An Extensive Evaluation of Different Knee Stability Assessment Measures: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
Risk of bias/Quality Assessment
2.4. Synthesis of Results
3. Results
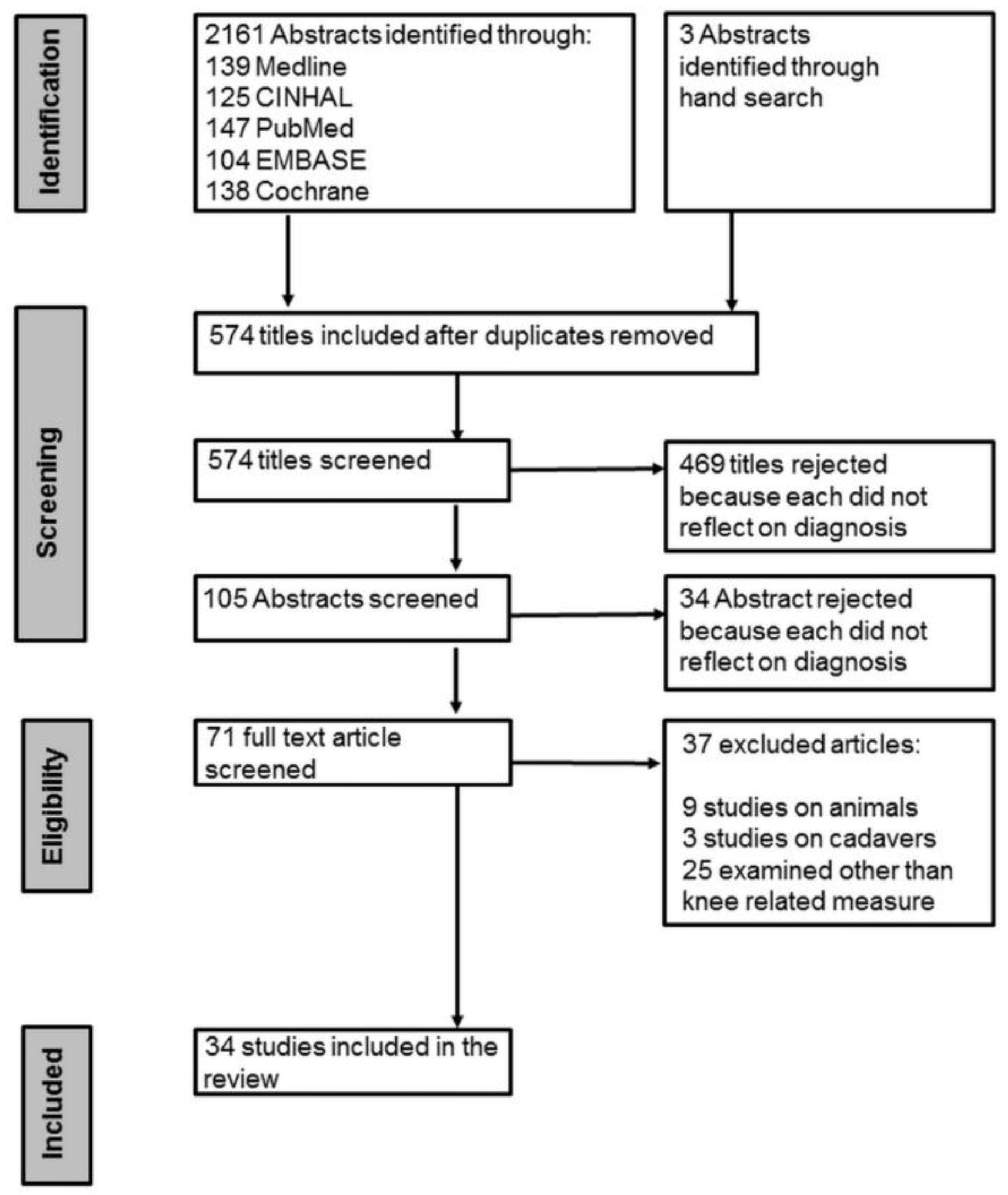
3.1. Selection of Studies
3.2. Quality Scores
3.3. Pooled Results from the Individual Knee Stability Measures
3.3.1. Quantitative Data
3.3.2. Qualitative Data
Lachman Test
Pivot Shift Test
Anterior Drawer Test
The Rolimeter
The Genucom Knee Analysis System
The KT-1000/KT-2000 Arthrometer
The Telos Stress Radiography Device
ACL-Hamstring Stretch Reflex
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ACL | Anterior Cruciate Ligament |
| MB | Mohamed Bakhsh |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| JA | Jawad Abulhasan |
| CA | Cameron Anley |
| QUADAS | Quality Assessment of Diagnostic Accuracy Studies |
| Mm | Millimetre |
| ITB | Iliotibial Band |
| ICC | Intra-class Correlation Coefficient |
| EMG | Electromyography |
| CI | Confidence Interval |
| MRI | Magnetic Resonance Image |
| MG | Michael Grey |
| MMF | Manual Muscle Force |
| AP | Anterior-Posterior |
References
- McCall, A.; Carling, C.; Davison, M.; Nedelec, M.; Le Gall, F.; Berthoin, S.; Dupont, G. Injury risk factors, screening tests and preventative strategies: A systematic review of the evidence that underpins the perceptions and practices of 44 football (soccer) teams from various premier leagues. Br. J. Sports Med. 2015, 49, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Ter Stege, M.H.; Dallinga, J.M.; Benjaminse, A.; Lemmink, K.A. Effect of interventions on potential, modifiable risk factors for knee injury in team ball sports: A systematic review. Sports Med. 2014, 44, 1403–1426. [Google Scholar] [CrossRef] [PubMed]
- Melnyk, M.; Faist, M.; Gothner, M.; Claes, L.; Friemert, B. Changes in stretch reflex excitability are related to “giving way” symptoms in patients with anterior cruciate ligament rupture. J. Neurophysiol. 2007, 97, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Gilchrist, J.; Mandelbaum, B.R.; Melancon, H.; Ryan, G.W.; Silvers, H.J.; Griffin, L.Y.; Watanabe, D.S.; Dick, R.W.; Dvorak, J. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am. J. Sports Med. 2008, 36, 1476–1483. [Google Scholar] [CrossRef] [PubMed]
- Mandelbaum, B.R.; Silvers, H.J.; Watanabe, D.S.; Knarr, J.F.; Thomas, S.D.; Griffin, L.Y.; Kirkendall, D.T.; Garrett, W. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-Year follow-up. Am. J. Sports Med. 2005, 33, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Ekstrand, J.; Hägglund, M.; Waldén, M. Injury incidence and injury patterns in professional football: The uefa injury study. Br. J. Sports Med. 2011, 45, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Prodromos, C.C.; Han, Y.; Rogowski, J.; Joyce, B.; Shi, K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury–reduction regimen. Arthroscopy 2007, 23, 1320–1325. [Google Scholar] [CrossRef] [PubMed]
- Pugh, L.; Mascarenhas, R.; Arneja, S.; Chin, P.Y.; Leith, J.M. Current concepts in instrumented knee-laxity testing. Am. J. Sports Med. 2009, 37, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Leblanc, M.-C.; Kowalczuk, M.; Andruszkiewicz, N.; Simunovic, N.; Farrokhyar, F.; Turnbull, T.; Debski, R.; Ayeni, O. Diagnostic accuracy of physical examination for anterior knee instability: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 2805–2813. [Google Scholar] [CrossRef] [PubMed]
- Barcellona, M.; Christopher, T.; Matthew, C.M. Bench testing of a knee joint arthrometer. Orthopedics 2013, 36, e1000–e1006. [Google Scholar] [CrossRef] [PubMed]
- Schoene, M.; Spengler, C.; Fahrbacher, B.; Hartmann, J.; Melnyk, M.; Friemert, B. The reliability of a method for measuring the anterior cruciate ligament-hamstring reflex: An objective assessment of functional knee instability. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 1107–1116. [Google Scholar] [CrossRef] [PubMed]
- Wiertsema, S.H.; van Hooff, H.J.A.; Migchelsen, L.A.A.; Steultjens, M.P.M. Reliability of the KT1000 arthrometer and the lachman test in patients with an acl rupture. Knee 2008, 15, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Kostov, H. Reliability assessment of arthroscopic findings versus MRI in ACL injuries of the knee. Acta Inform. Medica 2014, 22, 111–114. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: An updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br. J. Sports 2014, 48, 1543–1552. [Google Scholar] [CrossRef] [PubMed]
