Effect of Immediate Dentin Sealing on the Bonding Performance of Indirect Restorations: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Eligibility Criteria
2.3. Screening and Selection
2.4. Data Extraction
2.5. Risk of Bias (RoB) Assessment
2.6. Inter-Rater Reliability (IRR)
3. Results
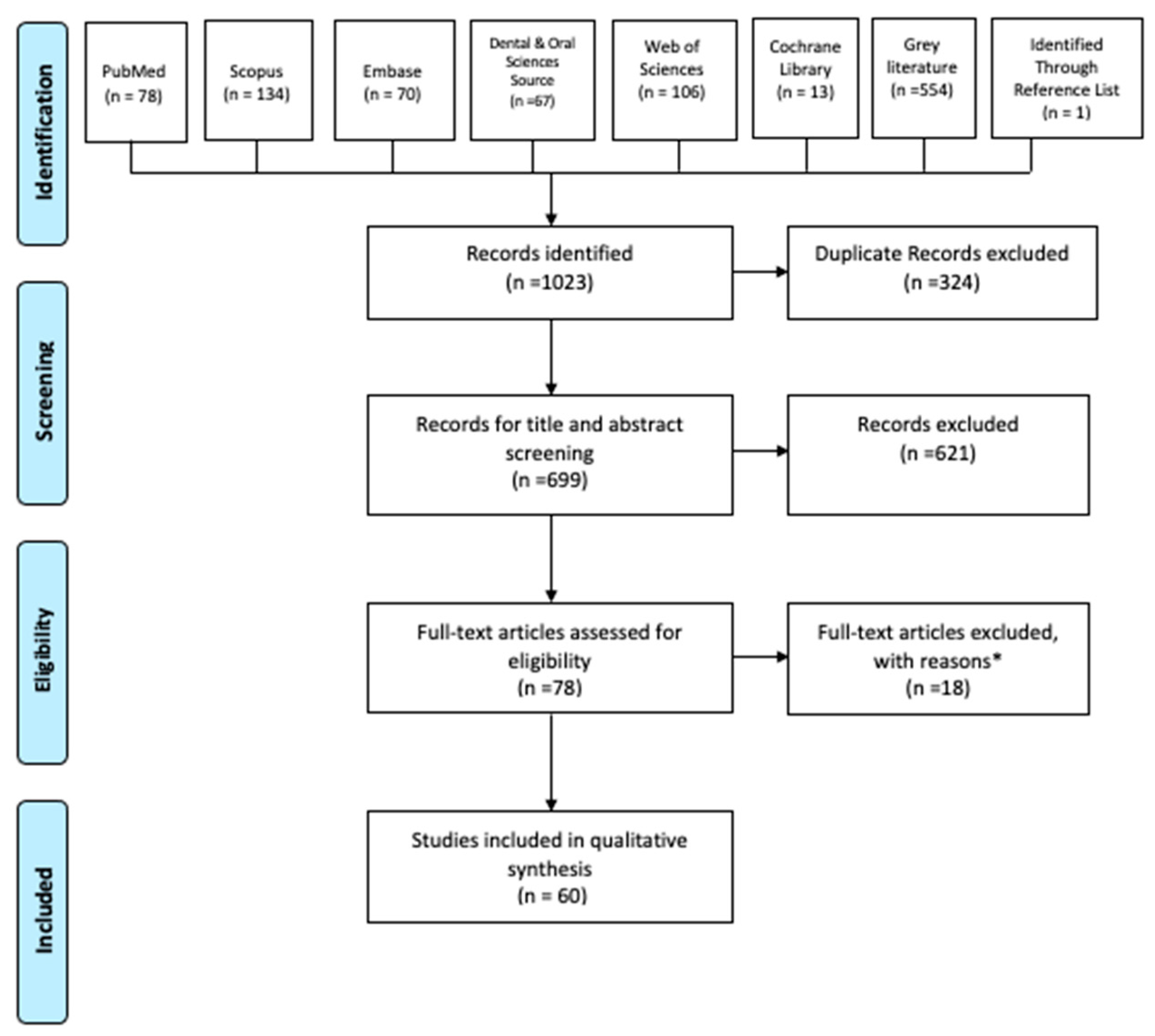
3.1. Search and Selection
3.2. Risk of Bias (RoB) Test of the Studies in the Systematic Review
3.3. Inter-Rater Reliability Results
4. Discussion
4.1. Effect of Dentin Bonding Agents and Flowable Resin-based Composites
4.2. Effect of Impression Materials
4.3. Effect of Temporary Materials and Conditioning Methods
4.4. Effect of Resin Cement
4.5. Bonding Efficiency to Different Restorative Materials and Preparation Types
4.6. Effect of Aging Conditions
4.7. Study Limitations
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Spohr, A.M.; Borges, G.A.; Platt, J.A. Thickness of immediate dentin sealing materials and its effect on the fracture load of a reinforced all-ceramic crown. Eur. J. Dent. 2013, 7, 474–483. [Google Scholar] [CrossRef] [PubMed]
- Cohen, R.G.; Razzano, M.V. Immediate dentin sealing using an antibacterial self-etching bonding system. Pract. Proced. Aesthet. Dent. 2006, 18, 561–565. [Google Scholar] [PubMed]
- Pashley, E.L.; Comer, R.W.; Simpson, M.D.; Horner, J.A.; Pashley, D.H.; Caughman, W.F. Dentin permeability: Sealing the dentin in crown preparations. Oper. Dent. 1992, 17, 13–20. [Google Scholar]
- Paul, S.J.; Schärer, P. The dual bonding technique: A modified method to improve adhesive luting procedures. Int. J. Periodontics Restorative Dent. 1997, 17, 536–545. [Google Scholar]
- Nikaido, T.; Tagami, J.; Yatani, H.; Ohkubo, C.; Nihei, T.; Koizumi, H.; Maseki, T.; Nishiyama, Y.; Takigawa, T.; Tsubota, Y. Concept and clinical application of the resin-coating technique for indirect restorations. Dent. Mater. J. 2018, 37, 192–196. [Google Scholar] [CrossRef]
- Nikaido, T.; Inoue, G.; Takagaki, T.; Takahashi, R.; Sadr, A.; Tagami, J. Resin Coating Technique for Protection of Pulp and Increasing Bonding in Indirect Restoration. Curr. Oral Health Rep. 2015, 2, 81–86. [Google Scholar] [CrossRef]
- Dillenburg, A.L.; Soares, C.G.; Paranhos, M.P.; Spohr, A.M.; Loguercio, A.D.; Burnett Jr, L.H. Microtensile bond strength of prehybridized dentin: Storage time and surface treatment effects. J. Adhes. Dent. 2009, 11, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Magne, P. Immediate dentin sealing: A fundamental procedure for indirect bonded restorations. J. Esthet. Restor. Dent. 2005, 17, 144–154. [Google Scholar] [CrossRef]
- Magne, P.; Nielsen, B. Interactions between impression materials and immediate dentin sealing. J. Prosthet. Dent. 2009, 102, 298–305. [Google Scholar] [CrossRef]
- El Mourad, A.M. Assessment of Bonding Effectiveness of Adhesive Materials to Tooth Structure using Bond Strength Test Methods: A Review of Literature. Open Dent. J. 2018, 12, 664–678. [Google Scholar] [CrossRef]
- Bertschinger, C.; Paul, S.J.; Lüthy, H.; Schärer, P. Dual application of dentin bonding agents: Its effect on the bond strength. Am. J. Dent. 1996, 9, 115–119. [Google Scholar] [PubMed]
- Paul, S.J.; Schaerer, P. Effect of provisional cements on the bond strength of various adhesive bonding systems on dentine. J. Oral Rehabil. 1997, 24, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Page, M.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Hardan, L.; Devoto, W.; Bourgi, R.; Cuevas-Suárez, C.E.; Lukomska-Szymanska, M.; Fernández-Barrera, M.Á.; Cornejo-Ríos, E.; Monteiro, P.; Zarow, M.; Jakubowicz, N.; et al. Immediate dentin sealing for adhesive cementation of indirect restorations: A systematic review and meta-analysis. Gels 2022, 8, 175. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.; Lang, S.; Mante, F.; Pavelić, K.; Ozer, F. Antimicrobial and Mechanical Effects of Zeolite Use in Dental Materials: A Systematic Review. Acta Stomatol. Croat. 2021, 55, 76–89. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Medica 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Magne, P.; Kim, T.H.; Cascione, D.; Donovan, T.E. Immediate dentin sealing improves bond strength of indirect restorations. J. Prosthet. Dent. 2005, 94, 511–519. [Google Scholar] [CrossRef]
- Magne, P.; So, W.S.; Cascione, D. Immediate dentin sealing supports delayed restoration placement. J. Prosthet. Dent. 2007, 98, 166–174. [Google Scholar] [CrossRef]
- Duarte, S.; de Freitas, C.R.; Saad, J.R.; Sadan, A. The effect of immediate dentin sealing on the marginal adaptation and bond strengths of total-etch and self-etch adhesives. J. Prosthet. Dent. 2009, 102, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jayasooriya, P.R.; Pereira, P.N.; Nikaido, T.; Tagami, J. Efficacy of a resin coating on bond strengths of resin cement to dentin. J. Esthet. Restor. Dent. 2003, 15, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Nikaido, T.; Nakaoki, Y.; Ogata, M.; Foxton, R.; Tagami, J. The resin-coating technique. Effect of a single-step bonding system on dentin bond strengths. J. Adhes. Dent. 2003, 5, 293–300. [Google Scholar]
- Islam, M.R.; Takada, T.; Weerasinghe, D.S.; Uzzaman, M.A.; Foxton, R.M.; Nikaido, T.; Tagami, J. Effect of resin coating on adhesion of composite crown restoration. Dent. Mater. J. 2006, 25, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Okuda, M.; Nikaido, T.; Maruoka, R.; Foxton, R.M.; Tagami, J. Microtensile bond strengths to cavity floor dentin in indirect composite restorations using resin coating. J. Esthet. Restor. Dent. 2007, 19, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Sultana, S.; Nikaido, T.; Matin, K.; Ogata, M.; Foxton, R.M.; Tagami, J. Effect of resin coating on dentin bonding of resin cement in Class II cavities. Dent. Mater. J. 2007, 26, 506–513. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Frankenberger, R.; Lohbauer, U.; Taschner, M.; Petschelt, A.; Nikolaenko, S.A. Adhesive luting revisited: Influence of adhesive, temporary cement, cavity cleaning, and curing mode on internal dentin bond strength. J. Adhes. Dent. 2007, 9, 269–273. [Google Scholar] [PubMed]
