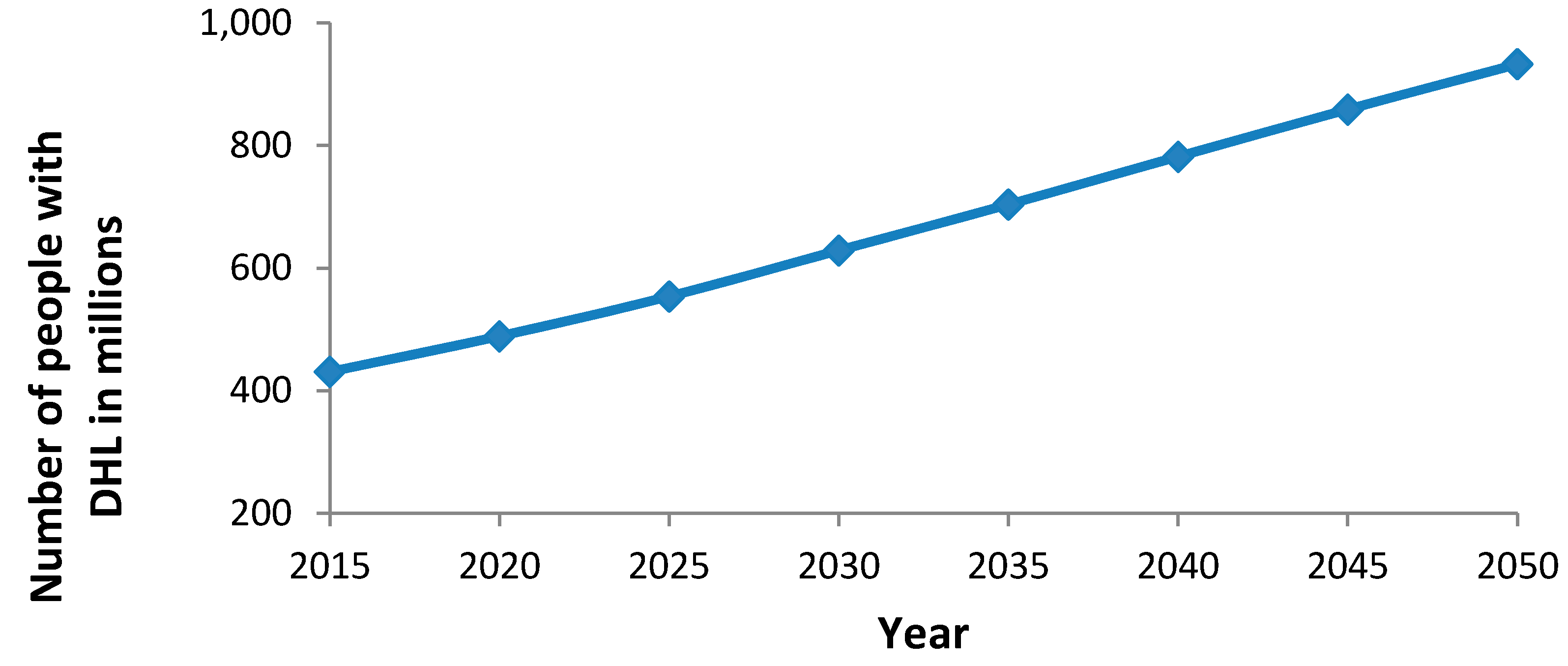
Newborn and Infant Hearing Screening Facing Globally Growing Numbers of People Suffering from Disabling Hearing Loss
Abstract
1. Introduction
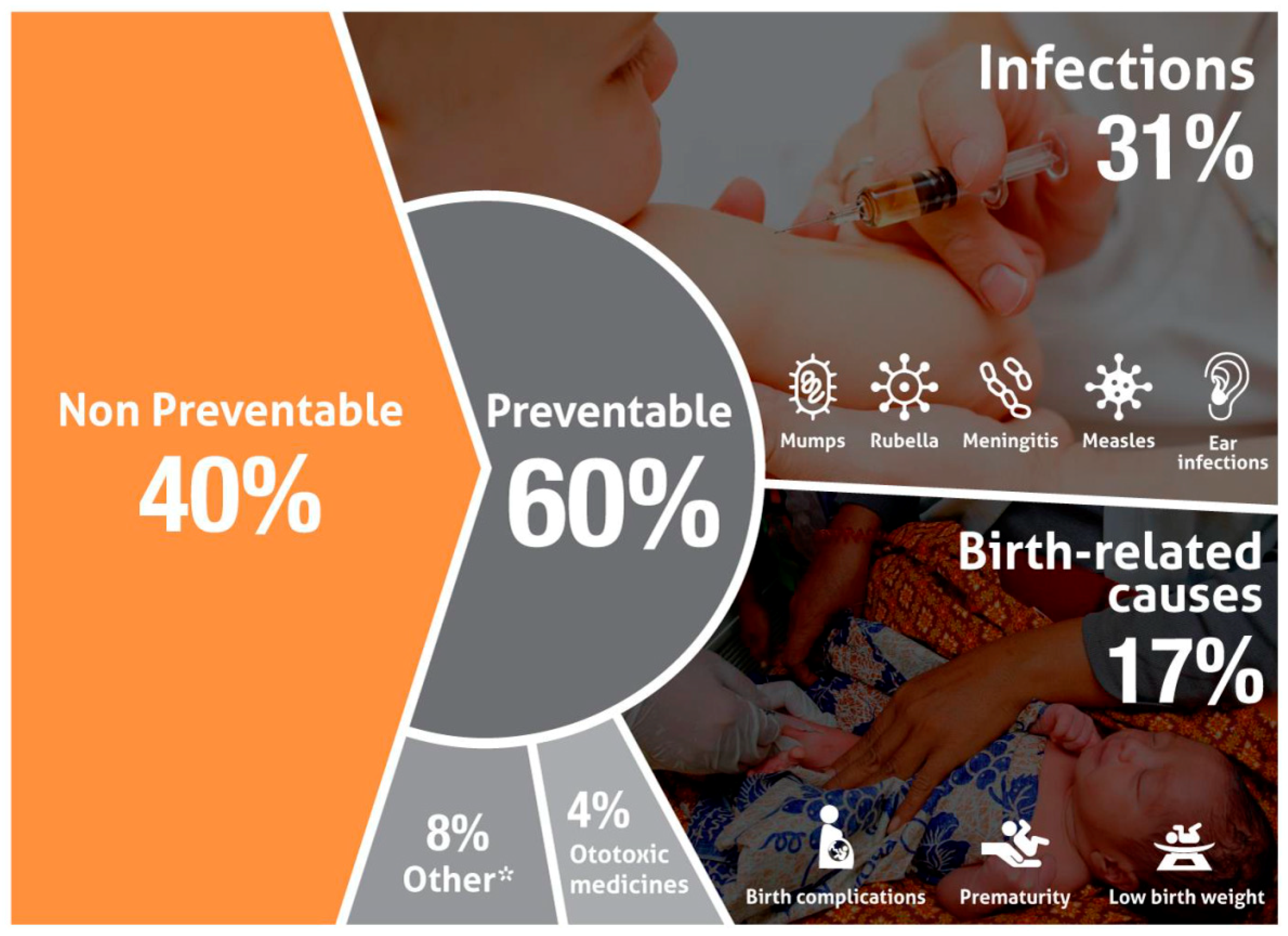
2. Prevention of Childhood Hearing Loss
3. Relevance and Principles of Newborn Hearing Screening
- A universal newborn hearing screening program should involve at least 95% of the newborns in a region.
- Newborn hearing screening procedures should target the detection of at least all infants with bilateral hearing loss of ≥35 dB in the better hearing ear.
- The proportion of babies who fail the newborn hearing screen and are referred for formal audiological testing should not exceed 4%.
