Whole-Genome Sequence Analysis of Candida glabrata Isolates from a Patient with Persistent Fungemia and Determination of the Molecular Mechanisms of Multidrug Resistance
Abstract
1. Introduction
2. Materials and Methods
2.1. Fungal Isolates and Antifungal Susceptibility Testing
2.2. Whole-Genome Sequencing
2.3. In Vivo Virulence Analysis Using Galleria Mellonella
2.4. Statistical Analysis
2.5. Deposition of the Raw Sequence Data
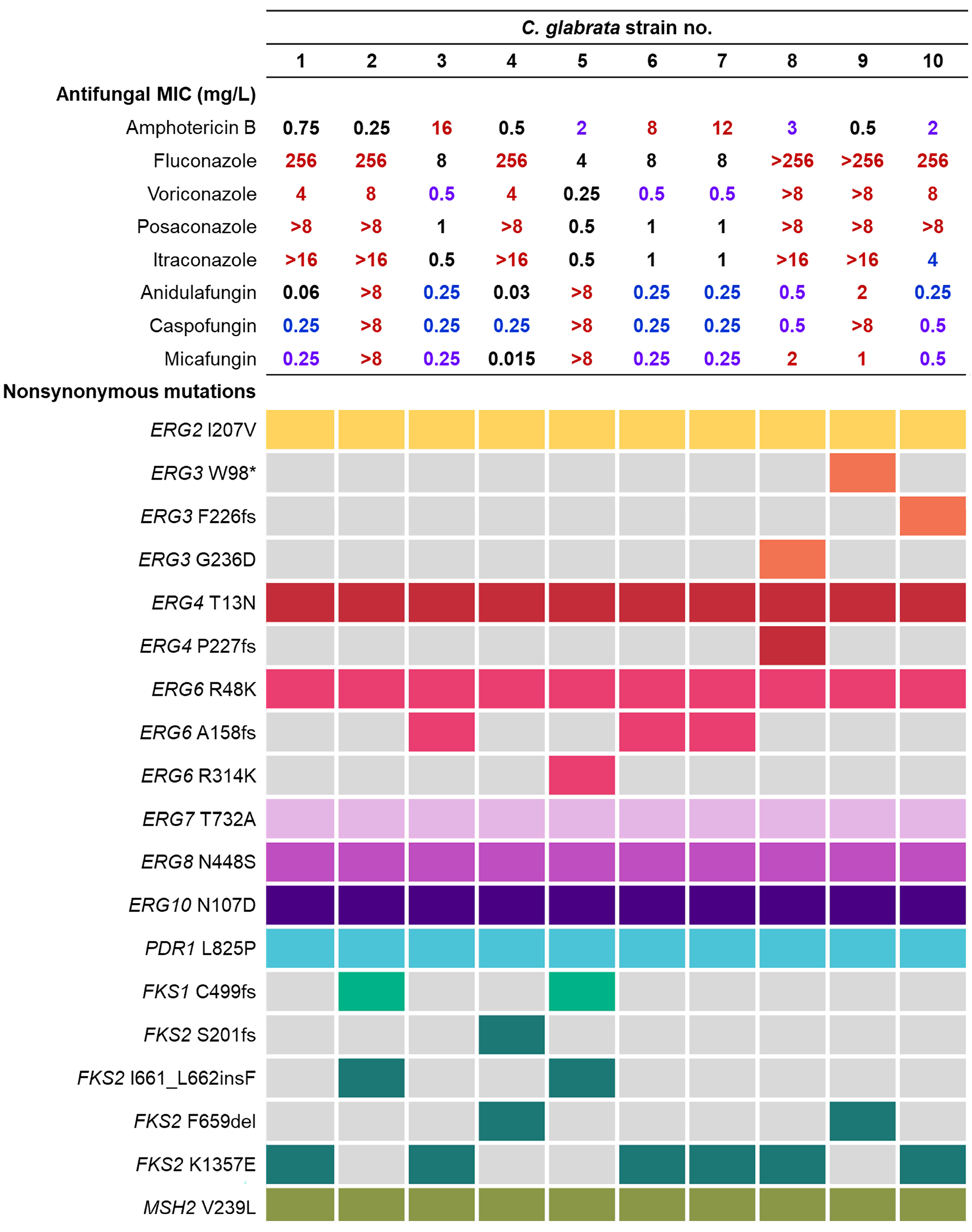
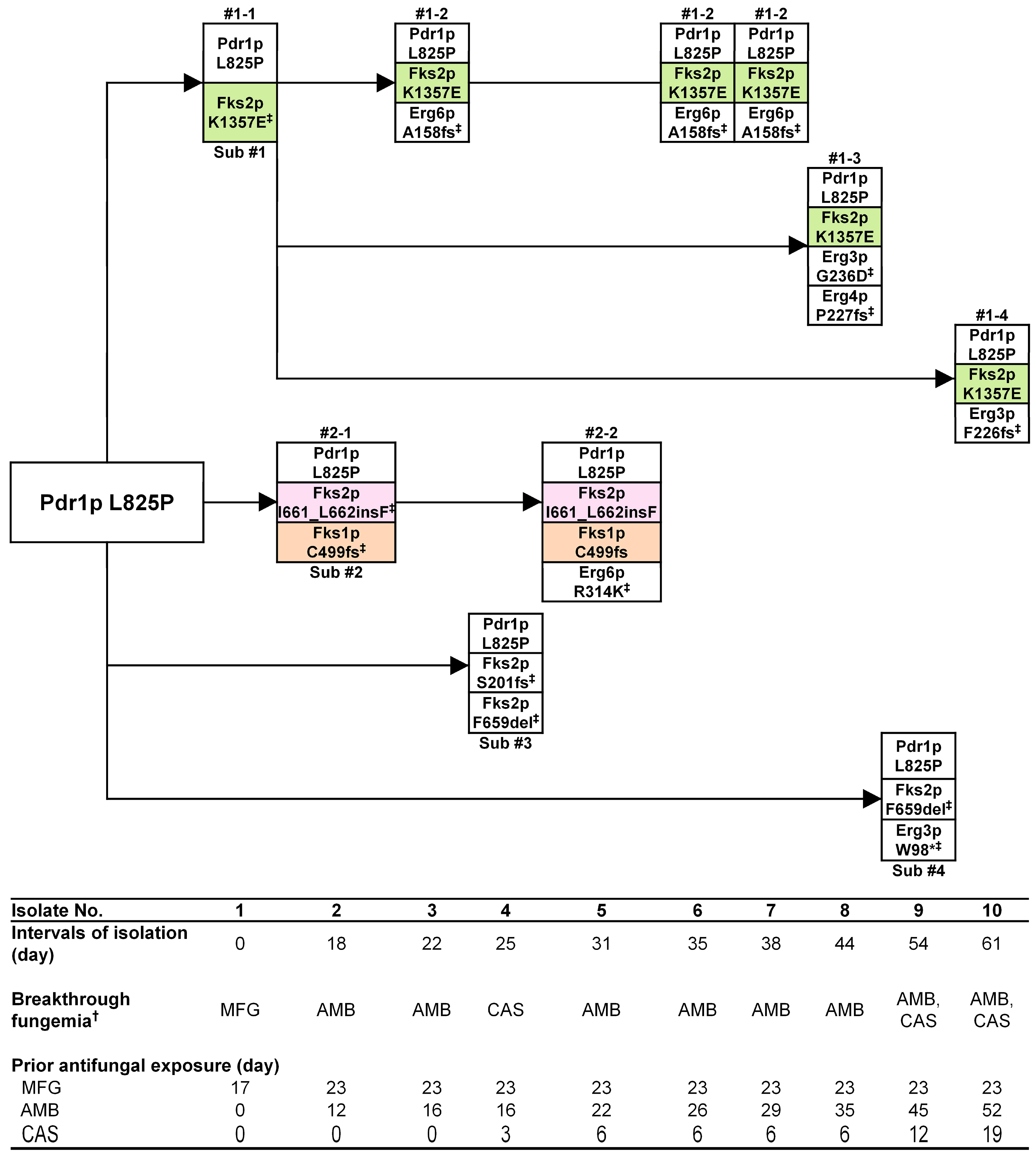
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Falagas, M.E.; Apostolou, K.E.; Pappas, V.D. Attributable mortality of candidemia: A systematic review of matched cohort and case-control studies. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2006, 25, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.J.; Won, E.J.; Jeong, S.H.; Shin, K.S.; Shin, J.H.; Kim, Y.R.; Kim, H.S.; Kim, Y.A.; Uh, Y.; Kim, T.S.; et al. Dynamics and Predictors of Mortality Due to Candidemia Caused by Different Candida Species: Comparison of Intensive Care Unit-Associated Candidemia (ICUAC) and Non-ICUAC. J. Fungi 2021, 7, 597. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.A.; Diekema, D.J.; Turnidge, J.D.; Castanheira, M.; Jones, R.N. Twenty years of the SENTRY antifungal surveillance program: Results for Candida species from 1997–2016. Open Forum Infect. Dis. 2019, 6 (Suppl. S1), S79–S94. [Google Scholar] [CrossRef] [PubMed]
- Arastehfar, A.; Lass-Florl, C.; Garcia-Rubio, R.; Daneshnia, F.; Ilkit, M.; Boekhout, T.; Gabaldon, T.; Perlin, D.S. The quiet and underappreciated rise of drug-resistant invasive fungal pathogens. J. Fungi 2020, 6, 138. [Google Scholar] [CrossRef] [PubMed]
- Lockhart, S.R.; Etienne, K.A.; Vallabhaneni, S.; Farooqi, J.; Chowdhary, A.; Govender, N.P.; Colombo, A.L.; Calvo, B.; Cuomo, C.A.; Desjardins, C.A.; et al. Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2017, 64, 134–140. [Google Scholar] [CrossRef]
- Lee, W.G.; Shin, J.H.; Uh, Y.; Kang, M.G.; Kim, S.H.; Park, K.H.; Jang, H.C. First three reported cases of nosocomial fungemia caused by Candida auris. J. Clin. Microbiol. 2011, 49, 3139–3142. [Google Scholar] [CrossRef]
- Kwon, Y.J.; Shin, J.H.; Byun, S.A.; Choi, M.J.; Won, E.J.; Lee, D.; Lee, S.Y.; Chun, S.; Lee, J.H.; Choi, H.J.; et al. Candida auris clinical isolates from South Korea: Identification, antifungal susceptibility, and genotyping. J. Clin. Microbiol. 2019, 57, e01624-18. [Google Scholar] [CrossRef]
