Abstract
Background. The management of a recurrent inguinal hernia varies depending on multiple factors. In the case of recurrent inguinal hernias after open anterior repair, the laparoscopic approach is recommended. TEP and TAPP procedures are considered to have similar results. The purpose of the study is to evaluate on our sample if there are differences between primary inguinal hernia cases and recurrent hernia after laparoscopic TAPP and TEP procedures. Materials and Methods. We retrospectively reviewed the medical records of 300 patients who underwent laparoscopic inguinal hernia repairs at our hospital from March 2013 to March 2023. Results. Of the 300 patients, 39 of them (13%) had recurrent hernias after open anterior procedures. The mean age of patients with recurrent hernias was 56.82 years, compared to 50.47 years in those with primary hernias. In 27 cases we used the TAPP approach (69%), while in the remaining 12 cases the TEP approach (31%). Operative time for recurrent hernias was 72.69 minutes as opposed to 58.49 minutes for primary hernias. The percentage of peritoneal tears was higher for recurrent hernias (38%) than for primary hernias (18%). Conclusions. Surgery for inguinal hernia recurrence, is often more complex and time-consuming than for a primary hernia. However, postoperative results are favorable, with a low complication rate. Out of the two minimally invasive approach options, TAPP is our choice, especially due to the increased incidence of peritoneal tears.
Introduction
Inguinal hernia repair (IHR) is one of the most common surgical procedures worldwide. It is estimated that more than 20 million IHR are performed every year [1].
The most important criteria for outcomes after inguinal hernia repair is the quality of life as evaluated by recurrence rate and chronic postoperative inguinal pain rate, which were the major components of this analysis. According to these criteria, the main goal of every groin hernia repair is a rate of less than 1% for either of them. Recurrence rate is still a major concern for both the hernia surgeon and the patient, despite development of modern techniques, meshes and technology.
Recurrence rates reported in the literature are variable, related to the patient (age, gender, comorbidities) and to the surgeon (technique used, surgeon's experience, length of time of postoperative follow-up) [2,3].
Surgical repair of a hernia recurrence is more complex than the treatment of a primary one. The elements contributing to that increased complexity of a recurrence are the existence of scar tissue, the possibility of large, multiple defects, and modified anatomy [3]. Equally important are the degree of recurrence, the presence or absence of the mesh and the experience and expertise of the surgeon. When compared to open primary IHR, open repair of recurrent inguinal hernias (IH) leads to increased intraoperative and postoperative complications, higher recurrence rate and increased pain [4].
According to European guidelines, for recurrences after open anterior procedures, the endoscopic procedure is recommended, because the operation will be performed in an anatomical scar-free plane, which will allow a relatively ease at dissection [4,5,6]. Both TAPP (transabdominal preperitoneal patch plasty) and TEP (total extraperitoneal patch plasty) techniques can be used for the treatment of recurrence after previous procedures if the surgeon has sufficient experience [7,8].
Our study is focused on the identification of the differences between TAPP and TEP repair of primary and recurrent inguinal hernias.
Materials and Methods
Patients’ selection
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. No animal was used for this study. Informed written consent was obtained from all patients before surgery.
After obtaining our institutional review board approval (September 2022), we retrospectively reviewed, from a prospective kept data base, the medical records of 300 patients who underwent endoscopic IHR at our institution from March 2013 to March 2023. During the period under review, we compared minimally invasive interventions for recurrent inguinal hernias with primary groin hernia repairs. TEP and TAPP procedures were performed following the surgical technique described in the Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [7].
Variables studied
We collected and analyzed the following demographic, perioperative, and long-term follow-up variables: age, sex, general risk factors (obesity, diabetes mellitus, cardiovascular disease, anticoagulant therapy, etc.), location and type of hernia (EHS classification), surgical technique for recurrent hernia repair, duration of surgery, conversion of laparoscopic to open procedure, intra- and postoperative complications and recurrence. The analysis was performed to determine the success of different repair methods, as shown by IHR recurrence rates and complications.
Initially all patients over 18 years of age, undergoing minimally invasive surgery for IH during the reviewed period were included in the study. Out of these patients, we excluded the ones with recurrent hernias who presented chronic pain and the ones operated as emergencies. In all cases, informed consent was obtained after discussion, providing a reasonable disclosure [9].