- de Andrade, O.S.; de Goes, M.F.; Montes, M.A. Marginal adaptation and microtensile bond strength of composite indirect restorations bonded to dentin treated with adhesive and low-viscosity composite. Dent. Mater. 2007, 23, 279–287. [Google Scholar] [CrossRef]
- Ariyoshi, M.; Nikaido, T.; Foxton, R.M.; Tagami, J. Microtensile bond strengths of composite cores to pulpal floor dentin with resin coating. Dent. Mater. J. 2008, 27, 400–407. [Google Scholar] [CrossRef]
- Nikaido, T.; Kitasako, Y.; Burrow, M.F.; Umino, A.; Maruoka, R.; Ikeda, M.; Tagami, J. Effect of resin coating on dentin bond durability of a resin cement over 1 year. Am J Dent. 2008, 21, 64–68. [Google Scholar]
- Kameyama, A.; Oishi, T.; Sugawara, T.; Hirai, Y. Microtensile bond strength of indirect resin composite to resin-coated dentin: Interaction between diamond bur roughness and coating material. Bull Tokyo Dent Coll. 2009, 50, 13–22. [Google Scholar] [CrossRef][Green Version]
- Kitayama, S.; Pilecki, P.; Nasser, N.A.; Bravis, T.; Wilson, R.F.; Nikaido, T.; Tagami, J.; Watson, T.F.; Foxton, R.M. Effect of resin coating on adhesion and microleakage of computer-aided design/computer-aided manufacturing fabricated all-ceramic crowns after occlusal loading: A laboratory study. Eur. J. Oral. Sci. 2009, 117, 454–462. [Google Scholar] [CrossRef]
- Takahashi, R.; Nikaido, T.; Ariyoshi, M.; Foxton, R.M.; Tagami, J. Microtensile bond strengths of a dual-cure resin cement to dentin resin-coated with an all-in-one adhesive system using two curing modes. Dent. Mater. J. 2010, 29, 268–276. [Google Scholar] [CrossRef]
- Feitosa, V.P.; Medina, A.D.; Puppin-Rontani, R.M.; Correr-Sobrinho, L.; Sinhoreti, M.A.C. Effect of resin coat technique on bond strength of indirect restorations after thermal and load cycling. Bull. Tokyo Dent. Coll. 2010, 51, 111–118. [Google Scholar] [CrossRef]
- Duque, A. Influence of Immediate Dentin Sealing on the Bond Strength of Indirect Bonded Restorations. Master’s Thesis, Nova Southeastern University, Fort Lauderdale, FL, USA, 2014. [Google Scholar]
- Giannini, M.; Takagaki, T.; Bacelar-Sá, R.; Vermelho, P.M.; Ambrosano, G.M.B.; Sadr, A.; Nikaido, T.; Tagami, J. Influence of resin coating on bond strength of self-adhesive resin cements to dentin. Dent. Mater. J. 2015, 34, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Santana, V.B.; de Alexandre, R.S.; Rodrigues, J.A.; Ely, C.; Reis, A.F. Effects of Immediate Dentin Sealing and Pulpal Pressure on Resin Cement Bond Strength and Nanoleakage. Oper. Dent. 2016, 41, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, C.J.R.; Gonçalves, I.C.S.; Botelho, M.P.J.; Guiraldo, R.D.; Lopes, M.B.; Júnior, A.G. Interactions between resin-based temporary materials and immediate dentin sealing. Appl. Adhes. Sci. 2016, 4, 1–9. [Google Scholar] [CrossRef]
- Brigagão, V.C.; Barreto, L.F.D.; Gonçalves, K.A.S.; Amaral, M.; Vitti, R.P.; Neves, A.C.; Silva-Concílio, L.R. Effect of interim cement application on bond strength between resin cements and dentin: Immediate and delayed dentin sealing. J. Prosthet. Dent. 2017, 117, 792–798. [Google Scholar] [CrossRef] [PubMed]
- Ishii, N.; Maseki, T.; Nara, Y. Bonding state of metal-free CAD/CAM onlay restoration after cyclic loading with and without immediate dentin sealing. Dent. Mater. J. 2017, 36, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-Filho, R.C.; Ely, C.; Amaral, R.C.; Rodrigues, J.A.; Roulet, J.F.; Cassoni, A.; Reis, A.F. Effect of Different Adhesive Systems Used for Immediate Dentin Sealing on Bond Strength of a Self-Adhesive Resin Cement to Dentin. Oper. Dent. 2018, 43, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Hironaka, N.G.L.; Ubaldini, A.L.M.; Sato, F.; Giannini, M.; Terada, R.S.; Pascotto, R.C. Influence of immediate dentin sealing and interim cementation on the adhesion of indirect restorations with dual-polymerizing resin cement. J. Prosthet. Dent. 2018, 119, 678.e1–678.e8. [Google Scholar] [CrossRef] [PubMed]
- Murata, T.; Maseki, T.; Nara, Y. Effect of immediate dentin sealing applications on bonding of CAD/CAM ceramic onlay restoration. Dent. Mater. J. 2018, 37, 928–939. [Google Scholar] [CrossRef]
- van den Breemer, C.R.G.; Özcan, M.; Cune, M.S.; Ayres, A.A.; Van Meerbeek, B.; Gresnigt, M. Effect of Immediate Dentin Sealing and Surface Conditioning on the Microtensile Bond Strength of Resin-based Composite to Dentin. Oper. Dent. 2019, 44, e289–e298. [Google Scholar] [CrossRef] [PubMed]
- Akehashi, S.; Takahashi, R.; Nikaido, T.; Burrow, M.F.; Tagami, J. Enhancement of dentin bond strength of resin cement using new resin coating materials. Dent. Mater. J. 2019, 38, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, K.; Maeno, M.; Nara, Y. Influence of immediate dentin sealing and temporary restoration on the bonding of CAD/CAM ceramic crown restoration. Dent. Mater. J. 2019, 38, 970–980. [Google Scholar] [CrossRef] [PubMed]
