Formulation, Characterization, and In Vitro Drug Release Study of β-Cyclodextrin-Based Smart Hydrogels
Abstract
:1. Introduction
2. Results and Discussion
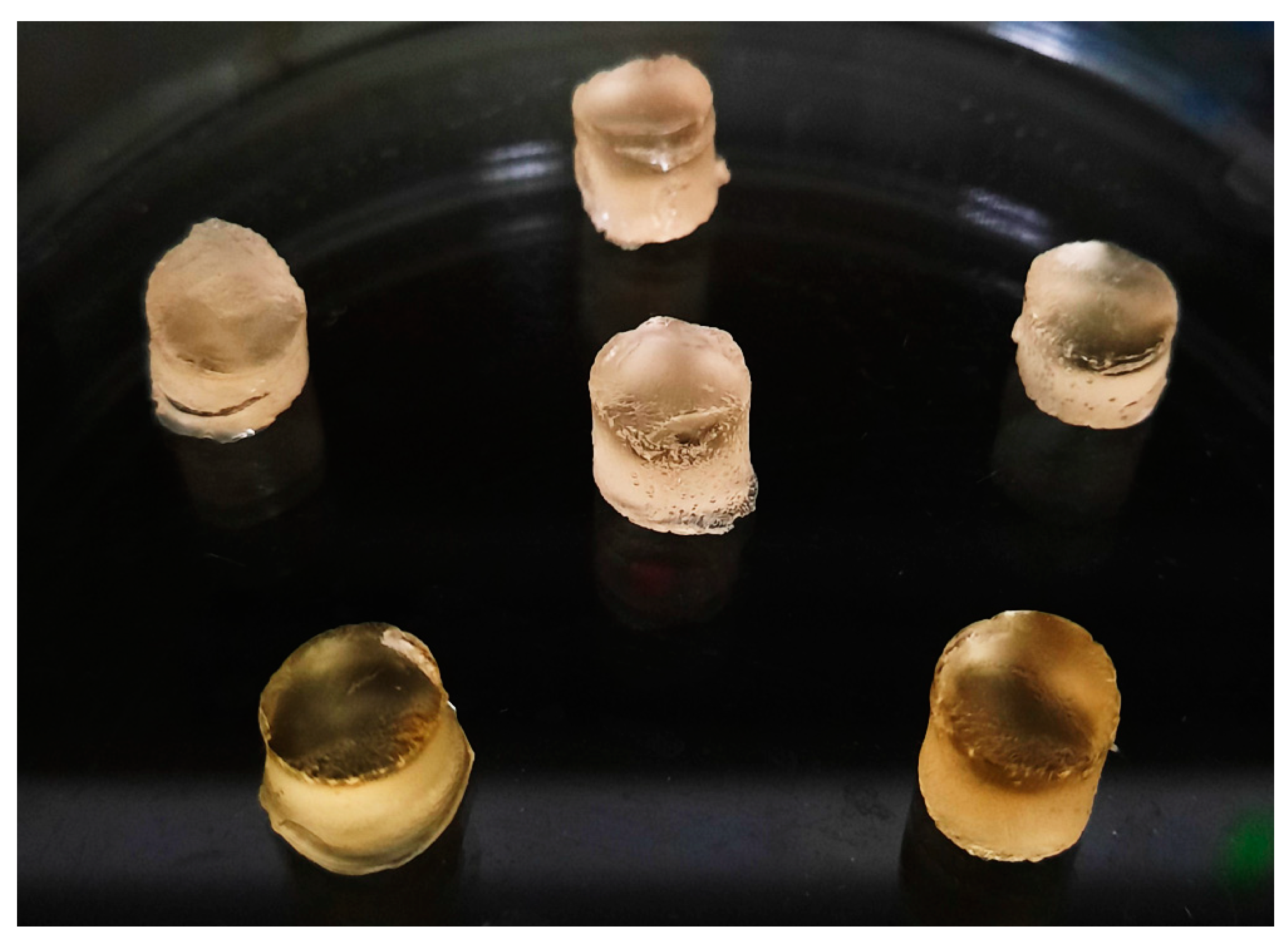
2.1. Synthesis of β-CD-g-P(Aa/Ia) Hydrogels
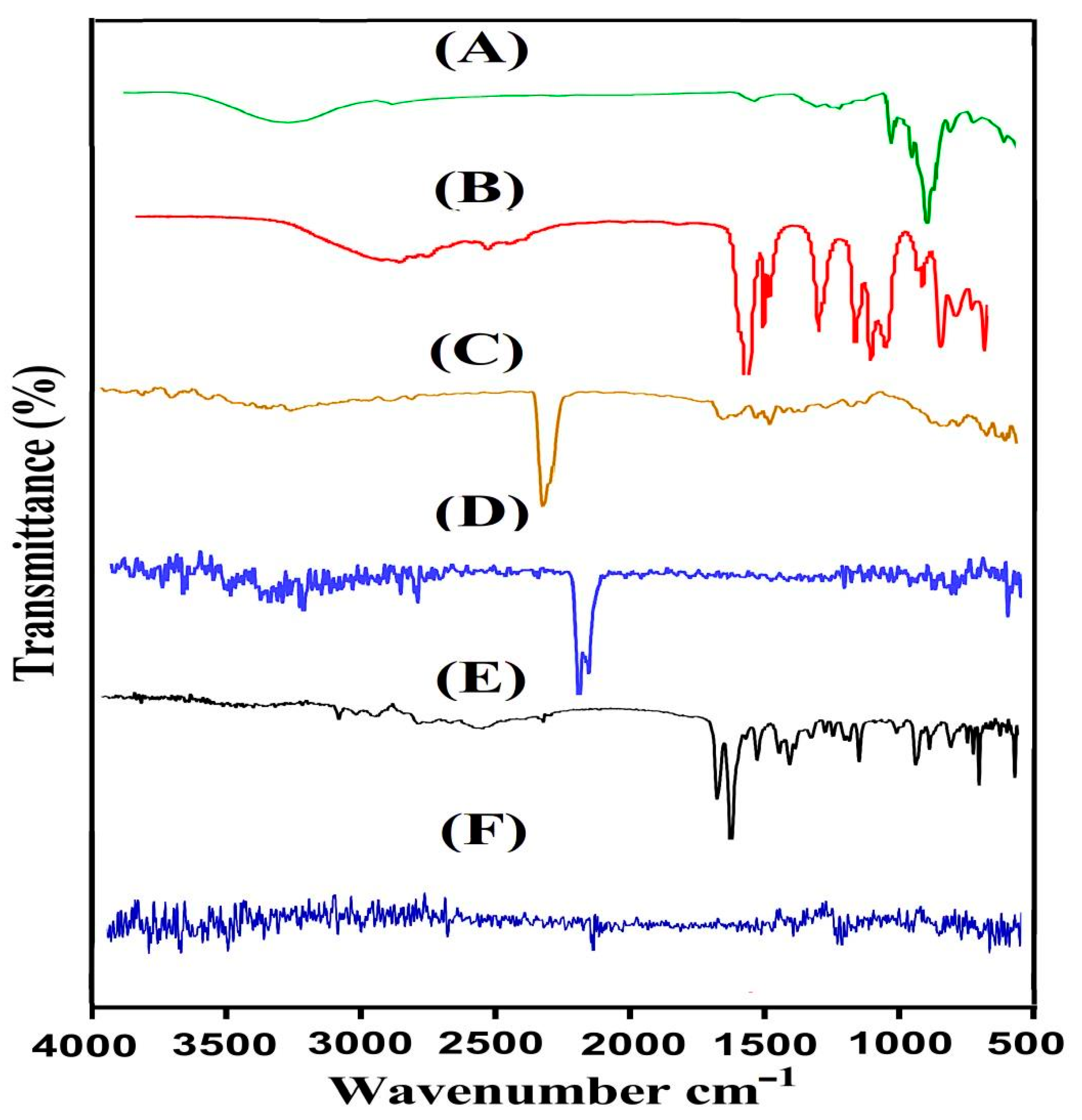
2.2. Fourier Transform Infrared Spectroscopy (FTIR)
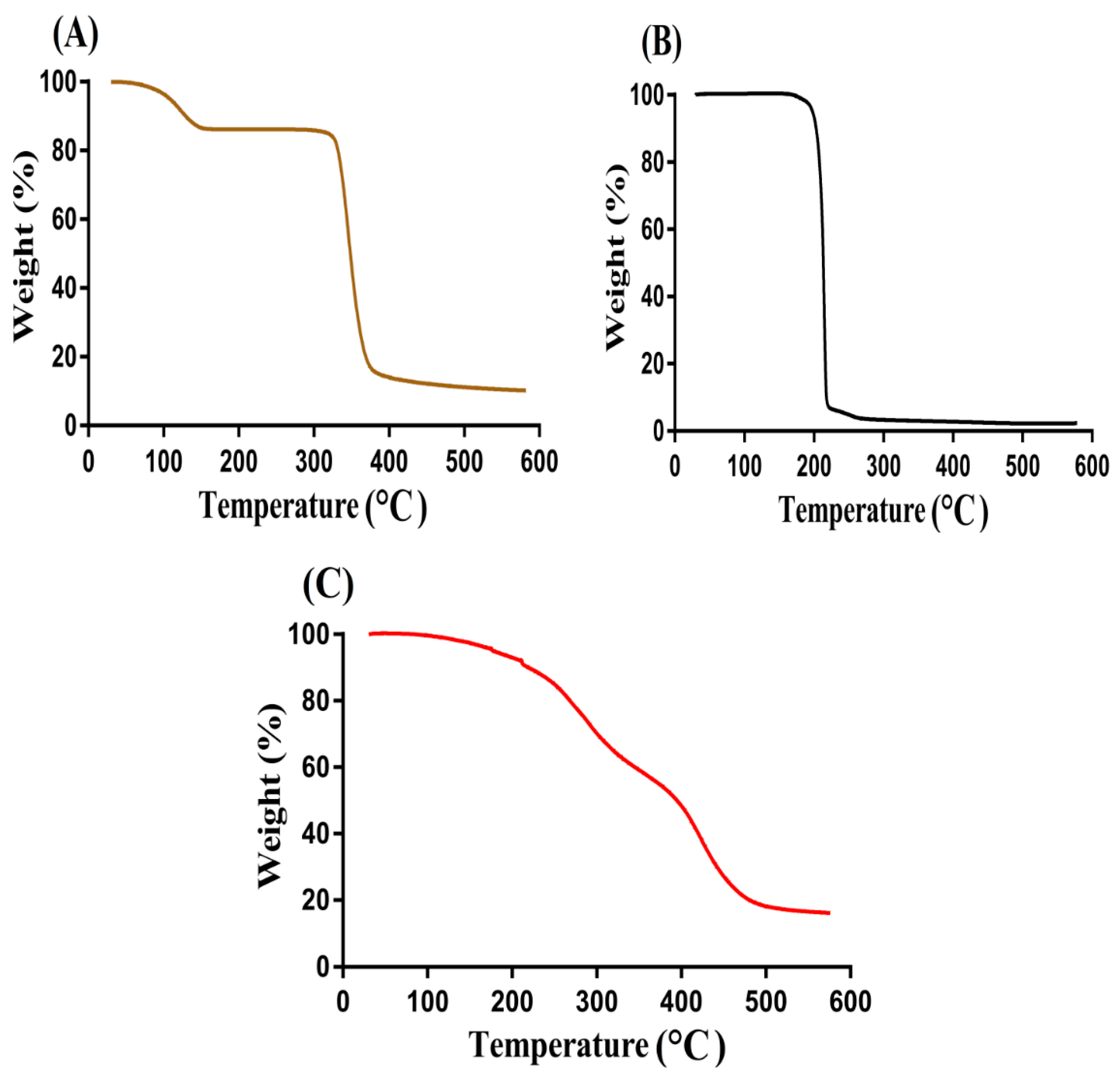
2.3. Thermogravimetric Analysis (TGA)
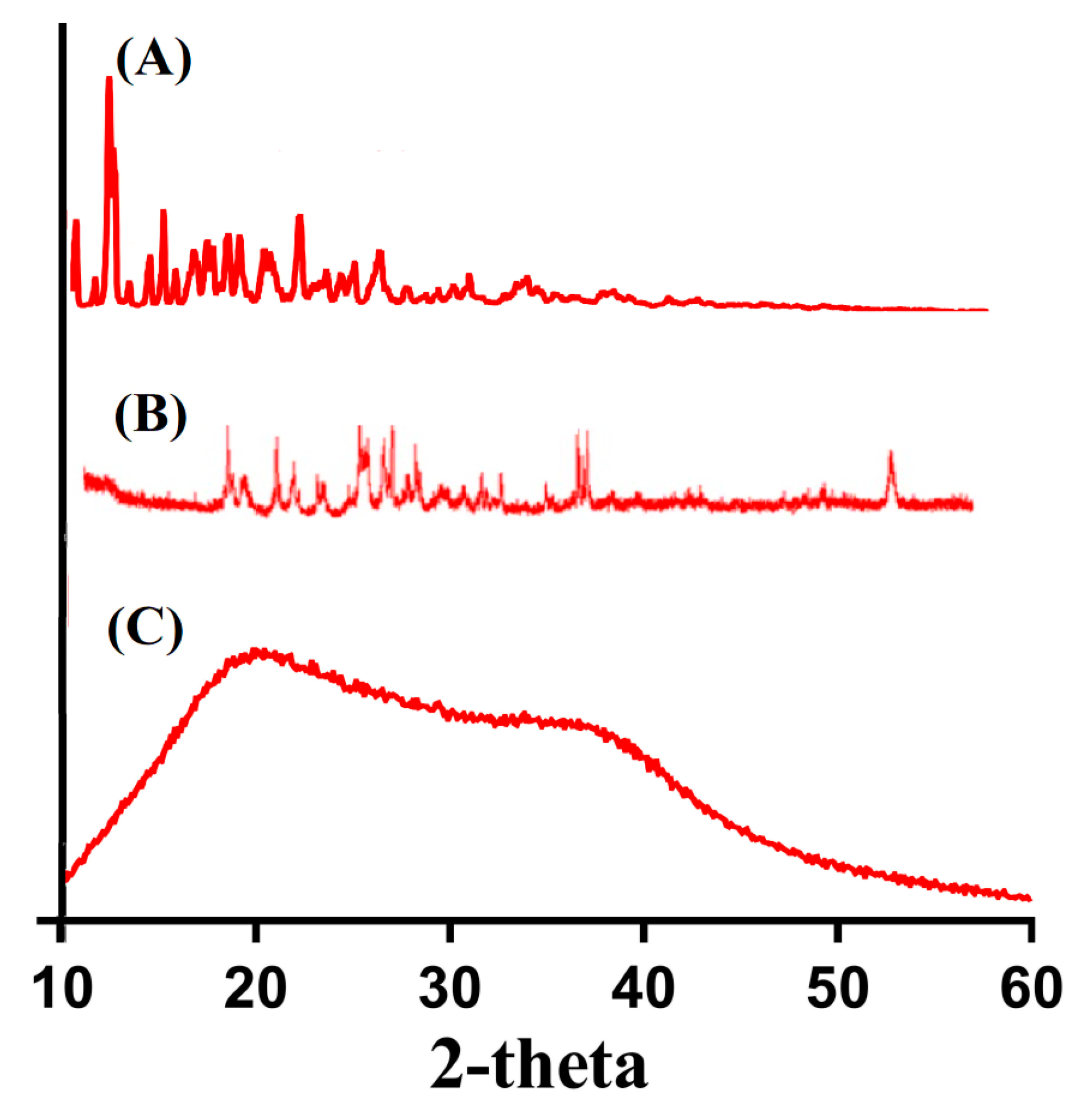
2.4. X-ray Diffraction Studies (XRD)
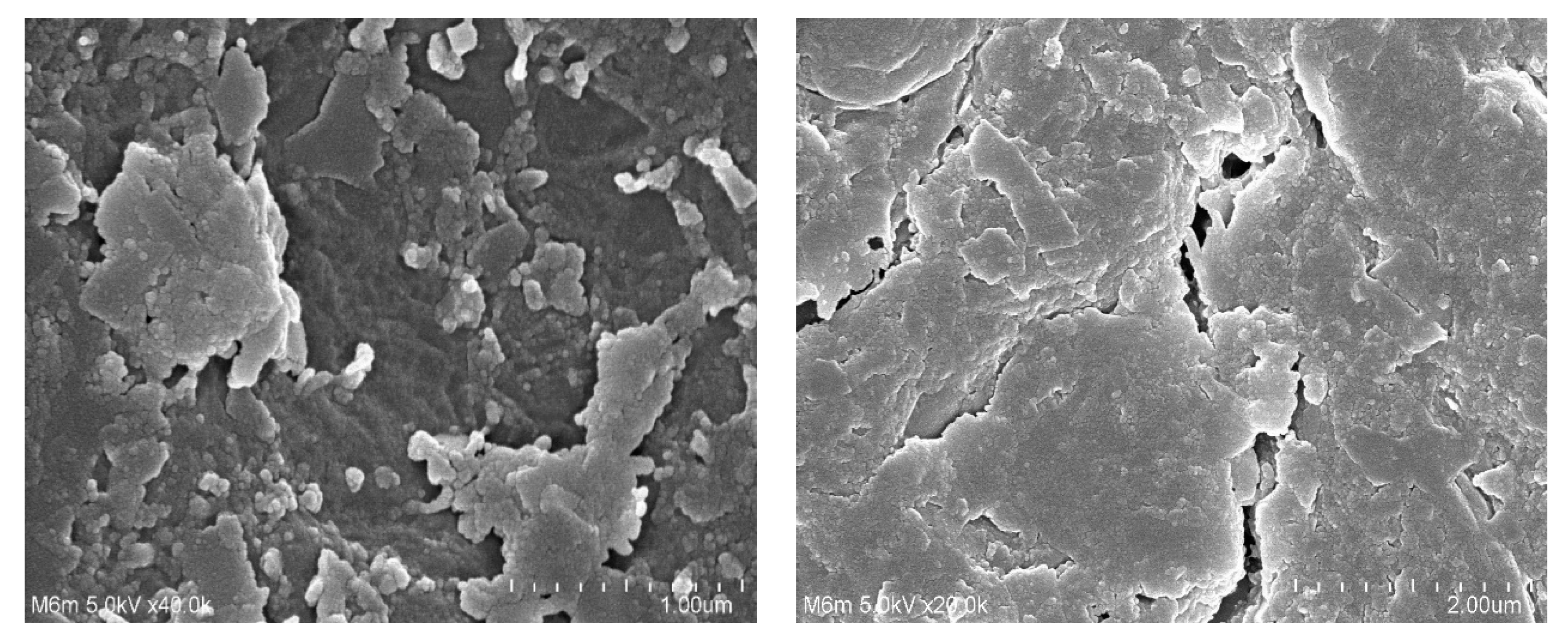
2.5. Scanning Electron Microscopy (SEM)
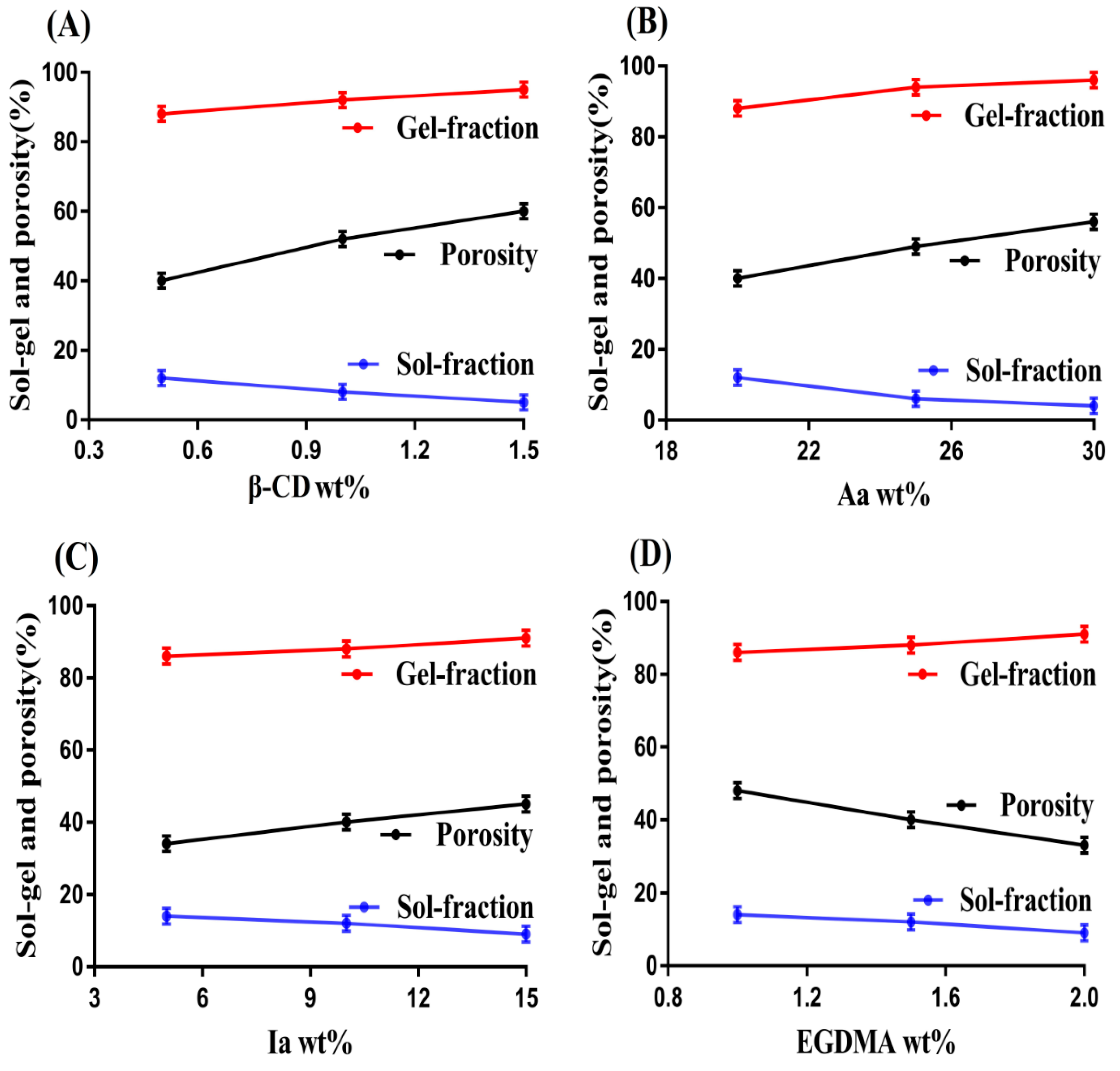
2.6. Sol–Gel Fractions
2.7. Porosity Study
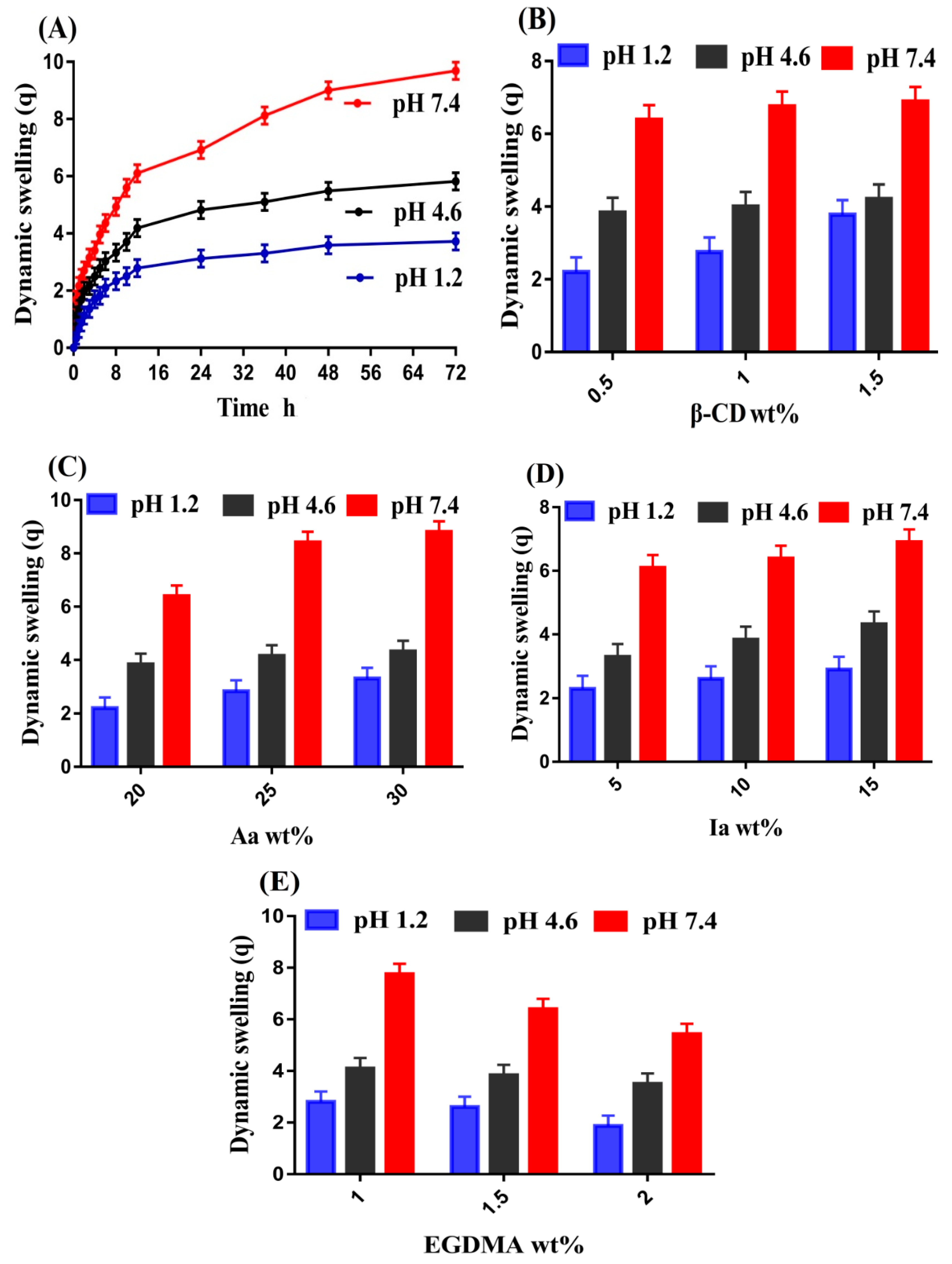
2.8. Swelling Study
2.9. Polymer Volume Fraction
2.10. Drug Loading
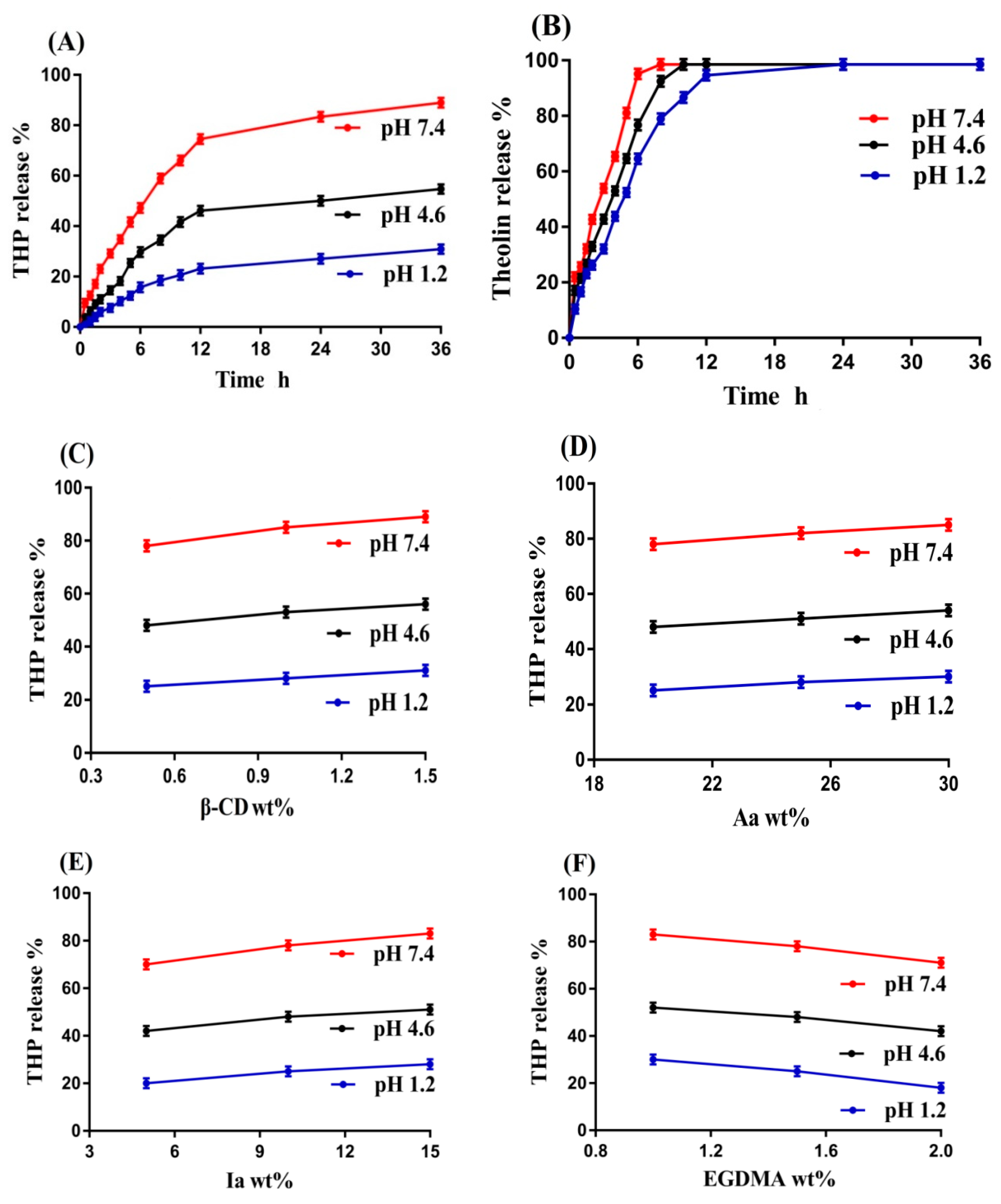
2.11. Drug Release Studies
2.12. Kinetic Modeling
3. Conclusions
4. Materials and Methods
4.1. Materials
4.2. Synthesis of β-CD-g-P(Aa/Ia) Hydrogels
4.3. Fourier Transform Infrared Spectroscopy (FTIR)
4.4. Thermogravimetric Analysis (TGA)
4.5. X-ray Diffraction Studies (XRD)
4.6. Scanning Electron Microscopy (SEM)
4.7. Sol–Gel Fractions
4.8. Porosity Study
4.9. Swelling Study
4.10. Polymer Volume Fraction
4.11. Drug Loading
4.12. Drug Release Studies
4.13. Kinetic Modeling
4.14. Statistical Analysis
Author Contributions
Funding
Conflicts of Interest
References
- Ogilvie, R.I. Clinical pharmacokinetics of theophylline. Clin. Pharm. 1978, 3, 267–293. [Google Scholar] [CrossRef] [PubMed]
- Barnes, P.J. Theophylline: New perspectives for an old drug. Am. J. Respir. Crit. Care Med. 2003, 167, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Ram, F.S.; Jardin, J.R.; Atallah, A.; Castro, A.A.; Mazzini, R.; Goldstein, R.; Lacasse, Y.; Cendon, S. Efficacy of theophylline in people with stable chronic obstructive pulmonary disease: A systematic review and meta-analysis. Respir. Med. 2005, 99, 135–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mellstrand, T.; Svedmyr, N.; Fagerstrom, P.O. Absorption of theophylline from conventional and sustained-release tablets. Eur. J. Respir. Dis. Suppl. 1980, 109, 54–60. [Google Scholar] [PubMed]
- Kumar Singh Yadav, H.; Shivakumar, H.G. In Vitro and In Vivo Evaluation of pH-Sensitive Hydrogels of Carboxymethyl Chitosan for Intestinal Delivery of Theophylline. ISRN Pharm. 2012, 2012, 763127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, W.F.; Chen, X.G.; Li, P.W.; He, Q.Z.; Zhou, H.Y. Preparation and characterization of theophylline loaded chitosan/β-cyclodextrin microspheres. J. Mater. Sci. Mater. Med. 2008, 19, 305–310. [Google Scholar] [CrossRef]
