Cone-Beam Computerized Tomography Evaluation of the Relationship between Orthodontic Vertical Direction Parameters and the Distance from the Apex of the Upper Central Tooth to the Nasal Floor and Anterior Nasal Spine
Abstract
1. Introduction
2. Materials and Methods
2.1. Cephalometric Measurements
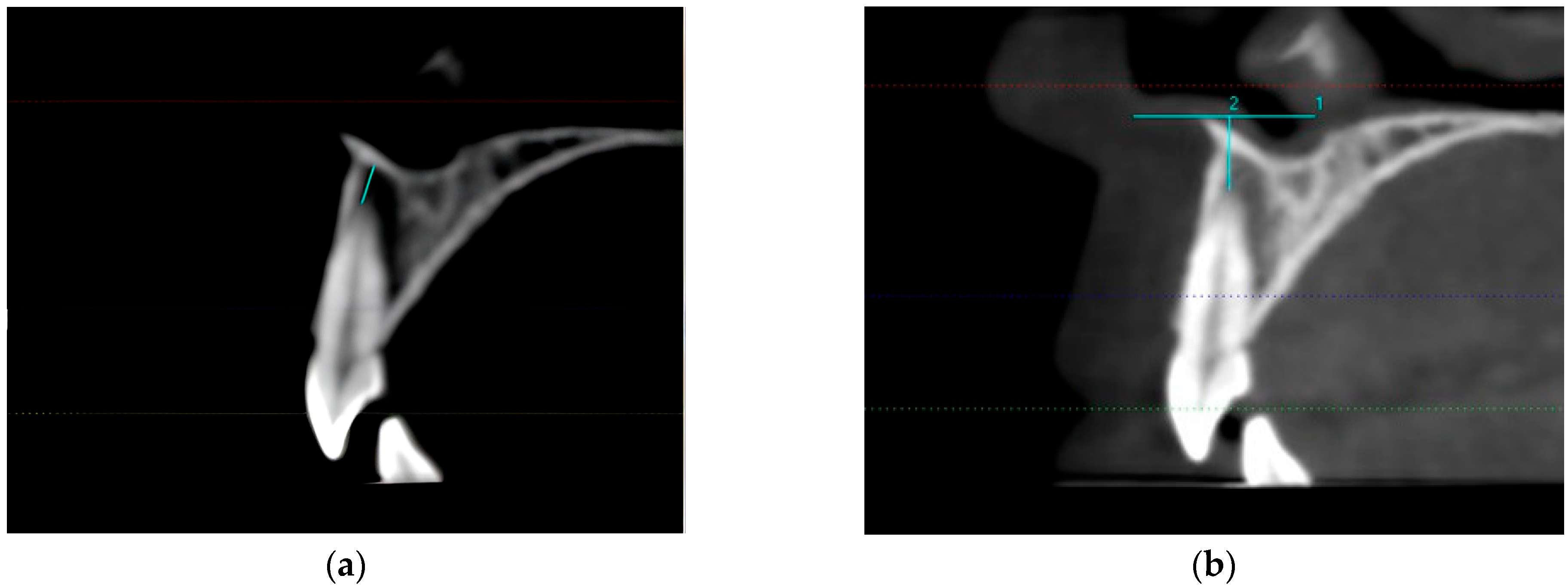
2.2. CBCT Measurements
2.3. Statistical Analysis
3. Results
3.1. Relationship between NF-U1A and Cephalometric Measurements
3.2. Relationship between ANS-U1A and Cephalometric Measurements
3.3. Evaluation of ANS-U1A and NF-U1A Measurements According to ANS-Me Value
3.4. Evaluation of ANS-U1A and NF-U1A Measurements According to ANS-Gn Value
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kiełczykowsk, M.; Kamiński, K.; Perkowski, K.; Zadurska, M.; Czochrowska, E. Application of Artificial Intelligence (AI) in a Cephalometric Analysis: A Narrative Review. Diagnostics 2023, 13, 2640. [Google Scholar] [CrossRef] [PubMed]
- Devereux, L.; Moles, D.; Cunningham, S.J.; McKnight, M. How important are lateral cephalometric radiographs in orthodontic treatment planning? Am. J. Orthod. Dentofac. Orthop. 2011, 139, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, A.K.; Chen, Y.; Almalki, A.; Sivamurthy, G.; Kafle, D. Cephalometric Analysis in Orthodontics Using Artificial Intelligence-A Comprehensive Review. Biomed. Res. Int. 2022, 2022, 1880113. [Google Scholar] [CrossRef] [PubMed]
- Sherwood, R.J.; Oh, H.S.; Valiathan, M.; McNulty, K.P.; Duren, D.L.; Knigge, R.P.; Hardin, A.M.; Holzhauser, C.L.; Middleton, K.M. Bayesian approach to longitudinal craniofacial growth: The Craniofacial Growth Consortium Study. Anat. Rec. 2021, 304, 991–1019. [Google Scholar] [CrossRef] [PubMed]
- Rai, S.; Saidath, K.; Mathew, K.A.; Shetty, S.S. Assessment and comparison of cranial base morphology in individuals with long face and short face. J. Orthod. Sci. 2023, 12, 30. [Google Scholar] [PubMed]
- McNamara, J.J. A method of cephalometric evaluation. Am. J. Orthod. 1984, 86, 449–469. [Google Scholar] [CrossRef] [PubMed]
- Rajak, R.R.K.; Shrestha, R.M.; Koju, S. Reliability of Panoramic Radiography in Assessing Gonial Angle Compared to Lateral Cephalogram in Patients with Class I Malocclusion. Taiwan J. Orthod. 2021, 33, 53–59. [Google Scholar] [CrossRef]
- Latif, V.B.; Keshavaraj; Rai, R.; Hegde, G.; Shajahan, S. Assessment of Antero-Posterior Skeletal and Soft Tissue Relationships of Adult Indian Subjects in Natural Head Position and Centric Relation. J. Int. Oral Health 2015, 7, 41–47. [Google Scholar]
- Novruzov, Z.; Uslu, O. Distribution and evaluation of the mandibular rotation model according to the sagittal maxillomandibular position. J. AU Fac. Dent. 2006, 33, 11–16. [Google Scholar]
