A Pedunculated Esophageal Chondromatous Hamartoma in a Child
Abstract
Introduction
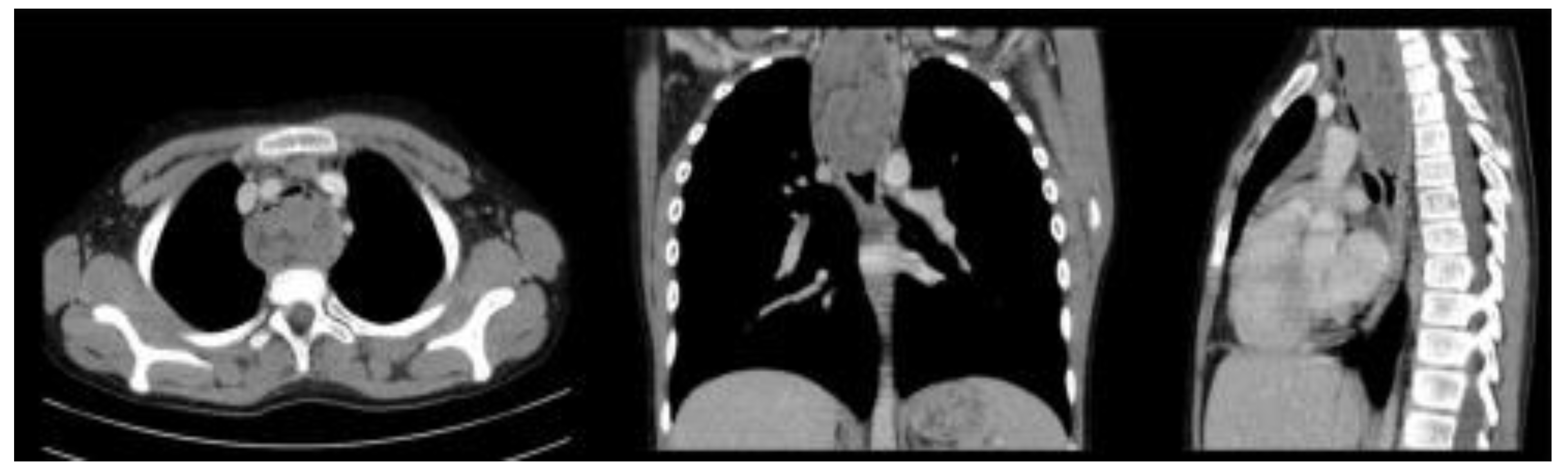
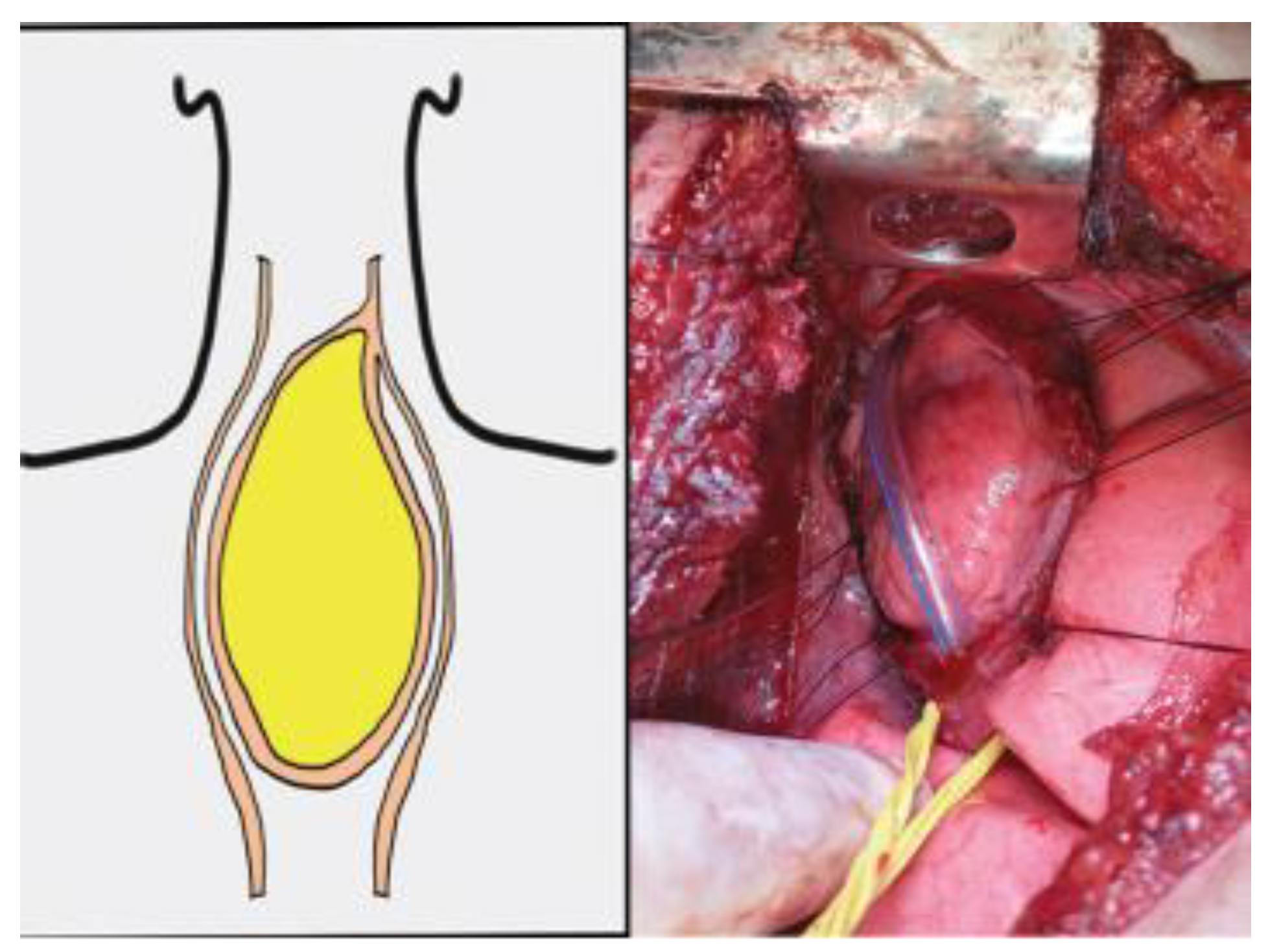
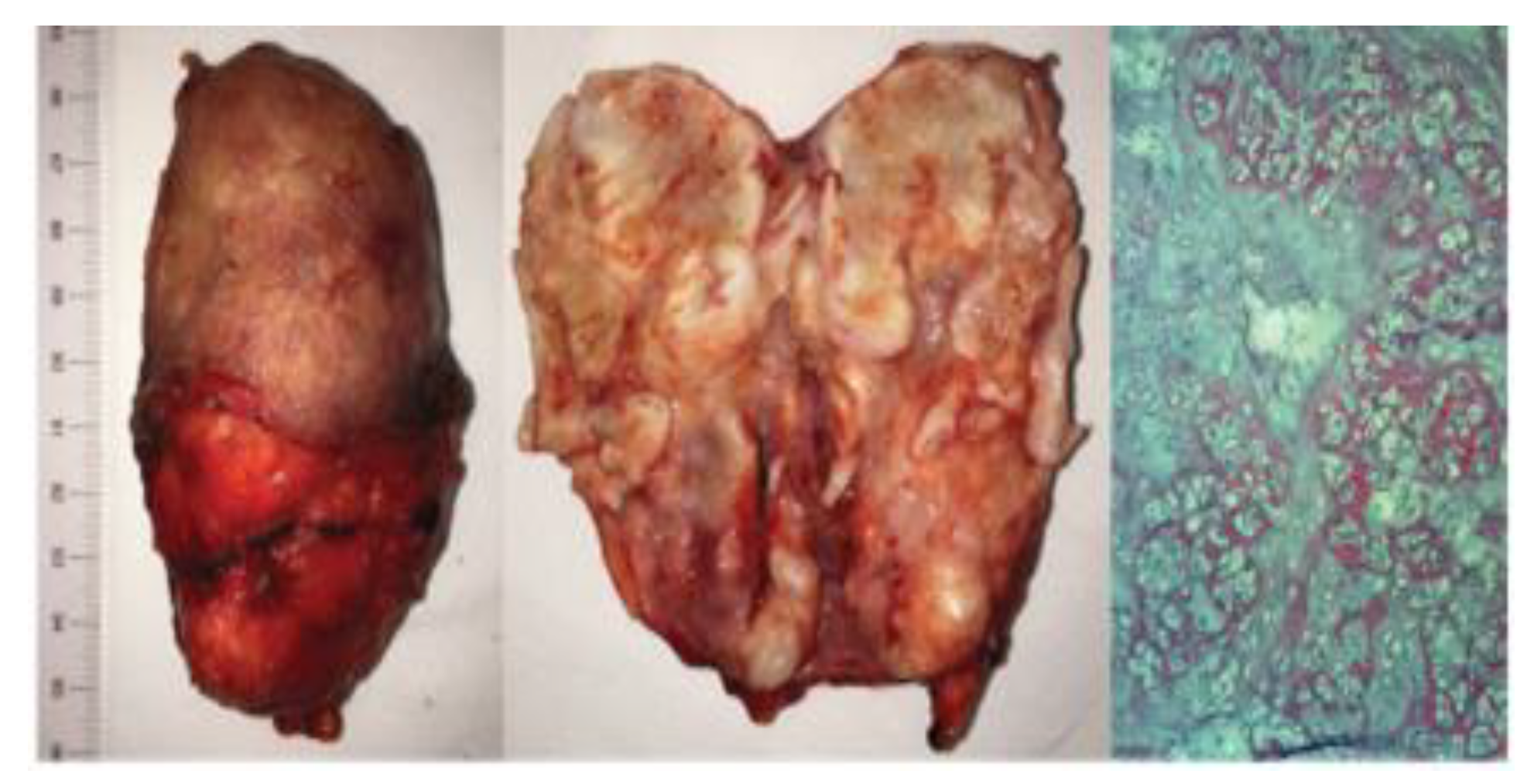
Case Report
Discussions
Highlights
- ✓
- Esophageal tumors in the pediatric population are extremely rare entities with a low incidence of occurrence in the clinical practice of a pediatrician.
- ✓
- The diagnosis is delayed by nonspecific symptoms and radiologic findings.
- ✓
- The wide range of pathological entities similar to it require extensive planning and interdisciplinary collaboration between the radiologist, oncologist, pediatric surgeon and endoscopist. The surgical treatment should preserve the native esophagus and prevent long term complications.
Conclusions
Conflict of interest disclosure
Compliance with ethical standards
References
- McCarville, M.B. Malignant pulmonary and mediastinal tumors in children: differential diagnoses. Cancer Imaging. 2010, 10, S35–S41. [Google Scholar] [CrossRef] [PubMed]
- Theilen, T.M.; La Quaglia, M. Esophageal Tumors in Childhood and Adolescence: Benign and Malignant. In Esophageal and Gastric Disorders in Infancy and Childhood; Till, H., Thomson, M., Foker, J., Holcomb, G., III, Khan, K., Eds.; Springer: Berlin, Heidelberg, 2017. [Google Scholar] [CrossRef]
- Septer, S.; Cuffari, C.; Attard, T.M. Esophageal polyps in pediatric patients undergoing routine diagnostic upper gastrointestinal endoscopy: a multicenter study. Dis Esophagus. 2014, 27, 24–29. [Google Scholar] [CrossRef]
- Hou, S.; Wei, J.; Lu, W.; Wang, L.; Liu, H.; Zhang, Q. Intramural chondroid hamartoma in the distal esophagus in an adult: A case report and review of the literature. Mol Clin Oncol. 2017, 6, 19–22. [Google Scholar] [CrossRef] [PubMed]