- The false negative rate for babies who passed the screening despite a substantial hearing loss should approach zero.
- At least 95% of the babies failing the screening should be followed up with audiological diagnostics and, in cases of confirmed hearing loss, receive appropriate treatment.
- The follow-up and access to diagnosis and treatment should be well organized, so that parents whose babies have failed the hearing screening can be referred directly to medical and audiological service centers that are qualified to provide accurate diagnostics and appropriate treatment for infants.
- The audiometric diagnostics should be completed before 3 months of age and treatment for those with hearing loss should be initiated before 6 months of age.
- NIHS programs should include a data collection system to ensure that the program meets the criteria specified above and is capable of tracking babies who have failed or missed the screening.
- Procedures and tools for training and supervision of the people carrying out hearing screening should be implemented to ensure that screening is properly done.
- Family history of permanent childhood sensorineural hearing loss
- In-utero infection of mothers (e.g., cytomegalovirus, rubella, herpes, syphilis, and toxoplasmosis)
- Syndromes which may be associated with hearing loss (Down, Waardenburg, Pendred, Jervell, Lange–Nielson), or stigmata and findings associated with such syndromes (such as white forelock for Waardenburg syndrome)
- Craniofacial malformations, including those that involve the pinna and/or ear canal, such as ear tags, ear pits, and temporal bone anomalies
- Diseases or conditions that require extended neonatal intensive care
- Persistent pulmonary hypertension associated with mechanical ventilation, and conditions requiring the use of extracorporeal membrane oxygenation
- Elevated levels of hyperbilirubinemia
- Exposure to ototoxic medications (aminoglycosides, loop diuretics)
- Postnatal infections associated with hearing loss such as bacterial meningitis
4. Newborn and Infant Hearing Screening as Part of a National Plan on Ear and Hearing Care
5. Further Actions Regarding NIHS Programs
6. Suggestions for Moving Forward
7. Conclusions
Funding
Conflicts of Interest
References
- World Health Organization. Addressing the Rising Prevalence of Hearing Loss. Available online: http://apps.who.int/iris/bitstream/handle/10665/260336/9789241550260-eng.pdf?sequence=1&ua=1 (accessed on 3 November 2018).
- Cunningham, L.L.; Tucci, D.L. Hearing loss in adults. N. Engl. J. Med. 2017, 377, 2465–2473. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Prevention of Blindness and Deafness. Grades of Hearing Impairment. Available online: http://www.who.int/pbd/deafness/hearing_impairment_grades/en/ (accessed on 3 November 2018).
- World Health Organization. Prevention of Blindness and Deafness. Estimates. Global Estimates on Prevalence of Hearing Loss. Available online: http://www.who.int/pbd/deafness/estimates/en/ (accessed on 3 November 2018).
- World Health Organization. Deafness and Hearing Loss. Key Facts. Available online: http://www.who.int/mediacentre/factsheets/fs300/en/ (accessed on 3 November 2018).
