Abstract
Wildland firefighting represents a physically and mentally demanding endeavour fraught with various risk factors. The primary aim of this study is to delineate occupational chemical exposure within the firefighting work environment on the firefront and its implications for firefighters’ health status. A systematic literature review was conducted utilising diverse keyword combinations across Scopus, Web of Science, Academic Search Complete, and ScienceDirect databases. Only English-language journal articles, real-world monitoring reports, and studies featuring samples of firefighters were considered for inclusion. Forty-one studies were analysed, with 26 focusing on firefighters’ occupational exposure to chemical agents during wildland firefighting and 15 addressing the health impairments of wildland firefighting activities. Polycyclic aromatic hydrocarbons (PAHs), VOCs, and particulates emerged as the most prevalent chemical agents in the exposure profiles of frontline firefighters. They were shown to be the main incidents of cardiovascular disease, respiratory disease, and work-related cancer. The rigorous demands of wildland firefighting have been demonstrated to significantly impact firefighter health, resulting in a notable prevalence of fatalities and illnesses. Given that an elevated number of health issues are common in this occupation, adopting advanced assessment technologies is imperative.
1. Introduction
Firefighters face several occupational risks at the fire front, often challenging to identify. Limited studies assess real-time occupational exposure of firefighters [1,2], impeding a comprehensive understanding of the risks associated with wildfires and hindering the development of effective mitigation measures [3,4,5]. Firefighting training is vital in reducing exposure risks, yet even highly skilled firefighters face exposure due to their frontline role. The professional structure predominantly manages wild firefighting, representing 360,000 firefighters in 2022 in the European Union (UE). Consequently, prioritising risk mitigation and improving conditions are increasingly crucial. Demands physical and mental during diverse emergencies and extended working hours characterise firefighters’ work. These demands and exposure to hazards like heat, dust, or carbon monoxide can intensify psychophysiological reactions, posing risks of injuries or fatalities [6]. Between 2000 and 2021, in the USA, 1096 firefighter deaths were recorded out of a total of 2598 during the execution of the activity, 90% of which were caused by myocardial infarction [7]. Data from the Centers for Disease Control and Prevention (CDC) shows that between 1994 and 2023, 499 firefighters died in wildfires [8].
Firefighters are increasingly operating in sophisticated environments that allow for high efficiency in firefighting and fire protection [9]. The exposure risks between the two types of fire (urban/industrial and forest) are identical. Still, the exposure concentration is different since these two types of fire occur in different spatial situations. An urban/industrial fire is caused by combustion in urban and industrial buildings without control over time and space [10], while a forest fire is the combustion process in a forest area, uncontrolled in time and space [11,12]. Smoke inhalation in high concentrations during forest firefighting demonstrates the need for improved respiratory protection for firefighters [12]. Some equipment that is not yet certified is being used by firefighters in forest fires, which can increase the risk of exposure because the efficiency of this equipment, the length of time it will be effective or because there is not enough knowledge about how to use it, is not known [13].
In wildland fires, firefighters are exposed to different hazards like chemical agents, for example, carbon monoxide (CO), benzene, particulate, polynuclear aromatic compounds, and others [14]. The aforementioned occupational exposures demonstrate a significant correlation with adverse health outcomes among firefighters, facilitating the identification of diseases with elevated prevalence rates, notably cardiovascular, respiratory, and cancerous conditions [14,15]. Depending on the time spent fighting and the conditions on the ground, firefighters can be exposed to concentrations well above the exposure limits defined by organisations such as NIOSH and OSHA [16]. The synergy and variety of the different chemicals that can be encountered during firefighting potentiate the increase in the incidence and symptomatology of firefighters. In the long term, some diseases directly related to firefighters’ exposure to these chemical agents are already known, namely cardiovascular and respiratory diseases and cancer [15,17,18,19,20,21,22,23]. Carbon monoxide, polycyclic aromatic hydrocarbons, particulates, and volatile organic compounds are the main components most prevalent in forest fires and have the most significant impact on firefighters’ health [24].
Climate change has increasingly complicated the fight against wildfires in recent years due to factors such as the heightened intensity of fires. This difficulty in combating wildfires has posed significant challenges to the safety and health of firefighters, making it a pressing issue for occupational health and safety teams to develop effective strategies in this field. Over the years, there has been a noted difficulty in innovating the production of personal protective equipment (PPE) that offers better protection for firefighters. In addition to chemical exposure and the severe respiratory impacts directly related to such exposure, cardiovascular diseases are also a major health concern for firefighters, strongly associated with exposure to environmental pollutants such as particulates and carbon monoxide (CO). There are other direct health impacts on firefighters associated with chemical exposure that can lead to death and the onset of debilitating diseases [25]. The present study is a small part of a scoping review that surveys firefighters’ occupational exposure at the wildfire frontlines.
In structural fires, innovative solutions have already been presented that reduce firefighters’ exposure and improve firefighting techniques. Techniques for predicting fire in structures have already been demonstrated, reducing the incidence of fire and material/human loss [26,27,28]. Unlike structural fires, forest fires have not yet seen significant developments in forest firefighting innovation that would increase firefighters’ occupational health and safety. Technological innovation, whether in terms of PPE or work equipment, can cause some barriers in the perception of safety felt by firefighters. Despite this, few studies have assessed the acceptance of new technologies used in emergency response [29]. Innovation in the fire service needs a good explanation of its importance in carrying out tasks and how it can effectively solve problems and reduce occupational exposure. We have seen that innovation does not always allow information to be translated correctly, and there is no good understanding of the dangers to which firefighters are exposed during firefighting [30]. Virtual reality is an effective way of transmitting knowledge and applying innovative equipment. This innovation has been studied in various areas of occupational safety, particularly in the construction industry, as it optimises learning and improves safety performance [31,32]. Virtual reality has become a tool that, in addition to transmitting knowledge, has performed well in training sessions simulating real situations. Associated with virtual reality is the use of drones to manage forest firefighting. Some logarithms are already known to allow images of the fire line to be captured in real time and processed to improve the effectiveness of forest firefighting. By inserting robots into the fire line, this technological innovation reduces the firefighter’s exposure to the fire [33]. The development of this new software enables not only the protection of human life but also environmental protection [34]. In this sense, the innovation seen in the development of firefighting and fire-prevention equipment now has a dual function, helping to map forest fires quickly and effectively. Some agencies already use this equipment attached to helicopters to carry out thermal assessments of the terrain to rapidly detect fire outbreaks [35,36,37].
The main objective of this study is to characterise the occupational chemical exposure at the firefront of wildland fires by identifying the chemical agents, their concentration and toxicological effects, and their respective consequences on the physiological effects and health status of firefighters. To accomplish the specified objective, a scoping review was conducted on the occupational exposure of firefighters at the firefront of wildfire suppression. The findings presented in this article represent a portion of the preliminary research outcomes.
2. Materials and Methods
The methodological Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement was used to conduct the current systematic review. The present article is part of the overall review of the protocol previously published [38] and registered in PROSPERO with ID CRD42023456338. The present research results are focused on chemical exposure during wildland firefighting. The research strategy was developed based on the extension for Protocols (PRISMA-P) [39,40,41].
The scientific multidisciplinary databases for our search are SCOPUS, Web of Science, Pubmed, Science Direct, and Academic Search Complete. We combined two groups of keywords using the Boolean connectors ‘AND’ and ‘OR’ as shown in Table 1.

Table 1.
Keyword combination in the databases.
Some filters were adopted when searching the databases before selecting the articles, as can be seen in Table 2.

Table 2.
Filters adopted.
The selection of articles took place in three different phases. Initially, a search was carried out in the various databases, including the different filters, where each article was selected by title, keywords, and abstract. In the second phase of the research, all the articles selected in the previous stage were methodologically analysed, confirming compliance with the inclusion/exclusion criteria. The inclusion/exclusion criteria were that there were no age or gender restrictions, only articles that did not include samples of firefighters were included, articles with exclusively laboratory analyses were excluded, and articles that assessed the occupational exposure of firefighters in the context of forest fires or prescribed burns were accepted, as they represented occupational exposure situations in real scenarios and fire simulation scenarios with organic material. Articles that did not use samples of firefighters, articles about environmental pollution, articles about other types of fires, and articles about animals or sick people were excluded. In the third and final stage of the research, the snowballing technique was applied to ensure that as many articles as possible were included in the review. The entire analysis was carried out by two authors in an independent blind round, with a third author responsible for resolving inconsistent decisions.
Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies, by the National Heart, Lung and Blood Institute (NHLBI), was applied [42] and classified articles with “Very good”, “Good”, or “Fair” quality levels. All articles with more than 30% of the answers as “Not reported” and less than 50% of the answers as “Yes” were classified as fair quality. The “Good” quality was classified, with positive answers representing 50–70% of the questionnaire. The “Very good” quality was considered whenever the articles responded positively to the questions in more than 70% of the questionnaire. Studies rated as “Good” or “Very good” carry more weight in contributing to this review. Conversely, articles rated as “Fair” are excluded and will not be included in the review.
3. Results
3.1. Study Selection
A total of 4143 articles were obtained, but only 41 were included because they were relevant to the topic and met the objectives of the current review. All the selected articles underwent a rigorous screening process to check the eligibility criteria. Figure 1 shows the PRISMA flowchart.
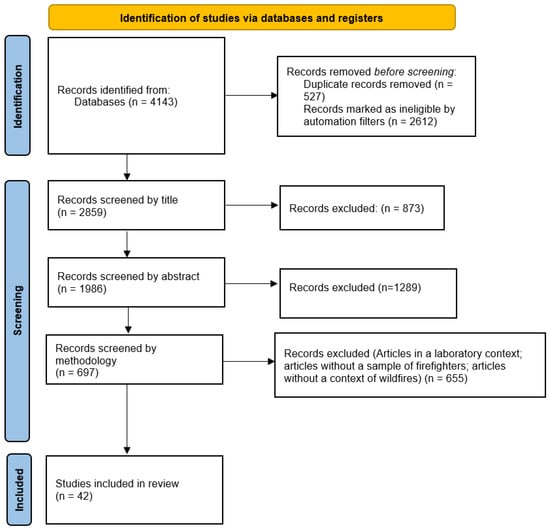
Figure 1.
PRISMA Statement flow diagram of the identification and screening processes.
3.2. Study Characteristics
The distribution of included articles throughout the years reveals a peak in this research field in 2019. Conversely, from 2008 to the present day, there has been significant progress in the studies within this research area, as illustrated in Figure 2.
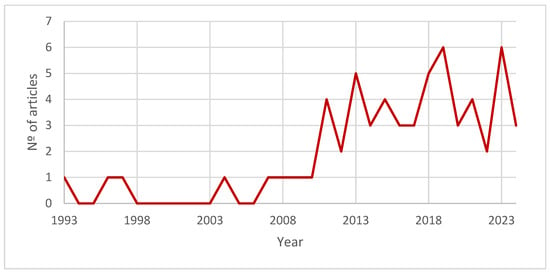
Figure 2.
Studies by year of publication.
Nevertheless, the United States is leading in advancing firefighter health and safety, with 27 contributions [43,44,45]. Notably, it is renowned for being among the most advanced countries in innovation, new methodologies, and implementing novel safety measures. Australia is another country that has made significant strides in this scientific domain, with eight notable contributions which began to gain momentum in 2011. This heightened progress may be attributed to the increasing severity of wildfires in recent years. Portugal demonstrated a high evolution in this study theme and presented eight articles about chemical agents and their impacts on wild firefighters’ health, as illustrated in Figure 3.
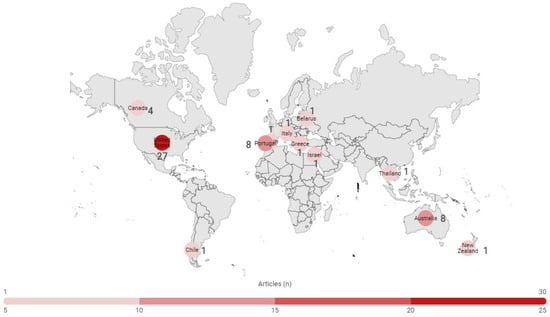
Figure 3.
Number of Studies Studies per Country.
3.3. Summary of Results
Out of the 42 articles reviewed, 27 pertain to exposure to chemical agents, while 15 address the health status of forest firefighters. Our review comprehensively characterises all chemical agents found in forest fires, synthesising findings from previous studies. Understanding the association between exposure to chemical agents and health outcomes is crucial for identifying occupational illnesses. In this study, we elucidate the primary occupational diseases and their causative factors linked to exposure to chemical agents, as detailed in the subsequent sections. Some articles are duplicated within the dataset due to their coverage of multiple topics of interest. Appendix A provides an extended comprehensive summary of all results and evidence extracted from the articles incorporated in this review.
3.3.1. Chemical Hazards
Information on the firefighter’s environment is essential to make it difficult to assess the different occupational risks involved in wildfires, which hinders the development of measures to mitigate them [3,4,5]. Firefighting training is an essential factor in decreasing the risk of Exposure. Even with a high level of expertise, firefighters are commonly exposed because they are at the front line during [46] and fine particulate matter (PM2.5), while aldehydes and polycyclic aromatic hydrocarbons have also been referenced by the authors [47]. These chemical substances have been demonstrated to exert detrimental effects on health. They have emerged as significant concerns within the scientific community, primarily due to their presence in the smoke emitted by fires at concentrations exceeding established regulatory standards. It was considered evidence of exposure in all articles that demonstrated concentrations above the recommended values and with evidence of signs and symptoms of disease. All articles that failed to provide this evidence were considered as not demonstrating Exposure.
Table 3 illustrates the correlation between these chemical agents and the exposure levels observed in studies that met the inclusion criteria.

Table 3.
Chemical Agents (n = 27).
In this knowledge domain, a notable void exists, characterised by limited diversity in assessing chemical agents during forest firefighting activities. Nonetheless, certain studies have found challenges in revealing professional Exposure, possibly stemming from the complexities of data collection in fires and the robustness of measurement equipment. Furthermore, monitoring conducted in simulated scenarios may not faithfully mirror the authentic occupational Exposure encountered by firefighters during real firefighting, which can present a limitation in the analysis of evidence.
