Abstract
Background. In orthopedics, the patients’ quality of life relative to the preoperative and postoperative phase is referred with a low impact compared to other branches of medicine. In this context, our interest focused on assessing the quality of life in patients with traumatic and non-traumatic coxarthrosis by longitudinally following the evolution of the patients. Materials and Methods. The well-established instrument Short Form Survey SF-36 was applied in a retrospective study, conducted on a cohort of 203 participants who underwent THA (Total Hip Arthroplasty). Statistical analysis was generated using GraphPad Prism (version 9.5.1). Results. In the pre-operative phase, physical functioning was more affected in participants with traumatic coxarthrosis, while fatigue was specific to nontraumatic coxarthrosis. Emotional well-being and social functioning were high in patients with traumatic coxarthrosis. One month after surgery, we recorded an increased physical functioning and improvement in the perception of the ability to exercise roles in non-traumatic group. Energy/vitality and general health and well-being were at high level in traumatic group, 1st month post-surgery, although pain was still frequent. Age was the sole strong independent predictor of postoperative physical functioning in the traumatic group, while in the non-traumatic group, we identified gender, age, symptoms and type of prosthesis as strong predictors of postoperative physical functioning. The overall results related to daily living activities indicated that the traumatic group displayed more favorable post-surgery evolution and higher autonomy compared to the non-traumatic one. Conclusions. We conclude that SF-36 questionnaire is a specific, useful and inexpensive tool for evaluating the outcomes of orthopedic treatment and patients’ evolution after arthroplasty, especially in terms of functional outcome scores relative to coxarthrosis etiology.
Introduction
In the last decades, the interest of the scientific community has focused on the quality of life of people in general and in particular of people who have passed through medical interventions. A well- established instrument in the international medical community is the Short Form Survey - SF-36 [1,2,3,4], being one of the most popular methods of measuring health status that evaluates the quality of life, the severity of the disease and helps to discriminate between different ailments chronic. The concepts covered by the SF-36 from the health area are: physical functioning, bodily pain, role limitations due to physical health problems, role limitations due to personal or emotional problems, emotional well-being, social functioning, energy/fatigue and general health perception [5]. The literature frequently reports that a low SF-36 score is associated with a high degree of disability, therefore, a high score indicates high functioning [6,7,8]. Nowadays, arthroplasty has shown positive outcomes and significant improvement in the quality of life, particularly in total hip replacement (THR) which is performed aiming pain relief and restoration of hip function [9,10]. On the other hand, in terms of postoperative complications, THR may have adverse effects on the quality of life, while reporting of complications after total hip arthroplasty (THA) is not standardized or validated [11,12]. According to Brokelman et al. [13], patient satisfaction is a concept based on a combination of subjective and social-cultural feelings with cognitive, behavioral, and psychological influences, being an important metric in order to assess subjective outcomes during the follow-up of arthroplasty procedures [14,15,16]. However, it has been reported that patients undergoing THA for traumatic reason have been shown to have poorer functional outcome scores [17]. The number and type of co-morbidities and a low preoperative quality of life score are the well-known negative predictors [18]. We chose to apply the SF-36 in order to assess the quality of life of pre- and post-operative patients because it is a self-administered questionnaire with a short administration time (approximately 12 minutes). This questionnaire investigates the state of physical, mental and social health, being divided into 8 subscales: physical functioning, mental health, social functioning, general health perceptions, limitations due to emotional and physical problems, bodily pain and vitality. In orthopedics, all these subfields are important to evaluate the current state of the patient and follow the postoperative evolution over time. Another advantage of using the SF-36 is for therapists to give the best recommendations for a quick and efficient recovery: physical exercises, professional adaptation advice, pain treatment or psychological evaluation [19,20,21]. Particularly in orthopedics, the patients’ quality of life relative to the preoperative and postoperative phase is referred with a low frequency compared to other branches of medicine (such as neurology, oncology). In this context, our interest focused on assessing the quality of life and daily living activities (ADL) of patients with traumatic and non-traumatic coxarthrosis by longitudinally following (between the preoperative and postoperative phase) the evolution of the patients. The literature review does not indicate studies that have adequately investigated this issue of major importance in recovery. ADL are essential routine tasks that most healthy people can perform without assistance. The inability to perform essential activities of daily living can lead to unsafe conditions and a decrease in quality of life. The postoperative care team should be aware of the importance of ADL assessment to ensure that patients who need assistance can receive it.
In this context, our objective was to evaluate the quality of life in patients with coxarthrosis in the pre- and post- surgical phase, through the Short Form Survey SF-36, the results being assessed in relation to coxarthrosis etiology, gender, age, diagnostic, symptoms, type of prosthesis and type of surgical intervention in order to find the best predictors contributing to improvement in patient's functionality and improved quality of life.
Materials and Methods
Study Design
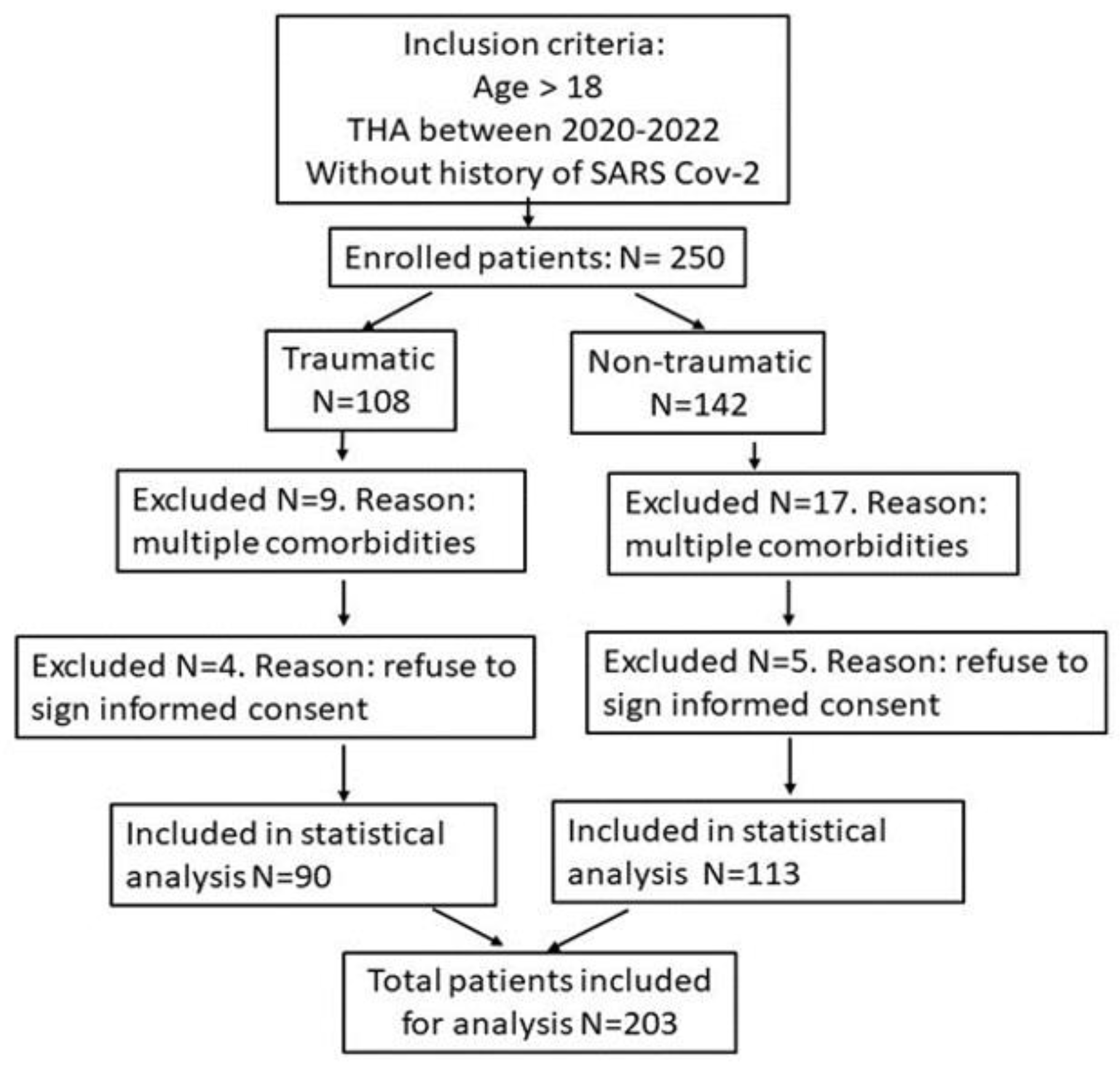
This study was implemented between September 2020 and September 2022, comprising a total number of 203 participants, aged between 18 and 90 years (m=58.44; SD=17.41), of which 92 women (45.3%) and 111 men (54.7%), being conducted in the Orthopedics Department of Emergency County Clinical Hospital, Oradea, Romania. A total of 66 participants were investigated in 2020 (32.5%), 101 participants in 2021 (49.8%), and 36 participants in 2022 (17.7%). Initially, 250 patients were enrolled in the study, based on inclusion criteria: adults who underwent THA, non-smokers, without history of SARS-CoV-2 infection. Exclusion criteria: patients with multiple comorbidities (including patients with a history of malignant tumors, or organ failure) and refusal to participate in the study and to sign the informed consent. The initial selection of subjects followed the formation of two groups: traumatic and non-traumatic, according to coxarthrosis etiology. The flow chart containing the study design is presented in Figure 1. The participants were asked to complete the 36-item Short-Form (SF-36) Health Survey (supplementary material) and the data were longitudinally analyzed between the preoperative (T1) and postoperative (T2) phases, assessing the dimensions of the quality of life according to the mode of coxarthrosis cooccurrence (traumatic or nontraumatic).
