Abstract
The increase in the number of births by Caesarean section is a phenomenon whose global expansion is generated by numerous factors and especially by the contemporary perceptions of women regarding childbirth meeting the interests of the professionals in the field. However, the opinion of many women towards the benefits of Caesarean delivery is often not based on the experience or information from reliable sources. This study aimed at sharing the experience of women who gave birth both vaginally and by Caesarean section, focusing on their perception of these events. The study included 26 women and the conclusion of the vast majority (77%) was that natural birth is preferable and they would recommend it as the first option to future mothers. In addition, the analysis of the cases in which, on the contrary, they would recommend birth by Caesarean section (23%) revealed that they objectively had births that had not been optimally managed and hence, the recommendation for careful, professional evaluation of the conditions of birth for each case. Reaching an optimal rate of Caesarean sections is an objective that can be achieved through correct information, health education and the correct management of the cases.
Introduction
Significant changes have taken place in obstetric practices over the last three decades. If in the ’70s and ’80s, the percentage of births by Caesarean section, in tertiary maternity hospitals in Romania, was 12-15% and currently, in the same type of units, the percentage of births by Caesarean section exceeds 60%. On the other hand, the percentage of forceps deliveries was around 7-8% and now the applications of forceps, along with other obstetric maneuvers performed relatively frequently in the past, have become a rarity.
The phenomenon of increasing Caesarean section rates is found not only in Romania, where, at the national level, the birth rate by Caesarean section was 44% in 2017 but also, more generally, worldwide [1]. In the same year, in Australia, almost 30% of primiparous women gave birth by Caesarean section [1]. The overall Caesarean section rate was 32% in the USA [2], 45% in South Korea, 53% in Turkey [3], in the EU ranged from 16.5% in Finland to 54.8% in Cyprus [4].
This high rate of Caesarean sections has drawn the attention of researchers who have tried to find explanations for this evolution and to analyze whether this phenomenon brings any benefit to the health of mothers and newborns [5,6,7].
The conclusion of the research conducted under the auspices of the WHO was that: “At the population level, Caesarean section rates higher than 10% are not associated with reductions in maternal and newborn mortality rates” [8]. There are many reasons for this increase in the rate of Caesarean sections, some related to the psychology of future mothers, the emergence of new standards in the social environment regarding births, but also causes related to the professionals involved in childbirth care, their training, trying to reduce unpredictability, the time of labor, avoiding ambiguous situations or those that generate allegations of malpractice [9,10].
It can be stated that, most of the time, the desire of many pregnant women to give birth by Caesarean section has met the preference of many obstetricians for this kind of childbirth resolution [11].
The concept of Caesarean childbirth on demand has also appeared, currently accepted and even promoted by some specialists, although the WHO recommendation is that “Caesarean sections should only be performed when medically necessary” [10,11,12].
In this complex context we naturally asked ourselves “What is the opinion of women who have experienced both vaginal delivery and Caesarean section about giving birth? What would their preference be?” and “What would they recommend to other future mothers about giving birth?”
Through this study, we aim at evaluating the perception on childbirth methods for women who gave birth both vaginally and by Caesarean section.
Materials and Methods
We conducted a descriptive cross-sectional study, similar to the opinion poll, based on a questionnaire. The answers have been recorded in a database.
The study group included 26 women who presented to the specialized outpatient clinic of the Bucur Maternity—St. John’s Emergency Clinical Hospital, for routine consultations between January 2019–February 2020. They had to meet the following criteria: to have given birth both vaginally and by Caesarean section, at least one year from the last birth to have passed, not to suffer from mental illnesses that can affect their judgement and to be able to provide verifiable medical data.
The exclusion criteria were: not having childbirths by both methods mentioned, less than one year after the last birth, mental illnesses that might affect their judgement, the inability to provide verifiable medical data.
All the patients who agreed to participate in the study had signed the informed consent. The study protocol was approved by the Ethics Committee of St. John’s Emergency Clinical Hospital, the activities carried out in this study were in accordance with the Helsinki Declaration with its later amendments and with the ethical standards of the National Research Committee.
