Postoperative Complicated Appendectomy Revealing Crohn’s Disease in a Pediatric Patient
Abstract
Introduction
Case report
Discussions
- −
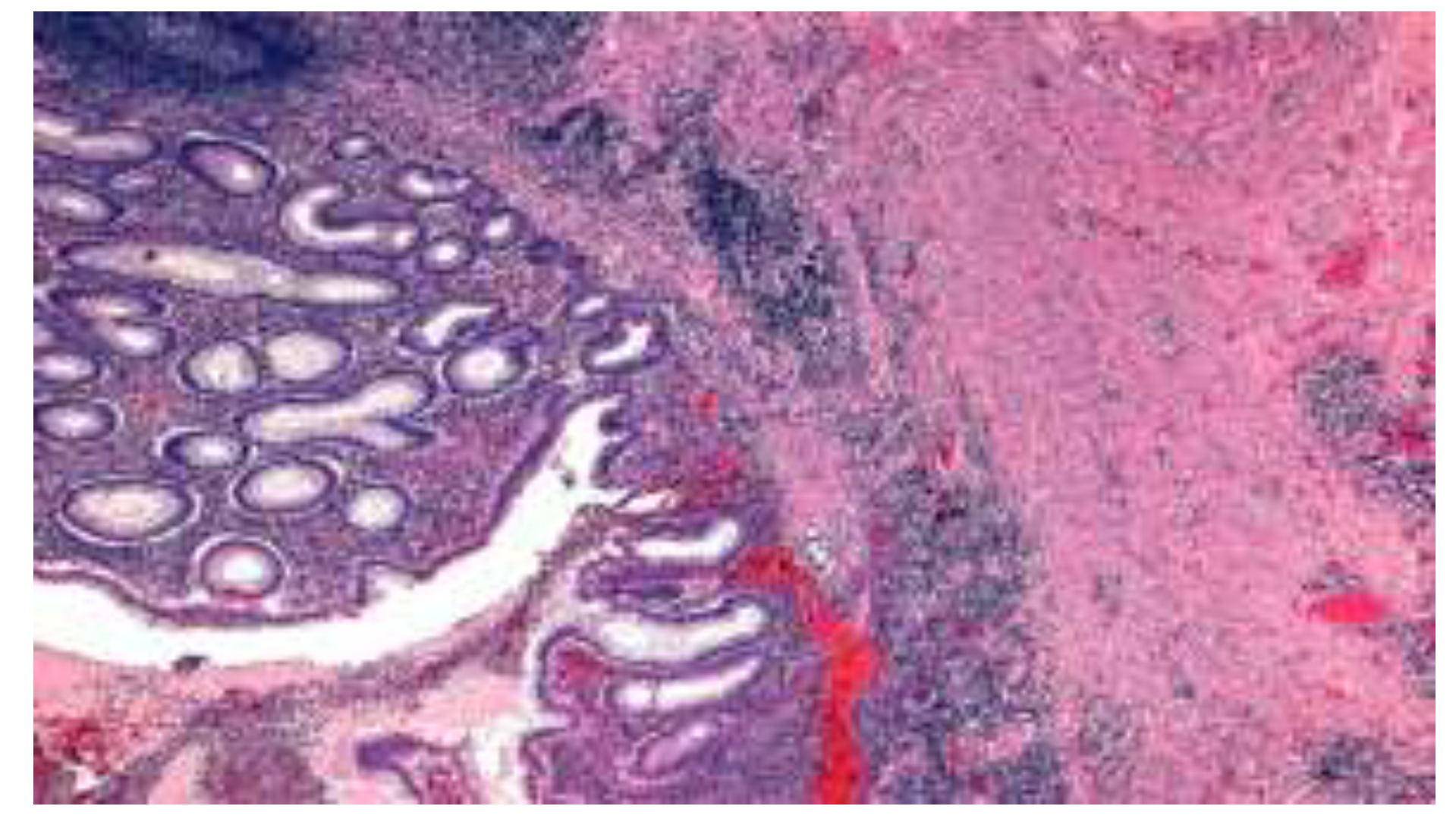
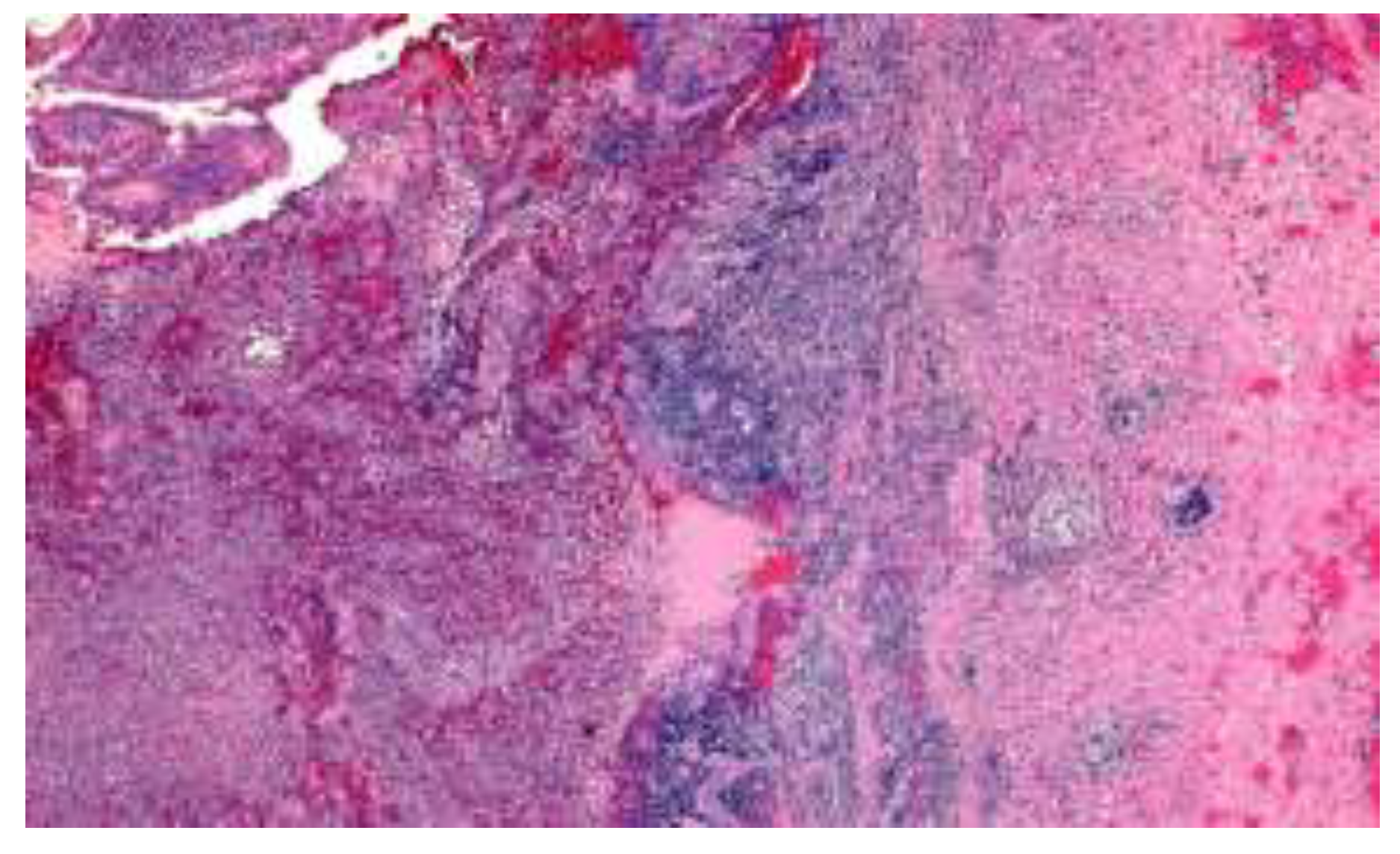
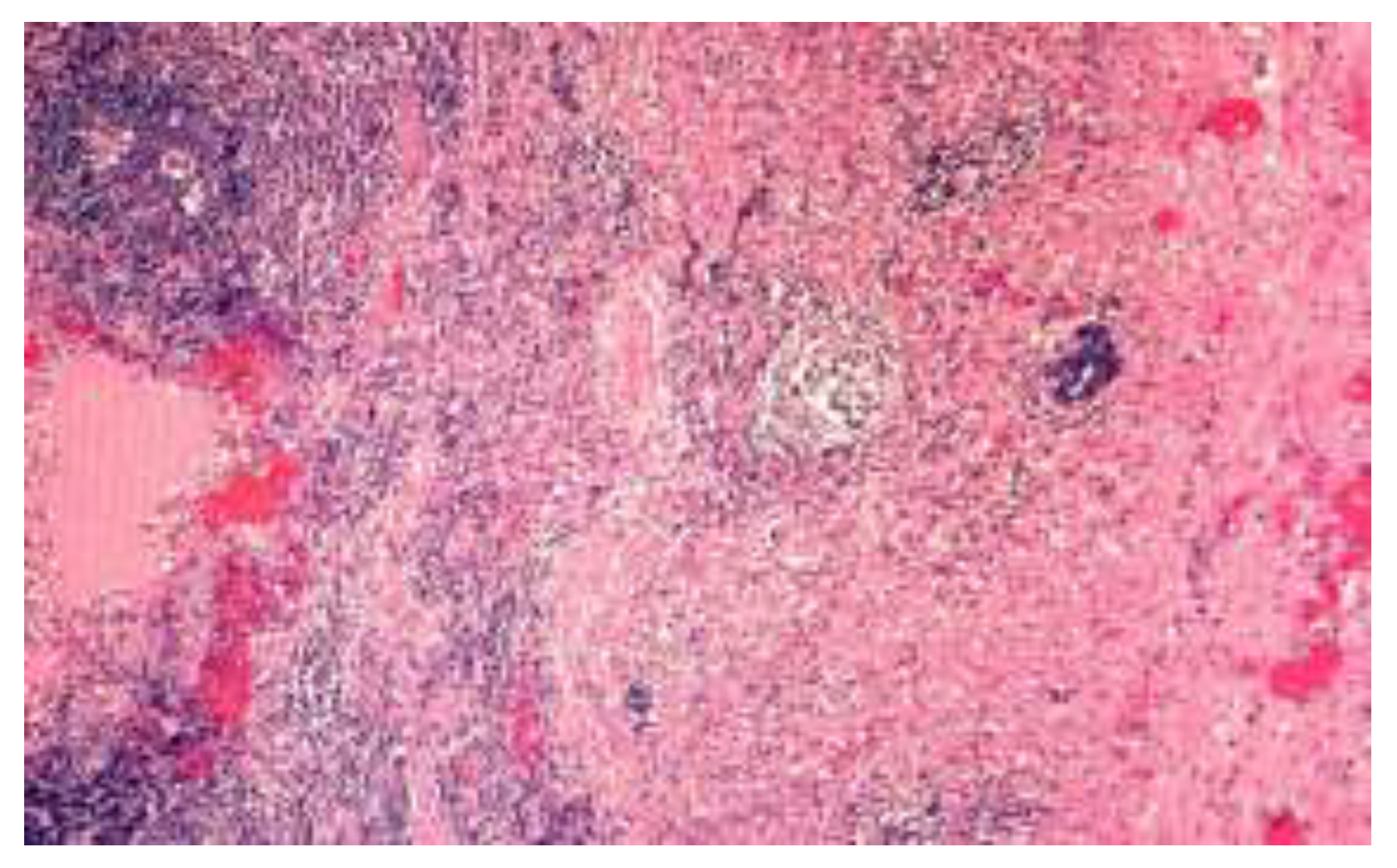
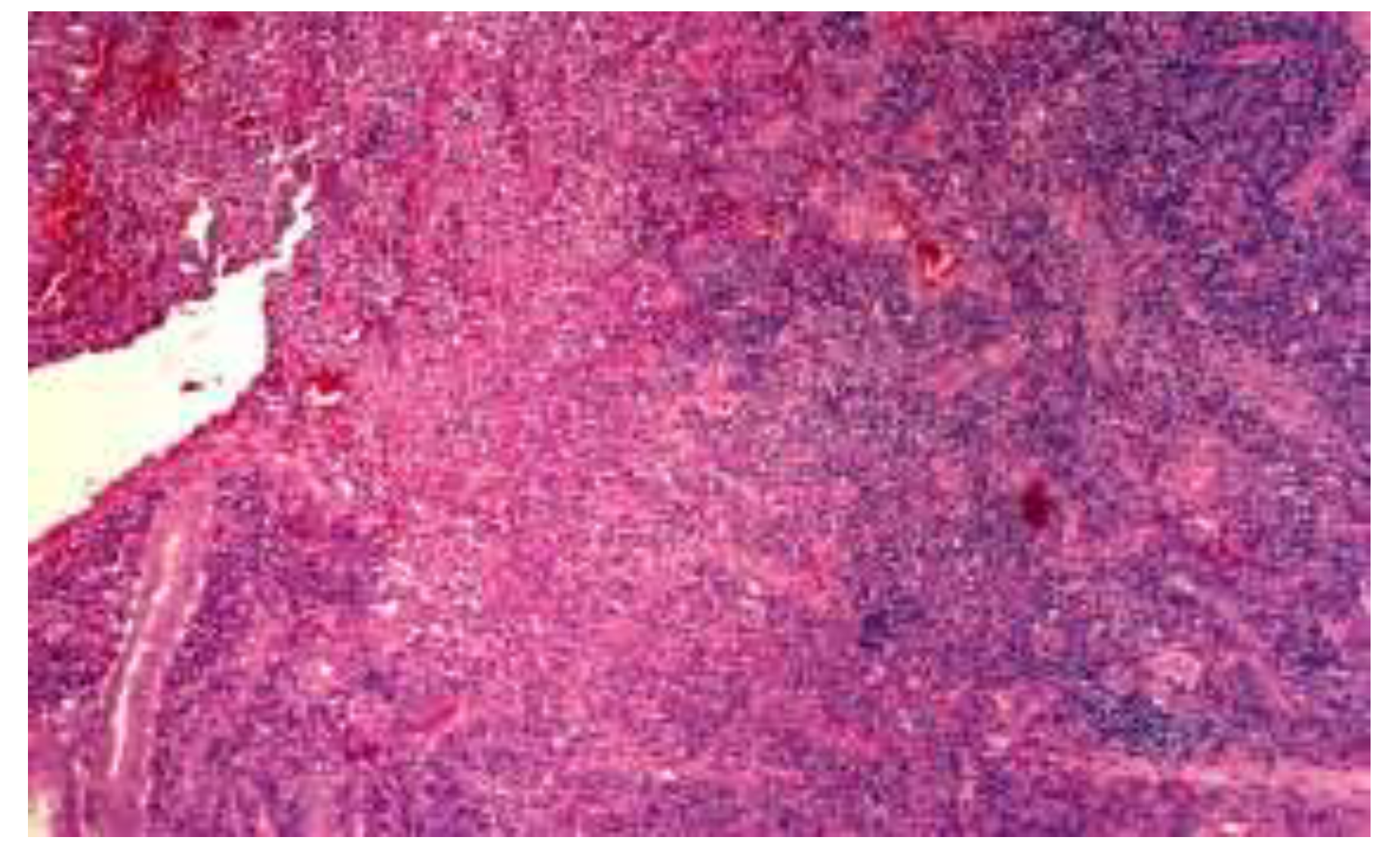
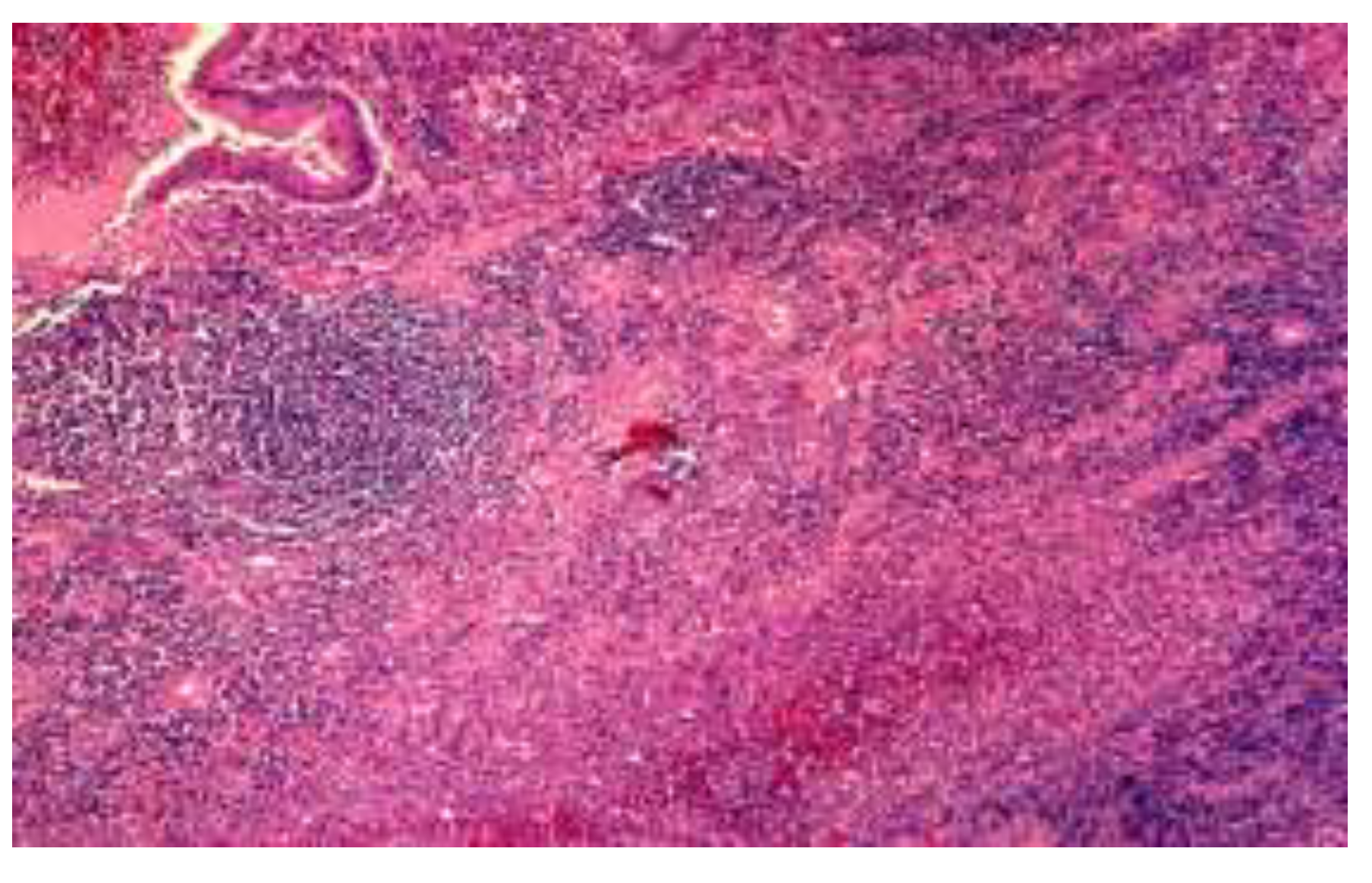
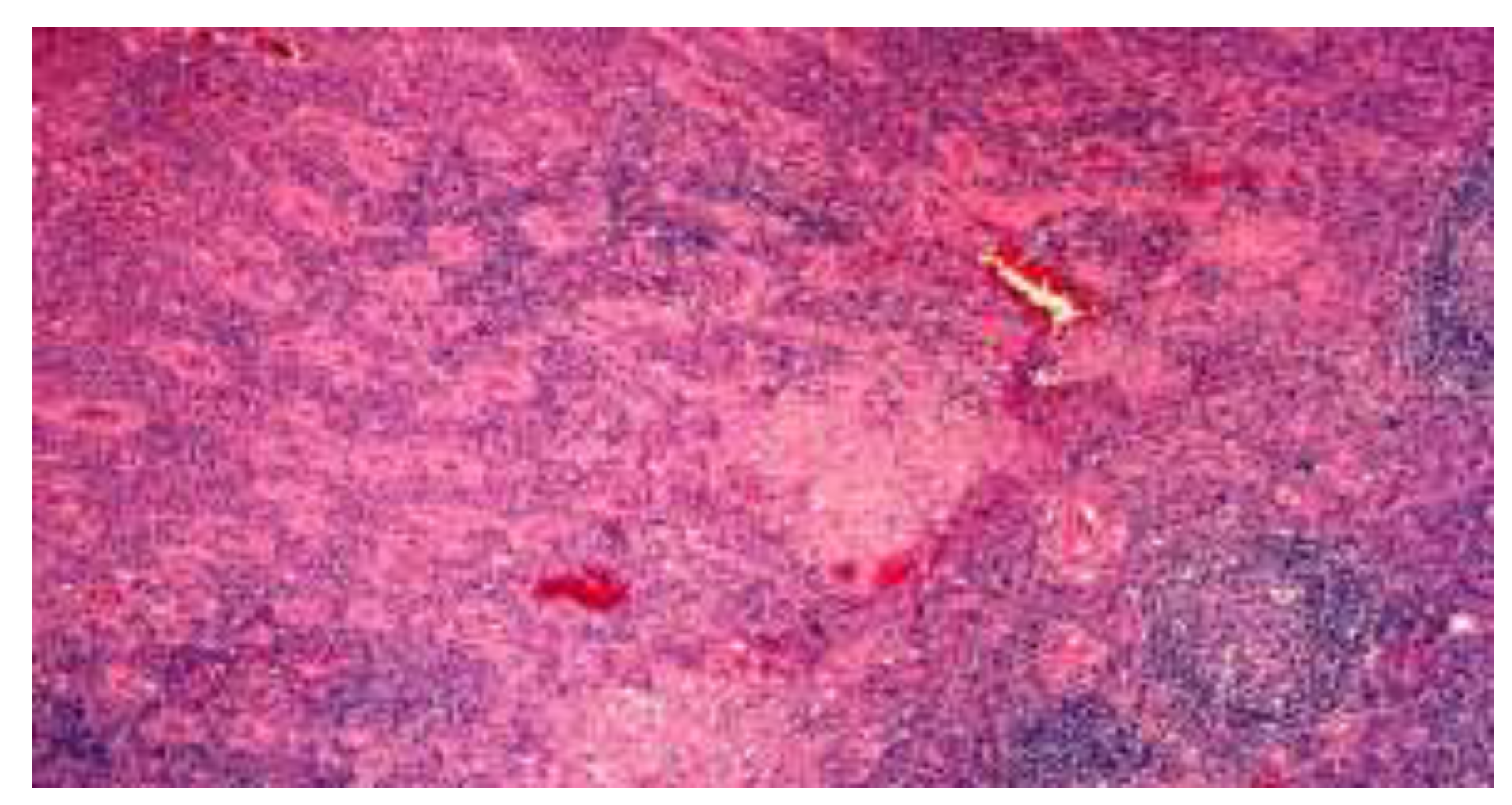
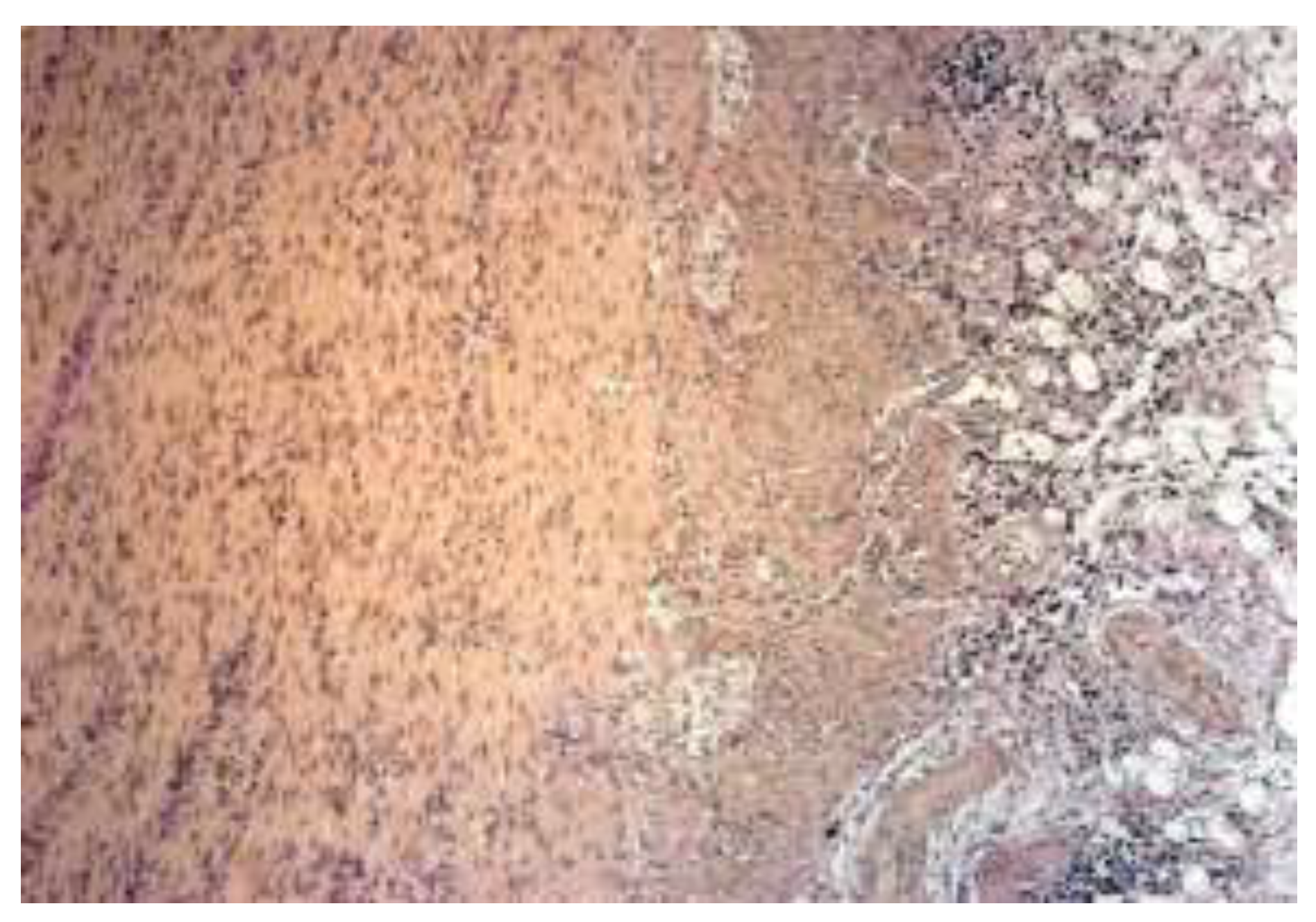
- the focal or the discontinuous inflammation of the mucosa with or without the lengthening and distortion of the crypts, with predomination of histiocytes and lymphocytes in the inflammatory infiltrate.
- −
- epithelioid granulomas.
- −
- the presence of lymphoid aggregates at the border of the muscularis propria and subserosa, associated with the infiltration of the muscular layer by mononuclear leukocytes in most cases [30].
Highlights
- ✓
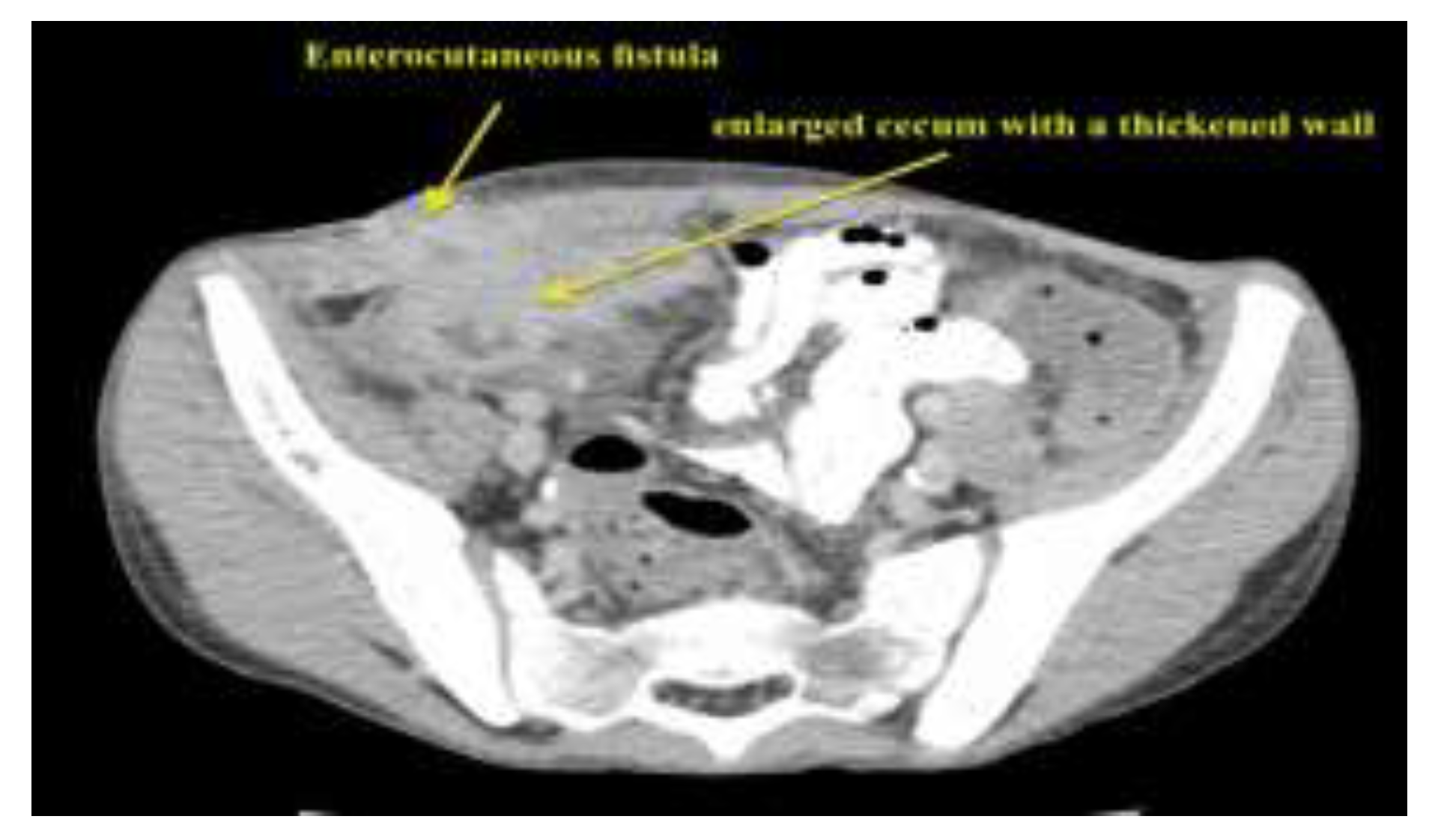
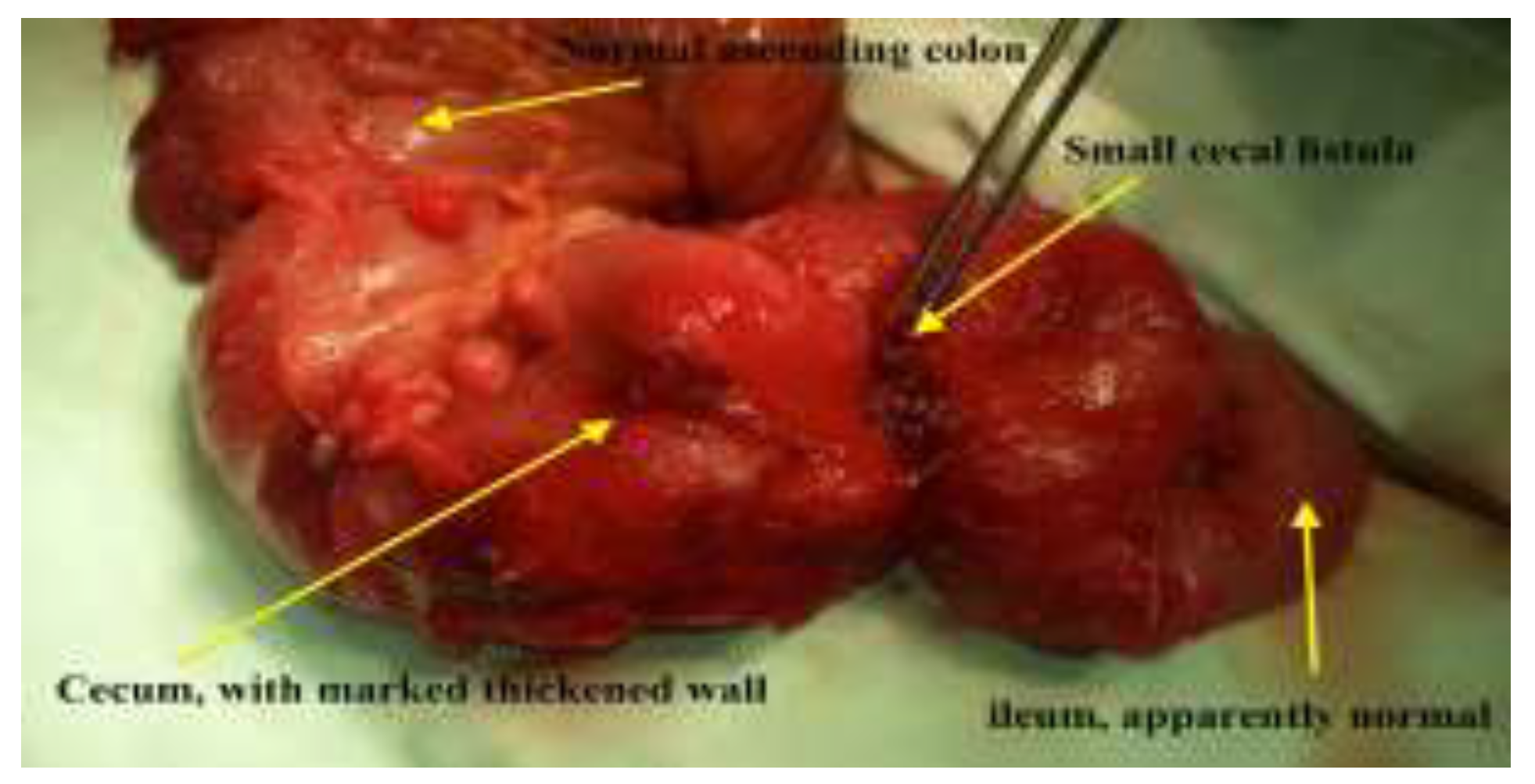
- The entero-cutaneous fistula is a severe postoperative complication of appendectomy. In rare cases, its underlying cause is granulomatous appendectomy – an initial manifestation of Crohn’s disease.
- ✓
- The patient we present did not have any relevant history of Crohn’s disease. The histopathological examination of the appendix played an important role in the final diagnosis, accounting for the aggravating evolution of the patient who had undergone appendectomy.
Conclusions
Abbreviations
Conflict of interest disclosure
Compliance with ethical standards
References
- Blair, N.P.; Bugis, S.P.; Turner, L.J.; MacLeod, M.M. Review of the pathologic diagnoses of 2,216 appendectomy specimens. Am J Surg. 1993, 165, 618–620. [Google Scholar] [CrossRef]
