Racism, Discrimination, and Harassment in Medical Schools in the UK: A Scoping Review
Abstract
1. Introduction
- -
- To map the types and nature of primary research activities concerning the extent and experience of discrimination, harassment, stereotyping, bullying, and victimisation in undergraduate medical education since the UK Parliament passed the Equality Act (2010). This act has been designated as a crucial landmark and main source of legal protection in the UK from racial harassment for university staff and students. The 2010 Act ensures that medical education institutions must provide equal opportunities for all students, regardless of their background or protected characteristics. This means that students must be given the same access to education, training, and resources, regardless of their protected characteristics. By following up on research after the Equality Act (2010) in this review, we anticipate that researchers, policymakers, and practitioners may identify areas where discrimination and inequality persist and develop strategies to address them.
- -
- To summarise and disseminate the current state of primary research activities concerning discrimination, harassment, stereotyping, bullying, and victimisation in undergraduate medical education and areas of content focus.
- -
- To determine areas of focus for undertaking full future systematic reviews of content.
- -
- To identify gaps in the existing evidence base in the context of discrimination, harassment, stereotyping, bullying, and victimisation in undergraduate medical education, providing directions for future research for the content of primary and secondary research.
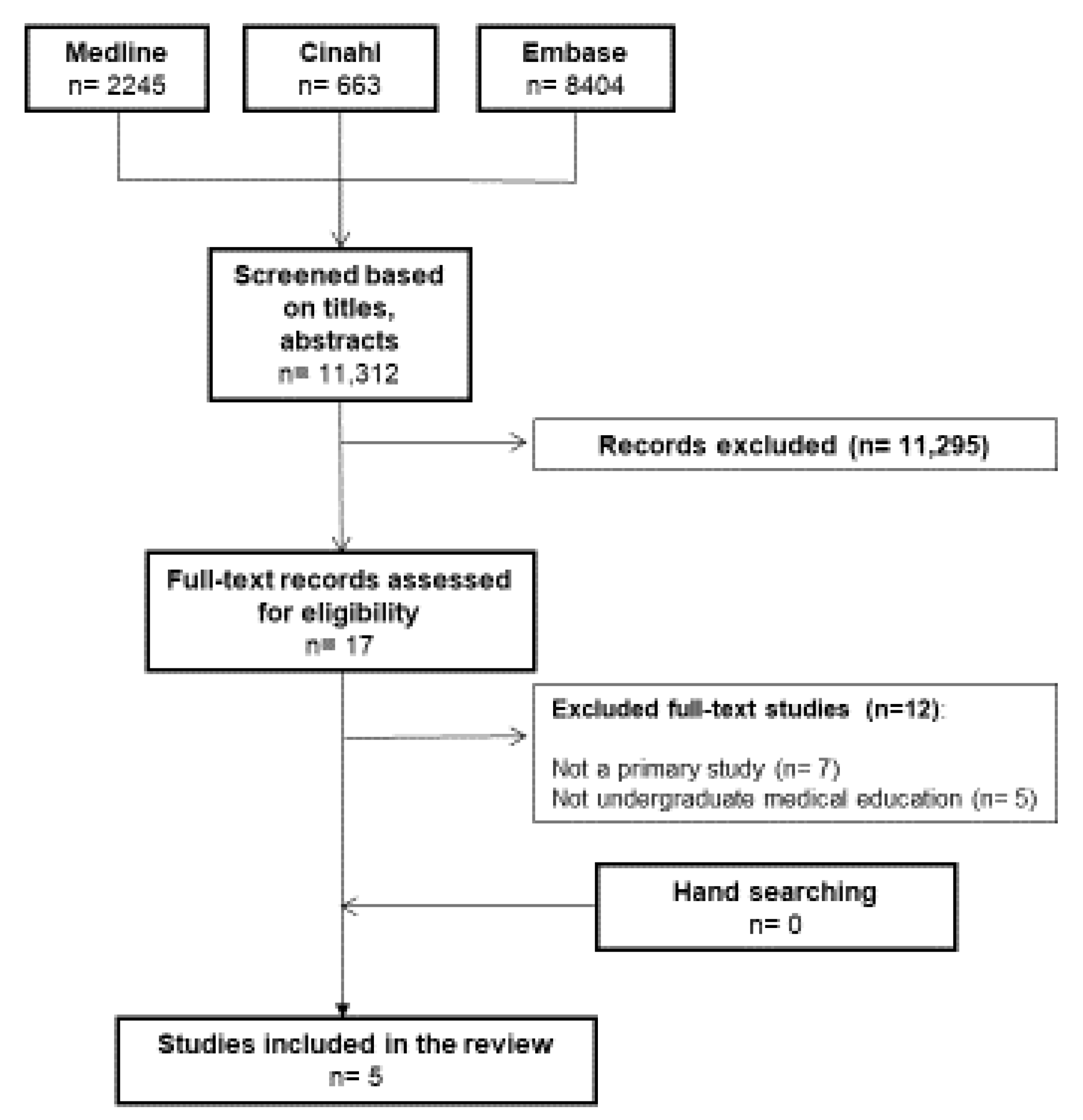
2. Methods
2.1. Stage 2: Identifying Relevant Studies
2.2. Stage 3: Study Selection
2.3. Stage 4: Charting the Data
- ▪
- Article identifiers (author(s), journal, and year of publication);
- ▪
- Geographic location;
- ▪
- Aim of the article, methods, ethics approval, and funding;
- ▪
- Number of participants;
- ▪
- Key findings in relation to the scope, conclusion, and limitations.
