Optimization of Aspergillus versicolor Culture and Aerosolization in a Murine Model of Inhalational Fungal Exposure
Abstract
1. Introduction
2. Materials and Methods
2.1. Culture of Aspergillus versicolor
2.2. A. versicolor Protein Extract & SDS PAGE Analysis
2.3. Microbial Metabolite Quantification
2.4. Sterigmatocystin Quantification
2.5. Endotoxin Quantification
2.6. Conidia Aerosolization
2.7. Murine Nose-Only Inhalation Exposures
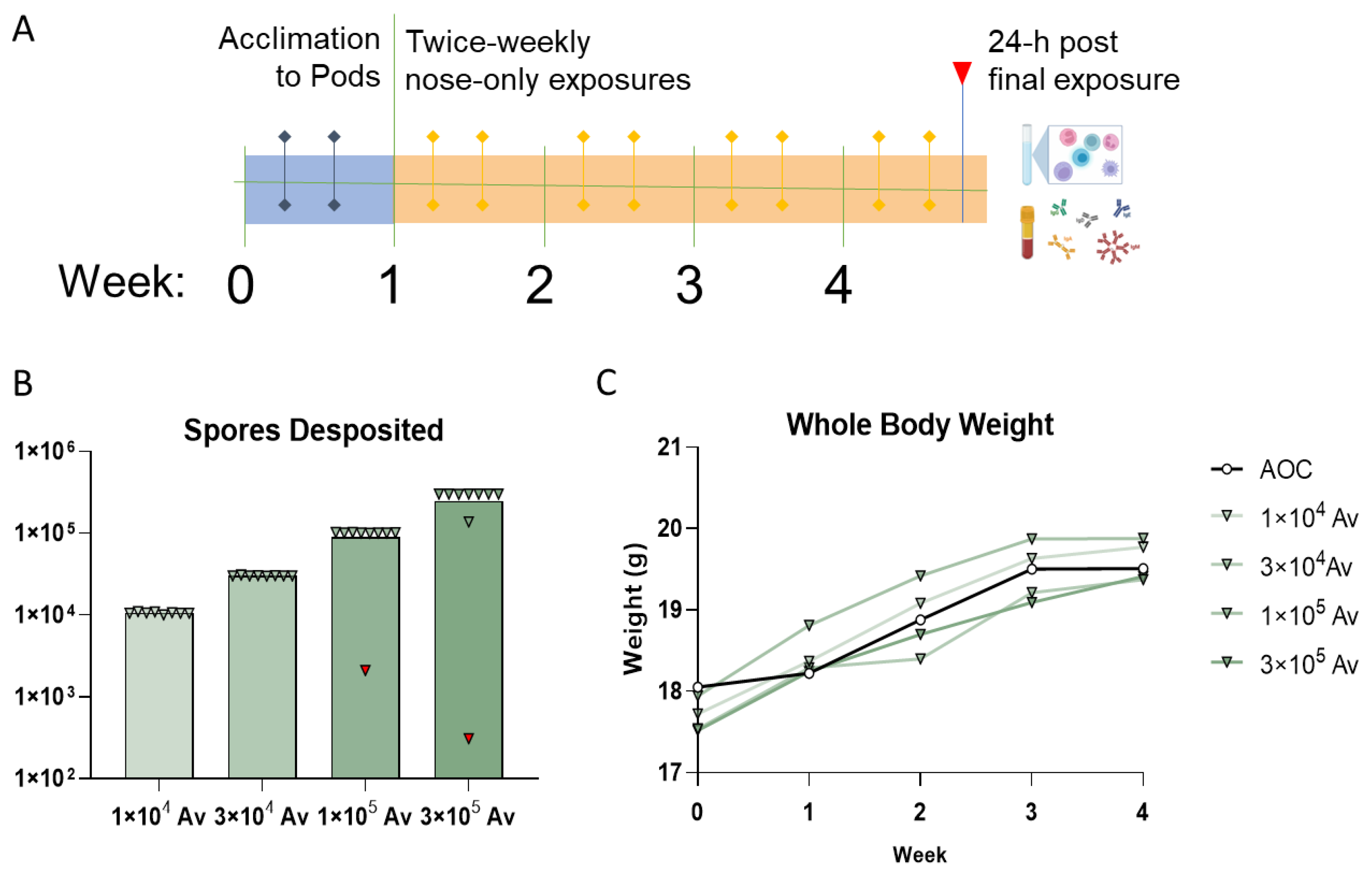
2.7.1. Conidia Deposition Studies
2.7.2. Modified Murine Local Lymph Node Assay (LLNA)
2.7.3. Dosimetry Studies
2.8. Histopathology
2.9. Quantifcation of Conidia in Airway
2.10. Serum Immunoglobulin Quantification
2.11. Flow Cytometry