Statistical analysis
The data obtained from the completion of the questionnaires were recorded in a database, according to the coding established after the approval of the final form of the questionnaires, in order to allow their statistical processing and the formulation of the research results. The information obtained was classified, serialized, coded and entered in Excel program. We have maintained and will maintain the confidentiality of the data in accordance with the legislation on personal data. The validation of the research was ensured by analyzing the operationalization of the data quality by verifying the correct application of the questionnaires and by analyzing the credibility of the results obtained.
Results
The study group included 26 women aged between 26 and 55 years who gave birth both by Caesarean section and naturally, the median age being 39 years (DS +/-7).
Out of the women included in study group, 23 had 2 births each and 3 patients had 3 births each. The first births were natural for all women, in 23 patients the second birth was by Caesarean section and 3 patients (those with 3 births) had the second birth naturally, but the last one by Caesarean section. Due to their rarity, there were no cases of women having natural births after Caesarean sections in the study group.
Regarding the first birth, there were 2 premature births and 24 full-term births, the next births being all full-term. The average time elapsed from the first birth was 17 years (SD +/-6.7) and until the last birth (the one by Caesarean section) of 7.7 years (SD +/-4.6).
The recorded problems related to the vaginal births were: preeclampsia in one case, hemorrhagic complications in another case and 5 women reported that the birth had a difficult and prolonged labor, although the data provided were within the physiological parameters. One of the births ended in the application of forceps. For all the women included in the study, births were assisted in the hospital and an episiotomy was performed. Two women gave birth to 2,500g newborns, 21 women gave birth to newborns weighing between 2,500g and 3,500g, three women gave birth to newborns over 3,500g (one of them having 4,100g). With the exception of one antepartum stillbirth (in a woman with preeclampsia) and one case in which an Apgar Score 5 was recorded, all newborns had an Apgar Score between 8 and 10.
All Caesarean births were at term. By analyzing the reason for which Caesarean section was performed, it was found that 13 women out of 26 (50%) did not consider it relevant and did not even remember it. A number of 3 women admitted that they had expressly requested this. For the remaining cases: 2 women had unspecified age-related problems, a case of cephalo-pelvic disproportion, a case of bleeding at the beginning of labor, a case of severe preeclampsia, 2 cases of dystocia presentations (pelvic presentation and transverse one), a case of dynamic dystocia and 2 cases with history of gynecological surgery (uterus after myomectomy).
The newborns’ weight ranged from 2,600g to 3,850g with an average of 3,234g (DS +/-335). With the exception of one newborn who had an Apgar Score of 7, all the other children had an Apgar Score between 8 and 10. A number of 13 patients underwent spinal anesthesia and the other 13 patients underwent general anesthesia (50%).
The answer to the key questions “If you were to give birth again by what method would you prefer to do it?” and “What method of childbirth would you recommend to future mothers?” 20 out of the 26 women interviewed (approx. 77%) answered that they would opt for natural childbirth and that they would recommend it to other women (Figure 1).
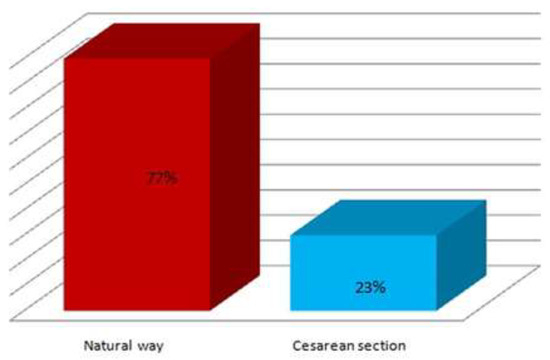
Figure 1.
The answer regarding the birth option.
Researching the reasons of those who recommended natural birth, those 20 women listed a number of disadvantages of Caesarean sections: 10 (50%) stated that recovery was more difficult, 7 (35%) stated that they had significant and prolonged abdominal pain, 6 (30%) woman had anesthesia-related problems, involving spinal anesthesia in 5 cases (technical difficulties—multiple punctures, partial anesthesia, persistent headache post-anesthesia, hypotension post-anesthesia) and general anesthesia in one case (the sensitive perception was not abolished and even led to a mental shock). The other problems mentioned were: wound infection in 2 cases, difficulties with breastfeeding, dyspareunia (Figure 2).