2.4. Stage 5: Collating, Summarising, and Reporting the Results
3. Results
3.1. Descriptive Findings: Characteristics of Included Studies
3.2. Characteristics of Participants
3.2.1. Prevalence of Discrimination and Harassment and Barriers to Reporting
3.2.2. Differential Attainment by Ethnicity in Medical Undergraduate Training
3.2.3. Barriers to Learning about Culture, Race, and Ethnicity
4. Discussion
5. Limitations
6. Conclusions
- The prevention and effective monitoring of harassment and discrimination in medical educational institutions;
- The standardisation of tools that measure harassment and discrimination;
- Detailed reporting on specific areas of any type of inequity in medical education are needed;
- One area of research here that requires quantitative analysis is the barrier to reporting; this may inform future interventions and reporting systems.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Study ID and Location | Aims, Objectives | Study Type | Recruitment, Sampling, Data Collection, and Analysis | Participant Description | Results | Limitations | Conclusions |
|---|---|---|---|---|---|---|---|
| Broad et al. (2018) Bristol | 1. Prevalence of harassment and discrimination 2. Reporting and factors that influence reporting | Mixed-method: quantitative survey, qualitative free-text reporting, and two single-gendered focus groups | 1318 medical students were e-mailed twice in March 2014. Convenience sampling was used to recruit eight male and eight female focus group participants for two focus groups. 16 students were included in the focus groups. Proportions and confidence intervals (CIs) were analysed using the Wilson score method, and associations were assessed with chi-squared analysis. The focus groups: framework analysis for the qualitative data and degrees of convergence. | 259 medical students all year groups. Gender: M 83 F 167, ethnicity: White 192, BME 61, heterosexual: 291, disability: 9 | 259 students responded to the survey (20%). Most participants experienced (63.3%, 95% CI 57.3 to 69.0) or witnessed (56.4%, 95% CI 50.3 to 62.3) at least one type of discrimination or harassment. Stereotyping was the most commonly witnessed (43.2%, 95%CI 37.4 to 49.3). Black and minority ethnic (BME) students witnessed and religious students experienced higher lack of provision (X2 4.73, p = 0.03; X2 4.38, p = 0.04); non-heterosexual students experienced higher joking, (X2 3.99, p = 0.04); students with disabilities experienced more stereotyping (X2 13.5, p < 0.01). Female students and students in clinical years had 2.6 (95% CI 1.3 to 5.3) and 3.6 (95% CI 1.9 to 7.0) greater likelihood of experiencing or witnessing all types of discrimination and harassment, respectively. Seven students reported incidents (5%, 95%CI 2.4 to 10.0); reporting was perceived as ineffective and victimising. | No validated questionnaire. The small sample size and the self-selected nature of the sample limit the conclusions. | Harassment and discrimination are prevalent in this sample and associated with gender, ethnicity, sexuality, disability, and year group. Reporting was rare and perceived as ineffective. |
| Study ID and Location | Aims, Objectives | Study Type | Recruitment, Sampling, Data Collection, and Analysis | Participant Description | Results | Limitations | Conclusions |
| Claridge et al. (2018) London | Exploring experiences of medical and biomedical science students and factors contributing to lower attainment | Qualitative, focus groups Audio-recorded, semi-structured interviews and ethnically homogenous student-led focus groups | An invitation was emailed to all ‘home’ students on undergraduate biomedical sciences and medicine courses (n = 1862) Exclusion: non-British non-domestic students. Participants for six focus groups were purposively recruited by ethnicity; Asian/Asian British (‘Asian’), Black/African/Caribbean/Black British (‘Black’), or White: English/Welsh/Scottish/Northern Irish/British. Staff range from lecturers to deans. | 41 students and 8 staff. 41 student participants with mean (SD, range) age = 21 (2.78, 18 to 31). Interviews were conducted with 24 students (12 female, 12 male, nine biomedical sciences, 15 medicine), with the following from each ethnicity: Asian: Bangladeshi (1), Chinese (1), Indian (5), Pakistani (3), and Other (2); Black: African (2) and Caribbean (1); White (8); and Irish (1) | Student data were best explained by two main themes: social factors and stereotyping, whilst staff data were also best explained by two main themes: social factors and student and staff behaviour. Social factors suggested that ethnically defined social networks and the informal transfer of knowledge impacted academic performance, isolating minority groups from