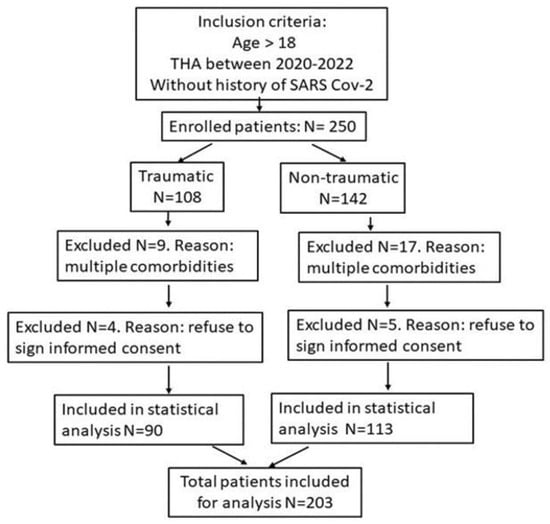
Figure 1.
Flow chart of the study, inclusion and exclusion criteria.
Statistical analysis
The experimental design is of 1 x 2 type. Descriptive statistics was performed including means, standard deviations and tests of statistical significance by applying Mann Whitney test for independent samples in the preoperative (T1) and postoperative (T2) phase, while the dependent variable was represented by the dimensions of quality of life. The comparison of longitudinal changes between the preoperative (T1) and postoperative (T2) phases regarding the oscillations in terms of quality of life was performed by Wilcoxon matched-pairs test for paired samples with respect to traumatic or nontraumatic occurrence of coxarthrosis. Depending on the etiology, the results were separately analyzed considering the independent variables represented by symptoms, type of prosthesis, surgical procedures, while the dependent variable was considered the postoperative evolution in terms of physical functioning in T2 phase, data being compared by applying Chi-square test and multiple linear regression analysis between clinical variables and postoperative physical functioning. Statistical analysis was generated using GraphPad Prism (version 9.5.1).
Ethical approval
The study was approved by the Institutional Review Board and Ethical Council of the Emergency County Clinical Hospital, Oradea, Bihor - Romania (no. 1267/14.01.2022 and 1087/13.01.2022). The research was conducted in compliance with the Declaration of the World Medical Association of Helsinki. Participation in the study was voluntary and written informed consent was obtained from all participants for accurate collection of information and data processing.
Results
Preoperative phase
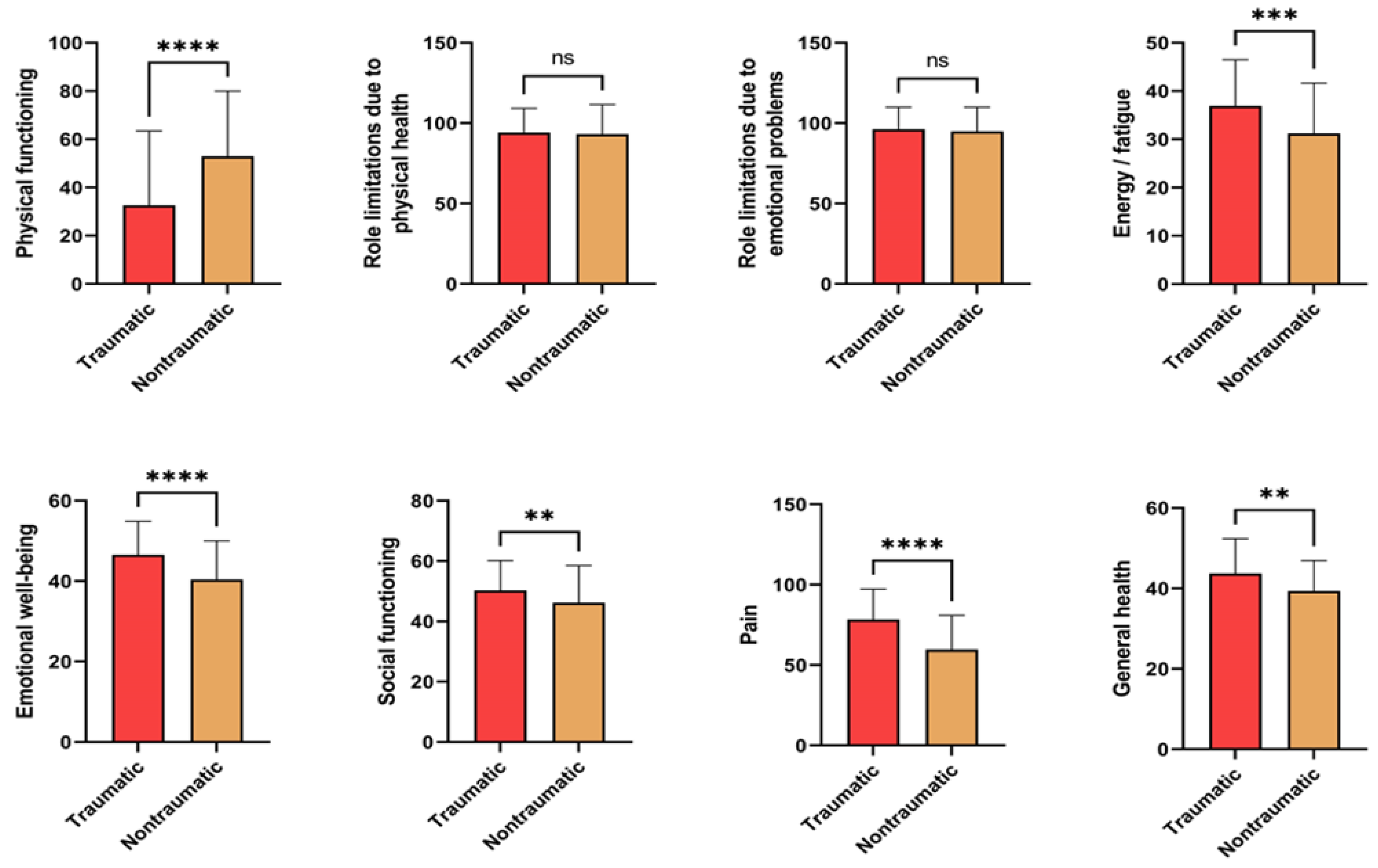
The results of Mann Whitney test comparisons (for independent samples) in the preoperative phase are presented in Figure 2, statistically significant differences being found in this study and marked. Thus, we noticed that physical functioning was higher in patients with non- traumatic coxarthrosis compared to traumatic coxarthrosis. In the preoperative phase, limitations of social roles due to physical health as well as due to emotional problems did not indicate differences with respect to the coxarthrosis etiology, while the energy / fatigue ratio was significantly higher in the traumatic group. Emotional well-being was significantly higher in the traumatic group compared to non-traumatic one, which leads to a better social functioning of these participants, who frequently do not have the same medical history as non-traumatic ones. Pain is a strong signal of decreased functionality and consequently, decreased quality of life. In our study, patients with traumatic coxarthrosis revealed higher frequencies of pain and discomfort compared to nontraumatic ones. The general health subscale also differs between the two groups of participants: participants in the traumatic group considered to have a generally better health status compared to participants from the non- traumatic group.
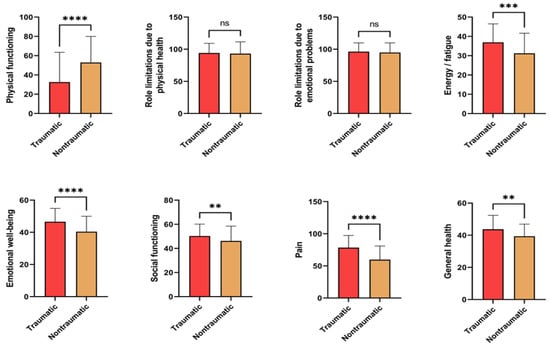
Figure 2.
Pre-operative test comparisons of scales: quality of life and disease severity according to the etiology of coxarthrosis (traumatic versus nontraumatic). Data are presented as the average scores ± SD and compared using Mann Whitney test; ns, non-significant, **P< 0.01, ***P< 0.001, ****P< 0.0001.
