Acute Chylous Peritonitis Due to Idiopathic Pancreatitis Mimicking Acute Appendicitis
Abstract
Introduction
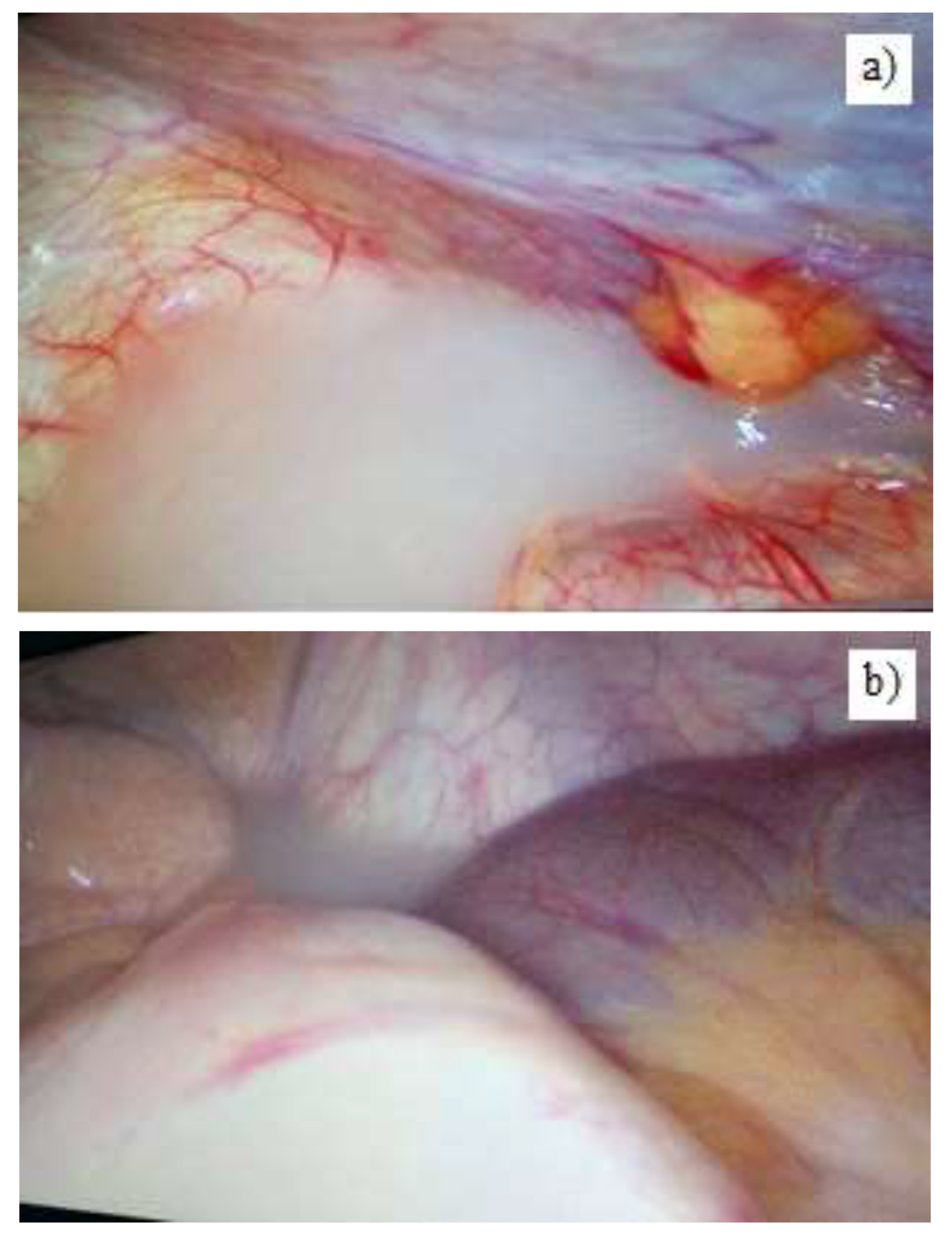
Case Report
Discussions
Highlights
- ✓
- Chylous peritonitis, as a rare event, is usually diagnosed during the surgical procedures which can rarely relieve the location of the disrupted lymph channel.
- ✓
- Minimally invasive surgery is effective for both the diagnosis and the treatment and carry a low rate of complications when compared to open surgery.