useful academic information. BAME students may also be at a further disadvantage, being unable to attend social and academic functions for cultural or family reasons. Black students also mentioned changing their behaviour to combat negative stereotypes in a variety of contexts. | The gender, ethnicity, and age of the interviewer may have impacted how both students and staff responded in the interviews, with some perhaps uncomfortable discussing some topics in greater depth than others. It is possible that participants were not representative of all attainment levels. | Conscious or unconscious discrimination may negatively impact the abilities of BAME students, both in examinations and in coursework choice. Social networks are important for the transfer of academic knowledge and the impact ethnicity may have on their formation, with issues around segregation and information sharing outside defined groups. |
| Study ID and Location | Aims, Objectives | Study Type | Recruitment, Sampling, Data Collection, and Analysis | Participant Description | Results | Limitations | Conclusions |
| Yeates et al. (2017) West Midlands Medical School | Influence of students’ ethnicity (White vs. British Asian) on (1) the scores and feedback from OSCE examiners and (2) examiners’ cognitive processing of those performances, including their recollection accuracy and activation of an Asian stereotype when examining Asian students | Two-group, double-blinded, randomised, Internet-based experimental design | Participants were current UK undergraduate Objective Structured Clinical Exam (OSCE) examiners. Recruitment was undertaken by email; medical schools around the UK disseminated the invitation to OSCE examiners. Data analysed using ANOVA. | Scripted video materials of OSCE of medical students with different ethnic backgrounds were analysed. Examiners performed different cognitive tests (cf. Objective measures) | 159 OSCE examiners from 20 UK medical schools, broad range of clinical specialties, predominantly of White ethnicity.... Examiners responded to Asian stereotypical words (716 ms, 95% confidence interval (CI) 702–731 ms) faster than neutral words (769 ms, 95% CI 753–786 ms, p < 0.001), suggesting Asian stereotypes were activated (or at least active) in examiners’ minds. This occurred regardless of whether examiners observed stereotype-consistent or stereotype-inconsistent performances. Student ethnicity had no influence on examiners’ scores, on the feedback examiners gave, or on examiners’ memories for one performance. | Study was conducted in a simulated context, rather than in a real OSCE. Cannot exclude the possibility that examiners’ judgements could be influenced by students’ ethnicity after a more prolonged series of performances due to (for example) fatigue or lapses in concentration, or that different samples of performance (displaying a different range of behaviours by Asian students) could produce an effect. | Examiners had a stereotype that was active at the time of judging performances, which does not appear to have been applied to their judgements. Examiner bias is not responsible for differential attainment by BME students. |
| Study ID and Location | Aims, Objectives | Study Type | Recruitment, Sampling, Data Collection, and Analysis | Participant Description | Results | Limitations | Conclusions |
| Roberts et al. (2010) Two medical schools in northern England | To explore the impact on students of two contrasting pedagogic approaches (a school offering early patient contact in the first 2 years was compared with one using paper-based patient scenarios only) to undergraduate learning about cultural diversity | An exploratory, qualitative research method was used, adopting an ‘inductive’ approach to data analysis and theory generation | Pragmatic recruitment. Focus groups were conducted at each site over a 3-month period, in small teaching rooms familiar to the students. Discussion was audio-recorded after seeking informed written consent from all participants. | Students (years 1 and 2) from seven selected groups (n = 49) were recruited pragmatically at sites A and B. Ethnic minority students = 20 (40.8%) | Barriers to learning about race, culture and ethnicity identified: (a) ‘institutional marginalisation’ of the subject, and (b) ‘student resistance’ to formal learning about cultural diversity. | The study was conducted using only year two medical students. Data collection was limited to two medical schools situated in northern England. Research team composition was British, White, and female. | The study found two potentially competing views. First, students claimed that although cultural diversity was important, their medical schools marginalised and failed to adequately support effective teaching. Second, in contrast, they claimed that the medical school was an ‘inappropriate’ setting for successful teaching about cultural diversity. Students did not consider the subject matter to be of central relevance to biomedicine. |