- Albarakati, S.F.; Kula, K.S.; Ghoneima, A.A. The reliability and reproducibility of cephalometric measurements: A comparison of conventional and digital methods. Dento Maxillo Facial Radiol. 2012, 41, 11–17. [Google Scholar] [CrossRef]
- Kim, T.K.; Jeong, J.Y. Surgical anatomy for Asian rhinoplasty: Part II. Arch. Craniofac Surg. 2020, 21, 143–155. [Google Scholar] [CrossRef]
- Abdelkarim, A. Cone-Beam Computed Tomography in Orthodontics. Dent. J. 2019, 7, 89. [Google Scholar] [CrossRef] [PubMed]
- Korbmacher, H.; Kahl-Nieke, B.; Schollchen, M.; Heiland, M. Value of two cone-beam computed tomography systems from an orthodontic point of view. J. Orofac. Orthop. 2007, 68, 278–289. [Google Scholar] [CrossRef] [PubMed]
- Aboudara, C.A.; Hatcher, D.; Nielsen, I.L.; Miller, A. A three-dimensional evaluation of the upper airway in adolescents. Orthod. Craniofac. Res. 2003, 6, 173–175. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, T.; Enciso, R.; Memon, A.; Mah, J.K.; Clark, G.T. Evaluation of 3D airway imaging of obstructive sleep apnea with cone-beam computed tomography. Stud. Health Technol. Inform. 2005, 111, 365–368. [Google Scholar] [PubMed]
- Enciso, R.; Nguyen, M.; Shigeta, Y.; Ogawa, T.; Clark, G.T. Comparison of cone-beam CT parameters and sleep questionnaires in sleep apnea patients and control subjects. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Schendel, S.A.; Hatcher, D. Automated 3-dimensional airway analysis from cone-beam computed tomography data. J. Oral Maxillofac. Surg. 2010, 68, 696–701. [Google Scholar] [CrossRef]
- El, A.S.; El, H.; Palomo, J.M.; Baur, D.A. A 3-dimensional airway analysis of an obstructive sleep apnea surgical correction with cone beam computed tomography. J. Oral Maxillofac. Surg. 2011, 69, 2424–2436. [Google Scholar] [CrossRef]
- Schendel, S.; Powell, N.; Jacobson, R. Maxillary, mandibular, and chin advancement: Treatment planning based on airway anatomy in obstructive sleep apnea. J. Oral Maxillofac. Surg. 2011, 69, 663–676. [Google Scholar] [CrossRef]
- Applegate, K.E.; Thomas, K. Pediatric CT—The challenge of dose records. Pediatr. Radiol. 2011, 41, 523–527. [Google Scholar] [CrossRef]
- Hans, M.G.; Palomo, J.M.; Valiathan, M. History of imaging in orthodontics from Broadbent to cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Kamburoglu, K. Use of dentomaxillofacial cone beam computed tomography in dentistry. World J. Radiol. 2015, 7, 128–130. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Oh, S.H.; Kim, S.H.; Ahn, H.W.; Kang, Y.G.; Choi, Y.S.; Kook, Y.A.; Nelson, G. Effectiveness of 2D radiographs in detecting CBCT-based incidental findings in orthodontic patients. Sci. Rep. 2021, 11, 9280. [Google Scholar] [CrossRef] [PubMed]