Follow-up evaluation
In our institution the follow-up period for inguinal surgery usually is 1, 6, 12 and 24 months. The recommended periods for follow-up were made known to patients during hospitalization and were included as a recommendation on the referral letter. At the time of writing the article, we contacted patients operated for recurrences for further follow-up using a questionnaire (Table 1) [10].

Table 1.
Questionnaire used by us for last follow-up
Statistical analysis
Data were expressed as mean ± standard deviation (sd). Continuous variables were analyzed by ANOVA variance test followed by unpaired 2 tail Student’s test assuming unequal variance and the binary outcomes with the χ2 test. Pearson correlation (r) was used with the regression equation. Probabilities smaller than 0.05 were considered as statistically significant. SPSS statistic version 22.0, 2018 (IBM Chicago, Il, USA) was used to perform statistical analysis.
Results
Over the study period, 300 patients with primary and recurrent inguinal hernias were admitted in the Clinical Department of Surgery. Amongst them, 39 (13%) had recurrent inguinal hernias after open anterior repairs; the large majority of the patients were males (35 – 90%). The mean age was 56.82 ± 13.48 (min 26 – max 87) years (Table 2).

Table 2.
Demographic characteristics of the patients
Half of the patients had single or associated comorbidities: 13 arterial hypertension, 4 heart disease, 4 obesity, 1 diabetes mellitus, 2 chronic oral anticoagulant therapy.
The mean time from the primary hernia repair to the admittance for recurrence repair was 15.5 ± 14.7 years (range 0.5 – 55 years) with a wide range in time-lapse (Table 2). The awareness of recurrence varies between 1 month and over 5 years before presentation (mean 2.3 ± 0.9 years) (Table 2). But the second benchmark is more relative, being only declarative, strictly related to the patient.
Twenty-one patients reported various degrees of incapacity of performing daily activities and 13 of them were unsatisfied with the cosmetic aspect of their groins.
The primary repair of the hernias was a tissular technique in 31 patients (79%), while in the remaining 8 (21%) a prosthetic reinforcement was performed. Seven patients had a multiple hernia recurrencies (5 cases at 2nd recurrence, 2 cases at 3rd recurrence).
All our patients were operated under general anesthesia with a mean ASA score of 2.7 ± 0.4 (min 1 – max 3). TAPP was used in 27 patients (69%); in the remaining TEP was the procedure of choice. The decision to apply the TEP or TAPP procedure was made according to the surgeon’s preference. The location and dimensions of the abdominal defect were determined intraoperatively according with the EHS classification (Table 3).

Table 3.
Classification of operated recurrent hernias
We identified 2 femoral defects and 1 obturator defect in addition to recurrent IH. Nine of the patients had bilateral hernias (primary hernia on one side and recurrent hernia on the opposite side), in one case the recurrence was bilateral. In 1 case where the indication for TAPP approach was for primary hernia, we found recurrent hernia on the contralateral side.
All operations could be completed by minimally invasive approach. In 1 TEP case, due to technical difficulties, the patient was converted to TAPP.
The inserted meshes were flat polypropylene, ranging in size from 15x10 cm to 15x13 cm. For primary IHs the mean operative time was 58.49 minutes. For recurrent hernias the mean operative time was 72.69 (71.76 ± 21.6 minutes). The difference was statistically significant (p = 0.026). In the case of bilateral hernias, only the duration of one of the hernias was taken into account (Table 4).

Table 4.
Comparative data analysis
According to the duration of the interventions performed for recurrent hernias we found that 13 of them (33%) lasted less than one hour. For the rest of the operations that lasted more than 60 minutes (26 patients - 67%), we analyzed the operating files to find possible explanations. The reasons for the increased operative time were difficult dissection (5 patients), adhesions at the deep inguinal ring (5 patients), peritoneal sac adherent to the prosthesis (4 patients), and a bulky peritoneal sac (2 cases). Operative time in patients with previous tissue repair was shorter (68.4 ± 27.5 minutes) than in patients with mesh repair (84.2 ± 17.8 minutes) and the difference was significant (p = 0.018).
In 15 cases (38%) we recorded peritoneal tears during dissection, 6 cases during the TAPP operations (22%) and 7 cases for the TEP operations (58%). Peritoneal tears were recorded in 46 patients (18%) of the primary hernia group (p = 0.029).