| Study ID and Location | Aims, Objectives | Study Type | Recruitment, Sampling, Data Collection, and Analysis | Participant Description | Results | Limitations | Conclusions |
| Morrison et al. (2019) | Examining the potential reasons for under performance by BME graduate-entry medical students, exploring their experiences of undergraduate medical training and their perceptions of barriers and facilitators to performance | Qualitative methods (focus groups with semi-structured interviews) | Graduate-entry MBChB students from all four cohorts were recruited using volunteer and snowball sampling. For each group, participants were randomly assigned a number to ease anonymisation during transcription. Participants were subsequently asked to self-report their ethnicity using the 2011 UK census categories. | 24 graduate-entry MBChB students self-identified as being from Black and Minority Ethnic (BME) backgrounds | Lack of BME representation and lack of understanding of cultural differences among staff impacted their experiencee. Students also reported a lack of trust in the institution’s ability to support BME students, with many not seeking support. Students’ narratives indicated that they had to mask their identity to fit in among their peers and to avoid negative stereotyping. Although rare, students faced overt racism from their peers and from patients. Many students reported feelings of isolation, reduced self-confidence, and low self-esteem. | BME students were not a homogeneous group: as individuals, they had unique identities as well as different ethnic, cultural, socioeconomic, and educational backgrounds. This study was not able to examine how these intersect to shape individual students’ experiences of medical education. | BME students reported experiencing relationship issues with other students and academic and clinical staff, lack of trust in the institution, and some racist events. |
| Excluded Studies | Reason for Exclusion |
|---|---|
| Al-Haddad et al. (2022) | Meta-ethnography (systematic review) |
| Joseph et al. (2021) | Narrative review |
| Khan and Mian (2020) | Opinion letter |
| Lim et al. (2021) | View of students on institutional discrimination—not a primary study |
| Woolf et al. (2018) | Postgraduate medical education |
| Gostelow et al. (2018) | Symposium workshop of students on institutional discrimination—not a primary study |
| Nightingale et al. (2022) | No medical students included in this study |
| Alwazzan (2018) | Review |
| Clements et al. (2020) | Postgraduate students |
| Denney et al. (2013) | Postgraduate students |
| Woolf et al. (2018) | Postgraduate students |
| Fyfe et al. (2022) | Guidelines |
Appendix B. MEDLINE EBSCOhost Platform
| # | Query | Limiters/Expanders | Last Run Via | Results |
| S22 | S14 AND S21 | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S21 | S17 OR S20 | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S20 | S18 OR S19 | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S19 | “junior doctor” OR (MH “Physician Assistants+”) OR (MH “Medical Staff, Hospital”) | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S18 | junior doctor | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S17 | S15 OR S16 | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S16 | postgraduate medical education | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S15 | (MH “Education, Medical+”) OR (MH “Education, Medical, Undergraduate”) OR (MH “Education, Medical, Graduate+”) OR (MH “Education, Medical, Continuing”) OR (MH “Education, Premedical”) OR “medical education” | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S14 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S13 | inequity | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S12 | inequality | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S11 | (MH “Discrimination, Psychological+”) OR (MH “Discrimination Learning”) OR (MH “Social Discrimination+”) OR (MH “Racism+”) OR (MH “Sexism”) OR (MH “Weight Prejudice”) OR (MH “Speech Discrimination Tests”) OR “discrimination” | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S10 | (MH “Bullying+”) OR “bullying” OR (MH “Cyberbullying”) | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S9 | S5 OR S6 OR S7 OR S8 | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S8 | “stereotype” | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S7 | stereotype | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S6 | (MH “Stereotyping”) | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S5 | stereotyping | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S4 | “Intimidation” | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S3 | S1 OR S2 | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S2 | “harassment” | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