- Meyerding, E.V.; Bertram, H.F. Nonspecific granulomatous inflammation (Crohn's disease) of the appendix; a case report. Surgery. 1953, 34, 891–894. [Google Scholar] [PubMed]
- Bronner, M.P. Granulomatous appendicitis and the appendix in idiopathic inflammatory bowel disease. Semin Diagn Pathol. 2004, 21, 98–107. [Google Scholar] [CrossRef]
- Yayla, D.; Alpman, B.N.; Dolek, Y. Granulomatous appendicitis in a 12-year-old boy. J Pediatr Surg. 2010, 45, e27-9. [Google Scholar] [CrossRef] [PubMed]
- Richards, M.L.; Aberger, F.J.; Landercasper, J. Granulomatous appendicitis: Crohn's disease, atypical Crohn's or not Crohn's at all? J Am Coll Surg. 1997, 185, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Genier, F.; Plattner, V.; Letessier, E.; Armstrong, O.; Heloury, Y.; Le Neel, J.C. Fistules caecales post-appendicectomies. A propos de vingt-deux cas [Post-appendectomy fistulas of the cecum. Apropos of 22 cases]. J Chir (Paris). 1995, 132, 393–398. [Google Scholar]
- Orangio, G.R. Enterocutaneous fistula: medical and surgical management including patients with Crohn's disease. Clin Colon Rectal Surg. 2010, 23, 169–175. [Google Scholar] [CrossRef]
- Serban, D.; Spataru, R.I.; Vancea, G.; Balasescu, S.A.; Socea, B.; Tudor, C.; Dascalu, A.M. Informed consent in all surgical specialties: from legal obligation to patient satisfaction. Rom J Leg Med. 2020, 28, 317–321. [Google Scholar] [CrossRef]
- Ham, M.; Longhi, M.S.; Lahiff, C.; Cheifetz, A.; Robson, S.; Moss, A.C. Vitamin D levels in adults with Crohn's disease are responsive to disease activity and treatment. Inflamm Bowel Dis. 2014, 20, 856–860. [Google Scholar] [CrossRef]