2.12. Statistics and Data Representation
3. Results
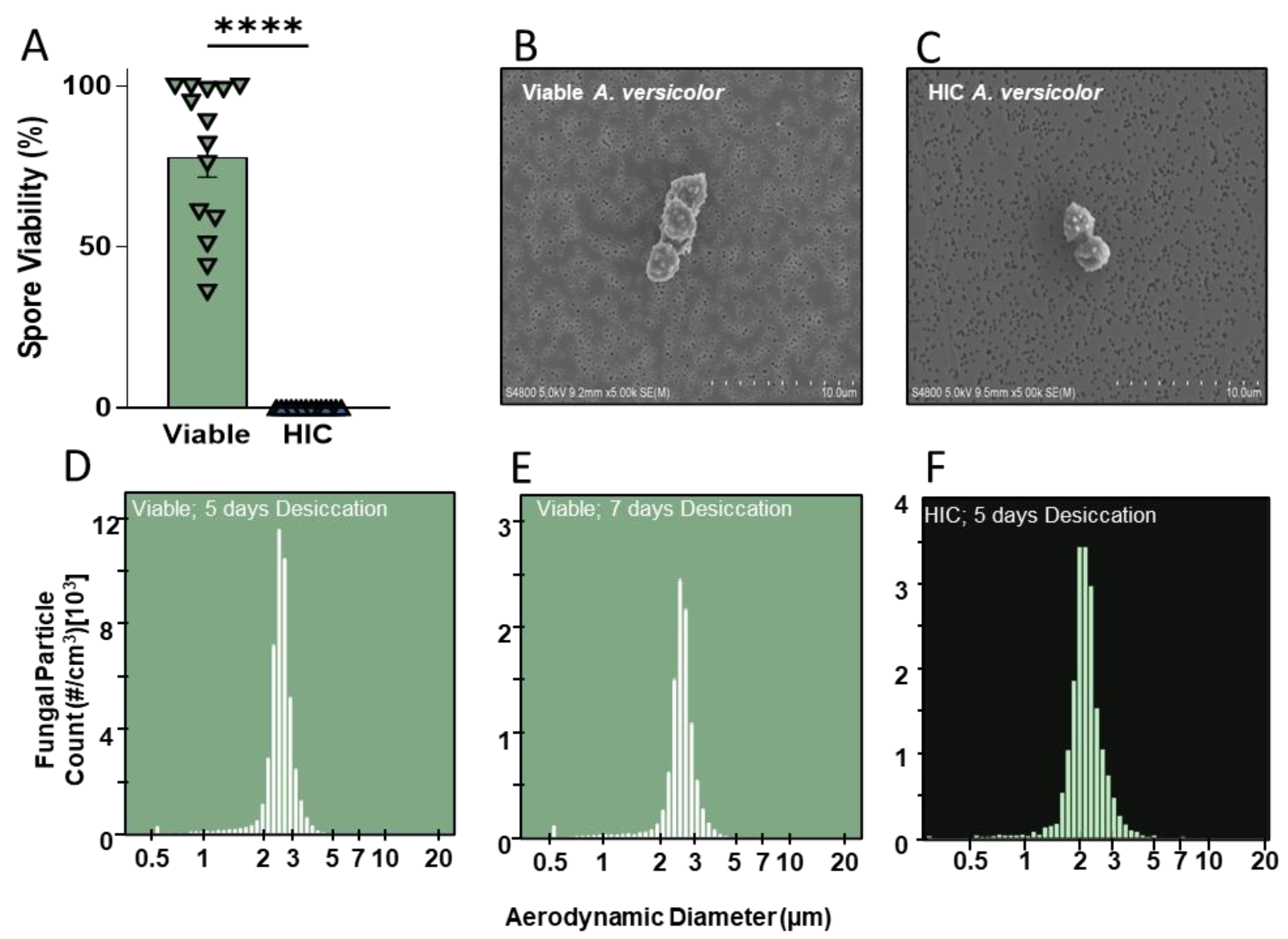
3.1. A. versicolor Culture and Heat-Inactivation
3.2. Aerosolization of Viable and Heat-Inactivated A. versicolor Conidia Using AGS
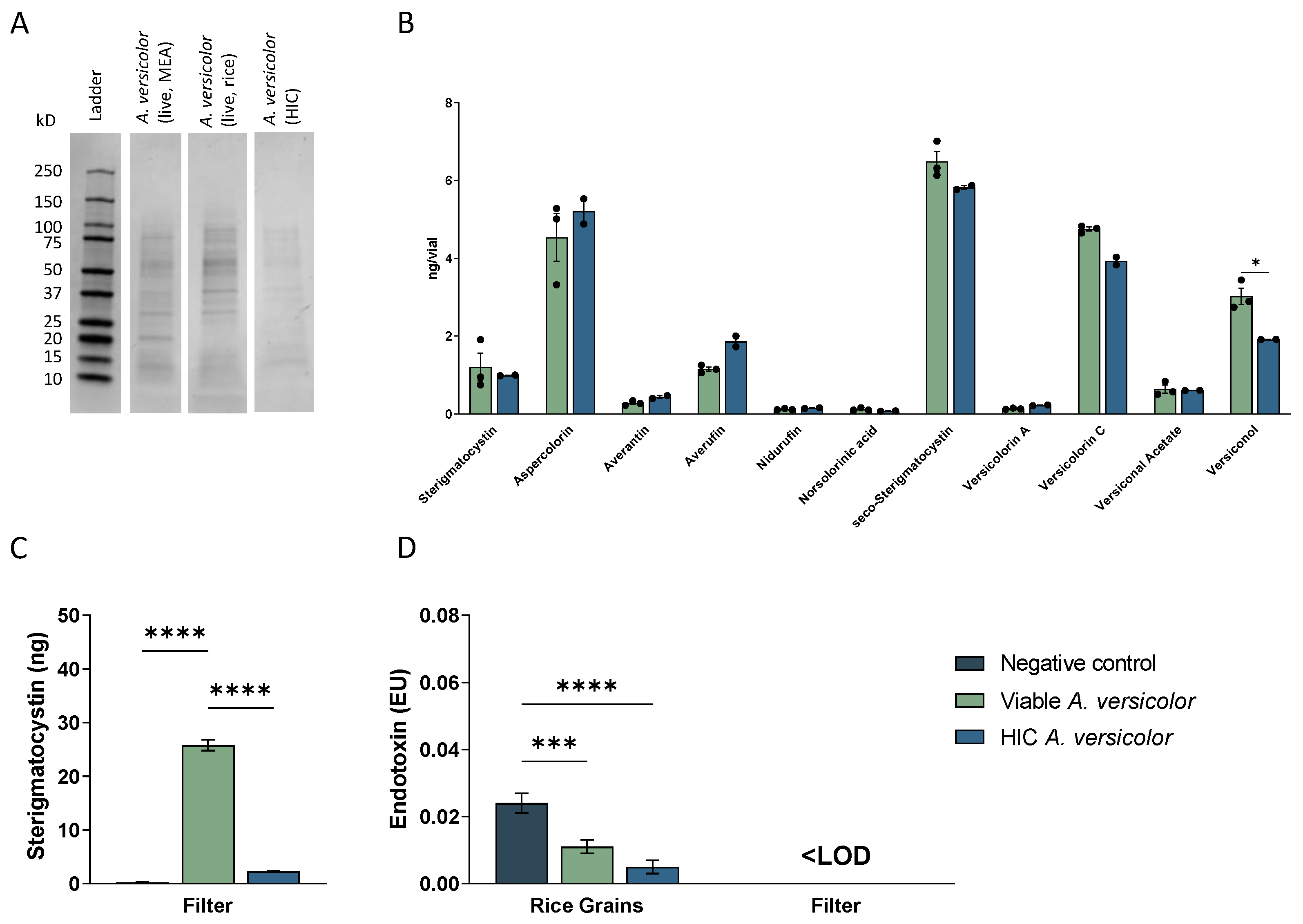
3.3. Viable and Heat-Inactivated Conidia Characterization
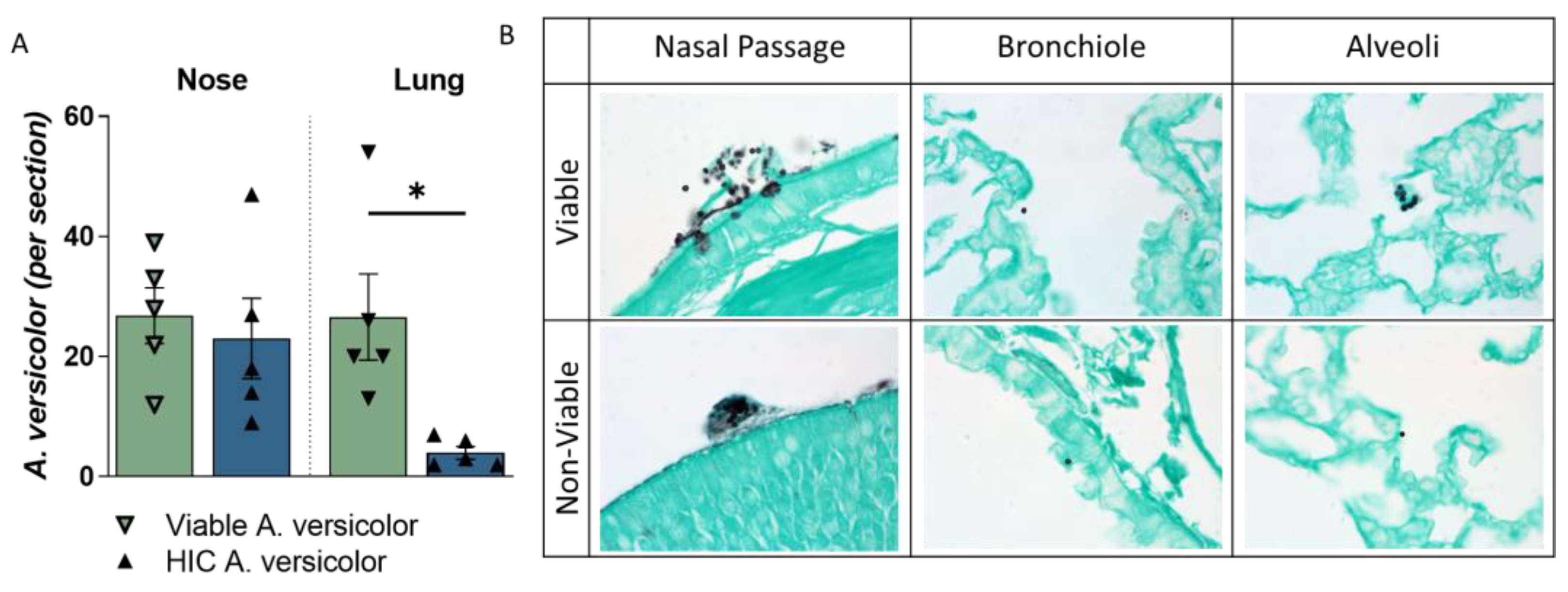
3.4. A. versicolor Conidia Are Deposited into Lung following Nose-Only Exposure
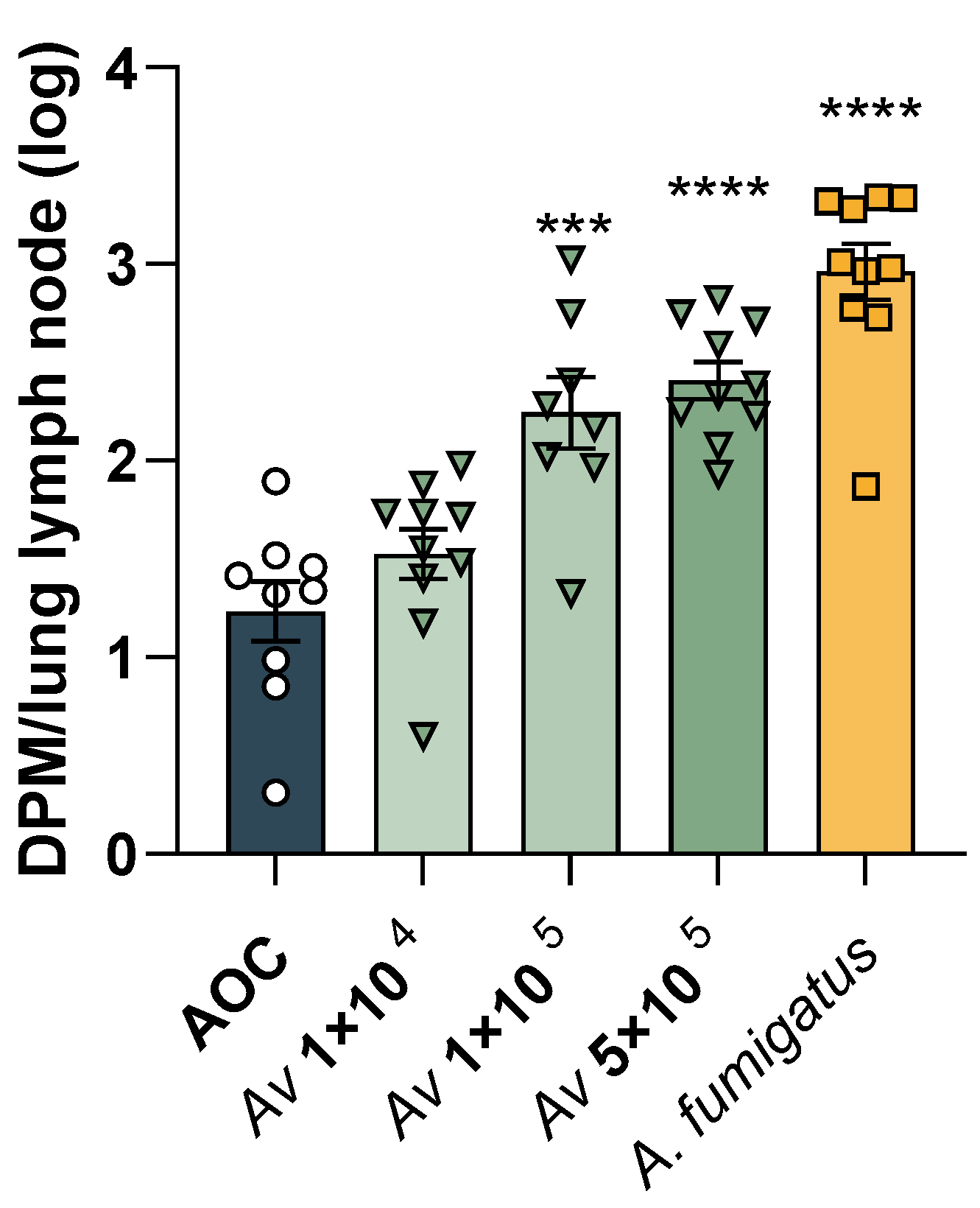
3.5. Identifying the Lymphoproliferative Dose of A. versicolor
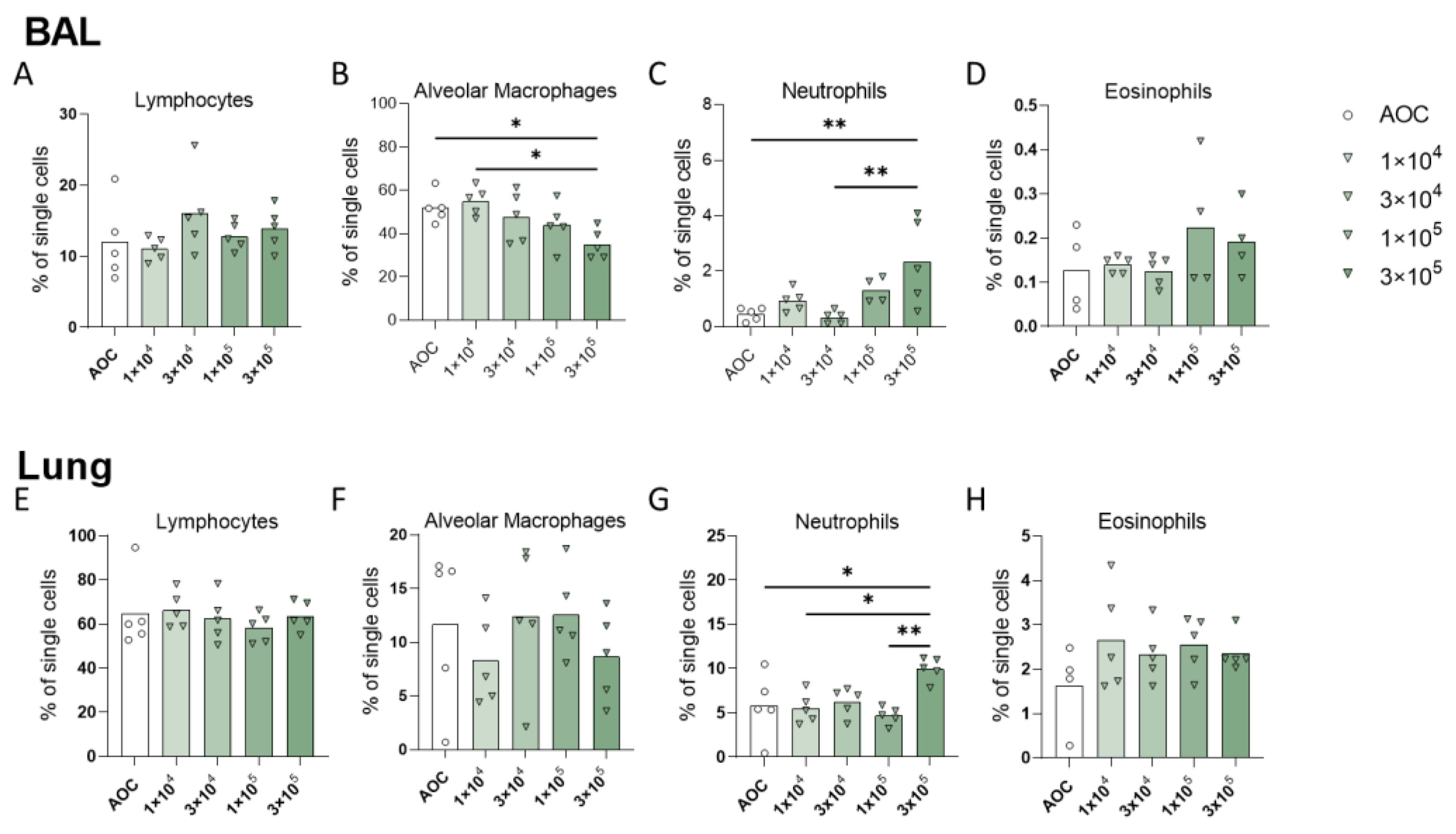
3.6. Repeated Exposure to A. versicolor Conidia
