Synthesis of Altissimacoumarin D and Other Prenylated Coumarins and Their Ability to Reverse the Multidrug Resistance Phenotype in Candida albicans
Abstract
1. Introduction
2. Experimental Section
2.1. General Experiment Procedure
2.2. Synthetic Procedures
2.2.1. 3,5-Dibromo-2,4-dihydroxybenzaldehyde
2.2.2. 2,4-Dihydroxy-3,5-dimethoxybenzaldehyde
2.2.3. 7-Hydroxy-6,8-dimethoxy-2H-chromen-2-one (isofraxidin)
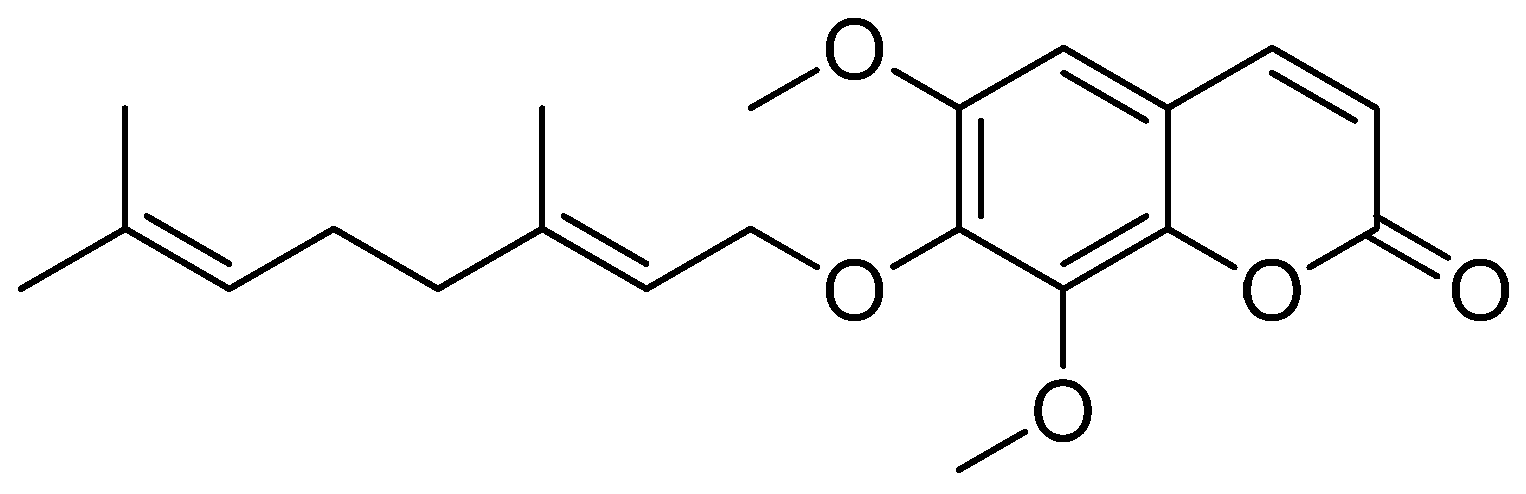
2.2.4. €-7-((3,7-Dimethylocta-2,6-dien-1-yl)oxy)-6,8-dimethoxy-2H-chromen-2-one (ACS51)
2.2.5. 6,8-Dimethoxy-7-((3-methylbut-2-en-1-yl)oxy)-2H-chromen-2-one (ACS50)
2.2.6. (E)-7-((3,7-Dimethylocta-2,6-dien-1-yl)oxy)-2H-chromen-2-one (ACS48)
2.2.7. 7-((3-Methylbut-2-en-1-yl)oxy)-2H-chromen-2-one (ACS47)
2.2.8. (E)-7-((3,7-Dimethylocta-2,6-dien-1-yl)oxy)-4-methyl-2H-chromen-2-one (ACS52)
2.2.9. 4-Methyl-7-((3-methylbut-2-en-1-yl)oxy)-2H-chromen-2-one (ACS54)
2.2.10. (E)-7-((3,7-Dimethylocta-2,6-dien-1-yl)oxy)-3,4,8-trimethyl-2H-chromen-2-one (ACS55)
2.2.11. 3,4,8-Trimethyl-7-((3-methylbut-2-en-1-yl)oxy)-2H-chromen-2-one (ACS56)
2.3. Biological Assays
2.3.1. Strains
2.3.2. Antifungal Activity of Coumarins against C. albicans and S. cerevisiae Strains
2.3.3. Antifungal Activity of Coumarins Combined with Fluconazole against S. cerevisiae Strains
2.3.4. Synergism Evaluation through Checkerboard Assay
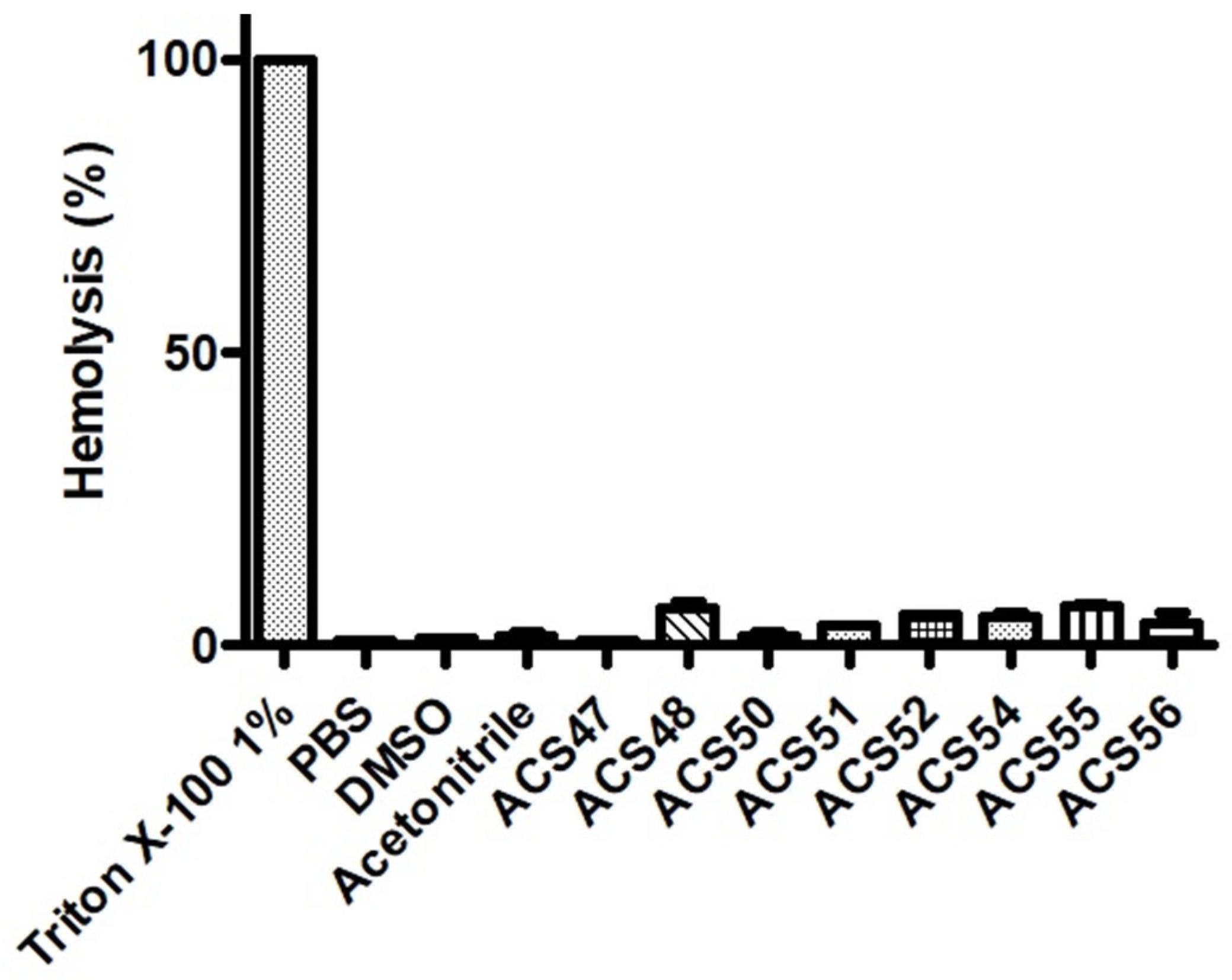
2.3.5. Erythrocyte Viability
2.3.6. In Silico Toxicity Prediction
2.3.7. Statistical Analysis
3. Results
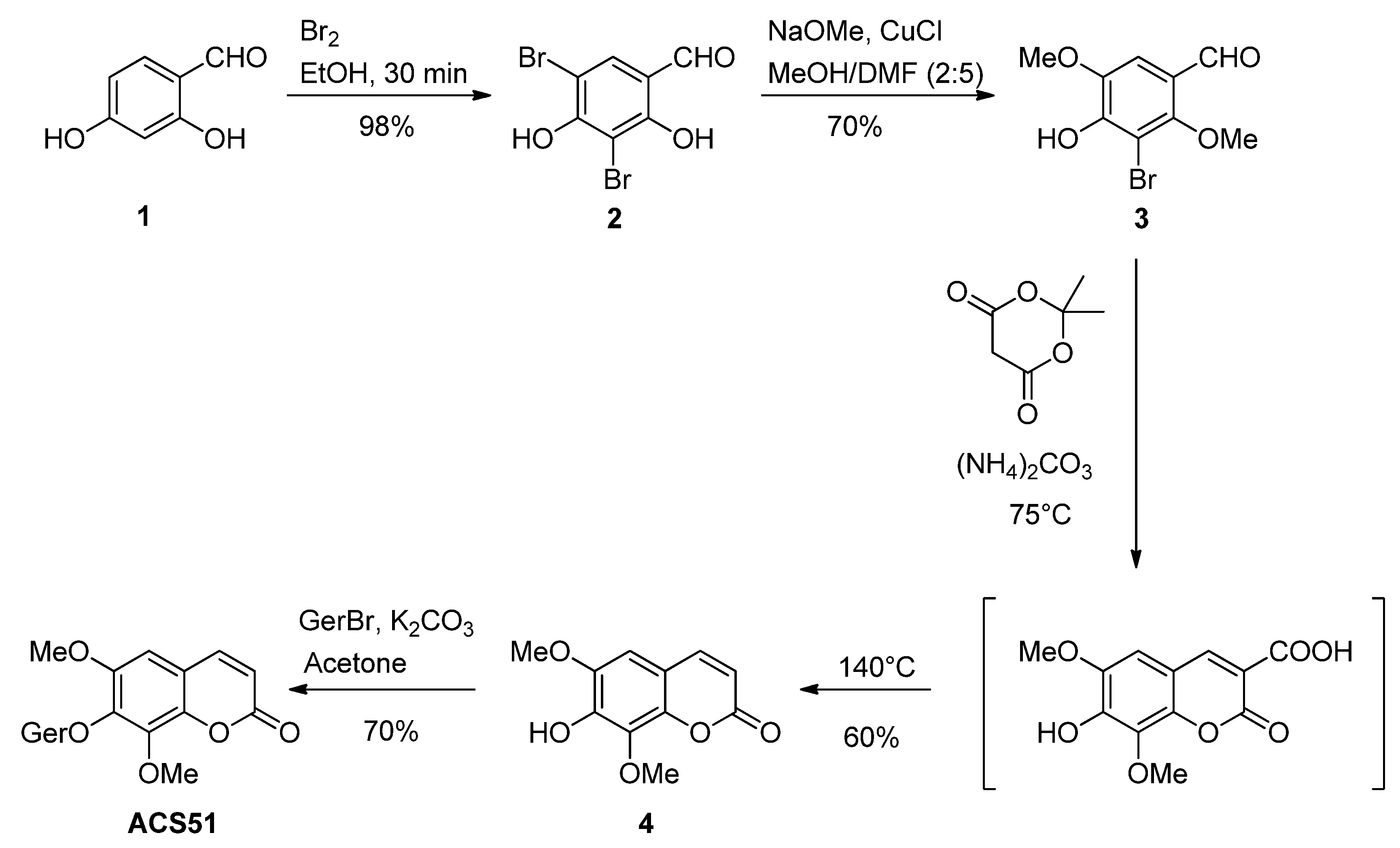
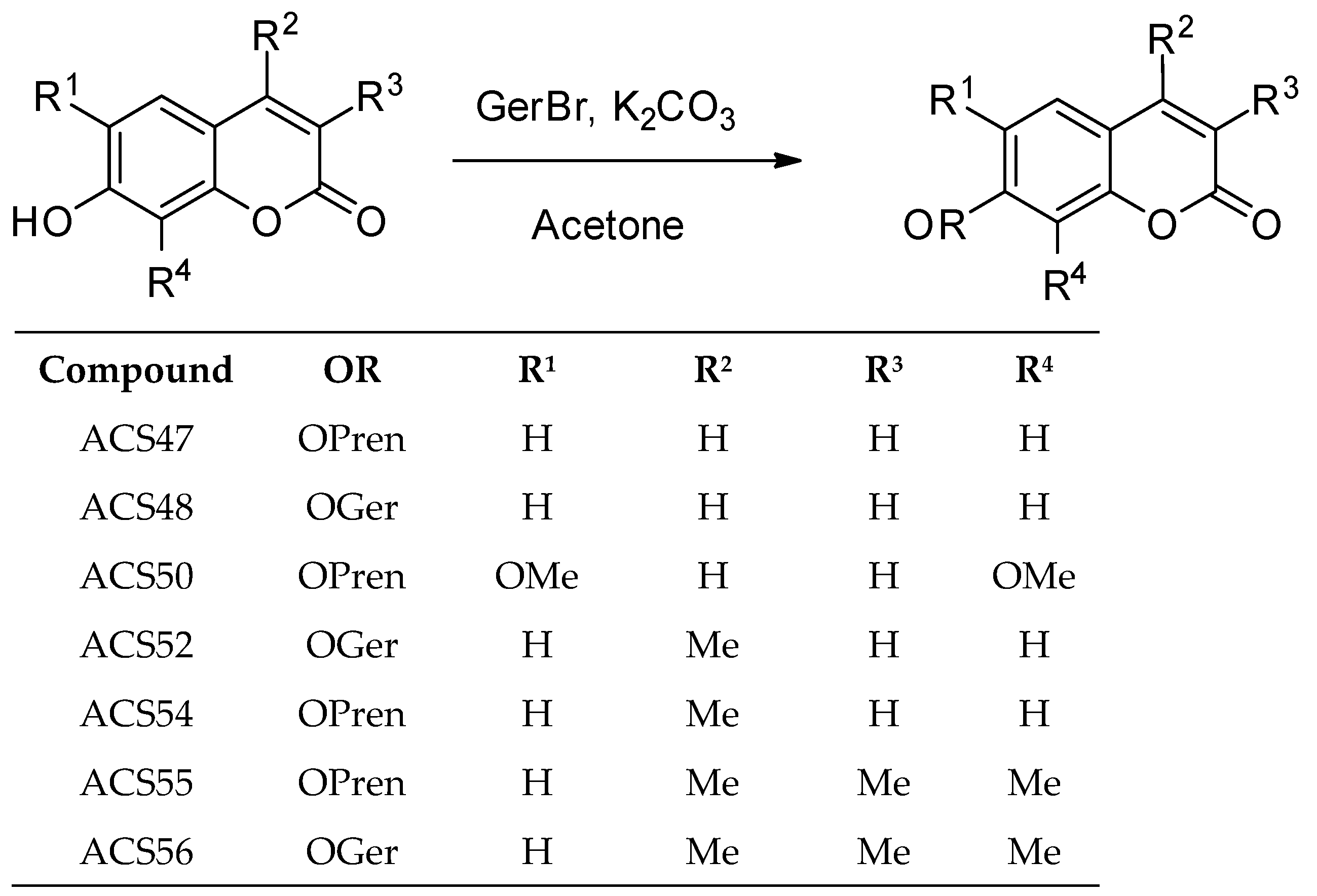
3.1. Synthesis
3.2. Antifungal Activity of Coumarins against C. albicans and S. cerevisiae Strains
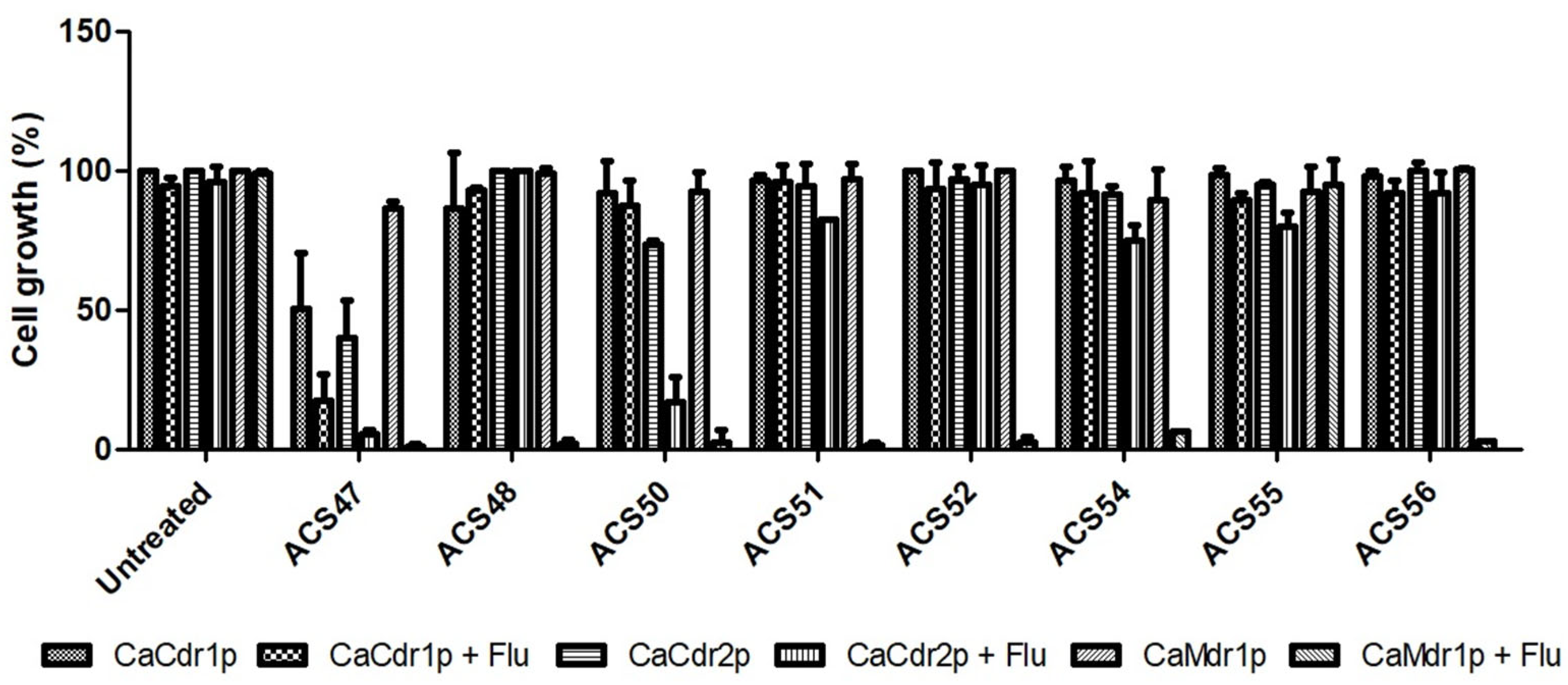
3.3. Antifungal Activity of Coumarins Combined with Fluconazole against S. cerevisiae Strains
3.4. Synergism Evaluation through Checkerboard Assay
3.5. Erythrocyte Viability
3.6. In Silico Toxicity Prediction
4. Discussion
4.1. Synthesis of Prenylated Coumarins
4.2. Antifungal Activity of Coumarins against C. albicans and S. cerevisiae Strains