- Fletcher, J.; Cooper, S.C.; Ghosh, S.; Hewison, M. The Role of Vitamin D in Inflammatory Bowel Disease: Mechanism to Management. Nutrients. 2019, 11, 1019. [Google Scholar] [CrossRef]
- Stanescu, A.M.A.; Grajdeanu, I.V.; Iancu, M.A.; Stoian, A.P.; Bratu, O.G.; Socea, B.; Socea, L.I.; Diaconu, C.C. Correlation of Oral Vitamin D Administration with the Severity of Psoriasis and the Presence of Metabolic Syndrome. Rev Chim. 2018, 69, 1668–1672. [Google Scholar] [CrossRef]
- Stoian, A.P.; Elian, V.; Nitipir, C.; Negoita, O.; Iancu, D.M.; Ditu, G. Association between vitamin D insufficiency and metabolic syndrome. INTERDIAB 2017: DIABETES MELLITUS IN INTERNAL MEDICINE Book Series: International Conference on Interdisciplinary Management of Diabetes Mellitus and its Complications. 2017; 232–242. [Google Scholar]
- Dragasevic, S.; Stankovic, B.; Kotur, N.; Sokic-Milutinovic, A.; Milovanovic, T.; Lukic, S.; Milosavljevic, T.; Srzentic Drazilov, S.; Klaassen, K.; Pavlovic, S.; Popovic, D. Metabolic Syndrome in Inflammatory Bowel Disease: Association with Genetic Markers of Obesity and Inflammation. Metab Syndr Relat Disord. 2020, 18, 31–38. [Google Scholar] [CrossRef]
- Suceveanu, A.I.; Stoian, A.P.; Parepa, I.; Voinea, C.; Hainarosie, R.; Manuc, D.; Nitipir, C.; Mazilu, L.; Suceveanu, A.P. Gut Microbiota Patterns in Obese and Type 2 Diabetes (T2D) Patients from Romanian Black Sea Coast Region. Rev Chim. 2018, 69, 2260–2267. [Google Scholar] [CrossRef]