- Ahirrao, S.; Gide, P.; Shrivastav, B.; Sharma, P. Extended release of theophylline through sodium alginate hydrogel beads: Effect of glycerol on entrapment efficiency, drug release. Part. Sci. Technol. 2014, 32, 105–111. [Google Scholar] [CrossRef]
- Chai, Q.; Jiao, Y.; Yu, X. Hydrogels for biomedical applications: Their characteristics and the mechanisms behind them. Gels 2017, 3, 6. [Google Scholar] [CrossRef] [Green Version]
- Suhail, M.; Rosenholm, J.M.; Minhas, M.U.; Badshah, S.F.; Naeem, A.; Khan, K.U.; Fahad, M. Nanogels as drug-delivery systems: A comprehensive overview. Ther. Deliv. 2019, 10, 697–717. [Google Scholar] [CrossRef]
- Emam, H.E.; Shaheen, T.I. Design of a dual pH and temperature responsive hydrogel based on esterified cellulose nanocrystals for potential drug release. Carbohydr. Polym. 2022, 278, 118925. [Google Scholar] [CrossRef]
- Emam, H.E.; Mohamed, A.L. Controllable Release of Povidone-Iodine from Networked Pectin@ Carboxymethyl Pullulan Hydrogel. Polymers 2021, 13, 3118. [Google Scholar] [CrossRef] [PubMed]
- Mamidi, N.; Delgadillo, R.M.V. Design, fabrication and drug release potential of dual stimuli-responsive composite hydrogel nanoparticle interfaces. Coll. Surf. B Biointerfaces 2021, 204, 111819. [Google Scholar] [CrossRef] [PubMed]
- Sarfraz, R.M.; Ahmad, M.; Mahmood, A.; Akram, M.R.; Abrar, A. Development of β-cyclodextrin-based hydrogel microparticles for solubility enhancement of rosuvastatin: An in vitro and in vivo evaluation. Drug Des. Dev. Ther. 2017, 11, 3083. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, L.; Ahmad, M.; Aamir, M.N.; Minhas, M.U.; Shah, H.H.; Shah, M.A. Cross-linked pH-sensitive pectin and acrylic acid based hydrogels for controlled delivery of metformin. Pak. J. Pharm. Sci. 2020, 33, 4. [Google Scholar]
- Kirimura, K.; Sato, T.; Nakanishi, N.; Terada, M.; Usami, S. Breeding of starch-utilizing and itaconic-acid-producing koji molds by interspecific protoplast fusion between Aspergillus terreus and Aspergillus usamii. Appl. Microbiol. Biotechnol. 1997, 47, 127–131. [Google Scholar] [CrossRef]
- Sen, M.; Yakar, A. Controlled release of antifungal drug terbinafine hydrochloride from poly(N-vinyl 2-pyrrolidone/itaconic acid) hydrogels. Int. J. Pharm. 2001, 228, 33–41. [Google Scholar] [CrossRef]
- Tasdelen, B.; Kayaman-Apohan, N.; Guven, O.; Baysal, B.M. Preparation of poly (N-isopropylacrylamide/itaconic acid) copolymeric hydrogels and their drug release behavior. Int. J. Pharm. 2004, 278, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Peppas, N.; Torres-Lugo, M.; Pacheco-Gomez, J.; Foss, A.; Huang, Y.; Ichikawa, H.; Leobandung, W. Intelligent hydrogels and their biotechnological and separation applications. In Radiation Synthesis of Intelligent Hydrogels and Membranes for Separation Purposes; IAEA: Vienna, Austria, 2000; pp. 1–14. [Google Scholar]