- Serban, D.; Spataru, R.I.; Vancea, G.; Balasescu, S.A.; Socea, B.; Tudor, C.; Dascalu, A.M. Informed consent in all surgical specialties: from legal obligation to patient satisfaction. Rom J Leg Med. 2020, 28, 317–321. [Google Scholar] [CrossRef]
- Ioannides, A.S.; Copp, A.J. Embryology of oesophageal atresia. Semin Pediatr Surg. 2009, 18, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Spataru, R.I.; Popoiu, M.C.; Ivanov, M. Foregut duplication cyst associated with esophageal atresia-one-stage neonatal surgical repair. Indian J Surg. 2015, 77 (Suppl 1), 52–55. [Google Scholar] [CrossRef][Green Version]
- Everett, C.; Volberg, F.; Ulshen, M.; Murray, G. Intramural esophageal hamartoma: a report of two cases and review of the literature. Gastrointest Radiol. 1980, 5, 317–319. [Google Scholar] [CrossRef]
- Zhang, C.; Xu, J.; Wang, Z.; He, Z.; Yang, H.; Hu, J. Chondromatous hamartoma of cervical esophagus: a case report and literature review. J Thorac Dis. 2017, 9, E236–E244. [Google Scholar] [CrossRef]
- Rebelo, P.G.; Ormonde, J.V.; Ormonde Filho, J.B. Congenital esophageal stenosis owing to tracheobronchial remnants. Rev Paul Pediatr. 2013, 31, 406–410. [Google Scholar] [CrossRef]
- Serban, D.; Smarandache, A.M.; Cristian, D.; Tudor, C.; Duta, L.; Dascalu, A.M. Medical errors and patient safety culture - shifting the healthcare paradigm in Romanian hospitals. Rom J Leg Med. 2020, 28, 195–201. [Google Scholar] [CrossRef]
- Stanciu, A.E.; Zamfir-Chiru-Anton, A.; Stanciu, M.M.; Stoian, A.P.; Jinga, V.; Nitipir, C.; Bucur, A.; Pituru, T.S.; Arsene, A.L.; Dragoi, C.M.; Hainarosie, R.; Nicolae, A.C.; Gherghe, M.; Gheorghe, D.C.; Spandidos, D.A.; Tsatsakis, A.; Papasavva, M.; Drakoulis, N. Clinical significance of serum melatonin in predicting the severity of oral squamous cell carcinoma. Oncol Lett. 2020, 19, 1537–1543. [Google Scholar] [CrossRef] [PubMed]