- Rozan, S.; Takahashi, R.; Nikaido, T.; Tichy, A.; Tagami, J. CAD/CAM-fabricated inlay restorations: Can the resin-coating technique improve bond strength and internal adaptation? Dent. Mater. J. 2020, 39, 941–949. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, M.A.; Lazari-Carvalho, P.C.; Polonial, I.F.; de Souza, J.B.; Magne, P. Significance of immediate dentin sealing and flowable resin coating reinforcement for unfilled/lightly filled adhesive systems. J. Esthet. Restor. Dent. 2021, 33, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Oda, Y.; Takahashi, R.; Nikaido, T.; Tagami, J. Influence of the resin-coating technique on the bonding performance of self-adhesive resin cements in single-visit computer-aided design/computer-aided manufacturing resin restorations. J. Esthet. Restor. Dent. 2022, 34, 721–728. [Google Scholar] [CrossRef]
- Gailani, H.F.A.; Benavides-Reyes, C.; Bolaños-Carmona, M.V.; Rosel-Gallardo, E.; González-Villafranca, P.; González-López, S. Effect of Two Immediate Dentin Sealing Approaches on Bond Strength of Lava™ CAD/CAM Indirect Restoration. Materials 2021, 14, 1629. [Google Scholar] [CrossRef]
- Abo-Alazm, E.A.E.; Safy, R.K. Impact of Immediate Dentin Sealing Using Universal Adhesive under Simulated Pulp Pressure on Microtensile Bond Strength of Indirect Resin Composite Restorations and Dentin Permeability. Eur. J. Dent. 2022, 16, 536–542. [Google Scholar] [CrossRef]
- Abdou, A.; Takahashi, R.; Saad, A.; Nozaki, K.; Nikaido, T.; Tagami, J. Influence of resin-coating on bond strength of resin cements to dentin and CAD/CAM resin block in single-visit and multiple-visit treatment. Dent. Mater. J. 2021, 40, 674–682. [Google Scholar] [CrossRef]
- Nakazawa, M.; Maeno, M.; Komoto, M.; Nara, Y. Appropriate Immediate Dentin Sealing to Improve the Bonding of CAD/CAM Ceramic Crown Restorations. Polymers 2022, 14, 4541. [Google Scholar] [CrossRef]
- Sooksang, O.; Wanachantararak, S.; Sukapattee, M. Effects of single and double application of immediate dentin sealing techniques on marginal leakage and microtensile bond strength of resin cement. J. Int. Dent. Med. Res. 2023, 16, 542–548. [Google Scholar]
- Kimyai, S.; Bahari, M.; Abed-Kahnamouei, M.; Ebrahimi-Chaharom, M.E.; Asl-Oskouei, M.H. Effect of different application strategies of universal adhesive used for immediate and delayed dentin sealing on the microtensile bond strength of self-adhesive resin cement to dentin with and without aging. J. Clin. Exp. Dent. 2023, 15, e210. [Google Scholar] [CrossRef]
- Erkut, S.; Küçükesmen, H.C.; Eminkahyagil, N.; Imirzalioglu, P.; Karabulut, E. Influence of previous provisional cementation on the bond strength between two definitive resin-based luting and dentin bonding agents and human dentin. Oper. Dent. 2007, 32, 84–93. [Google Scholar] [CrossRef]
- Lee, J.I.; Park, S.H. The effect of three variables on shear bond strength when luting a resin inlay to dentin. Oper. Dent. 2009, 34, 288–292. [Google Scholar] [CrossRef]
- Choi, Y.S.; Cho, I.H. An effect of immediate dentin sealing on the shear bond strength of resin cement to porcelain restoration. J. Adv. Prosthodont. 2010, 2, 39–45. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sailer, I.; Oendra, A.E.; Stawarczyk, B.; Hämmerle, C.H. The effects of desensitizing resin, resin sealing, and provisional cement on the bond strength of dentin luted with self-adhesive and conventional resin cements. J. Prosthet. Dent. 2012, 107, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Dalby, R.; Ellakwa, A.; Millar, B.; Martin, F.E. Influence of immediate dentin sealing on the shear bond strength of pressed ceramic luted to dentin with self-etch resin cement. Int. J. Dent. 2012, 2012, 310702. [Google Scholar] [CrossRef] [PubMed]
- Falkensammer, F.; Arnetzl, G.V.; Wildburger, A.; Krall, C.; Freudenthaler, J. Influence of different conditioning methods on immediate and delayed dentin sealing. J. Prosthet. Dent. 2014, 112, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.; Khan, T.A.; Khan, W.; Khurram, M.S. The effect of resin coating technique on shear bond strength. Pakistan Oral Dent. J. 2011, 31, 225. [Google Scholar]
- Reboul, T.; Hoang Thaï, H.A.; Cetik, S.; Atash, R. Comparison between shear forces applied on the overlay-dental tissue interface using different bonding techniques: An in vitro study. J. Indian. Prosthodont. Soc. 2018, 18, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Rigos, A.E.; Dandoulaki, C.; Kontonasaki, E.; Kokoti, M.; Papadopoulou, L.; Koidis, P. Effect of Immediate Dentin Sealing on the Bond Strength of Monolithic Zirconia to Human Dentin. Oper. Dent. 2019, 44, e167–e179. [Google Scholar] [CrossRef] [PubMed]
- van den Breemer, C.R.G.; Özcan, M.; Pols, M.R.; Postema, A.R.; Cune, M.S.; Gresnigt, M. Adhesion of resin cement to dentin: Effects of adhesive promoters, immediate dentin sealing strategies, and surface conditioning. Int. J. Esthet. Dent. 2019, 14, 52–63. [Google Scholar]
- Sag, B.U.; Bektas, O.O. Effect of immediate dentin sealing, bonding technique, and restorative material on the bond strength of indirect restorations. Braz. Dent. Sci. 2020, 23, 1–12. [Google Scholar] [CrossRef]
- Sakr, O.M. Immediate Dentin Sealing versus Dentin Air Abrasion Prior to Composite Inlay Luting Procedures. Med. Forum. 2021, 32, 8–11. [Google Scholar]
- Sakr, O.M. Immediate Dentin Sealing Versus Erbium (Er): YAG laser Dentin Ablation Prior to Composite Inlay Luting Procedures. Med. Forum. 2021, 32, 20–23. [Google Scholar]
- Deniz, S.T.; Oglakci, B.; Yesilirmak, S.O.; Dalkilic, E.E. The effect of immediate dentin sealing with chlorhexidine pretreatment on the shear bond strength of dual-cure adhesive cement. Microsc. Res. Tech. 2021, 84, 3204–3210. [Google Scholar] [CrossRef]
- Pheerarangsikul, N.; Wayakanon, P.; Wayakanon, K. Effects of Various Functional Monomers on Adhesion Between Immediate Dentin Sealing and Resin Cement. Oper. Dent. 2022, 47, 562–573. [Google Scholar] [CrossRef]