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benedict, K.; Park, B.J. Invasive Fungal Infections after Natural Disasters. Emerg. Infect. Dis. 2014, 20, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Federal Emergency Management Agency. Fact Sheet: Mold: Problems and Solutions; Federal Emergency Management Agency: Washington, DC, USA, 2017.
- Gorny, R.L.; Reponen, T.; Willeke, K.; Schmechel, D.; Robine, E.; Boissier, M.; Grinshpun, S.A. Fungal Fragments as Indoor Air Biocontaminants. Appl. Environ. Microbiol. 2002, 68, 3522–3531. [Google Scholar] [CrossRef] [PubMed]
- Dubey, T. Indoor air pollution due to mycoflora causing acute lower respiratory infections. In The Microbiology of Respiratory System Infections; Elsevier: Amsterdam, The Netherlands, 2016; pp. 95–112. [Google Scholar] [CrossRef]
- Straus, D.C. The Possible Role of Fungal Contamination in Sick Building Syndrome. Front. Biosci. 2011, 3, 562–580. [Google Scholar] [CrossRef] [PubMed]
- Sharpe, R.A.; Bearman, N.; Thornton, C.R.; Husk, K.; Osborne, N.J. Indoor Fungal Diversity and Asthma: A Meta-Analysis and Systematic Review of Risk Factors. J. Allergy Clin. Immunol. 2015, 135, 110–122. [Google Scholar] [CrossRef]
- Mudarri, D.; Fisk, W.J. Public Health and Economic Impact of Dampness and Mold. Indoor Air 2007, 17, 226–235. [Google Scholar] [CrossRef]
- Mudarri, D.H. Valuing the Economic Costs of Allergic Rhinitis, Acute Bronchitis, and Asthma from Exposure to Indoor Dampness and Mold in the US. J. Environ. Public. Health 2016, 2016, 2386596. [Google Scholar] [CrossRef]
- Medrek, S.K.; Kao, C.C.; Yang, D.H.; Hanania, N.A.; Parulekar, A.D. Fungal Sensitization Is Associated with Increased Risk of Life-Threatening Asthma. J. Allergy Clin. Immunol. Pract. 2017, 5, 1025–1031. [Google Scholar] [CrossRef]
- Mejía-Santos, H.; Montoya, S.; Chacón-Fuentes, R.; Zielinski-Gutierrez, E.; Lopez, B.; Ning, M.F.; Farach, N.; García-Coto, F.; Rodríguez-Araujo, D.S.; Rosales-Pavón, K.; et al. Mucormycosis Cases during the COVID-19 Pandemic; US Department of Health and Human Services, Centers for Disease Control and Prevention, Ed.; Morbidity and Mortality Weekly Report; Federal Government Organization: Washington, DC, USA, 2021.
