Food Sensitization Impact on Asthma Attacks in Children According to Age Group
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Subjects
2.3. Clinical and Epidemiological Methods
2.4. Lung Function Testing
2.5. Immunological Assessment
2.6. Statistical Methods
3. Results
3.1. Demographic and Clinical Characteristics
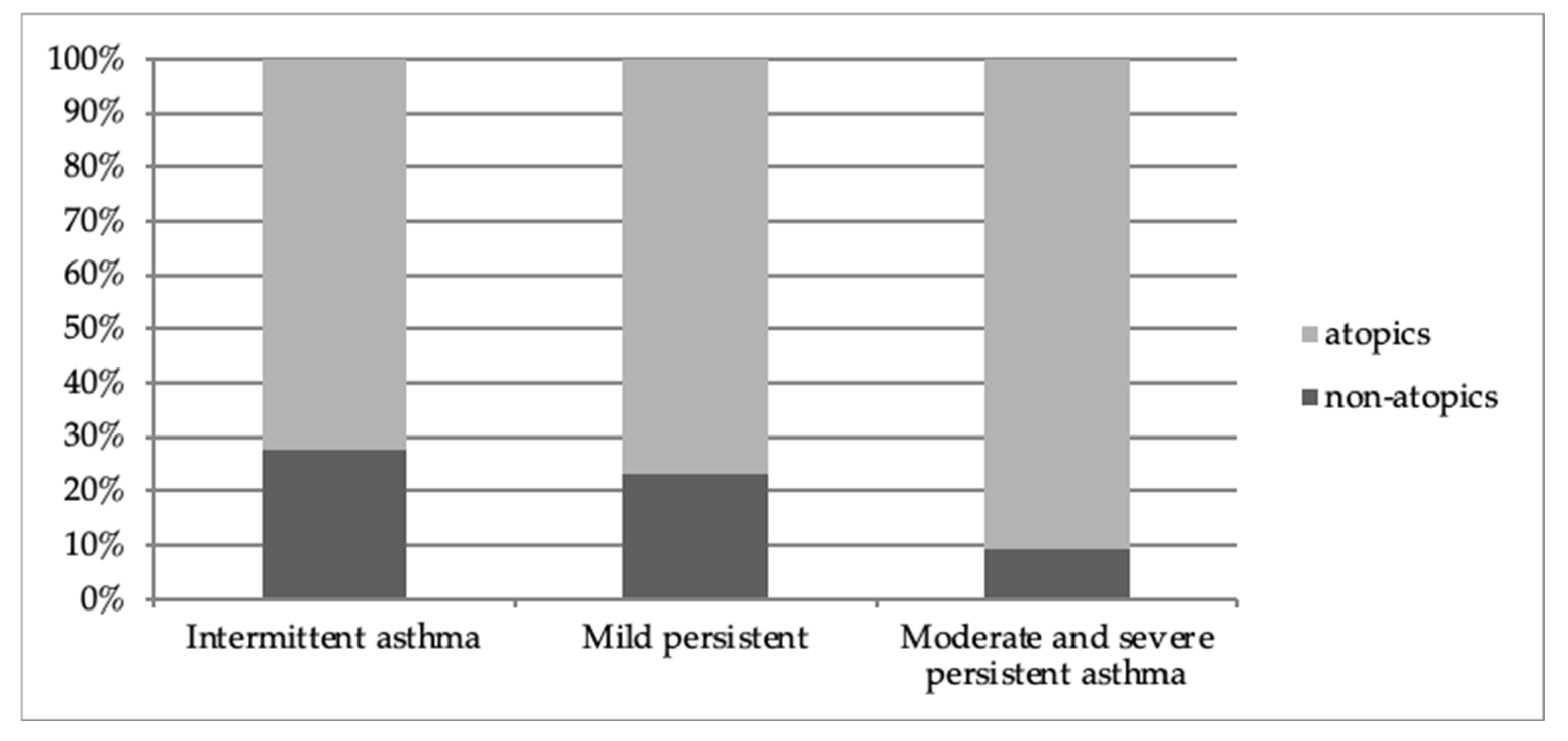
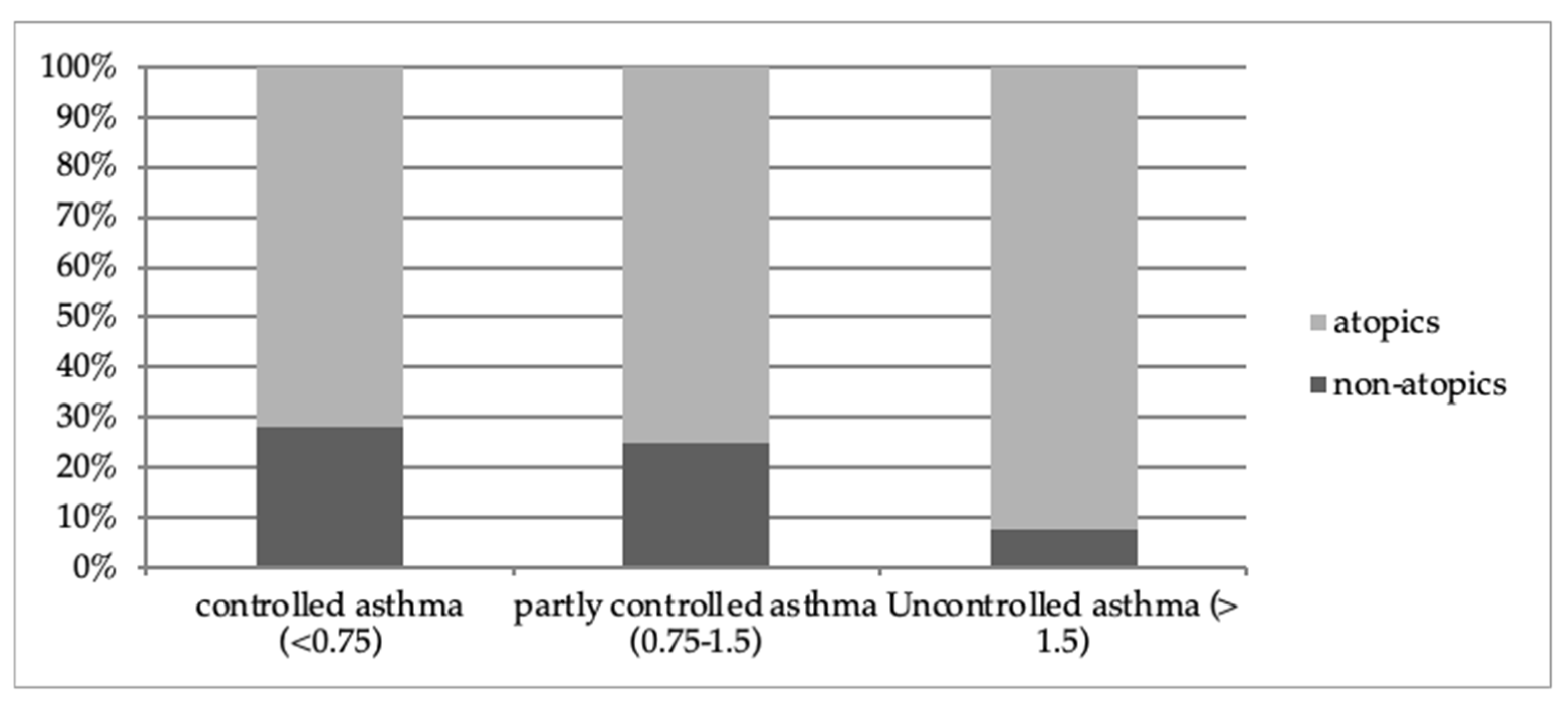
3.2. Asthma Control and Asthma Severity
3.3. Spirometry Evaluation
3.4. Atopic Status Evaluation
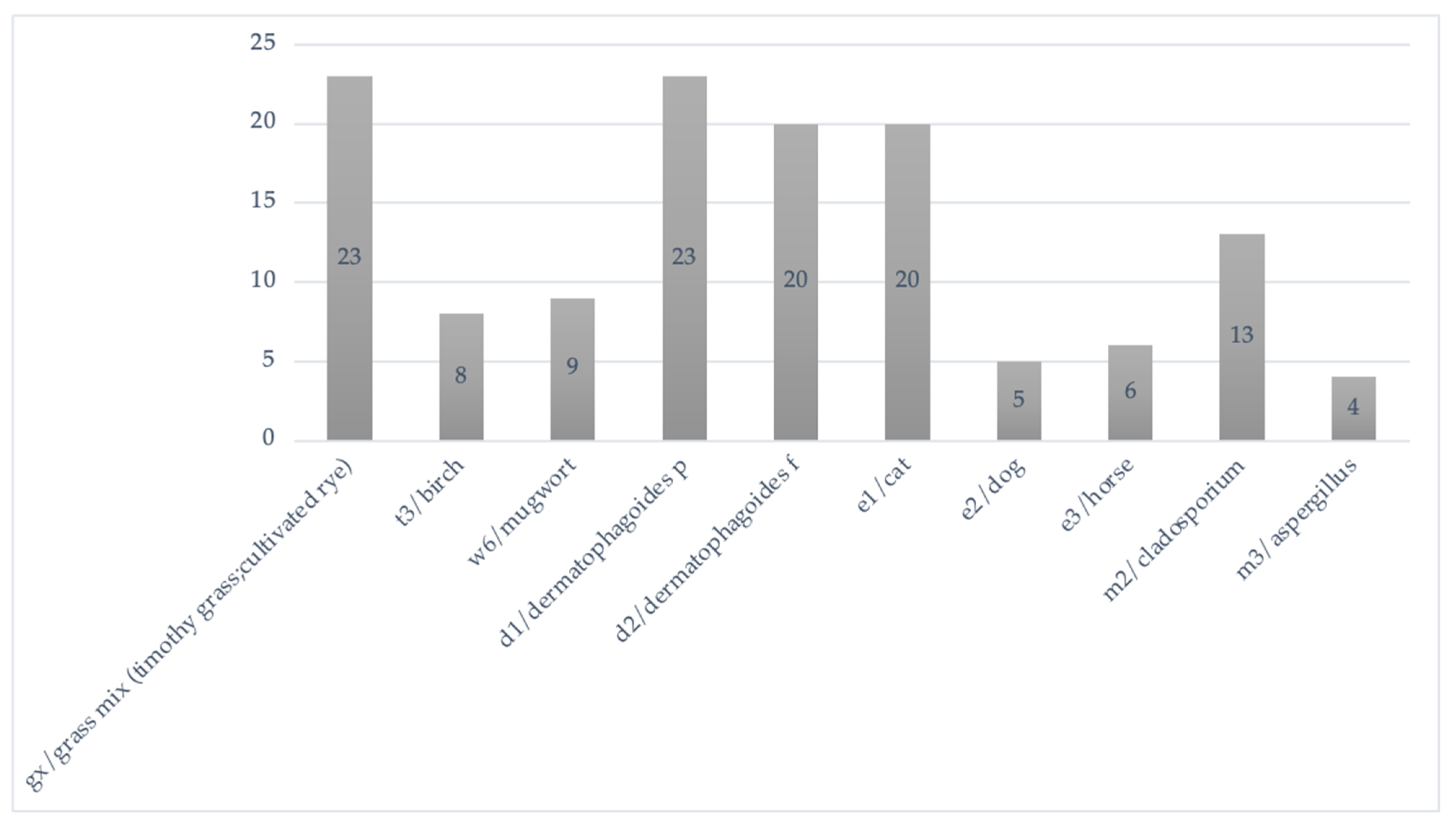
3.4.1. Respiratory Allergens Sensitization
3.4.2. Food Allergens Sensitization
3.4.3. Respiratory and Food Allergens Sensitization
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wong, C.-Y.; Yeh, K.-W.; Huang, J.-L.; Su, K.-W.; Tsai, M.-H.; Hua, M.-C.; Liao, S.-L.; Lai, S.-H.; Chen, L.-C.; Chiu, C.-Y. Longitudinal Analysis of Total Serum IgE Levels with Allergen Sensitization and Atopic Diseases in Early Childhood. Sci. Rep. 2020, 10, 21278. [Google Scholar] [CrossRef] [PubMed]
- Tham, E.H.; Leung, D.Y.M. Mechanisms by Which Atopic Dermatitis Predisposes to Food Allergy and the Atopic March. Allergy. Asthma Immunol. Res. 2019, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Eckl-Dorna, J.; Villazala-Merino, S.; Campion, N.J.; Byazrova, M.; Filatov, A.; Kudlay, D.; Karsonova, A.; Riabova, K.; Khaitov, M.; Karaulov, A.; et al. Tracing IgE-Producing Cells in Allergic Patients. Cells 2019, 8, 994. [Google Scholar] [CrossRef] [PubMed]
- Satitsuksanoa, P.; Daanje, M.; Akdis, M.; Boyd, S.D.; Veen, W. Biology and Dynamics of B Cells in the Context of IgE-mediated Food Allergy. Allergy 2021, 76, 1707–1717. [Google Scholar] [CrossRef]
- Tsuge, M.; Ikeda, M.; Matsumoto, N.; Yorifuji, T.; Tsukahara, H. Current Insights into Atopic March. Children 2021, 8, 1067. [Google Scholar] [CrossRef]
- Wahn, U.; Nickel, R.; Grüber, C.; Lau, S.; Illi, S. The Atopic March. Asthma Prev. 2005, 120, 313–331. [Google Scholar] [CrossRef]
- Togias, A. Rhinitis and Asthma: Evidence for Respiratory System Integration. J. Allergy Clin. Immunol. 2003, 111, 1171–1183. [Google Scholar] [CrossRef]
- Upton, E.; Martin, B.; Wehmeyer, A. Allergic Rhinitis: To Sneeze or to Wheeze. Pollen Is the Question, What Is the Answer? South African Pharm. J. 2018, 85, 37–42. [Google Scholar]
- Migueres, M.; Dávila, I.; Frati, F.; Azpeitia, A.; Jeanpetit, Y.; Lhéritier-Barrand, M.; Incorvaia, C.; Ciprandi, G. Types of Sensitization to Aeroallergens: Definitions, Prevalences and Impact on the Diagnosis and Treatment of Allergic Respiratory Disease. Clin. Transl. Allergy 2014, 4, 16. [Google Scholar] [CrossRef]
- Lazova, S.; Baleva, M.; Priftis, S.; Naseva, E.; Velikova, T. Atopic Status in Children with Asthma and Respiratory Allergies—Comparative Analysis of Total IgE, ImmunoCAP Phadiatop/Fx5 and Euroimmun Pediatric Immunoblot. Sinusitis 2021, 6, 1. [Google Scholar] [CrossRef]
- Lazova, S.; Velikova, T.; Priftis, S.; Petrova, G. Identification of Specific IgE Antibodies and Asthma Control Interaction and Association Using Cluster Analysis in a Bulgarian Asthmatic Children Cohort. Antibodies 2020, 9, 31. [Google Scholar] [CrossRef] [PubMed]
- Gern, J.E. Virus/Allergen Interaction in Asthma Exacerbation. Ann. Am. Thorac. Soc. 2015, 12 (Suppl. S2), S137–S143. [Google Scholar] [CrossRef] [PubMed]
- Spergel, J.M. From Atopic Dermatitis to Asthma: The Atopic March. Ann. Allergy Asthma Immunol. 2010, 105, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-H.; Lue, K.-H. Association between Sensitized to Food Allergens and Childhood Allergic Respiratory Diseases in Taiwan. J. Microbiol. Immunol. Infect. 2020, 53, 812–820. [Google Scholar] [CrossRef] [PubMed]
- Wan, K.-S.; Wu, W.-F.; Liu, Y.-C.; Huang, C.-S.; Wu, C.-S.; Hung, C.-W.; Chang, Y.-S. Effects of Food Allergens on Asthma Exacerbations in Schoolchildren with Atopic Asthma. Food Agric. Immunol. 2017, 28, 310–314. [Google Scholar] [CrossRef][Green Version]
- 2021 GINA Report, Global Strategy for Asthma Management and Prevention. Available online: https://ginasthma.org/gina-reports/ (accessed on 1 January 2022).
- Juniper, E.F.; Gruffydd-Jones, K.; Ward, S. Asthma Control Questionnaire in Children: Validation, Measurement Properties, Interpretation. Eur. Respir. J. 2010, 36, 1410–1416. [Google Scholar] [CrossRef]
- Juniper, E.F.; Bousquet, J.; Abetz, L.; Bateman, E.D.; Goal Committee. Identifying “well-Controlled” and “Not Wellcontrolled” Asthma Using the Asthma Control Questionnaire. Respir. Med. 2006, 100, 616–621. [Google Scholar] [CrossRef]
- Standardization of Spirometry, 1994 Update. American Thoracic Society. Am. J. Respir. Crit. Care Med. 1995, 152, 1107–1136. [CrossRef]
- Pellegrino, R. Interpretative Strategies for Lung Function Tests. Eur. Respir. J. 2005, 26, 948–968. [Google Scholar] [CrossRef]
- Costa, L.D.C.; Costa, P.S.; Camargos, P.A.M. Exacerbation of Asthma and Airway Infection: Is the Virus the Villain? J. Pediatr. (Rio. J.) 2014, 90, 542–555. [Google Scholar] [CrossRef]
- Kwon, J.-M.; Shim, J.W.; Kim, D.S.; Jung, H.L.; Park, M.S.; Shim, J.Y. Prevalence of Respiratory Viral Infection in Children Hospitalized for Acute Lower Respiratory Tract Diseases, and Association of Rhinovirus and Influenza Virus with Asthma Exacerbations. Korean J. Pediatr. 2014, 57, 29. [Google Scholar] [CrossRef] [PubMed]
- Pakkasela, J.; Ilmarinen, P.; Honkamäki, J.; Tuomisto, L.E.; Andersén, H.; Piirilä, P.; Hisinger-Mölkänen, H.; Sovijärvi, A.; Backman, H.; Lundbäck, B.; et al. Age-Specific Incidence of Allergic and Non-Allergic Asthma. BMC Pulm. Med. 2020, 20, 9. [Google Scholar] [CrossRef] [PubMed]
- Sinisgalli, S.; Collins, M.S.; Schramm, C.M. Clinical Features Cannot Distinguish Allergic from Non-Allergic Asthma in Children. J. Asthma 2012, 49, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Vazquez Garcia, G.; Blake, K. Considerations for the Child with Nonatopic Asthma. Pediatr. Allergy. Immunol. Pulmonol. 2020, 33, 39–42. [Google Scholar] [CrossRef] [PubMed]
- Bahreinian, S.; Ball, G.D.C.; Colman, I.; Becker, A.B.; Kozyrskyj, A.L. Depression Is More Common in Girls with Nonatopic Asthma. Chest 2011, 140, 1138–1145. [Google Scholar] [CrossRef] [PubMed]
- Ullmann, N.; Mirra, V.; Di Marco, A.; Pavone, M.; Porcaro, F.; Negro, V.; Onofri, A.; Cutrera, R. Asthma: Differential Diagnosis and Comorbidities. Front. Pediatr. 2018, 6, 276. [Google Scholar] [CrossRef]
- Schroeder, A.; Kumar, R.; Pongracic, J.A.; Sullivan, C.L.; Caruso, D.M.; Costello, J.; Meyer, K.E.; Vucic, Y.; Gupta, R.; Kim, J.S.; et al. Food Allergy Is Associated with an Increased Risk of Asthma. Clin. Exp. Allergy 2009, 39, 261–270. [Google Scholar] [CrossRef]
- Roberts, G.; Patel, N.; Levi-Schaffer, F.; Habibi, P.; Lack, G. Food Allergy as a Risk Factor for Life-Threatening Asthma in Childhood: A Case-Controlled Study. J. Allergy Clin. Immunol. 2003, 112, 168–174. [Google Scholar] [CrossRef]
- Friedlander, J.L.; Sheehan, W.J.; Baxi, S.N.; Kopel, L.S.; Gaffin, J.M.; Ozonoff, A.; Fu, C.; Gold, D.R.; Phipatanakul, W. Food Allergy and Increased Asthma Morbidity in a School-Based Inner-City Asthma Study. J. Allergy Clin. Immunol. Pract. 2013, 1, 479–484. [Google Scholar] [CrossRef]
- Emons, J.A.M.; Gerth van Wijk, R. Food Allergy and Asthma: Is There a Link? Curr. Treat. Options Allergy 2018, 5, 436–444. [Google Scholar] [CrossRef]
- Kulis, M.D.; Smeekens, J.M.; Immormino, R.M.; Moran, T.P. The Airway as a Route of Sensitization to Peanut: An Update to the Dual Allergen Exposure Hypothesis. J. Allergy Clin. Immunol. 2021, 148, 689–693. [Google Scholar] [CrossRef] [PubMed]
- Emran, H.; Chieng, C.S.E.; Taib, S.; Cunningham, A.C. House Dust Mite Sensitisation and Association with Atopic Dermatitis in Brunei. Clin. Transl. Allergy 2019, 9, 65. [Google Scholar] [CrossRef] [PubMed]
- Atta, A.; Elbehady, R.; El Shobaky, A.; El Shabrawy, R. The Effect of Food Elimination and Probiotic Supplementation in Asthmatic Children with Food Allergy. Egypt. J. Pediatr. Allergy Immunol. 2021, 19, 19–26. [Google Scholar] [CrossRef]
- Twaroch, T.E.; Curin, M.; Valenta, R.; Swoboda, I. Mold Allergens in Respiratory Allergy: From Structure to Therapy. Allergy. Asthma Immunol. Res. 2015, 7, 205. [Google Scholar] [CrossRef]
- Kiguchi, T.; Yamamoto-Hanada, K.; Saito-Abe, M.; Sato, M.; Irahara, M.; Ogita, H.; Miyagi, Y.; Inuzuka, Y.; Toyokuni, K.; Nishimura, K.; et al. Pollen-Food Allergy Syndrome and Component Sensitization in Adolescents: A Japanese Population-Based Study. PLoS ONE 2021, 16, e0249649. [Google Scholar] [CrossRef] [PubMed]
- James, J.M.; Eigenmann, P.A.; Eggleston, P.A.; Sampson, H.A. Airway Reactivity Changes in Asthmatic Patients Undergoing Blinded Food Challenges. Am. J. Respir. Crit. Care Med. 1996, 153, 597–603. [Google Scholar] [CrossRef]
- Roberts, G.; Lack, G. Relevance of Inhalational Exposure to Food Allergens. Curr. Opin. Allergy Clin. Immunol. 2003, 3, 211–215. [Google Scholar] [CrossRef]
- Vassilopoulou, E.; Konstantinou, G.N.; Dimitriou, A.; Manios, Y.; Koumbi, L.; Papadopoulos, N.G. The Impact of Food Histamine Intake on Asthma Activity: A Pilot Study. Nutrients 2020, 12, 3402. [Google Scholar] [CrossRef]
- Kim, J.-H.; Choi, G.-S.; Kim, J.-E.; Ye, Y.-M.; Park, H.-S. Three Cases of Rice-Induced Occupational Asthma. Ann. Allergy, Asthma Immunol. 2010, 104, 353–354. [Google Scholar] [CrossRef]
- Hanson, C.; Brigham, E. Maternal Nutrition and Child Respiratory Outcomes: Paradigms of Lung Health and Disease. Eur. Respir. J. 2020, 55, 1902437. [Google Scholar] [CrossRef]