| S1 | (MH “Harassment, Non-Sexual+” | Expanders- Apply equivalent subjects Search modes- Boolean/Phrase | Interface- EBSCOhost Research Databases Search Screen- Basic Search Database- MEDLINE with Full Text | Display |
References
- Ackerman-Barger, Kupiri, Dowin Boatright, Rosana Gonzalez-Colaso, Regina Orozco, and Darin Latimore. 2020. Seeking Inclusion Excellence: Understanding Racial Microaggressions as Experienced by Underrepresented Medical and Nursing Students. Academic medicine: Journal of the Association of American Medical Colleges 95: 758–763. [Google Scholar] [CrossRef] [PubMed]
- Alexander, Claire, and Jason Arday. 2015. Aiming Higher: Race, Inequality and Diversity in the Academy. London: Runnymede Trust. [Google Scholar]
- Alexander, Claire, and William Shankley. 2020. Ethnic inequalities in the state education system in England. In Ethnicity and Race in the UK: State of the Nation, 1st ed. Edited by Claire Alexander, William Shankley, Bridget Byrne, Omar Khan and James Nazro. Bristol: Bristol University Press, pp. 93–126. [Google Scholar] [CrossRef]
- Al-Haddad, Moh, Susan Jamieson, and Evi Germeni. 2022. International medical graduates’ experiences before and after migration: A meta-ethnography of qualitative studies. Medical Education 56: 504–15. [Google Scholar] [CrossRef] [PubMed]
- Alwazzan, Lulu. 2018. Conceptualising discrimination in medical education: The hierarchy, the power. Medical Education 52: 356–58. [Google Scholar] [CrossRef] [PubMed]
- Arday, Jason, and Heidi S. Mirza, eds. 2018. Dismantling Race in Higher Education. Basingstoke: Palgrave Macmillan. [Google Scholar]
- Arksey, Hilary, and Lisa O’Malley. 2005. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology 8: 19–32. [Google Scholar] [CrossRef]
- Bezrukova, Katerina, Chester S. Spell, Jamie L. Perry, and Karen A. Jehn. 2016. A meta-analytical integration of over 40 years of research on diversity training evaluation. Psychological Bulletin 142: 1227. [Google Scholar] [CrossRef]
- BMA (British Medical Assocation). 2022. Racism in Medicine. Available online: https://www.bma.org.uk/media/5746/bma-racism-in-medicine-survey-report-15-june-2022.pdf (accessed on 13 May 2022).
- Broad, Jonathan, Marion Matheson, Fabienne Verrall, Anna K. Taylor, Daniel Zahra, Louise Alldridge, and Gene Feder. 2018. Discrimination, harassment and non-reporting in UK medical education. Medical Education 52: 414–26. [Google Scholar] [CrossRef]
- Carter, Madeline, Neill Thompson, Paul Crampton, Gill Morrow, Bryan Burford, Christopher Gray, and Jan Illing. 2013. Workplace bullying in the UK NHS: A questionnaire and interview study on prevalence, impact and barriers to reporting. BMJ Open 3: e002628. [Google Scholar] [CrossRef]
- Claridge, Hugh, Stone Khadija, and Michael Ussher. 2018. The ethnicity attainment gap among medical and biomedical science students: A qualitative study. BMC Medical Education 18: 1–12. [Google Scholar] [CrossRef]
- Clements, Joshua M., Martin King, Rebecca Nicholas, Oliver Burdall, Elizabeth Elsey, Vittoria Bucknall, Ayoola Awopetu, Helen Mohan, Gemma Humm, Deirdre M. Nally, and et al. 2020. Bullying and undermining behaviours in surgery: A qualitative study of surgical trainee experiences in the United Kingdom (UK) and Republic of Ireland (ROI). International Journal of Surgery 84: 219–25. [Google Scholar] [CrossRef]
- Curtis, Ellen F., Janice L. Dreachslin, and Marie Sinioris. 2007. Diversity and cultural competence training in health care organizations: Hallmarks of success. The Health Care Manager 26: 255–62. [Google Scholar] [CrossRef]
- Daniel, Michelle, Morris Gordon, Madalena Patricio, Ahmad Hider, Cameron Pawlik, Rhea Bhagdev, Shoaib Ahmad, Sebastian Alston, Sophie Park, Teresa Pawlikowska, and et al. 2021. An update on developments in medical education in response to the COVID-19 pandemic: A BEME scoping review: BEME Guide No. 64. Medical Teacher 43: 253–71. [Google Scholar] [CrossRef]
- Denney, Mei L., Adrian Freeman, and Richard Wakeford. 2013. MRCGP CSA: Are the examiners biased, favouring their own by sex, ethnicity, and degree source? British Journal of General Practice 63: e718–e725. [Google Scholar] [CrossRef]
- EHRC (Equalities and Human Rights Commission). 2019. Tackling Racial Harassment: Universities Challenged. Available online: https://www.equalityhumanrights.com/en/publication-download/tackling-racial-harassment-universities-challenged (accessed on 10 June 2022).