- Nahoum, H.I. Vertical proportions and the palatal plan in anterior openbite. Am. J. Orthod. 1971, 59, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Gürsoy, N.; Uğur, T.; Gürsoy, S. Investigation of cephalometric norms in Turks with normal closure. Istanb. Univ. J. Dent. 1973, 7, 333–343. [Google Scholar]
- Iyer, V.S.; Lutz, W. Cephalometric comparison of Indian and English facial profiles. Am. J. Phys. Anthropol. 1966, 24, 117–126. [Google Scholar] [CrossRef]
- Ricketts, R.M. Planning treatment on the Basis of the facial pattern and an estimate of its growth. Angle Orthod. 1957, 27, 14–37. [Google Scholar]
- Celebi, A.A.; Tan, E.; Gelgor, İ.E.; Colak, T.; Ayyildiz, E. Comparison of Soft Tissue Cephalometric Norms between Turkish and European-American Adults. Sci. World J. 2013, 2013, 806203. [Google Scholar] [CrossRef]
- Pamukcu, H.; Tunçer, N.İ.; Pelin, İ.C.; Zengin, H.Y. Cephalometric Mandibular Dimensions in Growing Turkish Children: Trends of Change, Sex-Specific Differences, and Comparisons with Published Norms. Turk. J. Orthod. 2022, 35, 198–206. [Google Scholar] [CrossRef]
- Işımer, Y.; Uzel, İ.; Sağdıç, D. Comparison of neutral occlusion norms with Björk norms in our society. Turk. J. Orthod. 1990, 3, 65–71. [Google Scholar] [CrossRef]
- Björk, A. Measurement on radiographs. J. Dent. Res. 1962, 41, 672–680. [Google Scholar] [CrossRef] [PubMed]
- Tsunori, M.; Mashita, M.; Kasai, K. Relationship between facial types and tooth and bone characteristics of the mandible obtained by CT scanning. Angle Orthod. 1998, 68, 557–562. [Google Scholar] [PubMed]
- Ligthelm-Bakker, A.S.W.M.R.; Wattel, E.; Uljee, I.H.; Prahl-Andersen, B. Vertical growth of the anterior face: A new approach. Am. J. Orthod. Dentofac. Orthop. 1992, 101, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Janson, G.R.P.; Metaxas, A.; Woodside, D.G. Variation in maxillary and mandibular molar and incisor vertical dimension in 12-year-old subjects with excess, normal, and short lower anterior face height. Am. J. Orthod. Dentofac. Orthop. 1994, 106, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Riedel, R.A. Esthetics and its relation to orthodontic therapy. Angle Orthod. 1950, 20, 168–178. [Google Scholar] [PubMed]
- Rains, M.D.; Nanda, R. Soft-tissue changes associated with maxillary incisor retraction. Am. J. Orthod. 1982, 81, 481–488. [Google Scholar] [CrossRef]
- Arnett, G.W.; Bergman, R.T. Facial keys to orthodontic diagnosis and treatment planning. Part I. Am. J. Orthod. 1993, 103, 299–312. [Google Scholar] [CrossRef]
- Kokich, V. Esthetics and anterior tooth position: An orthodontic perspective part III: Mediolateral relationships. J. Esthet. Restor. Dent. 1993, 5, 200–207. [Google Scholar] [CrossRef]
