The Social and the Psychological Impact of Endometriosis on the Romanian Urban Population
Abstract
:Introduction
Materials and Methods
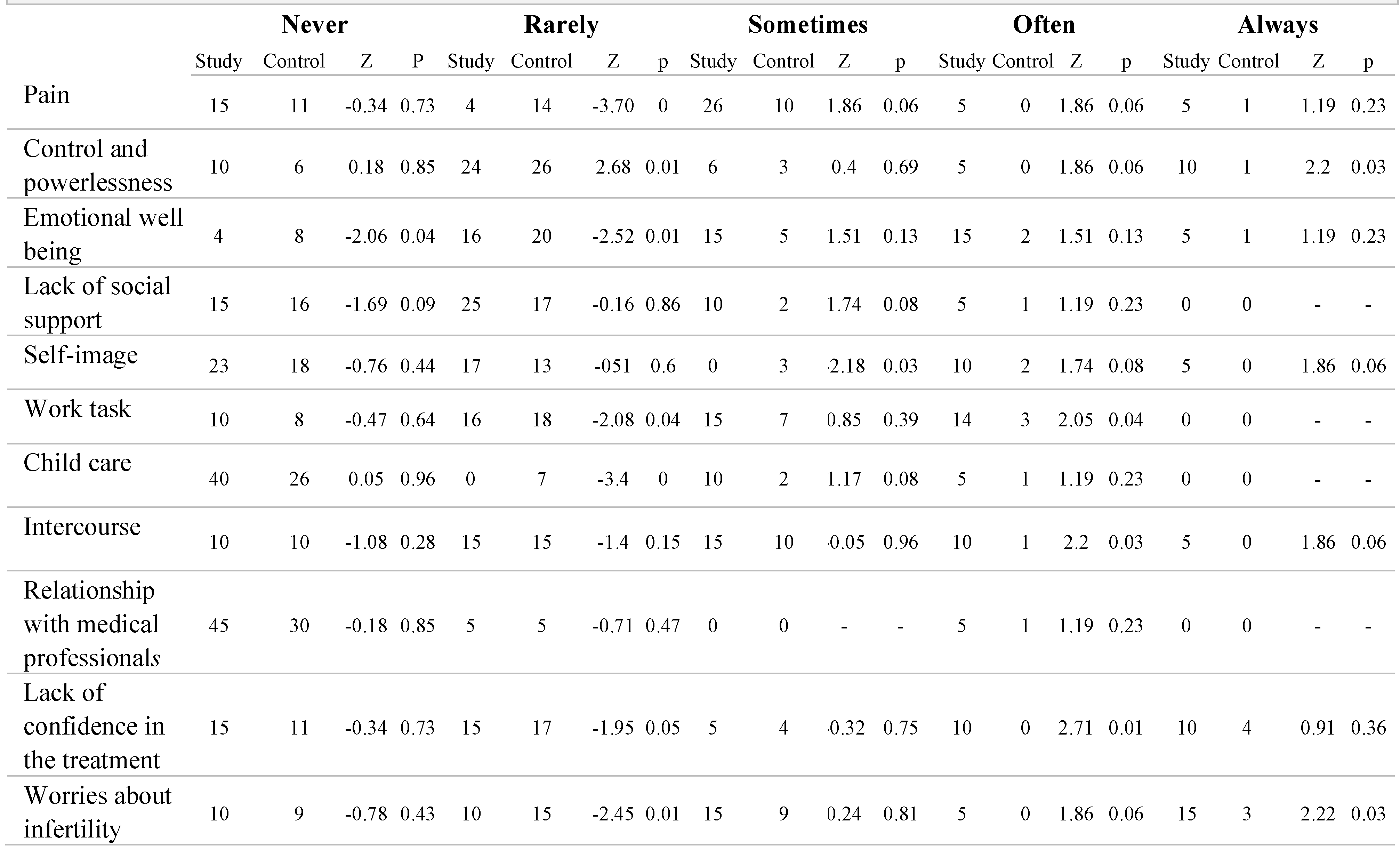
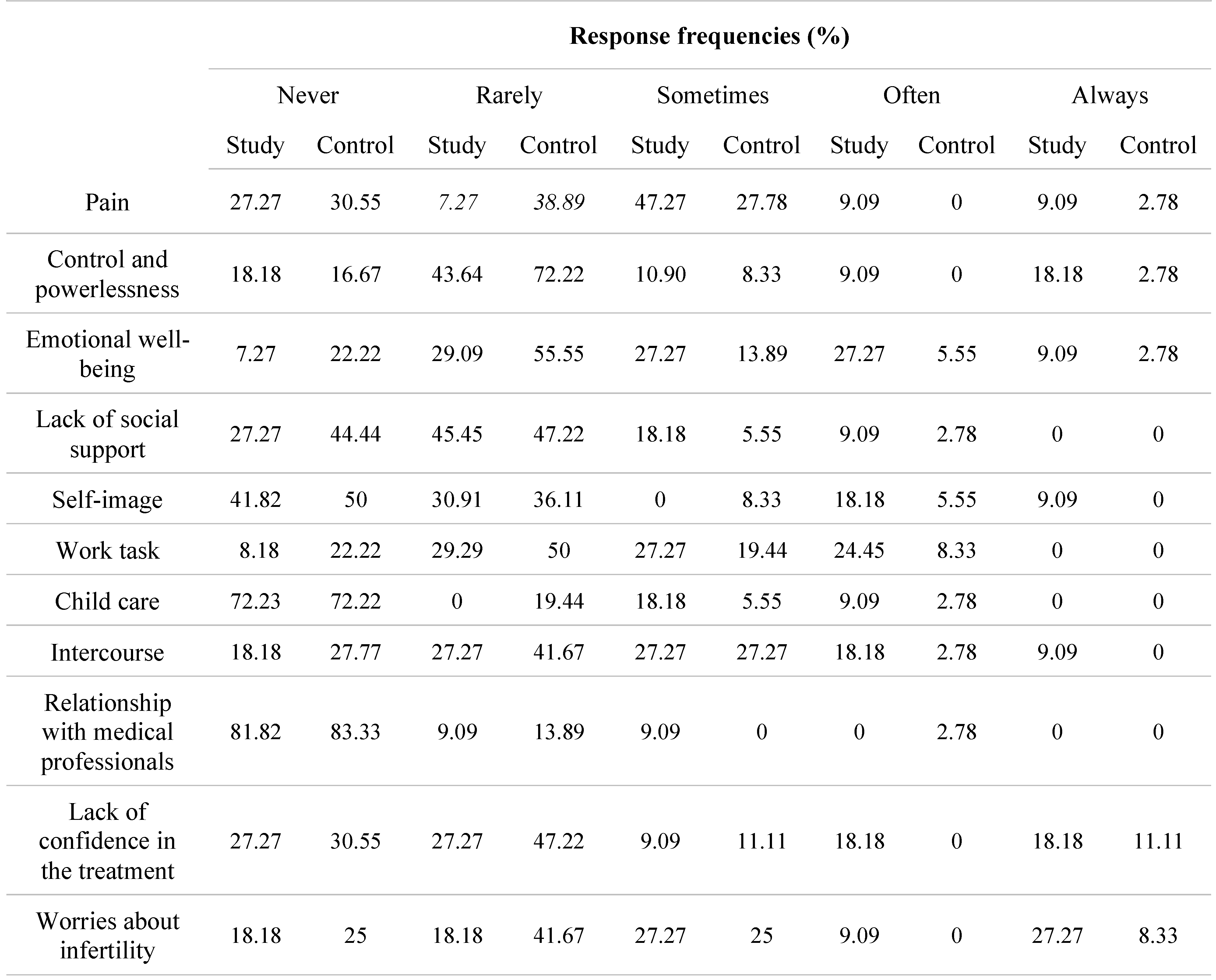
Results
Discussions
Conclusions
Conflict of interest disclosure
Compliance with ethical standards
Acknowledgments
References
- Viganò, P.; Parazzini, F.; Somigliana, E.; Vercellini, P. Endometriosis: Epidemiology and aetiological factors. Best Pract Res Clin Obstet Gynaecol. 2004, 18, 177–200. [Google Scholar] [CrossRef] [PubMed]
- Gica, N.; Panaitescu, A.M.; Iancu, G.; Botezatu, R.; Peltecu, G.; Gica, C. The role of biological markers in predicting infertility associated with non-obstructive endometriosis. Ginekol Pol. 2020, 91, 189–192. [Google Scholar] [CrossRef]
- Burney, R.O.; Giudice, L.C. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012, 98, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Parazzini, F.; Esposito, G.; Tozzi, L.; Noli, S.; Bianchi, S. Epidemiology of endometriosis and its comorbidities. Eur J Obstet Gynecol Reprod Biol. 2017, 209, 3–7. [Google Scholar] [CrossRef]
- Bulun, S.E. Endometriosis. N Engl J Med. 2009, 360, 268–279. [Google Scholar] [CrossRef] [PubMed]
- Gica, N.; Mustata, L.; Botezatu, R.; Chirculescu, R.; Cigaran, R.; Gica, C.; Panaitescu, M.; Peltecu, G. Management of Borderline Ovarian Tumors: Series of Case Report and Review of the Literature. Indian J Surg. 2020. [Google Scholar] [CrossRef]
- Gica, N.; Mat, C.; Cigaran, R.; Peltecu, G.; Panaitescu, A. Non-obstructive Endometriosis and Infertility. In Proceedings of the SOGR 2018: The 17th National Congress of The Romanian Society of Obstetrics and Gynecology & First Advanced Colposcopy Course, Iaşi, Romania, 19–22 September 2018; Filodiritto Publisher: Bologna, Italy, 2019; pp. 349–351. [Google Scholar]
- Bulletti, C.; Coccia, M.E.; Battistoni, S.; Borini, A. Endometriosis and infertility. J Assist Reprod Genet. 2010, 27, 441–447. [Google Scholar] [CrossRef]
- Wium-Andersen, M.K.; Ørsted, D.D.; Nielsen, S.F.; Nordestgaard, B.G. Elevated C-reactive protein levels, psychological distress, and depression in 73, 131 individuals. JAMA Psychiatry. 2013, 70, 176–184. [Google Scholar] [CrossRef]