- Saltzman, B.M.; Cvetanovich, G.L.; Nwachukwu, B.U.; Mall, N.A.; Bush-Joseph, C.A.; Bach, B.R. Economic analyses in anterior cruciate ligament reconstruction: A qualitative and systematic review. Am. J. Sports Med. 2015. [Google Scholar] [CrossRef] [PubMed]
- Van Eck, C.F.; Loopik, M.; van den Bekerom, M.P.; Fu, F.H.; Kerkhoffs, G.M. Methods to diagnose acute anterior cruciate ligament rupture: A meta-analysis of instrumented knee laxity tests. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1989–1997. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.; Rutjes, A.; Reitsma, J.; Bossuyt, P.; Kleijnen, J. The development of quadas: A tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med. Res. Methodol. 2003, 3. [Google Scholar] [CrossRef] [PubMed]
- Hegedus, E.J.; Goode, A.; Campbell, S.; Morin, A.; Tamaddoni, M.; Moorman, C.T.; Cook, C. Physical examination tests of the shoulder: A systematic review with meta-analysis of individual tests. Br. J. Sports Med. 2008, 42, 80–92. [Google Scholar] [CrossRef] [PubMed]
- Anderson, A.F.; Lipscomb, A.B. Preoperative instrumented testing of anterior and posterior knee laxity. Am. J. Sports Med. 1989, 17, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Anderson, A.F.; Snyder, R.B.; Federspiel, C.F.; Lipscomb, A.B. Instrumented evaluation of knee laxity: A comparison of five arthrometers. Am. J. Sports Med. 1992, 20, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Balasch, H.; Schiller, M.; Friebel, H.; Hoffmann, F. Evaluation of anterior knee joint instability with the Rolimeter A test in comparison with manual assessment and measuring with the KT-1000 arthrometer. Knee Surg. Sports Traumatol. Arthrosc. 1999, 7, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Beard, D.; Kyberd, P.; Fergusson, C.; Dodd, C. Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need for surgery? J. Bone Jt. Surg. Br. Vol. 1993, 75, 311–315. [Google Scholar]
- Bach, B.R., Jr.; Warren, R.; Flynn, W.; Kroll, M.; Wickiewiecz, T. Arthrometric evaluation of knees that have a torn anterior cruciate ligament. J. Bone Jt. Surg. Am. 1990, 72, 1299–1306. [Google Scholar]
- Fleming, B.C.; Brattbakk, B.; Peura, G.D.; Badger, G.J.; Beynnon, B.D. Measurement of anterior–posterior knee laxity: A comparison of three techniques. J. Orthop. Res. 2002, 20, 421–426. [Google Scholar] [CrossRef]
- Forster, I.; Warren-Smith, C.; Tew, M. Is the KT1000 knee ligament arthrometer reliable? J. Bone Jt. Surg. Br. Vol. 1989, 71, 843–847. [Google Scholar]
- Friemert, B.; Bumann-Melnyk, M.; Faist, M.; Schwarz, W.; Gerngross, H.; Claes, L. Differentiation of hamstring short latency versus medium latency responses after tibia translation. Exp. Brain Res. 2005, 160, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ganko, A.; Engebretsen, L.; Ozer, H. The rolimeter: A new arthrometer compared with the KT-1000. Knee Surg. Sports Traumatol. Arthrosc. 2000, 8, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Graham, G.P.; Johnson, S.; Dent, C.M.; Fairclough, J.A. Comparison of clinical tests and the KT1000 in the diagnosis of anterior cruciate ligament rupture. Br. J. Sports Med. 1991, 25, 96–97. [Google Scholar] [CrossRef] [PubMed]
- Hanten, W.P.; Pace, M.B. Reliability of measuring anterior laxity of the knee joint using a knee ligament arthrometer. Phys. Ther. 1987, 67, 357–359. [Google Scholar] [PubMed]
- Highgenboten, C.L.; Jackson, A.; Meske, N.B. Genucom, KT-1000, and stryker knee laxity measuring device comparisons device reproducibility and interdevice comparison in asymptomatic subjects. Am. J. Sports Med. 1989, 17, 743–746. [Google Scholar] [CrossRef] [PubMed]
- Hoshino, Y.; Araujo, P.; Ahlden, M.; Moore, C.G.; Kuroda, R.; Zaffagnini, S.; Karlsson, J.; Fu, F.H.; Musahl, V. Standardized pivot shift test improves measurement accuracy. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 732–736. [Google Scholar] [CrossRef] [PubMed]
- Küpper, J.; Loitz-Ramage, B.; Corr, D.; Hart, D.; Ronsky, J. Measuring knee joint laxity: A review of applicable models and the need for new approaches to minimize variability. Clin. Biomech. 2007, 22, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, R.; Hoshino, Y.; Nagamune, K.; Kubo, S.; Nishimoto, K.; Araki, D.; Yamaguchi, M.; Yoshiya, S.; Kurosaka, M. Intraoperative measurement of pivot shift by electromagnetic sensors. Oper. Tech. Orthop. 2008, 18, 190–195. [Google Scholar] [CrossRef]