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; et al. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- Wilson, B.S.; Tucci, D.L.; Merson, M.H.; O’Donoghue, G.M. Global hearing health care: New findings and perspectives. Lancet 2017, 390, 2503–2515. [Google Scholar] [CrossRef]
- Chadha, S.; Cieza, A.; Krug, E. Global hearing health: Future directions. Bull. World Health Organ. 2018, 96, 146. [Google Scholar] [CrossRef] [PubMed]
- Olusanya, B.O.; Neumann, K.J.; Saunders, J.E. The global burden of disabling hearing impairment: A call to action. Bull. World Health Organ. 2014, 92, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, I.; Smith, A. Deafness—The neglected and hidden disability. Ann. Trop. Med. Parasitol. 2009, 103, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Joint Committee on Infant Hearing, American Academy of Pediatrics; Muse, C.; Harrison, J.; Yoshinaga-Itano, C.; Grimes, A.; Brookhouser, P.E.; Epstein, S.; Buchman, C.; Mehl, A.; Vohr, B.; et al. Supplement to the JCIH 2007 position statement: Principles and guidelines for early intervention after confirmation that a child is deaf or hard of hearing. Pediatrics 2013, 131, e1324–e1349. [Google Scholar] [CrossRef]
- Pimperton, H.; Blythe, H.; Kreppner, J.; Mahon, M.; Peacock, J.L.; Stevenson, J.; Terlektsi, E.; Worsfold, S.; Yuen, H.M.; Kennedy, C.R. The impact of universal newborn hearing screening on long-term literacy outcomes: A prospective cohort study. Arch. Dis. Child. 2016, 101, 9–15. [Google Scholar] [CrossRef]
- World Health Organization. Neonatal and Infant Hearing Screening. Current Issues and Guiding Principles for Action. In Proceedings of the Outcome of a WHO Informal Consultation, Geneva, Switzerland, 9–10 November 2009; World Health Organization: Geneva, Switzerland, 2010; pp. 1–39, ISBN 978 92 4 159949 6. [Google Scholar]
- The Lancet. Hearing loss: Time for sound action. Lancet 2017, 390, 2414. [Google Scholar] [CrossRef]
- World Health Organization. Disability. World Report on Disability. p. 102. Available online: http://www.who.int/disabilities/world_report/2011/en/ (accessed on 3 November 2018).
- World Health Organization. Prevention of Blindness and Deafness. WHA48.9 Prevention of Hearing Impairment. Available online: http://www.who.int/pbd/publications/wha_eb/wha48_9/en/ (accessed on 3 November 2018).
- World Health Organization. Multi-Country Assessment of National Capacity to Provide Hearing care. In WHO Documents & Publications. 2013. Available online: https://www.who.int/pbd/publications/WHOReportHearingCare_Englishweb.pdf (accessed on 3 November 2018).
- World Health Organization. Childhood Hearing Loss: Strategies for Prevention and Care, 1st ed.; World Health Organization: Geneva, Switzerland, 2016; pp. 1–28. ISBN 978 92 4 151032 5. [Google Scholar]
- World Health Organization. Global Costs of Unaddressed Heading Loss and Cost-Effectiveness of Intervention. Available online: http://apps.who.int/iris/bitstream/handle/10665/254659/9789241512046-eng.pdf?sequence=1 (accessed on 3 November 2018).
- World Health Organization. Ear and Hearing Care: Situation Analysis Tool, 1st ed.; World Health Organization: Geneva, Switzerland, 2016; pp. 1–60. ISBN 978 92 4 150995 4. [Google Scholar]
- World Health Organization. Planning & Monitoring of National Strategies for Ear and Hearing Care: A Manual, 1st ed.; World Health Organization: Geneva, Switzerland, 2016; pp. 1–36. ISBN 978 92 4 154947 9 5. [Google Scholar]
- World Health Organization. Seventieth World Health Assembly, Provisional Agenda Item 15.8. A70/34. 4 May 2017. Prevention of Deafness and Hearing Loss. Available online: http://apps.who.int/gb/ebwha/pdf_files/WHA70/A70_R13-en.pdf (accessed on 3 November 2018).