However, the results allow us to verify that the main strength of studies in this area of knowledge involves the study of the composition of smoke caused by the fire and the different concentrations emitted. These articles identified some suffocating agents that are above reference limits.
3.3.2. Health Impairments
Exposure biomarkers are biological markers that reflect how humans interact with their exposure environment, enabling the identification and prevention of occupational diseases [43,45]. These markers are typically linked to Exposure to chemical agents and their influence on physiological and psychological processes. Additionally, exposure biomarkers can offer insights into cellular, structural, molecular, or biochemical alterations associated with the onset of diseases [13]. Several diseases associated with firefighter professional exposure have been identified in this review. However, it is known that identifying occupation-related diseases in this line of work can be a challenging task due to the diversity of exposure agents and the monitoring difficulties previously demonstrated. Identifying a disease entails long-term tracking of the individuals, which is only sometimes feasible. Therefore, Table 3 presents the studies in the occupational health category demonstrating the evidence between exposure and disease development.
Identifying the present hazardous agents in the workplace and understanding their health impacts represent the primary steps toward establishing a connection between Exposure and the incidence of occupational diseases. Thus, in Table 4, it is possible to analyse the relationship between firefighters’ Exposure and the emergence of various diseases highlighted in the included articles.

Table 4.
Occupational Chemical Exposure and Relationship to Health Impairments (n = 15).
Respiratory diseases show the strongest correlation with Exposure to forest fire smoke. Nevertheless, it has not been possible to conclude which pollutants may be the main contributors to respiratory diseases. Some authors consider that smoke exposure may also contribute to the onset of cardiovascular disease. However, it was observed in the articles included in this review that there is still a significant challenge in establishing the relationship between the risk factors found in forest fire fighting and their impact on the occupational health of firefighters.
3.4. Risk of Bias
Of all articles included in the study, 55.00% were categorised as having a high-quality risk of bias assessment. Only 15.00% received a classification of ‘Fair’ in terms of quality rating, as seen in Figure 4. Appendix B provides a comprehensive account of the risk of bias assessment conducted for each study included in the analysis.
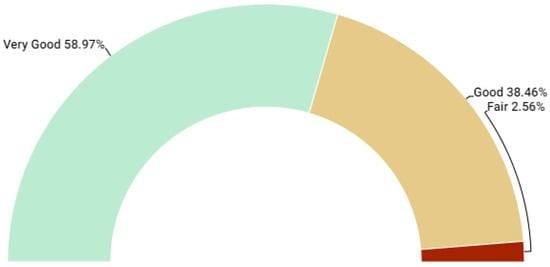
Figure 4.
Quality of studies.
Following a comprehensive assessment of bias risk and verification of exposure evidence provided within the articles, those categorised as “Fair” quality were omitted from this review to mitigate potential bias. However, one article was retained despite lacking a bias risk rating, as the methodology employed rendered bias assessment inapplicable [56]. Nevertheless, these two articles presented compelling evidence of exposure, as detailed in Table 5 and Table 6. The articles in the ‘Below Threshold Limit Value (TLV)’ column present articles that have been monitored for chemical agents but show results that do not exceed the recommended exposure limit values.

Table 5.
Chemical agent exposure.

Table 6.
Relationship between health impairment and chemical agent exposure.
In the context of chemical exposure, while certain authors have demonstrated compliance below the threshold values set by the ACGIH and OSHA, it is acknowledged that this observation may be attributed to disparities between prescribed burns and real-time fires. The composition of fuel in each fire appears to be an additional determinant affecting the concentration levels of various pollutants, alongside other variables such as meteorological conditions [65]. Nonetheless, proposing a correlation among the diverse chemical agents encountered by firefighters during firefighting serves as a method for evaluating firefighters’ occupational exposure. This approach aims to discern the potential synergistic effects of chemical agents on firefighters’ occupational hazards [44].
Regarding health impairment, it’s acknowledged that the utilisation of exposure biomarkers can be influenced by various factors such as sampling durations, environmental conditions at the sampling site, individual participant characteristics, or the participant’s health status. While all the studies included in health impairment demonstrate a correlation between exposure and health outcomes, it’s recognised that biomarker concentrations, such as urinary levels of levoglucosan, may be influenced by exposure to additional compounds present in wildfire smoke. This necessitates a more comprehensive evaluation in conjunction with other biomarkers, as individual analysis may not reveal concentrations exceeding recommended thresholds [45,53].
4. Discussion
4.1. Chemical Agents at Firefront
It is established that the composition of wildfire smoke is contingent upon the types of vegetation and materials involved [80]. For a good characterisation of occupational exposure, looking at the workers’ health and the conditions in which that exposure occurs is necessary. Thus, knowing which chemicals the fire releases is essential to prevent possible synergistic and cumulative effects on firefighters’ health [81,82].
During the suppression of wildfires, firefighters are subjected to smoke levels that exceed the recommended limits established by organisations like the National Institute for Occupational Safety and Health (NIOSH) and the Occupational Safety and Health Administration (OSHA) [83]. Throughout a fire season, firefighters battle multiple fires, and the duration and intensity of their exposure are influenced by various factors, not all of which are within their control. The potential for smoke exposure during wildfires is linked to the concentration of chemical agents. It depends on the nature of the tasks carried out, the terrain’s topography, and the environmental dispersion, all of which are affected by prevailing weather conditions [54].
Several of the chemicals to which these individuals are exposed are classified as carcinogens and have the potential to elevate the risk of heart disease. Concentration levels exceeding the World Health Organization (WHO) guidelines were observed for CO, PM2.5, and NO2 [48,50,65,71,84]. CO is an invisible and odourless hazardous gas found in smoke and equipment with internal combustion engines used in firefighting operations. Chainsaws and firefighting vehicles are equipment types that notably contribute to CO exposure. Additionally, the direction of the wind plays a role in influencing exposure [48,62]. Even though firefighters consistently experience occupational exposure surpassing recommended threshold values, the highest recorded peak for CO reached 499.80 ppm [48]. It was determined that firefighters exceeded the prescribed personal CO exposure limits during 88% of their shifts [20] and that values could be exceeded quickly [65].
Simultaneously, it was discovered that firefighters encounter elevated concentrations of these pollutants and Volatile Organic Compounds (VOCs) [59]. While this value is lower than the study referenced earlier, it is essential to interpret it in the context of exposure duration. Therefore, NIOSH establishes its exposure limit value at 200 ppm. On average, a firefighter experiences exposure to roughly 150 ppm of CO over 45 min. Nevertheless, the diffusion tube measurement yielded a CO level of 63 ppm over 1.2 h [48], where three different methods of CO measurement were tested [60,61]. The time-weighted average of CO was 120 ppm, close to the limit value [48].
There is a strong correlation between exposure to CO and PM2.5 [61]. Particles are present in wildfire smoke ranging from the smallest size (0.52 µm) to the largest (21.3 µm) [52]. Exposure to PM2.5 concentration is the best predictor of respiratory symptoms [67], along with concentrations of Levoglucosano (LG), which are typically higher in the range of respirable particles, with concentrations tending to increase from 26 mg/mL to 35 mg/mL between the beginning and end of the shift [53]. Firefighters operating at the firefront, where a combination of contaminants is present, experience the most significant decline in forced expiratory volume at 1 s [52]. Besides CO, specific toxic, suffocating agents emitted from fire smoke exacerbate exposure, including Acrolein, Benzene, Carbon Dioxide (CO2), and Formaldehyde, with a potentiating effect. Among these chemicals, benzene is the most commonly found [55]. Firefighters’ exposure is statistically significant in direct fire suppression, with 3.5, 6.0, and 63.1 ppb for acrolein, benzene, and formaldehyde, respectively [49]. Nevertheless, distinctions in exposure levels between the commencement of a wildfire intervention and a controlled prescribed fire are acknowledged. During the initial stages of the intervention, carbon dioxide (CO2) and formaldehyde register the highest pollutant concentrations [46].
Furthermore, there are other detectable compounds, including polycyclic aromatic hydrocarbons (PAHs), with anthracene being one of the common ones [56]. PAHs are distinguished by their lipophilic nature and are classified as hazardous environmental pollutants [85]. Wildland fires serve as a primary source of PAH release into the environment [86], the outcome of incomplete combustion of organic matter, frequently derived from contaminated soils [85]. NIOSH recommends that the workplace exposure limit for PAHs should be set at the lowest detectable concentration of 0.1 mg/m3, whereas OSHA suggests a TWA of 0.2 mg/m3. Given that forest fires constitute the primary source of PAH release and considering that firefighters are exposed to concentrations exceeding the recommended thresholds, PAHs emerge as a predominant factor in the onset of occupational illnesses [87].
4.2. Health Impairments
4.2.1. Respiratory Diseases
Firefighters face various substances in smoke during environmental exposure to fires, which can elicit an immune response, resulting in respiratory symptoms and diminished respiratory function [75]. The effects on the lungs depend on the chemical composition of the smoke, the particle size, and the combustion temperature, which are different for different materials [88,89].
Smoke exposure triggers an inflammatory response through granulocyte production [47] and eosinophilic and neutrophilic inflammation in the airways at the bronchial level during and after acute exposure to forest fires [75]. The toxic agents released during fires produce changes in lung tissues [90]. It was found that there is a statistical relationship between the number of years of professional exposure, age, and smoking status of the individuals and symptoms of respiratory disease. Firefighters’ occupational exposure can lead to the onset of chronic respiratory symptoms. However, it is known that smoking individuals may have a cumulative effect [17,91].
It is crucial to note that Personal Protective Equipment (PPE), especially hoods utilised for respiratory protection in forest firefighting, may only sometimes be the most effective or readily available in adequate quantities for all personnel. Furthermore, during firefighting activities, individuals may decide to remove their PPE, impacting their exposure. It has already been indicated that firefighters have a decreased respiratory function in forest fires [72]. In fact, with the high respiratory exposure and diversified chemical contaminants in the working atmosphere of a wildfire, the incidence of lung cancer and cardiovascular diseases is high [70]. Despite this, changes in the lung function of firefighters during the work shift are not evident and do not rule out the possibility of a cumulative effect resulting from exposure over several days [77].
4.2.2. Cancer Diseases
Oncological diseases are one of the occupational diseases with the highest incidence in the professional group of firefighters, such as prostate, lung, and kidney cancer [88,89]. The assessment of exposure to radionuclides emitted by smoke during a forest fire can be used as an indicator of cancer incidence, in particular lung cancer [92].
In a wildfire, firefighters are exposed to genotoxic compounds [43]. Some authors propose the hypothesis of adverse effects on urinary mono-hydroxyl polycyclic aromatic hydrocarbon levels and genotoxic biomarkers of oxidative impact, including baseline Deoxyribonucleic Acid (DNA) and oxidative DNA damage [78]. It is known that there can be significant impacts on individuals. More significant baseline DNA damage was found in firefighters aged 29–38 than in younger groups, and smoke exposure was related to the damage found [93].
The human body absorbs PAHs through inhalation, ingestion, and dermal exposure. Short-term exposure can manifest as eye irritation, nausea, and vomiting. However, prolonged exposure poses health risks, including kidney and liver damage, respiratory difficulties, and related symptoms [85]. PAHs stand as a notable factor contributing to carcinogenic and mutagenic diseases, with skin, lung, pancreatic, oesophagal, bladder, colon, and breast cancers commonly associated with prolonged exposure to these compounds [86]. The European Union has been addressing the matter of occupational cancer, with findings in 2016 indicating that 120,000 cases were attributed to exposure to carcinogens in the workplace, resulting in the deaths of approximately 80,000 workers [94]. Conversely, some authors highlight that the link between cancer development in non-smoking firefighters and elevated levels of polycyclic aromatic hydrocarbons (PAH) in peripheral leukocytes remains uncertain. Exposure to fire smoke encompasses numerous genotoxic compounds that may interplay and intensify their carcinogenic potential [69]. Some studies also demonstrate a lack of correlation between engagement in forest firefighting and PAH-DNA levels, implying that dietary factors may play a role as triggering agents [79]. Specific metabolites associated with exposure to compounds like Bisphenol A (BPA), BP-3, triclosan, methylparaben (MP), ethylparaben (EP), butylparaben (BP), and n-propylparaben (PP) can result in substantial health consequences for individuals exposed to fire smoke [80]. Nonetheless, it is worth noting that there are no discrepancies in biomarker outcomes concerning the onset of respiratory symptoms during exposure [60]. Despite this, it is suggested that 4-hydroxyphenanthrenes can be applicable as biomarkers of forest fire exposure and may be associated with symptoms [45].
It should be noted that firefighters are exposed to oxidative damage of nucleobases. Still, this exposure may be influenced by the number of years as a firefighter due to its cumulative effect [66]. Thus, it is essential to assess the different types of exposures they are subjected to, the existence of other occupational activities, their lifestyle (particularly if they smoke or have respiratory diseases, and their length of service as firefighters [3,70,93,95,96,97].
4.3. Proven Exposure to Chemical Exposure and Health Issues
Real-time measurement during a wildfire poses a significant challenge in deploying monitoring equipment and innovative sampling techniques. Parameters such as ambient temperature, CO, and oxygen levels enable the assessment of physical conditions impacting firefighter safety and can serve as warning indicators when these conditions become detrimental to the professionals’ health. Telemetry sensors designed for firefighter monitoring, coupled with physiological variables, are already established in the field [97]. The integration of environmental and physiological variables may serve as a pivotal method for signalling fatigue alerts induced by exposure to the occupational setting of forest fires.
Indeed, throughout this review, it was observed that the articles predominantly concentrate on environmental exposure and overlap with recommended limit values by regulatory agencies such as OSHA and NIOSH. Furthermore, they delve into the consequential impacts of this exposure on firefighter health, notably linking exposure to fire smoke with diminished lung function [75,77,90] and the onset of work-related cancer [78,92,93]. Upon scrutinising the included studies, it became evident that the primary risk factor for work-related cancer stemming from occupational exposure to chemical agents in forest fire smoke lies in the mutagenicity of DNA chains, predominantly attributed to compounds like PAH. Nevertheless, it is recognised that exposure to other substances, such as CO, may also significantly impair lung function among firefighters. This is owing to the elevated concentrations to which they are exposed and the ensuing impact on individuals, particularly in terms of diminishing oxygen concentration in the blood [18,52,65,77,98,99]. Nevertheless, it is crucial to consider the potentially significant impact of these compounds on other systems within the human body, especially concerning cardiovascular alterations. Over the long term, such alterations may precipitate the onset of diseases [86].
