Addressing Substance Use Utilizing a Community-Based Program among Urban Native American Youth Living in Florida
Abstract
1. Introduction
Theoretical Framework
2. Method
Research Design
3. Urban Talking Circle (UTC) Intervention
4. Standard Substance Abuse Education (SE)
4.1. Sample and Setting
4.2. Measurements
5. Results
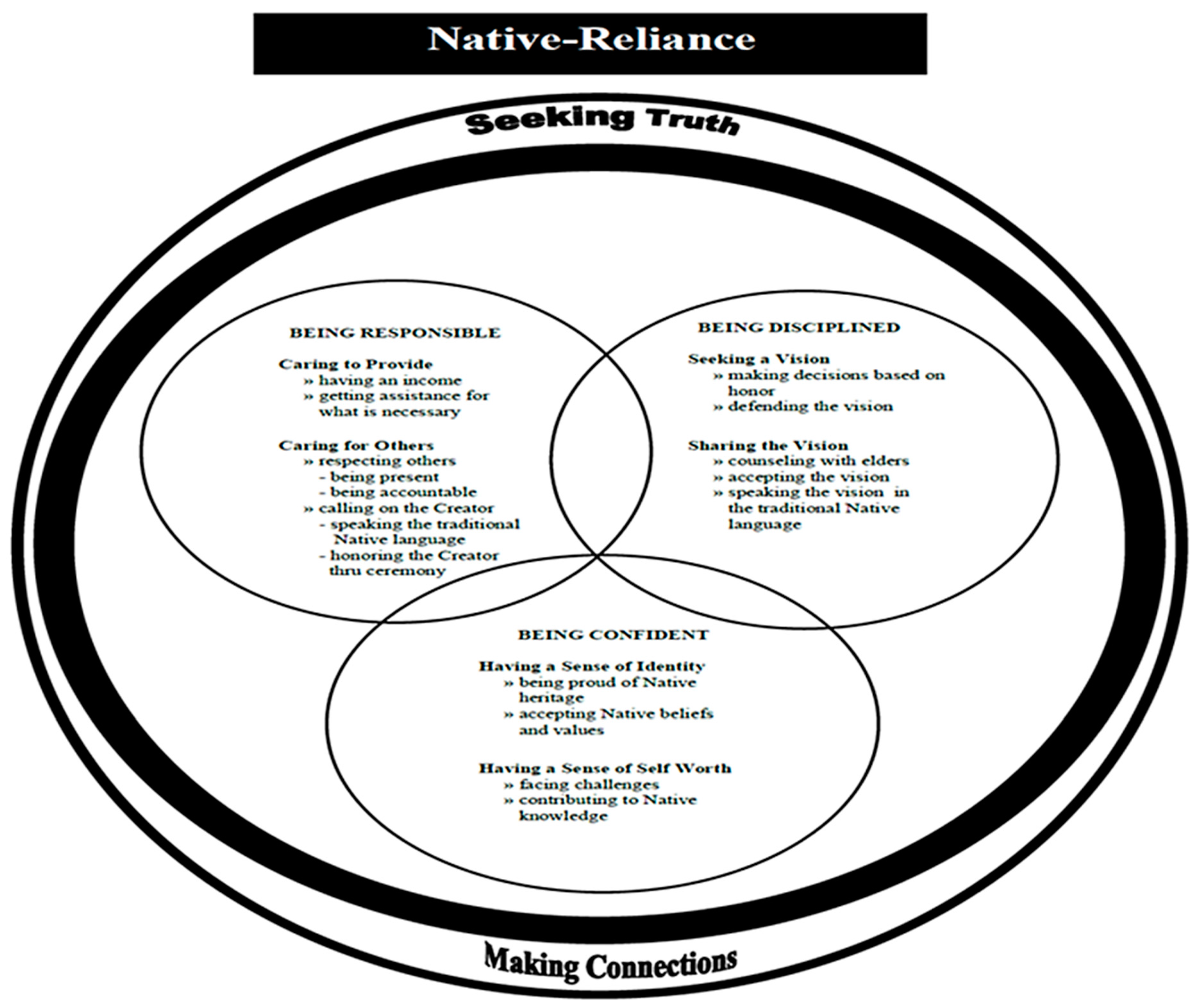
5.1. Native-Reliance
5.2. Drug Use Interest
5.3. NAAMY
6. Discussion
Further Research
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Allen, James, Gerald V. Mohatt, Carlotta Ching Ting Fok, David Henry, Rebekah Burket, and People Awakening Team. 2014. A protective factors model for alcohol abuse and suicide prevention among Alaska Native youth. American Journal of Community Psychology 54: 125–39. [Google Scholar] [CrossRef]
- CDC (Centers for Disease Control and Prevention). 2013. CDC Health Disparities & Inequalities Report—United States, 2013. Centers for Disease Control and Prevention Morbidity and Mortality Report 62: 1–184. Available online: http://www.cdc.gov/mmwr/pdf/other/su6203.pdf (accessed on 14 June 2016).