- Kuroda, R.; Hoshino, Y.; Araki, D.; Nishizawa, Y.; Nagamune, K.; Matsumoto, T.; Kubo, S.; Matsushita, T.; Kurosaka, M. Quantitative measurement of the pivot shift, reliability, and clinical applications. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 686–691. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Osti, L.; Henry, M.; Bocchi, L. The diagnosis of acute complete tears of the anterior cruciate ligament. Comparison of mri, arthrometry and clinical examination. J. Bone Jt. Surg. Br. Vol. 1995, 77, 586–588. [Google Scholar]
- Lopomo, N.; Zaffagnini, S.; Bignozzi, S.; Visani, A.; Marcacci, M. Pivot-shift test: Analysis and quantification of knee laxity parameters using a navigation system. J. Orthop. Res. 2010, 28, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Lopomo, N.; Zaffagnini, S.; Amis, A.A. Quantifying the pivot shift test: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 767–783. [Google Scholar] [CrossRef] [PubMed]
- Mitsou, A.; Vallianatos, P. Clinical diagnosis of ruptures of the anterior cruciate ligament: A comparison between the lachman test and the anterior drawer sign. Injury 1988, 19, 427–428. [Google Scholar] [CrossRef]
- Mulligan, E.P.; Harwell, J.L.; Robertson, W.J. Reliability and diagnostic accuracy of the lachman test performed in a prone position. J. Orthop. Sports Phys. Ther. 2011, 41, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Panisset, J.C.; Ntagiopoulos, P.G.; Saggin, P.R.; Dejour, D. A comparison of Telos™ stress radiography versus Rolimeter™ in the diagnosis of different patterns of anterior cruciate ligament tears. Orthop. Traumatol. Surg. Res. 2012, 98, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Sernert, N.; Kartus, J.; Köhler, K.; Ejerhed, L.; Karlsson, J. Evaluation of the reproducibility of the KT-1000 arthrometer. Scand. J. Med. Sci. Sports 2001, 11, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Steiner, M.E.; Brown, C.; Zarins, B.; Brownstein, B.; Koval, P.; Stone, P. Measurement of anterior-posterior displacement of the knee. J. Bone Jt. Surg. 1990, 72, 1307–1315. [Google Scholar]
- Tsuda, E.; Okamura, Y.; Otsuka, H.; Komatsu, T.; Tokuya, S. Direct evidence of the anterior cruciate ligament-hamstring reflex arc in humans. Am. J. Sports Med. 2001, 29, 83–87. [Google Scholar] [PubMed]
- Wroble, R.R.; van Ginkel, L.A.; Grood, E.S.; Noyes, F.R.; Shaffer, B.L. Repeatability of the KT-1000 arthrometer in a normal population. Am. J. Sports Med. 1990, 18, 396–399. [Google Scholar] [CrossRef] [PubMed]
- Monaco, E.; Labianca, L.; Maestri, B.; de Carli, A.; Conteduca, F.; Ferretti, A. Instrumented measurements of knee laxity: KT-1000 versus navigation. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 617–621. [Google Scholar] [CrossRef] [PubMed]
- Kopf, S.; Kauert, R.; Halfpaap, J.; Jung, T.; Becker, R. A new quantitative method for pivot shift grading. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 718–723. [Google Scholar] [CrossRef] [PubMed]
- Gurtler, R.A.; Stine, R.; Torg, J.S. Lachman test evaluated: Quantification of a clinical observation. Clin. Orthop. Relat. Res. 1987, 216, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Torg, J.S.; Conrad, W.; Kalen, V. Clinical I diagnosis of anterior cruciate ligament instability in the athlete. Am. J. Sports Med. 1976, 4, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Rebman, L.W. Suggestions from the field: Lachman’s test—An alternative method. J. Orthop. Sports Phys. Ther. 1988, 9, 381–382. [Google Scholar] [CrossRef]
- Draper, D.O.; Schulthies, S. A test for eliminating false positive anterior cruciate ligament injury diagnoses. J. Athl. Train. 1993, 28, 355–357. [Google Scholar] [PubMed]
- Dussik, K. Über die möglichkeit, hochfrequente mechanische schwingungen ALS diagnostisches hilfsmittel zu verwerten. Zeitschrift Für Die Gesamte Neurologie Und Psychiatrie 1942, 174, 153–168. [Google Scholar] [CrossRef]