The challenges associated with employing varied sampling techniques appear to stem from the harsh conditions confronted by firefighters during combat tasks, rendering equipment deployment fraught with complexities that impede error-free monitoring. Physiological variables, in particular, pose heightened sensitivity, and their real-time monitoring can prompt individuals to cease task execution, potentially heightening health risks for both the individual and the researcher. Consequently, the need for more diversity in studies within this domain may be attributed to the inherent difficulties in real-time physiological monitoring during forest firefighting. Although initiatives to develop real-time health monitoring systems for firefighters have commenced, these systems have yet to be universally applied to high-risk firefighting activities, nor have they been designed with variables that furnish comprehensive insights into firefighters’ health status during task execution. Indeed, the evaluation of firefighters’ health status, and by extension, their occupational exposure, often encompasses a limited array of variables, as evidenced by the included studies. However, the amalgamation of these and additional variables as indicators for real-time assessment of firefighters’ health status remains challenging, not only due to the exigencies of on-site assessment during fire incidents but also owing to the imperative to devise resilient equipment capable of withstanding the adverse conditions encountered in such scenarios [13].
It is considered necessary to include the assessment of prolonged exposure and exposure through other sources of contamination, such as contamination by PPE (Personal Protective Equipment) and motorised equipment used in firefighting. Moreover, this exposure varies depending on the type of vegetation and fuel involved in the fire [100]. Nevertheless, it is known that the primary source of contamination for firefighters in wildfires is the lack of PPE that can ensure respiratory protection because it is not commonly used [70,101,102].
4.4. Biases and Limitations
While many of the risks firefighters face are well-established, more research is needed concerning the comprehensive assessment and detailed characterisation of occupational exposure for firefighters operating at the firefront. Furthermore, adopting preventive and corrective measures to mitigate occupational exposure has yet to show much progress. It is also advisable to explore alternative approaches for the treatment of the results, such as conducting a meta-analysis.
The primary risk associated with this review is tied to the studies’ diversity. The methodologies employed in these various studies are not easily comparable, rendering the extraction of raw data a challenging task. This data would have been instrumental in the authors drawing more definitive conclusions. However, several studies have found no significant differences in chemical exposure characterisation data between different groups of firefighters. In our study, no articles were identified that specifically addressed chemical exposure from pollutants deposited on firefighters’ personal protective equipment (PPE) and emissions from vehicle engines and equipment like chainsaws. Nonetheless, this variable could represent an aggravating factor for the health of these individuals, underscoring the need for further studies involving such assessments. It is worth noting that conducting monitoring at the forefront is a demanding endeavour fraught with various practical implications.
4.5. Implications for Practice
A fire is delineated by the combustion of material under elevated temperatures and in an unregulated fashion. The distinction between a forest fire and a structural fire can be encapsulated by the occurrence of the former within forested regions. In contrast, the latter ensues within residential towers and is typified by combustible materials contained within structures, including building components. Fires occurring within industrial facilities may be compounded by the presence of combustible materials, particularly the inclusion of chemical products [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103]. When addressing the challenge of combating forest fires, the complexity lies in their propagation, which typically proves challenging to forecast. Variables such as wind patterns, ambient temperature, humidity levels, and fuel composition can amplify the fire’s intensity and determine its behaviour [104]. Additionally, it is recognised that Personal Protective Equipment (PPE) usage varies between the two fire types, with respiratory protection being notably limited for forest fires, despite firefighters facing similar risks as structural fires [105]. Commonly, in forest fires, the implementation of a particulate respirator mask represents the most effective means of respiratory protection [103,106], in contrast to urban or industrial fires, where respiratory protection typically involves goggles and an open-circuit self-contained breathing apparatus (SCBA) [10]. Reconciling environmental and health variables makes it possible to monitor the health status of firefighters better and prevent occupational diseases since some are carcinogenic and present a high risk of heart disease.
Firefighters often employ equipment that needs more certification for use in wildfire conditions. This situation can heighten the risk of exposure due to potential deficiencies in protective capabilities, limited duration, and inadequate knowledge regarding their utilisation, especially in the case of respiratory protection gear. The need for more innovation in firefighting equipment for wildfires has been compounded by the limited progress in normative standards governing respiratory protection. Only ISO 16073-2:2019 Compatibility is recognised in this context. The challenge in developing more Personal Protective Equipment (PPE) is more than just ensuring its optimal performance. It also hinges on its practicality in wildland firefighting and the certification process by accredited entities, which proves to be a complex undertaking [82]. Volunteer firefighters are the most affected when it comes to lack of equipment and the use of equipment that is not validated. A few countries worldwide ensure assistance through volunteer firefighters, including Russia, Poland, Portugal, the United States, Germany, Japan, Canada, and Chile.
Forest firefighting has been demonstrated to be a high-exposure endeavour, attributed not only to the inadequacy of effective Personal Protective Equipment (PPE) but also to the amalgamation of chemical exposure experienced by firefighters, as outlined throughout this review, along with various other factors imposing significant physical and mental strains. As evidence, the chemical exposure encountered by firefighters constitutes a primary source of illness and respiratory symptoms. Nevertheless, additional factors beyond chemical exposure have garnered attention within the scientific community. Instances include extreme heat, which has been documented to elicit psychological, psychophysiological, and pathological effects [107,108]. Indeed, one of the indicators of fatigue in hot environments with chemical exposure is cardiovascular load. Considering the variability in slope and terrain stability during forest firefighting, this could be another exacerbating factor and indicator of cardiovascular disease. About 45% of firefighters’ deaths on duty are caused by cardiovascular diseases [109]. These figures can be justified by associating exposure to fumes [109] with the additional effort caused by physically demanding activities and aggravated by the increase in core temperature caused by them [110].
Fatigue stands as the primary catalyst for human error and can precipitate serious accidents. One of the variables frequently employed as an indicator of fatigue is lactate [111]. Lactate is already used to determine pathologies and the bioenergetic consumption of muscle cells [112]. The association between elevated lactate levels and exposure to environments with high carbon monoxide concentrations suggests that lactate can be a reliable indicator of overload. Lactate levels tend to rise in environments lacking oxygen [113]. Therefore, lactate is considered an invasive parameter that may hinder its inclusion in biotelemetry systems. The anaerobic threshold can be estimated using heart rate, a parameter easily measured by portable meters [114,115]. However, it is known that further evaluation is needed to determine the agreement of the different variables [116,117]. Despite the challenges associated with the probabilistic assessment of capillary lactate, one should consider the possible benefits of investing in biotelemetry sensors. Lactate is a parameter frequently utilised in athletics to assess changes in exercise intensity, observe various thresholds, and understand their physiological impact on heart rate and maximum oxygen consumption [118,119,120]. Lactate can be a strong indicator of assessing heavy work in an occupational context [121,122]. However, few studies on firefighters still evaluate capillary lactate and its relationship with environmental exposure [123].
This review has underscored the heightened occupational exposure of firefighters during forest firefighting, owing to the intricate nature of the activity and the diverse factors influencing this exposure. Indeed, there exists a pronounced imperative for occupational health and safety initiatives aimed at monitoring firefighter health, tailoring individual tasks, conducting thorough analyses of workplace accidents, and preemptively identifying occupational diseases. The United States has emerged as a leading proponent in this realm of occupational health and safety intervention [124]. Nevertheless, in countries such as Portugal, where the firefighting community comprises 94% of volunteer firefighters, there is currently no recognised program capable of addressing the occupational health and safety requirements inherent to a high-risk profession like firefighting, encompassing all dimensions of risk associated with the activity.
The importance of knowing firefighters’ exposure to forest fires has become increasingly important for improving methodologies and occupational disease risk management. Based on the findings outlined in this review, it is recommended that more comprehensive analyses be conducted, facilitating the development of programs tailored to encompass the diverse occupational hazards encountered by firefighters. This initiative aims to redefine the interpretation of occupational exposure within this professional group. Certain American guides and platforms are already recognised for serving as a reference for the monitoring and selection of firefighters [125]. Nevertheless, there are numerous avenues yet to be explored for the intervention of occupational health and safety services aimed at mitigating the work-related impacts on firefighters’ health. This is particularly pertinent in the context of forest firefighting, which appears to need significant intervention efforts.
5. Conclusions
The impacts of chemical exposure on the safety and health of firefighters during wildfire suppression are substantial and multifaceted. Exposure to environmental pollutants such as particulates and carbon monoxide (CO) not only exacerbates immediate respiratory risks but also significantly contributes to the development of cardiovascular diseases, which have a high incidence among firefighters. Furthermore, continuous exposure to toxic chemicals can result in severe and debilitating diseases, increasing the risk of mortality and morbidity within the firefighter population. Years of experience and exposure time are important factors to analyse, as they are significant contributors to the development of symptoms and disease. The difficulty in innovating the production of personal protective equipment (PPE) that provides adequate protection intensifies these risks, highlighting the urgent need for improvements in this area. Occupational health and safety strategies should, therefore, focus not only on the immediate mitigation of risks but also on the implementation of long-term solutions that include improving PPE, continuous health monitoring of firefighters, and developing rapid response protocols for chemical exposure incidents. Real-time monitoring has presented significant challenges in this field of research due to the difficulty of using equipment under wildfire conditions. This research has identified a strong need for intervention in the innovation of new analytical methodologies and the development of new products capable of meeting these needs. The present study recommends the implementation of technological innovation, robust occupational health policies, and continuous awareness of the risks involved in wildfire suppression by occupational health and safety teams.
Author Contributions
Conceptualization, T.T., I.D., J.S., M.V., J.S.B. and J.G.; methodology, T.T., I.D., J.S. and J.G.; formal analysis, T.T., I.D., L.A., J.S., M.V., J.S.B. and J.G.; research, T.T., I.D., J.S., M.V., J.S.B. and J.G.; draft writing preparation, T.T., J.S. and J.G.; drafting and editing revision, T.T., I.D., J.S., M.V., J.S.B. and J.G.; project administration, J.S.B., M.V. and J.G.; funding acquisition, J.S.B., M.V. and J.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Ministério da Ciência, Tecnologia e Ensino Superior—Fundação para a Ciência e a Tecnologia (FCT—Portugal), under the projects PCIF/SSO/0063/2018 and UIDB/50022/2020.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would also like to acknowledge the support of the Ph.D. Program in Occupational Health and Safety at the University of Porto. Thanks to the Associated Laboratory for Energy, Transports and Aeronautics (LAETA) for the support.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Summary of data on Chemical Agents (n = 26).
Table A1.
Summary of data on Chemical Agents (n = 26).