- Santos-Daroz, C.B.; Oliveira, M.T.; Góes, M.F.; Nikaido, T.; Tagami, J.; Giannini, M. Bond strength of a resin cement to dentin using the resin coating technique. Braz. Oral. Res. 2008, 22, 198–204. [Google Scholar] [CrossRef]
- Guilardi, L.F.; Dapieve, K.S.; Giordani, J.C.; Susin, A.H.; Valandro, L.F.; Rippe, M.P. Effect of immediate dentin sealing and temporary cement removal on bond strength of resin cements to dentin. Braz. Dent. Sci. 2022, 25, e2729. [Google Scholar] [CrossRef]
- Batista, J.M.N.; Leite, M.M.; Sabag, M.F.; Lopes, L.G.; Torres, É.M. Influence of the Flowable Resin Layer on Bond Strength Between Resin Cement and a Universal Adhesive Applied in the Immediate Dentin-sealing Technique. Oper. Dent. 2022, 47, 403–411. [Google Scholar] [CrossRef]
- Kitasako, Y.; Burrow, M.F.; Nikaido, T.; Tagami, J. Effect of resin-coating technique on dentin tensile bond strengths over 3 years. J. Esthet. Restor. Dent. 2002, 14, 115–122. [Google Scholar] [CrossRef]
- Nikaido, T.; Cho, E.; Nakajima, M.; Tashiro, H.; Toba, S.; Burrow, M.F.; Tagami, J. Tensile bond strengths of resin cements to bovine dentin using resin coating. Am. J. Dent. 2003, 16, 41A–46A. [Google Scholar]
- Duarte, R.M.; de Goes, M.F.; Montes, M.A. Effect of time on tensile bond strength of resin cement bonded to dentine and low-viscosity composite. J. Dent. 2006, 34, 52–61. [Google Scholar] [CrossRef]
- Takahashi, R.; Nikaido, T.; Ariyoshi, M.; Kitayama, S.; Sadr, A.; Foxton, R.M.; Tagami, J. Thin resin coating by dual-application of all-in-one adhesives improves dentin bond strength of resin cements for indirect restorations. Dent. Mater. J. 2010, 29, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Cesca, R.; Colombo, V.; Ernst, B.; Gallo, L.M.; Özcan, M. Tensile Strength and Failure Types of Direct and Indirect Resin Composite Copings for Perio-Overdentures Luted Using Different Adhesive Cementation Modalities. Materials 2020, 13, 3517. [Google Scholar] [CrossRef] [PubMed]
- Azad, E.; Atai, M.; Zandi, M.; Shokrollahi, P.; Solhi, L. Structure-properties relationships in dental adhesives: Effect of initiator, matrix monomer structure, and nano-filler incorporation. Dent. Mater. 2018, 34, 1263–1270. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, M.; Ando, S.; Hinoura, K.; Onose, H.; Moore, B.K. Influence of filler addition to bonding agents on shear bond strength to bovine dentin. Dent. Mater. 1995, 11, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Van Landuyt, K.L.; Snauwaert, J.; De Munck, J.; Peumans, M.; Yoshida, Y.; Poitevin, A.; Coutinho, E.; Suzuki, K.; Lambrechts, P.; Van Meerbeek, B. Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials 2007, 28, 3757–3785. [Google Scholar] [CrossRef] [PubMed]
- Eliades, G.C.; Caputo, A.A. The strength of layering technique in visible light-cured composites. J. Prosthet. Dent. 1989, 61, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Rueggeberg, F.A.; Margeson, D.H. The effect of oxygen inhibition on an unfilled/filled composite system. J. Dent. Res. 1990, 69, 1652–1658. [Google Scholar] [CrossRef]
- Bruzi, G.; Carvalho, A.O.; Maia, H.P. Are there combinations of resin liners and impression materials not compatible with IDS technique? Dent. Mater. J. 2013, 3, 200–208. [Google Scholar] [CrossRef]
- Bergmann, P.; Noack, M.J.; Roulet, J.F. Marginal adaptation with glass-ceramic inlays adhesively luted with glycerine gel. Quintessence Int. 1991, 22, 739–744. [Google Scholar]
- Ghiggi, P.C.; Steiger, A.K.; Marcondes, M.L.; Mota, E.G.; Júnior, L.H.B.; Spohr, A.M. Does immediate dentin sealing influence the polymerization of impression materials? Eur. J. Dent. 2014, 8, 366–372. [Google Scholar] [CrossRef]
- Khakiani, M.I.; Kumar, V.; Pandya, H.V.; Nathani, T.I.; Verma, P.; Bhanushali, N.V. Effect of immediate dentin sealing on polymerization of elastomeric materials: An ex vivo randomized controlled trial. Int. J. Clin. Pediatr. Dent. 2019, 12, 288. [Google Scholar] [CrossRef] [PubMed]
- Özcan, M.; Barbosa, S.H.; Melo, R.M.; Galhano, G.A.P.; Bottino, M.A. Effect of surface conditioning methods on the microtensile bond strength of resin composite to composite after aging conditions. Dent. Mater. 2007, 23, 1276–1282. [Google Scholar] [CrossRef]
- Stavridakis, M.M.; Krejci, I.; Magne, P. Immediate dentin sealing of onlay preparations: Thickness of pre-cured Dentin Bonding Agent and effect of surface cleaning. Oper. Dent. 2005, 30, 747–757. [Google Scholar] [PubMed]
- Ferracane, J.L.; Stansbury, J.W.; Burke, F.J.T. Self-adhesive resin cements–chemistry, properties and clinical considerations. J. Oral Rehabil. 2011, 38, 295–314. [Google Scholar] [CrossRef] [PubMed]
- Miotti, L.L.; Follak, A.C.; Montagner, A.F.; Pozzobon, R.T.; Da Silveira, B.L.; Susin, A.H. Is conventional resin cement adhesive performance to dentin better than self-adhesive? A systematic review and meta-analysis of laboratory studies. Oper. Dent. 2020, 45, 484–495. [Google Scholar] [CrossRef] [PubMed]
- Comba, A.; Paolone, G.; Baldi, A.; Vichi, A.; Goracci, C.; Bertozzi, G.; Scotti, N. Effects of Substrate and Cement Shade on the Translucency and Color of CAD/CAM Lithium-Disilicate and Zirconia Ceramic Materials. Polymers 2022, 14, 1778. [Google Scholar] [CrossRef] [PubMed]
- Udo, T.; Nikaido, T.; Ikeda, M.; Weerasinghe, D.S.; Harada, N.; Foxton, R.M.; Tagami, J. Enhancement of adhesion between resin coating materials and resin cements. Dent. Mater. J. 2007, 26, 519–525. [Google Scholar] [CrossRef][Green Version]