- Equality Act. 2010. s. 9 (1). Available online: www.legislation.gov.uk/ukpga/2010/15/section/9 (accessed on 10 June 2022).
- Esmail, Aneez, and Sam Everington. 2021. Eradicating ethnic disadvantage in medical education and regulation. BMJ 374: n1725. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, Chloë, and Samia Hurst. 2017. Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics 18: 1–18. [Google Scholar] [CrossRef]
- Fnais, Naif, Charlene Soobiah, Maggie H. Chen, Erin Lillie, Laure Perrier, Mariam Tashkhandi, Sharon E. Straus, Muhammad Mamdani, Mohammed Al-Omran, and Andrea C. Tricco. 2014. Harassment and discrimination in medical training: A systematic review and meta-analysis. Academic Medicine 89: 817–27. [Google Scholar] [CrossRef] [PubMed]
- Fyfe, Molly, Jo Horsburgh, Julia Blitz, Neville Chiavaroli, Sonia Kumar, and Jennifer Cleland. 2022. The do’s, don’ts and don’t knows of redressing differential attainment related to race/ethnicity in medical schools. Perspectives on Medical Education 11: 1–14. [Google Scholar] [CrossRef] [PubMed]
- General Medical Council. 2014. National Training Surveys. Available online: https://www.gmc-uk.org/education/surveys.asp (accessed on 10 April 2023).
- GMC (General Medical Council). 2022. Equality. Diversity and Inclusion Policy 2022. Available online: https://www.gmc-uk.org/about/how-we-work/equality-diversity-and-inclusion (accessed on 16 April 2023).
- Gordon, Morris, and Trevor Gibbs. 2014. STORIES Statement: Publication Standards for Healthcare Education Evidence Synthesis. BMC Medicine 12: 143. [Google Scholar] [CrossRef]
- Gostelow, Naomi, Amali Lokugamage, and Faye Gishen. 2018. Celebrating diversity to promote and create inclusive curricula. Medical Education 52: 551–52. [Google Scholar] [CrossRef]
- Green, Kaye-Alese, Rebecca Wolinsky, Sabreea J. Parnell, Daniela Del Campo, Ajay S. Nathan, Priya S. Garg, Samantha E. Kaplan, and Shoumita Dasgupta. 2022. Deconstructing Racism, Hierarchy, and Power in Medical Education: Guiding Principles on Inclusive Curriculum Design. Academic Medicine 97: 804–11. [Google Scholar] [CrossRef]
- Halim, Usman A., and David M. Riding. 2018. Systematic review of the prevalence, impact and mitigating strategies for bullying, undermining behaviour and harassment in the surgical workplace. British Journal of Surgery 105: 1390–97. [Google Scholar]
- Hammick, Marilyn, Timothy Dornan, and Yvonne Steinert. 2010. Conducting a best evidence systematic review. Part 1: From idea to data coding. BEME Guide No. 13. Medical Teacher 32: 3–15. [Google Scholar] [CrossRef]
- Haq, Inam, Jenny Higham, Richard Morris, and Jane Dacre. 2005. Effect of ethnicity and gender on performance in undergraduate medical examinations. Medical Education 39: 1126–28. [Google Scholar] [CrossRef] [PubMed]
- Hill, Katherine A., Elizabeth A. Samuels, Cary P. Gross, Mayur M. Desai, Nicole Sitkin Zelin, Darin Latimore, Stephen J. Huot, Laura D. Cramer, Ambrose H. Wong, and Dowin Boatright. 2020. Assessment of the prevalence of medical student mistreatment by sex, race/ethnicity, and sexual orientation. JAMA Internal Medicine 180: 653–65. [Google Scholar] [CrossRef]
- Johnson, Sarah. 2016. NHS Staff Lay Bare a Bullying Culture; The Guardian. Available online: https://www.theguardian.com/society/2016/oct/26/nhs-staff-bullying-culture-guardian-survey (accessed on 10 April 2023).