| Reference | Objective | Results | Evidence |
|---|---|---|---|
| [46] | Fire smoke exposure assessment | * General shift values: IA PF IP Acrolein (ppb) 1 1 9 Benzene (ppb) 3 4 16 CO2 (ppm) 391 439 450 CO (ppm) 1.6 2.8 4.1 Formaldehyde (ppb) 6 13 47 PR (mg/m3) 0.022 0.50 0.63 PT (15 mg/m3) 1.39 1.47 NA IR PELs (Em ≤ 1.0) ** 0.1 0.1 0.3 IR TLVs (Em ≤ 1.0) *** 0.1 0.2 0.4 Line of Fire: IA PF IP Acrolein (ppb) 5 2 15 Benzene (ppb) 14 6 28 CO2 (ppm) 488 465 519 CO (ppm) 7.4 4.0 6.9 Formaldehyde (ppb) 28 18 75 PR (mg/m3) 1.11 0.72 2.93 PT (15 mg/m3) 5.32 1.72 NA IR PELs (Em ≤ 1.0) 0.4 0.1 0.4 IR TLVs (Em ≤ 1.0) 0.6 0.3 0.7 | About 8% of the workers in prescribed fires exceeded the TLV limit value for CO while in the fire line. When the fire attack is upwind, firefighters are at low exposure to the released components |
| [47] | To characterize the acute pulmonary and systemic inflammatory effects of exposure to forest fire smoke | Δ[CO] = between 5 and 20 ppm | Exposure to smoke by firefighters triggers an inflammatory response caused by an increase in sputum granulocytes. |
| [64] | To evaluate the relationship between exposure to CO, PM, and Levoglucosan changes in urinary methoxy phenols. | [PM2.5] = 1054 ± 415 mg/m3 [LG] = 75 ± 49 mg/m3 [CO] = 2.8 ± 1.8 ppm; LG/PM ratio = 0.08 ± 0.04 CO/PM ratio = 3.6 ± 2.2 | The OSHA limit values for CO were not exceeded. |
| [48] | Analyzes data on individual exposure to CO, NO2, volatile organic compounds (VOCs), and PM2.5 obtained during an experimental fire. | CO (ppm) 1—TWA = 7.60; Peak Value = 493.30; TLV-STEL fulfilment = NO 2—TWA = 9.60; Peak Value = 486.60; TLV-STEL fulfilment = NO 3—TWA = 10.70; Peak Value = 198.80; TLV-STEL fulfilment = NO 4—TWA = 13.10; Peak Value = 386.60; TLV-STEL fulfilment = NO 5—TWA = 14.80; Peak Value = 499.80; TLV-STEL fulfilment = NO 6—TWA = 19.80; Peak Value = 454.40; TLV-STEL fulfilment= NO 7—TWA = n.d; Peak Value = n.d; TLV-STEL fulfilment = n.d 8—TWA = 11.80; Peak Value = 376.70; TLV-STEL fulfilment = NO 9—TWA = 13.70; Peak Value = 421.00; TLV-STEL fulfilment = NO 10—TWA = n.d; Peak Value = n.d; TLV-STEL fulfilment = n.d 11—TWA = 2.60; Peak Value = 112.00; TLV-STEL fulfilment = YES 12 —TWA = 6.80; Peak Value = 248.00; TLV-STEL fulfilment = NO 13—TWA = 5.80; Peak Value = 422.00; TLV-STEL fulfilment= NO 14—TWA = 12.50; Peak Value = 295.00; TLV-STEL fulfilment = NO 15—TWA = 19.30; Peak Value = 287.00; TLV-STEL fulfilment = YES 16—TWA = 5.70; Peak Value = 323.00; TLV-STEL fulfilment = YES 17—TWA = 1.30; Peak Value = 155.00; TLV-STEL fulfilment = YES 18—TWA = 12.70; Peak Value = 614.00; TLV-STEL fulfilment = NO 19—TWA = 6.10; Peak Value = 236.00; TLV-STEL fulfilment = NO 20—TWA = 4.10; Peak Value = 286.00; TLV-STEL fulfilment = YES NO2 (ppm) 1—TWA = 0.90; Peak Value = 3.00; TLV-STEL fulfilment = YES 2—TWA = 1.90; Peak Value = 9.00; TLV-STEL fulfilment = YES 3—TWA = 1.80; Peak Value = 8.00; TLV-STEL fulfilment = YES 4—TWA = 0.10; Peak Value = 33.00; TLV-STEL fulfilment = YES 5—TWA = 0.10; Peak Value = 22.00; TLV-STEL fulfilment = YES 6—TWA = n.d; Peak Value = n.d; TLV-STEL fulfilment = n.d 7—TWA = 1.10; Peak Value = 10.00; TLV-STEL fulfilment = YES 8—TWA = 0.10; Peak Value = 4.00; TLV-STEL fulfilment= YES 9—TWA = 2.20; Peak Value = 5.00; TLV-STEL fulfilment = YES 10—TWA = 0.02; Peak Value = 4.00; TLV-STEL fulfilment = YES 11—TWA = 0.06; Peak Value = 16.8; TLV-STEL fulfilment = YES 12—TWA = 0.03; Peak Value = 2.60; TLV-STEL fulfilment = YES 13—TWA = 0.05; Peak Value = 5.90; TLV-STEL fulfilment = YES 14—TWA = 0.02; Peak Value = 5.00; TLV-STEL fulfilment = YES 15—TWA = 0.11; Peak Value = 9.70; TLV-STEL fulfilment = YES 16—TWA = 0.12; Peak Value = 5.10; TLV-STEL fulfilment = YES 17—TWA = 0.03; Peak Value = 5.70; TLV-STEL fulfilment = YES 18—TWA = 0.09; Peak Value = 12.00; TLV-STEL fulfilment = YES 19—TWA = 0.09; Peak Value = 3.70; TLV-STEL fulfilment = YES 20—TWA = 0.09; Peak Value = 8.50; TLV-STEL fulfilment = YES VOC (ppm) 1—TWA = 0.19; Peak Value = 88.00; TLV-STEL fulfilment = n.a 2—TWA = 0.28; Peak Value = 35.00; TLV-STEL fulfilment = n.a 3—TWA = 0.03; Peak Value = 4.00; TLV-STEL fulfilment = n.a 4—TWA = 0.16; Peak Value = 11.00; TLV-STEL fulfilment = n.a 5—TWA = 0.12; Peak Value = 12.00; TLV-STEL fulfilment = n.a 6—TWA = 0.47; Peak Value = 63.00; TLV-STEL fulfilment = n.a 7—TWA = 0.22; Peak Value = 23.00; TLV-STEL fulfilment = n.a 8—TWA = 0.19; Peak Value = 15.00; TLV-STEL fulfilment = n.a 9—TWA = 0.69; Peak Value = 20.00; TLV-STEL fulfilment = n.a 10—TWA = 0.25; Peak Value = 15.00; TLV-STEL fulfilment = n.a 11—TWA = 0.00; Peak Value = 68.00; TLV-STEL fulfilment = n.a 12—TWA = 0.03; Peak Value = 7.0; TLV-STEL fulfilment = n.a 13—TWA = 0.03; Peak Value = 29.00; TLV-STEL fulfilment = n.a 14—TWA =0.02; Peak Value = 15.00; TLV-STEL fulfilment = n.a 15—TWA = 0.03; Peak Value = 9.00; TLV-STEL fulfilment = n.a 16—TWA = 0.86; Peak Value = 76.00; TLV-STEL fulfilment = n.a 17—TWA = 0.01; Peak Value = 5.00; TLV-STEL fulfilment = n.a 18—TWA = 0.17; Peak Value = 59.00; TLV-STEL fulfilment = n.a 19—TWA = 0.04; Peak Value = 12.00; TLV-STEL fulfilment = n.a 20—TWA = 0.06; Peak Value = 6.00; TLV-STEL fulfilment = n.a PM2.5 (µm−3) 1—TWA = 773.40; Peak Value = 13,593.00; TLV-STEL fulfilment = n.a 2—TWA = 551.00; Peak Value = 13,768.00; TLV-STEL fulfilment = n.a 3—TWA = 917.10; Peak Value = 15,590.00; TLV-STEL fulfilment = n.a 4—TWA = 1436.60; Peak Value = 19,953.00; TLV-STEL fulfilment = n.a 5—TWA = 2196.40; Peak Value = 19,134.00; TLV-STEL fulfilment = n.a 6—TWA = 2187.50; Peak Value = 16,516.00; TLV-STEL fulfilment = n.a 7—TWA = 2052.80; Peak Value = 17,635.00; TLV-STEL fulfilment = n.a 8—TWA = 1435.40; Peak Value = 14,469.00; TLV-STEL fulfilment = n.a 9—TWA = 1829.30; Peak Value = 18,286.00; TLV-STEL fulfilment = n.a 10—TWA = 618.50; Peak Value = 13,989.00; TLV-STEL fulfilment = n.a 11—TWA = 131.90; Peak Value = 6257.00; TLV-STEL fulfilment = n.a 12—TWA = 1201.60; Peak Value = 14,663.00; TLV-STEL fulfilment = n.a 13—TWA = 371.50; Peak Value = 10,049.00; TLV-STEL fulfilment = n.a 14—TWA = 943.70; Peak Value = 13,055.00; TLV-STEL fulfilment = n.a 15—TWA = 456.40; Peak Value = 13,390.00; TLV-STEL fulfilment = n.a 16—TWA = 120.10; Peak Value = 6934.00; TLV-STEL fulfilment = n.a 17—TWA = 198.00; Peak Value = 8896.00; TLV-STEL fulfilment = n.a 18—TWA = 1188.30; Peak Value = 12,929.00; TLV-STEL fulfilment = n.a 19—TWA = 528.90; Peak Value = 17,290.00; TLV-STEL fulfilment = n.a 20—TWA = 1072.9; Peak Value = 15,071.0; TLV-STEL fulfilment = n.a | Using the ACGHI reference value at the PM level, the concentrations found did not exceed the reference value. |
| [44] | Evaluate the association between PM2.5 particles and duration, fire size, work tasks, and meteorological variables to identify factors that influence exposure. | Burning day: µ[PM2.5] = 280 µg/m3 (95% CL = 140, 557 µg/m3, n = 177) No-burn days: µ[PM2.5] = 16 µg/m3 (95% CL = 10, 26 µg/m3, n = 35) | The values found by the authors do not exceed the OSHA or ACGIH limit values |
| [79] | Assess the high exposure risk related to forest fire smoke inhalation | CO (ppm) RP (mg/m3) Formaldehyde (ppm) Fuel reduction burns 12.2 >1.5 <0.192 Experimental burns 6.5 >0.73 <0.042 Slash or heap burns 2.9 >0.55 <0.042 Prescribed burns 9.1 >1.2 <0.161 Victorian wildfires 4.5 0.39 0.042 | The concentrations of pollutants varied significantly, making it difficult to assess the firefighters’ exposure. |
| [59] | Characterize forest fire smoke exposure and health impacts. | TLV-TWA: CO (25 ppm); NO2 (3 ppm); TLV-STEL: CO (200 ppm); NO2 (5 ppm); Peak: CO (400 ppm); NO2 (20 ppm). | The authors indicate that firefighters are exposed to high CO, NO2, and VOC concentrations in forest firefighting. |
| [60] | Investigate the effect of occupational smoke exposure through biomarkers. | µg[PM2.5] = 650 μg/m3; [PM2.5] = 288 a 1306 μg/m3 µg[CO] = 3.6 ppm; Δ[CO] = 1.54 a 19.85 ppm | Exposure to smoke induces inflammation. |
| [61] | CO exposure assessment of a group of US firefighters. | µg[CO] = 1.06 ppm; interval of concentration = 0–14 ppm | The samples exceed the NIOSH stipulated limit value of 200 ppm. |
| [65] | Evaluation of particles, levoglucosan and CO. | Δ[PM2.5] = 64 to 2068 µg m−3 Δ[CO] = 0.02 to 8.2 ppm Δ[LG] = 0.04 to 291 µg m−3 | PM and CO do not exceed the recommended limit values. |
| [66] | Smoke exposure assessment. | µ[PM2.5] = 248 μg/m3 µ[CO] = 1.0 ppm Pre-shift [8-Oxo-dG] = 81 μg/g creatinine [MDA] = 0.78 μmol/g creatinine Post-shift [8-Oxo-dG] = 70 μg/g creatinine [MDA] = 0.95 μmol/g creatinine | The authors suggest that firefighters are exposed to oxidative damage of nucleobases in forest fires, which may be influenced by the number of years in the firefighter’s career. |
| [53] | Evaluation of urinary levoglucosan as a biomarker of smoke exposure. | µg[LG] before the shift = 26 mg/mL µg[LG] after shift = 35 mg/mL µg[PM2.5] = 248 mg/m3 | Levoglucosan was not associated with PM2.5. |
| [52] | Characterize occupational exposures from wildland firefighting and evaluate their associations with changes in lung function. | µ[PMtotal] = 0.39 mg/m3 µ[PM](workers from other activities like excavation) = 0.88 mg/m3 µ[PM](workers on the fireline) = 0.35 mg/m3 µ[CO]Swampers = 6.24 ppm µ[CO]Sawyers = 8.19 ppm were µ[CO]line workers = 0.67 ppm (p < 0.001) [LG]line fire = 1.88 μg/m3 [LG]mop-pop = 0.26 μg/m3 (p < 0.05). [Organic Carbon] = 0.17 mg/m3. µ[CO TWA] = r = 0.54 (p < 0.001). | About 71% of the LG found is in the respirable particulate range. |
| [45] | Compare hydroxylated PAH metabolites concentration in urine samples before and after the shift. | [CO] = 1.34 ppm; [PM2.5] = 577 μg/m3 [LG] = 21 μg/m3 | All OH-PAHs were above the detection limits. There were consistent, substantial increases in OH-PAHs |
| [55] | Assessment of air pollutants in forest fires and wildfires. | Low molecular weight PAHs were identified at higher concentrations. Except for anthracene, all 2- and 3-ring PAHs were identified in at least 73% of the samples. | Containment and surveillance tasks have higher concentrations than those performed on firelines, particularly benzene. |
| [62] | Analyze the CO exposure data to assess the exposure of firefighters. | Chainsaw handling was the highest overall average CO level at 6.8 ppm during 1 min of exposure at 25 ppm. The CO exposure in this task is aggravated by using chainsaws for felling trees and bushes that facilitate firefighting. | A firefighter in environments with wind shifts or strictly downwind with speeds greater than 5mph is more exposed to CO |
| [56] | Characterize and understand the exposures of polycyclic aromatic hydrocarbons and PM2.5 in a forest fire. | Naphthalene, Retene, and Phenanthrene were the most commonly detected polycyclic aromatic hydrocarbons. PM2.5 concentrations were highest during the day. | Wildland firefighters engaged in fire suppression are often exposed to hazardous air pollutants. |
| [43] | Urinary mutagenicity assessment to characterize firefighter exposure on burning days compared to non-burning days. | Working days without firing: µ[PM2.5] = 35.1 μg/m3 µ[CO] = 0.005 ppm Working days with firing: µ[PM2.5] = 259.4 μg/m3 µ[CO] = 0.8 ppm | No statistically significant increases between work shifts were observed in urinary mutagenicity. |
| [67] | Assessing markers of exposure to forest fires. | PM2.5 were the most predictive of respiratory symptoms. | Concentrations of persistent inflammatory markers in plasma were related to exposure estimates. |
| [51] | Characterize pollutant emissions in forest fires during burning. | [PM2.5] = 1.47 mg/m3 [CO] = 8.50 ppm [BC] = 47.85 μg/m3 | 88% of shifts exceeded the imposed CO |
| [49] | Assessment of particulate matter and VOCs during forest firefighting. | The direct attack has statistically significant VOC exposure of 3.5, 6.0, and 63.1 ppb for acrolein, benzene, and formaldehyde, respectively. | The initial attack teams are the most exposed. |
| [71] | Assessment the exposure of firefighters in prescribed wildland fires and their occupational exposure | The findings indicate that the prescribed thresholds for PM2.5 were surpassed in all monitored fires, with recorded levels reaching 6188 and 9434 μg/m3 (Fire 1), 3841 and 6240 μg/m3 (Fire 2), 4328, 3789, and 3512 μg/m3 (Fire 3), 5452 μg/m3 (Fire 4), 7778, 4056, and 3784 μg/m3 (Fire 5), 3651, 5912, and 4962 μg/m3 (Fire 6), and 3468 μg/m3 (Fire 7). Conversely, the prescribed Time-Weighted Average (TWA) limits for NO2, SO2, and CO were consistently maintained within permissible bounds and were never exceeded. | The inhalation of silica dust, contingent upon exposure duration and intensity, can induce symptoms characteristic of silicosis (such as coughing, fatigue, shortness of breath, and chest pain), as well as provoke pulmonary inflammation and carcinogenesis. |
| [50] | Assessment exposure from one Interagency Hotshot Crew conducted at a wildfire incident | The mean-variance between pre- and post-shift levoglucosan levels amounted to 1.84, 4.6, and 74.4 μg/mg creatinine for days 1, 2, and 3, respectively. | Post-shift creatinine-adjusted levoglucosan concentrations exhibited an elevation in comparison to pre-shift levels, with the most significant disparity observed on day 3. |
| [68] | Characterization of levels of gaseous PAH in firefighters’ air during regular working activities at controlled forest fires and fire stations | The observed concentrations increased significantly during the fire event due to the rise in flame temperature, forest fuel load, and certain alterations noted in weather conditions during the fire event | The risk of lung cancer is estimated to exceed the values proposed by the WHO due to high exposure to carcinogenic agents. |
| [57] | To characterize polycyclic aromatic hydrocarbons (PAHs) present in the respiratory zone and on the skin of wildland firefighters, and evaluate their impact on urinary 1-hydroxypyrene (1-HP) levels across multiple firefighting rotations. | The samples exceeded the Biological Exposure Index of the American Conference of Governmental Industrial Hygienists for 1-HP. | There is a need to control the exposure of firefighters |
| [80] | Assess small airway dysfunction, spirometry, health-related quality of life (HR-QoL), and inflammatory biomarkers between the wildland firefighters and healthy controls. | The findings indicated a significantly greater alteration in the area under the reactance curve between 5 Hz and the resonant frequency (AX) during pollution periods compared to non-pollution periods among wildland firefighters, in contrast to healthy controls (adjusted mean difference = 0.15 kPa/L, 95% CI: 0.01, 0.28, p = 0.032). | Despite no observed changes in spirometry results, the authors suggest that there are alterations in respiratory parameters over a short period of time, as observed through biomarkers. |
| [58] | This study characterizes the baseline levels of OHPAHs in Portuguese wildland firefighters. Additionally, it offers a comprehensive evaluation of their current health status, encompassing parameters | The total levels of ΣOHPAHs corrected by creatinine ranged from 1.20 × 10−1 to 78.20 μmol/mol of creatinine, which were significantly higher in smokers. | There is a relationship between exposure to PAHs and changes in the levels of leukocytes and blood pressure. However, the authors consider that the fact that individuals are smokers may be an influencing factor. |
* IA—Beginning of the attack; PF—Fire design; IP—Prescribed Fire; NA—Not Applicable. ** Combined exposure (Em) to the mixture of respiratory irritants acrolein, formaldehyde, and respirable particulate, calculated as the summed ratios of each to their respective OSHA permissible exposure limits. *** Combined exposure (Em) to the mixture of respiratory irritants acrolein, formaldehyde, and respirable particulate, calculated as the summed ratios of each to their respective 2003 threshold limit values.