- Won, E.J.; Choi, M.J.; Kim, M.N.; Yong, D.; Lee, W.G.; Uh, Y.; Kim, T.S.; Byeon, S.A.; Lee, S.Y.; Kim, S.H.; et al. Fluconazole-resistant Candida glabrata bloodstream isolates, South Korea, 2008–2018. Emerg. Infect. Dis. 2021, 27, 779–788. [Google Scholar] [CrossRef]
- Cho, E.J.; Shin, J.H.; Kim, S.H.; Kim, H.K.; Park, J.S.; Sung, H.; Kim, M.N.; Im, H.J. Emergence of multiple resistance profiles involving azoles, echinocandins and amphotericin B in Candida glabrata isolates from a neutropenia patient with prolonged fungaemia. J. Antimicrob. Chemother. 2015, 70, 1268–1270. [Google Scholar] [CrossRef]
- Arendrup, M.C. Epidemiology of invasive candidiasis. Curr. Opin. Crit. Care 2010, 16, 445–452. [Google Scholar] [CrossRef]
- Rodrigues, C.F.; Silva, S.; Henriques, M. Candida glabrata: A review of its features and resistance. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 673–688. [Google Scholar] [CrossRef] [PubMed]
- Performance Standards for Antifungal Susceptibility Testing of Yeasts, 2nd ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020.