- Gale, M.S.; Darvell, B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, S.; Breschi, L.; Özcan, M.; Pfefferkorn, F.; Ferrari, M.; Van Meerbeek, B. Academy of Dental Materials guidance on in vitro testing of dental composite bonding effectiveness to dentin/enamel using micro-tensile bond strength (μTBS) approach. Dent. Mater. 2017, 33, 133–143. [Google Scholar] [CrossRef] [PubMed]
| #1 | “Immediate Dentin Sealing” OR “resin coating” OR “pre-hybridization” OR “prehybridization” OR “dual-bonding” |
| #2 | “bond strength” OR “bonding strength” |
| #1 and #2 |
| Author, Year | Type of Tooth | IDS Material (DBA + Resin Composite) | Restoration Material | Temporary Material | Cleaning Method of IDS Surface | Luting Cement | Aging | Specimen Number per Group | Test Method |
|---|---|---|---|---|---|---|---|---|---|
| Kitasako et al. [72] (2002) | Bovine | Clapearl bonding agent + Protect Liner F | Clearfil CR Inlay (indirect resin composite) | - | - | -Clapearl DC -Panavia 21 -Super Bond C&B | 37 °C tap water for 1 day, 6 months, 1 year and 3 years | 10 | TBS |
| Nikaido et al. [73] (2003) | Bovine | -Clearfil SE (SE) + Protect Liner F -Unifil Bond (SE) + Protect Liner F -One-Up Bond (SE) + Protect Liner F -Single Bond (ER) + Protect Liner F | Estenia (indirect resin composite) | Cavit-G | Cotton pellet moistened with 70% ethanol, etched with 37% phosphoric acid | -Panavia F -Link Max -Bistite II -Rely-X | Water at 37 °C for 1 day | 10 | TBS |
| Jayasooriya et al. [20] (2003) | Human (premolar) | -Clearfil SE Bond (SE) -Clearfil SE Bond (SE) + Protect Liner F -Single Bond (ER) -Single Bond (ER) + Protect Liner F | -Estenia (indirect resin composite) -Clearfil AP-X (direct resin composite) | Cavit-G | Cotton pellet moistened ethanol, etched with 37% phosphoric acid | Panavia F | Water at 37 °C for 24 h | 5 | µTBS |
| Nikaido et al. [21] (2003) | Human (molar) | RZ-II (SE)-experimental | -Metafil C (direct resin composite) -New Metacolor Infis (indirect resin composite) | Cavit-G | Coton pellet soaked in alcohol, 10% citric acid, and 3% ferric chloride for 10 s | Chemiace II | Water for 1 day | 4 | µTBS |
| Magne et al. [17] (2005) | Human (molar) | Optibond FL (ER) | Z 100 (direct resin composite) | Tempfil Inlay | Airborne-particle abrasion | - | Distilled water at room temperature for 24 h | 5 | µTBS |
| Islam et al. [22] (2006) | Human (lower first molar) | Hybrid Bond (SE) | Estenia (indirect resin composite) | - | 10% citric acid and 3% ferric chloride for 10 s | Chemiace II | Water at 37 °C for 24 h | 5 | µTBS |
| Duarte et al. [74] (2006) | Bovine (lower incisors) | Clearfil liner Bond 2V (SE) + Protect Liner F | Z 100 (indirect resin composite restoration) | - | - | Panavia F | Distilled water at 37 °C for 10 mins or 24 h or solution of deionized water and 0.4% sodium azide at 37 °C for 12 months | 10 | TBS |
| Okuda et al. [23] (2007) | Human (molar) | -Clearfil Protect Bond (SE) -Clearfil Protect Bond (SE) + Protect Liner F | -Estenia (indirect resin composite) -Clearfil AP-X (direct resin composite) | Cavit-G | Cotton pellet soaked in ethanol, 37% phosphoric acid for 10 s | Panavia F | Distilled water at 37 °C for 24 h | 3 | µTBS |
| Sultana et al. [24] (2007) | Human (third molar) | Clearfil SE Bond (SE) + Protect Liner F | Estenia (indirect resin composite) | Cavit-G | Coton pellet soaked in alcohol, 37% phosphoric acid for 10 s | Panavia F 2.0 | Water at 37 °C for 24 h | 11 | µTBS |
| Frankenberger et al. [25] (2007) | Human (third molar) | -XP Bond (ER) -XP Bond (ER) + X-Flow -Syntac (ER) -Syntac (ER) + X-Flow -Optibond FL (ER) -Optibond FL (ER) + X-Flow | Clearfil AP-X (indirect resin composite restoration) | -TempBond -TempBond NE | -Scaler -Prophypearls -Clinpro powder | Calibra | Distilled water at 37 °C for 24 h | 3 | µTBS |
| Magne et al. [18] (2007) | Human (molar) | -Optibond FL (ER) -SE bond (SE) | Z 100 (direct resin composite) | Tempfil Inlay | Airborne-particle abrasion | - | Distilled water at room temperature for 24 h | 5 | µTBS |
| de Andrade et al. [26] (2007) | Human (molar) | -Single Bond (ER) -Single Bond (ER) + Protect Liner F | Targis Dentin-220 (indirect resin composite) | - | - | Rely X ARC | 1200 thermal cycles | 6–15 sticks | µTBS |
| Erkut et al. [54] (2007) | Human (molar) | -Single Bond (ER) -One Step (SE) | - | -RelyX Temp NE -RelyX Temp E | Pumice | -RelyX ARC -Duo Link | 1000 thermal cycles, tap water at room temperature for one week | 10 | SBS |
| Ariyoshi et al. [27] (2008) | Human (molar) | -Clearfil SE Bond (SE) -Clearfil SE Bond (SE) + Clearfil Flow FX | Clearfil DC Core Automix (indirect resin composite core) | Caviton | Cotton pellet containing ethanol for 10 s | -Panavia F 2.0 -Clearfil DC Core Automix | Water at 37 °C for 24 h | 5 | µTBS |
| Nikaido et al. [28] (2008) | Human (molar) | -Clearfil SE Bond (SE) + Protect Liner F -Clearfil SE Bond (SE) + Ionosit MicroSpand | Estenia (indirect resin composite) | Cavit-G | - | Panavia F | 37 °C water for 1 day, 6 months, or 1 year | 10 sticks | µTBS |
| Santos-Daroz et al. [69] (2008) | Bovine (incisor) | -Single Bond (ER) -One-Up Bond F (SE) -Xeno III (SE) -AdheSE (SE) -Clearfil Protect Bond (SE) -Tyrian SPE/One-Step Plus SPE (SE) -Unifil Bond (SE) + Protect Liner F | - | Temp Bond NE | - | Panavia F | Water at 37 °C for 24 h | 8 | µSBS |
| Kameyama et al. [29] (2009) | Human (molar) | -UniFil Bond (SE) + UniFil Flow -Adper Single Bond (ER) + UniFil Flow | Gradia (indirect resin composite restoration) | - | Alcohol cotton pellet | Linkmax | Water at 37 °C for 24 h | 4 | µTBS |