4.3. Antifungal Activity of Coumarins Combined with Fluconazole against S. cerevisiae Strains
4.4. Antifungal Activity of Coumarins Combined with Fluconazole against Strains of C. albicans
4.5. Toxicity
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Soll, D.R.; Galask, R.; Schmid, J.; Hanna, C.; Mac, K.; Morrow, B. Genetic Dissimilarity of Commensal Strains of Candida Spp. Carried in Different Anatomical Locations of the Same Healthy Women. J. Clin. Microbiol. 1991, 29, 1702–1710. [Google Scholar] [CrossRef] [PubMed]
- Brown, G.D.; Denning, D.W.; Gow, N.A.R.; Levitz, S.M.; Netea, M.G.; White, T.C. Hidden Killers: Human Fungal Infections. Sci. Transl. Med. 2012, 4, 165rv13. [Google Scholar] [CrossRef] [PubMed]
- Lewis, R.E. Current Concepts in Antifungal Pharmacology. Mayo Clin. Proc. 2011, 86, 805–817. [Google Scholar] [CrossRef] [PubMed]
- Franz, R.; Kelly, S.L.; Lamb, D.C.; Kelly, D.E.; Ruhnke, M.; Morschhäuser, J. Multiple Molecular Mechanisms Contribute to a Stepwise Development of Fluconazole Resistance in Clinical Candida Albicans Strains. Antimicrob. Agents Chemother. 1998, 42, 3065–3072. [Google Scholar] [CrossRef] [PubMed]
- White, T.C.; Holleman, S.; Dy, F.; Mirels, L.F.; Stevens, D.A. Resistance Mechanisms in Clinical Isolates of Candida Albicans. Agents Chemother. 2002, 46, 1704–1713. [Google Scholar] [CrossRef]
- Ter Beek, J.; Guskov, A.; Slotboom, D.J. Structural Diversity of ABC Transporters. J. Gen. Physiol. 2014, 143, 419–435. [Google Scholar] [CrossRef]
- Kumari, S.; Kumar, M.; Khandelwal, N.K.; Kumari, P.; Varma, M.; Vishwakarma, P.; Shahi, G.; Sharma, S.; Lynn, A.M.; Prasad, R.; et al. ABC Transportome Inventory of Human Pathogenic Yeast Candida Glabrata: Phylogenetic and Expression Analysis. PLoS ONE 2018, 13, e0202993. [Google Scholar] [CrossRef]
- Cannon, R.D.; Lamping, E.; Holmes, A.R.; Niimi, K.; Baret, P.V.; Keniya, M.V.; Tanabe, K.; Niimi, M.; Goffeau, A.; Monk, B.C. Efflux-Mediated Antifungal Drug Resistance. Clin. Microbiol. Rev. 2009, 22, 291–321. [Google Scholar] [CrossRef]