- Sarver, D.M. The importance of incisor positioning in the esthetic smile: The smile arc. Am. J. Orthod. 2001, 120, 98–111. [Google Scholar] [CrossRef]
- Cho, E.A.; Kim, S.J.; Choi, Y.J.; Kyung, K.H.; Chung, C.J. of the incisive canal and its proximity to the maxillary central incisors using computed tomography images. Angle Orthod. 2016, 86, 571–576. [Google Scholar] [CrossRef]
- Uslu Akçam, Ö.; Novruzov, Z. Investıgatıon of Cephalometrıc Angles Used in Vertıcal Facıal Classıfıcatıon. Gazi Üniv. Diş. Hekim. Fak. Derg. 2011, 28, 17–22. [Google Scholar]
- Gracco, A.; Lombardo, L.; Mancuso, G.; Gravina, V.; Siciliani, G. Upper incisor position and bony support in untreated patients as seen on CBCT. Angle Orthod. 2009, 79, 692–702. [Google Scholar] [CrossRef] [PubMed]
- Sadek, M.M.; Sabet, N.E.; Hassan, I.T. Alveolar bone mapping in subjects with different vertical facial dimensions. Eur. J. Orthod. 2015, 37, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Enoki, C.; Telles, C.D.S.; Matsumoto, M.A.N. Dental-skeletal dimensions in growing individuals with variations in the lower facial height. Braz. Dent. J. 2004, 15, 68–74. [Google Scholar] [CrossRef]
- Guo, R.; Tian, Y.; Li, X.; Sun, Y. Facial profile evaluation and prediction of skeletal class II patients during camouflage extraction treatment: A pilot study. Head Face Med. 2023, 19, 51. [Google Scholar] [CrossRef]
- Jain, A.D.; Goyal, M.; Kumar, M.; Premsagar, S.; Mishra, S.; Tomar, S. Evaluating the Lower Anterior Facial Height in Patients Treated with Extraction Versus Non-extraction Fixed Mechanotherapy: “A Systematic Review and Meta-analysis”. J. Indian Orthod. Soc. 2021, 55, 355–366. [Google Scholar] [CrossRef]
- Deoghare, A.M.; Akhare, P.; Patil, R.; Shinh, A.S. Comparison of Incisor, Molar and Anterior Facial Height in Normal, Angle Class II Division 1 and Class III Malocclusion: A Cephalometric Study. J. Indian Orthod. Soc. 2012, 46, 304–307. [Google Scholar] [CrossRef]

| Vertical Direction Parameters | NF-U1A r p | ANS-U1A r p |
|---|---|---|
| N−S−AR | −0.065 0.476 | 0.017 0.853 |
| S−Ar−Go | 0.030 0.740 | −0.068 0.458 |
| Ar−Go−Me | 0.099 0.278 | 0.287 0.001 ** |
| Sum of posterior angles | 0.098 0.284 | 0.311 0.001 ** |
| N−Me | 0.547 0.001 ** | 0.384 0.001 ** |
| S−Go | 0.372 0.001 ** | 0.131 0.150 |
| SN/GoGn | 0.064 0.484 | 0.297 0.001 ** |
| N−ANS | 0.338 0.001 ** | 0.079 0.388 |
| ANS−Me | 0.585 0.001 ** | 0.534 0.001 ** |
| ANS−Gn | 0.611 0.001 ** | 0.531 0.001 ** |
| Y−axis angle | 0.219 0.015 * | 0.311 0.001 ** |
| SN−OcP | −0.163 0.073 | 0.082 0.369 |
| Female (n = 90) | Male (n = 32) | p | ||
|---|---|---|---|---|
| NF-UA1 distance (mm) | Mean ± Sd | 5.57 ± 2.37 | 6.14 ± 2.27 | a 0.243 |
| Min–Max | 1.1–11.4 | 2.1–11.1 | ||
