Abstract
Measles remains an important cause of morbidity and mortality worldwide. Most HIV-infected adults are immune against measles, so titres of measles antibodies should be determined prior to vaccination. A measles vaccine can be administered to HIV-positive patients who do not have protective antibody levels and who have a CD4 lymphocyte count ≥ 200 cells/mm3. We describe the case of an HIV-infected patient, diagnosed with complicated measles at our Infectious Diseases Hospital in April 2024.
1. Introduction
Measles remains an important cause of morbidity and mortality worldwide. In 2023, there were over 30,000 cases of measles globally [1]. From 1 September 2023 to 31 August 2024, 30 European Union Member States reported a total of 18,449 cases, of which 8206 (44.5%) were in children under five years of age and 5148 (27.9%) cases were aged 15 years or older. In August 2024, the highest number of cases was reported in Romania (532 cases), Germany (95), Italy (53) and Ireland (23). Of 15,855 cases with a known vaccination status, 13,814 (87.1%) were unvaccinated, 1305 (8.2%) were vaccinated with one dose, 691 (4.4%) were vaccinated with two or more doses, and 25 (0.2%) were vaccinated with an unknown number of doses [2].
Between 1 January 2023 and 31 December 2024, a total of 27,234 people were diagnosed with measles in Romania. During this period, there were 22 deaths recorded [3].
Human immunodeficiency virus (HIV) infection increases measles susceptibility in children. Most HIV-infected adults are immune against measles, so titres of measles antibodies should be determined prior to vaccination [4].
Children born to HIV-positive mothers have lower levels of antibodies against the measles virus, passively acquired from the mother, increasing susceptibility to measles at a younger age [5]. HIV-infected children may have a poor primary immune response to a measles vaccine and protective antibody levels may decrease in children not receiving antiretroviral treatment [6].
The World Health Organization recommends the measles vaccination of children living with HIV infection at 6 months of age rather than 9 months and measles revaccination after immune reconstitution with combination antiretroviral therapy [6].
In Romania, the measles vaccination of HIV-infected children, who are not severely immunocompromised is recommended: two doses of measles vaccine to patients with a CD4 count ≥ 200 cells/mm3 (first dose at 12 months of age and second dose at 6 years of age) and who have no evidence of immunity to measles [7]
The clinical presentation of measles in HIV-infected patients may be atypical. Exanthem may be absent or severe and desquamative; purpura has also been described. There should be a high level of suspicion when a patient living with HIV presents with pneumonia or encephalitis, particularly after measles exposure and despite previous immunization [8]. Severe complications, such as measles pneumonia, have been described in patients with low CD4 lymphocyte counts [9].
The European AIDS Clinical Society recommends testing for measles seropositivity at the time of HIV infection diagnosis and the administration of the measles vaccine in the case of seronegativity. Although the vaccine efficacy is lower in HIV-infected adults, this vaccine is considered to be safe in HIV-infected subjects with a CD4 count > 200 cells/mm3 [10].
The objective of this work is to present a case of complicated measles in an HIV-infected patient with a low grade of immunosuppression and an undetectable HIV viral load, incompletely vaccinated against measles, suggesting that a booster measles dose should be considered in HIV-infected individuals.
2. Case Report
We describe the case of a 33-year-old male, from a rural area, who was admitted on April 2024 to the Infectious Diseases Department of Craiova, Romania, reporting fever (39 °C), nasal congestion, sore throat, dry cough and a erythematous maculopapular rash. The onset of the disease was 6 days earlier. Two weeks before first symptoms appeared, the patient had close contact with a patient with acute respiratory infection, further confirmed to have measles by general practitioner.
His past medical history revealed that he was diagnosed with HIV in 1998 and began receiving ART after HIV diagnosis until now. The route of HIV acquisition was most likely mother-to-child transmission. The patient’s birth took place at home and he was tested for HIV during a hospitalization for a persistent lower respiratory tract infection at the age of 7. Then, his mother was also tested for HIV and the test was positive. Ten years ago, the patient has been diagnosed with chronic kidney disease and renovascular hypertension.