- Yorulmaz, E.; Adali, G.; Yorulmaz, H.; Ulasoglu, C.; Tasan, G.; Tuncer, I. Metabolic syndrome frequency in inflammatory bowel diseases. Saudi J Gastroenterol. 2011, 17, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Boyd, H.A.; Basit, S.; Harpsøe, M.C.; Wohlfahrt, J.; Jess, T. Inflammatory Bowel Disease and Risk of Adverse Pregnancy Outcomes. PLoS One. 2015, 10, e0129567. [Google Scholar] [CrossRef] [PubMed]
- Dimitriu, M.; Stoian, A.P.; Rosu, G.; Dan, A.; Caimacan, A.; Zygouropoulos, N.; Jacotă – Alexe, F. Postpartum Depression - a serious, dangerous, disabling, extremely frequent condition that is almost completely ignored in Romania. Mediterranean Journal of Clinical Psychology. 2020, 8, 3. [Google Scholar] [CrossRef]
- Merlo, E.M.; Stoian, A.P.; Motofei, I.G.; Settineri, S. Clinical Psychological Figures in Healthcare Professionals: Resilience and Maladjustment as the "Cost of Care". Front Psychol. 2020, 11, 607783. [Google Scholar] [CrossRef]
- Turcan, N.; Bohiltea, R.E.; Ionita-Radu, F.; Furtunescu, F.; Navolan, D.; Berceanu, C.; Nemescu, D.; Cirstoiu, M.M. Unfavorable influence of prematurity on the neonatal prognostic of small for gestational age fetuses. Exp Ther Med. 2020, 20, 2415–2422. [Google Scholar] [CrossRef]
- Grigoriu, C.; Furtunescu, F.; Gaman, L.E.; Balaceanu, A.L.; Buzatu, R.; Grigoriu, M. A Biochemical Marker of Preeclampsia - Hypertriglyceridemia - and the Impact of Secondary Prevention Therapy. Rev Chim. 2018, 69, 2740–2743. [Google Scholar] [CrossRef]
- Bandoli, G.; Chambers, C.D. Autoimmune conditions and comorbid depression in pregnancy: examining the risk of preterm birth and preeclampsia. J Perinatol. 2017, 37, 1082–1087. [Google Scholar] [CrossRef]