Table A2.
Summary of data on Health Impairments (n = 15).
Table A2.
Summary of data on Health Impairments (n = 15).
| Reference | Objective | Results | Evidence | |
|---|---|---|---|---|
| Cancer (n = 2) | [69] | To determine whether or not wildfire fighting is associated with elevated levels of PAH-DNA adduct in peripheral leukocytes. | No changes in PAH-DNA were identified in peripheral leukocytes. | The appearance of cancer in firefighters caused by these factors is unclear since other genotoxic substances may interact and increase cancer risk. |
| [70] | Assessing lung cancer risk and cardiovascular disease mortality related to smoking exposure. | Firefighter Short Season PM4 Daily Dose (mg) Mean (95th PCTL) Lung cancer CVD 0.15 (0.19) 1.08 (1.09) 1.16 (1.17) 0.30 (0.37) 1.13 (1.15) 1.19 (1.21) 0.45 (0.56) 1.18 (1.21) 1.22 (1.23) 0.60 (0.75) 1.22 (1.26) 1.23 (1.25) 0.74 (0.93) 1.26 (1.30) 1.25 (1.26) Firefighter Long Season P M4 Daily Dose (mg) Mean (95th PCTL) Lung cancer CVD 0.30 (0.37) 1.13 (1.15) 1.19 (1.21) 0.60 (0.75) 1.22 (1.26) 1.23 (1.25) 0.89 (1.12) 1.29 (1.35) 1.26 (1.28) 1.19 (1.50) 1.36 (1.43) 1.28 (1.30) 1.49 (1.87) 1.43 (1.51) 1.30 (1.32) | The results show that firefighters have a high risk of lung cancer and the onset of cardiovascular disease. | |
| Cardiovascular (n = 1) | [70] | Assessing lung cancer risk and cardiovascular disease mortality related to smoking exposure. | Firefighter Short Season PM4 Daily Dose (mg) Mean (95thPCTL) Lung cancer CVD 0.15 (0.19) 1.08 (1.09) 1.16 (1.17) 0.30 (0.37) 1.13 (1.15) 1.19 (1.21) 0.45 (0.56) 1.18 (1.21) 1.22 (1.23) 0.60 (0.75) 1.22 (1.26) 1.23 (1.25) 0.74 (0.93) 1.26 (1.30) 1.25 (1.26) Firefighter Long Season P M4 Daily Dose (mg) Mean (95thPCTL) Lung cancer CVD 0.30 (0.37) 1.13 (1.15) 1.19 (1.21) 0.60 (0.75) 1.22 (1.26) 1.23 (1.25) 0.89 (1.12) 1.29 (1.35) 1.26 (1.28) 1.19 (1.50) 1.36 (1.43) 1.28 (1.30) 1.49 (1.87) 1.43 (1.51) 1.30 (1.32) | The results show that firefighters have a high risk of lung cancer and the onset of cardiovascular disease. |
| Respiratory (n = 13) | [72] | Assessing the effects on the respiratory health of forest firefighters | Cross-shift Cough: Before the exhibition—25.7% During the exhibition—19.6% After exposure—26.1% Excretion: Before the exhibition—15.9% During the exhibition—22.0% After exposure—23.7% Sore throat: Before the exhibition—8.1% During the exhibition—19.6% After exposure—15.9% Tightness in the chest: Before the exhibition—4.6% During the exhibition—12.2% After exposure—15.3% Pain in the chest: Before the exhibition—1.4% During the exhibition—4.3% After exposure—4.3% Wheezing: Before the exhibition—4.1% During the exhibition—8.7% After exposure—4.3% Cross-season Cough: Before the exhibition—11.3% During the exhibition—NA After exposure—11.3% Expectoration: Before the exhibition—18.9% During the exhibition—NA After exposure—17.3% Chronic bronchitis: Before the exhibition—3.9% During the exhibition—NA After exposure—5.8% Wheezing: Before the exhibition—2.4% During the exhibition—NA After exposure—0.0% | In the firefighters evaluated, there was a decrease in lung function, but during the winter months, there was an improvement. |
| [73] | To characterize the respiratory function of active Portuguese volunteer firefighters exposed to forest fire smoke. | 5.9% of the individuals evaluated had risk factors for work-related lung disease and not as volunteer firefighters. 8.4% of the individuals already knew respiratory pathologies. 11.8% of the individuals presented criteria for bronchial obstruction. Individuals aged 40 years or older had a prevalence of 14.0% of obstructive patterns. 95.8% of the subjects did not use a cannula. | It was shown that the individual did not use personal protection means for the airways most of the time, and the lack of these means was verified in some corporations. | |
| [74] | To characterize the acute pulmonary and systemic inflammatory effects of exposure to forest fire smoke | Portable CO monitors show levels fluctuating between 5 and 20 ppm.65% of firefighters report having one or more respiratory symptoms. After exposure, on questionnaires, 16 subjects were asymptomatic, 13 had sputum production, 11 had a cough, 9 had nasal congestion, 6 had a headache, 6 had a sore throat, 5 had shortness of breath, and others had other symptoms. | Exposure to smoke by firefighters triggers an inflammatory response caused by an increase in sputum granulocytes. | |
| [47] | Evaluation of lung function during the firefighting season. | It was associated with declines in pre-shift Forced Vital Capacity (FVC) of 24 mL (p < 0.01) and 24 mL in pre-shift modified Tiffeneau-Pinelli index (FEV1) (p < 0.01) in non-allergic firefighters. Declines of 8ml of FVC (p < 0.01) and 4 mL of FEV1 (p < 0.01) in allergic firefighters. | No changes in lung function were evident between before and after shifts on fire days. However, it is known that there may be a cumulative effect after several days of exposure. | |
| [77] | Characterize forest fire smoke exposure and health impacts. | Threshold Limit Value-Time-Weighted Average (TLV-TWA): CO (25 ppm); NO2 (3 ppm); Short-term exposure limit value (TLV-STEL): CO (200 ppm); NO2 (5 ppm); Pico: CO (400 ppm); NO2 (20 ppm). | Firefighters significantly decrease respiratory function between the two measurements. | |
| [59] | Investigate the effect of occupational smoke exposure through biomarkers. | Evaluation of arithmetic averages of Biomarkers at 95% before exposure: Interleukin 1 beta (IL-1β) (pg/mL) (0.94 (0.51, 1.38)); Interleukin 8 (IL-8) (pg/mL) (0.93 (0.81, 1.06)); C-reactive protein (CRP) (ng/mL) (30.63 (19.72, 41.55)); Serum amyloid A (SAA) (ng/mL) (36.72 (21.17, 52.28)); Intercellular adhesion molecule-1 (ICAM-1) (ng/mL) (6.33 (5.50, 7.15)); Vascular cell adhesion protein 1 (VCAM-1) (ng/mL) (15.16 (13.00, 17.32)) Evaluation of arithmetic averages of Biomarkers at 95% after exposure: IL-1β (pg/mL) (0.58 (0.30, 0.86)); IL-8 (pg/mL) (1.67 (1.35, 1.99)); CRP (ng/mL) (31.63 (19.29, 43.97)); SAA (ng/mL) (33.92 (22.25, 45.60)); ICAM-1 (ng/mL) (6.29 (5.56, 7.03)); VCAM-1 (ng/mL) (14.53 (12.70, 16.36)) | There was no association between cross-shift and biomarker results compared to the onset of respiratory symptoms during exposure. | |
| [60] | Characterize occupational exposures from wildland firefighting and evaluate their associations with changes in lung function. | ΔFEV1 was a decline of 0.045 L (p = 0.08). | More significant drops in forced expiratory volume in 1 s were significantly associated with exposure to higher concentrations of LG in the respirable range. | |
| [52] | Assessing respiratory and airway health and systemic inflammation in Firefighters after fighting forest fires. | Respiratory symptoms such as wheezing, coughing, chest tightness, sneezing, and sputum were statistically significantly higher after firefighting (p = 0.028, p = 0.03, p = 0.02, p < 0.001, and p = 0.006, respectively). FEF25-75% predicted, and FEV1/FVC were statistically reduced in later exposure compared to off-season values (103 ± 32 vs. 111 ± 15, p = 0.026, and 84 ± 4 vs. 88 ± 8, p = 0.024, respectively). Increased neutrophils and eosinophils post-exposure compared to the off-season (48 ± 5% vs. 16 ± 4%, p = 0.035, and 3 ± 0.8% vs. 1.8 ± 0.7%, p = 0.05, respectively). IL-8 and TNF-α levels were statistically significantly higher in the post-exposure sputum compared to the off-season (p = 0.03 and p = 0.04, respectively). | Measurable eosinophilic and neutrophilic inflammation has been demonstrated in the airways at the bronchial level after acute exposure to forest firefighting. Firefighters’ Occupational exposure induces a systemic inflammation of the airways that is aggravated long-term during their exposure. | |
| [75] | Urinary mutagenicity assessment to characterize firefighter exposure on burning days compared to non-burning days. | Working days without firing µ[PM2.5] = 35.1 [95% CL: 15.9, 77.3] μg/m3 µ[CO] = 0.005 [95% CL: 0.002, 0.016] ppm Working days with firing µ[PM2.5] = 259.4 [95% LC: 156.1, 431.1] μg/m3 µ[CO] = 0.8 [95% LC: 0.4, 1.8] ppm [Urinary Creatinine] = 10 and 382 mg/dL, with 92% of samples above the lower end of the normal range (30–300 mg/dL). µ[MDA] = 894.6 (95% CL: 748.5, 1069.0) nmole/L and 84.3 (95% CL: 74.9, 95.0) μmol MDA/mole creatinine | No statistically significant increases between work shifts were observed in urinary mutagenicity. | |
| [43] | Determine acute pulmonary responses among firefighters. | Working days with firering µ[IL-8] = 0.02–0.03 pg/mL µ[CRP] = 2.40–2.56 pg/mL µ[sICAM-1] = 2.39–2.59 pg/mL µ[8- isoprostane] = 3.51–3.80 pg/mL | The results show no signs of airway inflammation after exposure. | |
| [76] | Investigate the association between polycyclic aromatic hydrocarbon-DNA adducts and occupational and dietary exposures to polycyclic aromatic hydrocarbons. | Times are charbroiled food in the past two weeks: 0 (weeks)—0.06 ± 0.07 (fmole/pg DNA) 1–2 (weeks)—0.10 ± 0.12 (fmole/pg DNA) 3–5 (weeks)—0.13 ± 0.13 (fmole/pg DNA) >5 (weeks)—0.21 ± 0.17 (fmole/pg DNA) Weeks since last ate charbroiled food: ≤1 week 0.13 ± 0.14 >1 week 0.07 ± 0.07 | There was no association between firefighting activity and PAH-DNA adduct level | |
| [78] | Assessing markers of exposure to forest fires. | Service A May Log total exposure PM2.5: 9.96 ± 1.22 Log highest day exposure: 7.95 ± 1.32 Days since the last deployment: 5.53 ± 4.25 Days since last fire: 4.22 ± 3.6 Dehydration score: 19.18 ± 17.68 Heat stress: 14.62 ± 13.17 Noise: 24.45 ± 19.04 Exhaustion: 43.93 ± 28.00 Musculoskeletal strain: 26.96 ± 21.14 August/September Log total exposure PM2.5: 9.96 ± 1.22 Log highest day exposure: - Days since the last deployment: 104.13 ± 15.57 Days since last fire: 69.66 ± 39.54 Dehydration score: - Heat stress: - Noise: - Exhaustion: - Musculoskeletal strain: - Service A August/September Log total exposure PM2. 9.96 ± 1.22 Log highest day exposure: 7.85 ± 1.33 Days since the last deployment: 103.25 ± 15.35 Days since last fire: 67.64 ± 39.21 Dehydration score: 20.8 ± 18.25 Heat stress: 17.4 ± 15.38 Noise: 24.61 ± 18.63 Exhaustion: 44.45 ± 28.32 Musculoskeletal strain: 27.37 ± 21.35 Service B August/September Log total exposure PM2: 12.23 ± 0.47 Log highest day exposure: 9.13 ± 1.01 Days since the last deployment: 74.74 ± 21.37 Days since last fire: 60.14 ± 31.23 Dehydration score: 47.81 ± 25.75 Heat stress: 50.65 ± 25.88 Noise: 39.35 ± 28.53 Exhaustion: 81.48 ± 20.52 Musculoskeletal strain: 61.23 ± 23.81 | PM2.5 were the most predictive of respiratory symptoms. |
Appendix B

Table A3.