- Joseph, Olivia Rochelle, Stuart W. Flint, Rianna Raymond-Williams, Rossby Awadzi, and Judith Johnson. 2021. Understanding Healthcare Students’ Experiences of Racial Bias: A Narrative Review of the Role of Implicit Bias and Potential Interventions in Educational Settings. International Journal of Environmental Research and Public Health 18: 12771. [Google Scholar] [CrossRef] [PubMed]
- Khan, Shujhat, and Areeb Mian. 2020. Racism and medical education. Lancet Infect Dis 20: 1009. [Google Scholar] [CrossRef]
- Kmietowicz, Zosia. 2020. Are medical schools turning a blind eye to racism? BMJ 368: m420. [Google Scholar] [CrossRef] [PubMed]
- Lim, Guan Hui Tricia, Zeluleko Sibanda, Joshua Erhabor, Soham Bandyopadhyay, and The Neurology and Neurosurgery Interest Group. 2021. Students’ perceptions on race in medical education and healthcare. Perspectives on Medical Education 10: 130–34. [Google Scholar] [CrossRef]
- Morrison, Nariell, Michelle Machado, and Clare Blackburn. 2019. Student perspectives on barriers to performance for black and minority ethnic graduate-entry medical students: A qualitative study in a West Midlands medical school. BMJ Open 9: e032493. [Google Scholar] [CrossRef]
- Nagpaul, Chaand. 2022a. Racism in Medicine must be Tacked for the NHS to Honour Its Founding Principles and Maximise Its Workforce Potential. NHS Race and Health Observatory Blog. Available online: https://www.nhsrho.org/blog/racism-in-medicine-must-be-tackled-if-the-nhs-is-to-maximise-its-workforce-potential-and-honour-its-founding-principles/ (accessed on 20 May 2022).
- Nagpaul, Chaand. 2022b. Racism is wrecking the lives of doctors, affecting patient care, and jeopardising services. BMJ 377: o1515. [Google Scholar] [CrossRef]
- Ng, Lillian, Charlie Lin, and Marcus A. Henning. 2019. A Narrative Review of Discrimination Experienced by Medical Students. Medical Science Educator 30: 577–84. [Google Scholar] [CrossRef]
- Nightingale, Julie, Jackie Parkin, Pete Nelson, Shirley Masterson-Ng, Jacqui Brewster, Temitope Labinjo, Deborah Amoakoh, David Lomas, Ifrah Salih, and Deborah Harrop. 2022. Multiple stakeholder perspectives of factors influencing differential outcomes for ethnic minority students on health and social care placements: A qualitative exploration. BMC Medical Education 22: 17. [Google Scholar] [CrossRef] [PubMed]
- Orom, Heather, Teresa Semalulu, and Willie Underwood, 3rd. 2013. The social and learning environments experienced by underrepresented minority medical students: A narrative review. Academic Medicine 88: 1765–77. [Google Scholar] [CrossRef] [PubMed]
- RCP (Royal College of Physicians). 2019. Survey of Medical Certificate of Completion of Training (CCT) Holders’ Career Progression. Available online: https://www.rcplondon.ac.uk/projects/outputs/2019-survey-medical-certificate-completion-training-cct-holders-career-progression (accessed on 20 May 2022).
- Roberts, Jane H., Tom Sanders, Karen Mann, and Val Wass. 2010. Institutional marginalisation and student resistance: Barriers to learning about culture, race and ethnicity. Advances in Health Sciences Education 15: 559–71. [Google Scholar] [CrossRef] [PubMed]
- Steele, Claude M., and Joshua Aronson. 1995. Stereotype threat and the intellectual test performance of African Americans. Journal of Personality and Social Psychology 69: 797. [Google Scholar] [CrossRef]
- Sue, Derald Wing, Christina M. Capodilupo, Gina C. Torino, Jennifer M. Bucceri, Aisha M. B. Holder, Kevin L. Nadal, and Marta Esquilin. 2007. Racial microaggressions in everyday life: Implications for clinical practice. American Psychologist 62: 271. [Google Scholar] [CrossRef]
- Tricco, Andrea C., Erin Lillie, Wasifa Zarin, Kelly K. O’Brien, Heather Colquhoun, Danielle Levac, David Moher, Micah D. J. Peters, Tanya Horsley, Laura Weeks, and et al. 2018. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine 169: 467–73. [Google Scholar] [CrossRef] [PubMed]
- Universities UK. 2019. Black and Ethnic Minority Student Attainment at UK Universities: Closing the Gap. Available online: https://www.universitiesuk.ac.uk/sites/default/files/field/downloads/2021-07/bame-student-attainment.pdf (accessed on 20 May 2022).