- Alwarith, J.; Kahleova, H.; Crosby, L.; Brooks, A.; Brandon, L.; Levin, S.M.; Barnard, N.D. The Role of Nutrition in Asthma Prevention and Treatment. Nutr. Rev. 2020, 78, 928–938. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Verduci, E.; Ghezzi, M.; Cena, H.; Pascuzzi, M.C.; Regalbuto, C.; Lamberti, R.; Rossi, V.; Manuelli, M.; Bosetti, A.; et al. Pediatric Obesity-Related Asthma: The Role of Nutrition and Nutrients in Prevention and Treatment. Nutrients 2021, 13, 3708. [Google Scholar] [CrossRef]
- Kim, H.Y.; Shin, Y.H.; Han, M.Y. Determinants of Sensitization to Allergen in Infants and Young Children. Korean J. Pediatr. 2014, 57, 205. [Google Scholar] [CrossRef] [PubMed]
- Carucci, L.; Nocerino, R.; Paparo, L.; Di Scala, C.; Berni Canani, R. Dietary Prevention of Atopic March in Pediatric Subjects With Cow’s Milk Allergy. Front. Pediatr. 2020, 8, 440. [Google Scholar] [CrossRef] [PubMed]
- Zicari, A.M.; Indinnimeo, L.; De Castro, G.; Zappalà, D.; Tancredi, G.; Bonci, E.; Celani, C.; Duse, M. Food Allergy and the Development of Asthma Symptoms. Int. J. Immunopathol. Pharmacol. 2012, 25, 731–740. [Google Scholar] [CrossRef]
- De Amici, M.; Ciprandi, G. The Age Impact on Serum Total and Allergen-Specific IgE. Allergy Asthma Immunol. Res. 2013, 5, 170. [Google Scholar] [CrossRef]
- Hong, S.-N.; Won, J.Y.; Nam, E.-C.; Kim, T.S.; Ryu, Y.-J.; Kwon, J.-W.; Lee, W.H. Clinical Manifestations of Allergic Rhinitis by Age and Gender: A 12-Year Single-Center Study. Ann. Otol. Rhinol. Laryngol. 2020, 129, 910–917. [Google Scholar] [CrossRef]
- Badloe, F.M.S.; De Vriese, S.; Coolens, K.; Schmidt-Weber, C.B.; Ring, J.; Gutermuth, J.; Kortekaas Krohn, I. IgE Autoantibodies and Autoreactive T Cells and Their Role in Children and Adults with Atopic Dermatitis. Clin. Transl. Allergy 2020, 10, 34. [Google Scholar] [CrossRef]


| Index | Value | |
|---|---|---|
| Number | 56 | |
| Sex | Male, n, % | 38, 68% |
| Female, n, % | 18, 32% | |
| Age, years, mean | 11.07 (5.3–17.5) | |
| Height, cm, mean | 111–181 (mean 145.2) | |
| Age, years, mean | 11.07 (5.3–17.5) | |
| Age groups | 5–8 yrs., n, % | 12, 21% |
| 8–12 yrs., n, % | 21, 38% | |
| 12–16 yrs, n, % | 15, 27% | |
| 16–18 yrs., n, % | 8, 14% | |
| FEV1 % predicted | >80%, n, % | 28, 50% |
| <80% and >60%, n, % | 18, 33% | |
| <60%, n, % | 10, 17% | |
| Mean BDR (ΔFEV1%pred., abs.change, mL) | 16.59%, 273 mL | |
| Atopic sensitization | Food and respiratory, n, % | 31, 55% |
| Food, n, % | 34, 60% | |
| Respiratory, n, % | 49, 87% | |
| ACQ7 score | Controlled asthma (<0.75) | 11, 20% |