Seroma was the most common postoperative complication, occurring in 5 patients (13%). In 2 cases evacuatory puncture was required, with subsequent favorable evolution. One patient presented with epididymitis and another with penoscrotal ecchymosis, with a self-limiting course. In the study group, 1 reoperation was required for a large hematoma, and the patient with chronic alcoholic liver disease also required transfusion. The hematoma was cleared during endoscopic revision, but no local source of bleeding was identified. The position of the mesh was found to be correct and therefore was left in place and a postoperative drain was again placed.
Neither wound nor mesh infections were recorded in the study group.
The average length of hospital stay was 2.58 ± 1.33 days, with limits between 1 and 9 days (in the case of the reoperated patient).
The presentation of the data patients at follow-up is shown in Table 5.

Table 5.
Presentation for follow-up
After further follow-up 3 patients were deceased (the causes of death were unrelated to the performed IHR) and 4 were lost to follow-up. All 32 patients (82%), who could be contacted had no hernia recurrence and no pain at the clinical examination.
Discussions
Despite the new techniques introduced, recurrence after IHR has remained the same in recent years, representing about 6-15% [11]. Recurrence rates vary in accordance with the length of follow-up [12], increasing in direct proportion to the time elapsed since surgery.
Recurrence rates based on how many patients came back to the same clinic are unreliable [2]. In fact, none of the patients with recurrent hernia in the analyzed group had been operated for primary hernia in our service.
Using the proportion of hernia repairs performed for recurrence is merely a surrogate for the true recurrence rate. Not all patients who suffer a recurrence will undergo reoperation [13]. It is estimated that the true recurrence rate would be up to twice as high as reoperations [1]. The risk of re-recurrence for recurrent IHs is higher than the risk of recurrence after primary IHR [13,14].
Significant risk factors for recurrence after IH surgery are male gender, smoking, direct inguinal hernias at the time of the primary procedure, and operation for a recurrent inguinal hernia. The potential risk factors identified for onset of recurrences were older age (age exceeding 50 years), obesity or more than a 12 kg loss of body weight [15], certain diseases (pulmonary disease, diabetes mellitus, aortic aneurysm, immunosuppression, inflammatory bowel disease etc.) [16,17,18,19], complications after primary hernia repair [13].
The recommendation in the European Hernia Society Guidelines for the treatment of recurrent inguinal hernias is to modify the technique in relation to the previous technique, and use a new plane of dissection for mesh implantation [4]. Non-compliance with guidelines is thought to be associated with higher rates of perioperative complications and a higher risk of recurrence [20,21,22]. Thus, for recurrences after open anterior approach, endoscopic/ laparoscopic approach is recommended. Due to the fact that the posterior route is free of scar, the groin can be reached more easily with an endoscopic approach [21]. Laparoscopic repair avoids the difficulties of operating through scarred groin tissue, particularly if a mesh has been inserted previously [22].
Conversely, laparoscopic procedures have the advantage of approaching and reducing the hernial sac through virgin tissues and covering the entire myopectineal orifice with a mesh. Abdominal wall reinforcement is achieved by using a large preperitoneal prosthetic mesh rather than by approximating already weakened and scarred aponeurotic and fascial entities [23]. In addition, the laparoscopic procedure is reported to be associated with less postoperative pain, shorter hospitalization, and earlier return to normal activities [5,13].
In the vast majority of cases, this is due to the fact that even when operating in another anatomic layer, for the recurrent operation, only rarely there is no scarring from the previous operation. As such, the conditions under which a recurrent operation is conducted are generally worse than those prevailing at the time of the primary operation [17,24]. In our case series only 33% of patients with recurrences had the duration of surgery equal to the average duration of primary hernia surgery. In addition, the risk of peritoneal tears is quite high. These usually can lead to loss of working space in TEP approach with difficulties of dissection and require suturing. We hold the opinion that they are more easily managed by the TAPP approach. Although for the approach of recurrent inguinal hernias, TEP and TAPP techniques are considered equivalent [13,25], we lately prefer the TAPP approach.
The open recurrent repair was associated with significant larger hernia defects, more medial [26,27,28,29], fewer femoral and lateral EHS classifications [17].
Although there have been situations where we have not encountered specific technical difficulties while operating after prosthetic procedures, the likelihood of having a cumbersome dissection is higher in recurrences where prostheses were used in the primary operation.
The operation time is mainly related to the complexity of the dissection. In these circumstances the adhesion of the hernia sac to the inguinal canal prosthesis seems to be the main explanation for the increased duration. Another explanation for the difficult dissection of the sac at the deep inguinal orifice is the possible anchoring of the ligated peritoneal stump (classic Barker maneuver).