Risk of Bias.
Table A3.
Risk of Bias.
| Criteria | Quality Rating | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
| [46] | Y | Y | NA | Y | N | NA | NA | Y | Y | Y | NA | NR | NA | Y | VG |
| [47] | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | NR | Y | Y | VG |
| [64] | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | NR | N | Y | VG |
| [48] | Y | Y | NR | Y | N | NA | NA | NA | Y | Y | NA | NR | NA | NR | G |
| [44] | Y | Y | NR | Y | N | NA | NA | NA | Y | Y | NA | NR | NA | NR | G |
| [54] | Y | Y | NR | Y | Y | Y | Y | Y | Y | Y | Y | NR | Y | NR | VG |
| [59] | Y | Y | NR | Y | N | NA | NA | NA | Y | Y | NA | NR | NA | NR | G |
| [60] | Y | Y | NR | Y | N | Y | Y | Y | Y | Y | Y | NR | Y | Y | VG |
| [61] | N | Y | Y | Y | N | NA | NA | NA | Y | Y | NA | NA | NA | NR | G |
| [65] | Y | Y | NR | Y | N | Y | Y | Y | Y | Y | Y | NR | Y | Y | VG |
| [66] | N | Y | Y | Y | N | NA | NA | NA | Y | Y | NA | NR | NA | NR | G |
| [53] | Y | Y | NR | Y | N | Y | Y | Y | Y | Y | Y | NR | NR | Y | VG |
| [52] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NR | Y | NR | VG |
| [45] | Y | Y | NR | Y | N | NA | NA | NA | Y | Y | Y | NA | NA | NR | VG |
| [55] | Y | Y | NR | Y | Y | Y | Y | Y | Y | Y | Y | NR | N | NR | VG |
| [62] | Y | Y | NR | Y | N | NA | NA | Y | Y | Y | NA | NA | NA | NR | G |
| [56] | Y | N | NA | NA | NA | NA | NA | NA | NA | N | NA | NR | NA | NR | - |
| [43] | Y | Y | NR | Y | N | Y | Y | Y | Y | Y | Y | NR | NA | Y | VG |
| [67] | Y | Y | NR | NR | Y | Y | Y | Y | Y | Y | Y | NA | NA | Y | VG |
| [51] | Y | Y | NR | Y | Y | NA | NR | NA | Y | Y | Y | NR | NR | NR | G |
| [49] | Y | Y | NR | Y | N | NA | NA | NA | Y | Y | NA | NR | NA | NR | G |
| [71] | Y | Y | NR | Y | NR | Y | Y | Y | Y | Y | Y | Y | NR | Y | VG |
| [50] | Y | Y | NR | Y | NR | Y | Y | Y | Y | Y | Y | Y | NR | Y | VG |
| [68] | Y | Y | NR | Y | NR | Y | Y | Y | Y | Y | Y | Y | NR | Y | VG |
| [57] | Y | Y | NR | Y | NR | Y | Y | Y | Y | Y | Y | Y | NR | Y | VG |
| [80] | Y | Y | NR | Y | NR | Y | Y | Y | Y | Y | Y | Y | NR | Y | VG |
| [58] | Y | Y | NR | Y | NR | Y | Y | Y | Y | Y | Y | Y | NR | T | VG |
| [69] | Y | Y | NR | Y | N | NA | NA | Y | Y | Y | NA | NR | NA | NR | G |
| [70] | Y | N | NR | NR | N | NA | NR | NA | Y | Y | NA | NA | NA | NR | F |
| [58] | Y | N | NA | NA | N | Y | Y | NA | N | Y | NA | NA | NA | NR | G |
| [72] | Y | Y | NR | Y | N | Y | Y | Y | Y | Y | Y | NR | NR | NR | G |
| [73] | Y | Y | NR | Y | N | N | NA | NA | NA | NA | Y | NR | NR | Y | G |
| [74] | Y | Y | Y | Y | Y | NA | NA | NA | NA | Y | Y | NR | NR | Y | VG |
| [47] | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | NR | Y | Y | VG |
| [77] | Y | Y | NR | Y | N | Y | Y | Y | NA | Y | Y | NR | NR | Y | G |
| [59] | Y | Y | NR | Y | N | NA | NA | NA | Y | Y | NA | NR | NA | NR | G |
| [60] | Y | Y | NR | Y | N | Y | Y | Y | Y | Y | Y | NR | Y | Y | VG |
| [52] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NR | Y | NR | VG |
| [75] | Y | Y | NR | Y | N | Y | Y | Y | Y | Y | Y | NR | N | Y | VG |
| [43] | Y | Y | NR | Y | N | Y | Y | Y | Y | Y | Y | NR | NA | Y | VG |
| [76] | Y | Y | NR | Y | Y | NA | NR | NA | Y | Y | Y | NR | NR | NR | G |
| [78] | Y | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NR | NA | NR | F |
Legend: Y—Yes; N—No; NA—Not Applicable; NR—Not Reported; F—Fair; G—Good; VG—Very Good.
References
- Bu, Y.; Wu, W.; Zeng, X.; Koehl, L.; Tartare, G. A Wearable Intelligent System for Real Time Monitoring Firefighter’s Physiological State and Predicting Dangers. In Proceedings of the 2015 IEEE 16th International Conference on Communication Technology (ICCT) 2016, Hangzhou, China, 18–20 October 2015; pp. 429–432. [Google Scholar] [CrossRef]
- Raj, J.V.; Sarath, T.V. An IoT Based Real-Time Stress Detection System for Fire-Fighters. In Proceedings of the 2019 International Conference on Intelligent Computing and Control Systems, ICCS 2019, Madurai, India, 15–17 May 2019; pp. 354–360. [Google Scholar]
- Groot, E.; Caturay, A.; Khan, Y.; Copes, R. A Systematic Review of the Health Impacts of Occupational Exposure to Wildland Fires. Int. J. Occup. Med. Environ. Health 2019, 32, 121–140. [Google Scholar] [CrossRef] [PubMed]
- Koopmans, E.; Fyfe, T.; Eadie, M.; Pelletier, C. Exploring Prevention and Mitigation Strategies to Reduce the Health Impacts of Occupational Exposure to Wildfires for Wildland Firefighters and Related Personnel: Protocol of a Scoping Study. Syst. Rev. 2020, 9, 119. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.J.; Cordeiro, C.R.; Ferreira, P.; Miranda, A.I.; Martins, V.; Viegas, D.X. Firefighter Occupational Exposures in Forest Fire Settings—Three Years of the FUMEXP Project. Eur. Respir. J. 2011, 38, 4169. [Google Scholar]
- Perroni, F.; Guidetti, L.; Cignitti, L.; Baldari, C. Psychophysiological Responses of Firefighters to Emergencies: A Review. Open Sports Sci. J. 2014, 7, 8–15. [Google Scholar] [CrossRef]
- Wohlgemuth, K.; Sekiguchi, Y.; Mota, J. Overexertion and Heat Stress in the Fire Service: A New Conceptual Framework. Am. J. Ind. Med. 2023, 66, 705–709. [Google Scholar] [CrossRef] [PubMed]
- CDC Fire Fighter Fatality Map. Available online: https://wwwn.cdc.gov/Wisards/fffmap/ (accessed on 11 June 2024).
- Grant, C.; Hamins, A.; Bryner, N.; Jones, A.; Koepke, G. Research Roadmap for Smart Fire Fighting; Summary Report Research Roadmap for National Institute of Standards and Technology; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2015. [Google Scholar]
- De Castro, C.F.; Abrantes, J.M.B. Combate a Incêndios Urbanos e Industriais; Escuela Nacional de Bomberos: Tegucigalpa, Honduras, 2005; Volume X, ISBN 9728792174. [Google Scholar]
- Lourenço, L.; Serra, G.; Mota, L.; Paúl, J.J.; Parola, J.; Reis, J. Manual de Combate a Incêndios Florestais para Equipas de Primeira Intervenção; Escuela Nacional de Bomberos: Tegucigalpa, Honduras, 2006; ISBN 9728792263. [Google Scholar]
- Carvalho, F.P.; Oliveira, J.M.; Malta, M. Exposure to Radionuclides in Smoke from Vegetation Fires. Sci. Total Environ. 2014, 472, 421–424. [Google Scholar] [CrossRef] [PubMed]
- Austin, C. Wildland Firefighter Health Risks and Respiratory Protection; IRSST: Montreal, QC, Canada, 2008; ISBN 9782896312962. [Google Scholar]
- Melius, J. Occupational Health for Firefighters. Occup. Med. 2000, 16, 101–108. [Google Scholar]
- Soteriades, E.S.; Kim, J.; Christophi, C.A.; Kales, S.N. Cancer Incidence and Mortality in Firefighters: A State-of-the-Art Review and Meta-َAnalysis. Asian Pac. J. Cancer Prev. 2019, 20, 3221–3231. [Google Scholar] [CrossRef]
- Broyles, G. Wildland Firefighter Smoke Exposure; United States Department of Agriculture: Washington, DC, USA, 2013. [Google Scholar]
- Mustajbegovic, J.; Zuskin, E.; Schachter, E.N.; Kern, J.; Vrcic-Keglevic, M.; Heimer, S.; Vitale, K.; Nada, T. Respiratory Function in Active Firefighters. Am. J. Ind. Med. 2001, 40, 55–62. [Google Scholar] [CrossRef]
- Harrison, R.; Materna, B.L.; Rothman, N. Respiratory Health Hazards and Lung Function in Wildland Firefighters. Occup. Med. 1995, 10, 857–870. [Google Scholar]
- Bigert, C.; Gustavsson, P.; Straif, K.; Taeger, D.; Pesch, B.; Kendzia, B.; Schüz, J.; Stücker, I.; Guida, F.; Brüske, I.; et al. Lung Cancer Among Firefighters. J. Occup. Environ. Med. 2016, 58, 1137–1143. [Google Scholar] [CrossRef] [PubMed]
- LeMasters, G.K.; Genaidy, A.M.; Succop, P.; Deddens, J.; Sobeih, T.; Barriera-Viruet, H.; Dunning, K.; Lockey, J. Cancer Risk among Firefighters: A Review and Meta-Analysis of 32 Studies. J. Occup. Environ. Med. 2006, 48, 1189–1202. [Google Scholar] [CrossRef]
- Interventions, E.; Congruence, C. Firefighters’ Cardiovascular Risk Behaviors. Workplace Health Saf. 2014, 62, 27–34. [Google Scholar] [CrossRef]
- Whitworth, J.A.; Williamson, P.M.; Mangos, G.; Kelly, J.J. Cardiovascular Consequences of Cortisol Excess. Vasc. Health Risk Manag. 2005, 1, 291–299. [Google Scholar] [CrossRef]
- Yoo, H.L.; Franke, W.D. Prevalence of Cardiovascular Disease Risk Factors in Volunteer Firefighters. J. Occup. Environ. Med. 2009, 51, 958–962. [Google Scholar] [CrossRef]
- Adetona, O.; Reinhardt, T.E.; Domitrovich, J.; Broyles, G.; Adetona, A.M.; Kleinman, M.T.; Ottmar, R.D.; Naeher, L.P. Review of the Health Effects of Wildland Fire Smoke on Wildland Firefighters and the Public. Inhal. Toxicol. 2016, 28, 95–139. [Google Scholar] [CrossRef]
- Withen, P. Climate Change and Wildland Firefighter Health and Safety. New Solut. A J. Environ. Occup. Health Policy 2015, 24, 577–584. [Google Scholar] [CrossRef]
- Kamran, M.; Wattimena, R.K.; Armaghani, D.J.; Asteris, P.G.; Jiskani, I.M.; Mohamad, E.T. Intelligent Based Decision-Making Strategy to Predict Fire Intensity in Subsurface Engineering Environments. Process Saf. Environ. Prot. 2023, 171, 374–384. [Google Scholar] [CrossRef]
- Ullah, B.; Kamran, M.; Rui, Y. Predictive Modeling of Short-Term Rockburst for the Stability of Subsurface Structures Using Machine Learning Approaches: T-SNE, K-Means Clustering and XGBoost. Mathematics 2022, 10, 449. [Google Scholar] [CrossRef]
- Kamran, M.; Shahani, N.M. Decision Support System for the Prediction of Mine Fire Levels in Underground Coal Mining Using Machine Learning Approaches. Min. Metall. Explor. 2022, 39, 591–601. [Google Scholar] [CrossRef]
- Weidinger, J.; Schlauderer, S.; Overhage, S. Is the Frontier Shifting into the Right Direction? A Qualitative Analysis of Acceptance Factors for Novel Firefighter Information Technologies. Inf. Syst. Front. 2018, 20, 669–692. [Google Scholar] [CrossRef]
- Adams, T.; Butler, B.; Brown, S.; Wright, V.; Black, A. Bridging the Divide between Fire Safety Research and Fighting Fire Safely: How Do We Convey Research Innovation to Contribute More Effectively to Wildland Firefighter Safety? Int. J. Wildland Fire 2017, 26, 107. [Google Scholar] [CrossRef][Green Version]
- Shamsudin, N.M.; Mahmood, N.H.N.; Rahim, A.R.A.; Mohamad, S.F.; Masrom, M. Virtual Reality Training Approach for Occupational Safety and Health: A Pilot Study. Adv. Sci. Lett. 2018, 24, 2447–2450. [Google Scholar] [CrossRef]
- Md Shamsudin, N.; NIk Mahmood, N.H.; Abdul Rahim, A.; Fathi, M.S.; Masrom, M. Virtual Reality for Construction Occupational Safety and Health Training: A Review. Adv. Sci. Lett. 2018, 24, 2444–2446. [Google Scholar] [CrossRef]
- Islam, S.; Huang, Q.; Afghah, F.; Fule, P.; Razi, A. Fire Frontline Monitoring by Enabling UAV-Based Virtual Reality with Adaptive Imaging Rate. In Proceedings of the Conference Record—Asilomar Conference on Signals, Systems and Computers, Pacific Grove, CA, USA, 3–6 November 2019; Volume 2019, pp. 368–372. [Google Scholar]
- Yfantis, E.A. A UAV with Autonomy, Pattern Recognition for Forest Fire Prevention, and AI for Providing Advice to Firefighters Fighting Forest Fires. In Proceedings of the 2019 IEEE 9th Annual Computing and Communication Workshop and Conference, CCWC 2019, Las Vegas, NV, USA, 7–9 January 2019; pp. 409–413. [Google Scholar]
- Hinkley, E.; Zajkowski, T.; Ambrosia, V.; Schoenung, S. Small UAS Demonstration for Wildlife Surveillance. In Proceedings of the AIAA Infotech@Aerospace 2007 Conference and Exhibit, Reston, VA, USA, 7–10 May 2007. [Google Scholar] [CrossRef]
- Park, M.; Tran, D.Q.; Jung, D.; Park, S. Wildfire-Detection Method Using Densenet and Cyclegan Data Augmentation-Based Remote Camera Imagery. Remote Sens. 2020, 12, 3715. [Google Scholar] [CrossRef]
- Bjurling, O.; Granlund, R.; Alfredson, J.; Arvola, M.; Ziemke, T. Drone Swarms in Forest Firefighting: A Local Development Case Study of Multi-Level Human-Swarm Interaction. In Proceedings of the 11th Nordic Conference on Human-Computer Interaction: Shaping Experiences, Shaping Society, Tallinn, Estonia, 25–29 October 2020; Association for Computing Machinery: New York, NY, USA, 2020. [Google Scholar]
- Teixeira, T.; Dias, I.; Santos, J.; Vaz, M.; Baptista, J.S.; Guedes, J.C. Occupational Exposure and Health of Wildland Firefighters: Protocol for a Systematic Review. Int. J. Occup. Environ. Saf. 2024, 8, 1. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L. PRISMA-P (Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols) 2015 Checklist: Recommended Items to Address in a Systematic Review Protocol *. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, T.P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- National Heart, Lung, and Blood Institute. Study Quality Assessment Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 13 June 2024).