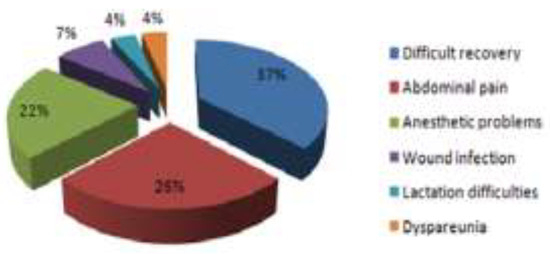
Figure 2.
Disadvantages of cesarean section in patient`s perception.
A number of 6 out of the 26 interviewed women (23%) answered that they would recommend Caesarean sections. In their perception, the reasons invoked as disadvantages of natural childbirth were: the feeling of insecurity, pain at birth, long labor, pain at the level of the episiotomy. Analyzing this subgroup, we noticed that it comprised a case in which the completion of the birth required the application of forceps, a woman who gave birth to a 4,100g fetus and a woman who gave birth to a child after a humeral dystocia resulted in clavicle rupture. The other three remaining women from this group reported mainly prolonged, exhausting, intensely painful labor.
Discussions
There are studies revealing that after having had their first birth naturally, for their second one, many women would change their options and opt for Caesarean sections [12,13,14]. In a study by Pang et al., in 2008, out of the 259 women who had given birth vaginally, almost 24% of them would prefer to give birth by Caesarean section the second time [7,15]. In other cases, Caesarean sections are considered a “practical solution”, as it can be seen in the conclusions of a study conducted in Brazil [16].
Women’s perception about birth is still a very subjective parameter [16,17]. Previous studies highlight the importance of midwifery support at birth for a positive experience [18,19,20].
Birth experience depends on many factors, some related to the newborn (weight, sex, Apgar score), others related to the mother (age, primiparous or multiparous state, gestational age, method of birth, perceived difficulty, complications, intensity of pain, mobilization, breastfeeding and psychological status) and some related to the health care system (chosen method of birth, peripartum support) [21,22].
Certain behavioral socio-demographic factors have been associated with maternal depression. Moreover, birth memories can have a long-term influence on the mother’s mental state and can influence her decision about a future birth [23,24,25].
As a novelty, the present study reveals the opinion of women who gave birth by both methods, naturally and by Caesarean section, showing that most of these women recommend giving birth naturally.
There are other arguments in favor of natural childbirth. In addition to studies that have shown that over a certain percentage the increase in the number of Cesarean operations does not bring improvements in terms of morbidity and mortality for both the newborn and the mother [23,26,27,28,29]. Recently, we are experiencing a significant increase in related pathology of the uterine scars and especially, we would like to mention the insertion of the placenta at the level of the uterine scar, which can lead to very serious cases of placenta previa and percreta [30,31,32,33].
A study demonstrating the correlation of placental abnormalities with a previous Caesarean birth was performed in our hospital within the time period 2014-2017. It included a group of 99 patients diagnosed with placenta previa, all of whom had a history of at least one Caesarean delivery. A number of 7 out of these patients associated the placenta percreta [17,18].
The risk of developing placental abnormalities increases with the number of Caesarean births. Numerous ultrasonography studies have shown the link between uterine scar and placental insertion at this level [21,22,23,24]. In order to explain the predisposition of the placental adhesion to the uterine scar, in the Bucur Maternity Hospital, the St. John Emergency Clinical Hospital, 164 biopsies of the uterine scar were made between 2015 and 2019. Their histological analysis identified several parameters that account for the predisposition of the placenta to insert at the scar level. The lack of decidualization at the scar level significantly increases the risk of placenta percreta [26,28].
Many authors advocate in favor of vaginal birth, reducing the number of Caesarean sections and the complications that result from it [4,5,6,7]. Uterine rupture and placental abnormalities are the most serious complications of scarred uterus after Caesarean sections. These can lead to emergency hysterectomies with an impact on fertility and the maternal psychological state [32,33,34,35].