- CDC (Centers for Disease Control and Prevention). 2014a. American Indian & Alaska Native Populations: Ten Leading Causes of Death. Available online: http://www.cdc.gov/nchs/fa10mericanerican-indian-health.htm (accessed on 14 June 2016).
- CDC (Centers for Disease Control and Prevention). 2014b. Youth risk behavior surveillance: United States, 2013. Morbidity and Mortality Weekly Report 63: 1–168. Available online: http://www.cdc.gov/mmwr/pdf/ss/ss6304.pdf (accessed on 14 June 2016).
- CDC (Centers for Disease Control and Prevention). 2015. American Indian and Alaska Native Populations. Available online: http://www.cdc.gov/nchs/fa10mericanerican-indianhealth.htm (accessed on 14 June 2016).
- CDC (Centers for Disease Control and Prevention). 2017. Leading Causes of Death and Numbers of Deaths, by Sex, race, and Hispanic Origin: United States, 1980 and 2017. Available online: https://www.cdc.gov/nchs/data/hus/2018/008.pdf (accessed on 14 August 2017).
- CDC (Centers for Disease Control and Prevention), and J. Heron. 2019. Deaths: Leading Causes for 2017. National Vital Statistics Reports 68: 1–77. Available online: https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_06-508.pdf (accessed on 10 January 2019).
- CDC (Centers for Disease Control and Prevention), K. Kochanek, S. Murphy, J. Xu, and E. Arias. 2019a. Deaths Final Data for 2017. National Vital Statistics Reports 68: 1–77. Available online: https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_09-508.pdf (accessed on 10 January 2019).
- CDC (Centers for Disease Control and Prevention), S. Scholl, M. Kariisa, N. Wilson, and G. Baldwin. 2019b. Drug and opioid-involved overdose deaths—United States, 2013–2017. Morbidity and Mortality Weekly Report (MMWR), 1–9. Available online: https://www.cdc.gov/mmwr/volumes/67/wr/pdfs/mm675152e1-H.pdf (accessed on 10 January 2019).
- Chadwick, Bruce, and Joseph Stauss. 1975. The assimilation of American Indians into urban society: The Seattle case. Human Organization 34: 359–69. Available online: http://www. sfaajournals.net/doi/abs/10.17730/humo.34.4.12p371m06785376m?journalCode=humo (accessed on 10 January 2019). [CrossRef]
- Croff, Raina L., Traci R. Rieckmann, and John Doug Spence. 2014. Provider and state perspectives on implementing cultural-based models of care for American Indian and Alaska Native patients with substance use disorders. The Journal of Behavioral Health Services & Research 41: 64–79. [Google Scholar] [CrossRef]
- DARE (Drug Resistance Education Program). 2016. DARE’s Keepin’ it Real Elementary and Middle School Curriculums Adhere to Lessons from Prevention Research Principles. Available online: http://www.dare.org/d-a-r-e-s-keepin-it-real-elementary-and-middle-schoolcurriculums-adhere-to-lessons-from-prevention-research-principles/ (accessed on 10 January 2019).