- Adetona, A.M.; Martin, W.K.; Warren, S.H.; Hanley, N.M.; Adetona, O.; Zhang, J.J.; Simpson, C.; Paulsen, M.; Rathbun, S.; Wang, J.-S.; et al. Urinary Mutagenicity and Other Biomarkers of Occupational Smoke Exposure of Wildland Firefighters and Oxidative Stress. Inhal. Toxicol. 2019, 31, 73–87. [Google Scholar] [CrossRef]
- Adetona, O.; Dunn, K.; Hall, D.; Achtemeier, G.; Stock, A.; Naeher, L. Personal PM2.5 Exposure Among Wildland Firefighters Working at Prescribed Forest Burns in Southeastern United States. J. Occup. Environ. Hyg. 2011, 8, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Adetona, O.; Simpson, C.D.; Li, Z.; Sjodin, A.; Antonia, M.; Naeher, L.P.; Sciences, O.H. Hydroxylated Polycyclic Aromatic Hydrocarbons as Biomarkers of Exposure to Wood Smoke in Wildland Firefighters. J. Expo. Sci. Environ. Epidemiol. 2017, 27, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Reinhardt, T.E.; Ottmar, R.D. Baseline Measurements of Smoke Exposure among Wildland Firefighters. J. Occup. Environ. Hyg. 2004, 1, 593–606. [Google Scholar] [CrossRef] [PubMed]
- Swiston, J.R.; Davidson, W.; Attridge, S.; Li, G.T.; Brauer, M.; Van Eeden, S.F. Wood Smoke Exposure Induces a Pulmonary and Systemic Inflammatory Response in Firefighters. Eur. Respir. J. 2008, 32, 129–138. [Google Scholar] [CrossRef]
- Miranda, A.I.; Martins, V.; Cascão, P.; Amorim, J.H.; Valente, J.; Tavares, R.; Borrego, C.; Tchepel, O.; Ferreira, A.J.; Cordeiro, C.R.; et al. Monitoring of Firefighters Exposure to Smoke during Fire Experiments in Portugal. Environ. Int. 2010, 36, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Navarro, K.M.; West, M.R.; O’Dell, K.; Sen, P.; Chen, I.-C.; Fischer, E.V.; Hornbrook, R.S.; Apel, E.C.; Hills, A.J.; Jarnot, A.; et al. Exposure to Particulate Matter and Estimation of Volatile Organic Compounds across Wildland Firefighter Job Tasks. Environ. Sci. Technol. 2021, 55, 11795–11804. [Google Scholar] [CrossRef] [PubMed]
- Navarro, K.M.; Fent, K.; Mayer, A.C.; Brueck, S.E.; Toennis, C.; Law, B.; Meadows, J.; Sammons, D.; Brown, S. Characterization of Inhalation Exposures at a Wildfire Incident during the Wildland Firefighter Exposure and Health Effects (WFFEHE) Study. Ann. Work Expo. Health 2023, 67, 1011–1017. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-M.; Song, C.; Chartier, R.; Kremer, J.; Naeher, L.; Adetona, O. Characterization of Occupational Smoke Exposure among Wildland Firefighters in the Midwestern United States. Environ. Res. 2021, 193, 110541. [Google Scholar] [CrossRef]
- Gaughan, D.M.; Piacitelli, C.A.; Chen, B.T.; Law, B.F.; Virji, M.A.; Edwards, N.T.; Enright, P.L.; Schwegler-Berry, D.E.; Leonard, S.S.; Wagner, G.R.; et al. Exposures and Cross-Shift Lung Function Declines in Wildland Firefighters. J. Occup. Environ. Hyg. 2014, 11, 591–603. [Google Scholar] [CrossRef]
- Naeher, L.P.; Barr, D.B.; Adetona, O.; Simpson, C.D. Urinary Levoglucosan as a Biomarker for Woodsmoke Exposure in Wildland Firefighters. Int. J. Occup. Environ. Health 2013, 19, 304–310. [Google Scholar] [CrossRef]
- Reisen, F.; Hansen, D.; Meyer, P. Exposure to Bushfire Smoke during Prescribed Burns and Wildfires: Firefighters’ Exposure Risks and Options. Environ. Int. 2011, 37, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Navarro, K.M.; Cisneros, R.; Noth, E.M.; Balmes, J.R.; Hammond, S.K. Occupational Exposure to Polycyclic Aromatic Hydrocarbon of Wildland Firefighters at Prescribed and Wildland Fires. Environ. Sci. Technol. 2017, 51, 6461–6469. [Google Scholar] [CrossRef] [PubMed]
- Navarro, K.M.; Cisneros, R.; Schweizer, D.; Chowdhary, P.; Noth, E.M.; Balmes, J.R.; Hammond, S.K. Incident Command Post Exposure to Polycyclic Aromatic Hydrocarbons and Particulate Matter during a Wildfire. J. Occup. Environ. Hyg. 2019, 16, 735–744. [Google Scholar] [CrossRef] [PubMed]
- Cherry, N.; Broznitsky, N.; Fedun, M.; Kinniburgh, D.; Shum, M.; Tiu, S.; Zadunayski, T.; Zarft, M.; Zhang, X. Exposures to Polycyclic Aromatic Hydrocarbons and Their Mitigation in Wildland Firefighters in Two Canadian Provinces. Ann. Work Expo. Health 2023, 67, 354–365. [Google Scholar] [CrossRef] [PubMed]
- Barros, B.; Paiva, A.M.; Oliveira, M.; Alves, S.; Esteves, F.; Fernandes, A.; Vaz, J.; Slezakova, K.; Costa, S.; Teixeira, J.P.; et al. Baseline Data and Associations between Urinary Biomarkers of Polycyclic Aromatic Hydrocarbons, Blood Pressure, Hemogram, and Lifestyle among Wildland Firefighters. Front. Public. Health 2024, 12, 1338435. [Google Scholar] [CrossRef] [PubMed]
- Miranda, A.I.; Martins, V.; Casco, P.; Amorim, J.H.; Valente, J.; Borrego, C.; Ferreira, A.J.; Cordeiro, C.R.; Viegas, D.X.; Ottmar, R. Wildland Smoke Exposure Values and Exhaled Breath Indicators in Firefighters. J. Toxicol. Environ. Health Part A Curr. Issues 2012, 75, 831–843. [Google Scholar] [CrossRef] [PubMed]
- Hejl, A.M.; Adetona, O.; Diaz-Sanchez, D.; Carter, J.D.; Commodore, A.A.; Rathbun, S.L.; Naeher, L.P. Inflammatory Effects of Woodsmoke Exposure among Wildland Firefighters Working at Prescribed Burns at the Savannah River Site, SC. J. Occup. Environ. Hyg. 2013, 10, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Dunn, K.H.; Shulman, S.; Stock, A.L.; Naeher, L.P. Personal Carbon Monoxide Exposures among Firefighters at Prescribed Forest Burns in the Southeastern United States. Arch. Environ. Occup. Health 2013, 68, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Henn, S.A.; Butler, C.; Li, J.; Sussell, A.; Hale, C.; Broyles, G.; Reinhardt, T. Carbon Monoxide Exposures among U.S. Wildland Firefighters by Work, Fire, and Environmental Characteristics and Conditions. J. Occup. Environ. Hyg. 2019, 16, 793–803. [Google Scholar] [CrossRef]
- Adetona, A.M.; Adetona, O.; Chartier, R.T.; Paulsen, M.H.; Simpson, C.D.; Rathbun, S.L.; Naeher, L.P. Differences in Fine Particle Exposure and Estimated Pulmonary Ventilation Rate with Respect to Work Tasks of Wildland Firefighters at Prescribed Burns: A Repeated Measures Study. Ann. Work Expo. Health 2022, 66, 985–997. [Google Scholar] [CrossRef]
- Neitzel, R.; Naeher, L.P.; Paulsen, M.; Dunn, K.; Stock, A.; Simpson, C.D. Biological Monitoring of Smoke Exposure among Wildland Firefighters: A Pilot Study Comparing Urinary Methoxyphenols with Personal Exposures to Carbon Monoxide, Particular Matter, and Levoglucosan. J. Expo. Sci. Environ. Epidemiol. 2009, 19, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Adetona, O.; Simpson, C.; Onstad, G.; Naeher, L. Exposure of Wildland Firefighters to Carbon Monoxide, Fine Particles, and Levoglucosan. Ann. Occup. Hyg. 2013, 57, 979–991. [Google Scholar] [CrossRef] [PubMed]
- Adetona, O.; Zhang, J.J.; Hall, D.B.; Wang, J.-S.; Vena, J.E.; Naeher, L.P. Occupational Exposure to Woodsmoke and Oxidative Stress in Wildland Firefighters. Sci. Total Environ. 2013, 449, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Cherry, N.; Beach, J.; Galarneau, J.-M. Are Inflammatory Markers an Indicator of Exposure or Effect in Firefighters Fighting a Devastating Wildfire? Follow-up of a Cohort in Alberta, Canada. Ann. Work Expo. Health 2021, 65, 635–648. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, J.; Bessa, M.J.; Delerue-Matos, C.; Sarmento, B.; Santos-Silva, A.; Rodrigues, F.; Oliveira, M. Firefighters’ Personal Exposure to Gaseous PAHs during Controlled Forest Fires: A Case Study with Estimation of Respiratory Health Risks and in Vitro Toxicity. Sci. Total Environ. 2024, 908, 168364. [Google Scholar] [CrossRef] [PubMed]
- Rothman, N.; Correa-Villaseńor, A.; Patrick Ford, D.; Poirier, M.C.; Haas, R.; Hansen, J.A.; O’Toole, T.; Strickland, P.T. Contribution of Occupation and Diet to White Blood Cell Polycyclic Aromatic Hydrocarbon-DNA Adducts in Wildland Firefighters. Cancer Epidemiol. Biomark. Prev. 1993, 2, 341–347. [Google Scholar]
- Navarro, K.M.; Kleinman, M.T.; Mackay, C.E.; Reinhardt, T.E.; Balmes, J.R.; Broyles, G.A.; Ottmar, R.D.; Naher, L.P.; Domitrovich, J.W. Wildland Firefighter Smoke Exposure and Risk of Lung Cancer and Cardiovascular Disease Mortality. Environ. Res. 2019, 173, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, J.V.; Alvim-Ferraz, M.C.M.; Martins, F.G.; Sousa, S.I.V. Occupational Exposure of Firefighters to Hazardous Pollutants during Prescribed Fires in Portugal. Chemosphere 2024, 352, 141355. [Google Scholar] [CrossRef] [PubMed]
- Serra, A.; Mocci, F.; Sanna Randaccio, F. Pulmonary Function in Sardinian Fire Fighters. Am. J. Ind. Med. 1996, 30, 78–82. [Google Scholar] [CrossRef]
- Betchley, C.; Koenig, J.Q.; Van Belle, G.; Checkoway, H.; Reinhardt, T. Pulmonary Function and Respiratory Symptoms in Forest Firefighters. Am. J. Ind. Med. 1997, 31, 503–509. [Google Scholar] [CrossRef]
- Almeida, A.G.; Duarte, R.; Mieiro, L.; Paiva, A.C.; Rodrigues, A.M.; Almeida, M.H.; Bárbara, C. Pulmonary Function in Portuguese Firefighters. Rev. Port. Pneumol. 2007, XIII, 149–157. [Google Scholar] [CrossRef]
- Gianniou, N.; Giannakopoulou, C.; Dima, E.; Kardara, M.; Katsaounou, P.; Tsakatikas, A.; Roussos, C.; Koulouris, N.; Rovina, N. Acute Effects of Smoke Exposure on Airway and Systemic Inflammation in Forest Firefighters. J. Asthma Allergy 2018, 11, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-M.; Adetona, A.; Song, C.; Naeher, L.; Adetona, O. Measuring Acute Pulmonary Responses to Occupational Wildland Fire Smoke Exposure Using Exhaled Breath Condensate. Physiol. Behav. 2020, 176, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Adetona, O.; Hall, D.; Naeher, L. Lung Function Changes in Wildland Firefighters Working at Prescribed Burns. Inhal. Toxicol. 2011, 23, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.; Costa, S.; Vaz, J.; Fernandes, A.; Slezakova, K.; Delerue-Matos, C.; Teixeira, J.P.; Carmo Pereira, M.; Morais, S. Firefighters Exposure to Fire Emissions: Impact on Levels of Biomarkers of Exposure to Polycyclic Aromatic Hydrocarbons and Genotoxic/Oxidative-Effects. J. Hazard. Mater. 2020, 383, 121179. [Google Scholar] [CrossRef] [PubMed]
- Niyatiwatchanchai, N.; Pothirat, C.; Chaiwong, W.; Liwsrisakun, C.; Phetsuk, N.; Duangjit, P.; Choomuang, W. Short-Term Effects of Air Pollutant Exposure on Small Airway Dysfunction, Spirometry, Health-Related Quality of Life, and Inflammatory Biomarkers in Wildland Firefighters: A Pilot Study. Int. J. Environ. Health Res. 2023, 33, 850–863. [Google Scholar] [CrossRef] [PubMed]
- Dvornik, A.A.; Dvornik, A.M.; Korol, R.A.; Shamal, N.V.; Gaponenko, S.O.; Bardyukova, A.V. Potential Threat to Human Health during Forest Fires in the Belarusian Exclusion Zone. Aerosol Sci. Technol. 2018, 52, 923–932. [Google Scholar] [CrossRef]
- ACGIH. Limites de Exposição Para Substâncias Químicas e Agentes Físicos & Índices Biológicos de Exposição; 2008. [Google Scholar]
- Austin, C. Wildland Firefighter Health Risks and Respiratory Protection: Risques Pour la Santé des Pompiers Forestiers et Protection Respiratoire; Institut de Recherche Robert-Sauvé en Santé et en Sécurité du Travail (IRSST): Montreal, QC, Canada, 2008; ISBN 9782896312962. [Google Scholar]
- Baxter, C.S.; Ross, C.S.; Lockey, J.E. Characterization of Firefighter Smoke Exposure. Fire Technol. 2014, 50, 993–1019. [Google Scholar] [CrossRef]
- Materna, B.L.; Koshland, C.P.; Harrison, R.J.; Materna, B.L.; Koshland, C.P.; Harrison, R.J. Carbon Monoxide Exposure in Wildland Firefighting: A Comparison of Monitoring Methods Carbon Monoxide Exposure in Wildland Firefighting: A Comparison of Monitoring Methods. J. Occup. Environ. Hyg. 2011, 8, 0898. [Google Scholar] [CrossRef]
- Venkatraman, G.; Giribabu, N.; Mohan, P.S.; Muttiah, B.; Govindarajan, V.K.; Alagiri, M.; Abdul Rahman, P.S.; Karsani, S.A. Environmental Impact and Human Health Effects of Polycyclic Aromatic Hydrocarbons and Remedial Strategies: A Detailed Review. Chemosphere 2024, 351, 141227. [Google Scholar] [CrossRef]
- Mallah, M.A.; Changxing, L.; Mallah, M.A.; Noreen, S.; Liu, Y.; Saeed, M.; Xi, H.; Ahmed, B.; Feng, F.; Mirjat, A.A.; et al. Polycyclic Aromatic Hydrocarbon and Its Effects on Human Health: An Overeview. Chemosphere 2022, 296, 133948. [Google Scholar] [CrossRef]
- CDC Polycyclic Aromatic Hydrocarbons (PAHs). Available online: https://wwwn.cdc.gov/TSP/ToxFAQs/ToxFAQsDetails.aspx?faqid=121&toxid=25 (accessed on 27 January 2024).