Postoperative phase
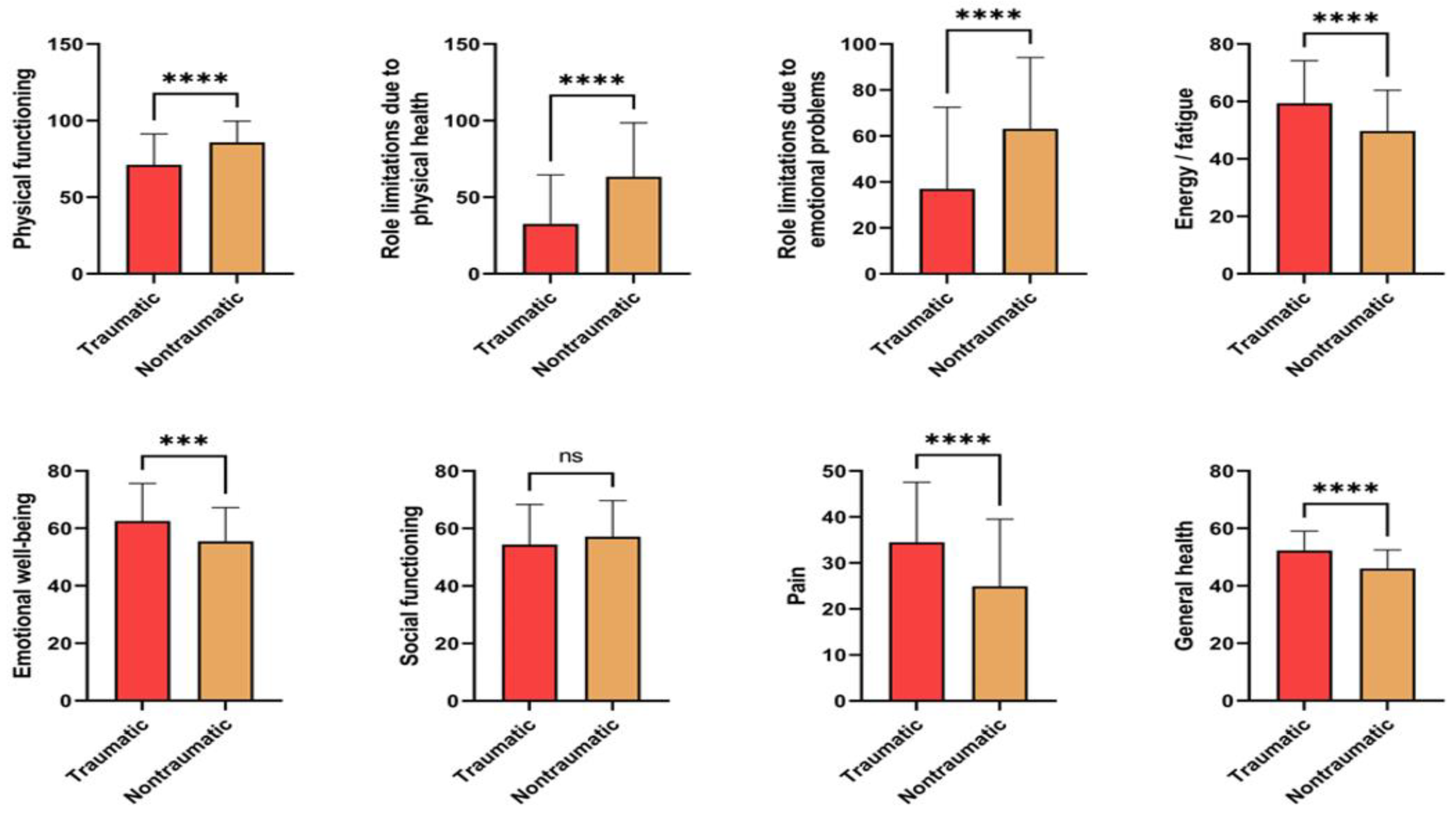
The results of the subscales were compared with respect to coxarthrosis occurrence (traumatic versus non- traumatic) in order to identify changes regarding the quality of life in patients undergoing THA. In the post- operative phase (Figure 3), we noticed higher physical functioning of the participants with non-traumatic coxarthrosis as well as an improvement in the perception of the ability to exercise roles, being supported by their physical and emotional health. Similar to pre-operative phase, the energy subscale indicates higher means of participants with traumatic coxarthrosis compared to nontraumatic ones, as well as the emotional well-being scales. Social functioning indicated better scores in non- traumatic group, while the pain subscale and general health status indicates a behavior similar to the preoperative stage, with lower averages recorded in the non-traumatic group.
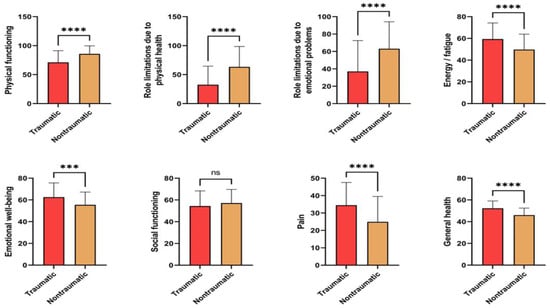
Figure 3.
Post-operative test comparisons of scales: quality of life and disease severity according to the etiology of coxarthrosis (traumatic versus nontraumatic). Data are presented as the average scores ± SD and compared using Mann Whitney test; ns, non-significant, ***P< 0.001, ****P< 0.0001.
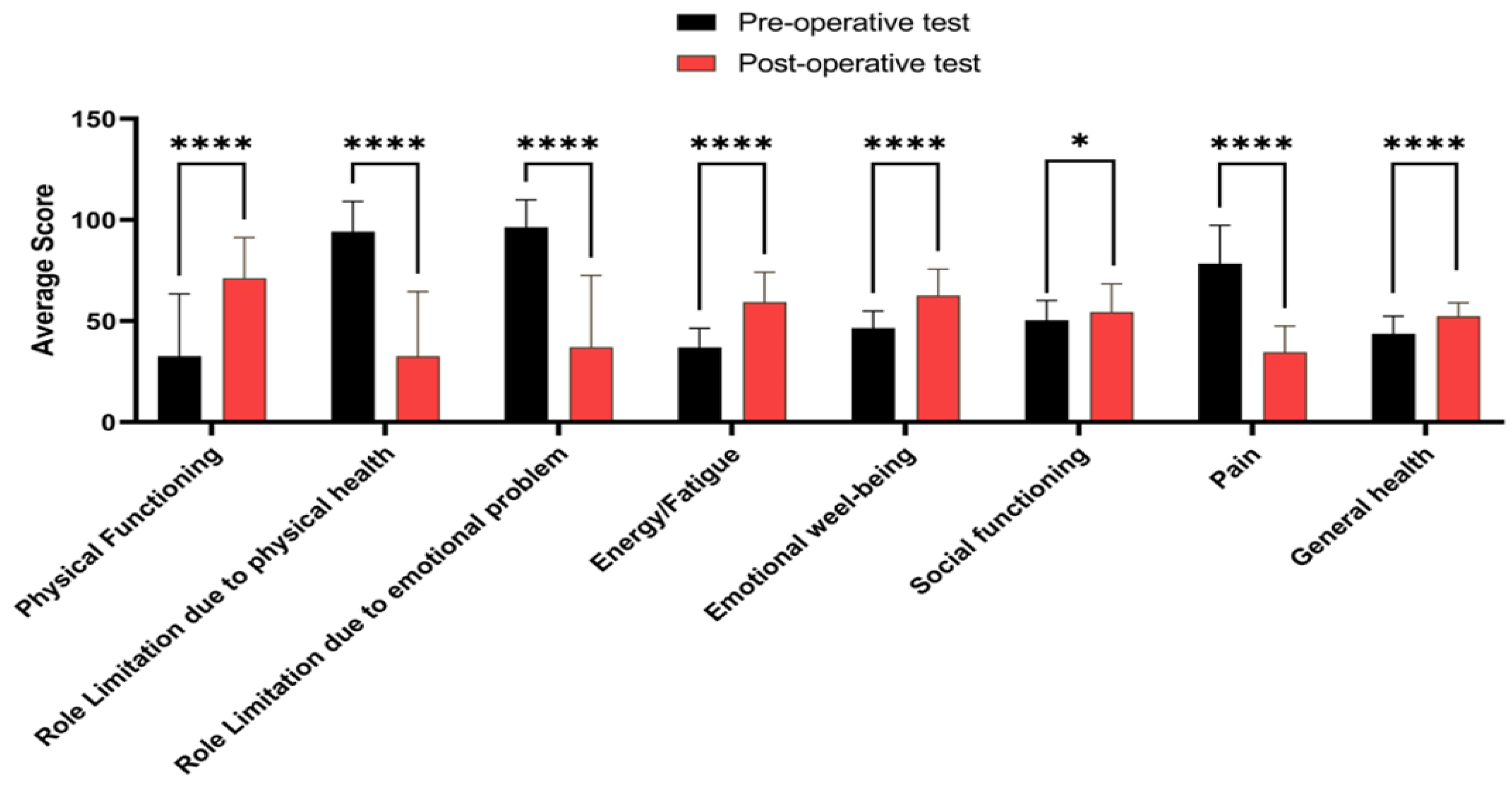
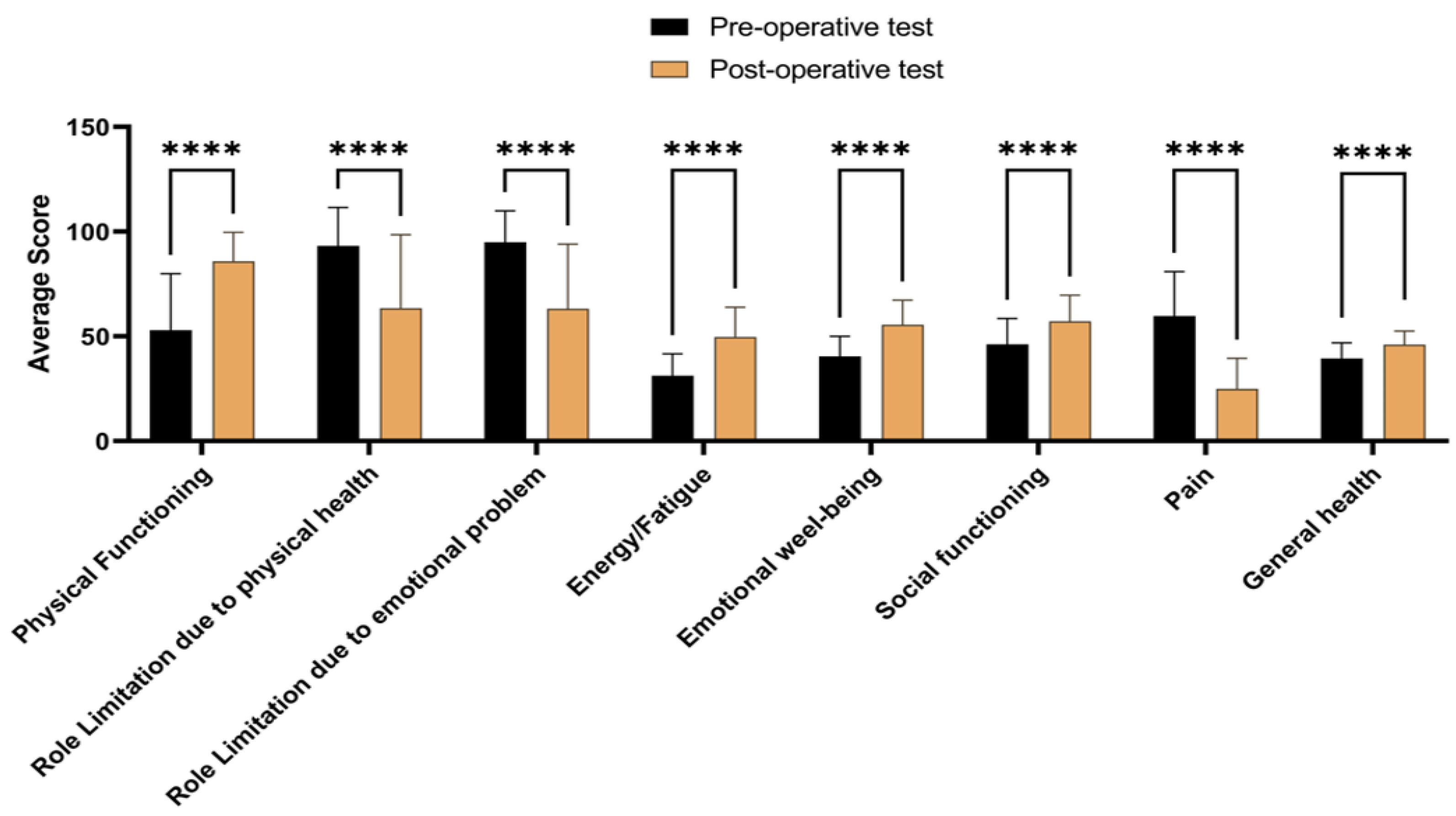
Preoperative versus Postoperative phase
In order to highlight the oscillations in terms of the perception of the quality of life between pre- and post- operative stages, Wilcoxon matched-pair was applied, regardless the etiology of coxarthrosis. In Figure 4, the longitudinal comparisons (pre- and post-surgery) of the quality of life’ scales within the traumatic group are presented. We noticed post operative (T2) higher values in terms of physical functioning, and lower values of role limitation due to physical health or due to emotional problems. Also, when comparing T2 and T1 stages, an increase in energy, emotional well-being, and social functioning can be observed, while a lower level of pain was noticed. Overall, an improvement in general health was recorded in patients undergoing total hip arthroplasty after traumatic coxarthrosis.
