Cryptococcosis in Colombia: Analysis of Data from Laboratory-Based Surveillance 2017–2024
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Case Definition
2.3. Epidemiological Analysis
2.4. Laboratory Tests, Antifungal Susceptibility Testing and Molecular Typing
2.5. Patients Living with HIV Versus HIV-Negative Patients
2.6. Ethical Considerations
2.7. Statistical Analysis
3. Results
3.1. Survey Data
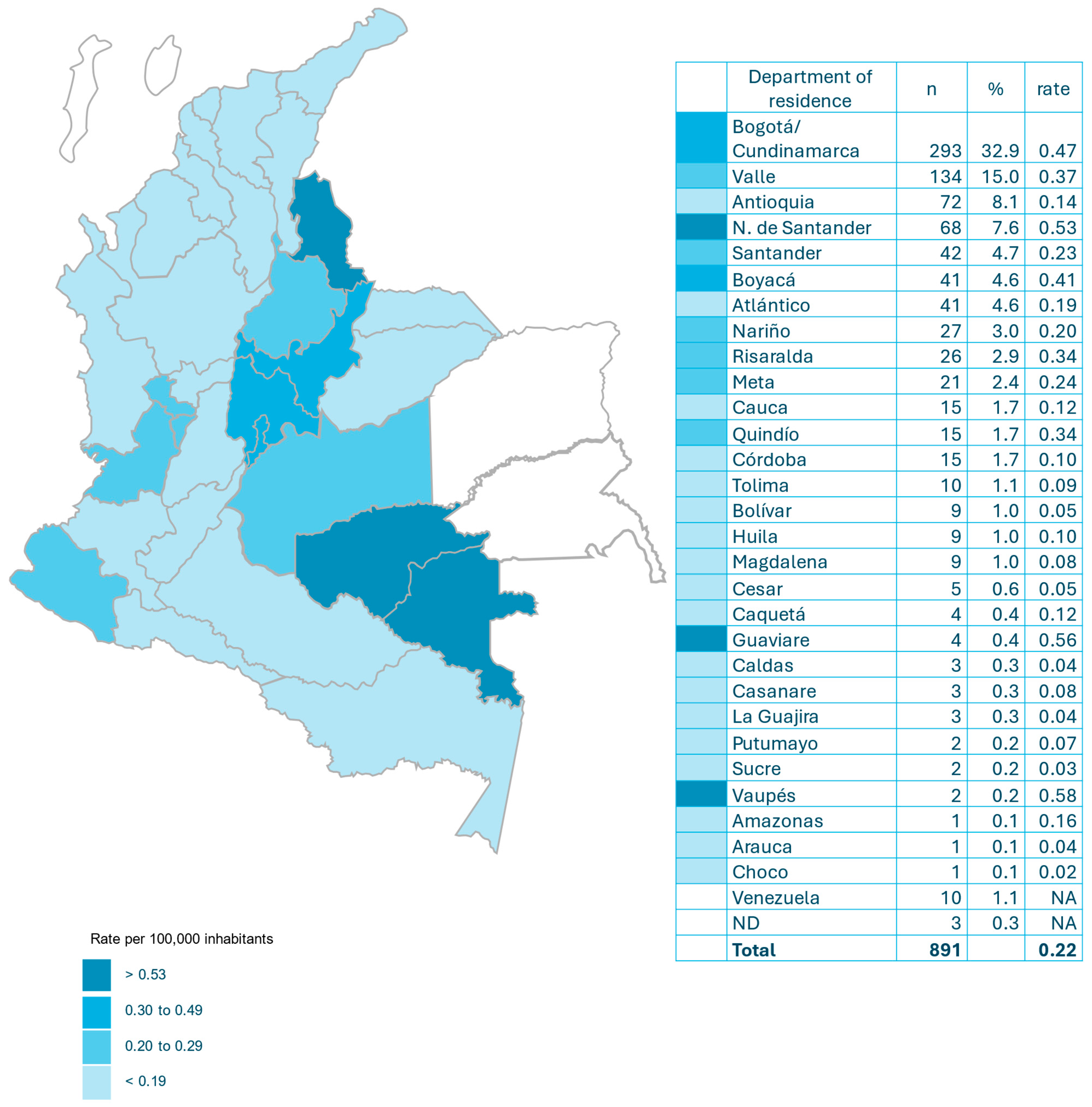
3.2. Incidence
3.3. Demographic Characteristics
3.4. Risk Factors
3.5. Clinical Manifestations
3.6. Diagnostic Images
3.7. Treatment
3.8. Mortality and Relapses
3.9. Mycological Diagnosis of Cryptococcosis
3.10. Antifungal Susceptibility
3.11. Characteristics in Patients Living with HIV and HIV-Negative Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Fungal Priority Pathogens List to Guide Research, Development and Public Health Action; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Rajasingham, R.; Govender, N.P.; Jordan, A.; Loyse, A.; Shroufi, A.; Denning, D.W.; Meya, D.B.; Chiller, T.M.; Boulware, D.R. The global burden of HIV-associated cryptococcal infection in adults in 2020: A modelling analysis. Lancet Infect. Dis. 2022, 22, 1748–1755. [Google Scholar] [CrossRef]
- George, I.A.; Spec, A.; Powderly, W.G.; Santos, C.A.Q. Comparative epidemiology and outcomes of Human Immunodeficiency Virus (HIV), non-HIV non-transplant, and solid organ transplant associated Cryptococcosis: A population-based study. Clin. Infect. Dis. 2018, 66, 608–611. [Google Scholar] [CrossRef]
- Paccoud, O.; Desnos-Ollivier, M.; Cassaing, S.; Boukris-Sitbon, K.; Alanio, A.; Bellanger, A.P.; Bonnal, C.; Bonhomme, J.; Botterel, F.; Bougnoux, M.E.; et al. Cryptococcus neoformans infections differ among Human Immunodeficiency Virus (HIV)-seropositive and HIV-seronegative individuals: Results from a nationwide surveillance program in France. Open Forum Infect. Dis. 2023, 11, ofad658. [Google Scholar] [CrossRef]
- Namie, H.; Takazono, T.; Hidaka, Y.; Morimoto, S.; Ito, Y.; Nakada, N.; Ashizawa, N.; Hirayama, T.; Takeda, K.; Iwanaga, N.; et al. The prognostic factors for cryptococcal meningitis in non-human immunodeficiency virus patients: An observational study using nationwide database. Mycoses 2024, 67, e13658. [Google Scholar] [CrossRef]