- Li, X.; Li, Y.; Ma, S.; Zhao, Q.; Wu, J.; Duan, L.; Xie, Y.; Wang, S. Traditional Uses, Phytochemistry, and Pharmacology of Ailanthus Altissima (Mill.) Swingle Bark: A Comprehensive Review. J. Ethnopharmacol. 2021, 275, 114121. [Google Scholar] [CrossRef]
- Qin, H.L.; Zhang, Z.W.; Ravindar, L.; Rakesh, K.P. Antibacterial Activities with the Structure-Activity Relationship of Coumarin Derivatives. Eur. J. Med. Chem. 2020, 207, 112832. [Google Scholar] [CrossRef]
- Tan, N.; Yazıcı-Tütüniş, S.; Bilgin, M.; Tan, E.; Miski, M. Antibacterial Activities of Pyrenylated Coumarins from the Roots of Prangos Hulusii. Molecules 2017, 22, 1098. [Google Scholar] [CrossRef] [PubMed]
- Fotso, G.W.; Ngameni, B.; Storr, T.E.; Ngadjui, B.T.; Mafu, S.; Stephenson, G.R. Synthesis of Novel Stilbene–Coumarin Derivatives and Antifungal Screening of Monotes Kerstingii-Specialized Metabolites against Fusarium Oxysporum. Antibiotics 2020, 9, 537. [Google Scholar] [CrossRef] [PubMed]
- Iranshahi, M.; Arfa, P.; Ramezani, M.; Jaafari, M.R.; Sadeghian, H.; Bassarello, C.; Piacente, S.; Pizza, C. Sesquiterpene Coumarins from Ferula Szowitsiana and in Vitro Antileishmanial Activity of 7-Prenyloxycoumarins against Promastigotes. Phytochemistry 2007, 68, 554–561. [Google Scholar] [CrossRef] [PubMed]
- Tayarani-Najaran, Z.; Tayarani-Najaran, N.; Eghbali, S. A Review of Auraptene as an Anticancer Agent. Front. Pharmacol. 2021, 12, 698352. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.P.; Yan, G.; Xie, Y.T.; Lin, T.C.; Zhang, W.; Li, J.; Wu, Y.J.; Zhou, J.Y.; Fu, Y.H. Bioactive Prenylated Coumarins as Potential Anti-Inflammatory and Anti-HIV Agents from Clausena Lenis. Bioorg. Chem. 2020, 97, 103699. [Google Scholar] [CrossRef] [PubMed]
- Dao, T.T.; Tran, T.L.; Kim, J.; Nguyen, P.H.; Lee, E.H.; Park, J.; Jang, I.S.; Oh, W.K. Terpenylated Coumarins as SIRT1 Activators Isolated from Ailanthus Altissima. J. Nat. Prod. 2012, 75, 1332–1338. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.C.; Benelkebir, H.; Lopes, R.S.C.; Lopes, C.C.; Ganesan, A. Total Synthesis of Altissimacoumarin D, a Small Molecule Sirtuin 1 Activator. J. Braz. Chem. Soc. 2018, 29, 1157–1161. [Google Scholar]