| Kitayama et al. [30] (2009) | Human (lower third molar) | Clearfil Tri-S Bond (SE) | CEREC-Blocs (feldspathic ceramic) | - | Cotton pellet soaked in isopropyl alcohol | Clearfil Esthetic Cement | 250,000 cycles of mechanical loading or storage in distilled water at 37 °C for 28 h | 7 | µTBS |
| Duarte et al. [19] (2009) | Human (third molar) | -Adper Single Bond (ER) -Adper Prompt L-pop (SE) | Targis Ceromer system | Fermit | Pumice and water | RelyX ARC | 1000 thermal cycles | 5 | µTBS |
| Lee and Park [55] (2009) | Human (premolar) | AdheSe (SE) | Tescera ATL system (indirect resin composite) | Fermit | - | -Duo-Link -Filtek Z250 | 100% humidity at 37 °C for one day | 15 | SBS |
| Takahashi et al. [31] (2010) | Human (molar) | Tokuyama Bond Force (SE) (single and double layer) | Pearleste (indirect resin composite) | Caviton | Alcohol-soaked cotton pellets for 10 s, etching with 38% phosphoric acid | Bistite II | Water at 37 °C for 24 h | 3 | µTBS |
| Takahashi et al. [75] (2010) | Bovine (incisor) | -G-Bond (SE) -Clearfil Tri-S Bond (SE) -Tokuyama Bond Force (SE) -Hybrid-Coat (SE) (single and double layer) | Pearleste (indirect resin composite) | Caviton | Alcohol-soaked cotton pellets for 10 s, etching with 37% phosphoric acid | -Link Max -Clearfil Esthetic Cement -Bistite II -Chemiace II | Water at 37 °C for 24 h | 10 | TBS |
| Feitosa et al. [32] (2010) | Human (third molar) | -Clearfil S3 (SE) -Clearfil S3 (SE) + Clearfil Protect Liner -Clearfil SE Bond (SE) -Clearfil SE Bond (SE) + Clearfil Protect Liner | Sinfony (indirect resin composite) | Cavit | Pumice stone and water | Panavia F | 1500 thermal cycles and 200,000 cyclic loading | 5 | µTBS |
| Choi and Cho [56] (2010) | Human (molar) | -Clearfil SE Bond (SE) -Adapter Single Bond 2 (ER) | Porcelain | - | - | Variolink II | Distilled water at 37 °C for 24 h | 10 | SBS |
| Hassan et al. [60] (2011) | Human (premolar) | -Clearfil SE Bond (SE) -Syntac® Sprint (ER) | Metal disc (Cobalt Chromium alloy) | - | - | -Panavia F -Variolink II | 100% relative humidity at 37 °C for 24 h | 12 | SBS |
| Sailer et al. [57] (2012) | Human (molar) | Clearfil SE Bond (SE) | - | Freegenol | Abrasive fluoride-free polishing paste in combination with rubber cup | -RelyX Unicem -Variolink II -Panavia 21 | Water storage at 37 °C for 24 h or 1500 thermal cycles or water storage at room temperature for 1 h | 12 | SBS |
| Dalby et al. [58] (2012) | Human (third molar) | -Optibond FL (ER) -Single bond (ER) -One Coat Bond (SE) -Go! (SE) | Authentic (Glass ceramic) | - | - | RelyX Unicem | Distilled water at room temperature for one week | 16 | SBS |
| Falkensammer et al. [59] (2014) | Human (premolar) | AdheSe (SE) | Vitablocks Mark II (felspathic ceramic blocks) | Temp Bond NE | Pumice, airborne-particle abrasion combined with silicoated aluminum oxide, glycine and calcium carbonate powder | Variolink II | Saline solution at 37 °C for 24 h | 11 | SBS |
| Duque [33] (2014) | Human (third molar) | -OptiBond FL (ER) -Optibond Solo Plus (ER) | Gradia (indirect resin composite) | - | RelyX Luting Plus | - | 10 | µTBS | |
| Giannini et al. [34] (2015) | Human (third molar) | Clearfil SE Bond (SE) + Clearfil Majesty Flow | AP-X (indirect resin composite restoration) | - | -RelyX Unicem -RelyX Unicem 2 -Clearfil SA Cement -G-Cem -Panavia F 2.0 | 5000 thermocycles | 5 | µTBS | |
| Santana et al. [35] (2016) | Human (third molar) | Clearfil SE Bond (SE) | Filtek Z250 (indirect resin composite restoration) | - | Airborne-particle abrasion | -RelyZ Unicem -Clearfil SA Luting -RelyX ARC -Panavia F | Distilled water for 24 h | 5 | µTBS |
| da Silva et al. [36] (2016) | Human (molar) | Adper ScotchBond Multipurpose (ER) | Z350 XT (direct resin composite) | -Dycal -Temp bond NE -Clip F | Pumice | - | Distilled water at 37 °C for 24 h | 8 | µTBS |
| Brigagão et al. [37] (2017) | Human (third molar) | Scotchbond Universal (SE and ER) | Z 100 (indirect resin composite restoration) | RelyX Temp | Rotary brush with pumice | -RelyX ARC -RelyX U200 | Distilled water at 37 °C for 7 days | 5 | µTBS |
| Ishii et al. [38] (2017) | Human (mandibular first molar) | Scotchbond Universal (SE) + Filtek Supreme Ultra Flowable | -Lava Ultimate (indirect resin composite) -VITA ENAMIC (hybrid) -VITABLOCS Mark II (feldspathic ceramic) | - | Etching | RelyX Ultimate | Cyclic loading for 3 × 105 cycles | 4 | µTBS |
| Ferreira-Filho et al. [39] (2018) | Human (third molar) | -Xeno V (SE) -Clearfil SE Bond (SE) -XP Bond (ER) -Optibond FL (ER) | Filtek Z250 (indirect resin composite restoration) | - | - | RelyX Unicem | 7 days or 3 months water storage at 37 °C | 6 | µTBS |
| Hironaka et al. [40] (2018) | Human (third molar) | Clearfil SE Bond 2 (SE) + Protect Liner F | Filtek Z250 (indirect resin composite restoration) | Temp Bond NE | Pumice and water | Panavia F 2.0 | Artificial saliva at 37 °C for 24 h | 10 | µTBS |
| Murata et al. [41] (2018) | Human (maxillary first molar) | Scotchbond Universal (SE) + Filtek Supreme Ultra Flowable Restorative | VITABLOCS Mark II (feldspathic ceramic block) | - | - | Panavia V5 | Cyclic loading for 3 × 105 cycles | 8 | µTBS |
| Reboul et al. [61] (2018) | Human (mandibular third molar) | OptiBond FL (ER) | Suprinity block (glass ceramic) | - | - | -Panavia V5 -Heated resin composite | Distilled water at room temperature for 7 days | 10 | SBS |
| Rigos et al. [62] (2019) | Human (third molar) | OptiBond FL (ER) | BruxZir (Monolithic zirconia block) | - | - | -Panavia F2.0 -PermaCem Dual Smartmix | Distilled water at 37 °C for 24 h | 14–15 | SBS |
| van den Breemer et al. [42] (2019) | Human (molar) | -OptiBond FL (ER) (1 and 2 layers) - OptiBond FL+Grand IO Flow | Enamel plus HFO (direct resin composite) | Durelon | -Pumice -Pumice + silica coating (Cojet) | - | 1 week or 6 months of storage | 24 sticks | µTBS |