- Suciu, N.; Serban, A.; Toader, O.; Oprescu, D.; Spataru, R.I. Case report of fetal lingual tumor - perinatal care and neonatal surgical intervention. J Matern Fetal Neonatal Med. 2014, 27, 314–319. [Google Scholar] [CrossRef]
- Samad, L.; Ali, M.; Ramzi, H.; Akbani, Y. Respiratory distress in a child caused by lipoma of the esophagus. J Pediatr Surg. 1999, 34, 1537–1538. [Google Scholar] [CrossRef]
- Motofei, I.G. Malignant Melanoma: Autoimmunity and Supracellular Messaging as New Therapeutic Approaches. Curr Treat Options Oncol. 2019, 20, 45. [Google Scholar] [CrossRef] [PubMed]
- Tudosie, M.S.; Truta, E.; Davitoiu, A.M.; Stanciulescu, L.; Jinescu, G.; Mitu, A.M.; Forje, M.; Horhota, L.; Bojescu, A.A.; Mares, A.M.; Ionica, M. The Impact of Copper in Children with Attention Deficit Hyperactivity Disorder. Rev. Chim. 2017, 68, 279–283. [Google Scholar] [CrossRef]
- Coury, J.; Steinfeld, J.; Zwillenberg, D.; Zwillenberg, S. Esophageal hamartoma as an unusual cause of neonatal apnea and bradycardia. Ear Nose Throat J. 2010, 89, E7–E11. [Google Scholar]
- Dodrill, P.; Gosa, M.M. Pediatric Dysphagia: Physiology, Assessment, and Management. Ann Nutr Metab. 2015, 66 (Suppl 5), 24–31. [Google Scholar] [CrossRef] [PubMed]
- Tofolean, D.E.; Mazilu, L.; Stăniceanu, F.; Mocanu, L.; Suceveanu, A.I.; Baz, R.O.; Parepa, R.I.; Suceveanu, A.P.; Bondari, S.; Bondari, D.; Voinea, F. Clinical presentation of a patient with cutis laxa with systemic involvement: a case report. Rom J Morphol Embryol. 2015, 56, 1205–1210. [Google Scholar]
- Rusescu, A.; Pietrosanu, C.; Ionita, I.; Stefanescu, C.D.; Stoian, A.M.P.; Camen, A.; Zainea, V.; Hainarosie, R. Chemical Ablation of the Submucosal Tissue in Volumetric Reduction of Inferior Turbinate. Rev. Chim. 2018, 69, 642–644. [Google Scholar] [CrossRef]