- Nasyrova, R.F.; Sotnikova, L.S.; Baystrukova, N.V.; Krivoschchekova, G.V.; Novitsky, V.V.; Kupriyanova, I.E.; Semke, V.Y.; Naslednikova, I.O.; Baykov, A.N. Psychoimmune interactions in women of reproductive age with endometriosis. Bull Exp Biol Med. 2011, 152, 93–97. [Google Scholar] [CrossRef]
- Facchin, F.; Barbara, G.; Saita, E.; Mosconi, P.; Roberto, A.; Fedele, L.; Vercellini, P. Impact of endometriosis on quality of life and mental health: Pelvic pain makes the difference. Journal of Psychosomatic Obstetrics & Gynecology. 2015, 36, 135–141. [Google Scholar] [CrossRef]
- Simoens, S.; Dunselman, G.; Dirksen, C.; Hummelshoj, L.; Bokor, A.; Brandes, I.; Brodszky, V.; Canis, M.; Colombo, G.L.; DeLeire, T.; Falcone, T.; Graham, B.; Halis, G.; Horne, A.; Kanj, O.; Kjer, J.J.; Kristensen, J.; Lebovic, D.; Mueller, M.; Vigano, P.; Wullschleger, M.; D’Hooghe, T. The burden of endometriosis: Costs and quality of life of women with endometriosis and treated in referral centres. Hum Reprod. 2012, 27, 1292–1299. [Google Scholar] [CrossRef] [PubMed]
- Huntington, A.; Gilmour, J.A. A life shaped by pain: Women and endometriosis. J Clin Nurs. 2005, 14, 1124–1132. [Google Scholar] [CrossRef] [PubMed]
- Laganà, A.S.; La Rosa, V.L.; Rapisarda, A.M.C.; Valenti, G.; Sapia, F.; Chiofalo, B.; Rossetti, D.; Ban Frangež, H.; Vrtačnik Bokal, E.; Vitale, S.G. Anxiety and depression in patients with endometriosis: Impact and management challenges. Int J Womens Health. 2017, 9, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Souza, C.A.; Oliveira, L.M.; Scheffel, C.; Genro, V.K.; Rosa, V.; Chaves, M.F.; Cunha Filho, J.S. Quality of life associated to chronic pelvic pain is independent of endometriosis diagnosis--a cross-sectional survey. Health Qual Life Outcomes. 2011, 9, 41. [Google Scholar] [CrossRef]
- Tripoli, T.M.; Sato, H.; Sartori, M.G.; de Araujo, F.F.; Girão, M.J.; Schor, E. Evaluation of quality of life and sexual satisfaction in women suffering from chronic pelvic pain with or without endometriosis. J Sex Med. 2011, 8, 497–503. [Google Scholar] [CrossRef]
- Denny, E.; Mann, C.H. A clinical overview of endometriosis: A misunderstood disease. Br J Nurs. 2007, 16, 1112–1116. [Google Scholar] [CrossRef]