- Darroch, Francine, Audrey Giles, Priscilla Sanderson, Lauren Brooks-Cleator, Anna Schwartz, Darold Joseph, and Roger Nosker. 2017. The United States does CAIR about cultural safety: Examining cultural safety within Indigenous health contexts in Canada and the United States. Journal of Transcultural Nursing: Official Journal of the Transcultural Nursing Society 28: 269–77. [Google Scholar] [CrossRef]
- Dickerson, Daniel, Francis Robichaud, Cheryl Teruya, Kathleen Nagaran, and Yih-Ing Hser. 2012. Utilizing drumming for American Indians/Alaska Natives with substance use disorders: A focus group study. The American Journal of Drug and Alcohol Abuse 38: 505510. [Google Scholar] [CrossRef]
- Donovan, Dennis M., Lisa Rey Thomas, Robin Little Wing Sigo, Laura Price, Heather Lonczak, Nigel Lawrence, Katie Ahvakana, Lisette Austin, Albie Lawrence, Abby Purser, and et al. 2015. Healing of the canoe: Preliminary results of a culturally grounded intervention to prevent substance abuse and promote tribal identity for Native youth in two Pacific Northwest tribes. American Indian and Alaska Native Mental Health Research Online 22: 42–76. Available online: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4374439/ (accessed on 10 January 2019). [CrossRef] [PubMed]
- Evans-Campbell, Teresa. 2008. Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. Journal of Interpersonal Violence 23: 316–38. [Google Scholar] [CrossRef] [PubMed]
- Gone, Joseph P., and Joseph E. Trimble. 2012. American Indian and Alaska Native mental health: Diverse perspective on enduring disparities. Annual Review of Clinical Psychology 8: 131–60. [Google Scholar] [CrossRef] [PubMed]
- Goodkind, Jessica R., Kimberly Ross-Toledo, Susie John, Janie Lee Hall, Lucille Ross, Lance Freeland, Twila Becenti-Fundark, Charlene Poola, Regina Roanhorse, Ernest Coletta, and et al. 2011. Rebuilding trust: A community, multiagency, state, and university partnership to improve behavioral health care for American Indian youth, their families, and communities. American Journal of Community Psychology 39: 452–77. [Google Scholar] [CrossRef]
- Hodge, Felicia S., and Karabi Nandy. 2011. Predictors of wellness and American Indians. Journal of Health Care for the Poor & Underserved 22: 791–803. [Google Scholar] [CrossRef]
- Hook, Joshua N., Don E. Davis, Jesse Owen, Everett L. Worthington, Jr., and Shawn O. Utsey. 2013. Cultural humility: Measuring openness to culturally diverse clients. Journal of Counseling Psychology 60: 353–66. [Google Scholar] [CrossRef]
- Knibb-Lamouche, James, and IOM (Institute of Medicine). 2012. Culture as a Social Determinant of Health. Available online: http://www.ncbi.nlm.nih.gov/books/NBK201298/ (accessed on 14 June 2016).
- Kulis, Stephen, Leslie Jumper Reeves, Patricia Allen Dustman, and Marissa O’Neill. 2011. Strategies to resist drug offers among urban American Indian youth of the Southwest: An enumeration, classification, and analysis by substance and offeror. Substance Use & Misuse 46: 1395–409. [Google Scholar] [CrossRef]
- Lowe, John. 2002. Cherokee self-reliance. Journal of Transcultural Nursing 13: 287–95. [Google Scholar] [CrossRef]
- Lowe, John. 2017. Self-Reliance Chapter. In Middle Range Theory for Nursing. Edited by Mary Jane Smith and Patricia R. Liehr. New York: Springer. [Google Scholar]
- Lowe, John, and Rose Wimbish-Cirilo. 2016. The use of talking circles to describe a Native American transcultural caring immersion experience. Journal of Holistic Nursing 34: 280–90. [Google Scholar] [CrossRef]
- Lowe, John, and Roxanne Struthers. 2001. A conceptual framework of nursing in Native American culture. Journal of Nursing Scholarship 33: 279–83. Available online: http://www.ncbi.nlm.nih.gov/pubmed/11552556 (accessed on 14 June 2016). [CrossRef]
- Lowe, John, Huigang Liang, Cheryl Riggs, Jim Henson, and Tribal Elder. 2012. Community partnership to affect substance abuse among Native American adolescents. The American Journal of Drug and Alcohol Abuse 38: 450–55. [Google Scholar] [CrossRef] [PubMed]
- Lowe, John, Huigang Liang, Jim Henson, and Cheryl Riggs. 2016. Preventing Substance Use among Native American Early Adolescents. Journal of Community Psychology 44: 997–1010. [Google Scholar] [CrossRef]
- Lowe, John, Eric Wagner, Michelle M. Hospital, Staci Leon Morris, Michelle Thompson, Meenal Sawant, Melessa Kelley, and Eugenia Millender. 2019. Utility of the Native-Reliance theoretical framework, model, and questionnaire. Journal of Cultural Diversity 26: 61–68. Available online: https://search. proquest.com/openview/d7c2c38ea7508d184787a710936ce63d/1?pq-origsite=gscholar&cbl=34124 (accessed on 10 January 2019).