Conclusions
Conflict of interest disclosure
Compliance with ethical standards
References
- Vettoretto, N.; Odeh, M.; Romessis, M.; Pettinato, G.; Taglietti, L.; Giovanetti, M. Acute abdomen from chylous peritonitis: a surgical diagnosis. Case report and literature review. Eur Surg Res. 2008, 41, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Serban, D.; Spataru, R.I.; Vancea, G.; Balasescu, S.A.; Socea, B.; Tudor, C.; Dascalu, A.M. Informed consent in all surgical specialties: from legal obligation to patient satisfaction. Rom J Leg Med. 2020, 28, 317–321. [Google Scholar] [CrossRef]
- Ozgüç, H.; Narmanlı, M.; Keskin, M.K. Acute chylous peritonitis: Report of a case. Int J Surg Case Rep. 2013, 4, 419–421. [Google Scholar] [CrossRef]
- Fazili, F.M.; Khawaja, F.I. Acute chylous peritonitis simulating acute appendicitis: A case report and review of the literature. Ann Saudi Med. 1999, 19, 236–238. [Google Scholar] [CrossRef] [PubMed]
- Ben-Ami, H.; Nagachandran, P.; Assalia, A.; Edoute, Y. Acute transient chylous ascites associated with acute biliary pancreatitis. Am J Med Sci. 1999, 318, 122–123. [Google Scholar] [CrossRef]
- Chuang, S.C.; Lee, K.T.; Wang, S.N.; Kuo, K.K.; Chen, J.S. Hypertriglyceridemia-associated acute pancreatitis with chylous ascites in pregnancy. J Formos Med Assoc. 2006, 105, 583–587. [Google Scholar] [CrossRef]
- Georgiou, G.K.; Harissis, H.; Mitsis, M.; Batsis, H.; Fatouros, M. Acute chylous peritonitis due to acute pancreatitis. World J Gastroenterol. 2012, 18, 1987–1990. [Google Scholar] [CrossRef]
- D'Amata, G.; Rega, M.; Viola, V.; Bove, V.; Simeone, P.; Baiano, G. Chyloperitoneum associated with idiopathic pancreatitis: case report and review of the literature. G Chir. 2016, 37, 167–170. [Google Scholar] [CrossRef]
- Smith, E.K.; Ek, E.; Croagh, D.; Spain, L.A.; Farrell, S. Acute chylous ascites mimicking acute appendicitis in a patient with pancreatitis. World J Gastroenterol. 2009, 15, 4849–4852. [Google Scholar] [CrossRef]
- Serban, D.; Smarandache, A.M.; Cristian, D.; Tudor, C.; Duta, L.; Dascalu, A.M. Medical errors and patient safety culture – shifting the healthcare paradigm in Romanian hospitals. Rom J Leg Med. 2020, 28, 195–201. [Google Scholar] [CrossRef]
- Spataru, R.I.; Sirbu, A.; Sirbu, D. Forensic ramifications in diagnosing and treating high forms of the Hirschsprung's disease. Rom J Leg Med. 2013, 21, 105–110. [Google Scholar] [CrossRef]
- Spataru, R. The use of mechanical suture in the treatment of Hirschsprung's disease: experience of 17 cases. Chirurgia (Bucur). 2014, 109, 208–212. [Google Scholar]
- Shimajiri, H.; Egi, H.; Yamamoto, M.; Kochi, M.; Mukai, S.; Ohdan, H. Laparoscopic management of refractory chylous ascites using fluorescence navigation with indocyanine green: A case report. Int J Surg Case Rep, 1: 49. [CrossRef]
- Alius, C.; Tudor, C.; Badiu, C.D.; Dascalu, A.M.; Smarandache, C.G.; Sabau, A.D.; Tanasescu, C.; Balasescu, S.A.; Serban, D. Indocyanine Green-Enhanced Colorectal Surgery-between Being Superfluous and Being a Game-Changer. Diagnostics (Basel). 2018, 49, 149–152. [Google Scholar] [CrossRef]
- Rogdakis, A.; Bouras, P.; Giannakakis, P.; et al. Spontaneous chylous peritonitis presenting as acute surgical abdomen. Hellenic J Surg 2011, 83, 166–169. [Google Scholar] [CrossRef]
- Kypson, A.P.; Onaitis, M.W.; Feldman, J.M.; Tyler, D.S. Carcinoid and chylous ascites: an unusual association. J Gastrointest Surg. 2002, 6, 781–783. [Google Scholar] [CrossRef]