- Muller, B.; Hofbauer, M.; Rahnemai-Azar, A.A.; Wolf, M.; Araki, D.; Hoshino, Y.; Araujo, P.; Debski, R.E.; Irrgang, J.J.; Fu, F.H. Development of computer tablet software for clinical quantification of lateral knee compartment translation during the pivot shift test. Comput. Methods Biomech. Biomed. Eng. 2015, 19, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Floyd, R.T.; Peery, D.S.; Andrews, J.R. Advantages of the prone lachman versus the traditional lachman. Orthopedics 2008, 31. [Google Scholar] [CrossRef]
- Galway, H.B.A.; Maclntosh, D.L. Pivot-shift: A clinical sign of symptomatic anterior cruciate defeciency. J. Bone Jt. Surg. Br. Vol. 1972, 54-B, 763–764. [Google Scholar]
- Kong, K.C.; Hamlet, M.R.; Peckham, T.; Mowbray, M.A.S. Displaced bucket handle tears of the medial meniscus masking anterior cruciate deficiency. Arch. Orthop. Trauma Surg. 1994, 114, 51–52. [Google Scholar] [CrossRef] [PubMed]
- Hoshino, Y.; Araujo, P.; Ahldén, M.; Samuelsson, K.; Muller, B.; Hofbauer, M.; Wolf, M.R.; Irrgang, J.J.; Fu, F.H.; Musahl, V. Quantitative evaluation of the pivot shift by image analysis using the ipad. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, T.; Althoff, B.; Peterson, L.; Renström, P. Clinical diagnosis of ruptures of the anterior cruciate ligament: A comparative study of the lachman test and the anterior drawer sign. Am. J. Sports Med. 1982, 10, 100–102. [Google Scholar] [CrossRef] [PubMed]
- Colombet, P.; Jenny, J.; Menetrey, J.; Plaweski, S.; Zaffagnini, S. Current concept in rotational laxity control and evaluation in ACL reconstruction. Orthop. Traumatol. Surg. Res. 2012, 98, S201–S210. [Google Scholar] [CrossRef] [PubMed]
- Scholten, R.; Opstelten, W.; van der Plas, C.G.; Bijl, D.; Deville, W.; Bouter, L.M. Accuracy of physical diagnostic tests for assessing ruptures of the anterior cruciate ligament: A meta-analysis. J. Fam. Pract. 2003, 52, 689–696. [Google Scholar] [PubMed]
- Cannon, W.D. Use of arthrometers to assess knee laxity and outcomes. Sports Med. Arthrosc. 2002, 10, 191–200. [Google Scholar] [CrossRef]
- Hirschmann, M.; Müller, W. Complex function of the knee joint: The current understanding of the knee. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 2780–2788. [Google Scholar] [CrossRef] [PubMed]
- Klos, T.V.; Habets, R.J.; Banks, A.Z.; Banks, S.A.; Devilee, R.J.; Cook, F.F. Computer assistance in arthroscopic anterior cruciate ligament reconstruction. Clin. Orthop. Relat. Res. 1998, 354, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Lopomo, N.; Bignozzi, S.; Martelli, S.; Zaffagnini, S.; Iacono, F.; Visani, A.; Marcacci, M. Reliability of a navigation system for intra-operative evaluation of antero-posterior knee joint laxity. Comput. Biol. Med. 2009, 39, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Colombet, P.; Robinson, J.; Christel, P.; Franceschi, J.-P.; Djian, P. Using navigation to measure rotation kinematics during ACL reconstruction. Clin. Orthop. Relat. Res. 2007, 454, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Pearle, A.D.; Solomon, D.J.; Wanich, T.; Moreau-Gaudry, A.; Granchi, C.C.; Wickiewicz, T.L.; Warren, R.F. Reliability of navigated knee stability examination a cadaveric evaluation. Am. J. Sports Med. 2007, 35, 1315–1320. [Google Scholar] [CrossRef] [PubMed]
- Degenhart, M. Computer-navigated ACL reconstruction with the orthopilot. Surg. Technol. Int. 2004, 12, 245–251. [Google Scholar] [PubMed]
- Mcquade, K.J.; Sidles, J.A.; Larson, R.V. Reliability of the genucom knee analysis system. A pilot study. Clin. Orthop. Relat. Res. 1989, 245, 216–219. [Google Scholar] [PubMed]
- Daniel, D.M.; Malcom, L.L.; Losse, G.; Stone, M.L.; Sachs, R.; Burks, R. Instrumented measurement of anterior laxity of the knee. J. Bone Jt. Surg. Am. 1985, 67, 720–726. [Google Scholar]
- Isberg, J.; Faxèn, E.; Brandsson, S.; Eriksson, B.; Kärrholm, J.; Karlsson, J. KT-1000 records smaller side-to-side differences than radiostereometric analysis before and after an ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Jardin, C.; Chantelot, C.; Migaud, H.; Gougeon, F.; Debroucker, M.; Duquennoy, A. Reliability of the KT-1000 arthrometer in measuring anterior laxity of the knee: Comparative analysis with telos of 48 reconstructions of the anterior cruciate ligament and intra-and interobserver reproducibility. Rev. Chir. Orthop. Répar. Appar. Mot. 1999, 85, 698–707. [Google Scholar]