Conclusions
Of the women who had given births both naturally and by Caesarean section, the vast majority (77%) stated that natural birth is preferable and they would recommend it as the first choice when it comes to giving birth.
The analysis of the cases in which they would recommend birth by Caesarean section revealed that they objectively had births that were not optimally managed and hence the recommendation of careful, professional evaluation of the conditions of birth for each case.
Reaching an optimal rate of Caesarean sections is an objective that can be achieved through correct information, health education, option sharing with those who have had these experiences, the correct assessment of the cases and the choice of the birth path according to specific medical conditions.
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
Compliance with ethical standards
The St. John’s Emergency Clinical Hospital Ethical Committee approved this descriptive cross-sectional study. All procedures performed in this study were in accordance with the ethical standards of the national research committee and with the Helsinki declaration and its latter amendments.
Authors’ contributions
OOG contributed to the selection of patients, the establishment of study groups, the analysis and interpretation of patient data, and the writing of the article. ADS, LP and CR contributed to the establishment of groups, the analysis and interpretation of patient data, and the writing of the article. ODB contributed to the establishment of groups, and the analysis and interpretation the data used for the article.
References
- Dimitriu, M.; Ionescu, C.A.; Matei, A.; Viezuina, R.; Rosu, G.; Ilinca, C.; Banacu, M.; Ples, L. The problems associated with adolescent pregnancy in Romania: A cross-sectional study. J Eval Clin Pract. 2019, 25, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Stoll, K.H.; Hauck, Y.L.; Downe, S.; Payne, D.; Hall, W.A.; International Childbirth Attitudes-Prior to Pregnancy (ICAPP) Study Team. Preference for cesarean section in young nulligravid women in eight OECD countries and implications for reproductive health education. Reprod Health. 2017, 14, 116. [Google Scholar] [CrossRef] [PubMed]
- Erasun, D.; Alonso-Molero, J.; Gómez-Acebo, I.; Dierssen-Sotos, T.; Llorca, J.; Schneider, J. Low birth weight trends in Organisation for Economic Co-operation and Development countries, 2000-2015: Economic, health system and demographic conditionings. BMC Pregnancy Childbirth. 2021, 21, 13. [Google Scholar] [CrossRef]
- Keag, O.E.; Norman, J.E.; Stock, S.J. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med. 2018, 15, e1002494. [Google Scholar] [CrossRef] [PubMed]
- Betran, A.P.; Torloni, M.R.; Zhang, J.; Ye, J.; Mikolajczyk, R.; Deneux-Tharaux, C.; Oladapo, O.T.; Souza, J.P.; Tunçalp, Ö.; Vogel, J.P.; Gülmezoglu, A.M. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health. 2015, 12, 57. [Google Scholar] [CrossRef] [PubMed]
- Harrison, M.S.; Pasha, O.; Saleem, S.; Ali, S.; Chomba, E.; Carlo, W.A.; Garces, A.L.; Krebs, N.F.; Hambidge, K.M.; Goudar, S.S.; Kodkany, B.; Dhaded, S.; Derman, R.J.; Patel, A.; Hibberd, P.L.; Esamai, F.; Liechty, E.A.; Moore, J.L.; Wallace, D.; Mcclure, E.M.; Miodovnik, M.; Koso-Thomas, M.; Belizan, J.; Tshefu, A.K.; Bauserman, M.; Goldenberg, R.L. A prospective study of maternal, fetal and neonatal outcomes in the setting of cesarean section in low-and middle-income countries. Acta Obstet Gynecol Scand. 2017, 96, 410–420. [Google Scholar] [CrossRef]