| ANS-UA1 distance (mm) | Mean ± Sd | 5.93 ± 2.27 | 5.62 ± 2.53 | a 0.516 |
| Min–Max | 1–11 | 1.5–12.2 |
| Level | n | % | |
|---|---|---|---|
| ANS-Me | Decreased (≤63.9) | 66 | 54.1 |
| Normal (64–74.9) | 49 | 40.2 | |
| Increased (≥75) | 7 | 5.7 | |
| ANS-Gn | Decreased (≤63.9) | 76 | 62.3 |
| Normal (64–72.9) | 36 | 29.5 | |
| Increased (≥73) | 10 | 8.2 | |
| Y-Axis Angle | Decreased (≤52.9) | 3 | 2.4 |
| Normal (53–66.9) | 100 | 82 | |
| Increased (≥67) | 19 | 15.6 |
| ANS-Me Level | NF-U1A | ANS-U1A | |
|---|---|---|---|
| Decreased (≤63.9) | n | 66 | 66 |
| Min–max | 1.1–10.1 | 1.5–10 | |
| Mn ± SD | 4.57 ± 1.84 | 4.86 ± 1.91 | |
| Normal (64–74.9) | n | 49 | 49 |
| Min–max | 2.2–11.4 | 1–11 | |
| Mn ± SD | 6.94 ± 2.13 | 6.80 ± 2.15 | |
| Increased (≥75) | n | 7 | 7 |
| Min–max (median) | 5.5–10.8 | 5–12.2 | |
| Mn ± SD | 8.06 ± 2.35 | 8.54 ± 2.70 | |
| a p | 0.001 ** | 0.001 ** | |
| ANS-Gn Level | NF-U1A | ANS-U1A | |
|---|---|---|---|
| Decreased (≤63.9) | n | 76 | 76 |
| Min–max | 1.1–9.3 | 1.5–10 | |
| Mn ± SD | 4.76 ± 1.88 | 5.01 ± 1.88 | |
| Norm (64–72.9) | n | 36 | 36 |
| Min–max | 2.2–11.4 | 1–11 | |
| Mn ± SD | 7.03 ± 2.19 | 7.00 ± 2.36 | |
| Increased (≥73) | n | 10 | 10 |
| Min–Max | 5.5–10.8 | 5–12.2 | |
| Mn ± Sd | 8.30 ± 2.08 | 8.11 ± 2.33 | |
| a p | 0.001 ** | 0.001 ** | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Çınarsoy Ciğerim, S.; Sezen Erhamza, T. Cone-Beam Computerized Tomography Evaluation of the Relationship between Orthodontic Vertical Direction Parameters and the Distance from the Apex of the Upper Central Tooth to the Nasal Floor and Anterior Nasal Spine. Tomography 2024, 10, 37-46. https://doi.org/10.3390/tomography10010004
Çınarsoy Ciğerim S, Sezen Erhamza T. Cone-Beam Computerized Tomography Evaluation of the Relationship between Orthodontic Vertical Direction Parameters and the Distance from the Apex of the Upper Central Tooth to the Nasal Floor and Anterior Nasal Spine. Tomography. 2024; 10(1):37-46. https://doi.org/10.3390/tomography10010004
Chicago/Turabian StyleÇınarsoy Ciğerim, Saadet, and Türkan Sezen Erhamza. 2024. "Cone-Beam Computerized Tomography Evaluation of the Relationship between Orthodontic Vertical Direction Parameters and the Distance from the Apex of the Upper Central Tooth to the Nasal Floor and Anterior Nasal Spine" Tomography 10, no. 1: 37-46. https://doi.org/10.3390/tomography10010004
APA StyleÇınarsoy Ciğerim, S., & Sezen Erhamza, T. (2024). Cone-Beam Computerized Tomography Evaluation of the Relationship between Orthodontic Vertical Direction Parameters and the Distance from the Apex of the Upper Central Tooth to the Nasal Floor and Anterior Nasal Spine. Tomography, 10(1), 37-46. https://doi.org/10.3390/tomography10010004