- Serban, D.; Smarandache, C.G.; Tudor, C.; Duta, L.N.; Dascalu, A.M.; Aliuș, C. Laparoscopic Surgery in COVID-19 Era- Safety and Ethical Issues. Diagnostics (Basel). 2020, 10, 673. [Google Scholar] [CrossRef]
- Hryhorczuk, A.L.; Lee, E.Y.; Eisenberg, R.L. Esophageal abnormalities in pediatric patients. AJR Am J Roentgenol. 2013, 201, W519-32. [Google Scholar] [CrossRef] [PubMed]
- Räsänen, J.; Ilonen, I.; Ristimäki, A.; Salo, J.A.; Mäkitie, A.A. A hamartoma presenting as an intramural upper oesophageal tumour. J Thorac Dis. 2017, 9, E698–E701. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alius, C.; Tudor, C.; Badiu, C.D.; Dascalu, A.M.; Smarandache, C.G.; Sabau, A.D.; Tanasescu, C.; Balasescu, S.A.; Serban, D. Indocyanine Green-Enhanced Colorectal Surgery-between Being Superfluous and Being a Game-Changer. Diagnostics (Basel). 2020, 10, 742. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.W.; Murray, G.F.; Wilcox, B.R. Intramural esophageal hamartoma. An unusual cause of progressive stricture in a child. J Thorac Cardiovasc Surg. 1976, 72, 315–318. [Google Scholar] [CrossRef]
- Savlovschi, C.; Serban, D.; Andreescu, C.; Dascalu, A.; Pantu, H. Economic analysis of medical management applied for left colostomy. Chirurgia (Bucur). 2013, 108, 666–669. [Google Scholar]
- Motofei, I.G. Biology of Cancer; From Cellular Cancerogenesis to Supracellular Evolution of Malignant Phenotype. Cancer Invest. 2018, 36, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Spataru, R. The use of mechanical suture in the treatment of Hirschsprung's disease: experience of 17 cases. Chirurgia (Bucur). 2014, 109, 208–212. [Google Scholar]
- Ryan, M.L.; Zhuge, Y.; Smothers, C.D.; Zhang, J.; Huang, E.Y. Intraluminal esophageal teratoma in a neonate. J Ped Surg Case Reports. 2015, 3, 451–454. [Google Scholar] [CrossRef]