- Pang, M.W.; Leung, T.N.; Lau, T.K.; Hang Chung, T.K. Impact of first childbirth on changes in women’s preference for mode of delivery: Follow-up of a longitudinal observational study. Birth. 2008, 35, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Boatin, A.A.; Schlotheuber, A.; Betran, A.P.; Moller, A.B.; Barros, A.J.D.; Boerma, T.; Torloni, M.R.; Victora, C.G.; Hosseinpoor, A.R. Within country inequalities in caesarean section rates: Observational study of 72 low and middle income countries. BMJ. 2018, 360, k55. [Google Scholar] [CrossRef] [PubMed]
- Ples, L.; Sima, R.M.; Carp, D.; Alexandroaia, C.; Balalau, D.O.; Stanescu, A.D.; Olaru, O.G. The psychosocial impact of vaginal delivery and caesarean section in primiparous woman. J Mind Med Sci. 2018, 5, 70–74. [Google Scholar] [CrossRef]
- Bălălău, O.D.; Olaru, O.G.; Dumitru, V.; Păunică, I.; Stănescu, A.D. Maternal infections with an increased risk of transmission to the foetus; a literature review. J Clin Invest Surg. 2020, 5, 66–72. [Google Scholar] [CrossRef]
- Deng, W.; Klemetti, R.; Long, Q.; Wu, Z.; Duan, C.; Zhang, W.H.; Ronsmans, C.; Zhang, Y.; Hemminki, E. Cesarean section in Shanghai: Women’s or healthcare provider’s preferences? BMC Pregnancy Childbirth. 2014, 14, 285. [Google Scholar] [CrossRef]
- Ye, J.; Zhang, J.; Mikolajczyk, R.; Torloni, M.R.; Gülmezoglu, A.M.; Betran, A.P. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: A worldwide population-based ecological study with longitudinal data. BJOG. 2016, 123, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Saisto, T.; Halmesmäki, E. Fear of childbirth: A neglected dilemma. Acta Obstet Gynecol Scand. 2003, 82, 201–208. [Google Scholar]
- Eide, K.T.; Morken, N.H.; Bærøe, K. Maternal reasons for requesting planned cesarean section in Norway: A qualitative study. BMC Pregnancy Childbirth. 2019, 19, 102. [Google Scholar] [CrossRef]
- Pang, M.W.; Leung, T.N.; Lau, T.K.; Hang Chung, T.K. Impact of first childbirth on changes in women’s preference for mode of delivery: Follow-up of a longitudinal observational study. Birth. 2008, 35, 121–128. [Google Scholar] [CrossRef]
- Finger, C. Caesarean section rates skyrocket in Brazil. Many women are opting for caesareans in the belief that it is a practical solution. Lancet. 2003, 362, 628. [Google Scholar] [CrossRef]
- Alexandroaia, C.; Sima, R.M.; Balalau, O.D.; Olaru, O.G.; Ples, L. Patients’ perception of childbirth according to the delivery method: The experience in our clinic. J Mind Med Sci. 2019, 6, 311–318. [Google Scholar] [CrossRef]
- Bălălău, O.-D.; Bacalbașa, N.; Olaru, O.G.; Pleș, L.; Stănescu, D.A. Vaginal birth after cesarean section—Literature review and modern guidelines. J Clin Invest Surg. 2020, 5, 13–17. [Google Scholar] [CrossRef]
- Ross-Davie, M.; McElligott, M.; King, K.; Little, M. Midwifery support in labour: How important is it to stay in the room? Pract Midwife. 2014, 17, 19–22. [Google Scholar]
- Motofei, I.G.; Rowland, D.L.; Georgescu, S.R.; Tampa, M.; Paunica, S.; Constantin, V.D.; Balalau, C.; Manea, M.; Baleanu, B.C.; Sinescu, I. Post-Finasteride Adverse Effects in Male Androgenic Alopecia: A Case Report of Vitiligo. Skin Pharmacol Physiol. 2017, 30, 42–45. [Google Scholar] [CrossRef]
- Sigurdardottir, V.L.; Gamble, J.; Gudmundsdottir, B.; Kristjansdottir, H.; Sveinsdottir, H.; Gottfredsdottir, H. The predictive role of support in the birth experience: A longitudinal cohort study. Women Birth. 2017, 30, 450–459. [Google Scholar] [CrossRef] [PubMed]