| van den Breemer et al. [63] (2019) | Human (molar) | -Clearfil SE Bond (SE) (1 and 2 layers -OptiBond FL (ER) (1 and 2 layers) - Clearfil SE Bond + Grandio Flow - OptiBond FL + Grandio Flow | - | TempBond NE | -Pumice -Pumice + silica coating (Cojet) | Variolink II | 10,000 thermocycles | 10 | SBS |
| Akehashi et al. [43] (2019) | Human (molar) | Clearfil SE Bond 2 (SE) + -Clearfil Protect Liner F -Clearfil Majesty LV -Panavia V5 (DC/LC) | -Estenia C&B (indirect resin composite) -Clearfil AP-X (direct resin composite) | - | - | -Panavia V5 -Panavia F2.0 | Distilled water at 37 °C for 24 h | 4 | µTBS |
| Hayashi et al. [44] (2019) | Human (mandibular premolar) | Clearfil Universal Bond Quick (SE) + Clearfil Majesty ES Flow | VITABLOCS Mark II (feldspathic ceramic block) | TempBond NE | Polishing brush underwater | Panavia V5 | Cyclic loading for 3 × 105 cycles | 15 sticks | µTBS |
| Sag et al. [64] (2020) | Human (molar) | Clearfil SE Bond (SE) + Filtek Ultimate Flowable | -Lava Ultimate (Resin nano CAD-CAM block) -Solidex (indirect resin composite) | DiaTemp | - | -RelyX Unicem -RelyX Ultimate Clicker | - | 10 | SBS |
| Rozan et al. [45] (2020) | Human (third molar) | -G-Premio Bond (SE) -Clearfil SE Bond 2 (SE) + Clearfil Majesty ES Flow | Cerasmart (resin CAD/CAM block) | - | - | -RelyX Ultimate -G-CEM LinkForce -Panavia V5 | 5000 thermocycles | 8 | µTBS |
| Cesca et al. [76] (2020) | Human (maxillary central incisor, canine, and premolar) | Syntac (ER) | Tetric Ceram (direct and indirect resin composite restoration) | Cavit | Air-abrasion | -Preheated Tetric Ceram (resin composite) -Variolink II | Distilled water for 1 week | 10 | TBS |
| Carvalho et al. [46] (2021) | Human (third molar) | -Optibond FL (ER) -Scotchbond Multi-Purpose(ER) -Single Bond Plus (ER) -Clearfil SE Bond (SE) -Scotchbond Universal (SE) + Filtek Bulk Fill Flow | Filtek Z100 (direct resin composite) | Relotec LC | Air-abrasion and phosphoric acid | - | Distilled water at room temperature for at least 24 h | 5 | µTBS |
| Sakr [65] (2021) | Human (molar) | Optibond FL (ER) | Filtek Z350XT (indirect resin composite restoration) | - | - | RelyX | Distilled water for 24 h | 10 | SBS |
| Sakr [66] (2021) | Human (molar) | Optibond FL (ER) | Filtek Z350XT (indirect resin composite restoration) | - | - | RelyX | Distilled water for 24 h | 15 | SBS |
| Gailani et al. [48] (2021) | Human (molar) | -OptiBond FL -OptiBond Universal -Prime and Bond active universal -Scotchbond Universal Adhesive -Future bond Universal single bond -Universal Primer Dual Cured Adhesive -All Bond Universal -Adhese Universal -One coat7 Universal | Lava Ultimate blocks | Telio CS Onlay | Sandblast with cleaning powder | -Maxcem Elite cement -Calibra Ceram Adhesive Resin Cement -Relyx Ultimate Adhesive Resin Cement -Rebilda DC Cement -Duo-Link Universal -Variolink -Solocem cement | Simulated pulpal pressure at room temperature for 24 h | 4 | μTBS |
| Deniz et al. [67] (2021) | Human (molar) | -Adper Single Bond 2 (ER) -Single Bond Universal (ER) | - | - | - | RelyX Ultimate Clicker | Distilled water at 37 °C for 24 h | 15 | SBS |
| Abo-Alazm et al. [49] (2021) | Human (third molar) | -iBOND (SE) -GLUMA Bond Universal (SE) | Grandio (CAD/CAM resin block) | Cavex | Airborne-particle abrasion (CoJet) | RelyX Unicem | 24 h or 6 months of water storage in distilled water | 5 | μTBS |
| Abdou et al. [50] (2021) | Bovine (incisor) | -Clearfil Universal Bond Quick -Scotchbond Universal Adhesive -Optibond All-in-one | Katana Avencia Block (CAD/CAM resin block) | Temp bond NE (for multiple-visit) | Alcohol-soaked cotton pellets for 10 s (for multiple visits) | -Panavia V5 -RelyX Ultimate -NX3 Nexus | - | 5 | μTBS |
| Oda et al. [47] (2022) | Human (molar) | Clearfil SE Bond 2 (SE) + Clearfil Majesty ES Flow | Katana Avencia Block (CAD/CAM resin blocks) | - | - | -Panavia SA cement plus -Panavia SA cement universal | - | 5 | μTBS |
| Guilardi et al. [70] (2022) | Bovine (incisor) | -Single Bond 2 (ER) -Single Bond Universal (SE) | - | Temp-Bond NE | Pumice | -RelyX U200 -Multilink Automix | Distilled water at 37 °C for 24 h | 5 | μSBS |
| Nakazawa et al. [51] (2022) | Human (mandibular first molar) | -Clearfil Universal Bond Quick -Clearfil Universal Bond Quick + Clearfil Majesty ES Flow | -Vitablocks Mark II (feldspathic ceramic block) | - | - | -Panavia SA Cement Universal | Cyclic loading for 3 × 105 cycles | 16 slabs | μTBS |
| Pheerarangsikul et al. [68] (2022) | Human (premolar) | -Single Bond Universal (SE/ER) -OptiBond XTR (SE) -Clearfil SE Bond (SE) | Ceram.x SphereTec one (indirect resin composite restoration) | - | Pumice | -RelyX Ultimate -NX3 Nexus -Panavia V5 -Super-Bond C&B | 5000 thermocycles | 10 | SBS |
| Batista et al. [71] (2022) | Bovine (lower incisor) | -Single Bond Universal (SE) -Single Bond Universal (SE) + Filtek Z350 XT Flow | - | - | Pumice, 37% phosphoric acid | -RelyX Ultimate | 24 h or 3 months in distilled water at 37 °C | 15 | μSBS |
| Sooksang et al. [52] (2023) | Human (third molar) | -Single Bond Universal (SE) -Optibond FL (ER) (Single and double application) | - | Temp-Bond NE | Pumice | -RelyX U200 | Cyclic loading for 50,000 cycles | 5 (10 sticks) | μTBS |
| Kimyai et al. [53] (2023) | Human (third molar) | -All-Bond Universal (SE/ER) | Spectrum (indirect resin composite restoration) | - | - | Bifix SE | 7 days at 37 °C or 10,000 thermocycles | 30 sticks | μTBS |