- Bhardwaj, R.; Vaziri, H.; Gautam, A.; Ballesteros, E.; Karimeddini, D.; Wu, G.Y. Chylous Ascites: A Review of Pathogenesis, Diagnosis and Treatment. J Clin Transl Hepatol. 2018, 6, 105–113. [Google Scholar] [CrossRef]
- Al-Busafi, S.A.; Ghali, P.; Deschênes, M.; Wong, P. Chylous Ascites: Evaluation and Management. ISRN Hepatol. 2014, 2014, 240473. [Google Scholar] [CrossRef]
- de la Torre-Saldaña, V.A.; Cruz-Fabián, S.; Ayala-Haro, N.; et al. Chylous Ascites as Initial Manifestation of Colon Cancer. Med Int Mex. 2014, 30, 99–107. [Google Scholar]
- Ciocirlan, M.; Draghia, L.; Manuc, D.; et al. Nutritional status of patients with digestive cancers. In Proceedings of the Conference: 3rd International Conference on Interdisciplinary Management of Diabetes Mellitus and its Complications (INTERDIAB), Bucharest, Romania, 2–4 March 2017; Sponsor(s): Assoc Renal Metab & Nutrit Studies; AstraZeneca Diabetes; MSD Diabetes; novo nordisk; SANOFI, INTERDIAB 2017: DIABETES MELLITUS IN INTERNAL MEDICINE Book SeriesInternational Conference on Interdisciplinary Management of Diabetes Mellitus and its Complications. 2017; pp. 132–138. [Google Scholar]
- Draghici, T.; Negreanu, L.; Bratu, O.; et al. Paraneoplastic syndromes in digestive tumors: a review. Rom Biotechnol Lett. 2019, 24, 813–819. [Google Scholar] [CrossRef]
- Apikotoa, S.; Wijesuriya, R. Idiopathic acute chylous peritonitis during pregnancy, mimicking perforated acute appendicitis: A case report. Int J Surg Case Rep. 2021, 81, 105790. [Google Scholar] [CrossRef]
- Brănescu, C.; Serban, D.; Dascălu, A.M.; Oprescu, S.M.; Savlovschi, C. Interleukin 6 and lipopolysaccharide binding protein - markers of inflammation in acute appendicitis. Chirurgia (Bucur). 2013, 108, 206–214. [Google Scholar]
- Tănăsescu, C.; Faur, M.; Sabău, D. Day-case Surgery in the Context of Inguinal Hernia Repair by the Modified Lichtenstein Technique - A Single Centre Experience. Chirurgia (Bucur). 2019, 114, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Popoiag, R.E.; Pantea-Stoian, A.; Suceveanu, A.P.; et al. The relationship between gut microbiota and spontaneous bacterial peritonitis in patients with liver cirrhosis - a literature review. J Mind Med Sci. 2019, 6, 26–30. [Google Scholar] [CrossRef]
- Tanasescu, C.; Patrusel, D.; Perisanu, S.; Chis, F.; Antonescu, M. Difficult case of thoraco-abdominal injuries due to a motor vehicle accident. Chirurgia (Bucur). 2011, 106, 265–268. [Google Scholar] [PubMed]
- Fang, F.C.; Hsu, S.D.; Chen, C.W.; Chen, T.W. Spontaneous chylous peritonitis mimicking acute appendicitis: a case report and review of literature. World J Gastroenterol. 2006, 12, 154–156. [Google Scholar] [CrossRef] [PubMed]
- Kiss, L.; Kiss, R.; Porr, P.J.; Nica, C.; Nica, C.; Bardac, O.; Tănăsescu, C.; Bărbulescu, B.; Bundache, M.; Ilie, S.; Maniu, D.; Zaharie, S.I.; Hulpuş, R. Pathological evidence in support of total mesorectal excision in the management of rectal cancer. Chirurgia (Bucur). 2011, 106, 347–52. [Google Scholar]
- Grigoriu, M.E.; Costea, R.V.; Grigoriu, C.I.; Furtunescu. Endoscopic management of choledocolithiasis related to periampullary duodenal divericula. Medical-Surgical Journal-Revista Medico-Chirurgicala. 2018, 122, 102–108. [Google Scholar]
- Huang, L.L.; Xia, H.H.; Zhu, S.L. Ascitic Fluid Analysis in the Differential Diagnosis of Ascites: Focus on Cirrhotic Ascites. J Clin Transl Hepatol. 2014, 2, 58–64. [Google Scholar] [CrossRef]