- Coussement, J.; Heath, C.H.; Roberts, M.B.; Lane, R.J.; Spelman, T.; Smibert, O.C.; Longhitano, A.; Morrisey, O.; Nield, B.; Tripathy, M.; et al. Current epidemiology and clinical features of Cryptococcus infection in patients without Human Immunodeficiency Virus: A multicenter study in 46 hospitals in Australia and New Zealand. Clin. Infect. Dis. 2023, 77, 976–986. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, T.G.; Castañeda, E.; Nielsen, K.; Wanke, B.; Lazéra, M.S. Environmental niches for Cryptococcus neoformans and Cryptococcus gattii. In Cryptococcus: From Human Pathogen to Model Yeast; Heitman, J., Kozel, T.R., Kyung, J., Kwon-Chung, J.R., Perfect, A.C., Eds.; American Society for Microbiology Press: Washington, DC, USA, 2011; pp. 235–259. ISBN 9781119737858. [Google Scholar] [CrossRef]
- Baddley, J.W.; Chen, S.C.; Huisingh, C.; Benedict, K.; DeBess, E.E.; Galanis, E.; Jackson, B.R.; MacDougall, R.; Marsdden-Haug, N.; Oletan, H.; et al. MSG07: An international cohort study comparing epidemiology and outcomes of patients with Cryptococcus neoformans or Cryptococcus gattii infections. Clin. Infect. Dis. 2021, 73, 1133–1141. [Google Scholar] [CrossRef]
- Lahiri, S.; Manjunath, N.; Bhat, M.; Hagen, F.; Bahubali, V.H.; Palaniappan, M.; Maji, S.; Chandrashekar, N. Clinical insights and epidemiology of central nervous system infection due to Cryptococcus neoformans/gattii species complexes: A prospective study from South India. Med. Mycol. 2020, 58, 600–608. [Google Scholar] [CrossRef]
- Escandón, P.; Lizarazo, J.; Agudelo, C.I.; Castañeda, E. Cryptococcosis in Colombia: Compilation and analysis of data from laboratory-based surveillance. J. Fungi 2018, 4, 32. [Google Scholar] [CrossRef] [PubMed]
- Chuang, Y.M.; Ho, Y.C.; Chang, H.T.; Yu, C.J.; Yang, P.C.; Hsueh, P.R. Disseminated cryptococcosis in HIV-uninfected patients. Eur. J. Clin. Microbiol. Infect. Dis. 2008, 27, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Departamento Administrativo Nacional de Estadística. Available online: https://www.dane.gov.co/index.php/estadisticas-por-tema/demografia-y-poblacion/proyecciones-de-poblacion (accessed on 5 July 2025).
- Cuenta de Alto Costo (CAC), Fondo Colombiano de Enfermedades de Alto Costo. Situación del VIH en Colombia 2024; Cuenta de Alto Costo: Bogotá, Colombia, 2005.
- Castañeda, E.; Lizarazo, J. Protocolo de estudio y manejo de los pacientes con criptococosis. Infectio 2012, 16, 123–125. [Google Scholar] [CrossRef][Green Version]
- Kwon-Chung, J.; Polacheck, I.T.; Bennet, J.E. Improved diagnostic medium for separation of Cryptococcus neoformans var. neoformans (serotypes A and D) and Cryptococcus neoformans var. gattii (serotypes B and C). J. Clin. Microbiol. 1982, 5, 535–537. [Google Scholar] [CrossRef]
- CLSI M57S; Principles and Procedures for the Development of Epidemiological Cutoff Values for Antifungal Susceptibility Testing. Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2022.