- Yu, A.; Friedman, S.; Ananthakrishnan, A.N. Incidence and Predictors of Flares in the Postpartum Year Among Women With Inflammatory Bowel Disease. Inflamm Bowel Dis. 2020, 26, 1926–1932. [Google Scholar] [CrossRef]
- Brănescu, C.; Serban, D.; Dascălu, A.M.; Oprescu, S.M.; Savlovschi, C. Interleukin 6 and lipopolysaccharide binding protein - markers of inflammation in acute appendicitis. Chirurgia (Bucur). 2013, 108, 206–214. [Google Scholar] [PubMed]
- Serban, D.; Smarandache, C.G.; Tudor, C.; Duta, L.N.; Dascalu, A.M.; Aliuș, C. Laparoscopic Surgery in COVID-19 Era-Safety and Ethical Issues. Diagnostics (Basel). 2020, 10, 673. [Google Scholar] [CrossRef]
- Suceveanu, A.I.; Mazilu, L.; Suceveanu, A.P.; et al. Assertion for Montelukast in the COVID-19 pandemics? Farmacia. 2020, 68, 579–585. [Google Scholar] [CrossRef]
- Tănăsescu, C.; Faur, M.; Sabău, D. Day-case Surgery in the Context of Inguinal Hernia Repair by the Modified Lichtenstein Technique - A Single Centre Experience. Chirurgia (Bucur). 2019, 114, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Lamps, L.W.; Madhusudhan, K.T.; Greenson, J.K.; Pierce, R.H.; Massoll, N.A.; Chiles, M.C.; Dean, P.J.; Scott, M.A. The role of Yersinia enterocolitica and Yersinia pseudotuberculosis in granulomatous appendicitis: a histologic and molecular study. Am J Surg Pathol. 2001, 25, 508–515. [Google Scholar] [CrossRef]
- Guo, G.; Greenson, J.K. Histopathology of interval (delayed) appendectomy specimens: strong association with granulomatous and xanthogranulomatous appendicitis. Am J Surg Pathol. 2003, 27, 1147–1151. [Google Scholar] [CrossRef]