- Cárdenas, A.; Chopra, S. Chylous ascites. Am J Gastroenterol. 2002, 97, 1896–1900. [Google Scholar] [CrossRef]
- Hibbeln, J.F.; Wehmueller, M.D.; Wilbur, A.C. Chylous ascites: CT and ultrasound appearance. Abdom Imaging. 1995, 20, 138–140. [Google Scholar] [CrossRef]
- Tofolean, D.E.; Mazilu, L.; Stăniceanu, F.; Mocanu, L.; Suceveanu, A.I.; Baz, R.O.; Parepa, R.I.; Suceveanu, A.P.; Bondari, S.; Bondari, D.; Voinea, F. Clinical presentation of a patient with cutis laxa with systemic involvement: a case report. Rom J Morphol Embryol. 2015, 56, 1205–1210. [Google Scholar] [PubMed]
- Spataru, R.I.; Martius, E.; Ivan, L.E.; Sirbu, D.; Hostiuc, S. Pseudomembranous colitis complicating the natural course of Crohn's disease in a pediatric patient. Rom J Leg Med. 2014, 22, 161–166. [Google Scholar] [CrossRef][Green Version]
- Widjaja, A.; Gratz, K.F.; Ockenga, J.; Wagner, S.; Manns, M.P. Octreotide for therapy of chylous ascites in yellow nail syndrome. Gastroenterology. 1999, 116, 1017–1018. [Google Scholar] [CrossRef]
- Motofei, I.G.; Rowland, D.L.; Georgescu, S.R.; Tampa, M.; Paunica, S.; Constantin, V.D.; Balalau, C.; Manea, M.; Baleanu, B.C.; Sinescu, I. Post-Finasteride Adverse Effects in Male Androgenic Alopecia: A Case Report of Vitiligo. Skin Pharmacol Physiol. 2017, 30, 42–45. [Google Scholar] [CrossRef]
- Mittleider, D.; Dykes, T.A.; Cicuto, K.P.; Amberson, S.M.; Leusner, C.R. Retrograde cannulation of the thoracic duct and embolization of the cisterna chyli in the treatment of chylous ascites. J Vasc Interv Radiol. 2008, 19 Pt 1, 285–290. [Google Scholar] [CrossRef]
- Benedix, F.; Lippert, H.; Meyer, F. Post-surgical lymphocutaneous fistula, chylous ascites and chylothorax--infrequent but serious complications: etiology, diagnosis and therapeutic options. Zentralbl Chir. 2007, 132, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Serban, D.; Smarandache, C.G.; Tudor, C.; Duta, L.N.; Dascalu, A.M.; Aliuș, C. Laparoscopic Surgery in COVID-19 Era-Safety and Ethical Issues. Diagnostics (Basel). 2020, 10, 673. [Google Scholar] [CrossRef]
- Ozgüç, H.; Narmanlı, M.; Keskin, M.K. Acute chylous peritonitis: Report of a case. Int J Surg Case Rep. 2013, 4, 419–421. [Google Scholar] [CrossRef]
© 2021 by the author. 2021 Dan Bratu, Alin Mihetiu, Dragoș Virgil Davițoiu, Vlad Dumitru Băleanu, Liliana Florina Andronache, Oana Popescu
Share and Cite
Bratu, D.; Mihetiu, A.; Davițoiu, D.V.; Băleanu, V.D.; Andronache, L.F.; Popescu, O. Acute Chylous Peritonitis Due to Idiopathic Pancreatitis Mimicking Acute Appendicitis. J. Mind Med. Sci. 2021, 8, 149-153. https://doi.org/10.22543/7674.81.P149153
Bratu D, Mihetiu A, Davițoiu DV, Băleanu VD, Andronache LF, Popescu O. Acute Chylous Peritonitis Due to Idiopathic Pancreatitis Mimicking Acute Appendicitis. Journal of Mind and Medical Sciences. 2021; 8(1):149-153. https://doi.org/10.22543/7674.81.P149153
Chicago/Turabian StyleBratu, Dan, Alin Mihetiu, Dragoș Virgil Davițoiu, Vlad Dumitru Băleanu, Liliana Florina Andronache, and Oana Popescu. 2021. "Acute Chylous Peritonitis Due to Idiopathic Pancreatitis Mimicking Acute Appendicitis" Journal of Mind and Medical Sciences 8, no. 1: 149-153. https://doi.org/10.22543/7674.81.P149153
APA StyleBratu, D., Mihetiu, A., Davițoiu, D. V., Băleanu, V. D., Andronache, L. F., & Popescu, O. (2021). Acute Chylous Peritonitis Due to Idiopathic Pancreatitis Mimicking Acute Appendicitis. Journal of Mind and Medical Sciences, 8(1), 149-153. https://doi.org/10.22543/7674.81.P149153