- Kiss, L.; Kiss, R.; Porr, P.J.; Nica, C.; Nica, C.; Bardac, O.; Tănăsescu, C.; Bărbulescu, B.; Bundache, M.; Ilie, S.; Maniu, D.; Zaharie, S.I.; Hulpuş, R. Pathological evidence in support of total mesorectal excision in the management of rectal cancer. Chirurgia (Bucur). 2011, 106, 347–352. [Google Scholar]
- Ekinci, G.H.; Hacıömeroğlu, O.; Ersev, A.; Alpay, L.; Özgen, H.; Yılmaz, A. The frequency of lung cancer in patients with pulmonary hamartomas: An evaluation of clinical, radiological, and pathological features and follow-up data of 96 patients with pulmonary hamartomas. Rev Port Pneumol (2006). 2017, 23, 280–286. [Google Scholar] [CrossRef]




© 2021 by the author. 2021 Dan-Alexandru Iozsa, Maria Puscasu, Catalin Gabriel Cirstoveanu, Vlad Denis Constantin, Anca Silvia Dumitriu, Stana Paunica, Nicolae Sebastian Ionescu
Share and Cite
Iozsa, D.-A.; Puscasu, M.; Cirstoveanu, C.G.; Constantin, V.D.; Dumitriu, A.S.; Paunica, S.; Ionescu, N.S. A Pedunculated Esophageal Chondromatous Hamartoma in a Child. J. Mind Med. Sci. 2021, 8, 161-166. https://doi.org/10.22543/7674.81.P161166
Iozsa D-A, Puscasu M, Cirstoveanu CG, Constantin VD, Dumitriu AS, Paunica S, Ionescu NS. A Pedunculated Esophageal Chondromatous Hamartoma in a Child. Journal of Mind and Medical Sciences. 2021; 8(1):161-166. https://doi.org/10.22543/7674.81.P161166
Chicago/Turabian StyleIozsa, Dan-Alexandru, Maria Puscasu, Catalin Gabriel Cirstoveanu, Vlad Denis Constantin, Anca Silvia Dumitriu, Stana Paunica, and Nicolae Sebastian Ionescu. 2021. "A Pedunculated Esophageal Chondromatous Hamartoma in a Child" Journal of Mind and Medical Sciences 8, no. 1: 161-166. https://doi.org/10.22543/7674.81.P161166
APA StyleIozsa, D.-A., Puscasu, M., Cirstoveanu, C. G., Constantin, V. D., Dumitriu, A. S., Paunica, S., & Ionescu, N. S. (2021). A Pedunculated Esophageal Chondromatous Hamartoma in a Child. Journal of Mind and Medical Sciences, 8(1), 161-166. https://doi.org/10.22543/7674.81.P161166