| Study | (I) Teeth Randomization | (II) Materials Used According to Manufacturer’s Instructions | (III) Single Operator | (IV) Sample Size | (V) Standardized sample | (VI) Blinding Operator | VII) Failure Mode | Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| Kitasako et al. [72] | N | Y | N | N | Y | N | Y | HIGH |
| Nikaido et al. [73] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Jayasooriya et al. [20] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Nikaido et al. [21] | N | Y | N | N | Y | N | Y | HIGH |
| Magne et al. [17] | N | Y | N | N | Y | N | Y | HIGH |
| Islam et al. [22] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Duarte et al. [74] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Okuda et al. [23] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Sultana et al. [24] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Frankenberger et al. [25] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Magne et al. [18] | N | Y | N | Y | Y | N | Y | MEDIUM |
| de Andrade et al. [26] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Erkut et al. [54] | N | Y | N | N | Y | N | Y | HIGH |
| Ariyoshi et al. [27] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Nikaido et al. [28] | N | Y | N | N | Y | N | Y | HIGH |
| Santos-Daroz et al. [69] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Kameyama et al. [29] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Kitayama et al. [30] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Duarte et al. [19] | N | Y | N | N | Y | N | Y | HIGH |
| Lee and Park [55] | Y | Y | N | N | Y | N | N | HIGH |
| Takahashi et al. [31] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Takahashi et al. [75] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Feitosa et al. [32] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Choi and Cho [56] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Hassan et al. [60] | N | Y | N | N | Y | N | N | HIGH |
| Sailer et al. [57] | N | Y | N | N | Y | N | Y | HIGH |
| Dalby et al. [58] | Y | Y | Y | N | Y | N | Y | MEDIUM |
| Falkensammer et al. [59] | N | Y | N | N | Y | N | Y | HIGH |
| Duque [33] | Y | Y | Y | Y | Y | N | N | MEDIUM |
| Giannini et al. [34] | N | Y | N | N | Y | N | Y | HIGH |
| Santana et al. [35] | Y | Y | N | N | Y | N | Y | MEDIUM |
| da Silva et al. [36] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Brigagão et al. [37] | N | N | N | N | Y | N | Y | HIGH |
| Ishii et al. [38] | N | Y | N | N | Y | N | Y | HIGH |
| Ferreira-Filho et al. [39] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Hironaka et al. [40] | N | Y | N | N | Y | N | Y | HIGH |
| Murata et al. [41] | N | Y | N | N | Y | N | Y | HIGH |
| Reboul et al. [61] | Y | Y | Y | N | Y | N | Y | MEDIUM |
| Rigos et al. [62] | Y | Y | Y | N | Y | N | Y | MEDIUM |
| van den Breemer et al. [42] | Y | N | N | N | Y | N | Y | HIGH |
| van den Breemer et al. [63] | Y | N | N | N | Y | N | Y | HIGH |
| Akehashi et al. [43] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Hayashi et al. [44] | N | Y | N | N | Y | N | Y | HIGH |
| Sag et al. [64] | Y | Y | N | N | Y | N | N | HIGH |
| Rozan et al. [45] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Cesca et al. [76] | Y | Y | N | Y | Y | N | Y | MEDIUM |
| Carvalho et al. [46] | Y | Y | N | Y | Y | N | Y | MEDIUM |
| Sakr [65] | Y | Y | N | N | Y | N | N | HIGH |
| Sakr [66] | Y | Y | N | N | Y | N | N | HIGH |
| Gailani et al. [48] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Deniz et al. [67] | Y | Y | Y | Y | Y | Y | Y | LOW |
| Abo-Alazm et al. [49] | Y | Y | N | Y | Y | N | N | MEDIUM |
| Abdou et al. [50] | N | Y | N | N | Y | N | Y | HIGH |
| Oda et al. [47] | Y | N | N | N | Y | N | Y | HIGH |
| Guilardi et al. [70] | Y | Y | N | Y | Y | N | Y | MEDIUM |
| Nakazawa et al. [51] | Y | N | N | N | Y | N | Y | HIGH |
| Pheerarangsikul et al. [68] | Y | Y | N | Y | Y | N | Y | MEDIUM |
| Batista et al. [71] | Y | Y | N | N | Y | N | Y | MEDIUM |
| Sooksang et al. [52] | N | N | N | N | Y | N | Y | HIGH |
| Kimyai et al. [53] | Y | Y | Y | N | Y | N | N | MEDIUM |
| % User Agreement | Kappa | % Data That Are Reliable (through Cohen’s Kappa Test) | Level of Agreement | |
|---|---|---|---|---|
| (I) Randomization of Teeth | 98.33% | 0.9597 | 92.10% | Almost Perfect |
| (II) Manufacturer’s Instructions | 95.00% | 0.774 | 59.985% | Moderate |
| (III) Single Operator | 100.00% | 1 | 100% | Almost Perfect |
| (IV) Sample Size | 100.00% | 1 | 100% | Almost Perfect |
| (V) Standardized Sample | 100.00% | 1 | 100% | Almost Perfect |
| (VI) Blinding Operator | 100.00% | 1 | 100% | Almost Perfect |
| (VII) Failure Mode | 100.00% | 1 | 100% | Almost Perfect |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ozer, F.; Batu Eken, Z.; Hao, J.; Tuloglu, N.; Blatz, M.B. Effect of Immediate Dentin Sealing on the Bonding Performance of Indirect Restorations: A Systematic Review. Biomimetics 2024, 9, 182. https://doi.org/10.3390/biomimetics9030182
Ozer F, Batu Eken Z, Hao J, Tuloglu N, Blatz MB. Effect of Immediate Dentin Sealing on the Bonding Performance of Indirect Restorations: A Systematic Review. Biomimetics. 2024; 9(3):182. https://doi.org/10.3390/biomimetics9030182
Chicago/Turabian StyleOzer, Fusun, Zeynep Batu Eken, Jessica Hao, Nuray Tuloglu, and Markus B. Blatz. 2024. "Effect of Immediate Dentin Sealing on the Bonding Performance of Indirect Restorations: A Systematic Review" Biomimetics 9, no. 3: 182. https://doi.org/10.3390/biomimetics9030182
APA StyleOzer, F., Batu Eken, Z., Hao, J., Tuloglu, N., & Blatz, M. B. (2024). Effect of Immediate Dentin Sealing on the Bonding Performance of Indirect Restorations: A Systematic Review. Biomimetics, 9(3), 182. https://doi.org/10.3390/biomimetics9030182