- Siedentopf, F.; Tariverdian, N.; Rücke, M.; Kentenich, H.; Arck, P.C. Immune status, psychosocial distress and reduced quality of life in infertile patients with endometriosis. Am J Reprod Immunol. 2008, 60, 449–461. [Google Scholar] [CrossRef]
- Berek, J.S. Berek and Novak’s Gynecology, 15th ed.; Lippincott Williams & Wilkins, North American Edition: Philadelphia, PA, USA, 2012; ISBN-13: 978-1451114331. [Google Scholar]
- Fourquet, J.; Báez, L.; Figueroa, M.; Iriarte, R.I.; Flores, I. Quantification of the impact of endometriosis symptoms on health-related quality of life and work productivity. Fertil Steril. 2011, 96, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.; Jenkinson, C.; Kennedy, S. Development of the Short Form Endometriosis Health Profile Questionnaire: The EHP-5. Qual Life Res. 2004, 13, 695–704. [Google Scholar] [CrossRef]
- Cavaggioni, G.; Lia, C.; Resta, S.; Antonielli, T.; Benedetti Panici, P.; Megiorni, F.; Porpora, M.G. Are mood and anxiety disorders and alexithymia associated with endometriosis? A preliminary study. Biomed Res Int. 2014, 2014, 786830. [Google Scholar] [CrossRef]
- Missmer, S.A.; Tu, F.F.; Agarwal, S.K.; Chapron, C.; Soliman, A.M.; Chiuve, S.; Eichner, S.; Flores-Caldera, I.; Horne, A.W.; Kimball, A.B.; Laufer, M.R.; Leyland, N.; Singh, S.S.; Taylor, H.S.; As-Sanie, S. Impact of Endometriosis on Life- Course Potential: A Narrative Review. Int J Gen Med. 2021, 14, 9–25. [Google Scholar] [CrossRef] [PubMed]
- Pană, M.; Sima, R.-M.; Bălălău, O.-D.; Stănescu, A.-D.; Pleş, L.; Poenaru, M.-O. The quality of sexual life after vaginal surgical interventions. J Mind Med Sci. 2020, 7, 201–205. [Google Scholar] [CrossRef]
- Sperschneider, M.L.; Hengartner, M.P.; Kohl-Schwartz, A.; Geraedts, K.; Rauchfuss, M.; Woelfler, M.M.; Haeberlin, F.; von Orelli, S.; Eberhard, M.; Maurer, F.; Imthurn, B.; Imesch, P.; Leeners, B. Does endometriosis affect professional life? A matched case-control study in Switzerland, Germany and Austria. BMJ Open. 2019, 9, e019570. [Google Scholar] [CrossRef] [PubMed]
