Have Chest Imaging Habits Changed in the Emergency Department after the Pandemic?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Study Population
2.3. Data Collection and Processing
2.4. Variables
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raoof, S.; Feigin, D.; Sung, A.; Raoof, S.; Irugulpati, L.; Rosenow, E.C. Interpretation of Plain Chest Roentgenogram. Chest 2012, 141, 545–558. [Google Scholar] [CrossRef] [PubMed]
- Simpson, G.; Hartrick, G.S. Use of thoracic computed tomography by general practitioners. Med. J. Aust. 2007, 187, 43–46. [Google Scholar] [CrossRef][Green Version]
- Tigges, S.; Roberts, D.L.; Vydareny, K.H.; Schulman, D.A. Routine chest radiography in a primary care setting. Radiology 2004, 233, 575–578. [Google Scholar] [CrossRef] [PubMed]
- Renwick, I.G.; Butt, W.P.; Steele, B. How well can radiographers triage x-ray films in accident and emergency departments? BMJ 1991, 302, 568–569. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Durhan, G.; Akpinar, M.G. Thorax CT in Emergency Department. GGHS 2018, 6, 213–219. [Google Scholar] [CrossRef]
- Turkish Republic Ministry of Health, Health Statistics Annuals. Available online: https://dosyasb.saglik.gov.tr/Eklenti/45317,siy2021-ingilizcepdf.pdf?0 (accessed on 20 October 2023).
- Selvarajan, S.K.; Levin, D.C.; Parker, L. The Increasing Use of Emergency Department Imaging in the United States: Is It Appropriate? Am. J. Roentgenol. 2019, 213, W180–W184. [Google Scholar] [CrossRef]
- Bellolio, F.; Heien, H.C.; Sangaralingham, L.R.; Jeffery, M.M.; Campbell, R.L.; Cabrera, D.; Shah, N.D.; Hess, E.P. Increased Computed Tomography Utilization in the Emergency Department and Its Association with Hospital Admission. West. J. Emerg. Med. 2017, 18, 835–845. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Halacli, B.; Kaya, A.; Topeli, A. Critically-ill COVID-19 patient. Turk. J. Med. Sci. 2020, 50, 585–591. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Chi, W.-Y.; Li, Y.-D.; Huang, H.-C.; Chan, T.E.H.; Chow, S.-Y.; Su, J.-H.; Ferrall, L.; Hung, C.-F.; Wu, T.-C. COVID-19 vaccine update: Vaccine effectiveness, SARS-CoV-2 variants, boosters, adverse effects, and immune correlates of protection. J. Biomed. Sci. 2022, 29, 82. [Google Scholar] [CrossRef] [PubMed]
- WHO Director-General’s Opening Remarks at the Media Briefing—May 5 2023. Available online: https://www.who.int/news-room/speeches/item/who-director-general-s-opening-remarks-at-the-media-briefing---5-may-2023 (accessed on 4 June 2023).