- Stäubli, H.-U.; Jakob, R.P. Anterior knee motion analysis measurement and simultaneous radiography. Am. J. Sports Med. 1991, 19, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.A.; Hegedus, E.J.; Lenchik, L.; Kuhn, K.J.; Santiago, L.; Smoliga, J.M. Diagnostic accuracy of various imaging modalities for suspected lower extremity stress fractures: A systematic review with evidence-based recommendations for clinical practice. Am. J. Sports Med. 2015. [Google Scholar] [CrossRef] [PubMed]
- Melnyk, M.; Gollhofer, A. Submaximal fatigue of the hamstrings impairs specific reflex components and knee stability. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Jennings, A.; Seedhom, B. Proprioception in the knee and reflex hamstring contraction latency. J. Bone Jt. Surg. Br. Vol. 1994, 76, 491–494. [Google Scholar]
- Friemert, B.; Faist, M.; Spengler, C.; Gerngross, H.; Claes, L.; Melnyk, M. Intraoperative direct mechanical stimulation of the anterior cruciate ligament elicits short- and medium-latency hamstring reflexes. J. Neurophysiol. 2005, 94, 3996–4001. [Google Scholar] [CrossRef] [PubMed]
- Reiman, M.P.; Goode, A.P.; Hegedus, E.J.; Cook, C.E.; Wright, A.A. Diagnostic accuracy of clinical tests of the hip: A systematic review with meta-analysis. Br. J. Sports Med. 2012. [Google Scholar] [CrossRef] [PubMed]
- Rosen, A.; Ko, J.; Brown, C. Diagnostic accuracy of instrumented and manual talar tilt tests in chronic ankle instability populations. Scand. J. Med. Sci. Sports 2015, 25, e214–e221. [Google Scholar] [CrossRef] [PubMed]
- Reiman, M.P.; Loudon, J.K.; Goode, A.P. Diagnostic accuracy of clinical tests for assessment of hamstring injury: A systematic review. J. Orthop. Sports Phys. Ther. 2013, 43, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Musahl, V.; Hoshino, Y.; Ahlden, M.; Araujo, P.; Irrgang, J.; Zaffagnini, S.; Karlsson, J.; Fu, F. The pivot shift: A global user guide. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Rozzi, S.L.; Lephart, S.M.; Gear, W.S.; Fu, F.H. Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am. J. Sports Med. 1999, 27, 312–319. [Google Scholar] [PubMed]
- Waldén, M.; Hägglund, M.; Werner, J.; Ekstrand, J. The epidemiology of anterior cruciate ligament injury in football (soccer): A review of the literature from a gender-related perspective. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Marsh, J.D.; Birmingham, T.B.; Giffin, J.R.; Isaranuwatchai, W.; Hoch, J.S.; Feagan, B.G.; Litchfield, R.; Willits, K.; Fowler, P. Cost-effectiveness analysis of arthroscopic surgery compared with non-operative management for osteoarthritis of the knee. BMJ Open 2016, 6. [Google Scholar] [CrossRef] [PubMed]
- Grobbelaar, N.; Bouffard, J.A. Sonography of the knee, a pictorial review. Semin. Ultrasound CT MR 2000, 21, 231–274. [Google Scholar] [CrossRef]
| Medline, CINHAL, EMBASE, PubMed and Cochrane |
|---|
| “Knee laxity” |
| KT-1000 |
| KT-2000 |
| ACL and stability |
| “Laxity testing” and knee |
| “Physical examination” and knee |
| “Instrumented devices” and knee |
| “Stability testing” and knee |
| Instability and knee |
| Imaging and knee |
| Lachman |
| Genucome |
| Rolimeter |
| “Pivot shift” |
| “Anterior drawer” |
| Authors | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anderson and Lipscomp [19] | Y | Y | Y | Y | Y | N | Y | N | Y | U | Y | Y | Y | N | 10 |
| Anderson et al. [20] | Y | Y | Y | N | Y | N | Y | Y | N | N | Y | Y | Y | N | 9 |
| Balasch et al. [21] | Y | Y | Y | Y | U | N | Y | Y | Y | U | Y | Y | N | N | 9 |
| Beard et al. [22] | Y | Y | Y | Y | Y | Y | Y | Y | N | N/A | Y | Y | N | N | 10 |
| Bach et al. [23] | Y | Y | Y | N | Y | Y | Y | Y | N | N | Y | Y | N | U | 9 |
| Fleming et al. [24] | Y | Y | Y | Y | N | Y | Y | Y | Y | N | U | Y | N | N | 9 |
| Forster, Warren-Smith and Tew [25] | Y | Y | Y | U | U | N | Y | Y | Y | Y | Y | U | N | U | 8 |
| Friemert et al. [26] | Y | Y | Y | Y | N | Y | Y | Y | Y | U | U | Y | Y | Y | 11 |
| Ganko, Engebretsen and Ozer [27] | Y | Y | Y | Y | Y | N | Y | Y | Y | U | U | Y | N | U | 9 |
| Graham et al. [28] | Y | U | Y | Y | Y | Y | N | N | N | U | U | Y | Y | U | 7 |
| Hanten and Pace [29] | Y | Y | Y | U | U | Y | Y | Y | Y | N | U | Y | N | U | 8 |
| Highgenboten, Jackson and Meske [30] | Y | Y | Y | U | U | Y | Y | N | N | U | U | Y | N | U | 6 |
| Hoshino et al. [31] | Y | N | Y | U | U | Y | Y | Y | N | U | Y | U | U | U | 6 |
| Kupper et al. [32] | Y | N | Y | U | U | U | U | Y | N | Y | U | Y | U | U | 5 |