- Van Schijndel, J.; Molendijk, D.; Canalle, L.A.; Rump, E.T.; Meuldijk, J. Temperature Dependent Green Synthesis of 3-Carboxycoumarins and 3,4-Unsubstituted Coumarins. Curr. Org. Synth. 2018, 16, 130–135. [Google Scholar] [CrossRef]
- Lamping, E.; Monk, B.C.; Niimi, K.; Holmes, A.R.; Tsao, S.; Tanabe, K.; Niimi, M.; Uehara, Y.; Cannon, R.D. Characterization of Three Classes of Membrane Proteins Involved in Fungal Azole Resistance by Functional Hyperexpression in Saccharomyces cerevisiae. Eukaryot. Cell 2007, 6, 1150–1165. [Google Scholar] [CrossRef]
- Pinto, A.C.C.; Rocha, D.A.S.; Moraes, D.C.D.; Junqueira, M.L.; Ferreira-Pereira, A. Candida Albicans Clinical Isolates from a Southwest Brazilian Tertiary Hospital Exhibit MFS-Mediated Azole Resistance Profile. An. Acad. Bras. Cienc. 2019, 91, e20180654. [Google Scholar] [CrossRef]
- Clemente de Moraes, D.; do Carmo Freire Ribeiro Pinto, M.; Tenório Sousa Domingos, L.; do Valle Pereira Midlej, V.; Ferreira-Pereira, A. Effects of β-Lapachone and β-nor-Lapachone on Multidrug Efflux Transporters and Biofilms of Candida Glabrata. Bioorg. Med. Chem. 2022, 63, 116749. [Google Scholar] [CrossRef] [PubMed]
- Niimi, K.; Harding, D.R.K.; Parshot, R.; King, A.; Lun, D.J.; Decottignies, A.; Niimi, M.; Lin, S.; Cannon, R.D.; Goffeau, A.; et al. Chemosensitization of Fluconazole Resistance in Saccharomyces Cerevisiae and Pathogenic Fungi by a D -Octapeptide Derivative. Antimicrob. Agents Chemother. 2004, 48, 1256–1271. [Google Scholar] [CrossRef] [PubMed]
- de Moraes, D.C.; Cardoso, K.M.; Domingos, L.T.S.; do Carmo Freire Ribeiro Pinto, M.; Monteiro, R.Q.; Ferreira-Pereira, A. β-Lapachone Enhances the Antifungal Activity of Fluconazole against a Pdr5p-Mediated Resistant Saccharomyces Cerevisiae Strain. Braz. J. Microbiol. 2020, 51, 1051–1060. [Google Scholar] [CrossRef] [PubMed]
- Lagunin, A.; Zakharov, A.; Filimonov, D.; Poroikov, V. QSAR Modelling of Rat Acute Toxicity on the Basis of PASS Prediction. Mol. Inform. 2011, 30, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.K.; Jeong, M.; Jang, D.S.; Choi, J.H. Anti-Inflammatory Effects of Canthin-6-One Alkaloids from Ailanthus Altissima. Planta Med. 2018, 84, 527–535. [Google Scholar] [CrossRef]
- Jeong, M.; Kim, H.M.; Ahn, J.H.; Lee, K.T.; Jang, D.S.; Choi, J.H. 9-Hydroxycanthin-6-One Isolated from Stem Bark of Ailanthus Altissima Induces Ovarian Cancer Cell Apoptosis and Inhibits the Activation of Tumor-Associated Macrophages. Chem. Biol. Interact. 2018, 280, 99–108. [Google Scholar] [CrossRef]
- Shao, Q.; Li, T.Y.; Quan, W.; Wang, H.; Yan, K.Y.; Qiu, P.C.; Tang, H.F.; Lu, Y.Y. The Alkaloids with Neuroprotective Effect from the Root Bark of Ailanthus Altissima. Nat. Prod. Res. 2022, 1–7. [Google Scholar] [CrossRef]
- Li, Y.; Zhao, M.; Zhang, Z. Quantitative Proteomics Reveals the Antifungal Effect of Canthin-6-One Isolated from Ailanthus Altissima against Fusarium Oxysporum f. Sp. Cucumerinum in Vitro. PLoS ONE 2021, 16, e0250712. [Google Scholar] [CrossRef]
- Annunziata, F.; Pinna, C.; Dallavalle, S.; Tamborini, L.; Pinto, A. An Overview of Coumarin as a Versatile and Readily Accessible Scaffold with Broad-Ranging Biological Activities. Int. J. Mol. Sci. 2020, 21, 4618. [Google Scholar] [CrossRef]
- Kurdelas, R.R.; Lima, B.; Tapia, A.; Feresin, G.E.; Sierra, M.G.; Rodríguez, M.V.; Zacchino, S.; Enriz, R.D.; Freile, M.L. Antifungal Activity of Extracts and Prenylated Coumarins Isolated from Baccharis Darwinii Hook & Arn. (Asteraceae). Molecules 2010, 15, 4898–4907. [Google Scholar] [CrossRef]
- Jia, C.; Zhang, J.; Yu, L.; Wang, C.; Yang, Y.; Rong, X.; Xu, K.; Chu, M. Antifungal Activity of Coumarin against Candida Albicans Is Related to Apoptosis. Front. Cell. Infect. Microbiol. 2019, 9, 445. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Mukwaya, E.; Wong, M.S.; Zhang, Y. A Systematic Review on Biological Activities of Prenylated Flavonoids. Pharm. Biol. 2014, 52, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Nim, S.; Nothias, L.F.; Gallard, J.F.; Rawal, M.K.; Costa, J.; Roussi, F.; Prasad, R.; Di Pietro, A.; Paolini, J.; et al. Evaluation of Jatrophane Esters from Euphorbia Spp. as Modulators of Candida Albicans Multidrug Transporters. J. Nat. Prod. 2017, 80, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Fatima, Z.; Ahmad, K.; Hameed, S. Fungicidal Action of Geraniol against Candida Albicans Is Potentiated by Abrogated CaCdr1p Drug Efflux and Fluconazole Synergism. PLoS ONE 2018, 13, e0203079. [Google Scholar] [CrossRef]