- Hoth, S.; Neumann, K. Das OAE-Handbuch. Otoakustische Emissionen in der Praxis, 1st ed.; Thieme: Stuttgart, Germany, 2006; pp. 92–96, ISBN 3-13-142561-X, 978-3-13-142561-4. [Google Scholar]
- Hoth, S.; Mühler, R.; Neumann, K.; Walger, M. Objektive Audiometrie im Kindesalter, 1st ed.; Springer: Berlin, Germany, 2014; p. 239, ISBN 978-3-642-44935-2, 978-3-642-44936-9. [Google Scholar] [CrossRef]
- Zimmerman, E.; Lahav, A. Ototoxicity in preterm infants: Effects of genetics, aminoglycosides, and loud environmental noise. J. Perinatol. 2013, 33, 3–8. [Google Scholar] [CrossRef]
- Dettman, S.J.; Pinder, D.; Briggs, R.J.; Dowell, R.C.; Leigh, J.R. Communication development in children who receive the cochlear implant younger than 12 months: Risks versus benefits. Ear Hear 2007, 28, 11S–18S. [Google Scholar] [CrossRef] [PubMed]
- Kral, A.; Sharma, A. Developmental neuroplasticity after cochlear implantation. Trends Neurosci. 2012, 35, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Nelson, H.D.; Bougatsos, C.; Nygren, P. 2001 US Preventive Services Task Force. Universal newborn hearing screening: Systematic review to update the 2001 U.S. Preventive Services Task Force Recommendation. Pediatrics 2008, 122, e266–e276. [Google Scholar] [CrossRef] [PubMed]
- Neumann, K.; Gross, M.; Böttcher, P.; Euler, H.A.; Spormann-Lagodzinski, M.; Polzer, M. Effectiveness and efficiency of a universal newborn hearing screening in Germany. Folia Phoniatr. Logop. 2006, 58, 440–455. [Google Scholar] [CrossRef]
- Yoshinaga-Itano, C.; Sedey, A.L.; Coulter, D.K.; Mehl, A.L. Language of early- and later-identified children with hearing loss. Pediatrics 1998, 102, 1161–1171. [Google Scholar] [CrossRef] [PubMed]
- Ching, T.Y.; Crowe, K.; Martin, V.; Day, J.; Mahler, N.; Youn, S.; Street, L.; Cook, C.; Orsini, J. Language development and everyday functioning of children with hearing loss assessed at 3 years of age. Int. J. Speech Lang. Pathol. 2010, 12, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Ching, T.Y.C.; Dillon, H.; Leigh, G.; Cupples, L. Learning from the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study: Summary of 5-year findings and implications. Int. J. Audiol. 2018, 57, S105–S111. [Google Scholar] [CrossRef]
- National Institutes of Health. Early identification of hearing impairment in infants and young children. NIH Consens. Statement 1993, 11, 1–24. [Google Scholar]
- American Academy of Pediatrics, Task Force on Newborn and Infant Hearing. Newborn and Infant Hearing Loss: Detection and Intervention. Pediatrics 1999, 103, 527–530. [Google Scholar] [CrossRef]
- American Academy of Pediatrics, Joint Committee on Infant Hearing. Joint Committee on Infant Hearing 1994 Position Statement. Pediatrics 1995, 95, 152–156. [Google Scholar]
- Joint Committee on Infant Hearing; American Academy of Audiology; American Academy of Pediatrics; American Speech-Language-Hearing Association; Directors of Speech and Hearing Programs in State Health and Welfare Agencies. Year 2000 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics 2000, 106, 798–817. [Google Scholar]
- American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics 2007, 120, 898–921. [Google Scholar] [CrossRef] [PubMed]
- Grandori, F.; Lutman, M.E. European Consensus Statement on Neonatal Hearing Screening. Finalised at the European Consensus Development Conference on Neonatal Hearing Screening, 15–16 May 1998, Milan. Int. J. Pediatr. Otorhinolaryngol. 1998, 44, 309–310. [Google Scholar] [CrossRef] [PubMed]
- Neumann, K. Current status of newborn and infant hearing screening programs in Africa and how to set up a well-functioning program in a resource limited setting. In Proceedings of the All Africa ENT and Audiology Congress, Kigali, Rwanda, 20–22 June 2016; pp. 38–39. [Google Scholar]