- Muller, H.; Thierry, A.; Coppee, J.Y.; Gouyette, C.; Hennequin, C.; Sismeiro, O.; Talla, E.; Dujon, B.; Fairhead, C. Genomic polymorphism in the population of Candida glabrata: Gene copy-number variation and chromosomal translocations. Fungal Genet. Biol. FG B 2009, 46, 264–276. [Google Scholar] [CrossRef]
- Chapeland-Leclerc, F.; Hennequin, C.; Papon, N.; Noel, T.; Girard, A.; Socie, G.; Ribaud, P.; Lacroix, C. Acquisition of flucytosine, azole, and caspofungin resistance in Candida glabrata bloodstream isolates serially obtained from a hematopoietic stem cell transplant recipient. Antimicrob. Agents Chemother. 2010, 54, 1360–1362. [Google Scholar] [CrossRef] [PubMed]
- Bizerra, F.C.; Jimenez-Ortigosa, C.; Souza, A.C.; Breda, G.L.; Queiroz-Telles, F.; Perlin, D.S.; Colombo, A.L. Breakthrough candidemia due to multidrug-resistant Candida glabrata during prophylaxis with a low dose of micafungin. Antimicrob. Agents Chemother. 2014, 58, 2438–2440. [Google Scholar] [CrossRef] [PubMed]
- Pham, C.D.; Iqbal, N.; Bolden, C.B.; Kuykendall, R.J.; Harrison, L.H.; Farley, M.M.; Schaffner, W.; Beldavs, Z.G.; Chiller, T.M.; Park, B.J.; et al. Role of FKS mutations in Candida glabrata: MIC values, echinocandin resistance, and multidrug resistance. Antimicrob. Agents Chemother. 2014, 58, 4690–4696. [Google Scholar] [CrossRef]
- Park, S.; Kelly, R.; Kahn, J.N.; Robles, J.; Hsu, M.J.; Register, E.; Li, W.; Vyas, V.; Fan, H.; Abruzzo, G.; et al. Specific substitutions in the echinocandin target Fks1p account for reduced susceptibility of rare laboratory and clinical Candida sp. isolates. Antimicrob. Agents Chemother. 2005, 49, 3264–3273. [Google Scholar] [CrossRef] [PubMed]
- Arendrup, M.C.; Patterson, T.F. Multidrug-resistant Candida: Epidemiology, molecular mechanisms, and treatment. J. Infect. Dis. 2017, 216 (Suppl. S3), S445–S451. [Google Scholar] [CrossRef]
- Farmakiotis, D.; Tarrand, J.J.; Kontoyiannis, D.P. Drug-resistant Candida glabrata infection in cancer patients. Emerg. Infect. Dis. 2014, 20, 1833–1840. [Google Scholar] [CrossRef]
- Marr, K.A. Fungal infections in hematopoietic stem cell transplant recipients. Med. Mycol. 2008, 46, 293–302. [Google Scholar] [CrossRef]
- Marr, K.A.; Seidel, K.; White, T.C.; Bowden, R.A. Candidemia in allogeneic blood and marrow transplant recipients: Evolution of risk factors after the adoption of prophylactic fluconazole. J. Infect. Dis. 2000, 181, 309–316. [Google Scholar] [CrossRef]
- Singh-Babak, S.D.; Babak, T.; Diezmann, S.; Hill, J.A.; Xie, J.L.; Chen, Y.L.; Poutanen, S.M.; Rennie, R.P.; Heitman, J.; Cowen, L.E. Global analysis of the evolution and mechanism of echinocandin resistance in Candida glabrata. PLoS Pathog. 2012, 8, e1002718. [Google Scholar] [CrossRef] [PubMed]
- Biswas, C.; Marcelino, V.R.; Van Hal, S.; Halliday, C.; Martinez, E.; Wang, Q.; Kidd, S.; Kennedy, K.; Marriott, D.; Morrissey, C.O.; et al. Whole genome sequencing of Australian Candida glabrata isolates reveals genetic diversity and novel sequence types. Front. Microbiol. 2018, 9, 2946. [Google Scholar] [CrossRef] [PubMed]
- Epidemiological Cutoff Values for Antifungal Susceptibility Testing M59, 3rd ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020.
- MIC and Zone Diameter Distributions and ECOFFs. Available online: https://www.eucast.org/mic_and_zone_distributions_and_ecoffs (accessed on 12 April 2023).
- Shields, R.K.; Nguyen, M.H.; Press, E.G.; Cumbie, R.; Driscoll, E.; Pasculle, A.W.; Clancy, C.J. Rate of FKS mutations among consecutive Candida isolates causing bloodstream infection. Antimicrob. Agents Chemother. 2015, 59, 7465–7470. [Google Scholar] [CrossRef] [PubMed]
- Tavanti, A.; Gow, N.A.; Senesi, S.; Maiden, M.C.; Odds, F.C. Optimization and validation of multilocus sequence typing for Candida albicans. J. Clin. Microbiol. 2003, 41, 3765–3776. [Google Scholar] [CrossRef] [PubMed]
- BBTools. Available online: http://jgi.doe.gov/data-and-tools/bb-tools/ (accessed on 12 October 2022).
- Li, H.; Durbin, R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics 2010, 26, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Skrzypek, M.S.; Binkley, J.; Binkley, G.; Miyasato, S.R.; Simison, M.; Sherlock, G. The Candida Genome Database (CGD): Incorporation of Assembly 22, systematic identifiers and visualization of high throughput sequencing data. Nucleic Acids Res. 2017, 45, D592–D596. [Google Scholar] [CrossRef]
- Picard Tools. Available online: http://broadinstitute.github.io/picard/ (accessed on 26 August 2022).