- Maputle, M.S. Support provided by midwives to women during labour in a public hospital, Limpopo Province, South Africa: A participant observation study. BMC Pregnancy Childbirth. 2018, 18, 210. [Google Scholar] [CrossRef]
- Cetisli, N.E.; Arkan, G.; Top, E.D. Maternal attachment and breastfeeding behaviors according to type of delivery in the immediate postpartum period. Rev Assoc Med Bras (1992). 2018, 64, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Zaręba, K.; Banasiewicz, J.; Rozenek, H.; Wójtowicz, S.; Jakiel, G. Peripartum Predictors of the Risk of Postpartum Depressive Disorder: Results of a Case-Control Study. Int J Environ Res Public Health. 2020, 17, 8726. [Google Scholar] [CrossRef]
- Ye, J.; Zhang, J.; Mikolajczyk, R.; Torloni, M.R.; Gülmezoglu, A.M.; Betran, A.P. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: A worldwide population-based ecological study with longitudinal data. BJOG. 2016, 123, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Bălălău, O.D.; Bacalbașa, N.; Stănescu, A.D. Caesarean scar defects and placental abnormalities: A three-year survey study. J Mind Med Sci. 2017, 4, 156–162. [Google Scholar] [CrossRef]
- Yang, Q.; Wen, S.W.; Oppenheimer, L.; Chen, X.K.; Black, D.; Gao, J.; Walker, M.C. Association of caesarean delivery for first birth with placenta praevia and placental abruption in second pregnancy. BJOG. 2007, 114, 609–613. [Google Scholar] [CrossRef]
- Bălălău, O.D.; Bacalbașa, N.; Bălălău, C.; Negrei, C.; Gălățeanu, B.; Ghinghină, O.; Răduță, C.; Pleș, L.; Stănescu, A.D.; Dumitru, V.A. The correlation between histopathological and ultrasound findings regarding Caesarean section scars—A three-year survey study. J Mind Med Sci. 2019, 6, 143–149. [Google Scholar] [CrossRef]
- Walker, S.P.; McCarthy, E.A.; Ugoni, A.; Lee, A.; Lim, S.; Permezel, M. Cesarean delivery or vaginal birth: A survey of patient and clinician thresholds. Obstet Gynecol. 2007, 109, 67–72. [Google Scholar] [CrossRef]
- Leung, A.S.; Leung, E.K.; Paul, R.H. Uterine rupture after previous cesarean delivery: Maternal and fetal consequences. Am J Obstet Gynecol. 1993, 169, 945–950. [Google Scholar] [CrossRef]
- Bălălău, O.D.; Sima, R.M.; Bacalbașa, N.; Pleș, L.; Stănescu, A.D. Emergency peripartum hysterectomy, physical and mental consequences: A 6-year study. J Mind Med Sci. 2016, 3, 65–70. [Google Scholar]
- Stănescu, A.D.; Bălălău, O.D.; Pleș, L.; Paunica, S.; Bălălău, C. Postpartum depression: Prevention and multimodal therapy. J Mind Med Sci. 2018, 5, 164–168. [Google Scholar] [CrossRef]
- Pană, M.; Sima, R.-M.; Bălălău, O.-D.; Stănescu, A.-D.; Pleş, L.; Poenaru, M.-O. The quality of sexual life after vaginal surgical interventions. J Mind Med Sci. 2020, 7, 201–205. [Google Scholar] [CrossRef]
- Balalau, C.; Voiculescu, S.; Motofei, I.; Scaunasu, R.V.; Negrei, C. Low dose tamoxifen as treatment of benign breast proliferative lesions. Farmacia. 2015, 63, 371–375. [Google Scholar]
- Morlando, M.; Sarno, L.; Napolitano, R.; Capone, A.; Tessitore, G.; Maruotti, G.M.; Martinelli, P. Placenta accreta: Incidence and risk factors in an area with a particularly high rate of cesarean section. Acta Obstet Gynecol Scand. 2013, 92, 457–460. [Google Scholar] [CrossRef]
© 2008 by the author. 2008 Octavian Gabriel Olaru, Anca Daniela Stanescu, Cristina Raduta, Liana Ples, Adriana Vasilache, Nicolae Bacalbasa, Andrei Vasilache, Oana Denisa Balalau