- Genovesi, M.G.; Tashkin, D.P.; Chopra, S.; Morgan, M.; McElroy, C. Transient Hypoxemia in Firemen Following Inhalation of Smoke. Chest 1977, 71, 441–444. [Google Scholar] [CrossRef]
- Haponik, E.F. Clinical Smoke Inhalation Injury: Pulmonary Effects. Occup. Med. 1993, 8, 430–468. [Google Scholar]
- Witt, M.; Goniewicz, M.; Pawłowski, W.; Goniewicz, K. Analysis of the Impact of Harmful Factors in the Workplace on Functioning of the Respiratory System of Firefighters. Ann. Agric. Environ. Med. 2017, 24, 406–410. [Google Scholar] [CrossRef] [PubMed]
- Orysiak, J.; Młynarczyk, M.; Piec, R.; Jakubiak, A. Lifestyle and Environmental Factors May Induce Airway and Systemic Inflammation in Firefighters. Environ. Sci. Pollut. Res. 2022, 29, 73741–73768. [Google Scholar] [CrossRef]
- Viner, B.; Jannik, T.; Stone, D.; Hepworth, A.; Naeher, L.; Adetona, O.; Blake, J.; Eddy, T. Modelling and Mitigating Dose to Firefighters from Inhalation of Radionuclides in Wildland Fire Smoke. Int. J. Wildland Fire 2015, 24, 723–733. [Google Scholar] [CrossRef]
- Abreu, A.; Costa, C.; Pinho e Silva, S.; Morais, S.; do Carmo Pereira, M.; Fernandes, A.; Moraes de Andrade, V.; Teixeira, J.P.; Costa, S. Wood Smoke Exposure of Portuguese Wildland Firefighters: DNA and Oxidative Damage Evaluation. J. Toxicol. Environ. Health Part A Curr. Issues 2017, 80, 596–604. [Google Scholar] [CrossRef]
- EU-OSHA—2024 Work-Related Cancer. Available online: https://osha.europa.eu/en/themes/work-related-.diseases/work-related-cancer (accessed on 27 January 2024).
- Evangeliou, N.; Balkanski, Y.; Cozic, A.; Hao, W.M.; Møller, A.P. Wildfires in Chernobyl-Contaminated Forests and Risks to the Population and the Environment: A New Nuclear Disaster about to Happen? Environ. Int. 2014, 73, 346–358. [Google Scholar] [CrossRef]
- Gill, B.; Britz-McKibbin, P. Biomonitoring of Smoke Exposure in Firefighters: A Review. Curr. Opin. Environ. Sci. Health 2020, 15, 57–65. [Google Scholar] [CrossRef]
- Uprety, S.; Caglio, J.; Ho, M.; Chio, C.H.; Mckeefery, S.; Goh, J.H.; Marcellin, M.; Melde, K. A Telemetry System for Firefighters. In Proceedings of the International Telemetering Conference, Las Vegas, NV, USA, 26–29 October 2009; Volume 45. [Google Scholar]
- Barbosa, J.V.; Farraia, M.; Branco, P.T.B.S.; Alvim-Ferraz, M.C.M.; Martins, F.G.; Annesi-Maesano, I.; Sousa, S.I.V. The Effect of Fire Smoke Exposure on Firefighters’ Lung Function: A Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 16799. [Google Scholar] [CrossRef]
- CDC Carbon Monoxide. Available online: https://www.cdc.gov/niosh/npg/npgd0105.html (accessed on 20 December 2019).
- Bott, R.C.; Kirk, K.M.; Logan, M.B.; Reid, D.A. Diesel Particulate Matter and Polycyclic Aromatic Hydrocarbons in Fire Stations. Environ. Sci. Process Impacts 2017, 19, 1320–1326. [Google Scholar] [CrossRef] [PubMed]
- Caton, S.E.; Hakes, R.S.P.; Gorham, D.J.; Zhou, A.; Gollner, M.J. Review of Pathways for Building Fire Spread in the Wildland Urban Interface Part I: Exposure Conditions. Fire Technol. 2017, 53, 429–473. [Google Scholar] [CrossRef]
- Kganyago, M.; Shikwambana, L. Assessment of the Characteristics of Recent Major Wildfires in the USA, Australia and Brazil in 2018–2019 Using Multi-Source Satellite Products. Remote Sens. 2020, 12, 1803. [Google Scholar] [CrossRef]
- De Castro, C.F.; Serra, G.; Parola, J.; Reis, J.; Lourenço, L.; Correia, S. Combate a Incêndios Florestais; Escuela Nacional de Bomberos: Tegucigalpa, Honduras, 2003; Volume XIII, ISBN 9728792131. [Google Scholar]
- de Carvalho, J.B.; Lopes, J.P. Classificação de Incêndios Florestais—Manual Do Utilizador; Escuela Nacional de Bomberos: Tegucigalpa, Honduras, 2001; ISBN 972-8097-34-4. [Google Scholar]
- Department of Homeland Security Science and Technology Directorate. Wildland Firefighter Respiratory Protection. 2018. Available online: https://www.dhs.gov/science-and-technology/saver/respiratory-protection-wildland-firefighting (accessed on 15 January 2024).
- Autoridade Nacional de Emergência e Proteção Civil. Incêndios Florestais. 2010. Available online: https://prociv.gov.pt/pt/legislacao/ (accessed on 15 January 2024).
- CDC HEAT-RELATED ILLNESSES 2017. Available online: https://www.cdc.gov/niosh/topics/heatstress/heatrelillness.html (accessed on 15 March 2024).
- Savioli, G.; Zanza, C.; Longhitano, Y.; Nardone, A.; Varesi, A.; Ceresa, I.F.; Manetti, A.C.; Volonnino, G.; Maiese, A.; La Russa, R. Heat-Related Illness in Emergency and Critical Care: Recommendations for Recognition and Management with Medico-Legal Considerations. Biomedicines 2022, 10, 2542. [Google Scholar] [CrossRef] [PubMed]
- Kales, S.N.; Soteriades, E.S.; Christophi, C.A.; Christiani, D.C. Emergency duties and deaths from heart disease among firefighters in the United States. N. Engl. J. Med. 2007, 356, 1207–1215. [Google Scholar] [CrossRef] [PubMed]
- Marks, A.N.; Sol, J.A.; Domitrovich, J.W.; West, M.R.; Ruby, B.C. Total Energy Intake and Self-Selected Macronutrient Distribution During Wildland Fire Suppression. Wilderness Environ. Med. 2020, 31, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Bal, E.; Arslan, O.; Tavacioglu, L. Prioritization of the Causal Factors of Fatigue in Seafarers and Measurement of Fatigue with the Application of the Lactate Test. Saf. Sci. 2015, 72, 46–54. [Google Scholar] [CrossRef]
- Mamouei, M.; Budidha, K.; Baishya, N.; Qassem, M.; Kyriacou, P. Comparison of Wavelength Selection Methods for In-Vitro Estimation of Lactate: A New Unconstrained, Genetic Algorithm-Based Wavelength Selection. Sci. Rep. 2020, 10, 16905. [Google Scholar] [CrossRef] [PubMed]
- Doğan, N.; Savrun, A.; Levent, S.; Günaydin, G.P.; Çelik, G.K.; Akküçük, H.; Çevik, Y. Can Initial Lactate Levels Predict the Severity of Unintentional Carbon Monoxide Poisoning? Hum. Exp. Toxicol. 2015, 34, 324–329. [Google Scholar] [CrossRef]
- Akintola, A.A.; van de Pol, V.; Bimmel, D.; Maan, A.C.; van Heemst, D. Comparative Analysis of the Equivital EQ02 Lifemonitor with Holter Ambulatory ECG Device for Continuous Measurement of ECG, Heart Rate, and Heart Rate Variability: A Validation Study for Precision and Accuracy. Front. Physiol. 2016, 7, 1–14. [Google Scholar] [CrossRef]
- Tharion, W.J.; Buller, M.J.; Clements, C.M.; Dominguez, M.D.; Sampsonis, M.C.; Mullen, S.P.; Karis, A.J.; Potter, A.W. Human Factors Evaluation of the Hidalgo Equivital TM Eq-02; U.S. Army Research Institute of Environmental Medicine: Natick, MA, USA, 2013; ISBN 5082334735. [Google Scholar]
- Henrique, L.; Messias, D.; Elias, E.; Polisel, C.; Manchado-gobatto, B. Advances of the Reverse Lactate Threshold Test: Non-Invasive Proposal Based on Heart Rate and Effect of Previous Cycling Experience. PLoS ONE 2018, 13, e0194313. [Google Scholar] [CrossRef]
- Huang, S.C.; Casaburi, R.; Liao, M.F.; Liu, K.C.; Chen, Y.J.; Fu, T.C.; Su, H.R. Noninvasive Prediction of Blood Lactate through a Machine Learning-Based Approach. Sci. Rep. 2019, 9, 2180. [Google Scholar] [CrossRef]
- Beneke, R.; Leithäuser, R.M.; Ochentel, O. Blood Lactate Diagnostics in Exercise Testing and Training. Int. J. Sports Physiol. Perform. 2011, 6, 8–24. [Google Scholar] [CrossRef]
- Campbell, I. Intermediary Metabolism. Anaesth. Intensive Care Med. 2017, 18, 147–149. [Google Scholar] [CrossRef]
- Dennison, K.J.; Mullineaux, D.R.; Yates, J.W.; Abel, M.G. The Effect of Fatigue and Training Status on Firefighter Performance. J. Strength Cond. Res. 2012, 26, 1101–1109. [Google Scholar] [CrossRef]
- Fasching, P.; Rinnerhofer, S.; Wultsch, G.; Birnbaumer, P.; Hofmann, P. The First Lactate Threshold Is a Limit for Heavy Occupational Work. J. Funct. Morphol. Kinesiol. 2020, 5, 66. [Google Scholar] [CrossRef] [PubMed]
- Fasching, P.; Rinnerhofer, S.; Wultsch, G.; Tschakert, G.; Hofmann, P.; von Duvillard, S. First Lactate Turn Point: A Limiting Factor for Heavy Occupational Work. Med. Sci. Sports Exerc. 2014, 46, 707. [Google Scholar] [CrossRef]
- Foxdal, P.; Sjödin, A.; Östman, B.; Sjödin, B. The Effect of Different Blood Sampling Sites and Analyses on the Relationship~ between Exercise Intensity and 4.0 Mmol ·1- Blood Lactate Concentration. Eur. J. Appl. Physiol. Occup. Physiol. 1991, 63, 52–54. [Google Scholar] [CrossRef]
- USFA. Summary Incident Report. Available online: https://apps.usfa.fema.gov/firefighter-.fatalities/reportBuilder/data?deathDt=01%2F06%2F2021 (accessed on 17 March 2024).
- National Joint Council for Local Authority Fire and Rescue Services. Firefighter Fitness: Best Practice Guide. 2016. Available online: https://www.fbu.org.uk/circulars/2016hoc0147mw/firefighter-fitness-best-practice-guide (accessed on 17 March 2024).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).