- Lucero, Nancy Marie. 2009. Creating an Indian Space in the City: Development, Maintenance, and Evolution of Cultural Identity and Cultural Connectedness among Multiple Generations of Urban American Indians. Ph.D. dissertation, University of Denver, Denver, CO, USA. [Google Scholar]
- National Council of Urban Indian Health. 2016. Evidence-Based Practice & Practice-Based Evidence. Available online: http://www.ncuih.org/krc/Dbigfoot_PBE (accessed on 14 June 2016).
- Northwest Portland Area Indian Health Board. 2019. American Indian & Alaska Native Opioid & Drug Overdose Data Brief. Available online: http://www.npaihb.org/wp-content/uploads/2019/05/WA-Opioid-Data-Brief.pdf (accessed on 10 January 2019).
- Office of Disease Prevention and Health Promotion. 2020. Disparities by Race and Ethnicity. Available online: https://www.healthypeople.gov/2020/data/disparities/detail/Chart/5199/3/2018 (accessed on 2 May 2020).
- Papps, Elaine, and Irihapeti Ramsden. 1996. Cultural safety in nursing: The New Zealand experience. International Journal for Quality in Health Care: Journal of the International Society for Quality in Health Care 8: 491–97. [Google Scholar] [CrossRef] [PubMed]
- Patchell, Beverly A. 2011. Native American Indian adolescents: Response to a culturally tailored, school-based substance abuse intervention. Ph.D. dissertation, New Mexico State University, Las Cruces, NM, USA. [Google Scholar]
- Patchell, Beverly A., Leslie K. Robbins, John A. Lowe, and Mary M. Hoke. 2015. The effect of a culturally tailored substance abuse prevention intervention with Plains Indian adolescents. Journal of Cultural Diversity 22: 3–6. Available online: https://www.questia.com/library/journal/1P3-3650930521/the-effect-of-aculturally-tailored-substance-abuse (accessed on 14 June 2016).
- Reinschmidt, Kerstin M., Agnes Attakai, Carmella B. Kahn, Shannon Whitewater, and Nicolette Teufel-Shone. 2016. Shaping a stories of resilience model from urban American Indian elders’ narratives of historical trauma and resilience. American Indian and Alaska Native Mental Health Research 23: 63–85. [Google Scholar] [CrossRef]
- Richardson, Anna, Judy Yarwood, and Sandra Richardson. 2017. Expressions of cultural safety in public health nursing practice. Nursing Inquiry 24: 35–42. [Google Scholar] [CrossRef]
- Robbins, Rebecca L. 1992. Self-determination and subordination: The past, present, and future of American Indian governance. In The State of Native America: Genocide, Colonization, and Resistance. Edited by M. Annette Jaimes. Brooklyn: South End Press, pp. 99–110. [Google Scholar]
- SAMHSA (Substance Abuse and Mental Health Services Administration). 2013. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Available online: http://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf (accessed on 14 June 2016).
- SAMHSA (Substance Abuse and Mental Health Services Administration). 2015. Behavioral Health Barometer United States, Volume 5: Indicators as Measured through the 2017 National Survey on Drug Use and Health and the National Survey of Substance Abuse Treatment Services. pp. 1–54. Available online: https://store.samhsa.gov/system/files/sma19-baro-17-us.pdf (accessed on 14 June 2016).
- SAMHSA (Substance Abuse and Mental Health Services Administration), and CBHSQ (Center for Behavioral Health Statistics and Quality). 2015. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15-4927, NSDUH Series H-50). pp. 1–36. Available online: https://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf (accessed on 14 June 2016).