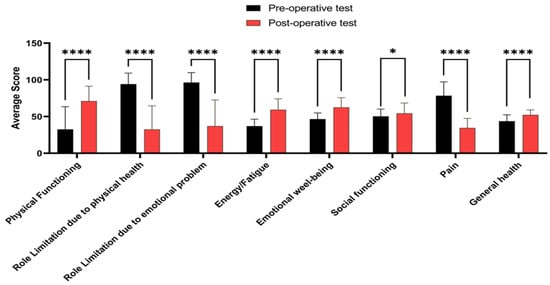
Figure 4.
Longitudinal comparisons (pretest - posttest) of the quality of life’ dimensions and disease sever-ity in patients with traumatic coxarthrosis. Data are presented as the mean ± SD and compared using Wilcoxon matched- pairs test; *P< 0.05, ****P< 0.0001.
Similar longitudinal comparisons were analyzed for the patients from nontraumatic group, the data being presented in Figure 5. Lower values were recorded postoperatively (T2) in terms of role limitation due to physical health and role limitation due to emotional problems. On the other hand, an increase in physical functioning, energy, emotional well-being and social functioning values were noticed. Also, the post-operative phase (T2) highlighted a decrease level of pain and an improvement in general health status.
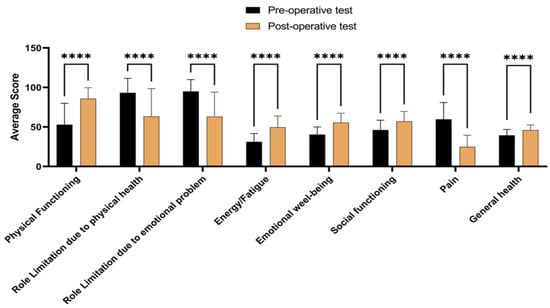
Figure 5.
Longitudinal comparisons (pretest - posttest) of quality of life’ dimensions and disease severity in patients with non-traumatic coxarthrosis. Data are presented as the mean ± SD and compared using Wilcoxon matched-pairs test; ****P< 0.0001
Although the longitudinal comparisons are relevant in terms of the dynamic of changes in quality of life and well- being, they do not indicate which are the determinant factors contributing to improved physical functioning in the postoperative phase (T2). For this purpose, the analysis by multiple regression model was applied to find the best predictors contributing to improvement in patient's functionality and improved quality of life in our study. In Table 1 are presented the details of the results obtained of the multiple regression analysis performed between clinical variables and postoperative physical functioning for our study sample.