Up to now, the patient has been hospitalized many times for multiple infections, especially respiratory ones. He received one dose of measles-containing vaccine at 12 months of age and then, at the age of 6, he did not show up for the full vaccination schedule. Also, 7 years ago, the patient was diagnosed with pulmonary tuberculosis, for which he received antituberculous drugs.
The objective examination at the time of admission in our clinic revealed a moderate general condition, a febrile patient, with normal weight (body mass index = 22.4 kg/m2), an erythematous maculopapular rash localized on the face, thorax and abdomen, and on the upper and lower limbs, hyperemia of the tonsils and pharyngeal mucosa, Koplik spots, generalized polyadenopathy, vesicular breath sounds on lung auscultation, oxygen saturation = 92%, heart rate = 106 beats per minute, blood pressure = 119/72 mmHg, a soft abdomen, which was painless on palpation, and no signs of meningeal irritation.
The initial laboratory tests are shown in Table 1.

Table 1.
Results of laboratory test.
Anti-measles virus IgG antibodies were not performed.
Two months ago, immunovirological data revealed a low-grade immunosuppression (CD4 count = 509 cells/mm3) and an undetectable HIV viral load.
The chest X-ray showed no active lesions.
The patient’s initial treatment included vitamin A in 100.000 international units (UI) per day, vitamin D in 2000 UI per day, 4–5 liters of O2 per minute, corticosteroids (sputum smear for MTB was negative, chest X-ray showed no active lesions, the patient presented with dyspnea and a low level of oxygen saturation), antiretroviral treatment (Tenofovir disoproxil fumarate + Darunavir/ritonavir + Raltegravir), parenteral hydro-electrolytic rebalancing therapy and symptomatic drugs.
On the seventh day of hospitalization, the patient’s condition worsened and he began to exhibit chest pain, recurrence of fever after 4 days of being afebrile, and right basal subcrepitant rales. A chest X-ray was performed, which showed an inhomogeneous opacity (3.8/3.7 cm) on the lower right lobe and a residual inhomogeneous opacity on the upper left lobe (Figure 1). Biological tests showed leukocytosis (31.910 cells/mm3) with neutrophilia (81.3%) and lymphopenia (7%), an inflammatory syndrome (erythrocyte sedimentation rate (ESR) = 27 mm/1 h, fibrinogen = 507 mg/dL, procalcitonin = 12.27 ng/mL), a syndrome of nitrogen retention (creatinine = 1.91 mg/dL, urea = 107 mg/dL), and a CD4 count = 395 cells/mm3. The patient received antibiotic treatment with Meropenem 1 g/12 h (empirical treatment for bacterial suprainfection; creatinine clearance = 48 mL/min) and the initial antiretroviral therapy was replaced with Bictegravir/Emtricitabine/Tenofovir Alafenamide (for regimen simplification).
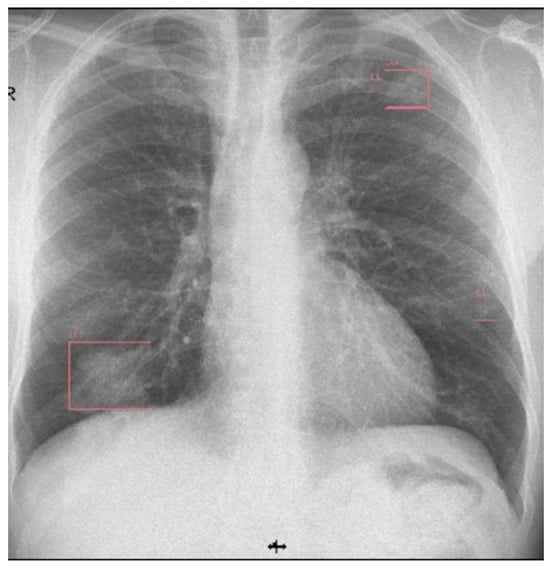
Figure 1.
Chest X-ray (day 7).
On the fourteenth day, the number of leucocytes and inflammatory markers continued to increase (L = 42.000 cells/mm3, ESR = 30 mm/1 h, C-reactive protein = 102 mg/L) and the chest X-ray found reticulomicronodular opacities with pleural effusion on the right (Figure 2).