Patients presented discharge notes from primary hernia care in only 9 cases (26.47%). In these circumstances we relied only on the information provided by the patients (usually the patients indicated that they were operated with or without mesh). Due to minimally invasive surgical techniques employed, we had no possibility to intraoperatively recognize the previously used open procedure. In the patients with prosthesis, we did not identify plugs or other types of prosthesis in the preperitoneal space, so we considered the initial operation to be Lichtenstein type.
An anterior technique for recurrence after open anterior repair implies that scar tissues, with distorted tissue planes, must be entered [1,15]. Under these conditions, restoration of anatomical structures often requires a more difficult dissection, which translates into increased operating time and risk of complications (risk of testicular atrophy, bleeding, nerve injury and nerve entrapment, sometimes orchiectomy, higher infection rates) [1,15,29,30,31]. Re- operative herniorrhaphy through a transinguinal approach is reflected in the significantly longer operating times of the mesh group versus either the Shouldice or laparoscopic groups, even in a specialized hernia center [28]. One explanation could be the relative inexperience of surgeons in the mesh era with recurrent hernias [28]. The main reason for introducing the laparoscopic approach to inguinal hernias in our current practice was precisely to avoid dealing with recurrences by open anterior approach.
We prefer, in our current practice, the minimally invasive approach to recurrent hernias after open anterior procedures, which accounted for 73,58% of the total number of recurrent hernias operated on during the study period. Our reasons for preferring the repeated open approach in 14 other cases were large hernial defects (defect 3 according to EHS hernia classification) or scrotal hernia. Eleven operations were recurrences after tissue operations and 3 case after prosthetic surgery. Mean duration was 89.64 minutes (range 60 to 150 minutes). We recorded 1 epididymitis, and 1 superficial wound infection. We performed Lichtenstein operation in 13 cases and Wantz operation in 1 case.
During the same time interval, we operated by open anterior approach 208 IHs (40.94% of the total number of IHs operated on). The indication for open repair was given by large defects with bulky peritoneal sacs, association with hydrocele and the need to perform orchiectomy, contraindication of general anesthesia, patient's option to be operated by open procedures. Under these circumstances, we state that for IHs with large, inguinoscrotal defects, or complex hernias [32], we prefer the open approach, both for primary or recurrent hernias. In our experience, for this kind of cases, the minimally invasive approach would have been more difficult than the open approach. Without our own experience, perhaps the robotic approach will make it easier to solve scrotal hernia cases [33,34]. In these circumstances, our management of patients with IH is detailed in the Table 3.
The minimally invasive repair should not be a goal, but a modern way to treat primary and recurrent IHs. According to European guidelines, the Lichtenstein technique remains the gold standard of IH treatment [1]. The type of approach should be chosen according to the size of the defect and the volume of the herniated viscera, the patient's surgical, medical history and choice, the department's equipment and the experience of the surgical team (Figure 1).
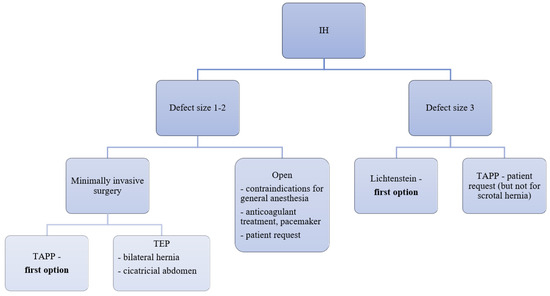
Figure 1.
Our protocol of the patients with IH
Laparoscopic repair of recurrent hernias offered similar recurrence rates to primary repair which is different from past studies [27,28], and recovery seems to be similar to primary repair [26].
We estimated that presentation of patients at follow-up by self-initiative would have been low, but were found to be similar to other data in literature [26,34]. The fact that at the time of writing of this article, we did not identify patients with recurrences is encouraging. But taking into consideration that the time interval since surgery is variable (between less than 1 year and more than 10 years), it is possible that some of them may develop recurrences over time.
The present study has some limitations. The main limitation with this study was its retrospective nature. In addition, we analyzed a relatively small number of cases, which were treated in a non-randomized design.
Conclusions
Surgery for inguinal hernia recurrence, mainly done for older patients than those with primary hernias, is often more complex and time-consuming than for a primary hernia. Postoperative results are however favorable, with a low complication rate.