- Van Ryn, Michelle, Diana J. Burgess, John F. Dovidio, Sean M. Phelan, Somnath Saha, Jennifer Malat, Joan M. Griffin, Steven S. Fu, and Sylvia Perry. 2011. The impact of racism on clinician cognition, behavior, and clinical decision making. Du Bois Review 8: 199–218. [Google Scholar] [CrossRef]
- Vaughan, Suzanne. 2013. Medical Students’ Experience and Achievement: The Effect of Ethnicity and Social Networks. Doctoral thesis, University of Manchester, Manchester, UK. [Google Scholar]
- Woolf, Katherine. 2009. The academic underperformance of medical students from ethnic minorities. Ph.D. thesis, UCL, (University College London), London, UK. [Google Scholar]
- Woolf, Katherine. 2020. Differential attainment in medical education and training. BMJ 368: m339. [Google Scholar] [CrossRef]
- Woolf, Katherine, Henry W. W. Potts, and Chris I. McManus. 2011. Ethnicity and academic performance in UK trained doctors and medical students: Systematic review and meta-analysis. BMJ 342: d901. [Google Scholar] [CrossRef]
- Woolf, Katherine, Judith Cave, Trisha Greenhalgh, and Jane Dacre. 2008. Ethnic stereotypes and the underachievement of UK medical students from ethnic minorities: Qualitative study. BMJ 337: a1220. [Google Scholar] [CrossRef]
- Woolf, Katherine, Rowena Viney, Antonia Rich, Hirosha Jayaweera, and Ann Griffin. 2018. Organisational perspectives on addressing differential attainment in postgraduate medical education: A qualitative study in the UK. BMJ Open 8: e021314. [Google Scholar] [CrossRef] [PubMed]
- Yeates, Peter, Katherine Woolf, Emyr Benbow, Ben Davies, Mairhead Boohan, and Kevin Eva. 2017. A randomised trial of the influence of racial stereotype bias on examiners’ scores, feedback and recollections in undergraduate clinical exams. BMC Medicine 15. [Google Scholar] [CrossRef] [PubMed]
| Inclusion | Exclusion | |
|---|---|---|
| Population | Undergraduate medical students | Studies not related to undergraduate medical training |
| Exposure | Any type of harassment, discrimination, stereotyping, bullying, victimisation, marginalisation, etc. (as defined in the study) | NA |
| Outcome | Impact on student attainment, wellbeing, perceptions, trust, experiences (or as described in the study) | NA |
| Setting | UK (studies performed from 2010 onwards) | Any other country or year |
| Study design | Primary research studies (qualitative, quantitative, mixed-method studies) | Guidelines, systematic reviews, literature reviews, ideas, editorials, opinion letters |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montasem, A.; Gjuladin-Hellon, T.; Awan, H.; Aine, B.; Whyte, J.; Alqadah, N.; Ibeachu, C. Racism, Discrimination, and Harassment in Medical Schools in the UK: A Scoping Review. Genealogy 2023, 7, 32. https://doi.org/10.3390/genealogy7020032
Montasem A, Gjuladin-Hellon T, Awan H, Aine B, Whyte J, Alqadah N, Ibeachu C. Racism, Discrimination, and Harassment in Medical Schools in the UK: A Scoping Review. Genealogy. 2023; 7(2):32. https://doi.org/10.3390/genealogy7020032
Chicago/Turabian StyleMontasem, Alexander, Teuta Gjuladin-Hellon, Hassan Awan, Brian Aine, Julian Whyte, Norah Alqadah, and Chukwuemeka Ibeachu. 2023. "Racism, Discrimination, and Harassment in Medical Schools in the UK: A Scoping Review" Genealogy 7, no. 2: 32. https://doi.org/10.3390/genealogy7020032
APA StyleMontasem, A., Gjuladin-Hellon, T., Awan, H., Aine, B., Whyte, J., Alqadah, N., & Ibeachu, C. (2023). Racism, Discrimination, and Harassment in Medical Schools in the UK: A Scoping Review. Genealogy, 7(2), 32. https://doi.org/10.3390/genealogy7020032