- Simmons, David E. 2014. Improving the wellbeing of American Indian and Alaska Native children and families through state-level efforts to improve Indian Child Welfare Act compliance. Available online: http://www.nicwa.org/government/documents/Improving%20the%20Wellbeing% 20of%20American%20Indian%20and%20Alaska%20Native%20Children %20and%20Families_2014.pdf (accessed on 14 June 2016).
- Simpson, Leanne. 2000. Stories, dreams, and ceremonies: Anishinaabe ways of learning. Tribal College Journal of American Higher Education 11: 26–29. Available online: https://eric.ed.gov/?id=EJ606927 (accessed on 14 June 2016).
- U.S. Census Bureau. 2016. The American Indian and Alaska Native Population: 2010. Available online: http://www.census.gov/prod/cen2010/briefs/c2010br-10.pdf (accessed on 14 June 2016).
- UIHI (Urban Indian Health Institute). 2014. Facts Sheet & Tool Kits. Available online: http://www.uihi.org/resources/fact-sheets-tool-kits/ (accessed on 14 June 2016).
- Urban Indian Health Commission. 2015. Invisible tribes: Urban Indians and Their Health in a Changing World. pp. 1–39. Available online: https://www2.census.gov/cac/nac/meetings/2015-10-13/invisible-tribes.pdf?# (accessed on 14 June 2016).
- Urban Indian Health Commission, and Robert Wood Johnson Foundation. 2007. Invisible Tribes: Urban Indians and Their Health in a Changing World. Available online: http://www.uihi.org/wpcontent/uploads/2009/09/UIHC_Report_FINAL.pdf (accessed on 14 June 2016).
- USDHHS (U.S. Department of Health & Human Services). 2014. Healthy People 2020: An Opportunity to Address Societal Determinants of Health in the United States. Available online: http://www.healthypeople.gov/2010/hp2020/advisory/SocietalDeterminantsHealth.htm (accessed on 14 June 2016).
- Walters, Karina L., Jane M. Simoni, and Teresa Evans-Campbell. 2002. Substance use among American Indians and Alaska natives: Incorporating culture in an “indigenist” stress-coping paradigm. Public Health Reports 117: S104–17. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1913706/ (accessed on 14 June 2016).
- Wiechelt, Shelly A., and Joshua N. Okundaye. 2012. Working with children of parents with substance use disorders: Evaluation of a course module. Journal of Social Work Education 48: 93–103. [Google Scholar] [CrossRef]
- Wilson, Denise, and Stephen Neville. 2009. Culturally safe research with vulnerable populations. Contemporary Nurse 33: 69–79. [Google Scholar] [CrossRef] [PubMed]
- Wolf, Paulette Running, and Julie A. Rickard. 2003. Talking circles: A Native American approach to experiential learning. Journal of Multicultural Counseling and Development 31: 39–44. [Google Scholar] [CrossRef]



© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wimbish-Cirilo, R.; Lowe, J.; Millender, E.; Orellana, E.R. Addressing Substance Use Utilizing a Community-Based Program among Urban Native American Youth Living in Florida. Genealogy 2020, 4, 79. https://doi.org/10.3390/genealogy4030079
Wimbish-Cirilo R, Lowe J, Millender E, Orellana ER. Addressing Substance Use Utilizing a Community-Based Program among Urban Native American Youth Living in Florida. Genealogy. 2020; 4(3):79. https://doi.org/10.3390/genealogy4030079
Chicago/Turabian StyleWimbish-Cirilo, Rose, John Lowe, Eugenia Millender, and E. Roberto Orellana. 2020. "Addressing Substance Use Utilizing a Community-Based Program among Urban Native American Youth Living in Florida" Genealogy 4, no. 3: 79. https://doi.org/10.3390/genealogy4030079
APA StyleWimbish-Cirilo, R., Lowe, J., Millender, E., & Orellana, E. R. (2020). Addressing Substance Use Utilizing a Community-Based Program among Urban Native American Youth Living in Florida. Genealogy, 4(3), 79. https://doi.org/10.3390/genealogy4030079