- Huang, J.C.; Appelman, H.D. Another look at chronic appendicitis resembling Crohn's disease. Mod Pathol. 1996, 9, 975–981. [Google Scholar]
- Stangl, P.C.; Herbst, F.; Birner, P.; Oberhuber, G. Crohn's disease of the appendix. Virchows Arch. 2002, 440, 397–403. [Google Scholar] [CrossRef]
- Agha, F.P.; Ghahremani, G.G.; Panella, J.S.; Kaufman, M.W. Appendicitis as the initial manifestation of Crohn's disease: radiologic features and prognosis. AJR Am J Roentgenol. 1987, 149, 515–518. [Google Scholar] [CrossRef]
- Bass, J.A.; Goldman, J.; Jackson, M.A.; Gasior, A.C.; Sharp, S.W.; Drews, A.A.; Saunders, C.J.; St Peter, S.D. Pediatric Crohn disease presenting as appendicitis: differentiating features from typical appendicitis. Eur J Pediatr Surg. 2012, 22, 274–278. [Google Scholar] [CrossRef]
- Kambouri, K.; Gardikis, S.; Agelidou, M.; Vaos, G. Local peritonitis as the first manifestation of Crohn's disease in a child. J Indian Assoc Pediatr Surg. 2014, 19, 100–102. [Google Scholar] [CrossRef] [PubMed]
- Spataru, R. The use of mechanical suture in the treatment of Hirschsprung's disease: experience of 17 cases. Chirurgia (Bucur). 2014, 109, 208–212. [Google Scholar]
- Alius, C.; Tudor, C.; Badiu, C.D.; Dascalu, A.M.; Smarandache, C.G.; Sabau, A.D.; Tanasescu, C.; Balasescu, S.A.; Serban, D. Indocyanine Green-Enhanced Colorectal Surgery-between Being Superfluous and Being a Game-Changer. Diagnostics (Basel). 2020, 10, 742. [Google Scholar] [CrossRef]
- Kim, N.K.; Senagore, A.J.; Luchtefeld, M.A.; MacKeigan, J.M.; Mazier, W.P.; Belknap, K.; Chen, S.H. Long-term outcome after ileocecal resection for Crohn's disease. Am Surg. 1997, 63, 627–633. [Google Scholar]