- McTaggart, L.R.; Cabrera, A.; Cronin, K.; Kus, J.V. Antifungal susceptibility of clinical yeast isolates from a large Canadian reference laboratory and application of whole-genome sequence analysis to elucidate mechanisms of acquired resistance. Antimicrob. Agents Chemother. 2020, 64, e00402-20. [Google Scholar] [CrossRef]
- Dahiya, S.; Sharma, N.; Punia, A.; Choudhary, P.; Gulia, P.; Parmar, V.S.; Chhillar, A.K. Antimycotic drugs and their mechanisms of resistance to Candida species. Curr. Drug Targets 2022, 23, 116–125. [Google Scholar] [CrossRef]
- Morio, F.; Jensen, R.H.; Le Pape, P.; Arendrup, M.C. Molecular basis of antifungal drug resistance in yeasts. Int. J. Antimicrob. Agents 2017, 50, 599–606. [Google Scholar] [CrossRef]
- Vu, B.G.; Thomas, G.H.; Moye-Rowley, W.S. Evidence that ergosterol biosynthesis modulates activity of the Pdr1 transcription factor in Candida glabrata. mBio 2019, 10, e00934-19. [Google Scholar] [CrossRef]
- Carrete, L.; Ksiezopolska, E.; Gomez-Molero, E.; Angoulvant, A.; Bader, O.; Fairhead, C.; Gabaldon, T. Genome comparisons of Candida glabrata serial clinical isolates reveal patterns of genetic variation in infecting clonal populations. Front. Microbiol. 2019, 10, 112. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Tamura, K.; Nei, M. MEGA: Molecular Evolutionary Genetics Analysis software for microcomputers. Comput. Appl. Biosci. CABIOS 1994, 10, 189–191. [Google Scholar] [CrossRef] [PubMed]
- Won, E.J.; Choi, M.J.; Shin, J.H.; Park, Y.J.; Byun, S.A.; Jung, J.S.; Kim, S.H.; Shin, M.G.; Suh, S.P. Diversity of clinical isolates of Aspergillus terreus in antifungal susceptibilities, genotypes and virulence in Galleria mellonella model: Comparison between respiratory and ear isolates. PLoS ONE 2017, 12, e0186086. [Google Scholar] [CrossRef] [PubMed]
- Gago, S.; Garcia-Rodas, R.; Cuesta, I.; Mellado, E.; Alastruey-Izquierdo, A. Candida parapsilosis, Candida orthopsilosis, and Candida metapsilosis virulence in the non-conventional host Galleria mellonella. Virulence 2014, 5, 278–285. [Google Scholar] [CrossRef]
- Kastanis, G.J.; Santana-Quintero, L.V.; Sanchez-Leon, M.; Lomonaco, S.; Brown, E.W.; Allard, M.W. In-depth comparative analysis of Illumina((R)) MiSeq run metrics: Development of a wet-lab quality assessment tool. Mol. Ecol. Resour. 2019, 19, 377–387. [Google Scholar] [CrossRef]
- Healey, K.R.; Zhao, Y.; Perez, W.B.; Lockhart, S.R.; Sobel, J.D.; Farmakiotis, D.; Kontoyiannis, D.P.; Sanglard, D.; Taj-Aldeen, S.J.; Alexander, B.D.; et al. Prevalent mutator genotype identified in fungal pathogen Candida glabrata promotes multi-drug resistance. Nat. Commun. 2016, 7, 11128. [Google Scholar] [CrossRef]
- Carrete, L.; Ksiezopolska, E.; Pegueroles, C.; Gomez-Molero, E.; Saus, E.; Iraola-Guzman, S.; Loska, D.; Bader, O.; Fairhead, C.; Gabaldon, T. Patterns of genomic variation in the opportunistic pathogen Candida glabrata suggest the existence of mating and a secondary association with humans. Curr. Biol. 2018, 28, 15–27.e17. [Google Scholar] [CrossRef]
- Martel, C.M.; Parker, J.E.; Bader, O.; Weig, M.; Gross, U.; Warrilow, A.G.; Kelly, D.E.; Kelly, S.L. A clinical isolate of Candida albicans with mutations in ERG11 (encoding sterol 14alpha-demethylase) and ERG5 (encoding C22 desaturase) is cross resistant to azoles and amphotericin B. Antimicrob. Agents Chemother. 2010, 54, 3578–3583. [Google Scholar] [CrossRef]