| Kuroda et al. [33] | N | N | Y | U | U | Y | U | Y | U | U | Y | Y | U | U | 5 |
| Kuroda et al. [34] | Y | N | Y | U | U | Y | U | Y | U | U | Y | Y | U | U | 6 |
| Liu et al. [35] | Y | N | Y | Y | Y | Y | Y | N | N | Y | Y | Y | N | Y | 10 |
| Lopomo et al. [36] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | U | 12 |
| Lopomo, Zaffagnini and Amis [37] | Y | Y | Y | Y | N | Y | Y | Y | Y | U | Y | U | Y | U | 10 |
| Melnyk and Gollhofer [3] | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | U | U | 11 |
| Mitsou and Vallianatos [38] | Y | Y | N | N | N | U | U | Y | U | N | N | N | N | N | 3 |
| Mulligan, Harwell and Robertson [39] | Y | Y | Y | Y | U | U | Y | Y | U | Y | Y | Y | Y | Y | 11 |
| Panisset et al., 2012 [40] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | U | 12 |
| Pugh et al. [8] | Y | N | Y | U | U | U | U | Y | N | Y | Y | Y | U | U | 6 |
| Schoene et al. [11] | Y | Y | Y | U | U | Y | Y | Y | Y | Y | U | Y | Y | U | 10 |
| Sernert et al. [41] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | U | 12 |
| Steiner et al. [42] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | U | U | 11 |
| Tsuda et al. [43] | Y | Y | Y | U | U | Y | Y | U | Y | Y | Y | Y | U | U | 9 |
| Wroble et al. [44] | Y | N | Y | Y | N | N | U | N | N | N | Y | Y | U | U | 5 |
| Barcellona et al. [10] | Y | N | Y | Y | N | Y | Y | N | N | U | U | Y | N | N | 6 |
| Van Eck et al. [16] | Y | Y | Y | Y | U | Y | Y | Y | U | Y | Y | Y | Y | Y | 12 |
| Monaco et al. [45] | Y | U | Y | Y | N | Y | Y | Y | N | Y | U | Y | U | U | 8 |
| Kopf et al. [46] | Y | N | Y | U | N | U | N | Y | N | U | U | Y | Y | U | 5 |
| Leblanc et al. [9] | Y | Y | Y | U | Y | Y | Y | Y | Y | N | U | Y | Y | Y | 11 |
| Authors | Devices/Technique Studied | Sample Size | Age, Mean | Sensitivity/Specificity, p < 0.05 | Conclusion | QUADAS Quality Score | Effect Size |
|---|---|---|---|---|---|---|---|
| Anderson and Lipscomp [19] | KT-1000, Lachman test, anterior drawer, pivot shift | 50 | 19.8 | N/A | Clinical examination by an experienced examiner is the most accurate method to determine ACL integrity; however, instrumented testing was beneficial | 10 | N/A |
| Anderson et al. [20] | KT-1000, Genucom, Acufex, Dyonics dynamic cruciate tester | 100 | 26 | N/A | This study establishes that anterior knee laxity measurements cannot be generalized from one device to another in both normal and ACL-injured participants | 9 | 0.2 |
| Bach et al. [23] | KT-1000 | 401 | Not mentioned | At manual maximum force (MMF), sensitivity = 79%, specificity = 77%; at 89 Newton, sensitivity = 75%, specificity = 83% | KT-1000 is a helpful knee laxity measure adjunct to a careful history and physical examination of ACL-injured patients | 9 | 0.0 |
| Balasch et al. [21] | Rolimeter | 60 | 33.6 | N/A | Rolimeter provides an economic, exact and simple operating device for quantifying anterior knee joint instability | 9 | N/A |
| Barcellona et al. [10] | KT-2000 | 3 KT-Arthrometers | N/A | N/A | KT-2000 knee joint arthrometers overestimates anterior displacement with a predictable relative systematic error | 6 | N/A |
| Beard et al. [22] | Reflex Hamstring Contraction Latency (RHCL) | 30 | 24.8 | N/A | The reflex hamstring contraction latency is a measure of proprioception and can be used to provide objective data for the management of patients with ACL deficiency | 10 | 1.46 |
| Van Eck et al. [16] | KT-1000, Genucom, anterior drawer | Review article | N/A | Sensitivity of KT-1000 = 0.93, anterior drawer = 0.74; Genucom = 0,76; specificity of KT-1000 = 0.93 , anterior drawer = 0.82; Genucom = 0.76 | The KT arthrometer performed with maximum manual force has the highest sensitivity, specificity and accuracy for diagnosing ACL rupture | 12 | N/A |
| Fleming et al. [24] | KT-1000, planer stress radiography, RSA | 15 | 34 | N/A | KT-1000 and RSA document temporal changes in anterior-posterior knee laxity following ACL reconstruction that were not documented by planer stress radiography | 9 | 0.42 |
| Forster, Warren-Smith and Tew [25] | KT-1000 | 10 | 30 | N/A | The KT-1000 was not capable of overcoming result variation and providing reliable and reproducible measurement of laxity of the ACL | 8 | 0.8 |