Table 1.
Multiple linear regression analysis between clinical variables and postoperative physical functioning
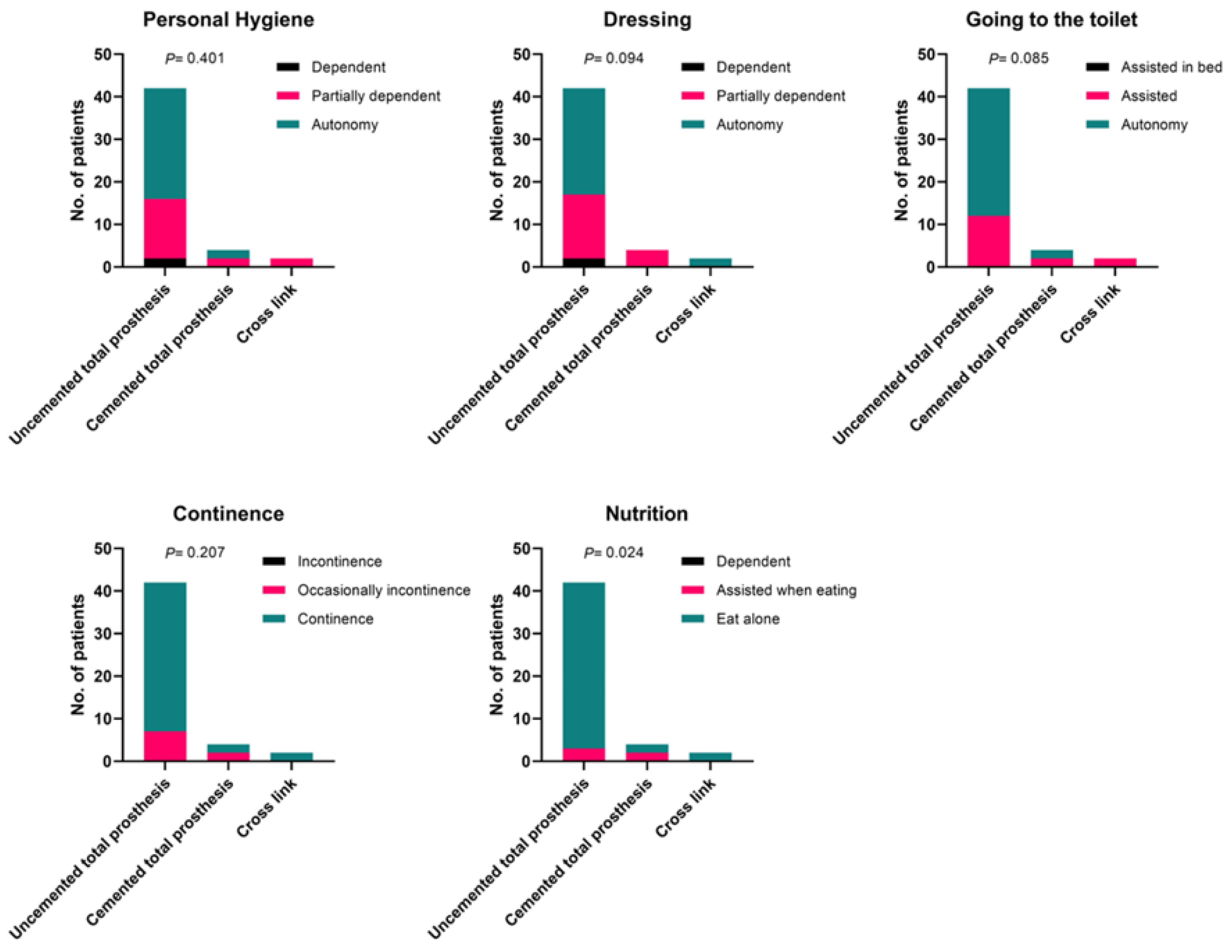
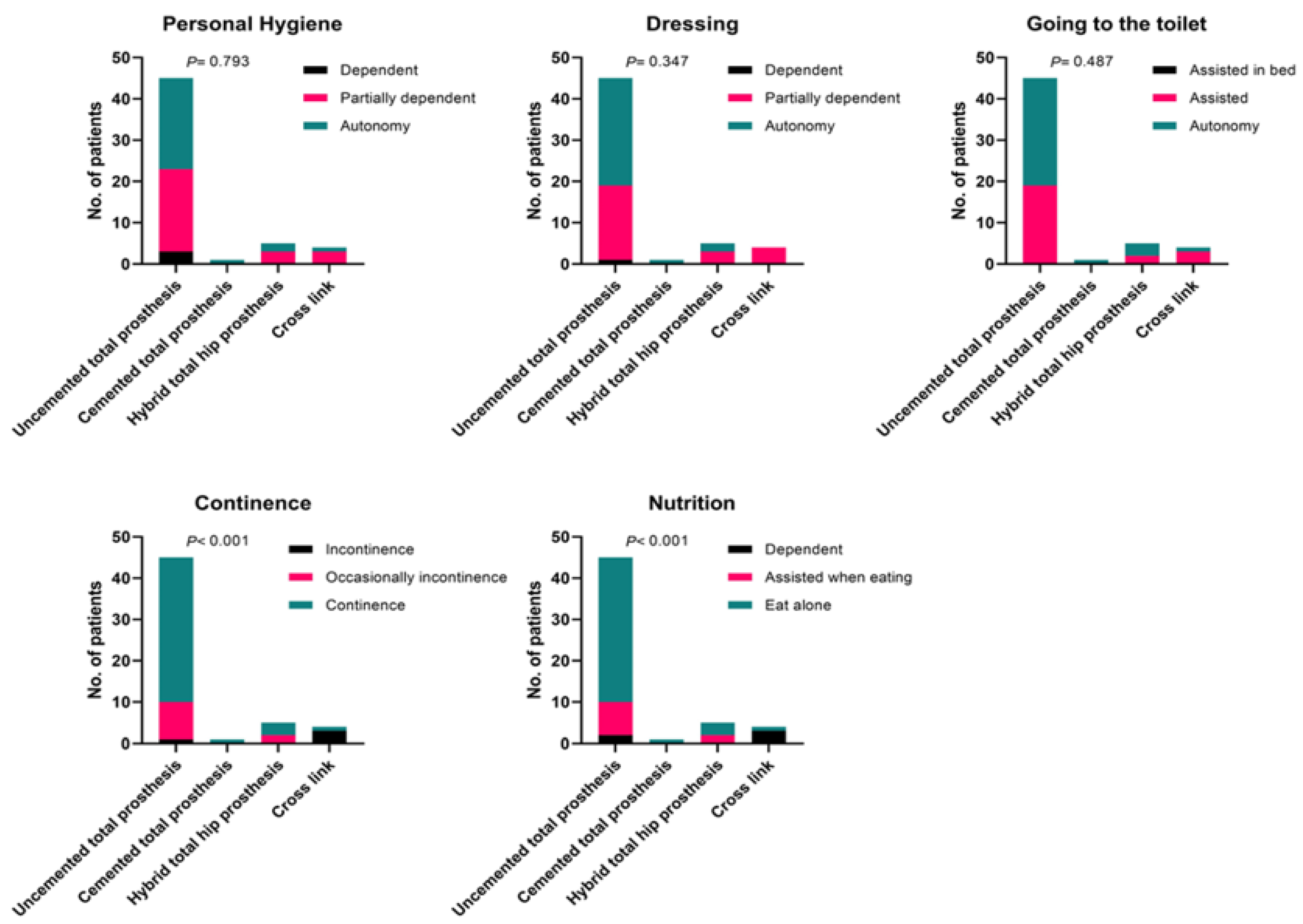
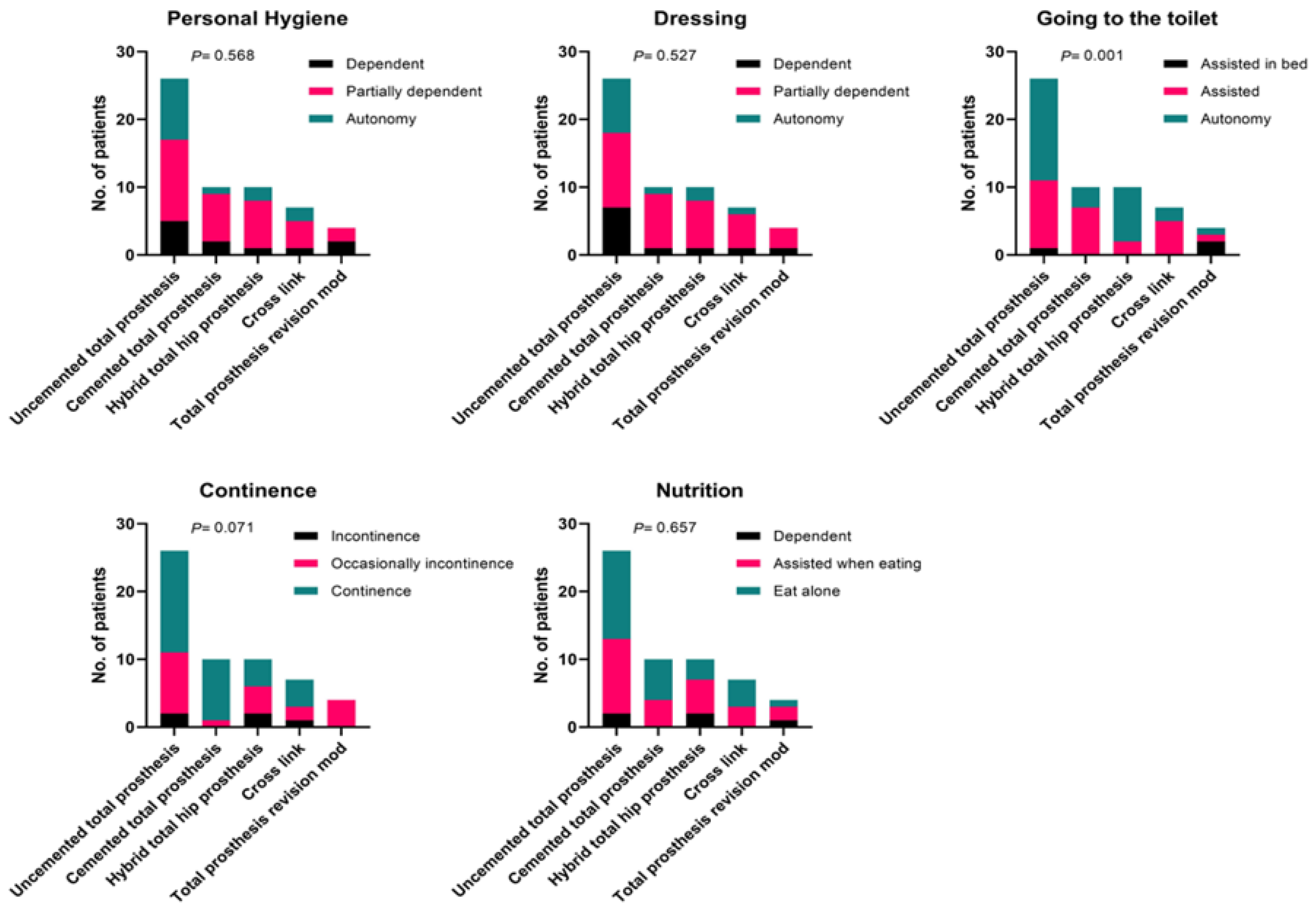
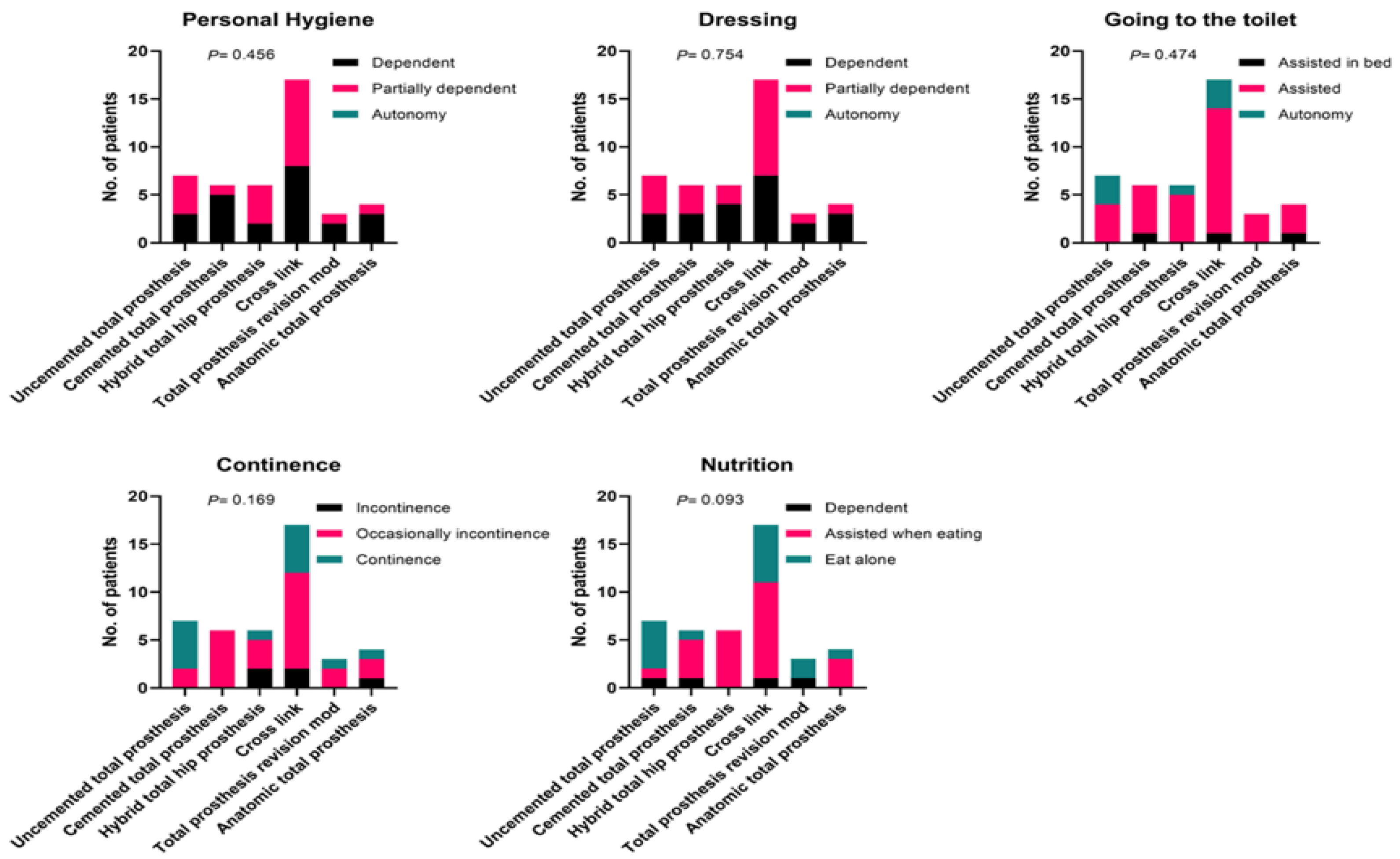
The relationship between daily living activities and type of prosthesis
We were interested in analyzing (depending on the initial diagnosis) the postoperative effect of the type of prosthesis on ADL, emphasizing aspects related to self- care. In Figures 6, 7, 8 and 9 are presented the effect of the type of prosthesis on postoperative daily living activities according to diagnosis, respectively left coxarthrosis operated (LCO, Figure 6), right coxarthrosis operated (RCO, Figure 7), bilateral coxarthrosis operated unilaterally (BCOU, Figure 8) and bilateral coxarthrosis operated bilaterally (BCOB, Figure 9). In terms of performing personal hygiene, we noticed high percentage of patients diagnosed with BCOB being totally dependent on other person, or partially dependent, regardless the type of prosthesis. The best scores for autonomy in terms of personal hygiene was recorded for the patients who benefited from uncemented total prosthesis diagnosed with LCO and RCO, while the patients with BCOU were preponderant partly dependent. However, the values of the frequencies regarding the need for partial assistance or even dependence in performing body hygiene are progressively increasing. The results indicate that, regardless the diagnostics, each category of patients revealed a partial dependence on another person in order to perform body hygiene activities.