- Loftus, T.M.; Wessling, E.G.; Cruz, D.S.; Schmidt, M.J.; Kim, H.S.; McCarthy, D.M.; Malik, S. Impact of the COVID pandemic on emergency department CT utilization: Where do we go from here? Emerg. Radiol. 2022, 29, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Coskun, M.; Cilengir, A.H.; Cetinoglu, K.; Horoz, M.; Sinci, A.; Demircan, B.; Uluc, E.; Gelal, F. Did radiation exposure increase with chest CT use among different ages during the COVID-19 pandemic? A multicenter study with 42028 Chest CT scans. Diagn. Interv. Radiol. 2023, 29, 373–378. [Google Scholar] [CrossRef]
- Kiliç, P.; Şendur, H.N. Impacts of COVID-19 Pandemic on Computed Tomography Usages in Emergency Department: Cross-sectional Study. Turk. Klin. J. Med. Sci. 2021, 41, 274–279. [Google Scholar] [CrossRef]
- Barten, D.G.; Latten, G.H.P.; Van Osch, F.H.M. Reduced Emergency Department Utilization during the Early Phase of the COVID-19 Pandemic: Viral Fear or Lockdown Effect? Disaster Med. Public Heal. Prep. 2022, 16, 36–39. [Google Scholar] [CrossRef]
- Hartnett, K.P.; Kite-Powell, A.; DeVies, J.; Coletta, M.A.; Boehmer, T.K.; Adjemian, J.; Gundlapalli, A.V. Impact of the COVID-19 Pandemic on Emergency Department Visits-United States, 1 January 2019–30 May 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Adarve Castro, A.; Díaz Antonio, T.; Cuartero Martínez, E.; García Gallardo, M.M.; Bermá Gascón, M.L.; Domínguez Pinos, D. The usefulness of chest X-rays for evaluating prognosis in patients with COVID-19. Radiologia Engl. Ed. 2021, 63, 476–483. [Google Scholar] [CrossRef]
- Sharperson, C.; Hanna, T.N.; Herr, K.D.; Zygmont, M.E.; Gerard, R.L.; Johnson, J.O. The effect of COVID-19 on emergency department imaging: What can we learn? Emerg. Radiol. 2021, 28, 339–347. [Google Scholar] [CrossRef]