- Portnoy, J.M.; Jara, D. Mold Allergy Revisited. Ann. Allergy Asthma Immunol. 2015, 114, 83–89. [Google Scholar] [CrossRef]
- Fakunle, A.G.; Jafta, N.; Naidoo, R.N.; Smit, L.A.M. Association of Indoor Microbial Aerosols with Respiratory Symptoms among under-Five Children: A Systematic Review and Meta-Analysis. Environ. Health 2021, 20, 77. [Google Scholar] [CrossRef]
- Fukutomi, Y.; Taniguchi, M. Sensitization to Fungal Allergens: Resolved and Unresolved Issues. Allergol. Int. 2015, 64, 321–331. [Google Scholar] [CrossRef]
- Abdel-Azeem, A.M.; Salem, F.M.; Abdel-Azeem, M.A.; Nafady, N.A.; Mohesien, M.T.; Soliman, E.A. Biodiversity of the Genus Aspergillus in Different Habitats. In New and Future Developments in Microbial Biotechnology and Bioengineering; Elsevier: Amsterdam, The Netherlands, 2016; pp. 3–28. [Google Scholar] [CrossRef]
- Jussila, J.; Komulainen, H.; Kosma, V.M.; Nevalainen, A.; Pelkonen, J.; Hirvonen, M.R. Spores of Aspergillus Versicolor Isolated from Indoor Air of a Moisture-Damaged Building Provoke Acute Inflammation in Mouse Lungs. Inhal. Toxicol. 2002, 14, 1261–1277. [Google Scholar] [CrossRef]
- Mousavi, B.; Hedayati, M.T.; Hedayati, N.; Ilkit, M.; Syedmousavi, S. Aspergillus Species in Indoor Environments and Their Possible Occupational and Public Health Hazards. Curr. Med. Mycol. 2016, 2, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, A. Role of Aspergillus in Bioremediation Process. In New and Future Developments in Microbial Biotechnology and Bioengineering; Elsevier: Amsterdam, The Netherlands, 2016; pp. 209–214. [Google Scholar] [CrossRef]
- Pasanen, P.; Korpi, A.; Kalliokoski, P.; Pasanen, A.-L. Growth and Volatile Metabolite Production of Aspergillus Versicolor in House Dust. Environ. Int. 1997, 23, 425–432. [Google Scholar] [CrossRef]
- Raksha; Singh, G.; Urhekar, A.D. Virulence Factors Detection in Aspergillus Isolates from Clinical and Environmental Samples. J. Clin. Diagn. Res. 2017, 11, DC13–DC18. [Google Scholar] [CrossRef] [PubMed]
- Eduard, W. Fungal Spores: A Critical Review of the Toxicological and Epidemiological Evidence as a Basis for Occupational Exposure Limit Setting. Crit. Rev. Toxicol. 2009, 39, 799–864. [Google Scholar] [CrossRef] [PubMed]
- Korpi, A.; Kasanen, J.-P.; Raunio, P.; Pasanen, A.-L. Acute Effects of Aspergillus Versicolor Aerosols on Murine Airways. Indoor Air 2003, 13, 260–265. [Google Scholar]
- Libert, X.; Chasseur, C.; Bladt, S.; Packeu, A.; Bureau, F.; Roosens, N.H.; De Keersmaecker, S.C. Development and Performance Assessment of a Qualitative SYBR(R) Green Real-Time PCR Assay for the Detection of Aspergillus Versicolor in Indoor Air. Appl. Microbiol. Biotechnol. 2015, 99, 7267–7282. [Google Scholar] [CrossRef][Green Version]
- Luo, X.-W.; Lu, H.-M.; Chen, X.-Q.; Zhou, X.-F.; Gao, C.-H.; Liu, Y.-H. Secondary Metabolites and Their Biological Activities from the Sponge Derived Fungus Aspergillus Versicolor. Chem. Nat. Compd. 2020, 56, 716–719. [Google Scholar] [CrossRef]
- Buskirk, A.D.; Green, B.J.; Lemons, A.R.; Nayak, A.P.; Goldsmith, W.T.; Kashon, M.L.; Anderson, S.E.; Hettick, J.M.; Templeton, S.P.; Germolec, D.R.; et al. A Murine Inhalation Model to Characterize Pulmonary Exposure to Dry Aspergillus Fumigatus Conidia. PLoS ONE 2014, 9, e109855. [Google Scholar] [CrossRef]
- Buskirk, A.D.; Templeton, S.P.; Nayak, A.P.; Hettick, J.M.; Law, B.F.; Green, B.J.; Beezhold, D.H. Pulmonary Immune Responses to Aspergillus Fumigatus in an Immunocompetent Mouse Model of Repeated Exposures. J. Immunotoxicol. 2014, 11, 180–189. [Google Scholar] [CrossRef]
- Croston, T.L.; Lemons, A.R.; Barnes, M.A.; Goldsmith, W.T.; Orandle, M.S.; Nayak, A.P.; Germolec, D.R.; Green, B.J.; Beezhold, D.H. Inhalation of Stachybotrys CHARTARUM Fragments Induces Pulmonary Arterial Remodeling. Am. J. Respir. Cell Mol. Biol. 2020, 62, 563–576. [Google Scholar] [CrossRef] [PubMed]
- Croston, T.L.; Nayak, A.P.; Lemons, A.R.; Goldsmith, W.T.; Gu, J.K.; Germolec, D.R.; Beezhold, D.H.; Green, B.J. Influence of Aspergillus Fumigatus Conidia Viability on Murine Pulmonary microRNA and mRNA Expression Following Subchronic Inhalation Exposure. Clin. Exp. Allergy 2016, 46, 1315–1327. [Google Scholar] [CrossRef] [PubMed]