- Böttcher, P.; Matulat, P. Enhanced strategies in screening—Tracking—Follow-up. Different approaches from Germany, Iran, Uzbekistan, and Georgia. In Proceedings of the 8th Annual Coalition for Global Hearing Health, University of Miami, Miami, FL, USA, 12–14 October 2017. [Google Scholar]
- Matulat, P.; Lepper, I.; Böttcher, P.; Parfitt, R.; Oswald, H.; Am Zehnhoff-Dinnesen, A.; Deuster, D. Two-Way Radio Modem Data Transfer for Newborn Hearing Screening Devices. Telemed. J. e-Health 2017, 23, 49–54. [Google Scholar] [CrossRef] [PubMed]
- de Swanepoel, W.; Hall, J.W., 3rd. A systematic review of telehealth applications in audiology. Telemed. J. e-Health 2010, 16, 181–200. [Google Scholar] [CrossRef] [PubMed]
- Bright, T.; Mulwafu, W.; Thindwa, R.; Zuurmond, M.; Polack, S. Reasons for low uptake of referrals to ear and hearing services for children in Malawi. PLoS ONE 2017, 12, e0188703. [Google Scholar] [CrossRef] [PubMed]
- Friderichs, N.; Swanepoel, D.; Hall, J.W., 3rd. Efficacy of a community-based infant hearing screening program utilizing existing clinic personnel in Western Cape, South Africa. Int. J. Pediatr. Otorhinolaryngol. 2012, 76, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Olusanya, B.O.; Emokpae, A.; Renner, J.K.; Wirz, S.L. Costs and performance of early hearing detection programmes in Lagos, Nigeria. Trans. R. Soc. Trop. Med. Hyg. 2009, 103, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Uilenburg, N.; Kauffman-de Boer, M.; van der Ploeg, K.; Oudesluys-Murphy, A.M.; Verkerk, P. An implementation study of neonatal hearing screening in the Netherlands. Int. J. Audiol. 2009, 48, 108–116. [Google Scholar] [CrossRef]
- Smith, R.J.H.; Bale, J.F., Jr.; White, K.R. Sensorineural hearing loss in children. Lancet 2005, 18, 879–890. [Google Scholar] [CrossRef]
- Oudesluys-Murphy, A.M.; van Straaten, H.L.; Bholasingh, R.; van Zanten, G.A. Neonatal hearing screening. Eur. J. Pediatr. 1996, 155, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Deltenre, P.; Van Maldergem, L. Hearing loss and deafness in the pediatric population: Causes, diagnosis, and rehabilitation. Handb. Clin. Neurol. 2013, 113, 1527–1538. [Google Scholar] [CrossRef] [PubMed]
- Morton, C.C.; Nance, W.E. Newborn hearing screening—A silent revolution. N. Engl. J. Med. 2006, 354, 2151–2164. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Violence Prevention Alliance. Building Global Commitment to Violence Prevention. Available online: https://www.who.int/violenceprevention/en/ (accessed on 3 November 2018).
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neumann, K.; Chadha, S.; Tavartkiladze, G.; Bu, X.; White, K.R. Newborn and Infant Hearing Screening Facing Globally Growing Numbers of People Suffering from Disabling Hearing Loss. Int. J. Neonatal Screen. 2019, 5, 7. https://doi.org/10.3390/ijns5010007
Neumann K, Chadha S, Tavartkiladze G, Bu X, White KR. Newborn and Infant Hearing Screening Facing Globally Growing Numbers of People Suffering from Disabling Hearing Loss. International Journal of Neonatal Screening. 2019; 5(1):7. https://doi.org/10.3390/ijns5010007
Chicago/Turabian StyleNeumann, Katrin, Shelly Chadha, George Tavartkiladze, Xingkuan Bu, and Karl R. White. 2019. "Newborn and Infant Hearing Screening Facing Globally Growing Numbers of People Suffering from Disabling Hearing Loss" International Journal of Neonatal Screening 5, no. 1: 7. https://doi.org/10.3390/ijns5010007
APA StyleNeumann, K., Chadha, S., Tavartkiladze, G., Bu, X., & White, K. R. (2019). Newborn and Infant Hearing Screening Facing Globally Growing Numbers of People Suffering from Disabling Hearing Loss. International Journal of Neonatal Screening, 5(1), 7. https://doi.org/10.3390/ijns5010007



