- to 6- year old European preschool children: The ToyBox-study. PLoS ONE 2017, 12, e0172730. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Laddu, D.; Arena, R.; Ortega, F.B.; Alpert, M.A.; Kushner, R.F. Healthy Weight and Obesity Prevention: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1506–1531. [Google Scholar] [CrossRef]
| Intervention Participants (n = 120) | Control (n = 145) | p-Value | |
|---|---|---|---|
| Age (y) | 4.4 ± 0.4 | 4.5 ± 0.4 | 0.08 |
| Weight (k) | 18.6 ± 2.9 | 19.3 ± 3.1 | 0.06 |
| Height (cm) | 105.4 ± 4.6 | 106.6 ± 4.5 | 0.07 |
| Weight-for-age Z-score | 0.8 ± 1.2 | 0.7 ± 1.2 | 0.09 |
| Height-for-age | 0.05 | ||
| Z-score | −0.1 ± 1.0 | 0.1 ± 1.0 | |
| Weight-for-height | 0.04 * | ||
| Z-score | 0.8 ± 1.2 | 0.9 ± 1.2 |
| Obese Children | Normoweight Children | |||||
|---|---|---|---|---|---|---|
| Intervention Participants (n = 35) | Control (n = 42) | p-Value | Intervention Participants (n = 85) | Control (n = 103) | p-Value | |
| Age (y) | 4.4 ± 0.4 | 4.4 ± 0.4 | 0.85 | 4.4 ± 0.3 | 4.5 ± 0.4 | 0.06 |
| Weight (k) | 22.3 ± 2.5 | 23.6 ± 2.3 | 0.09 | 17.2 ± 1.7 | 17.8 ± 1.8 | 0.07 |
| Height (cm) | 107.2 ± 3.8 | 108.9 ± 3.8 | 0.07 | 104.7 ± 4.7 | 105.9 ± 4.5 | 0.09 |
| Weight-for-age Z-score | 2.2 ± 1.0 | 2.4 ± 0.9 | 0.11 | −0.1 ± 0.7 | −0.1 ± 1.1 | 0.87 |
| Height-for-age | ||||||
| Z-score | 0.3 ± 0.8 | 0.3 ± 0.8 | 0.92 | −0.3 ± 0.9 | −0.2 ± 1.0 | 0.33 |
| Weight-for-height | ||||||
| Z-score | 2.7 ± 0.8 | 3.0 ± 0.9 | 0.08 | 0.1 ± 0.5 | 0.3 ± 0.5 * | 0.04 |
| Obese Children | Normoweight Children | |||||
|---|---|---|---|---|---|---|
| Intervention Participants (n = 97) | Control (n = 86) | p-Value | Intervention Participants (n = 451) | Control (n = 305) | p-Value | |
| Age (y) | 4.5 ± 0.6 | 4.7 ± 0.6 | 0.07 | 4.5 ± 0.6 | 4.6 ± 0.5 | 0.08 |
| Weight (k) | 23.9 ± 3.1 | 23.4 ± 2.7 | 0.09 | 17.3 ± 1.8 | 17.3 ± 1.8 | 0.10 |
| Height (cm) | 107.1 ± 4.9 | 108.5 ± 5.0 | 0.05 | 104.5 ± 6.7 | 104.5 ± 4.9 | 0.07 |
| Weight-for-age | ||||||
| Z-score | 2.5 ± 1.1 | 2.4 ± 0.9 | 0.06 | −0.1 ± 0.7 | −0.1 ± 0.8 | 0.09 |
| Height-for-age | ||||||
| Z-score | 0.3 ± 1.0 | 0.4 ± 0.9 | 0.04 * | −0.2 ± 0.9 | −0.4 ± 1.0 | 0.03 * |
| Weight-for-height | ||||||
| Z-score | 3.1 ± 1.1 | 2.9 ± 0.8 | 0.02 * | 0.2 ± 0.5 | 0.2 ± 0.5 | 0.10 |
| Body Fat (%) | Intervention Participants | Controls | ||||
|---|---|---|---|---|---|---|
| Pre | Post | p-Value | Pre | Post | p-Value | |
| Total group | 25.0 ± 4.6 | 24.7 ± 4.8 | 0.04 * | 24.8 ± 4.4 | 25.1 ± 4.8 | 0.05 * |
| Obese | 31.6 ± 4.3 | 31.6 ± 4.7 | 0.88 | 30.7 ± 4.0 | 31.4 ± 4.7 | 0.03 * |
| Skinfolds | ||||||
| Sum of four skinfolds in obese children | 60.3 ± 15.6 | 57.9 ± 20.4 | 0.02 * | 52.6 ± 16.7 | 54.6± 19.6 | 0.05 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salazar, G.; Vasquez, F.; Andrade, M.; Rodriguez, M.d.P.; Berlanga, R.; Rojas, J.; Giadalah, A.; Muñoz, A. Effect of a Community-Based Program on Preschoolers’ Physical Activity and Nutrition in Chile. J. Funct. Morphol. Kinesiol. 2025, 10, 93. https://doi.org/10.3390/jfmk10010093
Salazar G, Vasquez F, Andrade M, Rodriguez MdP, Berlanga R, Rojas J, Giadalah A, Muñoz A. Effect of a Community-Based Program on Preschoolers’ Physical Activity and Nutrition in Chile. Journal of Functional Morphology and Kinesiology. 2025; 10(1):93. https://doi.org/10.3390/jfmk10010093
Chicago/Turabian StyleSalazar, Gabriela, Fabian Vasquez, Margarita Andrade, Maria del Pilar Rodriguez, Rocio Berlanga, Juanita Rojas, Antonio Giadalah, and Alvaro Muñoz. 2025. "Effect of a Community-Based Program on Preschoolers’ Physical Activity and Nutrition in Chile" Journal of Functional Morphology and Kinesiology 10, no. 1: 93. https://doi.org/10.3390/jfmk10010093
APA StyleSalazar, G., Vasquez, F., Andrade, M., Rodriguez, M. d. P., Berlanga, R., Rojas, J., Giadalah, A., & Muñoz, A. (2025). Effect of a Community-Based Program on Preschoolers’ Physical Activity and Nutrition in Chile. Journal of Functional Morphology and Kinesiology, 10(1), 93. https://doi.org/10.3390/jfmk10010093