- Lemons, A.R.; Croston, T.L.; Goldsmith, W.T.; Barnes, M.A.; Jaderson, M.A.; Park, J.-H.; McKinney, W.; Beezhold, D.H.; Green, B.J. Cultivation and Aerosolization of Stachybotrys Chartarum for Modeling Pulmonary Inhalation Exposure. Inhal. Toxicol. 2019, 31, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Nayak, A.P.; Green, B.J.; Lemons, A.R.; Marshall, N.B.; Goldsmith, W.T.; Kashon, M.L.; Anderson, S.E.; Germolec, D.R.; Beezhold, D.H. Subchronic Exposures to Fungal Bioaerosols Promotes Allergic Pulmonary Inflammation in Naive Mice. Clin. Exp. Allergy 2016, 46, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Pestka, J.J.; Yike, I.; Dearborn, D.G.; Ward, M.D.; Harkema, J.R. Stachybotrys Chartarum, Trichothecene Mycotoxins, and Damp Building-Related Illness: New Insights into a Public Health Enigma. Toxicol. Sci. 2008, 104, 4–26. [Google Scholar] [CrossRef]
- Milton, D.K.; Feldman, H.A.; Neuberg, D.S.; Bruckner, R.J.; Greaves, I.A. Environmental Endotoxin Measurement: The Kinetic Limulus Assay with Resistant-Parallel-Line Estimation. Environ. Res. 1992, 57, 212–230. [Google Scholar] [CrossRef]
- Weyel, D.A.; Ellakkani, M.; Alarie, Y.; Karol, M. An Aerosol Generator for the Resuspension of Cotton Dust. Toxicolgy Appl. Pharmacol. 1984, 76, 544–547. [Google Scholar] [CrossRef]
- Vincent, C.; Robinson, V.A.; Frazer, D.G. Pulmonary Reactions to Organic Dust Exposures: Development of an Animal Model. Environ. Health Perspect. 1996, 104, 41–53. [Google Scholar]
- Crissman, J.W.; Goodman, D.G.; Hildebrandt, P.K.; Maronpot, R.R.; Prater, D.A.; Riley, J.H.; Seaman, W.J.; Thake, D.C. Best practices guideline: Toxicologic histopathology. Toxicol. Pathol. 2004, 32, 126–131. [Google Scholar] [CrossRef]
- Aleksic, B.; Draghi, M.; Ritoux, S.; Bailly, S.; Lacroix, M.; Oswald, I.P.; Bailly, J.D.; Robine, E. Aerosolization of Mycotoxins after Growth of Toxinogenic Fungi on Wallpaper. Appl. Environ. Microbiol. 2017, 83, e01001-17. [Google Scholar] [CrossRef]
- Madsen, A.M.; Larsen, S.T.; Koponen, I.K.; Kling, K.I.; Barooni, A.; Karottki, D.G.; Tendal, K.; Wolkoff, P. Generation and Characterization of Indoor Fungal Aerosols for Inhalation Studies. Appl. Environ. Microbiol. 2016, 82, 2479–2493. [Google Scholar] [CrossRef] [PubMed]
- Murtoniemi, T.; Penttinen, P.; Nevalainen, A.; Hirvonen, M.R. Effects of Microbial Cocultivation on Inflammatory and Cytotoxic Potential of Spores. Inhal. Toxicol. 2005, 17, 681–693. [Google Scholar] [CrossRef]
- Reijula, K.; Tuomi, T. Mycotoxins of aspergilli: Exposure and Health Effects. Front. Biosci. A J. Virtual Libr. 2003, 8, s232–s235. [Google Scholar] [CrossRef][Green Version]
- Wuthrich, M.; Deepe, G.S., Jr.; Klein, B. Adaptive Immunity to Fungi. Annu. Rev. Immunol. 2012, 30, 115–148. [Google Scholar] [CrossRef] [PubMed]
- Man, W.H.; de Steenhuijsen Piters, W.A.; Bogaert, D. The Microbiota of the Respiratory Tract: Gatekeeper to Respiratory Health. Nat. Rev. Microbiol. 2017, 15, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Mensah-Attipoe, J.; Saari, S.; Veijalainen, A.M.; Pasanen, P.; Keskinen, J.; Leskinen, J.T.T.; Reponen, T. Release and Characteristics of Fungal Fragments in Various Conditions. Sci. Total Environ. 2016, 547, 234–243. [Google Scholar] [CrossRef]
- Oya, E.; Afanou, A.K.J.; Malla, N.; Uhlig, S.; Rolen, E.; Skaar, I.; Straumfors, A.; Winberg, J.O.; Bang, B.E.; Schwarze, P.E.; et al. Characterization and Pro-Inflammatory Responses of Spore And hyphae Samples from Various Mold Species. Indoor Air 2018, 28, 28–39. [Google Scholar] [CrossRef]
- Pei, R.; Gunsch, C.K. Inflammatory Cytokine Gene Expression in THP-1 Cells Exposed to Stachybotrys Chartarum and Aspergillus Versicolor. Environ. Toxicol. 2013, 28, 51–60. [Google Scholar] [CrossRef]
- Doran, E.; Cai, F.; Holweg, C.T.J.; Wong, K.; Brumm, J.; Arron, J.R. Interleukin-13 in Asthma and Other Eosinophilic Disorders. Front. Med. 2017, 4, 139. [Google Scholar] [CrossRef]
- Hahn, C.; Teufel, M.; Herz, U.; Renz, H.; Erb, K.J.; Wohlleben, G.; Brocker, E.B.; Duschl, A.; Sebald, W.; Grunewald, S.M. Inhibition of the IL-4/IL-13 Receptor System Prevents Allergic Sensitization without Affecting Established Allergy in a Mouse Model for Allergic Asthma. J. Allergy Clin. Immunol. 2003, 111, 1361–1369. [Google Scholar] [CrossRef]