- Espinel-Ingroff, A.; Aller, A.I.; Canton, E.; Castanon-Olivares, L.R.; Chowdhary, A.; Cordoba, S.; Cuenca-Estrella, M.; Fothergill, A.; Fuller, J.; Govender, N.; et al. Cryptococcus neoformans-Cryptococcus gattii species complex: An international study of wild-type susceptibility endpoint distributions and epidemiological cutoff values for fluconazole, itraconazole, posaconazole, and voriconazole. Antimicrob. Agents Chemother. 2012, 56, 5898–5906. [Google Scholar] [CrossRef]
- Espinel-Ingroff, A.; Chowdhary, A.; Cuenca-Estrella, M.; Fothergill, A.; Fuller, J.; Hagen, F.; Govender, N.; Guarro, J.; Johnson, E.; Lass-Flörl, C.; et al. Cryptococcus neoformans-Cryptococcus gattii species complex: An international study of wild-type susceptibility endpoint distributions and epidemiological cutoff values for amphotericin B and flucytosine. Antimicrob. Agents Chemother. 2012, 56, 3107–3113. [Google Scholar] [CrossRef]
- Escandón, P.; Sánchez, A.; Martínez, M.; Meyer, W.; Castañeda, E. Molecular epidemiology of clinical and environmental isolates of the Cryptococcus neoformans species complex reveals a high genetic diversity and the presence of the molecular type VGII mating type a in Colombia. FEMS Yeast Res. 2006, 6, 625–635. [Google Scholar] [CrossRef]
- Casali, A.K.; Goulart, L.; Rosa e Silva, L.K.; Ribeiro, A.M.; Amaral, A.A.; Alves, S.H.; Schrank, A.; Meyer, W.; Vainstein, M.H. Molecular typing of clinical and environmental Cryptococcus neoformans isolates in the Brazilian state Rio Grande do Soul. FEMS Yeast Res. 2003, 3, 405–415. [Google Scholar] [CrossRef]
- Dean, A.G.; Sullivan, K.M.; Soe, M.M. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Versión 3.01. Available online: www.OpenEpi.com (accessed on 20 November 2025).
- Doocy, S.; Page, K.R.; Liu, C.; Hoaglund, H.; Rodríguez, D.C. Venezuela: Out of the headlines but still in crisis. Bull. World Health Organ. 2022, 100, 466–466A. [Google Scholar] [CrossRef]
- Denning, D.W. Global incidence and mortality of severe fungal disease. Lancet Infect. Dis. 2024, 24, e428–e438. [Google Scholar] [CrossRef] [PubMed]
- Bitar, D.; Lortholary, O.; Le Strat, Y.; Nicolau, J.; Coignard, B.; Tattevin, P.; Che, D.; Dromer, F. Population-based analysis of invasive fungal infections, France, 2001–2010. Emerg. Infect. Dis. 2014, 20, 1149–1155. [Google Scholar] [CrossRef]
- Gangneux, J.P.; Bougnoux, M.; Hennequin, C.; Godet, C.; Chandenier, J.; Denning, D.W.; Dupont, B. LIFE program, the Société française de mycologie médicale SFMM-study group. An estimation of burden of serious fungal infections in France. J. Mycol. Med. 2016, 26, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Dos Reis, D.S.; de Brito, M.T.; Guimarães, R.J.; Quaresma, J.A. Cryptococcosis: Identification of risk areas in the Brazilian Amazon. Microorganisms 2022, 10, 1411. [Google Scholar] [CrossRef] [PubMed]
- Milburn, J.; Ntwayagae, O.; Suresh, R.; Ngoni, K.; Northcott, C.; Penney, J.; Kinsella, M.; Mechie, I.; Ensor, S.; Thamae, G.; et al. Tracking cryptococcal meningitis to monitor HIV program success during the treat all era: An analysis of national data in Botswana. Clin. Infect. Dis. 2024, 79, 462–468. [Google Scholar] [CrossRef]
- Guan, S.T.; Huang, Y.S.; Huang, S.T.; Hsiao, F.Y.; Chen, Y.C. The incidences and clinical outcomes of cryptococcosis in Taiwan: A nationwide, population-based study, 2002-2015. Med. Mycol. 2024, 62, myad125. [Google Scholar] [CrossRef]
- Stelzle, D.; Rangaraj, A.; Jarvis, J.N.; Razakasoa, N.H.; Perrin, G.; Low-Beer, D.; Doherty, M.; Ford, N.; Dalal, S. Prevalence of advanced HIV disease in sub-Saharan Africa: A multi-country analysis of nationally representative household surveys. Lancet Glob. Health 2025, 13, e437–e446. [Google Scholar] [CrossRef]
- Alemayehu, T.; Ayalew, S.; Buzayehu, T.; Daka, D. Magnitude of Cryptococcosis among HIV patients in sub-Saharan Africa countries: A systematic review and meta-analysis. Afr. Health Sci. 2020, 20, 114–121. [Google Scholar] [CrossRef]
- Marr, K.A.; Sun, Y.; Spec, A.; Lu, N.; Panackal, A.; Bennett, J.; Pappas, P.; Ostrander, D.; Datta, K.; Zhang, S.X.; et al. A Multicenter, Longitudinal Cohort Study of Cryptococcosis in Human Immunodeficiency Virus-negative people in the United States. Clin. Infect. Dis. 2020, 70, 252–261. [Google Scholar] [CrossRef]
- Bridi Cavassin, F.; Vidal, J.E.; Baú-Carneiro, J.L.; Silva de Miranda Godoy, C.; de Bastos Ascenço Soares, R.; Magri, M.M.; Rodríguez, D.; Sakuma de Oliveira, C.; Almeida Mendes, A.V.; Breda, G.L. Characteristics, mortality, associated variables with death, and therapeutic response among HIV-positive, solid organ transplant (SOT), and non-HIV-positive/non-transplant (NHNT) patients with cryptococcosis: First multicenter cohort study in Brazil. Med. Mycol. 2023, 61, myad011. [Google Scholar] [CrossRef] [PubMed]
- Kajeekul, R.; Mekawichai, P.; Chayakulkeeree, M. Clinical features of Cryptococcal meningoencephalitis in HIV-positive and -negative patients in a resource-limited setting. J. Fungi 2023, 9, 869. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Su, X.; Li, W.; Xu, L.; Li, D.; Dai, K.; Liu, J.; Peng, F. Clinical features and mortality risk factors in non-HIV elderly patients with cryptococcal meningitis: A retrospective cohort study from 2013 to 2022. PLoS Negl. Trop. Dis. 2025, 19, e0013521. [Google Scholar] [CrossRef]
- Teekaput, C.; Yasri, S.; Chaiwarith, R. Cryptococcal meningitis: Differences between patients with and without HIV-infection. Pathogens 2023, 12, 427. [Google Scholar] [CrossRef] [PubMed]
- Arechavala, A.; Negroni, R.; Messina, F.; Romero, M.; Marín, E.; Depardo, R.; Walker, L.; Santiso, G. Cryptococcosis in an infectious diseases hospital of Buenos Aires, Argentina. Revision of 2041 cases: Diagnosis, clinical features and therapeutics. Rev. Iberoam. Micol. 2018, 35, 1–10. [Google Scholar] [CrossRef]
- Zono, B.B.; Kasumba, D.M.; Situakibanza Nani-Tuma, H.; Bepouka Izizag, B.; Yambayamba Kapenga, M.; Nsuka Yanga, R.; Tshimy Tshimanga, Y.; Kamangu Ntambwe, E.; Hayette, M.P.; Mvumbi Lelo, G. Cryptococcosis in the Democratic Republic of Congo from 1953 to 2021: A systematic review and meta-analysis. Mycoses 2022, 65, 580–589. [Google Scholar] [CrossRef]
- Walukaga, S.; Fieberg, A.; Musubire, A.; Tugume, L.; Ssebambulidde, K.; Kagimu, E.; Kasibante, J.; Rutakingirwa, M.K.; Mpoza, E.; Gakuru, J.; et al. The evolution of HIV-associated cryptococcal meningitis in Uganda from 2010 to 2022. Med. Mycol. 2024, 63, myae115. [Google Scholar] [CrossRef]
- McClelland, E.E.; Hobbs, L.M.; Rivera, J.; Casadevall, A.; Potts, W.K.; Smith, J.M.; Ory, J.J. The role of host gender in the pathogenesis of Cryptococcus neoformans infections. PLoS ONE 2013, 8, e63632. [Google Scholar] [CrossRef]
- Paccoud, O.; Desnos-Ollivier, M.; Persat, F.; Demar, M.; Boukris-Sitbon, K.; Bellanger, A.P. French Mycoses Study Group. Features of cryptococcosis among 652 HIV-seronegative individuals in France: A cross-sectional observational study (2005–2020). Clin. Microbiol. Infect. 2024, 30, 937–944. [Google Scholar] [CrossRef]
- Gifford, A.; Jayawardena, N.; Carlesse, F.; Lizarazo, J.; McMullan, B.; Groll, A.H.; Warris, A. Pediatric Cryptococcosis. Pediatr. Infect. Dis. J. 2024, 43, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Mugabi, T.; Namombwe, S.; Dai, B.; Nalintya, E.; Nsangi, L.J.; Kabahubya, M.; Najjuka, S.M.; Okurut, S.; Namuju, O.C.; Kigozi, E.; et al. Etiology and outcomes of meningitis among adults in three Ugandan referral hospitals, 2018–2023: A prospective cohort study in a high-HIV endemic setting. Am. J. Trop. Med. Hyg. 2025, 112, 1273–1279. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Wang, Y.; He, J.; Cheng, Z.; Wu, S.; Wang, M.; Niu, T. Clinical characteristics and risk factors for mortality in cryptococcal meningitis: Evidence from a cohort study. Front. Neurol. 2022, 13, 779435. [Google Scholar] [CrossRef] [PubMed]
- Arango-Franco, C.A.; Rojas, J.; Firacative, C.; Migaud, M.; Agudelo, C.I.; Franco, J.L.; Castañeda, E.; Arias, A.A. Autoantibodies neutralizing GM-CSF in HIV-negative Colombian patients infected with Cryptococcus gattii and C. neoformans. J. Clin. Immunol. 2024, 44, 163. [Google Scholar] [CrossRef]
- Jiang, Y.K.; Zhou, L.H.; Cheng, J.H.; Zhu, J.H.; Luo, Y.; Li, L.; Zhu, M.; Zhu, R.S.; Qiu, W.J.; Zhao, H.Z.; et al. Anti-GM-CSF autoantibodies predict outcome of cryptococcal meningitis in patients not infected with HIV: A cohort study. Clin. Microbiol. Infect. 2024, 30, 660–665. [Google Scholar] [CrossRef]
- Quincho-Lopez, A.; Poma, N.; Montenegro-Idrogo, J.J. COVID-19 associated with cryptococcosis: A scoping review. Ther. Adv. Infect. Dis. 2024, 11, 20499361241232851. [Google Scholar] [CrossRef]
- Malli, I.A.; Alqhtani, S.A.; Abid, H.G.; Alqhtani, N.A.; Alharbi, G.E.; Alharbi, R.K.; Aboaljadiel, L.H.; Aletani, T.H.; Alamri, T.M. The outcomes of cryptococcal disease in HIV-positive individuals following COVID-19 infection: A systematic review and meta-analysis. J. Infect. Public Health 2025, 18, 102941. [Google Scholar] [CrossRef]
- Howard-Jones, A.R.; Sparks, R.; Pham, D.; Halliday, C.; Beardsley, J.; Chen, S.C. Pulmonary cryptococcosis. J. Fungi 2022, 8, 1156. [Google Scholar] [CrossRef] [PubMed]
- Loyse, A.; Moodley, A.; Rich, P.; Molloy, S.F.; Bicanic, T.; Bishop, L.; Rae, W.I.; Bhijgee, A.I.; Loubser, N.D.; Michowicz, A.J. Neurological, visual, and MRI brain scan findings in 87 South African patients with HIV-associated cryptococcal meningoencephalitis. J. Infect. 2015, 70, 668–675. [Google Scholar] [CrossRef]
- Gaudemer, A.; Covier, N.; Henry-Feugeas, M.C.; Timsit, J.F.; Lavallée, P.C.; de Montmollin, E.; Lecler, A.; Khalil, A.; Soneville, R.; Couffignal, C. Neuroimaging for prognosis of central nervous system infections: A systematic review and meta-analysis. Ann. Intensive Care 2025, 15, 101. [Google Scholar] [CrossRef]
- Teixeira, J.C.; de Oliveira, V.F.; Gomes, H.R.; Ribeiro, S.M.; de Araujo, E.D.; da Cruz, I.C.; Taborda, M.; Magri, A.S.; Vidal, J.E.; Nastri, A.C. Association between neuroimaging and clinical outcomes in individuals with central nervous system cryptococcosis. Mycoses 2024, 67, e13767. [Google Scholar] [CrossRef] [PubMed]
- Perfect, J.R.; Dismukes, W.E.; Dromer, F.; Goldman, D.L.; Graybill, J.R.; Hamill, R.J.; Harrison, T.S.; Larsen, R.A.; Lortholary, O.; Nguyen, M.H.; et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin. Infect. Dis. 2010, 50, 291–322. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines on the Diagnosis, Prevention and Management of Cryptococcal Disease in HIV-Infected Adults, Adolescents and Children: Supplement to the 2016 Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. Guidelines for Diagnosing, Preventing and Managing Cryptococcal Disease Among Adults, Adolescents and Children Living with HIV; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Chang, C.C.; Harrison, T.S.; Bicanic, T.A.; Chayakulkeeree, M.; Sorrell, T.C.; Warris, A.; Hagen, F.; Spec, A.; Oladele, R.; Govender, N.; et al. Global guideline for the diagnosis and management of cryptococcosis: An initiative of the ECMM and ISHAM in cooperation with the ASM. Lancet Infect. Dis. 2024, 24, e495–e512. [Google Scholar] [CrossRef]
- Mimicos, E.V.; Fossaluza, V.; Picone, C.M.; de Sena, C.C.; Gomes, H.R.; Lázari, C.D.; Ferreira da Silva, F.; Shimoda Nakanishi, E.; Vichr Nisida, E.; Carvalho Freitas, A.; et al. Prevalence and associated factors of cryptococcal antigenemia in HIV-infected patients with CD4 <200 cells/µL in São Paulo, Brazil: A bayesian analysis. J. Fungi 2022, 8, 1284. [Google Scholar] [CrossRef]
- Alves Soares, E.; Lazera, M.D.; Wanke, B.; Faria Ferreira, M.; Carvalhaes de Oliveira, R.V.; Oliveira, A.G.; Coutinho, Z.F. Mortality by cryptococcosis in Brazil from 2000 to 2012: A descriptive epidemiological study. PLoS Negl. Trop. Dis. 2019, 13, e0007569. [Google Scholar] [CrossRef]
- McHale, T.C.; Boulware, D.R.; Kasibante, J.; Ssebambulidde, K.; Skipper, C.P.; Abassi, M. Diagnosis and management of cryptococcal meningitis in HIV-infected adults. Clin. Microbiol. Rev. 2023, 36, e0015622. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lakoh, S.; Kamudumuli, P.S.; Penney, R.O.; Haumba, S.M.; Jarvis, J.N.; Hassan, A.J.; Moudoute, N.L.; Ocansey, B.K.; Izco, S.; Kipkerich, S. Diagnostic capacity for invasive fungal infections in advanced HIV disease in Africa: A continent-wide survey. Lancet Infect. Dis. 2023, 23, 598–608. [Google Scholar] [CrossRef]
- Boulware, D.R.; Rolfes, M.A.; Rajasingham, R.; von Hohenberg, M.; Qin, Z.; Taseera, K.; Schutz, C.; Kwizera, R.; Butler, E.K.; Meintjes, G.; et al. Multisite validation of cryptococcal antigen lateral flow assay and quantification by laser thermal contrast. Emerg. Infect. Dis. 2014, 20, 45–53. [Google Scholar] [CrossRef]
- Firacative, C.; Lizarazo, J.; Illnait-Zaragozí, M.T.; Castañeda, E. Latin American Cryptococcal Study Group. The status of cryptococcosis in Latin America. Mem. Inst. Oswaldo Cruz 2018, 113, e170554. [Google Scholar] [CrossRef] [PubMed]
- Melhem, M.S.; Leite Júnior, D.P.; Takahashi, J.P.; Macioni, M.B.; Oliveira, L.; de Araújo, L.S.; Fava, W.S.; Bonfietti, L.X.; Paniago, A.M.; Venturini, J.; et al. Antifungal resistance in cryptococcal infections. Pathogens 2024, 13, 128. [Google Scholar] [CrossRef] [PubMed]
- Doan, T.T.; Dieu Ta, N.T.; Bui, H.N.; Van Do, T. Determinants of mortality in HIV-associated cryptococcal meningitis in Vietnam: Implications for optimizing management for resource-limited settings. Clin. Infect. Pract. 2025, 27, 100497. [Google Scholar] [CrossRef]
- Kneale, M.; Bartholomew, J.S.; Davies, E.; Denning, D.W. Global access to antifungal therapy and its variable cost. J. Antimicrob. Chemother. 2016, 71, 3599–3606. [Google Scholar] [CrossRef]
- Lockhart, S.R.; Iqbal, N.; Bolden, C.B.; DeBess, E.E.; Marsden-Haug, N.; Worhle, R.; Thakur, R.; Harris, J.R. Cryptococcus gattii PNW Public Health Working Group. Epidemiologic cutoff values for triazole drugs in Cryptococcus gattii: Correlation of molecular type and in vitro susceptibility. Diagn. Microbiol. Infect. Dis. 2012, 73, 144–148. [Google Scholar] [CrossRef]
- Andrade-Silva, L.; Ferreira-Paim, K.; Mora, D.J.; Da Silva, P.R.; Andrade, A.A.; Araujo, N.E.; Pedrosa, A.L.; Silva-Vergara, M.L. Susceptibility profile of clinical and environmental isolates of Cryptococcus neoformans and Cryptococcus gattii in Uberaba, Minas Gerais, Brazil. Med. Mycol. 2013, 51, 635–640. [Google Scholar] [CrossRef]
- Tewari, A.; Behera, B.; Mathur, P.; Xess, I. Comparative analysis of the Vitek 2 antifungal susceptibility system and E-test with the CLSI M27-A3 broth microdilution method for susceptibility testing of indian clinical isolates of Cryptococcus neoformans. Mycopathologia 2012, 173, 427–433. [Google Scholar] [CrossRef]
- Harris, J.R.; Lockhart, S.; Debess, E.; Marsden-Haug, N.; Goldoft, M.; Wohrle, R.; Lee, S.; Smelser, C.; Chiller, T. Cryptococcus gattii in the United States: Clinical aspects of infection with an emerging pathogen. Clin. Infect. Dis. 2011, 53, 1188–1195. [Google Scholar] [CrossRef] [PubMed]
- Dao, A.; Kim, H.Y.; Garnham, K.; Kidd, S.; Sati, H.; Perfect, J.; Sorrell, T.C.; Harrison, T.; Rickerts, V.; Gigante, V. Cryptococcosis-a systematic review to inform the World Health Organization Fungal Priority Pathogens List. Med. Mycol. 2024, 62, myae043. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Salud. Resolución 1646 del 4 de Diciembre de 2018. Available online: https://www.ins.gov.co/Normatividad/Resoluciones/RESOLUCION%201646%20DE%202018.pdf (accessed on 9 October 2025).
- Lizarazo, J.; Linares, M.; De Bedout, C.; Restrepo, A.; Agudelo, C.I.; Castañeda, E. Grupo Colombiano para el Estudio de la Criptococosis. Estudio clínico y epidemiológico de la criptococosis en Colombia: Resultado de nueve años de la encuesta nacional, 1997–2005. Biomédica 2007, 27, 94–109. [Google Scholar] [CrossRef]
- Escandón, P.; De Bedout, C.; Lizarazo, J.; Agudelo, C.I.; Tobón, A.; Bello, S.; Restrepo, A.; Castañeda, E. Grupo Colombiano para el Estudio de la Criptococosis. Cryptococcosis in Colombia: Results of the national surveillance program for the years 2006–2010. Biomédica 2012, 32, 386–398. [Google Scholar] [PubMed]
| Patients‘ Epidemiological and Clinical Characteristics | Total | |
|---|---|---|
| n | % | |
| Sex | ||
| Male | 677 | 76.0 |
| Female | 214 | 24.0 |
| Total | 891 | 100.0 |
| Male: female ratio: 3.2:1 | ||
| Age group | ||
| ≤16 | 13 | 1.5 |
| 17–25 | 81 | 9.1 |
| 26–40 | 310 | 34.8 |
| 41–59 | 276 | 31.0 |
| ≥60 | 211 | 23.7 |
| Total | 891 | 100.0 |
| Risk factor * | ||
| AIDS | 561 | 63.0 |
| Corticosteroids/other immunosuppressive drugs | 127 | 14.3 |
| Chronic renal failure | 71 | 8.0 |
| Diabetes | 62 | 7.0 |
| Autoimmune disease | 50 | 5.6 |
| Solid tumor | 44 | 4.9 |
| Transplantation | 28 | 3.1 |
| Cirrhosis | 20 | 2.2 |
| Hematologic malignancies | 18 | 2.0 |
| Others ** | 4 | 0.4 |
| Unknown or no risk factors | 141 | 15.8 |
| Symptoms/signs | ||
| Headache | 554 | 62.2 |
| Fever | 369 | 41.4 |
| Confusion | 355 | 39.8 |
| Nausea/vomiting | 343 | 38.5 |
| Cough | 188 | 21.1 |
| Intracranial hypertension without hydrocephalus | 156 | 17.5 |
| Seizures | 135 | 15.2 |
| Neck stiffness/meningeal signs | 106 | 11.9 |
| Others *** | 273 | 30.6 |
| Clinical presentation | ||
| CNS | 554 | 62.2 |
| Disseminated | 277 | 31.1 |
| Pulmonary | 46 | 5.1 |
| Other **** | 14 | 1.6 |
| Total | 891 | 100.0 |
| Treatment | ||
| AmB alone | 117 | 23.0 |
| AmB combined | 338 | 66.4 |
| Others ***** | 54 | 10.6 |
| Total | 509 | 57.1 |
| Mortality | 181 | 20.3 |
| Relapses | 29 | 0.2 |
| Laboratory Data | n | % |
|---|---|---|
| Diagnostic method | ||
| Culture | 886 | 99.4 |
| Direct examination | 472 | 53.0 |
| Antigenemia (Latex, Lateral Flow Analysis (LFA)) * | 318 | 35.7 |
| Film array ** | 33 | 3.7 |
| Sample type | ||
| CSF | 596 | 67.3 |
| Blood | 313 | 35.4 |
| BAL | 29 | 3.3 |
| Biopsy (lung, skin, others) *** | 17 | 1.9 |
| Other sterile body fluids | 8 | 0.9 |
| Catheter | 2 | 0.2 |
| Tracheal aspirate | 1 | 0.1 |
| ND | 12 | 1.4 |
| Species complexes **** | ||
| C. neoformans | 779 | 93.1 |
| C. gattii | 58 | 6.9 |
| Total | 837 | 100.0 |
| Molecular patterm | ||
| VNI | 242 | 92.4 |
| VNII | 17 | 6.5 |
| VNIII | 3 | 1.1 |
| VNIV | 0 | 0 |
| Total | 262 | 100.0 |
| VGI | 19 | 35.2 |
| VGII | 25 | 46.3 |
| VGIII | 10 | 18.5 |
| VGIV | 0 | 0 |
| Total | 54 | 100.0 |
| Variable | HIV + N = 561 (63.0) | HIV − N = 330 (27.0) | Total N = 891 | p | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Sex | |||||||
| Male | 459 | 81.8 | 218 | 66.1 | 677 | 76.0 | <0.0001 |
| Female | 102 | 18.2 | 112 | 33.9 | 214 | 24.0 | |
| Male: female ratio | 4.5:1.0 | 1.9:1.0 | 3.2:1.0 | ||||
| Age group in years | |||||||
| ≤16 | 5 | 0.9 | 8 | 2.4 | 13 | 1.5 | <0.0001 |
| 17–25 | 67 | 11.9 | 14 | 4.2 | 81 | 9.1 | |
| 26–40 | 257 | 45.8 | 53 | 16.1 | 310 | 34.8 | |
| 41–59 | 181 | 32.3 | 95 | 28.8 | 276 | 31.0 | |
| ≥60 | 51 | 9.1 | 160 | 48.5 | 211 | 23.7 | |
| Risk factor | |||||||
| Corticosteroids/other immunosuppressive drugs | 48 | 8.6 | 79 | 23.9 | 127 | 14.8 | <0.0001 |
| Chronic kidney failure | 12 | 2.1 | 59 | 17.9 | 71 | 8.2 | <0.0001 |
| Diabetes | 11 | 2.0 | 51 | 15.5 | 62 | 7.2 | <0.0001 |
| Autoimmune disease | 7 | 1.2 | 43 | 13.0 | 50 | 5.8 | <0.0001 |
| Solid tumor | 6 | 1.1 | 38 | 11.5 | 44 | 5.1 | <0.0001 |
| Transplantation | 0 | 0.0 | 28 | 8.5 | 28 | 3.3 | <0.0001 |
| Cirrhosis | 8 | 1.4 | 12 | 3.6 | 20 | 2.3 | <0.05 |
| Hematologic neoplasms | 3 | 0.5 | 15 | 4.5 | 18 | 2.1 | <0.0001 |
| Others * | 2 | 0.4 | 2 | 0.6 | 4 | 0.4 | NA |
| Unknown or no risk factor | 0 | 0.0 | 141 | 42.7 | 141 | 16.4 | <0.0001 |
| Clinical presentation | |||||||
| CNS | 390 | 69.5 | 164 | 49.7 | 554 | 62.2 | <0.0001 |
| Disseminated | 157 | 28.0 | 120 | 36.4 | 277 | 31.1 | <0.004 |
| Pulmonary | 10 | 1.8 | 36 | 10.9 | 46 | 5.1 | <0.0001 |
| Other ** | 4 | 0.7 | 10 | 3.0 | 14 | 1.6 | NA |
| Symptoms/signs | |||||||
| Headache | 381 | 69.5 | 164 | 49.7 | 554 | 62.2 | <0.0001 |
| Fever | 252 | 44.9 | 117 | 35.4 | 369 | 41.4 | 0.002 |
| Confusion | 238 | 42.4 | 117 | 35.4 | 355 | 39.8 | 0.02 |
| Nausea/vomiting | 244 | 43.5 | 99 | 30.0 | 343 | 38.5 | <0.0001 |
| Cough | 133 | 23.7 | 55 | 16.7 | 188 | 21.1 | 0.006 |
| Intracranial hypertension without hydrocephalus | 111 | 19.8 | 45 | 13.6 | 156 | 17.5 | 0.009 |
| Seizures | 101 | 18.0 | 34 | 10.3 | 135 | 15.2 | 0.001 |
| Neck stiffness/meningeal signs | 81 | 14.4 | 25 | 7.6 | 106 | 11.9 | 0.001 |
| Others *** | 195 | 34.8 | 78 | 23.6 | 273 | 30.6 | NA |
| Treatment | |||||||
| AMB | 74 | 20.7 | 43 | 28.5 | 117 | 23.0 | |
| AMB combined | 248 | 69.3 | 90 | 59.6 | 338 | 66.4 | |
| Others **** | 36 | 10.0 | 18 | 11.9 | 54 | 10.6 | |
| Total | 358 | 100.0 | 151 | 100.0 | 509 | 100.0 | |
| Mortality | |||||||
| 109 | 19.4 | 72 | 21.8 | 181 | 20.3 | 0.19 | |
| Etiological agent | |||||||
| C. neoformans | 511 | 97.1 | 268 | 86.2 | 779 | 93.1 | <0.0001 |
| C. gattii | 15 | 2.9 | 43 | 13.8 | 58 | 6.9 | <0.0001 |
| Total | 526 | 62.8 | 311 | 37.2 | 837 | 93.9 | |
| Molecular types | |||||||
| VNI | 69 | 90.8 | 173 | 93.0 | 242 | 92.4 | 0.2 |
| VNII | 7 | 9.2 | 10 | 5.4 | 17 | 6.5 | |
| VNIII | 3 | 1.6 | 3 | 1.1 | |||
| Total | 76 | 186 | 262 | 100.0 | |||
| VGI | 5 | 35.7 | 14 | 35.0 | 19 | 35.2 | |
| VGII | 6 | 42.9 | 19 | 47.5 | 25 | 45.3 | |
| VGIII | 3 | 21.4 | 7 | 17.5 | 10 | 18.5 | |
| Total | 14 | 40 | 54 | 100.0 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Lizarazo, J.; Agudelo, C.I.; Escandón, P.; Castañeda, E. Cryptococcosis in Colombia: Analysis of Data from Laboratory-Based Surveillance 2017–2024. J. Fungi 2026, 12, 67. https://doi.org/10.3390/jof12010067
Lizarazo J, Agudelo CI, Escandón P, Castañeda E. Cryptococcosis in Colombia: Analysis of Data from Laboratory-Based Surveillance 2017–2024. Journal of Fungi. 2026; 12(1):67. https://doi.org/10.3390/jof12010067
Chicago/Turabian StyleLizarazo, Jairo, Clara Inés Agudelo, Patricia Escandón, and Elizabeth Castañeda. 2026. "Cryptococcosis in Colombia: Analysis of Data from Laboratory-Based Surveillance 2017–2024" Journal of Fungi 12, no. 1: 67. https://doi.org/10.3390/jof12010067
APA StyleLizarazo, J., Agudelo, C. I., Escandón, P., & Castañeda, E. (2026). Cryptococcosis in Colombia: Analysis of Data from Laboratory-Based Surveillance 2017–2024. Journal of Fungi, 12(1), 67. https://doi.org/10.3390/jof12010067