- Karaali, R.; Karakaya, Z.; Bora, E.S.; Akyol, P.Y.; Bilgin, S. Evaluation of Performance Between Thoracic Computed Tomography and Reverse Transcription- Polymerase Chain Reaction Test in Coronavirus Disease-19 Management. Erciyes Med. J. 2021, 43, 594–599. [Google Scholar] [CrossRef]
- Fang, Y.; Zhang, H.; Xie, J.; Lin, M.; Ying, L.; Pang, P.; Ji, W. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology 2020, 296, E115–E117. [Google Scholar] [CrossRef]
- Di Minno, A.; Ambrosino, P.; Calcaterra, I.; Di Minno, M.N.D. COVID-19 and Venous Thromboembolism: A Meta-analysis of Literature Studies. Semin. Thromb. Hemost. 2020, 46, 763–771. [Google Scholar] [CrossRef]
- Xu, X.; Yu, C.; Zhang, L.; Luo, L.; Liu, J. Imaging features of 2019 novel coronavirus pneumonia. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 1022–1023. [Google Scholar] [CrossRef]
- Li, Y.; Xia, L. Coronavirus Disease 2019 (COVID-19): Role of Chest CT in Diagnosis and Management. Am. J. Roentgenol. 2020, 214, 1280–1286. [Google Scholar] [CrossRef]
- Haak, S.L.; Renken, I.J.; Jager, L.C.; Lameijer, H.; van der Kolk, B.B.Y. Diagnostic accuracy of point-of-care lung ultrasound in COVID-19. Emerg. Med. J. 2021, 38, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Acar, H.; Yamanoğlu, A.; Arikan, C.; Bilgin, S.; Akyol, P.Y.; Kayali, A.; Karakaya, Z. Effectiveness of the CLUE protocol in COVID-19 triage. Cukurova Med. J. 2022, 47, 722–728. [Google Scholar] [CrossRef]
- Narinx, N.; Smismans, A.; Symons, R.; Frans, J.; Demeyere, A.; Gillis, M. Feasibility of using point-of-care lung ultrasound for early triage of COVID-19 patients in the emergency room. Emerg. Radiol. 2020, 27, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Kuru, L.I.; Günay, O.; Palaci, H.; Yarar, O. Determination of the effective radiation dose of the patient in computed tomography. J. BAUN Inst. Sci. Technol. 2019, 21, 436–443. [Google Scholar] [CrossRef][Green Version]
- Mitelman, F.; Johansson, B.; Mertens, F. The impact of translocations and gene fusions on cancer causation. Nat. Rev. Cancer 2007, 7, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.; Law, M.W.M.; Khong, P.L. Whole-Body PET/CT Scanning: Estimation of Radiation Dose and Cancer Risk. Radiology 2009, 251, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Baratella, E.; Ruaro, B.; Marrocchio, C.; Poillucci, G.; Pigato, C.; Bozzato, A.M.; Salton, F.; Confalonieri, P.; Crimi, F.; Wade, B.; et al. Diagnostic Accuracy of Chest Digital Tomosynthesis in Patients Recovering after COVID-19 Pneumonia. Tomography 2022, 24, 1221–1227. [Google Scholar] [CrossRef] [PubMed]
- Plasencia-Martínez, J.M.; Moreno-Pastor, A.; Lozano-Ros, M.; Jiménez-Pulido, C.; Herves-Escobedo, I.; Pérez-Hernández, G.; García-Santos, J.M. Digital tomosynthesis improves chest radiograph accuracy and reduces microbiological false negatives in COVID-19 diagnosis. Emerg. Radiol. 2023, 30, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Baratella, E.; Bussani, R.; Zanconati, F.; Marrocchio, C.; Fabiola, G.; Braga, L.; Maiocchi, S.; Berlot, G.; Volpe, M.C.; Moro, E.; et al. Radiological-pathological signatures of patients with COVID-19-related pneumomediastinum: Is there a role for the Sonic hedgehog and Wnt5a pathways? ERJ Open Res. 2021, 23, 00346-2021. [Google Scholar] [CrossRef] [PubMed]
- Novelli, F.; Pinelli, V.; Chiaffi, L.; Carletti, A.M.; Sivori, M.; Giannoni, U.; Chiesa, F.; Celi, A. Prognostic significance of peripheral consolidations at chest x-ray in severe COVID-19 pneumonia. Radiol. Med. 2022, 127, 602–608. [Google Scholar] [CrossRef]
- Agarwal, M.; Udare, A.; Patlas, M.; Ramonas, M.; Alaref, A.A.; Rozenberg, R.; Ly, D.L.; Golev, D.S.; Mascola, K.; van der Pol, C.B. Effect of COVID-19 on computed tomography usage and critical test results in the emergency department: An observational study. CMAJ Open 2020, 8, E568–E576. [Google Scholar] [CrossRef] [PubMed]

| Pre-Pandemic (Mean ± SD 1) | Pandemic (Mean ± SD) | Post-Pandemic (Mean ± SD) | p-Value * | |
|---|---|---|---|---|
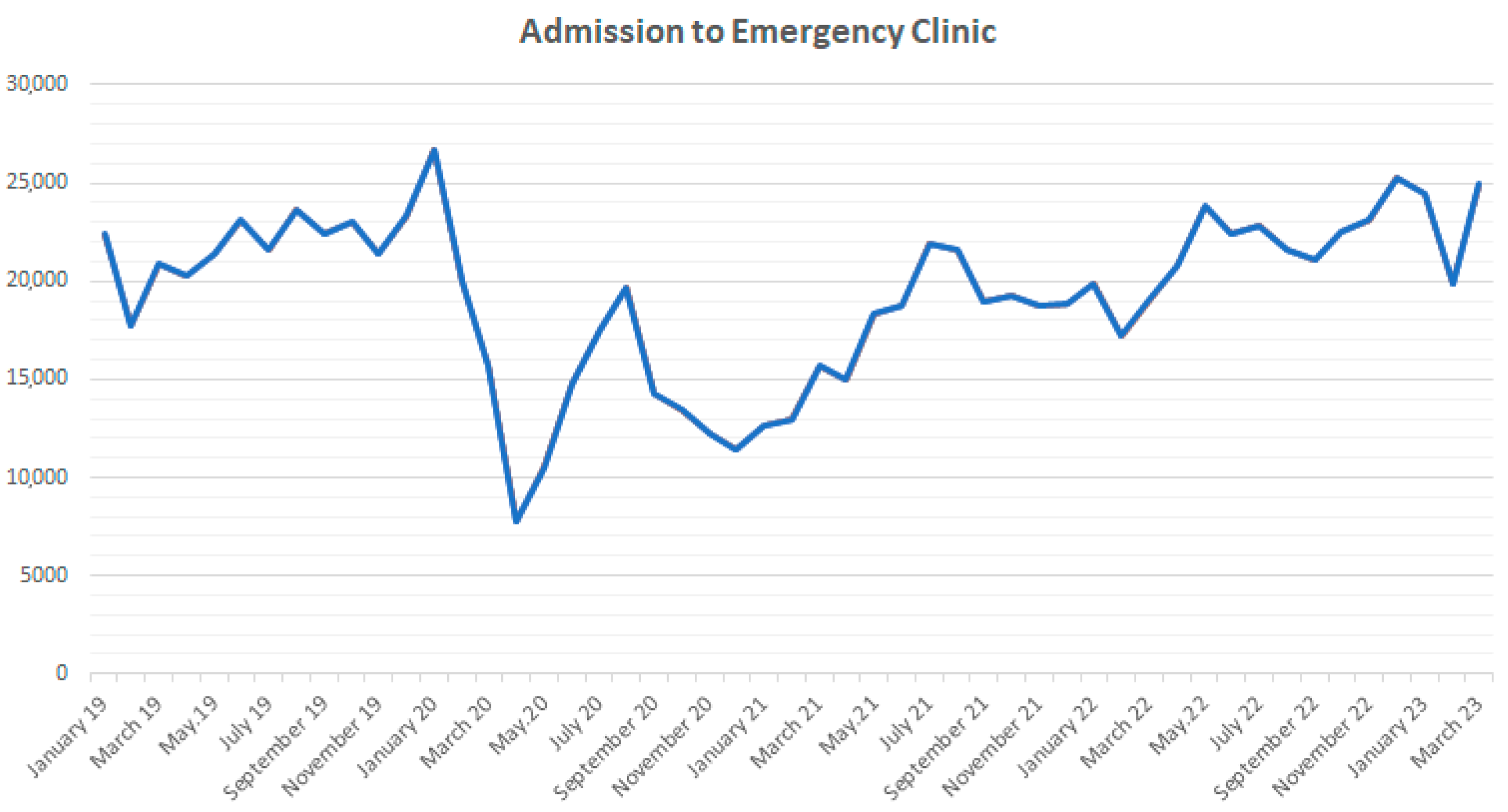
| Total Number of Patients | 21,984 ± 2087 | 16,248 ± 3643 | 22,732 ± 1701 | <0.001 |
| Female (%) | 47.3 ± 0.2 | 50.6 ± 0.4 | 47.8 ± 0.2 | <0.001 |
| Male (%) | 52.7 ± 0.2 | 49.4 ± 0.4 | 52.2 ± 0.2 | <0.001 |
| CXR 2 Mean Age | 56.6 ± 1.1 | 52.3 ± 1.7 | 53.3 ± 5.6 | <0.001 |
| CCT 3 Mean Age | 68.5 ± 1.7 | 59.6 ± 3.9 | 61.0 ± 4.0 | <0.001 |
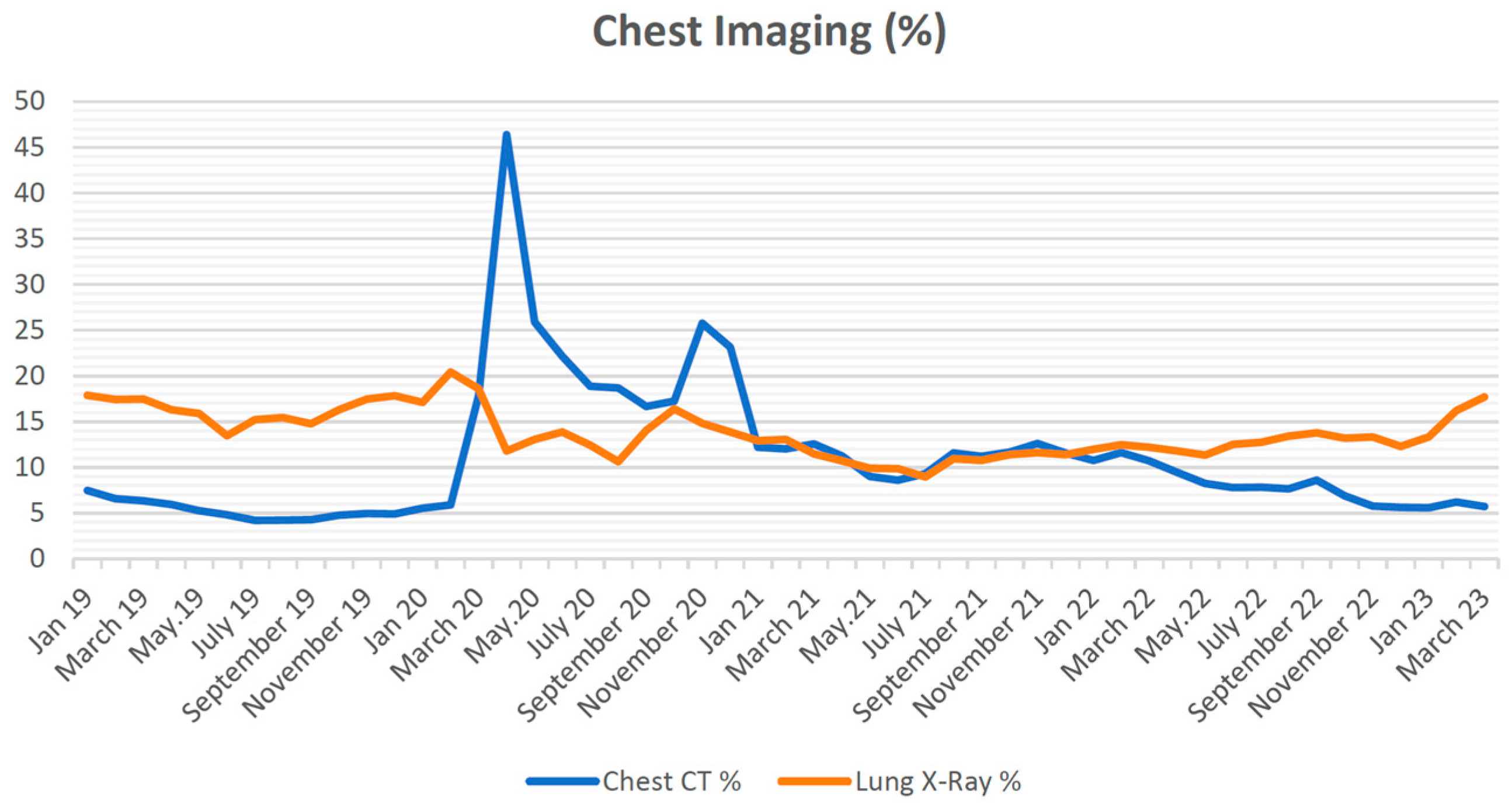
| CXR (%) | 16.6 ± 1.7 | 12.4 ±2.1 | 13.3 ± 1.9 | <0.001 |
| CCT (%) | 4.9 ± 0.9 | 15.9 ± 8.1 | 7.46 ± 1.2 | <0.001 |
| CXR Female (%) | 15.3 ± 1.7 | 10.9 ± 2.3 | 11.6 ± 2.1 | <0.001 |
| CXR Male (%) | 18.1 ± 1.8 | 13.8 ± 2.1 | 15.2 ± 2.0 | <0.001 |
| CCT Female (%) | 4.8 ± 1.0 | 14.8 ± 7.9 | 5.7 ± 1.0 | <0.001 |
| CCT Male (%) | 5.0 ± 0.9 | 17.0 ± 8.1 | 9.42 ± 1.7 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arıkan, C.; Bora, E.S.; Kanter, E.; Karaarslan, F.N. Have Chest Imaging Habits Changed in the Emergency Department after the Pandemic? Tomography 2023, 9, 2079-2088. https://doi.org/10.3390/tomography9060163
Arıkan C, Bora ES, Kanter E, Karaarslan FN. Have Chest Imaging Habits Changed in the Emergency Department after the Pandemic? Tomography. 2023; 9(6):2079-2088. https://doi.org/10.3390/tomography9060163
Chicago/Turabian StyleArıkan, Cüneyt, Ejder Saylav Bora, Efe Kanter, and Fatma Nur Karaarslan. 2023. "Have Chest Imaging Habits Changed in the Emergency Department after the Pandemic?" Tomography 9, no. 6: 2079-2088. https://doi.org/10.3390/tomography9060163
APA StyleArıkan, C., Bora, E. S., Kanter, E., & Karaarslan, F. N. (2023). Have Chest Imaging Habits Changed in the Emergency Department after the Pandemic? Tomography, 9(6), 2079-2088. https://doi.org/10.3390/tomography9060163