The endoscopic/laparoscopic approach to a recurrence after a tissue procedure appears to be simpler than after a prosthetic procedure. With a good preoperative indication, the endoscopic/laparoscopic approach is confirmed to be a good indication for recurrent hernias after an open approach.
Of the 2 minimally invasive approaches, due in particular to the increased incidence of peritoneal breach, we are inclined to use the TAPP procedure.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
References
- HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018, 22, 1–165. [Google Scholar] [CrossRef]
- Nolsøe A, Andresen K, Rosenberg J. Repair of recurrent hernia is often performed at a different clinic. Hernia. 2016, 20, 783–787. [Google Scholar] [CrossRef]
- Scheuerlein H, Schiller A, Schneider C, Scheidbach H, Tamme C, Köckerling F. Totally extraperitoneal repair of recurrent inguinal hernia. Surg Endosc. 2003, 17, 1072–1076. [Google Scholar] [CrossRef]
- Köckerling F, Koch A, Lorenz R, et al. Open Repair of Primary Versus Recurrent Male Unilateral Inguinal Hernias: Perioperative Complications and 1-Year Follow-up. World J Surg. 2016, 40, 813–825. [Google Scholar] [CrossRef]
- Simons MP, Aufenacker T, Bay-Nielsen M, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009, 13, 343–403. [Google Scholar] [CrossRef]
- Miserez M, Peeters E, Aufenacker T, et al. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2014, 18, 151–163. [Google Scholar] [CrossRef]
- Bittner R, Arregui ME, Bisgaard T, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc. 2011, 25, 2773–2843. [Google Scholar] [CrossRef]
- Bittner R, Montgomery MA, Arregui E, et al. Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society) [published correction appears in Surg Endosc. 2015, 29, 1655–6. Koeckerling, F [corrected to Köckerling, F]]. Surg Endosc. 2015, 29, 289–321. [Google Scholar] [CrossRef]
- Serban D, Spataru RI, Vancea G, Balasescu SA, Socea B, Tudor C, Dascalu AM. Informed consent in all surgical specialties: from legal obligation to patient satisfaction. Rom J Leg Med. 2020, 28, 317–321. [Google Scholar] [CrossRef]
- Tastaldi L, Barros PHF, Krpata DM, et al. Hernia recurrence inventory: inguinal hernia recurrence can be accurately assessed using patient-reported outcomes. Hernia. 2020, 24, 127–135. [Google Scholar] [CrossRef]
- Guillaumes S, Juvany M. Inguinal hernia repairs performed for recurrence in Spain: population-based study of 16 years and 1,302,788 patients. Hernia. 2022, 26, 1023–1032. [Google Scholar] [CrossRef]
- Köckerling F, Krüger C, Gagarkin I, et al. What is the outcome of re-recurrent vs recurrent inguinal hernia repairs? An analysis of 16,206 patients from the Herniamed Registry. Hernia. 2020, 24, 811–819. [Google Scholar] [CrossRef]
- Shah NR, Mikami DJ, Cook C, et al. A comparison of outcomes between open and laparoscopic surgical repair of recurrent inguinal hernias. Surg Endosc. 2011, 25, 2330–2337. [Google Scholar] [CrossRef]
- Sevonius D, Montgomery A, Smedberg S, Sandblom G. Chronic groin pain, discomfort and physical disability after recurrent groin hernia repair: impact of anterior and posterior mesh repair. Hernia. 2016, 20, 43–53. [Google Scholar] [CrossRef]
- Dedemadi G, Sgourakis G, Karaliotas C, Christofides T, Kouraklis G, Karaliotas C. Comparison of laparoscopic and open tension-free repair of recurrent inguinal hernias: a prospective randomized study. Surg Endosc. 2006, 20, 1099–1104. [Google Scholar] [CrossRef]
- Murphy BL, Zhang J, Ubl DS, Habermann EB, Farley DR, Paley K. Surgical trends of groin hernia repairs performed for recurrence in medicare patients. Hernia. 2019, 23, 677–683. [Google Scholar] [CrossRef]
- Köckerling F, Jacob D, Wiegank W, et al. Endoscopic repair of primary versus recurrent male unilateral inguinal hernias: Are there differences in the outcome? Surg Endosc. 2016, 30, 1146–1155. [Google Scholar] [CrossRef]