- Spataru, R.I.; Martius, E.; Ivan, L.E.; Sirbu, D.; Hostiuc, S. Pseudomembranous colitis complicating the natural course of Crohn's disease in a pediatric patient. Rom J Legal Med. 2014, 22, 161–166. [Google Scholar] [CrossRef][Green Version]
- Spataru, R.I.; Sirbu, A.; Sirbu, D. Forensic ramifications in diagnosing and treating high forms of the Hirschsprung's disease. Rom J Leg Med. 2013, 21, 105–110. [Google Scholar] [CrossRef]
- Suciu, N.; Serban, A.; Toader, O.; Oprescu, D.; Spataru, R.I. Case report of fetal lingual tumor - perinatal care and neonatal surgical intervention. J Matern Fetal Neonatal Med. 2014, 27, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Motofei, I.G.; Rowland, D.L.; Georgescu, S.R.; Tampa, M.; Paunica, S.; Constantin, V.D.; Balalau, C.; Manea, M.; Baleanu, B.C.; Sinescu, I. Post-Finasteride Adverse Effects in Male Androgenic Alopecia: A Case Report of Vitiligo. Skin Pharmacol Physiol. 2017, 30, 42–45. [Google Scholar] [CrossRef]
- Spataru, R.I.; Popoiu, M.C.; Ivanov, M. Foregut duplication cyst associated with esophageal atresia-one-stage neonatal surgical repair. Indian J Surg. 2015, 77 (Suppl 1), 52–55. [Google Scholar] [CrossRef][Green Version]
- Jones, A.E.; Phillips, A.W.; Jarvis, J.R.; Sargen, K. The value of routine histopathological examination of appendicectomy specimens. BMC Surg. 2007, 7, 17. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, A.; Gupta, A.; D'Mello, S.; Mezoff, A.; Podberesky, D.; Barnett, S.; Keswani, S.; Frischer, J.S. Crohn's disease limited to the appendix: a case report in a pediatric patient. Pediatr Surg Int. 2010, 26, 1125–1128. [Google Scholar] [CrossRef] [PubMed]