- Vandeputte, P.; Tronchin, G.; Larcher, G.; Ernoult, E.; Berges, T.; Chabasse, D.; Bouchara, J.P. A nonsense mutation in the ERG6 gene leads to reduced susceptibility to polyenes in a clinical isolate of Candida glabrata. Antimicrob. Agents Chemother. 2008, 52, 3701–3709. [Google Scholar] [CrossRef]
- Hull, C.M.; Bader, O.; Parker, J.E.; Weig, M.; Gross, U.; Warrilow, A.G.; Kelly, D.E.; Kelly, S.L. Two clinical isolates of Candida glabrata exhibiting reduced sensitivity to amphotericin B both harbor mutations in ERG2. Antimicrob. Agents Chemother. 2012, 56, 6417–6421. [Google Scholar] [CrossRef]
- Jensen, R.H.; Astvad, K.M.; Silva, L.V.; Sanglard, D.; Jorgensen, R.; Nielsen, K.F.; Mathiasen, E.G.; Doroudian, G.; Perlin, D.S.; Arendrup, M.C. Stepwise emergence of azole, echinocandin and amphotericin B multidrug resistance in vivo in Candida albicans orchestrated by multiple genetic alterations. J. Antimicrob. Chemother. 2015, 70, 2551–2555. [Google Scholar] [CrossRef] [PubMed]
- Krogh-Madsen, M.; Arendrup, M.C.; Heslet, L.; Knudsen, J.D. Amphotericin B and caspofungin resistance in Candida glabrata isolates recovered from a critically ill patient. Clin. Infect. Dis. 2006, 42, 938–944. [Google Scholar] [CrossRef] [PubMed]
- Martel, C.M.; Parker, J.E.; Bader, O.; Weig, M.; Gross, U.; Warrilow, A.G.; Rolley, N.; Kelly, D.E.; Kelly, S.L. Identification and characterization of four azole-resistant erg3 mutants of Candida albicans. Antimicrob. Agents Chemother. 2010, 54, 4527–4533. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Joseph, L.; Parker, J.E.; Asadzadeh, M.; Kelly, S.L.; Meis, J.F.; Khan, Z. ERG6 and ERG2 are major targets conferring reduced susceptibility to amphotericin B in clinical Candida glabrata isolates in Kuwait. Antimicrob. Agents Chemother. 2019, 63, e01900-18. [Google Scholar] [CrossRef]
- Vandeputte, P.; Tronchin, G.; Berges, T.; Hennequin, C.; Chabasse, D.; Bouchara, J.P. Reduced susceptibility to polyenes associated with a missense mutation in the ERG6 gene in a clinical isolate of Candida glabrata with pseudohyphal growth. Antimicrob. Agents Chemother. 2007, 51, 982–990. [Google Scholar] [CrossRef]
- Kelly, S.L.; Lamb, D.C.; Kelly, D.E.; Loeffler, J.; Einsele, H. Resistance to fluconazole and amphotericin in Candida albicans from AIDS patients. Lancet 1996, 348, 1523–1524. [Google Scholar] [CrossRef]
- Sanglard, D.; Ischer, F.; Parkinson, T.; Falconer, D.; Bille, J. Candida albicans mutations in the ergosterol biosynthetic pathway and resistance to several antifungal agents. Antimicrob. Agents Chemother. 2003, 47, 2404–2412. [Google Scholar] [CrossRef]
- Zweytick, D.; Hrastnik, C.; Kohlwein, S.D.; Daum, G. Biochemical characterization and subcellular localization of the sterol C-24(28) reductase, erg4p, from the yeast saccharomyces cerevisiae. FEBS Lett. 2000, 470, 83–87. [Google Scholar] [CrossRef]
- Geber, A.; Hitchcock, C.A.; Swartz, J.E.; Pullen, F.S.; Marsden, K.E.; Kwon-Chung, K.J.; Bennett, J.E. Deletion of the Candida glabrata ERG3 and ERG11 genes: Effect on cell viability, cell growth, sterol composition, and antifungal susceptibility. Antimicrob. Agents Chemother. 1995, 39, 2708–2717. [Google Scholar] [CrossRef]
- Arastehfar, A.; Daneshnia, F.; Zomorodian, K.; Najafzadeh, M.J.; Khodavaisy, S.; Zarrinfar, H.; Hagen, F.; Zare Shahrabadi, Z.; Lackner, M.; Mirhendi, H.; et al. Low level of antifungal resistance in Iranian isolates of Candida glabrata recovered from blood samples in a multicenter study from 2015 to 2018 and potential prognostic values of genotyping and sequencing of PDR1. Antimicrob. Agents Chemother. 2019, 63, e02503-18. [Google Scholar] [CrossRef]
- Hou, X.; Healey, K.R.; Shor, E.; Kordalewska, M.; Ortigosa, C.J.; Paderu, P.; Xiao, M.; Wang, H.; Zhao, Y.; Lin, L.Y.; et al. Novel FKS1 and FKS2 modifications in a high-level echinocandin resistant clinical isolate of Candida glabrata. Emerg. Microbes Infect. 2019, 8, 1619–1625. [Google Scholar] [CrossRef]
- Alexander, B.D.; Johnson, M.D.; Pfeiffer, C.D.; Jimenez-Ortigosa, C.; Catania, J.; Booker, R.; Castanheira, M.; Messer, S.A.; Perlin, D.S.; Pfaller, M.A. Increasing echinocandin resistance in Candida glabrata: Clinical failure correlates with presence of FKS mutations and elevated minimum inhibitory concentrations. Clin. Infect. Dis. 2013, 56, 1724–1732. [Google Scholar] [CrossRef] [PubMed]
- Castanheira, M.; Woosley, L.N.; Messer, S.A.; Diekema, D.J.; Jones, R.N.; Pfaller, M.A. Frequency of fks mutations among Candida glabrata isolates from a 10-year global collection of bloodstream infection isolates. Antimicrob. Agents Chemother. 2014, 58, 577–580. [Google Scholar] [CrossRef] [PubMed]
- Byun, S.A.; Won, E.J.; Kim, M.N.; Lee, W.G.; Lee, K.; Lee, H.S.; Uh, Y.; Healey, K.R.; Perlin, D.S.; Choi, M.J.; et al. Multilocus sequence typing (MLST) genotypes of Candida glabrata bloodstream isolates in Korea: Association with antifungal resistance, mutations in mismatch repair gene (Msh2), and clinical outcomes. Front. Microbiol. 2018, 9, 1523. [Google Scholar] [CrossRef] [PubMed]
- Healey, K.R.; Perlin, D.S. Fungal resistance to echinocandins and the MDR phenomenon in Candida glabrata. J. Fungi 2018, 4, 105. [Google Scholar] [CrossRef] [PubMed]
- Bordallo-Cardona, M.A.; Marcos-Zambrano, L.J.; Sanchez-Carrillo, C.; de la Pedrosa, E.G.G.; Canton, R.; Bouza, E.; Escribano, P.; Guinea, J. Mutant prevention concentration and mutant selection window of micafungin and anidulafungin in clinical Candida glabrata isolates. Antimicrob. Agents Chemother. 2018, 62, e01982-17. [Google Scholar] [CrossRef]
- Borghi, E.; Andreoni, S.; Cirasola, D.; Ricucci, V.; Sciota, R.; Morace, G. Antifungal resistance does not necessarily affect Candida glabrata fitness. J. Chemother. 2014, 26, 32–36. [Google Scholar] [CrossRef]
- Bordallo-Cardona, M.A.; Escribano, P.; Marcos-Zambrano, L.J.; Diaz-Garcia, J.; de la Pedrosa, E.G.; Canton, R.; Bouza, E.; Guinea, J. Low and constant micafungin concentrations may be sufficient to lead to resistance mutations in FKS2 gene of Candida glabrata. Med. Mycol. 2018, 56, 903–906. [Google Scholar] [CrossRef]
- Ames, L.; Duxbury, S.; Pawlowska, B.; Ho, H.L.; Haynes, K.; Bates, S. Galleria mellonella as a host model to study Candida glabrata virulence and antifungal efficacy. Virulence 2017, 8, 1909–1917. [Google Scholar] [CrossRef]
| Isolate No. | Total Mutation | Nonsynonymous Mutation | Nonsynonymous Mutation in the Resistant Gene † | ||||||
|---|---|---|---|---|---|---|---|---|---|