| Friemert et al. [26] | Reflex Hamstring Contraction Latency (RHCL) | 13 | 24.6 ± 5.5 | N/A | Short and medium latency responses of the hamstring stretch reflex exist after an ACL stimulation during isometric hamstring contraction | 11 | 0.15 |
| Ganko, Engebretsen and Ozer [27] | Rolimeter | 38 | 27.4 | Sensitivity = 89%, specificity = 95% | The rolimeter, when compared to the KT-1000, provides a valid measure of anterior knee laxity | 9 | 0.6 |
| Graham et al. [28] | Lachman test, anterior drawer, KT-1000 | 21 | Not mentioned | N/A | Anterior drawer and the Lachman test were found to be the most accurate indicators of ACL deficiency; the KT-1000 was found to be totally inaccurate | 7 | N/A |
| Hanten and Pace [29] | KT-1000 | 43 | 18.5 | N/A | Our results indicated relatively high reliability of KT-1000 and clinician can use such tool to get objective and reliable AP knee laxity measurements | 8 | N/A |
| Highgenboten, Jackson and Meske [30] | Genucom, KT-1000, Stryker | 30 | Not mentioned | N/A | All devices can provide reproducible quantitative measurements of knee laxity; however, due to differences in device sensitivities and design, numerical results from one device cannot be generalized to another device | 6 | 0.6 |
| Hoshino et al. [31] | Quantitative pivot shift test | 5 | Not mentioned | N/A | The sudden shift of the lateral compartment of the knee joint was successfully detected by the newly-developed image analysis measurement method | 6 | 0 |
| Kupper et al. [32] | KT-1000, Genucom, Stryker, rolimeter | Review article | N/A | N/A | The development of theoretical models that accurately represent knee joint laxity in combination with more precise and repeatable clinical assessment of ACL injuries should lead to an improved understanding of joint laxity and the factors associated with acute injury and genetic pathologies that affect joint stability | 5 | N/A |
| Kuroda et al. [33] | Pivot shift test | 30 | 21.2 | N/A | The new non-invasive measurement system enables monitoring instantaneous 3D position displacement of the knee by using an electromagnetic sensor; these measurements can be used for quantified evaluation of dynamic instability demonstrated by the pivot shift test | 5 | N/A |
| Kuroda et al. [34] | Quantitative pivot shift test | Review article | N/A | N/A | Accumulative biomechanical and clinical evidence have shown the usefulness of quantitative assessment of the pivot shift test | 6 | N/A |
| Liu et al. [35] | MRI, KT-1000, Lachman test, anterior drawer, pivot shift | 38 | 26 | KT-1000 sensitivity = 97%, Lachman test sensitivity = 95%, MRI sensitivity = 97%; specificity for all measure was not mentioned | No significant differences between the results of the Lachman test and the KT-1000, but these were significantly better than MRI and anterior drawer; it has been shown that inexpensive tests can allow treatment to proceed rapidly and in the most economical manner without the routine use of MRI | 10 | N/A |
| Lopomo et al. [36] | Pivot shift test | 18 | 33 | The PS test was reliable in identifying the surgical reconstruction. Correlation analysis showed good coefficients both for pre- (r = 0.7; p < 0.05) and post-operative (r = 0.9; p < 0.05) values | The new quantification method of the pivot shift test could be helpful in characterizing patient-specific knee laxity, thus quantifying the clinical relevance of the test | 12 | N/A |
| Lopomo, Zaffagnini and Amis [37] | Quantitative pivot shift test | Review article | N/A | N/A | Several methodologies have been identified to quantify the pivot shift test; clinicians are still lacking the “gold standard’’ method of the quantitative pivot shift test | 11 | N/A |
| Melnyk and Gollhofer [3] | Submaximal fatigue exercises of hamstring | 15 | 25 ± 2.6 | N/A | Submaximal hamstring fatigue is associated with a mechanical loss of knee stability; this instability might explain at least in part a higher risk of ACL injury | 11 | 1 |
| Mitsou and Vallianatos [38] | Lachman test, anterior drawer | 144 | Not mentioned | Not mentioned | The diagnostic accuracy of the Lachman test in recent ruptures when the patient is examined without general anaesthetic is superior to that of the anterior drawer test, while in chronic cases with third-degree instability, the two tests are equally reliable | 3 | N/A |