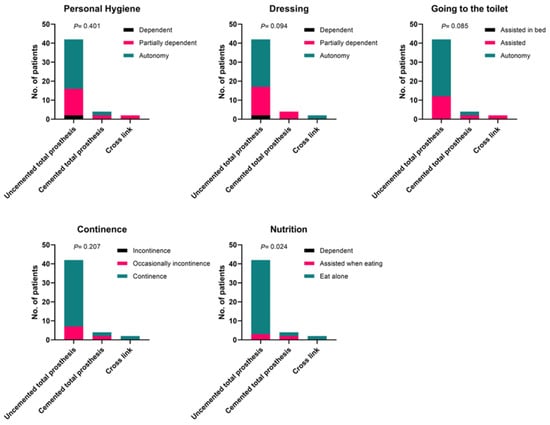
Figure 6.
Effect of the type of prosthesis on postoperative daily living activities (ADL) according to diagnosis with left coxarthrosis operated on (LCO). Data were compared using Chi-square test.
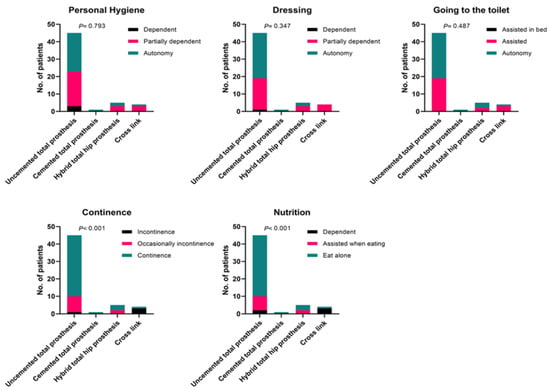
Figure 7.
Effect of the type of prosthesis on postoperative daily living activities (ADL) according to diagnosis with right coxarthrosis operated on. Data were compared using Chi-square test.
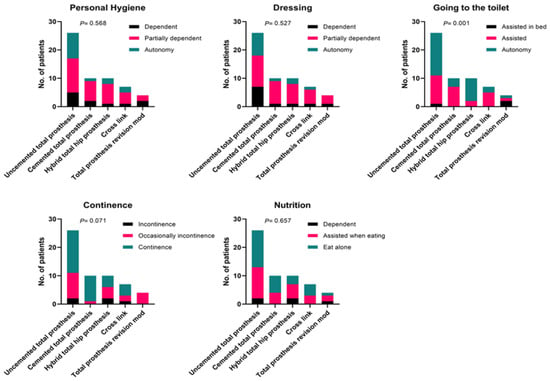
Figure 8.
Effect of the type of prosthesis on postoperative daily living activities (ADL) according to diagnosis with bi-lateral coxarthrosis operated unilaterally (BCOU). Data were compared using Chi-square test.
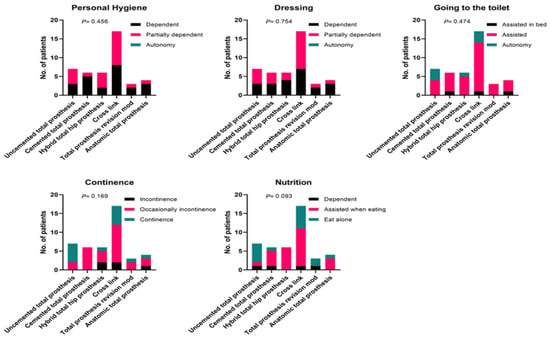
Figure 9.
Effect of the type of prosthesis on postoperative daily living activities (ADL) according to diagnosis with bi-lateral coxarthrosis operated bilaterally (BCOB). Data were compared using Chi-square test.
Regarding the autonomy in terms of ability to dress oneself, we did not record statistically significant coefficients with respect to the diagnosis, but autonomy decreased in the case of BCOU, while in the case of BCOB, higher frequencies in dependence on others or assistance for help was noticed, for all types of prosthesis. The patients diagnosed with LCO and RCO presented similar behavior in terms of dressing oneself, suggesting a better autonomy for uncemented total prosthesis, compared to cemented ones or crosslink. Significant differences were noted when comparing the four types of prostheses in relation to assistance in going to the toilet. The patients undergoing uncemented total prosthesis presented rather autonomy in the case of RCO or LCO and BCOU. A very different behavior was noticed for the patients diagnosed with BCOB, as they required assistance in higher percent, especially those with cross link intervention. In terms of continence, the data suggest that people diagnosed with right respectively left coxarthrosis operated, who benefited from uncemented total prosthesis are mostly continent. Significant differences between the four types of prosthesis are noted for BCOB (as incontinence occurred mostly in the cases with hybrid total prosthesis and cross link) and BCOU (with most incontinence for the patients with uncemented total prosthesis and hybrid prosthesis). Regarding the results in terms of ability of self-feeding, we noticed large differences for LCO or RCO suggesting the ability of patients with uncemented total prostheses to feed themselves. The observed frequencies are relatively equal to the theoretical ones in people with BCOU. On contrary, for BCOB we noticed a significant increased need for help in terms of ability of self-feeding for the patients with cross link and hybrid total hip replacement.
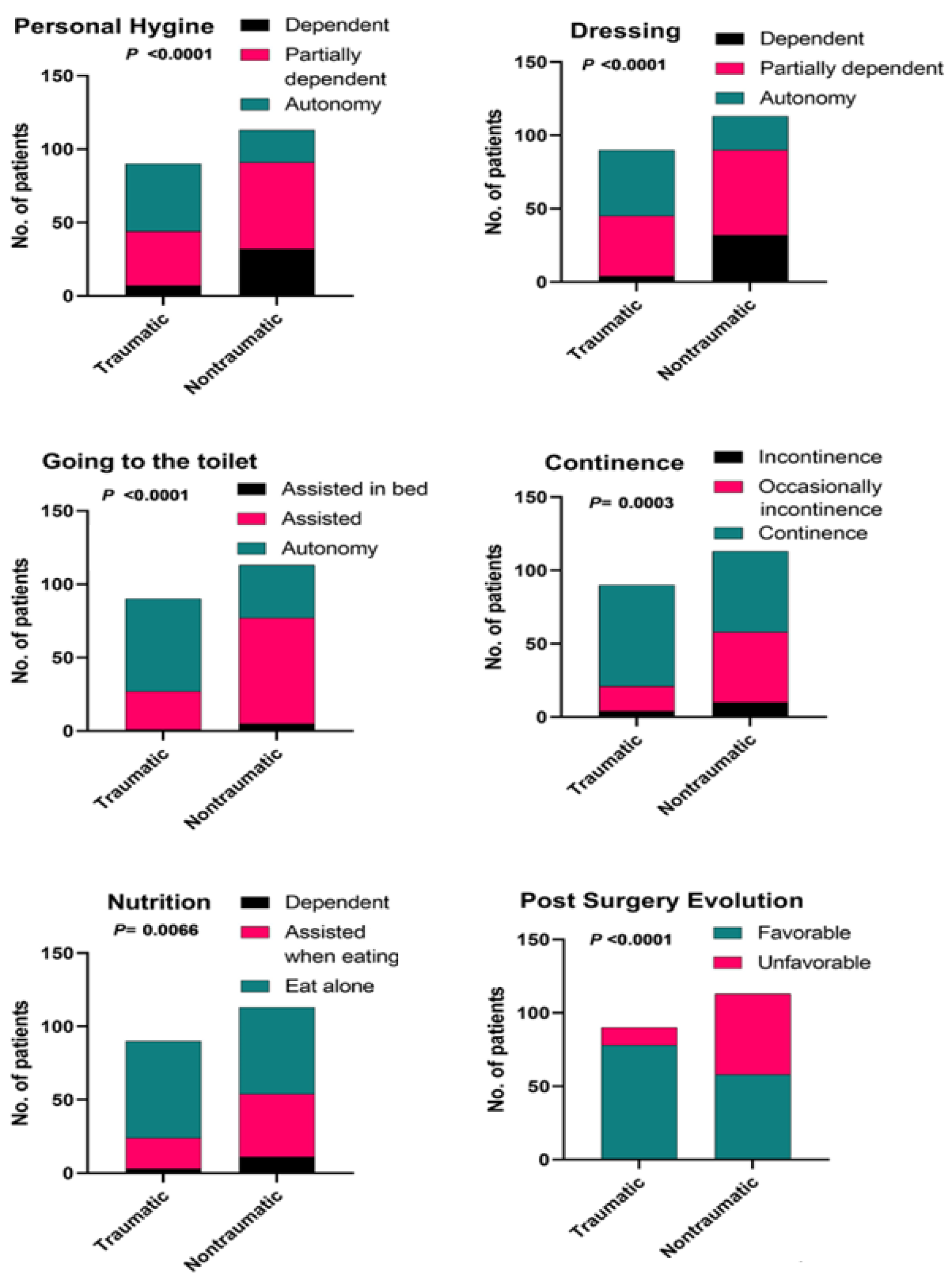
We also evaluated the effect of mode of production (traumatic vs. nontraumatic) on postoperative daily living activities (ADL) and post-surgery evolution. Figure 10 illustrates a significant correlation between the mode of production and postoperative daily living activities (ADL) and the subsequent progress after surgery.