- Khan, M.Z.; Makreski, P.; Murtaza, G. Preparation, optimization, in vitro evaluation and ex vivo permeation studies of finasteride loaded gel formulations prepared by using response surface methodology. Curr. Drug Deliv. 2018, 15, 1312–1322. [Google Scholar] [CrossRef]
- Gatiganti, D.L.; Srimathkandala, M.H.; Ananthula, M.B.; Bakshi, V. Formulation and evaluation of oral natural polysaccharide hydrogel microbeads of Irbesartan. Anal. Chem. Lett. 2016, 6, 334–344. [Google Scholar] [CrossRef]
- Ge, H.C.; Hua, T.T.; Wang, J.C. Preparation and characterization of poly (itaconic acid)-grafted crosslinked chitosan nanoadsorbent for high uptake of Hg2+ and Pb2+. Int. J. Biol. Macromol. 2017, 95, 954–961. [Google Scholar] [CrossRef]
- Betancourt, T.; Pardo, J.; Soo, K.; Peppas, N.A. Characterization of pH-responsive hydrogels of poly(itaconic acid-g-ethylene glycol) prepared by UV-initiated free radical polymerization as biomaterials for oral delivery of bioactive agents. J. Biomed. Mater. Res. A 2010, 93, 175–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khalid, I.; Ahmad, M.; Usman Minhas, M.; Barkat, K. Synthesis and evaluation of chondroitin sulfate based hydrogels of loxoprofen with adjustable properties as controlled release carriers. Carbohydr. Polym. 2018, 181, 1169–1179. [Google Scholar] [CrossRef] [PubMed]
- Minhas, M.U.; Ahmad, M.; Khan, S.; Ali, L.; Sohail, M. Synthesis and characterization of β-cyclodextrin hydrogels: Crosslinked polymeric network for targeted delivery of 5-fluorouracil. Drug Deliv. 2016, 9, 10. [Google Scholar]
- Coskun, R.; Soykan, C.; Delibas, A. Study of free-radical copolymerization of itaconic acid/2-acrylamido-2-methyl-1-propanesulfonic acid and their metal chelates. Eur. Polym. J. 2006, 42, 625–637. [Google Scholar] [CrossRef]
- Wei, W.; Hu, X.; Qi, X.; Yu, H.; Liu, Y.; Li, J.; Zhang, J.; Dong, W. A novel thermo-responsive hydrogel based on salecan and poly (N-isopropylacrylamide): Synthesis and characterization. Coll. Surf. B Biointerfaces 2015, 125, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Feng, L.; Wei, W.; Xie, A.; Wang, S.; Zhang, J.; Dong, W. Synthesis and characterization of a novel semi-IPN hydrogel based on Salecan and poly (N, N-dimethylacrylamide-co-2-hydroxyethyl methacrylate). Carbohydr. Polym. 2014, 105, 135–144. [Google Scholar] [CrossRef]
- Ray, M.; Pal, K.; Anis, A.; Banthia, A. Development and characterization of chitosan-based polymeric hydrogel membranes. Des. Monomers Polym. 2010, 13, 193–206. [Google Scholar] [CrossRef] [Green Version]