| INDEL | SNP | Total | INDEL | SNP | Total | INDEL | SNP | Total | |
| 1 | 9377 | 79,839 | 89,216 | 849 | 10,669 | 11,518 | 15 | 234 | 249 |
| 2 | 9646 | 81,239 | 90,885 | 872 | 10,814 | 11,686 | 18 | 229 | 247 |
| 3 | 9657 | 81,113 | 90,770 | 840 | 10,771 | 11,611 | 14 | 235 | 249 |
| 4 | 9578 | 81,220 | 90,798 | 869 | 10,820 | 11,689 | 17 | 233 | 250 |
| 5 | 9624 | 81,107 | 90,731 | 834 | 10,749 | 11,583 | 16 | 235 | 251 |
| 6 | 9643 | 81,252 | 90,895 | 847 | 10,833 | 11,680 | 17 | 236 | 253 |
| 7 | 9590 | 81,029 | 90,619 | 829 | 10,797 | 11,626 | 16 | 239 | 255 |
| 8 | 9653 | 81,374 | 90,027 | 839 | 10,800 | 11,639 | 14 | 236 | 250 |
| 9 | 9607 | 81,004 | 90,651 | 844 | 10,773 | 11,617 | 17 | 235 | 252 |
| 10 | 9633 | 81,268 | 90,901 | 843 | 10,812 | 11,655 | 17 | 235 | 252 |
| Total | 96,008 | 810,485 | 906,493 | 8466 | 107,838 | 116,304 | 161 | 2347 | 2508 |
| Average | 9601 | 81,049 | 90,650 | 847 | 10,784 | 11,630 | 16 | 235 | 251 |
| SD | 83 | 439 | 519 | 14 | 48 | 53 | 1 | 3 | 2 |
| Isolate No. | Antifungal Susceptibility * | Survival Rate (%) of Infected G. mellonella | |||||
|---|---|---|---|---|---|---|---|
| FLU | AMB | MFG | 24 h | 48 h | 72 h | 96 h | |
| Serial isolates in this study | |||||||
| 1 | R | S | I | 80.0 | 80.0 | 80.0 | 80.0 |
| 2 | R | S | R | 90.0 | 82.5 | 75.0 | 62.5 |
| 3 | SDD | R | I | 70.0 | 60.0 | 60.0 | 55.0 |
| 4 | R | S | S | 100.0 | 80.0 | 70.0 | 35.0 |
| 5 | SDD | R | R | 97.5 | 90.0 | 80.0 | 77.5 |
| Blood isolates from Korean multicenter surveillance cultures (Mean ± SD) | |||||||
| FR (N=18) | R | S | S | 93.7 ± 14.2 † | 82.6 ± 24.3 † | 64.7 ± 25.7 † | 49.6 ± 24.0 † |
| F-SDD (N=17) | R | S | S | 83.8 ± 6.8 | 61.5 ± 14.0 | 38.4 ± 21.2 | 25.7 ± 25.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, H.J.; Choi, M.J.; Byun, S.A.; Won, E.J.; Park, J.H.; Choi, Y.J.; Choi, H.-J.; Choi, H.-W.; Kee, S.-J.; Kim, S.H.; et al. Whole-Genome Sequence Analysis of Candida glabrata Isolates from a Patient with Persistent Fungemia and Determination of the Molecular Mechanisms of Multidrug Resistance. J. Fungi 2023, 9, 515. https://doi.org/10.3390/jof9050515
Lim HJ, Choi MJ, Byun SA, Won EJ, Park JH, Choi YJ, Choi H-J, Choi H-W, Kee S-J, Kim SH, et al. Whole-Genome Sequence Analysis of Candida glabrata Isolates from a Patient with Persistent Fungemia and Determination of the Molecular Mechanisms of Multidrug Resistance. Journal of Fungi. 2023; 9(5):515. https://doi.org/10.3390/jof9050515
Chicago/Turabian StyleLim, Ha Jin, Min Ji Choi, Seung A. Byun, Eun Jeong Won, Joo Heon Park, Yong Jun Choi, Hyun-Jung Choi, Hyun-Woo Choi, Seung-Jung Kee, Soo Hyun Kim, and et al. 2023. "Whole-Genome Sequence Analysis of Candida glabrata Isolates from a Patient with Persistent Fungemia and Determination of the Molecular Mechanisms of Multidrug Resistance" Journal of Fungi 9, no. 5: 515. https://doi.org/10.3390/jof9050515
APA StyleLim, H. J., Choi, M. J., Byun, S. A., Won, E. J., Park, J. H., Choi, Y. J., Choi, H.-J., Choi, H.-W., Kee, S.-J., Kim, S. H., Shin, M. G., Lee, S. Y., Kim, M.-N., & Shin, J. H. (2023). Whole-Genome Sequence Analysis of Candida glabrata Isolates from a Patient with Persistent Fungemia and Determination of the Molecular Mechanisms of Multidrug Resistance. Journal of Fungi, 9(5), 515. https://doi.org/10.3390/jof9050515