| Partly controlled asthma (0.75–1.5) | 14, 25% | |
| Uncontrolled asthma (>1.5) | 31, 55% | |
| Asthma exacerbations, mean | 3.04 | |
| Asthma hospitalizations, mean | 1.26 | |
| Asthma Control and Severity Classification | Non- Atopics, % | Atopics, % | p | |
|---|---|---|---|---|
| GINA step | 1 | 73.7% | 54.4% | >0.05 |
| 2 | 21.1% | 32.2% | ||
| 3 | 5.3% | 12.2% | ||
| 4 | 0.0% | 1.1% | ||
| Severity according spirometry (FEV1 %predicted value) | >80% | 50.0% | 75.3% | 0.030 |
| <80% and >60% | 50.0% | 17.3% | ||
| <60% | 0.0% | 7.4% | ||
| Asthma control (ACQ7) | Controlled asthma (<0.75) | 57.9% | 31.1% | 0.023 |
| Partly controlled asthma (0.75–1.5) | 21.1% | 13.3% | ||
| Uncontrolled asthma (>1.5) | 21.1% | 55.6% | ||
| Symptom severity | Intermittent asthma | 42.1% | 23.3% | 0.076 |
| Mild persistent | 31.6% | 22.2% | ||
| Moderate and severe persistent asthma | 26.3% | 54.4% | ||
| ANOVA | Title 2 | Title 3 | ||||
|---|---|---|---|---|---|---|
| Source of Variation | SS | Df | MS | F | p-value | F crit |
| Between groups | 44.66667 | 2 | 22.33333 | 0.643715 | 0.547911 | 4.256495 |
| Within groups | 312.25 | 9 | 34.69444 | |||
| Total | 356.9167 | 11 |
| Food Allergen Positivity | Respiratory Allergen Positivity | Correlation Coefficient | p Value |
|---|---|---|---|
| Hazelnuts | Birch | 0.489 | 0.000 |
| Carrot | Birch | 0.303 | 0.003 |
| Hazelnuts | Grass mix | 0.301 | 0.004 |
| Apple | Cladosporium | 0.326 | 0.000 |
| Potato | Cladosporium | 0.413 | 0.000 |
| Clinical Outcome | Specific IgE | p |
|---|---|---|
| Risk of hospitalization | Cat | 0.002 |
| Dog | 0.052 | |
| Cladosporum | 0.005 | |
| Aspergillus | 0.054 | |
| Wormwood | 0.013 | |
| Soybean | 0.013 | |
| Risk of exacerbation | Cladosporium | 0.048 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lazova, S.; Hristova, D.; Priftis, S.; Velikova, T. Food Sensitization Impact on Asthma Attacks in Children According to Age Group. Allergies 2022, 2, 44-56. https://doi.org/10.3390/allergies2020005
Lazova S, Hristova D, Priftis S, Velikova T. Food Sensitization Impact on Asthma Attacks in Children According to Age Group. Allergies. 2022; 2(2):44-56. https://doi.org/10.3390/allergies2020005
Chicago/Turabian StyleLazova, Snezhina, Diana Hristova, Stamatios Priftis, and Tsvetelina Velikova. 2022. "Food Sensitization Impact on Asthma Attacks in Children According to Age Group" Allergies 2, no. 2: 44-56. https://doi.org/10.3390/allergies2020005
APA StyleLazova, S., Hristova, D., Priftis, S., & Velikova, T. (2022). Food Sensitization Impact on Asthma Attacks in Children According to Age Group. Allergies, 2(2), 44-56. https://doi.org/10.3390/allergies2020005