© 2021 by the author. 2021 Augustina Enculescu, Mircea Denis Lupusoru, Catalin Cirstoveanu, Andra-Iulia Suceveanu, Liliana Florina Andronache, Adrian-Paul Suceveanu, Felix Voinea, Maria Puscasu
Share and Cite
Enculescu, A.; Lupusoru, M.D.; Cirstoveanu, C.; Suceveanu, A.-I.; Andronache, L.F.; Suceveanu, A.-P.; Voinea, F.; Puscasu, M. Postoperative Complicated Appendectomy Revealing Crohn’s Disease in a Pediatric Patient. J. Mind Med. Sci. 2021, 8, 154-160. https://doi.org/10.22543/7674.81.P154160
Enculescu A, Lupusoru MD, Cirstoveanu C, Suceveanu A-I, Andronache LF, Suceveanu A-P, Voinea F, Puscasu M. Postoperative Complicated Appendectomy Revealing Crohn’s Disease in a Pediatric Patient. Journal of Mind and Medical Sciences. 2021; 8(1):154-160. https://doi.org/10.22543/7674.81.P154160
Chicago/Turabian StyleEnculescu, Augustina, Mircea Denis Lupusoru, Catalin Cirstoveanu, Andra-Iulia Suceveanu, Liliana Florina Andronache, Adrian-Paul Suceveanu, Felix Voinea, and Maria Puscasu. 2021. "Postoperative Complicated Appendectomy Revealing Crohn’s Disease in a Pediatric Patient" Journal of Mind and Medical Sciences 8, no. 1: 154-160. https://doi.org/10.22543/7674.81.P154160
APA StyleEnculescu, A., Lupusoru, M. D., Cirstoveanu, C., Suceveanu, A.-I., Andronache, L. F., Suceveanu, A.-P., Voinea, F., & Puscasu, M. (2021). Postoperative Complicated Appendectomy Revealing Crohn’s Disease in a Pediatric Patient. Journal of Mind and Medical Sciences, 8(1), 154-160. https://doi.org/10.22543/7674.81.P154160