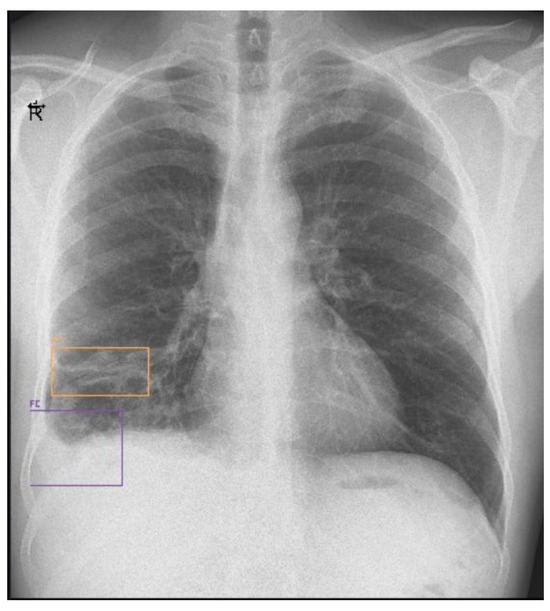
Figure 2.
Chest X-ray (day 14) showing pleural effusion.
On the twentieth day, the chest X-ray showed multiple hydro-aerial levels up to 85/90 mm on the right lung (Figure 3). A chest computed tomography (CT) revealed free air and fluid levels within the pleural space with collapsed lung parenchyma (hydropneumothorax) and mediastinal lymphadenopaty (Figure 4).
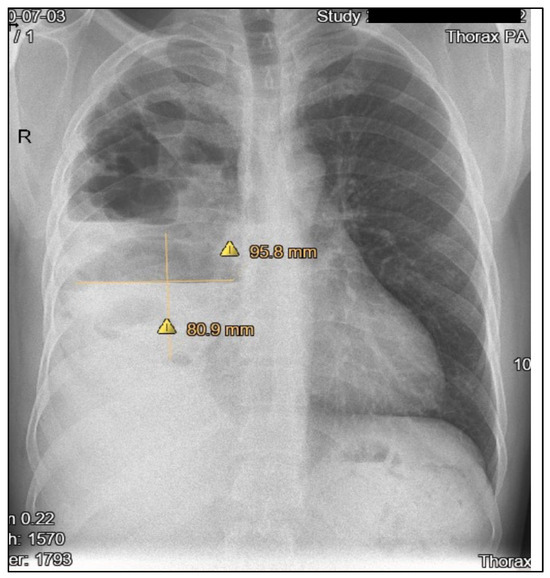
Figure 3.
Chest X-ray (day 20) showing hydro-aerial levels.
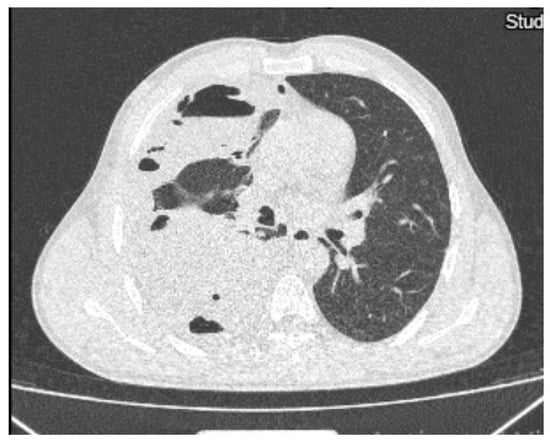
Figure 4.
Chest computed tomography showing hydropneumothorax.
For 17 days, the patient received treatment with antibiotics (Meropenem in 1 g/8 h, Vancomycin in 1 g/12 h, Ciprofloxacin in 400 mg/8 h for the lung abscess, for broad spectrum-aerobic, anaerobic, Gram-positive and Gram-negative bacteria), antifungals (Fluconazole in 200 mg/24 h), corticosteroids, oxygen therapy, antiretroviral and symptomatic drugs.