- Nasir, N.; Ahmad, M.; Minhas, M.U.; Barkat, K.; Khalid, M.F. pH-responsive smart gels of block copolymer [pluronic F127-co-poly (acrylic acid)] for controlled delivery of Ivabradine hydrochloride: Its toxicological evaluation. J. Polym. Res. 2019, 26, 1–15. [Google Scholar] [CrossRef]
- Hu, X.; Wang, Y.; Zhang, L.; Xu, M.; Dong, W.; Zhang, J. Redox/pH dual stimuli-responsive degradable Salecan-g-SS-poly (IA-co-HEMA) hydrogel for release of doxorubicin. Carbohydr. Polym. 2017, 155, 242–251. [Google Scholar] [CrossRef]
- Abdullah, O.; Usman Minhas, M.; Ahmad, M.; Ahmad, S.; Barkat, K.; Ahmad, A. Synthesis, optimization, and evaluation of polyvinyl alcohol-based hydrogels as controlled combinatorial drug delivery system for colon cancer. Adv. Polym. Technol. 2018, 37, 3348–3363. [Google Scholar] [CrossRef]
- Sinha, P.; Ubaidulla, U.; Nayak, A.K. Okra (Hibiscus esculentus) gum-alginate blend mucoadhesive beads for controlled glibenclamide release. Int. J. Biol. Macromol. 2015, 72, 1069–1075. [Google Scholar] [CrossRef] [PubMed]
- Khanum, H.; Ullah, K.; Murtaza, G.; Khan, S.A. Fabrication and in vitro characterization of HPMC-g-poly (AMPS) hydrogels loaded with loxoprofen sodium. Int. J. Biol. Macromol. 2018, 120, 1624–1631. [Google Scholar] [CrossRef] [PubMed]
- Abbadessa, A.; Blokzijl, M.; Mouser, V.; Marica, P.; Malda, J.; Hennink, W.; Vermonden, T. A thermo-responsive and photo-polymerizable chondroitin sulfate-based hydrogel for 3D printing applications. Carbohydr. Polym. 2016, 149, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Sarika, P.R.; James, N.R.; Kumar, P.R.A.; Raj, D.K. Preparation, characterization and biological evaluation of curcumin loaded alginate aldehyde-gelatin nanogels. Mat. Sci. Eng. C Mater. 2016, 68, 251–257. [Google Scholar] [CrossRef]
- Hussain, A.; Khalid, S.H.; Qadir, M.I.; Massud, A.; Ali, M.; Khan, I.U.; Saleem, M.; Iqbal, M.S.; Asghar, S.; Gul, H. Water uptake and drug release behaviour of methyl methacrylate-co-itaconic acid [P(MMA/IA)] hydrogels cross-linked with methylene bis-acrylamide. J. Drug Deliv. Sci. Technol. 2011, 21, 249–255. [Google Scholar] [CrossRef]
- Bukhari, S.M.H.; Khan, S.; Rehanullah, M.; Ranjha, N.M. Synthesis and characterization of chemically cross-linked acrylic acid/gelatin hydrogels: Effect of pH and composition on swelling and drug release. Int. J. Polym. Sci. 2015, 2015, 187961. [Google Scholar] [CrossRef]
- Lim, S.L.; Tang, W.N.H.; Ooi, C.W.; Chan, E.S.; Tey, B.T. Rapid swelling and deswelling of semi-interpenetrating network poly (acrylic acid)/poly (aspartic acid) hydrogels prepared by freezing polymerization. J. Appl. Polym. Sci. 2016, 133, 1–9. [Google Scholar] [CrossRef]
- Khan, S.A.; Azam, W.; Ashames, A.; Fahelelbom, K.M.; Ullah, K.; Mannan, A.; Murtaza, G. β-Cyclodextrin-based (IA-co-AMPS) Semi-IPNs as smart biomaterials for oral delivery of hydrophilic drugs: Synthesis, characterization, in-Vitro and in-Vivo evaluation. J. Drug Deliv. Sci. Technol. 2020, 60, 101970. [Google Scholar] [CrossRef]
- Al-Tabakha, M.M.; Khan, S.A.; Ashames, A.; Ullah, H.; Ullah, K.; Murtaza, G.; Hassan, N. Synthesis, Characterization and Safety Evaluation of Sericin-Based Hydrogels for Controlled Delivery of Acyclovir. Pharmaceuticals 2021, 14, 234. [Google Scholar] [CrossRef]
- Sullad, A.G.; Manjeshwar, L.S.; Aminabhavi, T.M. Novel pH-Sensitive Hydrogels Prepared from the Blends of Poly(vinyl alcohol) with Acrylic Acid-graft-Guar Gum Matrixes for Isoniazid Delivery. Ind Eng. Chem Res. 2010, 49, 7323–7329. [Google Scholar] [CrossRef]
- Khalid, S.; Qadir, M.; Massud, A.; Ali, M.; Rasool, M. Effect of degree of cross-linking on swelling and drug release behaviour of poly (methyl methacrylate-co-itaconic acid)[P (MMA/IA)] hydrogels for site specific drug delivery. J. Drug Deliv. Sci. Technol. 2009, 19, 413–418. [Google Scholar] [CrossRef]
- Caykara, T.; Turan, E. Effect of the amount and type of the crosslinker on the swelling behavior of temperature-sensitive poly(N-tert-butylacrylamide-co-acrylamide) hydrogels. Colloid Polym. Sci. 2006, 284, 1038–1048. [Google Scholar] [CrossRef]
- Teijon, C.; Olmo, R.; Blanco, M.D.; Teijon, J.M.; Romero, A. Effect of the crosslinking degree and the nickel salt load on the thermal decomposition of poly (2-hydroxyethyl methacrylate) hydrogels and on the metal release from them. J. Colloid Interface Sci. 2006, 295, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Teijon, J.M.; Trigo, R.M.; Garcia, O.; Blanco, M.D. Cytarabine trapping in poly(2-hydroxyethyl methacrylate) hydrogels: Drug delivery studies. Biomaterials 1997, 18, 383–388. [Google Scholar] [CrossRef]
- Vazquez, B.; Gurruchaga, M.; Goni, I. Hydrogels Based on Graft-Copolymerization of Hema Bma Mixtures onto Soluble Gelatin-Swelling Behavior. Polymer 1995, 36, 2311–2314. [Google Scholar] [CrossRef]
- Badshah, S.F.; Akhtar, N.; Minhas, M.U.; Khan, K.U.; Khan, S.; Abdullah, O.; Naeem, A. Porous and highly responsive cross-linked β-cyclodextrin based nanomatrices for improvement in drug dissolution and absorption. Life Sci. 2021, 267, 118931. [Google Scholar] [CrossRef]
- Majeed, A.; Pervaiz, F.; Shoukat, H.; Shabbir, K.; Noreen, S.; Anwar, M. Fabrication and evaluation of pH sensitive chemically cross-linked interpenetrating network [Gelatin/Polyvinylpyrrolidone-co-poly(acrylic acid)] for targeted release of 5-fluorouracil. Polym. Bull. 2022, 79, 1–20. [Google Scholar] [CrossRef]
- Murthy, P.S.K.; Mohan, Y.M.; Sreeramulu, J.; Raju, K.M. Semi-IPNs of starch and poly(acrylamide-co-sodium methacrylate): Preparation, swelling and diffusion characteristics evaluation. React. Funct. Polym. 2006, 66, 1482–1493. [Google Scholar] [CrossRef]
- Sohail, K.; Khan, I.U.; Shahzad, Y.; Hussain, T.; Ranjha, N.M. pH-sensitive polyvinylpyrrolidone-acrylic acid hydrogels: Impact of material parameters on swelling and drug release. Braz. J. Pharm. Sci. 2014, 50, 173–184. [Google Scholar] [CrossRef]
- Bera, R.; Dey, A.; Chakrabarty, D. Synthesis, Characterization, and drug release study of acrylamide-co-itaconic acid based smart hydrogel. Polym. Eng. Sci. 2015, 55, 113–122. [Google Scholar] [CrossRef]
- Sanli, O.; Ay, N.; Isiklan, N. Release characteristics of diclofenac sodium from poly(vinyl alcohol)/sodium alginate and poly(vinyl alcohol)-grafted-poly(acrylamide)/sodium alginate blend beads. Eur. J. Pharm. BioPharm. 2007, 65, 204–214. [Google Scholar] [CrossRef] [PubMed]
- Khalid, Q.; Ahmad, M.; Usman Minhas, M. Hydroxypropyl-β-cyclodextrin hybrid nanogels as nano-drug delivery carriers to enhance the solubility of dexibuprofen: Characterization, in vitro release, and acute oral toxicity studies. Adv. Polym. Technol. 2018, 37, 2171–2185. [Google Scholar] [CrossRef]
- Akhtar, M.F.; Ranjha, N.M.; Hanif, M. Effect of ethylene glycol dimethacrylate on swelling and on metformin hydrochloride release behavior of chemically crosslinked pH-sensitive acrylic acid-polyvinyl alcohol hydrogel. Daru 2015, 23, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, F.; Razzak, S.M.I.; Khan, Z.R.; Azad, M.A.K.; Chowdhury, J.A.; Reza, S. Theophylline loaded gastroretentive floating tablets based on hydrophilic polymers: Preparation and in vitro evaluation. Pak. J. Pharm. Sci. 2009, 22, 155–161. [Google Scholar] [PubMed]
- Bashir, S.; Teo, Y.Y.; Ramesh, S.; Ramesh, K. Synthesis, characterization, properties of N-succinyl chitosan-g-poly (methacrylic acid) hydrogels and in vitro release of theophylline. Polymer 2016, 92, 36–49. [Google Scholar] [CrossRef]
- Liu, M.; Wang, X.; Wang, Y.; Jiang, Z. Controlled stimulation-burst targeted release by pH-sensitive HPMCAS/theophylline composite nanofibers fabricated through electrospinning. J. Appl. Polym. Sci. 2020, 137, 48383. [Google Scholar] [CrossRef]
- Shoaib, M.H.; Tazeen, J.; Merchant, M.A.; Yousuf, R.I. Evaluation of drug release kinetics from ibuprofen matrix tablets using HPMC. Pak. J. Pharm. Sci. 2006, 19, 119–124. [Google Scholar]
- Maziad, N.A.; EL-Hamouly, S.; Zied, E.; EL Kelani, T.A.; Nasef, N.R. Radiation preparation of smart hydrogel has antimicrobial properties for controlled release of ciprofloxacin in drug delivery systems. Drug Deliv. 2015, 14, 15. [Google Scholar]
- Sohail, M.; Ahmad, M.; Minhas, M.U.; Ali, L.; Khalid, I.; Rashid, H. Controlled delivery of valsartan by cross-linked polymeric matrices: Synthesis, in vitro and in vivo evaluation. Int. J. Pharm. 2015, 487, 110–119. [Google Scholar] [CrossRef]
- Ullah, K.; Sohail, M.; Buabeid, M.A.; Murtaza, G.; Ullah, A.; Rashid, H.; Khan, M.A.; Khan, S.A. Pectin-based (LA-co-MAA) semi-IPNS as a potential biomaterial for colonic delivery of oxaliplatin. Int. J. Pharm. 2019, 569, 118557. [Google Scholar] [CrossRef]
- Ullah, K.; Sohail, M.; Mannan, A.; Rashid, H.; Shah, A.; Murtaza, G.; Khan, S.A. Facile synthesis of chitosan based-(AMPS-co-AA) semi-IPNs as a potential drug carrier: Enzymatic degradation, cytotoxicity, and preliminary safety evaluation. Curr. Drug Deliv. 2019, 16, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Sarfraz, R.; Khan, H.; Mahmood, A.; Ahmad, M.; Maheen, S.; Sher, M. Formulation and evaluation of mouth disintegrating tablets of atenolol and atorvastatin. Indian J. Pharm. Sci. 2015, 77, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ullah, K.; Khan, S.A.; Murtaza, G.; Sohail, M.; Manan, A.; Afzal, A. Gelatin-based hydrogels as potential biomaterials for colonic delivery of oxaliplatin. Int. J. Pharm. 2019, 556, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Zia, M.A.; Sohail, M.; Minhas, M.U.; Sarfraz, R.M.; Khan, S.; de Matas, M.; Hussain, Z.; Abbasi, M.; Shah, S.A.; Kousar, M. HEMA based pH-sensitive semi IPN microgels for oral delivery; a rationale approach for ketoprofen. Drug Dev. Ind. Pharm. 2020, 46, 272–282. [Google Scholar] [CrossRef] [PubMed]
- Ijaz, H.; Tulain, U.R.; Azam, F.; Qureshi, J. Thiolation of arabinoxylan and its application in the fabrication of pH-sensitive thiolated arabinoxylan grafted acrylic acid copolymer. Drug Dev. Ind. Pharm. 2019, 45, 754–766. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Ranjha, N.M. Effect of degree of cross-linking on swelling and on drug release of low viscous chitosan/poly (vinyl alcohol) hydrogels. Polym. Bull. 2014, 71, 2133–2158. [Google Scholar] [CrossRef]
- Peppas, N.A.; Sahlin, J.J. A simple equation for the description of solute release. III. Coupling of diffusion and relaxation. Int. J. Pharm. 1989, 57, 169–172. [Google Scholar] [CrossRef]
| F. Code | Polymer β-CD g/100 g | Monomer Aa g/100 g | Monomer Ia g/100 g | Initiator APS g/100 g | Crosslinker EGDMA g/100 g |
|---|---|---|---|---|---|
| BAIF-1 | 0.5 | 20 | 10 | 0.5 | 1.5 |
| BAIF-2 | 1.0 | 20 | 10 | 0.5 | 1.5 |
| BAIF-3 | 1.5 | 20 | 10 | 0.5 | 1.5 |
| BAIF-4 | 0.5 | 20 | 10 | 0.5 | 1.5 |
| BAIF-5 | 0.5 | 25 | 10 | 0.5 | 1.5 |
| BAIF-6 | 0.5 | 30 | 10 | 0.5 | 1.5 |
| BAIF-7 | 0.5 | 20 | 05 | 0.5 | 1.5 |
| BAIF-8 | 0.5 | 20 | 10 | 0.5 | 1.5 |
| BAIF-9 | 0.5 | 20 | 15 | 0.5 | 1.5 |
| BAIF-10 | 0.5 | 20 | 10 | 0.5 | 1.0 |
| BAIF-11 | 0.5 | 20 | 10 | 0.5 | 1.5 |
| BAIF-12 | 0.5 | 20 | 10 | 0.5 | 2.0 |
| Formulation Code | Polymer Volume Fraction | Drug Loaded (mg)/500 mg of Dry Gel | |||
|---|---|---|---|---|---|
| pH 1.2 | pH 4.6 | pH 7.4 | Weight Method | Extraction Method | |
| BAIF-1 | 0.454 | 0.260 | 0.156 | 81.8 ± 0.8 | 80 ± 1 |
| BAIF-2 | 0.363 | 0.250 | 0.150 | 104.4 ± 1 | 103.2 ± 1 |
| BAIF-3 | 0.248 | 0.242 | 0.147 | 116.3 ± 1 | 115.6 ± 1 |
| BAIF-4 | 0.454 | 0.260 | 0.156 | 81.8 ± 0.8 | 80 ± 1 |
| BAIF-5 | 0.352 | 0.245 | 0.146 | 110.1 ± 1 | 109.5 ± 1 |
| BAIF-6 | 0.240 | 0.236 | 0.138 | 121.2 ± 1 | 119.7 ± 1 |
| BAIF-7 | 0.470 | 0.270 | 0.163 | 75.4 ± 1 | 73.6 ± 1 |
| BAIF-8 | 0.454 | 0.260 | 0.156 | 81.8 ± 0.8 | 80 ± 1 |
| BAIF-9 | 0.434 | 0.255 | 0.151 | 86.7 ± 0.9 | 85.3 ± 1 |
| BAIF-10 | 0.416 | 0.245 | 0.128 | 88.2 ± 1 | 88 ± 1 |
| BAIF-11 | 0.454 | 0.260 | 0.156 | 81.8 ± 0.8 | 80 ± 1 |
| BAIF-12 | 0.532 | 0.280 | 0.184 | 70.3 ± 1 | 69.1 ± 1 |
| F. Code | Zero Order r2 | First Order r2 | Higuchi r2 | Korsmeyer–Peppas r2 n | |
|---|---|---|---|---|---|
| BAIF-1 | 0.9661 | 0.9283 | 0.9355 | 0.9843 | 0.5316 |
| BAIF-2 | 0.9825 | 0.9894 | 0.9695 | 0.9963 | 0.6073 |
| BAIF-3 | 0.9846 | 0.9952 | 0.9879 | 0.9986 | 0.6930 |
| BAIF-4 | 0.9661 | 0.9283 | 0.9355 | 0.9843 | 0.5316 |
| BAIF-5 | 0.9740 | 0.9795 | 0.9793 | 0.9893 | 0.6437 |
| BAIF-6 | 0.9881 | 0.9649 | 0.9670 | 0.9980 | 0.7120 |
| BAIF-7 | 0.9787 | 0.9081 | 0.9142 | 0.9822 | 0.6560 |
| BAIF-8 | 0.9661 | 0.9283 | 0.9355 | 0.9843 | 0.5316 |
| BAIF-9 | 0.9768 | 0.9763 | 0.9806 | 0.9810 | 0.6245 |
| BAIF-10 | 0.9803 | 0.8426 | 0.9218 | 0.9874 | 0.6173 |
| BAIF-11 | 0.9661 | 0.9283 | 0.9355 | 0.9843 | 0.5316 |
| BAIF-12 | 0.9545 | 0.9141 | 0.9681 | 0.9794 | 0.6989 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suhail, M.; Vu, Q.L.; Wu, P.-C. Formulation, Characterization, and In Vitro Drug Release Study of β-Cyclodextrin-Based Smart Hydrogels. Gels 2022, 8, 207. https://doi.org/10.3390/gels8040207
Suhail M, Vu QL, Wu P-C. Formulation, Characterization, and In Vitro Drug Release Study of β-Cyclodextrin-Based Smart Hydrogels. Gels. 2022; 8(4):207. https://doi.org/10.3390/gels8040207
Chicago/Turabian StyleSuhail, Muhammad, Quoc Lam Vu, and Pao-Chu Wu. 2022. "Formulation, Characterization, and In Vitro Drug Release Study of β-Cyclodextrin-Based Smart Hydrogels" Gels 8, no. 4: 207. https://doi.org/10.3390/gels8040207
APA StyleSuhail, M., Vu, Q. L., & Wu, P.-C. (2022). Formulation, Characterization, and In Vitro Drug Release Study of β-Cyclodextrin-Based Smart Hydrogels. Gels, 8(4), 207. https://doi.org/10.3390/gels8040207