| Mulligan, Harwell and Robertson [39] | Lachman test | 52 | 34 | Sensitivity = 70%, specificity = 97% | The prone Lachman test is a reliable technique that can be used to confirm the presence of an ACL tear | 11 | N/A |
| Panisset et al. [40] | Telos, rolimeter, clinical examination | 177 | 30.2 ± 11.7 | Sensitivity of Telos combined with CE = 88%, sensitivity of rolimeter combined with CE = 72.7; specificity of Telos combined with CE = 94.6%, specificity of rolimeter combined with CE = 92.4 | The combination of clinical examination with telos was more accurate than with rolimeter | 12 | 0.49 |
| Pugh et al. [8] | KT-1000, rolimeter, Telos, Genucom, Acufex, Dyonics dynamics cruciate tester, UCLA, Vermont | Review article | N/A | N/A | The KT-1000 knee arthrometer and the rolimeter provide the best results when testing anterior laxity at the knee, whereas the Telos device is superior for the assessment of posterior laxity | 6 | N/A |
| Schoene et al. [11] | Reflex Hamstring Contraction Latency (RHCL) | 34 | 20 | N/A | The study has demonstrated that the investigated method of measuring the ACL-hamstring reflex is both reliable and reproducible | 10 | 0.7 |
| Sernert et al. [41] | KT-1000 | 40 | 29 | Control group; sensitivity = 50%, specificity = 70% ; experimental group; sensitivity = 60%, specificity = 70% | The reproducibility of the KT-1000 measurements of anterior knee laxity between two experienced examiners was considered as fair | 12 | 0.1 |
| Steiner et al. [42] | KT-1000, Stryker, Genucom, Acufex | 28 | 25 | Sensitivity of Acufex = 90%, KT-1000 = 80%; Stryker = 85%; Genucom = 60%; specificity of Acufex = 85%, KT-1000 = 70%. Stryker = 70%, Genucom = 65% | We recommend the use of Acufex, KT-1000 and Stryker, as they had more reproducible measurements than Genucom, as it tended to report greater differences in displacement between the right and left knees of normal participants | 11 | 0.2 |
| Tsuda et al. [43] | Reflex Hamstring Contraction Latency (RHCL) | 9 | 30 | N/A | ACL-hamstring reflex arc exists after an isometric hamstring contraction | 9 | N/A |
| Wroble et al. [44] | KT-1000 | 6 | 26 | N/A | KT-1000 standard evaluation should report paired differences rather than individual knee measurements and should be supplemented by clinical examination | 5 | N/A |
| Monaco et al. [45] | KT-1000, navigation system | 30 | 29 (range 19 to 39) | N/A | This study validates the accuracy of the KT-1000 to exactly calculate anterior-posterior (AP) translation of the tibia, in comparison with the more accurate measurements obtained using a navigation system | 8 | 0.13 |
| Kopf et al. [46] | Pivot shift test | 20 | 27.8 (range 23.2 to 32.4) | N/A | Quantification of the pivot shift test is practicable when inertial sensors are used | 5 | N/A |
| Leblanc et al. [9] | Lachamn, pivot shift, anterior drawer and MRI | Review article | Lachman, all ruptures type 89%, complete rupture 96%, partial rupture 68%; pivot shift, all rupture types 79%, complete rupture 86%, practical rupture 67%; no data for other measures | Decreased sensitivity of Lachman and pivot shift tests for partial ACL rupture cases and for awake patients raised suspicions regarding the accuracy of these tests for the diagnosis of ACL insufficiency | 11 | N/A |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abulhasan, J.F.; Snow, M.D.; Anley, C.M.; Bakhsh, M.M.; Grey, M.J. An Extensive Evaluation of Different Knee Stability Assessment Measures: A Systematic Review. J. Funct. Morphol. Kinesiol. 2016, 1, 209-229. https://doi.org/10.3390/jfmk1020209
Abulhasan JF, Snow MD, Anley CM, Bakhsh MM, Grey MJ. An Extensive Evaluation of Different Knee Stability Assessment Measures: A Systematic Review. Journal of Functional Morphology and Kinesiology. 2016; 1(2):209-229. https://doi.org/10.3390/jfmk1020209
Chicago/Turabian StyleAbulhasan, Jawad F., Martyn D. Snow, Cameron M. Anley, Mohammad M. Bakhsh, and Michael J. Grey. 2016. "An Extensive Evaluation of Different Knee Stability Assessment Measures: A Systematic Review" Journal of Functional Morphology and Kinesiology 1, no. 2: 209-229. https://doi.org/10.3390/jfmk1020209
APA StyleAbulhasan, J. F., Snow, M. D., Anley, C. M., Bakhsh, M. M., & Grey, M. J. (2016). An Extensive Evaluation of Different Knee Stability Assessment Measures: A Systematic Review. Journal of Functional Morphology and Kinesiology, 1(2), 209-229. https://doi.org/10.3390/jfmk1020209