On the twenty-third day, the clinical examination of the patient found an abolished vesicular murmur on the right hemithorax and crepitant rales. Diagnostic thoracocentesis was performed, with the removal of 180 mL of pleural fluid. Cytological examination revealed a predominance of polymorphonuclear cells (85%), biochemical examination showed a high protein level (41.8 g/L) and a low glucose level (4 mg/dL) and the cultures were negative, as well as the GeneXpert MTB.
Between days 24 and 35 of hospitalization, the patient’s general condition was relatively stable, with periodic febrile episodes. Laboratory tests showed the persistence of the inflammatory syndrome (fibrinogen = 620 mg/dL, C-reactive protein = 43.35 mg/L) and negative blood cultures and the radiographic appearances remained the same.
After dynamic imaging, multiple pulmonology and thoracic surgery consultations, the patient’s diagnoses were a right pyopneumothorax, a lung abscess on the lower right lobe and middle lobe, and pulmonary sepsis.
On the thirty-sixth day, following the thoracic surgery consultation, a chest drain tube was inserted and 100 mL of liquid was evacuated. The cultures of pleural fluid revealed the presence of Pseudomonas aeruginosa. The patient received antimicrobial treatment (Moxifloxacin in 400 mg/24 h, 5 days + Piperacilin/Tazobactam, and 14 days of de-escalation based on the antibiogram).
During the following days of hospitalization, the patient’s evolution was favorable, with an improved general condition, a decrease in inflammatory markers and the partial resorption of right side hydropneumothorax (Figure 5).
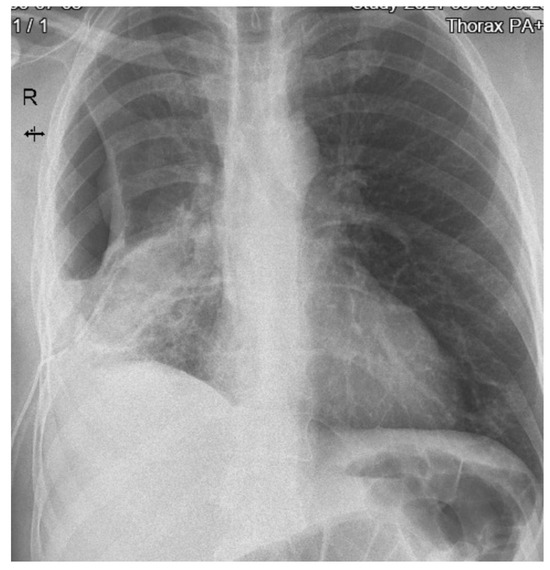
Figure 5.
Chest x-ray displaying partial resorption of right side hydropneumothorax.
After 19 days from drain tube’s insertion, a chest CT scan showed the important regression of lung lesions and pulmonary fibrosis (Figure 6).
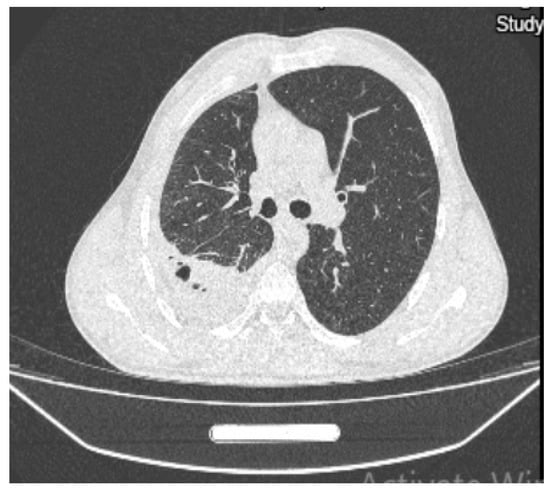
Figure 6.
Chest CT scan showing regression of lung lesions and pulmonary fibrosis.
The follow-up laboratory tests are shown in Figure 7.
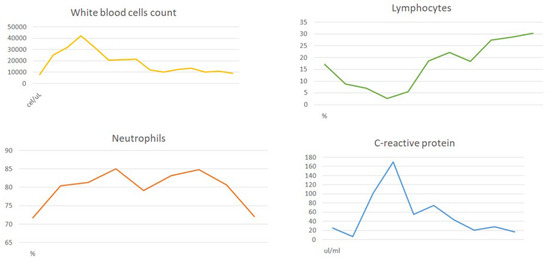
Figure 7.