- Serban D, Popa Cherecheanu A, Dascalu AM, et al. Hypervirulent Klebsiella pneumoniae Endogenous Endophthalmitis-A Global Emerging Disease. Life (Basel). 2021, 11, 676. [Google Scholar] [CrossRef]
- Silaghi A, Constantin VD, Socea B, et al. Inflammatory bowel disease: pathogenesis, diagnosis and current therapeutic approach. J Mind Med Sci. 2022, 9, 56–77. [Google Scholar] [CrossRef]
- Savlovschi C, Brănescu C, Serban D, et al. Hernia Amyand--caz clinic [Amyand's hernia--a clinical case]. Chirurgia (Bucur). 2010, 105, 409–414. [Google Scholar]
- Köckerling F, Bittner R, Kuthe A, et al. Laparo- endoscopic versus open recurrent inguinal hernia repair: should we follow the guidelines? Surg Endosc. 2017, 31, 3168–3185. [Google Scholar] [CrossRef]
- Poelman MM, van den Heuvel B, Deelder JD, et al. EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg Endosc. 2013, 27, 3505–3519. [Google Scholar] [CrossRef]
- Richards SK, Vipond MN, Earnshaw JJ. Review of the management of recurrent inguinal hernia. Hernia. 2004, 8, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Dumitrescu D, Savlovschi C, Borcan R, et al. Caz clinic--hernie diafragmatică voluminoasă--abdomen acut chirurgical: dificultăţi diagnostice şi terapeutice [Clinical case--voluminous diaphragmatic hernia-- surgically acute abdomen: diagnostic and therapeutical challenges]. Chirurgia (Bucur). 2011, 106, 657–660. [Google Scholar]
- Köckerling F, Bittner R, Kuthe A, et al. TEP or TAPP for recurrent inguinal hernia repair-register-based comparison of the outcome. Surg Endosc. 2017, 31, 3872–3882. [Google Scholar] [CrossRef] [PubMed]
- Haggerty S, Forester B, Hall T, et al. Laparoscopic repair of recurrent inguinal hernia offers similar outcomes and quality of life to primary laparoscopic repair. Hernia. 2021, 25, 165–172. [Google Scholar] [CrossRef]
- Staarink M, van Veen RN, Hop WC, Weidema WF. A 10-year follow-up study on endoscopic total extraperitoneal repair of primary and recurrent inguinal hernia. Surg Endosc. 2008, 22, 1803–1806. [Google Scholar] [CrossRef]
- Chan G, Chan CK. The characteristics of inguinal hernia recurrence in the modern era and the long-term outcomes after re-operation. Hernia. 2011, 15, 193–199. [Google Scholar] [CrossRef]
- Öberg S, Jessen ML, Andresen K, Rosenberg J. Technical details and findings during a second Lichtenstein repair or a second laparoscopic repair in the same groin: a study based on medical records. Hernia. 2021, 25, 149–157. [Google Scholar] [CrossRef]
- Moisin A, Faur M, Popa C, Gherman CD, et al. Laparoscopic versus open surgical treatment of umbilical hernia. J Mind Med Sci. 2022, 9, 143–151. [Google Scholar] [CrossRef]
- Öberg S, Jessen ML, Andresen K, Rothman JV, Rosenberg J. High complication rates during and after repeated Lichtenstein or laparoscopic inguinal hernia repairs in the same groin: a cohort study based on medical records. Hernia. 2020, 24, 801–810. [Google Scholar] [CrossRef]
- Oprea V, Grad O, Gheorghescu D, Moga D. Transinguinal Preperitoneal Mesh Plasty - An Alternative or a Dispensable Technique? A Prospective Analyze vs Lichtenstein Repair for Complex Unilateral Groin Hernias. Chirurgia (Bucur). 2019, 114, 48–56. [Google Scholar] [CrossRef]
- Dumitrescu V, Dumitrescu D, Stoica PL, Draghici G, Chirca A. Transabdominal pre-peritoneal repair procedure (TAPP) versus open hernia repair (OHR) in the treatment of inguinal hernia. J Mind Med Sci. 2022, 9, 175–180. [Google Scholar] [CrossRef]
- Bondi J, Botnen HG, Baekkelund O, Groven S. A retrospective review of a large series of groin hernia patients operated with robotically assisted laparoscopic technique (R-TAPP). J Robot Surg. 2023, 17, 653–658. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |