Blastomycosis-Associated Hospitalizations, United States, 2010–2020
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smith, D.J.; Williams, S.L.; Partners, G.E.M.S.; Benedict, K.M.; Jackson, B.R.; Toda, M. Surveillance for Coccidioidomycosis, Histoplasmosis, and Blastomycosis—United States, 2019. MMWR Surveill. Summ. 2022, 71, 1–14. [Google Scholar] [CrossRef] [PubMed]
- McDonald, R.; Dufort, E.; Jackson, B.R.; Tobin, E.H.; Newman, A.; Benedict, K.; Blog, D. Notes from the Field: Blastomycosis Cases Occurring Outside of Regions with Known Endemicity—New York, 2007-2017. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1077–1078. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.J.; Koo, S.; Woolley, A.E.; Zuckerman, R.A. Blastomycosis in New England: 5 Cases and a Review. Open Forum Infect. Dis. 2023, 10, ofad029. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, I.S.; Wiederhold, N.P.; Hanson, K.E.; Patterson, T.F.; Sigler, L. Blastomyces helicus, a New Dimorphic Fungus Causing Fatal Pulmonary and Systemic Disease in Humans and Animals in Western Canada and the United States. Clin. Infect. Dis. 2018, 68, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Benedict, K.; Gibbons-Burgener, S.; Kocharian, A.; Ireland, M.; Rothfeldt, L.; Christophe, N.; Signs, K.; Jackson, B.R. Blastomycosis Surveillance in 5 States, United States, 1987–2018. Emerg. Infect. Dis. 2021, 27, 999–1006. [Google Scholar] [CrossRef] [PubMed]
- Ireland, M.; Klumb, C.; Smith, K.; Scheftel, J. Blastomycosis in Minnesota, USA, 1999–2018. Emerg. Infect. Dis. J. 2020, 26, 866. [Google Scholar] [CrossRef] [PubMed]
- Seitz, A.E.; Younes, N.; Steiner, C.A.; Prevots, D.R. Incidence and trends of blastomycosis-associated hospitalizations in the United States. PLoS ONE 2014, 9, e105466. [Google Scholar] [CrossRef] [PubMed]
- Carignan, A.; Denis, M.; Abou Chakra, C.N. Mortality associated with Blastomyces dermatitidis infection: A systematic review of the literature and meta-analysis. Med. Mycol. 2019, 58, myz048. [Google Scholar] [CrossRef] [PubMed]
- Pullen, M.F.; Alpern, J.D.; Bahr, N.C. Blastomycosis-Some Progress but Still Much to Learn. J. Fungi 2022, 8, 824. [Google Scholar] [CrossRef] [PubMed]
- AHRQ. Overview of the National (Nationwide) Inpatient Sample (NIS). Available online: https://hcup-us.ahrq.gov/nisoverview.jsp (accessed on 18 May 2023).
- United States Census Bureau. Annual State Resident Population Estimates for 6 Race Groups (5 Race Alone Groups and Two or More Races) by Age, Sex, and Hispanic Origin: April 1, 2010 to July 1, 2019; April 1, 2020; and July 1, 2020 (SC-EST2020-ALLDATA6). Available online: https://www.census.gov/newsroom/press-kits/2020/population-estimates-detailed.html (accessed on 18 May 2023).
- Gillum, B.; Graves, E.; Kozak, L.J. Trends in Hospital Utilization: United States, 1988–1992; Vital Health Stat 13; NCBI: Bethesda, MD, USA, 1996; pp. 1–71.
- Rush, B.; Lother, S.; Paunovic, B.; Mooney, O.; Kumar, A. Outcomes With Severe Blastomycosis and Respiratory Failure in the United States. Clin. Infect. Dis. 2021, 72, 1603–1607. [Google Scholar] [CrossRef] [PubMed]
- O’Dowd, T.R.; Mc Hugh, J.W.; Theel, E.S.; Wengenack, N.L.; O’Horo, J.C.; Enzler, M.J.; Vergidis, P. Diagnostic Methods and Risk Factors for Severe Disease and Mortality in Blastomycosis: A Retrospective Cohort Study. J. Fungi 2021, 7, 888. [Google Scholar] [CrossRef] [PubMed]
- Villacorta Cari, E.; Leedy, N.; Ribes, J.A.; Soria, J.; Myint, T. Risk factors of severe blastomycosis and comparison of diagnosis and outcomes between immunocompetent and immunocompromised patients. Mycoses 2022, 65, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Chapman, S.W.; Dismukes, W.E.; Proia, L.A.; Bradsher, R.W.; Pappas, P.G.; Threlkeld, M.G.; Kauffman, C.A. Clinical Practice Guidelines for the Management of Blastomycosis: 2008 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2008, 46, 1801–1812. [Google Scholar] [CrossRef] [PubMed]
- Bruce Light, R.; Kralt, D.; Embil, J.M.; Trepman, E.; Wiebe, L.; Limerick, B.; Sarsfield, P.; Hammond, G.; MacDonald, K. Seasonal variations in the clinical presentation of pulmonary and extrapulmonary blastomycosis. Med. Mycol. 2008, 46, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Alpern, J.D.; Bahr, N.C.; Vazquez-Benitez, G.; Boulware, D.R.; Sellman, J.S.; Sarosi, G.A. Diagnostic Delay and Antibiotic Overuse in Acute Pulmonary Blastomycosis. Open Forum Infect. Dis. 2016, 3, ofw078. [Google Scholar] [CrossRef] [PubMed]
| Total | Died | Survived | ||
|---|---|---|---|---|
| Characteristic | n = 11,776 | n = 928 | n = 10,848 | p-Value |
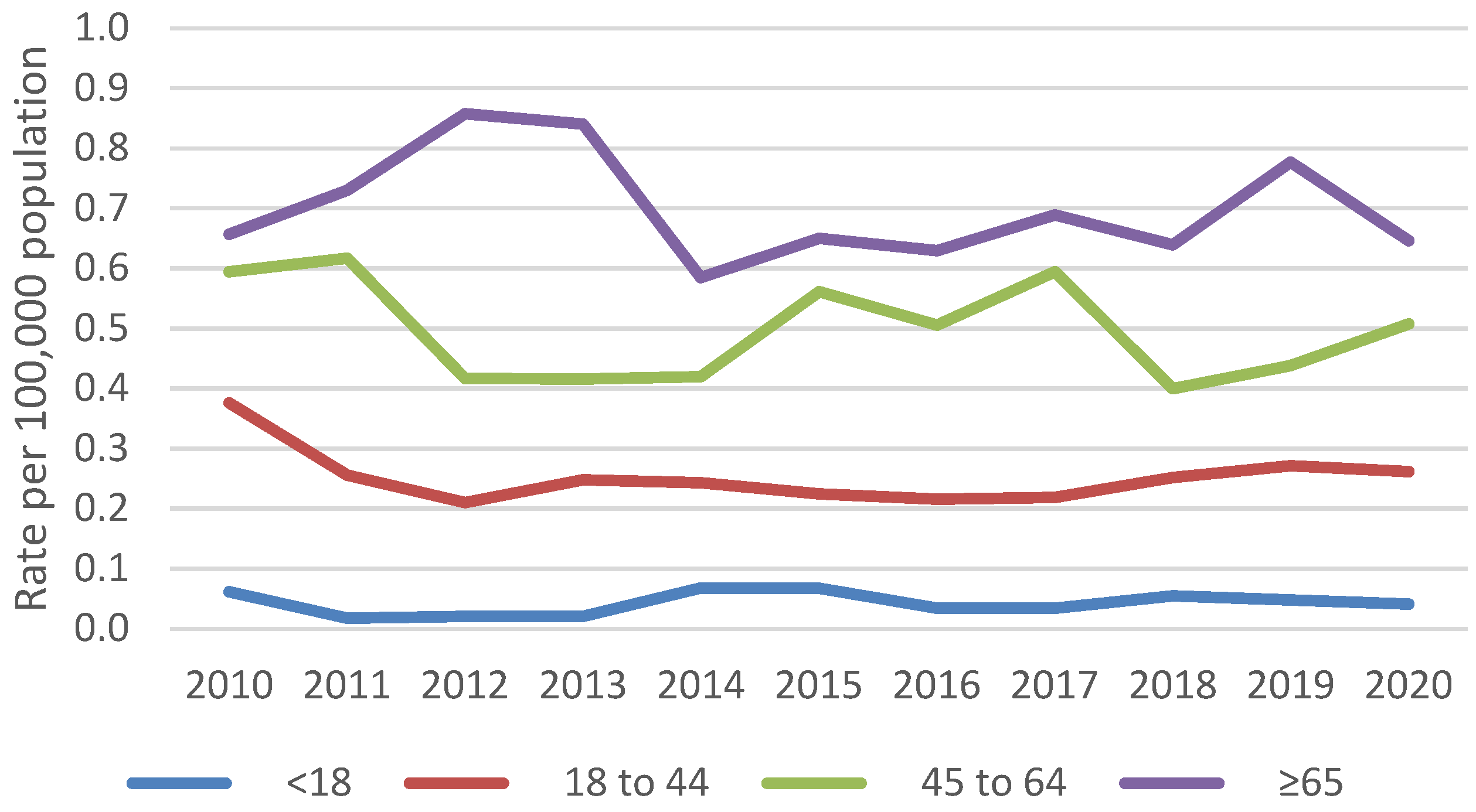
| Mean age, years (standard error [SE]) | 53.6 (0.48) | 61.8 (1.03) | 53.0 (0.51) | <0.001 |
| Age group, years | <0.001 | |||
| <18 | 344 (2.9%) | not shown 1 | not shown 1 | |
| 18 to 44 | 3212 (27.3%) | 94 (10.1%) | 3118 (28.7%) | |
| 45 to 64 | 4552 (38.7%) | 413 (44.5%) | 4139 (38.2%) | |
| ≥65 | 3668 (31.1%) | 416 (44.8%) | 3252 (30.0%) | |
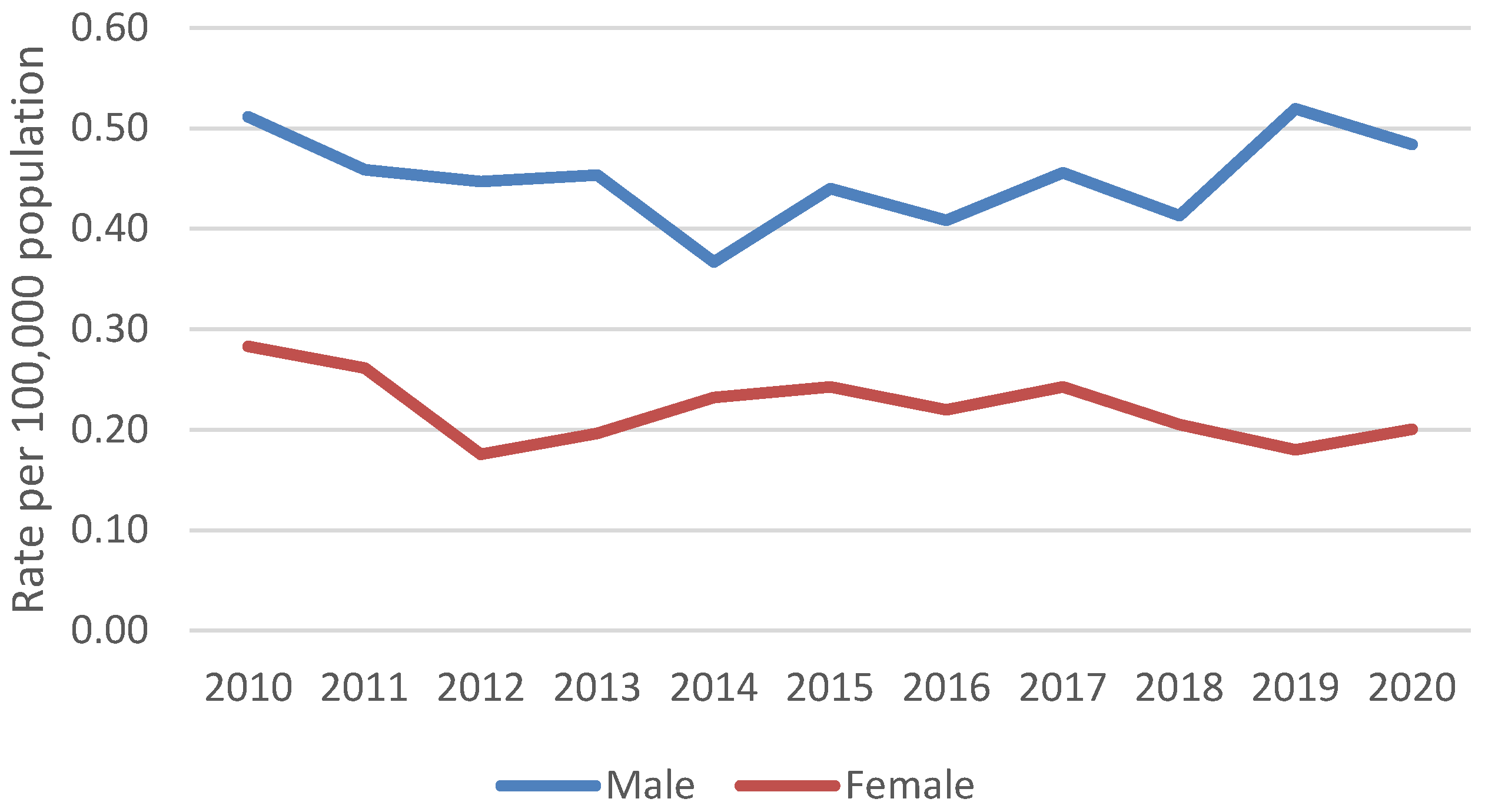
| Sex | 0.567 | |||
| Male | 7218 (61.3%) | 598 (64.4%) | 7218 (66.5%) | |
| Female | 3959 (33.6%) | 330 (35.6%) | 3629 (33.5%) | |
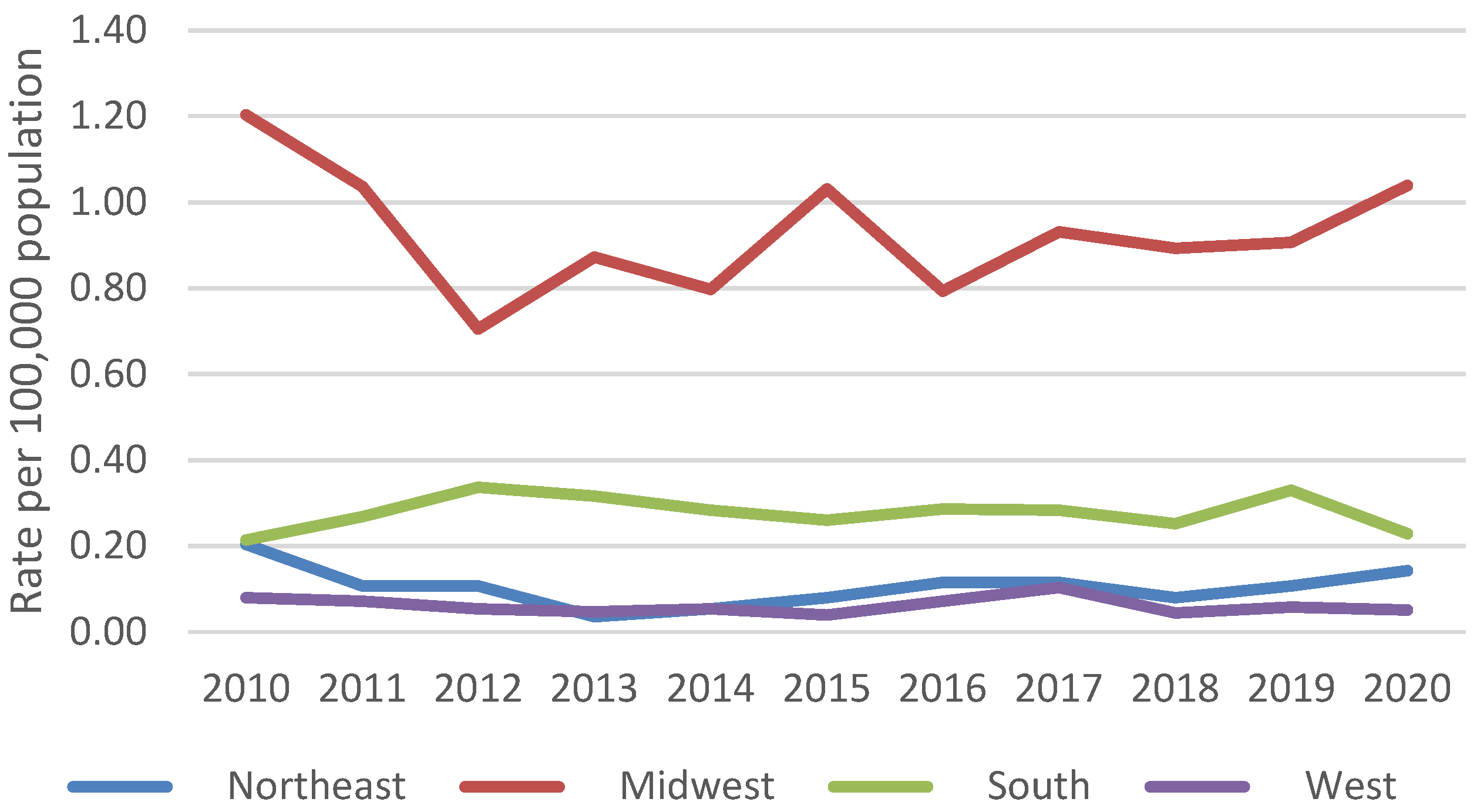
| Hospital region | 0.127 | |||
| Northeast | 643 (5.5%) | 33 (3.6%) | 610 (5.6%) | |
| Midwest | 6921 (58.8%) | 519 (55.9%) | 6401 (59.0%) | |
| South | 3702 (31.4%) | 350 (37.7%) | 3352 (30.9%) | |
| West | 510 (4.3%) | 25 (2.7%) | 485 (4.5%) | |
| Race/ethnicity (n = 10,994) | 0.079 | |||
| White | 7315 (66.5%) | 627 (75.2%) | 6687 (65.8%) | |
| Black | 1859 (16.9%) | 94 (11.3%) | 1765 (17.4%) | |
| Hispanic | 976 (8.9%) | 53 (6.4%) | 923 (9.1%) | |
| Other race/ethnicity | 845 (7.7%) | 60 (7.2%) | 785 (7.7%) | |
| Payer (n = 11,730) | <0.001 | |||
| Medicare | 4941 (42.1%) | 524 (56.8%) | 4417 (40.9%) | |
| Medicaid | 2009 (17.1%) | 99 (10.7%) | 1910 (17.7%) | |
| Private insurance | 4363 (37.2%) | 266 (28.8%) | 4097 (37.9%) | |
| Other payer | 418 (3.6%) | 34 (3.7%) | 384 (3.6%) | |
| Income quartile for patient’s ZIP code (n = 11,562) | 0.575 | |||
| 0 to 25th percentile | 4102 (35.5%) | 337 (37.3%) | 3765 (35.3%) | |
| 26th to 50th percentile | 3430 (29.7%) | 292 (32.3%) | 3138 (29.4%) | |
| 51st to 75th percentile | 2543 (22.0%) | 182 (20.2%) | 2361 (22.2%) | |
| 76th to 100th percentile | 1488 (12.9%) | 93 (10.3%) | 1395 (13.1%) | |
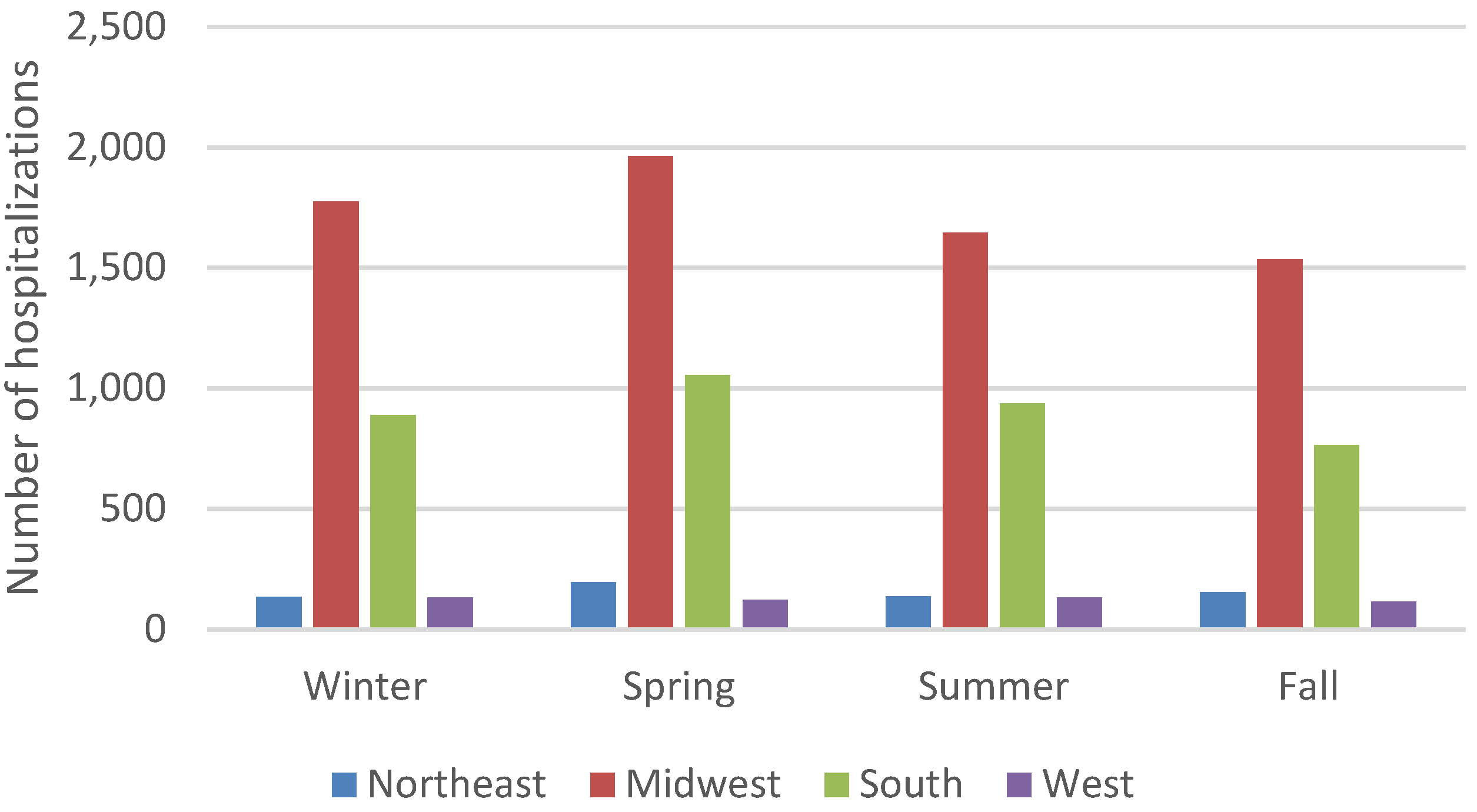
| Admission season | 0.182 | |||
| Winter | 2937 (25.1%) | 261 (28.3%) | 2676 (24.8%) | |
| Spring | 3343 (28.5%) | 223 (24.2%) | 3120 (28.9%) | |
| Summer | 2860 (24.4%) | 195 (21.1%) | 2665 (24.7%) | |
| Fall | 2577 (22.0%) | 244 (26.4%) | 2333 (21.6%) | |
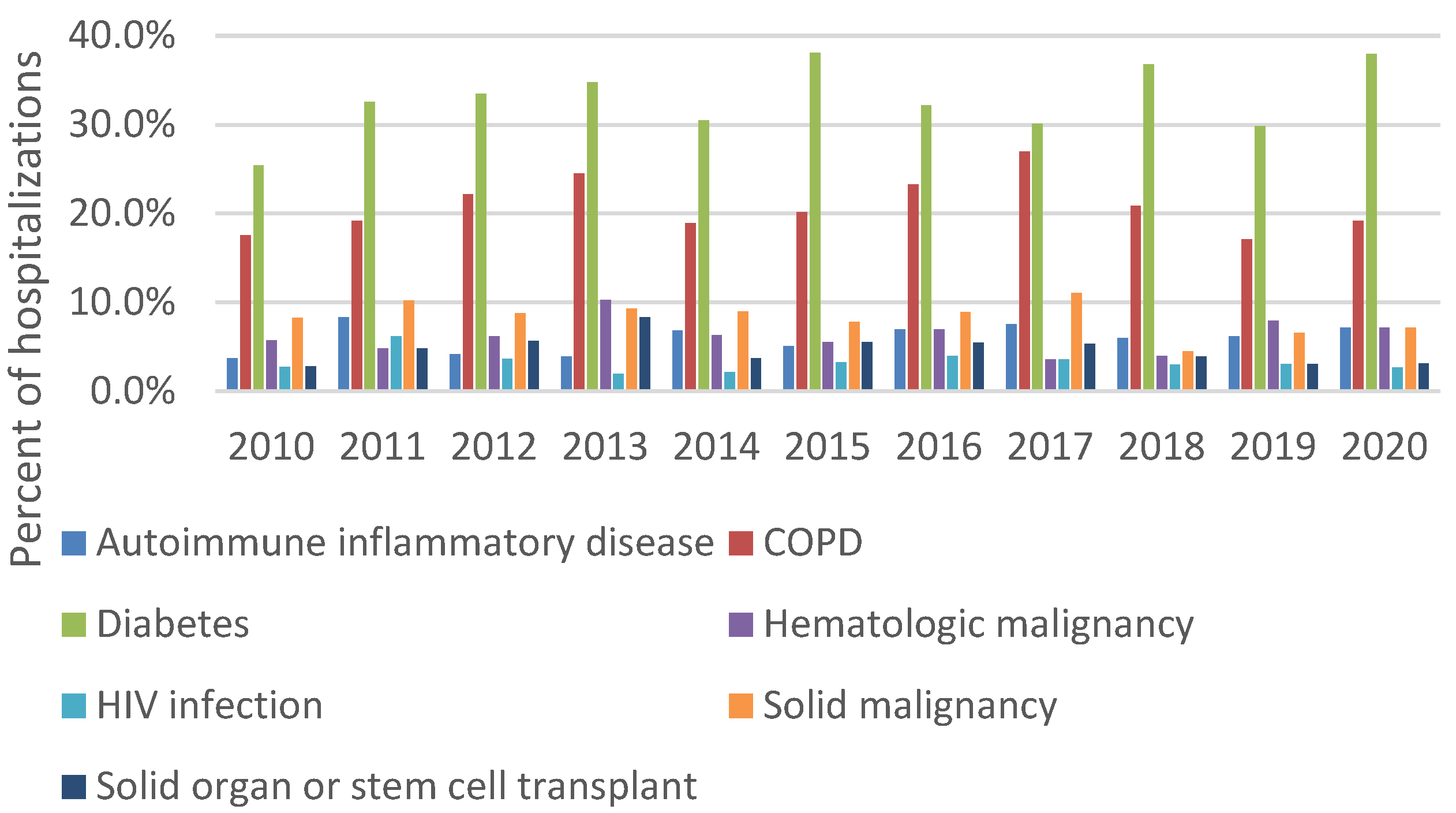
| Concurrent conditions | ||||
| Autoimmune inflammatory disease | 703 (6.0%) | 54 (5.8%) | 648 (6.0%) | 0.954 |
| Chronic obstructive pulmonary disease (COPD) | 2454 (20.8%) | 256 (27.6%) | 2198 (20.3%) | 0.020 |
| Diabetes | 3590 (30.5%) | 298 (32.1%) | 3652 (33.7%) | 0.836 |
| Hematologic malignancy | 729 (6.2%) | 100 (10.8%) | 629 (5.8%) | 0.008 |
| HIV infection | 387 (3.3%) | 39 (4.2%) | 348 (3.2%) | 0.462 |
| Solid malignancy | 989 (8.4%) | 143 (15.4%) | 846 (7.8%) | <0.001 |
| Solid organ or stem cell transplant | 549 (4.7%) | 25 (2.7%) | 524 (4.8%) | 0.178 |
| Mean length of hospitalization, days (SE) | 9.9 (0.25) | 14.0 (0.93) | 9.6 (0.25) | <0.001 |
| Clinical form of blastomycosis 2 | n = 5595 | n = 480 | n = 5115 | |
| Pulmonary | 2970 (53.1%) | 300 (62.5%) | 2670 (52.2%) | 0.055 |
| Cutaneous | 295 (5.3%) | 20 (4.2%) | 275 (5.4%) | 0.613 |
| Disseminated | 870 (15.5%) | 80 (16.7%) | 790 (15.4%) | 0.754 |
| Other or unspecified form | 1730 (30.9%) | 110 (22.9%) | 1620 (31.7%) | 0.076 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benedict, K.; Hennessee, I.; Gold, J.A.W.; Smith, D.J.; Williams, S.; Toda, M. Blastomycosis-Associated Hospitalizations, United States, 2010–2020. J. Fungi 2023, 9, 867. https://doi.org/10.3390/jof9090867
Benedict K, Hennessee I, Gold JAW, Smith DJ, Williams S, Toda M. Blastomycosis-Associated Hospitalizations, United States, 2010–2020. Journal of Fungi. 2023; 9(9):867. https://doi.org/10.3390/jof9090867
Chicago/Turabian StyleBenedict, Kaitlin, Ian Hennessee, Jeremy A. W. Gold, Dallas J. Smith, Samantha Williams, and Mitsuru Toda. 2023. "Blastomycosis-Associated Hospitalizations, United States, 2010–2020" Journal of Fungi 9, no. 9: 867. https://doi.org/10.3390/jof9090867
APA StyleBenedict, K., Hennessee, I., Gold, J. A. W., Smith, D. J., Williams, S., & Toda, M. (2023). Blastomycosis-Associated Hospitalizations, United States, 2010–2020. Journal of Fungi, 9(9), 867. https://doi.org/10.3390/jof9090867