Follow-up laboratory tests.
The patient was discharged after 58 days. The last chest X-ray was performed 8 weeks after being discharged (Figure 8).
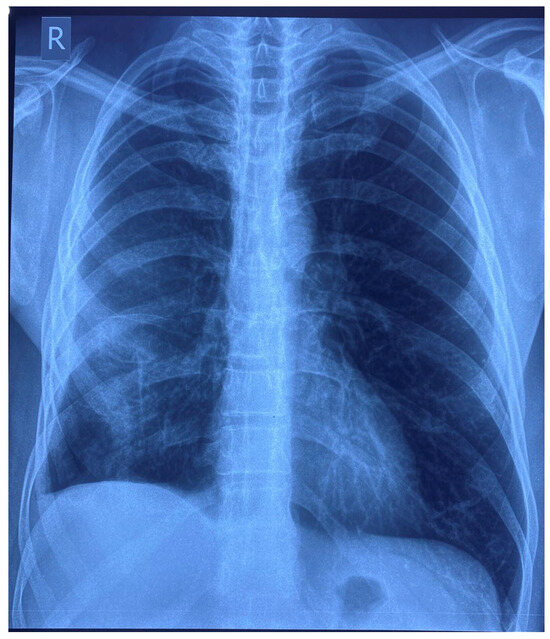
Figure 8.
Chest X-ray (8 weeks after discharge).
In September 2024, the CD4 cell count was 438 cells/mm3, HIV viremia was undetectable and the level of C-reactive protein was 2.87 mg/L.
3. Discussion
Measles remains a global public health problem. In patients living with HIV, measles is associated with atypical manifestations and higher mortality. Also, HIV infection is related to the delayed clearance of the measles virus and to prolonged measles viral shedding [11].
In a study performed in South Africa between 2009 and 2010, a group of 51 adult patients with suspected measles, admitted to the Infectious Diseases Unit of Charlotte Maxeke Johannesburg Academic Hospital, was analyzed. Thirty-three of these patients were confirmed to have measles by serology, twenty-four agreed to be tested for HIV infection and eighteen of these were HIV-infected. One HIV-infected patient reported a measles contact and two patients in the HIV-positive group had been vaccinated against measles in childhood. The median CD4 count was 109 cells/mm3 and the median HIV viral load was 15,000 copies/mL. Serious clinical manifestations were more frequent in HIV-positive than HIV-negative patients. One of the six HIV-negative patients developed pneumonia, while six of the eighteen HIV-positive patients had a clinical course complicated by pneumonia. HIV-infected patients had several other manifestations, like pancreatitis and encephalitis and also had a significantly longer hospital stay. There were three deaths reported in the HIV-positive group, but none in the HIV-negative group [11].
Despite the fact that the patient we presented received a dose of a measles vaccine, he developed serious complications related to measles virus infection and required a prolonged hospitalization.
The patient, being very adherent to ART, had a little drop in CD4 count compared to the last immunological evaluation (previous measles) and managed to fight against measles, even with major complications.
Several studies reflect that measles seropositivity is lower among vaccinated HIV-infected children, compared with HIV-uninfected children [4].
Children living with HIV can have poorer primary measles vaccine responses and a higher probability of waning immunity than HIV-uninfected children, so they can remain susceptible to measles despite vaccination.
In a study performed in Zambia between 2009 and 2013, 617 HIV-uninfected young people, 144 HIV-infected young people naive to ART and 128 HIV-infected young people who were receiving ART were tested for IgG antibodies to measles virus. The proportion of those who were seropositive for measles virus was significantly higher among the HIV-uninfected youths (92.5%) compared to the HIV-infected ART-naive youths (74.1%) and the HIV-infected youths receiving ART (71.9%) [12].