- Tojima, I.; Kouzaki, H.; Shimizu, S.; Ogawa, T.; Arikata, M.; Kita, H.; Shimizu, T. Group 2 Innate Lymphoid Cells are Increased in Nasal Polyps in Patients with Eosinophilic Chronic Rhinosinusitis. Clin. Immunol. 2016, 170, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bartemes, K.R.; Kita, H. Innate and Adaptive Immune Responses to Fungi in the Airway. J. Allergy Clin. Immunol. 2018, 142, 353–363. [Google Scholar] [CrossRef]
- Baxi, S.N.; Sheehan, W.J.; Sordillo, J.E.; Muilenberg, M.L.; Rogers, C.A.; Gaffin, J.M.; Permaul, P.; Lai, P.S.; Louisias, M.; Petty, C.R.; et al. Association between Fungal Spore Exposure in Inner-City Schools and Asthma Morbidity. Ann. Allergy Asthma Immunol. 2019, 122, 610–615.e1. [Google Scholar] [CrossRef] [PubMed]
- Black, P.; Udy, A.; Brodie, S. Sensitivity to Fungal Allergens is a Risk Factor for Life-Threatening Asthma. Allergy 2000, 55, 501–504. [Google Scholar] [CrossRef] [PubMed]
- Burge, H.A. An Update on Pollen and Fungal Spore Aerobiology. J. Allergy Clin. Immunol. 2002, 110, 544–552. [Google Scholar] [CrossRef] [PubMed]
- Stebegg, M.; Kumar, S.D.; Silva-Cayetano, A.; Fonseca, V.R.; Linterman, M.A.; Graca, L. Regulation of the Germinal Center Response. Front. Immunol. 2018, 9, 2469. [Google Scholar] [CrossRef]
- Ota, M.; Hoehn, K.B.; Ota, T.; Aranda, C.J.; Friedman, S.; Braga, W.F.; Malbari, A.; Kleinstein, S.H.; Sicherer, S.H.; Curotto de Lafaille, M.A. The Memory of Pathogenic Ige Is Contained within Cd23 (+) Igg1 (+) Memory B Cells Poised to Switch to Ige in Food Allergy. bioRxiv 2023, 1, 1–28. [Google Scholar] [CrossRef]
- Barnes, C.; Buckley, S.; Pacheco, F.; Portnoy, J. Ige-Reactive Proteins from Stachybotrys Chartarum. Ann. Allergy Asthma Immunol. 2001, 89, 29–33. [Google Scholar]
- Green, B.J.; Tovey, E.R.; Sercombe, J.K.; Blachere, F.M.; Beezhold, D.H.; Schmechel, D. Airborne Fungal Fragments and Allergenicity. Med. Mycol. 2006, 44 (Suppl. 1), S245–S255. [Google Scholar] [CrossRef]
- Eckl-Dorna, J.; Villazala-Merino, S.; Linhart, B.; Karaulov, A.V.; Zhernov, Y.; Khaitov, M.; Niederberger-Leppin, V.; Valenta, R. Allergen-Specific Antibodies Regulate Secondary Allergen-Specific Immune Responses. Front. Immunol. 2018, 9, 3131. [Google Scholar] [CrossRef]
- Chatila, T.A. Interleukin-4 Receptor Signaling Pathways in Asthma Pathogenesis. Trends Mol. Med. 2004, 10, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Panda, S.K.; Colonna, M. Innate Lymphoid Cells in Mucosal Immunity. Front. Immunol. 2019, 10, 861. [Google Scholar] [CrossRef] [PubMed]
- Poposki, J.A.; Klingler, A.I.; Tan, B.K.; Soroosh, P.; Banie, H.; Lewis, G.; Hulse, K.E.; Stevens, W.W.; Peters, A.T.; Grammer, L.C.; et al. Group 2 Innate Lymphoid Cells Are Elevated and Activated in Chronic Rhinosinusitis with Nasal Polyps. Immun. Inflamm. Dis. 2017, 5, 233–243. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blackwood, C.B.; Croston, T.L.; Barnes, M.A.; Lemons, A.R.; Rush, R.E.; Goldsmith, T.; McKinney, W.G.; Anderson, S.; Weaver, K.L.; Sulyok, M.; et al. Optimization of Aspergillus versicolor Culture and Aerosolization in a Murine Model of Inhalational Fungal Exposure. J. Fungi 2023, 9, 1090. https://doi.org/10.3390/jof9111090
Blackwood CB, Croston TL, Barnes MA, Lemons AR, Rush RE, Goldsmith T, McKinney WG, Anderson S, Weaver KL, Sulyok M, et al. Optimization of Aspergillus versicolor Culture and Aerosolization in a Murine Model of Inhalational Fungal Exposure. Journal of Fungi. 2023; 9(11):1090. https://doi.org/10.3390/jof9111090
Chicago/Turabian StyleBlackwood, Catherine B., Tara L. Croston, Mark A. Barnes, Angela R. Lemons, Rachael E. Rush, Travis Goldsmith, Walter G. McKinney, Stacey Anderson, Kelly L. Weaver, Michael Sulyok, and et al. 2023. "Optimization of Aspergillus versicolor Culture and Aerosolization in a Murine Model of Inhalational Fungal Exposure" Journal of Fungi 9, no. 11: 1090. https://doi.org/10.3390/jof9111090
APA StyleBlackwood, C. B., Croston, T. L., Barnes, M. A., Lemons, A. R., Rush, R. E., Goldsmith, T., McKinney, W. G., Anderson, S., Weaver, K. L., Sulyok, M., Park, J.-H., Germolec, D., Beezhold, D. H., & Green, B. (2023). Optimization of Aspergillus versicolor Culture and Aerosolization in a Murine Model of Inhalational Fungal Exposure. Journal of Fungi, 9(11), 1090. https://doi.org/10.3390/jof9111090