- Vesali, S.; Razavi, M.; Rezaeinejad, M.; Maleki-Hajiagha, A.; Maroufizadeh, S.; Sepidarkish, M. Endometriosis fertility index for predicting non-assisted reproductive technology pregnancy after endometriosis surgery: A systematic review and meta-analysis. BJOG. 2020, 127, 800–809. [Google Scholar] [CrossRef]
- Iordachescu, D.A.; Gica, C.; Vladislav, E.O.; Panaitescu, A.M.; Peltecu, G.; Furtuna, M.E.; Gica, N. Emotional disorders, marital adaptation and the moderating role of social support for couples under treatment for infertility. Ginekol Pol. 2021, 92, 98–104. [Google Scholar] [CrossRef]
- Garai, J.; Molnar, V.; Varga, T.; Koppan, M.; Torok, A.; Bodis, J. Endometriosis: Harmful survival of an ectopic tissue. Front Biosci. 2006, 11, 595–619. [Google Scholar] [CrossRef]
- Culley, L.; Law, C.; Hudson, N.; Denny, E.; Mitchell, H.; Baumgarten, M.; Raine-Fenning, N. The social and psychological impact of endometriosis on women’s lives: A critical narrative review. Hum Reprod Update. 2013, 19, 625–639. [Google Scholar] [CrossRef]

 |
 |
 |
© 2008 by the author. 2008 Iulia Baciu, Alecsandra Irimie-Ana, Anca Maria Panaitescu, Gheorghe Peltecu, Corina Gica, Nicolae Gica
Share and Cite
Baciu, I.; Irimie-Ana, A.; Panaitescu, A.M.; Peltecu, G.; Gica, C.; Gica, N. The Social and the Psychological Impact of Endometriosis on the Romanian Urban Population. J. Mind Med. Sci. 2021, 8, 120-126. https://doi.org/10.22543/7674.81.P120126
Baciu I, Irimie-Ana A, Panaitescu AM, Peltecu G, Gica C, Gica N. The Social and the Psychological Impact of Endometriosis on the Romanian Urban Population. Journal of Mind and Medical Sciences. 2021; 8(1):120-126. https://doi.org/10.22543/7674.81.P120126
Chicago/Turabian StyleBaciu, Iulia, Alecsandra Irimie-Ana, Anca Maria Panaitescu, Gheorghe Peltecu, Corina Gica, and Nicolae Gica. 2021. "The Social and the Psychological Impact of Endometriosis on the Romanian Urban Population" Journal of Mind and Medical Sciences 8, no. 1: 120-126. https://doi.org/10.22543/7674.81.P120126
APA StyleBaciu, I., Irimie-Ana, A., Panaitescu, A. M., Peltecu, G., Gica, C., & Gica, N. (2021). The Social and the Psychological Impact of Endometriosis on the Romanian Urban Population. Journal of Mind and Medical Sciences, 8(1), 120-126. https://doi.org/10.22543/7674.81.P120126