Another study conducted in the Pediatric Infectious Disease Clinic in Rabat included 50 HIV-infected children (mother-to-child transmission) and 64 HIV-uninfected children. The seroprotective rate for measles was significantly lower in the HIV-infected children (26%) than in the HIV-uninfected children (73%). Also, the HIV-infected children with no anti-measles antibodies IgG had lower CD4 counts and higher HIV viral loads (2.91 ± 2.24 log10 compared to 1.7 ± 1.5 log10) [13].
Although our patient had a CD4 count > 500 cells/mm3 and an undetectable HIV viral load, he developed a severe form of measles probably due to chronic inflammation caused by HIV infection and also due to suboptimal vaccination coverage.
A cross-sectional study conducted at an academic HIV clinic in Omaha, Nebraska between November 2019 and January 2020 included 351 patients living with HIV who were tested for the presence of measles IgG antibodies. The measles seroprevalence rate was 70.3%, which is lower than previously reported in patients living with HIV (92%), and considerably lower than the rate needed to maintain herd immunity (95%). No other risk factors like sex, ethnicity, body mass index, country of origin, CD4 nadir < 200 cells/mm3, history of opportunistic infections, history of malignancy, route of HIV transmission, duration of HIV disease, and use of immunosuppressant medications were found to be associated with seronegativity [14].
HIV infection has been associated with the reduced immunogenicity of measles containing viruses in children and with a more severe clinical course [15].
A multicenter study conducted at five clinics in the west of France, between April 2019 and April 2020, included 648 HIV-infected patients born after 1980; 603 of these were assessed. At inclusion in the study, 86% of patients had an undetectable HIV viral load, 161 (28.4%) patients were vaccinated against measles and 28 (4.3%) had a documented history of measles. Of the 603 patients evaluated, measles serology was positive in 526 (87.2%) cases, negative in 55 (9.1%) cases, and equivocal in 22 (3.7%) cases. All but one measles-seronegative patients had a CD4+ cell count greater than 200 cells/mm3 and would have been eligible for vaccination, according to current guidelines. Of the 155 patients with documented vaccination (one or two doses), 143 had no history of measles disease, of whom 117 (81.8%) presented with IgG antibodies. Rates of positive serology were 89.2%, 83.3%, and 79.8% when measles vaccination (one or two doses) was performed in the past 5 years, 5–10 years before serology, and, earlier, respectively (p > 0.05). Young age, the absence of social vulnerability and higher CD4 nadir were associated with measles seronegativity [16].
HIV-infected children without evidence of immunity and a CD4 count > 200 cells/mm3 should be administered an additional dose of measles-containing vaccine at six months of age in order to provide protection at a younger age, followed by two routine doses. Women living with HIV have a lower concentration of measles-specific antibodies and transmit lower measles antibodies to their infants, resulting in susceptibility to measles at a younger age than usual.
4. Conclusions
Measles remains a major cause of morbidity and mortality in Romania due to suboptimal vaccination coverage. People living with HIV are at higher risk of measles-related complications, even those with relatively preserved immune function. Further measles seroprevalence studies and benefits evaluations of the booster dose in HIV-positive patients without a history of measles or negative serology are needed.
Author Contributions
Conceptualization, E.-A.M., L.G., M.O. and F.D.; methodology, F.D.; software, C.-L.R.-T. and A.D.; validation, L.D, R.P., and M.O.; formal analysis, A.D., A.G.I. and I.-A.G.; investigation, E.-A.M. and A.G.I.; resources, F.D.; data curation, R.P. and M.O.; writing—original draft preparation, E.-A.M., F.D., L.D. and M.O.; writing—review and editing, L.G., M.O. and F.D.; visualization, M.O. and F.D.; supervision All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of the University of Medicine and Pharmacy of Craiova (Registration No. 148 on 30 May 2024).
Informed Consent Statement
Consent was obtained from the patient for the publication of the clinical data and images (with respect for their personal data).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Measles Cases Across Europe Continue to Surge, Putting Millions of Children at Risk. Available online: https://www.unicef.org/romania/press-releases/measles-cases-across-europe-continue-surge-putting-millions-children-risk (accessed on 14 October 2024).
- Factsheet About Measles. Available online: https://www.ecdc.europa.eu/en/measles/facts (accessed on 14 October 2024).
- Rujeola—Institutul Național de Sănătate Publică. Available online: https://insp.gov.ro/downloads/rujeola/ (accessed on 18 March 2025).
- Measles Immunity Gaps Among Children and Adolescents with HIV in Zambia Despite High Measles Vaccination and Antiretroviral Therapy Coverage—PMC. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10664789/ (accessed on 14 October 2024).
- Scott, S.; Moss, W.J.; Cousens, S.; Beeler, J.A.; Audet, S.A.; Mugala, N.; Quinn, T.C.; Griffin, D.E.; Cutts, F.T. The influence of HIV-1 exposure and infection on levels of passively acquired antibodies to measles virus in Zambian infants. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2007, 45, 1417–1424. [Google Scholar] [CrossRef] [PubMed]
- Moss, W.J.; Scott, S.; Mugala, N.; Ndhlovu, Z.; Beeler, J.A.; Audet, S.A.; Quinn, T.C.; Cousens, S.; Griffin, D.E.; Cutts, F.T.; et al. Immunogenicity of standard-titer measles vaccine in HIV-1-infected and uninfected Zambian children: An observational study. J. Infect. Dis. 2007, 196, 347–355. [Google Scholar] [PubMed]
- Centrul Național de Supraveghere şi Control al Bolilor Transmisibile—Calendarul National de Vaccinare. Available online: https://www.cnscbt.ro/index.php/calendarul-national-de-vaccinare (accessed on 18 March 2025).
- Measles: Clinical Manifestations, Diagnosis, Treatment, and Prevention. Available online: https://medilib.ir/uptodate/show/3021 (accessed on 14 October 2024).
- Crum-Cianflone, N.F.; Wallace, M.R. Vaccination in HIV-Infected Adults. AIDS Patient Care STDs 2014, 28, 397–410. [Google Scholar] [CrossRef] [PubMed]
- Dauby, N.; Martin, C.; Hainaut, M.; Grammens, T.; Van den Wijngaert, S.; Delforge, M.; Wit, S.D. Prevalence and risk factors of measles seronegativity in a cohort of HIV-positive subjects: A retrospective study. HIV Med. 2018, 19, 426–429. [Google Scholar] [CrossRef] [PubMed]
- Diana, N.E.; Feldman, C. Measles in adults: A comparison of hospitalised HIV-infected and HIV-uninfected patients. S. Afr. J. HIV Med. 2019, 20, 877. [Google Scholar]
- Sutcliffe, C.G.; Searle, K.; Matakala, H.K.; Greenman, M.; Rainwater-Lovett, K.; Thuma, P.E.; Moss, W.J. Measles and Rubella Seroprevalence Among HIV- Infected And Uninfected Zambian Youth. Pediatr. Infect. Dis. J. 2017, 36, 301–306. [Google Scholar] [PubMed]
- Haban, H.; Benchekroun, S.; Sadeq, M.; Tajounte, L.; Ahmed, H.J.; Benjouad, A.; Amzazi, S.; Oumzil, H.; Elharti, E. Seroprevalence of measles vaccine antibody response in vertically HIV-infected children, in Morocco. BMC Infect. Dis. 2018, 18, 680. [Google Scholar]
- Rearigh, L.; O’Neill, J.; Kubat, M.; Sayles, H.; Swindells, S.; Bares, S.H. Surprisingly Low Levels of Measles Immunity in Persons With HIV: A Seroprevalence Survey in a United States HIV Clinic. Open Forum Infect. Dis. 2020, 7, ofaa428. [Google Scholar] [CrossRef] [PubMed]
- de Moraes-Pinto, M.I. Interaction Between Pediatric HIV Infection and Measles. 2011. Available online: http://repositorio.unifesp.br/handle/11600/34323 (accessed on 27 October 2024).
- Lefebvre, M.; Secher, S.; Bouchez, S.; Vandamme, Y.-M.; Fialaire, P.; Leautez, S.; Brunet-Cartier, C.; Reliquet, V.; Gregoire, A.; Raffi, F.; et al. Measles seroprevalence in human immunodeficiency virus-infected adults born in the era of measles vaccination. AIDS Lond. Engl. 2022, 36, 1273–1278. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).