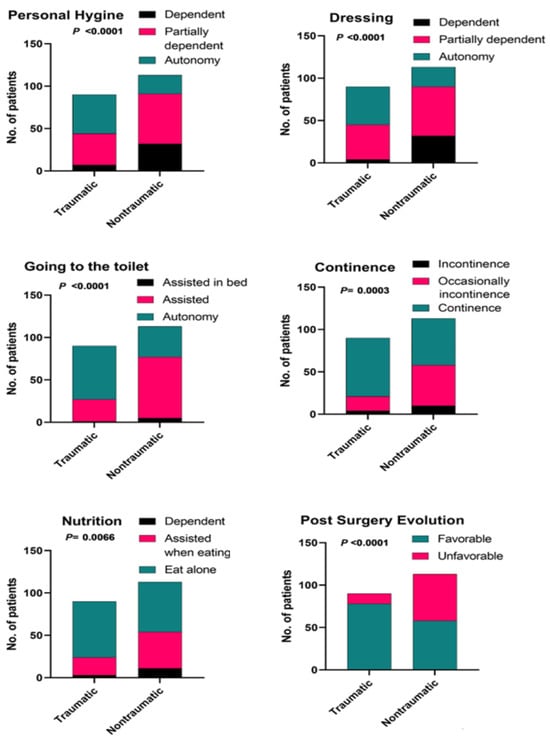
Figure 10.
Effect of mode of production (traumatic vs. nontraumatic) on postoperative daily living activities (ADL) and post-surgery evolution. Data were compared using Chi-square test.
Discussions
Coxarthrosis is a condition with a long-term evolution, the symptoms evolve over time and increase in frequency, becoming disabling for the patients in general and for older patients in particular [22,23,24]. Van Dijk et al. (2008) and Reeuwijk et al. (2010) emphasized the coexistence of coxarthrosis with a set of comorbidities, among which they highlighted HTN or diabetes. Associated diseases alter pain perception while others increase disability, and others affect both [25,26]. Total hip replacement (THR) aims mainly to improve quality of life via restoration of hip function and pain relief. The number of THA is being increased gradually driven by an aging population and higher rates of coxarthrosis diagnosis. Comparing to other medical branches, the orthopedic literature comprises only few works describing the evaluation of health-related quality of life in pre- and post -operative phase, after total hip arthroplasty [27,28,29].
Our study aimed to compare the outcomes in terms of quality of life of patients who had undergone THA at our County Hospital, in relation to coxarthrosis etiology (traumatic or non-traumatic), using the SF-36 test. A scoring algorithm was used to convert the raw scores into the eight dimensions of health status: physical functioning; physical role limitations; bodily pain; general health perceptions; energy/vitality; social functioning; emotional role limitations and mental health.
Our results indicated that physical functioning is more affected in participants with traumatic coxarthrosis, while fatigue is specific to nontraumatic coxarthrosis. On the other hand, emotional well-being and social functioning are high in patients with traumatic coxarthrosis, probably because they have not experienced emotional erosion and alienation compared to people with traumatic coxarthrosis.
Pain is a strong signal of decreased functionality and decreased quality of life, therefore traumatic participants report with a high frequency pain, but a good general state of health, as suggested also by Shiba et al. [30]. One month after surgery, we recorded an increase in physical functioning and improved perception of the ability to exercise roles in participants with nontraumatic coxarthrosis. Energy and well-being were at higher level in traumatic group, 1st month post-surgery, although pain was still predominant. A better general health was more evident in traumatic participants, probably as a result of restructuring the perception of health and illness. The evaluated symptoms in the preoperative phase, shown a significant influence on physical functioning parameters recorded in the postoperative phase, in the traumatic group. On the other hand, surgical procedures lead to an increase in postoperative functionality, a relationship mediated by the type of prosthesis, especially in the case of uncemented total arthroplasty and revision total arthroplasty.
The multiple regression model was conducted to determine the key predictors that contribute to the improvement in patients' functionality and enhanced quality of life. Within the context of the current study, several independent variables were examined for their impact on physical functioning during the postoperative phase. These variables included gender, age, diagnostic factors, symptoms, type of prosthesis, and surgical procedures. In the traumatic group, the regression model accounted for 43.6% of the variance in physical functioning during the postoperative phase. The model revealed that age was the sole strong independent predictor of postoperative physical functioning in the traumatic group. Conversely, in the non-traumatic group, the regression model explained 55.6% of the variance in physical functioning during the postoperative phase. It identified gender, age, symptoms, and type of prosthesis as strong predictors of postoperative physical functioning in the non-traumatic group.
The relationship between daily living activities and type of prosthesis was also evaluated, highlighting the aspects related to self-care. The term activities of daily living (ADL) was proposed by Sidney Katz in 1950, being used as an indicator of a person's functional status [31,32]. Inability to perform ADLs results in dependence on other people and/or mechanical devices. The inability to perform essential activities of daily living can lead to un-safe conditions and consequently, a low quality of life [33]. Evaluating a person's ADLs is of crucial importance, being predictive factors of the need for alter-native living arrangements, hospitalization, and use of home care [32,34]. The outcome of a treatment program can also be assessed by reviewing a patient's ADLs [35]. Particularly, the autonomy in terms of ability to go to the toilet alone is relevant for people in general and in particular for patients with coxarthrosis, having an important impact from psychological and social point of view.
Assessing the ADLs and evaluating the patient's routines, may help physicians and nursing staff to correctly monitor the patient's condition, to establish treatment plan and intervention appropriately. Edemekong et al. [32] consider that a specialist should address a patient's general medical condition when determining the level of achievement of the patient's functional capacities that otherwise ensure independent living and personal care. Our data indicates that traumatic patients exhibited a higher frequency of independence in terms of personal hygiene, dressing, and going to the toileting, along with a greater occurrence of continence and the ability to eat unassisted, compared to non-traumatic patients. Furthermore, the traumatic group displayed more favorable post-surgery evolution compared to the non-traumatic group.
To the best of our knowledge, this is the first study conducted in Romania, dealing with the complex aspects regarding the influence of coxarthrosis etiology on the patients’ quality of life, along with complementary evaluation of the relationship between daily living activities and type of prosthesis or surgical procedures. Worldwide, few papers were devoted to evaluation of health-related quality of life before and after total hip arthroplasty, with short or long-term follow-up [36,37,38,39,40], but none of them considered the etiology of coxarthrosis.
Our study has some limitations. Due to its observational and retrospective character, it lacks reliable baseline data and a control group. Also, we were not able to extend the follow up period, because after more than one month, most of the subjects lost their interest to participate in the study, although multiple attempts were made to trace all the patients for long follow-up evaluation. Finally, another limitation was the possible influence of COVID- 19 pandemic restrictions in terms of length of time on the waiting list for THR surgery, which might have influenced the pre-operative symptoms. It is well known that during the COVID-19 pandemic, all non-urgent surgeries were suspended.
Conclusions
Within the limitation of our study, we conclude that the Short Form 36 Health Survey Questionnaire (SF-36) is a useful tool in order to determine variations in health status and to assess the effectiveness of THA interventions related to coxarthrosis etiology. The multiple regression model revealed that age was the sole strong independent predictor of postoperative physical functioning in the traumatic group, while in the non-traumatic one, it identified gender, age, symptoms and type of prosthesis as strong predictors of postoperative physical functioning. The overall results indicated that the traumatic group displayed more favorable post-surgery evolution and higher autonomy compared to the non-traumatic one.
Contributions
Conceptualization, M.B., F.V.M. and S.C.; methodology, C.T.H., M.B., F.V.M. and A.M.A.; software, A.M.A.; validation, A.M.A. and M.B.; investigation, M.B. and C.T.H.; data curation, A.M.A. and F.V.M.; writing— original draft preparation, M.B and F.V.M.; writing— review and editing, S.C., A.M.A., F.V.M. visualization, A.M.A.; supervision, S.C.; project administration, M.B.; funding acquisition, M.B. and C.H. All authors have read and agreed to the published version of the manuscript.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript. Informed consent was obtained from all subjects involved in the study. The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board and Ethical Council of the Emergency County Clinical Hospital, Oradea, Bihor - Romania (no. 1267/14.01.2022 and 1087/13.01.2022).