- Lemos, A.S.O.; Florêncio, J.R.; Pinto, N.C.C.; Campos, L.M.; Silva, T.P.; Grazul, R.M.; Pinto, P.F.; Tavares, G.D.; Scio, E.; Apolônio, A.C.M.; et al. Antifungal Activity of the Natural Coumarin Scopoletin Against Planktonic Cells and Biofilms from a Multidrug-Resistant Candida Tropicalis Strain. Front. Microbiol. 2020, 11, 1525. [Google Scholar] [CrossRef]
- Nabekura, T.; Kawasaki, T.; Kato, Y.; Kawai, K.; Fiorito, S.; Epifano, F.; Genovese, S.; Uwai, Y. Citrus Auraptene Induces Drug Efflux Transporter P-Glycoprotein Expression in Human Intestinal Cells. Food Funct. 2020, 11, 5017–5023. [Google Scholar] [CrossRef]
- Mukhopadhyay, K.; Kohli, A.; Prasad, R. Drug Susceptibilities of Yeast Cells Are Affected by Membrane Lipid Composition. Antimicrob. Agents Chemother. 2002, 46, 3695–3705. [Google Scholar] [CrossRef]
- Moraes, D.C.; Reis de Sá, L.F.; Domingos, L.T.S.; Pinto, M.d.C.F.R.; Soares, R.M.d.A.; Ferreira-Pereira, A. Synergistic Interactions between β-Lapachone and Fluconazole in the Inhibition of CaCdr2p and CaMdr1p in Candida Albicans. Rev. Iberoam. Micol. 2020, 37, 104–106. [Google Scholar] [CrossRef]
- Maleki, E.H.; Bahrami, A.R.; Sadeghian, H.; Matin, M.M. Discovering the Structure–Activity Relationships of Different O-Prenylated Coumarin Derivatives as Effective Anticancer Agents in Human Cervical Cancer Cells. Toxicol. Vitr. 2020, 63, 104745. [Google Scholar] [CrossRef]
- Greco, I.; Molchanova, N.; Holmedal, E.; Jenssen, H.; Hummel, B.D.; Watts, J.L.; Håkansson, J.; Hansen, P.R.; Svenson, J. Correlation between Hemolytic Activity, Cytotoxicity and Systemic in Vivo Toxicity of Synthetic Antimicrobial Peptides. Sci. Rep. 2020, 10, 13206. [Google Scholar] [CrossRef]

| Strain | Efflux Transporter | Family | Species |
|---|---|---|---|
| Null mutant | None | - | S. cerevisiae |
| CaCdr1p+ | CaCdr1p | ABC | S. cerevisiae |
| CaCdr2p+ | CaCdr2p | ABC | S. cerevisiae |
| CaMdr1p+ | CaMdr1p | MFS | S. cerevisiae |
| 95-142 | CaCdr1p and CaCdr2p | ABC | C. albicans |
| PRI | CaMdr1p | MFS | C. albicans |
| ATCC 10231 | None | - | C. albicans |
| Strain and Compound | Compound (µg/mL) | Fluconazole (µg/mL) | ||||||
|---|---|---|---|---|---|---|---|---|
| MICa | MICb | FIC | MICa | MICb | FIC | FICI | Outcome | |
| CaCdr1p+ | ||||||||
| ACS47 | >100 | 50 | 0.250 | >250 | 62.5 | 0.125 | 0.375 | S |
| CaCdr2p+ | ||||||||
| ACS47 | >100 | 50 | 0.250 | 62.5 | 15.6 | 0.250 | 0.500 | S |
| ACS50 | >100 | 25 | 0.125 | 62.5 | 31.3 | 0.500 | 0.625 | A |
| CaMdr1p+ | ||||||||
| ACS47 | >100 | 25 | 0.125 | 62.5 | 3.91 | 0.063 | 0.188 | S |
| ACS48 | >100 | 50 | 0.250 | 62.5 | 7.81 | 0.125 | 0.375 | S |
| ACS50 | >100 | 25 | 0.125 | 62.5 | 15.6 | 0.250 | 0.375 | S |
| ACS51 | >100 | 50 | 0.250 | 62.5 | 15.6 | 0.250 | 0.500 | S |
| ACS52 | >100 | 12.5 | 0.063 | 62.5 | 15.6 | 0.250 | 0.313 | S |
| ACS54 | >100 | 12.5 | 0.063 | 62.5 | 7.81 | 0.125 | 0.188 | S |
| ACS55 | >100 | 100 | 0.500 | 62.5 | 31.3 | 0.500 | 1.000 | A |
| ACS56 | >100 | 100 | 0.500 | 62.5 | 15.6 | 0.250 | 0.750 | A |
| Strain and Compound | Compound (µg/mL) | Fluconazole (µg/mL) | ||||||
|---|---|---|---|---|---|---|---|---|
| MICa | MICb | FIC | MICa | MICb | FIC | FICI | Outcome | |
| 95-142 | ||||||||
| ACS47 | >100 | 50 | 0.250 | 500 | 62.5 | 0.125 | 0.375 | S |
| ACS50 | >100 | 50 | 0.250 | 500 | 125 | 0.250 | 0.500 | S |
| PRI | ||||||||
| ACS47 | >100 | 100 | 0.500 | 1000 | 15.6 | 0.016 | 0.516 | A |
| ACS48 | >100 | >100 | 1 | 1000 | 1000 | 1 | 2 | I |
| ACS50 | >100 | 100 | 0.500 | 1000 | 15.6 | 0.016 | 0.516 | A |
| ACS51 | >100 | >100 | 1 | 1000 | 1000 | 1 | 2 | I |
| ACS52 | >100 | >100 | 1 | 1000 | 1000 | 1 | 2 | I |
| ACS54 | >100 | >100 | 1 | 1000 | 1000 | 1 | 2 | I |
| ACS55 | >100 | >100 | 1 | 1000 | 1000 | 1 | 2 | I |
| ACS56 | >100 | >100 | 1 | 1000 | 1000 | 1 | 2 | I |
| Compound | Mutagenic | Tumorigenic | Irritant | Reproductive Effect |
|---|---|---|---|---|
| ACS47 | No | No | No | No |
| ACS48 | No | No | Yes | No |
| ACS50 | No | No | No | No |
| ACS51 | No | No | Yes | No |
| ACS52 | No | No | Yes | Yes |
| ACS54 | No | No | No | Yes |
| ACS55 | No | No | Yes | Yes |
| ACS56 | No | No | Yes | Yes |
| Compound | Rat IP LD50 | Rat IV LD50 | Rat Oral LD50 | Rat SC LD50 |
|---|---|---|---|---|
| ACS47 | 476.4 | 65.99 | 1551 | 2462 |
| ACS48 | 456.5 | 90.71 | 2157 | 1234 |
| ACS50 | 426.8 | 93.38 | 1057 | 1461 |
| ACS51 | 525 | 121.6 | 1401 | 845.7 |
| ACS52 | 401.5 | 83.72 | 1979 | 918.6 |
| ACS54 | 581.3 | 66.26 | 1470 | 2452 |
| ACS55 | 333.1 | 53.41 | 2445 | 1116 |
| ACS56 | 351.9 | 74.89 | 2690 | 948.3 |
| Fluconazole | 708 | 200.4 | 584.4 | 511.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, A.C.; de Moraes, D.C.; do Carmo, D.C.; Gomes, G.C.C.; Ganesan, A.; Lopes, R.S.C.; Ferreira-Pereira, A.; Lopes, C.C. Synthesis of Altissimacoumarin D and Other Prenylated Coumarins and Their Ability to Reverse the Multidrug Resistance Phenotype in Candida albicans. J. Fungi 2023, 9, 758. https://doi.org/10.3390/jof9070758
Silva AC, de Moraes DC, do Carmo DC, Gomes GCC, Ganesan A, Lopes RSC, Ferreira-Pereira A, Lopes CC. Synthesis of Altissimacoumarin D and Other Prenylated Coumarins and Their Ability to Reverse the Multidrug Resistance Phenotype in Candida albicans. Journal of Fungi. 2023; 9(7):758. https://doi.org/10.3390/jof9070758
Chicago/Turabian StyleSilva, Anna Claudia, Daniel Clemente de Moraes, Denilson Costa do Carmo, Giselle Cristina Casaes Gomes, A. Ganesan, Rosangela Sabbatini Capella Lopes, Antonio Ferreira-Pereira, and Cláudio Cerqueira Lopes. 2023. "Synthesis of Altissimacoumarin D and Other Prenylated Coumarins and Their Ability to Reverse the Multidrug Resistance Phenotype in Candida albicans" Journal of Fungi 9, no. 7: 758. https://doi.org/10.3390/jof9070758
APA StyleSilva, A. C., de Moraes, D. C., do Carmo, D. C., Gomes, G. C. C., Ganesan, A., Lopes, R. S. C., Ferreira-Pereira, A., & Lopes, C. C. (2023). Synthesis of Altissimacoumarin D and Other Prenylated Coumarins and Their Ability to Reverse the Multidrug Resistance Phenotype in Candida albicans. Journal of Fungi, 9(7), 758. https://doi.org/10.3390/jof9070758