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
Funding
This research was funded by University of Oradea, Romania.
References
- Burholt V, Nash P. Short Form 36 (SF-36) Health Survey Questionnaire: normative data for Wales. J Public Health (Oxf). 2011, 33, 587–603. [Google Scholar] [CrossRef]
- Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992, 305, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Barnett, A. SF-36 Health Survey. In: Michalos, A.C. (eds) Encyclopedia of Quality of Life and Well-Being Research. Springer, Dordrecht, 2014. [CrossRef]
- Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet. 2012, 380, 1768–1777. [Google Scholar] [CrossRef]
- Demiral Y, Ergor G, Unal B, et al. Normative data and discriminative properties of short form 36 (SF-36) in Turkish urban population. BMC Public Health. 2006, 6, 247. [Google Scholar] [CrossRef]
- McHorney CA, Ware JE Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994, 32, 40–66. [Google Scholar] [CrossRef]
- Abu-Awwad A, Tudoran C, Patrascu JM Jr, et al. Unexpected Repercussions of the COVID-19 Pandemic on Total Hip Arthroplasty with Cemented Hip Prosthesis versus Cementless Implants. Materials (Basel). 2023, 16, 1640. [Google Scholar] [CrossRef]
- Ware JE, Gandek B. The SF-36 Health Survey: Development and use in mental health research and the IQOLA Project. Int J Ment Health. 1994, 23, 49–73. [Google Scholar]
- Cavalu S, Simon V. Microstructure and bioactivity of acrylic bone cements for prosthetic surgery. J Optoelectron Adv Mater. 2006, 8, 1520–1523. [Google Scholar]
- Cavalu S, Simon V. Proteins adsorption to orthopaedic biomaterials: Vibrational spectroscopy evidence. J Optoelectron Adv Mater. 2007, 9, 3297. [Google Scholar]
- Healy WL, Iorio R, Clair AJ, Pellegrini VD, Della Valle CJ, Berend KR. Complications of Total Hip Arthroplasty: Standardized List, Definitions, and Stratification Developed by The Hip Society. Clin Orthop Relat Res. 2016, 474, 357–364. [Google Scholar] [CrossRef]
- Vicaş RM, Bodog FD, Fugaru FO, et al. Histopathological and immunohistochemical aspects of bone tissue in aseptic necrosis of the femoral head. Rom J Morphol Embryol. 2020, 61, 1249–1258. [Google Scholar] [CrossRef]
- Brokelman RB, Haverkamp D, van Loon C, Hol A, van Kampen A, Veth R. The validation of the visual analogue scale for patient satisfaction after total hip arthroplasty. Eur Orthop Traumatol. 2012, 3, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Voiță-Mekeres F, Buhaș CL, Mekeres GM, et al. Mekeres' Psychosocial Internalization Scale: A Scale for the Evaluation of Aesthetic Prejudice in Victims of Accidents and Violence. Healthcare (Basel). 2021, 9, 1440. [Google Scholar] [CrossRef]
- Mekeres GM, Voiţă-Mekereş F, Tudoran C, et al. Predictors for Estimating Scars' Internalization in Victims with Post-Traumatic Scars versus Patients with Postsurgical Scars. Healthcare (Basel). 2022, 10, 550. [Google Scholar] [CrossRef]
- Mekereș GM, Buhaș CL, Tudoran C, et al. The practical utility of psychometric scales for the assessment of the impact of posttraumatic scars on mental health. Front Public Health. 2023, 11, 1103714. [Google Scholar] [CrossRef]
- Aprato A, Massè A, Caranzano F, et al. Patient- Perceived Quality of Life after Total Hip Arthroplasty: Elective versus Traumatological Surgery. ISRN Orthop. 2011, 2011, 910392. [Google Scholar] [CrossRef]
- Canovas F, Dagneaux L. Quality of life after total knee arthroplasty. Orthop Traumatol Surg Res. 2018, 104, S41–S46. [Google Scholar] [CrossRef]
- Vosoughi AR, Kordi Yoosefinejad A, Safaei Dehbarez Y, Kargarshouraki Z, Mahdaviazad H. Evaluating the Validity and Reliability of the Persian Version of American Orthopedic Foot and Ankle Society Midfoot Scale. Evaluating the Validity and Reliability of the Persian Version of American Orthopedic Foot and Ankle Society Midfoot Scale. Foot Ankle Spec. 2022, 19386400211068242. [Google Scholar] [CrossRef]
- Costenoble A, Knoop V, Vermeiren S, et al. A Comprehensive Overview of Activities of Daily Living in Existing Frailty Instruments: A Systematic Literature Search. Gerontologist. 2021, 61, e12–e22. [Google Scholar] [CrossRef]
- Wang R, Wu C, Zhao Y, et al. Health related quality of life measured by SF-36: a population-based study in Shanghai, China. BMC Public Health. 2008, 8, 292. [Google Scholar] [CrossRef]
- Ozawa T, Shimizu K. Evaluation of patients' satisfaction after total hip arthroplasty (THA). J Phys Ther Sci. 2007, 19, 139–143. [Google Scholar] [CrossRef][Green Version]
- Tudoran C, Velimirovici DE, Berceanu-Vaduva DM, Rada M, Voiţă-Mekeres F, Tudoran M. Increased Susceptibility for Thromboembolic Events versus High Bleeding Risk Associated with COVID-19. Microorganisms. 2022, 10, 1738. [Google Scholar] [CrossRef]
- Walter N, Hinterberger T, Szymski D, Alt V, Rupp M. Psychological comorbidities in osteoarthritis in Germany. Sci Rep. 2023, 13, 2905. [Google Scholar] [CrossRef]
- van Dijk GM, Veenhof C, Schellevis F, et al. Comorbidity, limitations in activities and pain in patients with osteoarthritis of the hip or knee. BMC Musculoskelet Disord. 2008, 9, 95. [Google Scholar] [CrossRef]
- Reeuwijk KG, de Rooij M, van Dijk GM, Veenhof C, Steultjens MP, Dekker J. Osteoarthritis of the hip or knee: which coexisting disorders are disabling? Clin Rheumatol. 2010, 29, 739–747. [Google Scholar] [CrossRef]
- Balck F, Jeszenszky C, Günther KP, Kirschner S, Linke M. The impact of illness perception on functionality, pain, stiffness, and activity of daily living after total hip replacement surgery. J Psychosom Res. 2022, 155, 110749. [Google Scholar] [CrossRef]
- Shimizu K, Ozawa T, Watanabe H, Tanabe H, Kuroki Y. Usefulness of structural equation modeling in evaluation of prognosis of total hip replacement for coxarthrosis. J Phys Ther Sci. 2995, 17, 29–38. [Google Scholar] [CrossRef]
- Luo Y, Yang Z, Yeersheng R, Li D, Kang P. Clinical outcomes and quality of life after total hip arthroplasty in adult patients with a history of infection of the hip in childhood: a mid-term follow-up study. J Orthop Surg Res. 2019, 14, 38. [Google Scholar] [CrossRef]
- Shiba N, Tagawa Y, Nakashima Y, et al. Biomechanical effect and clinical application of the hip joint moment reduction brace. Biomechanical effect and clinical application of the hip joint moment reduction brace. Clin Orthop Relat Res. 1998, 149–157. [Google Scholar]
- Katz S, Ford AB, Heiple KG, Newill VA. Studies of illness in the aged: recovery after fracture of the hip. J Gerontol. 1964, 19, 285–293. [Google Scholar] [CrossRef]
- Edemekong PF, Bomgaars DL, Sukumaran S, et al. Activities of Daily Living. In: StatPearls [Internet]. /: Island (FL): StatPearls Publishing; 2023 Jan-. https, 2023.
- Guidet B, de Lange DW, Boumendil A, et al. The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med. 2020, 46, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Vergari C, Kim Y, Takemoto M; et al. The relationship between spino-pelvic-hip mobility and quality of life before and after total hip arthroplasty. Arch Orthop Trauma Surg 2023. [Google Scholar] [CrossRef] [PubMed]
- Messina S, Frongia AL, Antonaci L, et al. A critical review of patient and parent caregiver oriented tools to assess health-related quality of life, activity of daily living and caregiver burden in spinal muscular atrophy. Neuromuscul Disord. 2019, 29, 940–950. [Google Scholar] [CrossRef] [PubMed]
- M Moarrefzadeh A, Sarveazad A, Mohammadpour M, et al. Evaluation of health-related quality of life before and after total hip arthroplasty in the elderly in Iran: a prospective cohort study. BMC Psychol. 2022, 10, 64. [Google Scholar] [CrossRef]
- Mariconda M, Galasso O, Costa GG, Recano P, Cerbasi S. Quality of life and functionality after total hip arthroplasty: a long-term follow-up study. BMC Musculoskelet Disord. 2011, 12, 222. [Google Scholar] [CrossRef]
- Dehli T, Martinussen M, Mevik K, et al. Translation and validation of the Norwegian version of the fecal incontinence quality-of-life scale. Scand J Surg. 2011, 100, 190–195. [Google Scholar] [CrossRef]
- Wójcicki R, Pielak T, Erdmann J, et al. The Association between Acetabulum Fractures and Subsequent Coxarthrosis in a Cohort of 77 Patients-A Retrospective Analysis of Predictors for Secondary Hip Osteoarthritis. J Clin Med. 2023, 12, 6553. [Google Scholar] [CrossRef]
- Ray GS, Ekelund P, Nemes S, Rolfson O, Mohaddes M. Changes in health-related quality of life are associated with patient satisfaction following total hip replacement: an analysis of 69,083 patients in the Swedish Hip Arthroplasty Register. Acta Orthop. 2020, 91, 48–52. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |