Virtual Dissection: Emerging as the Gold Standard of Analyzing Living Heart Anatomy
Abstract
1. Introduction
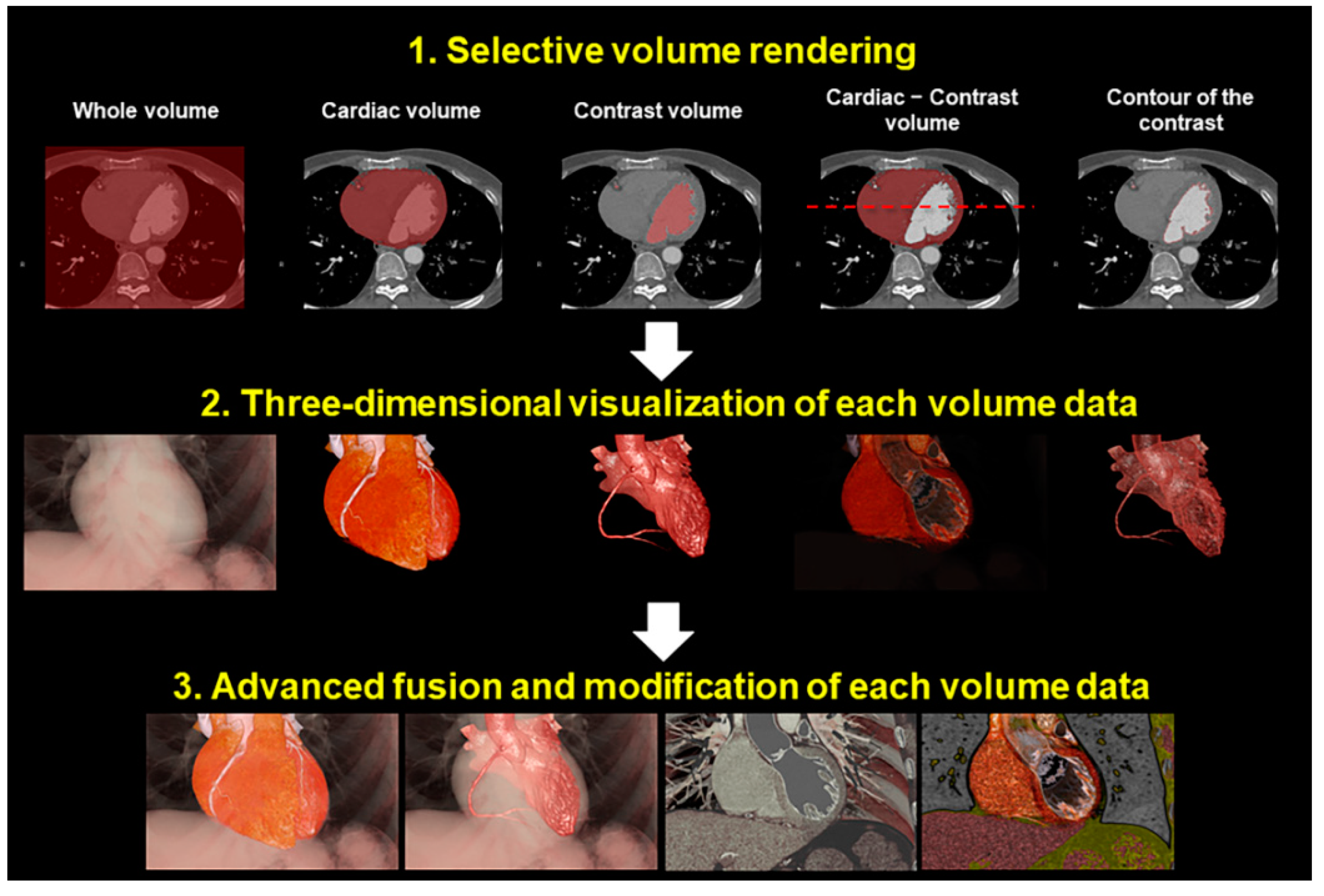
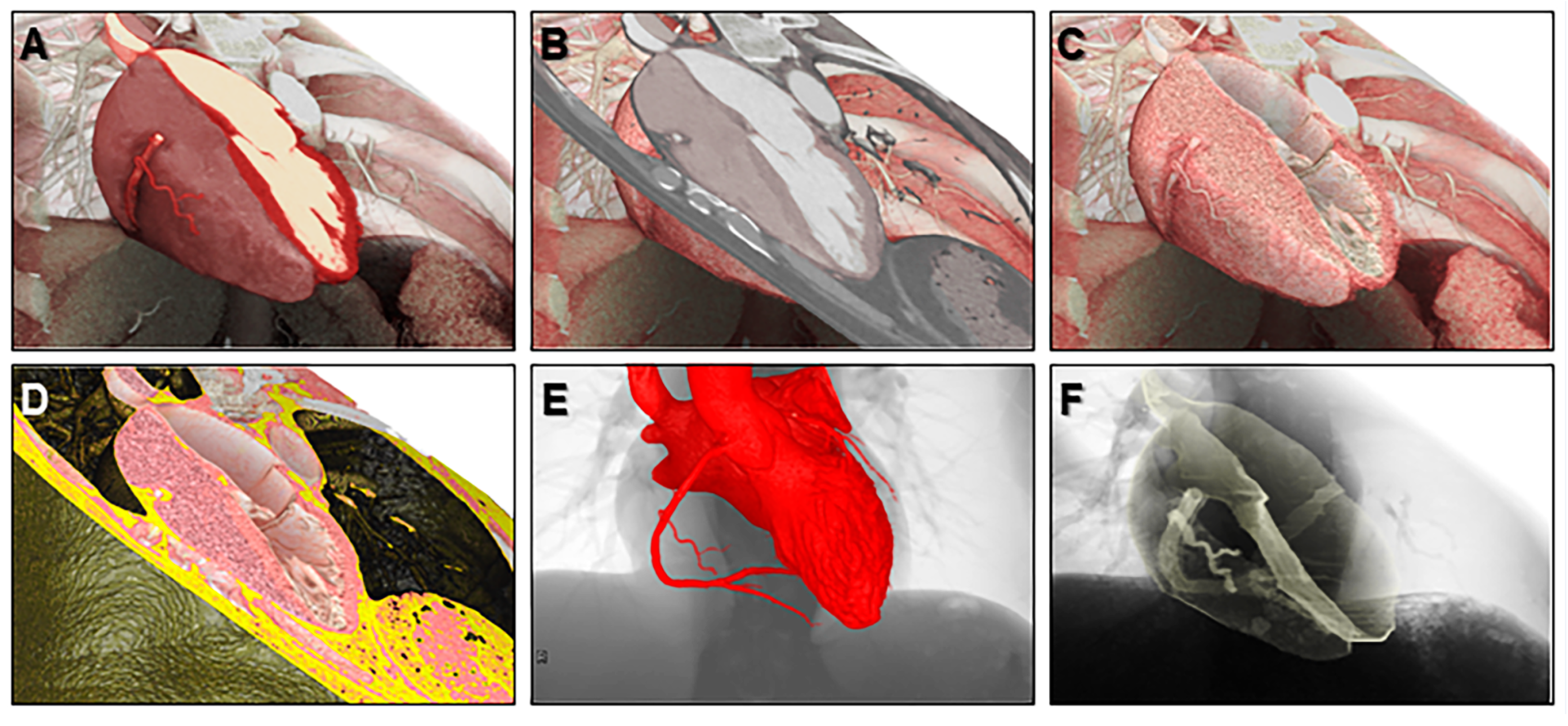
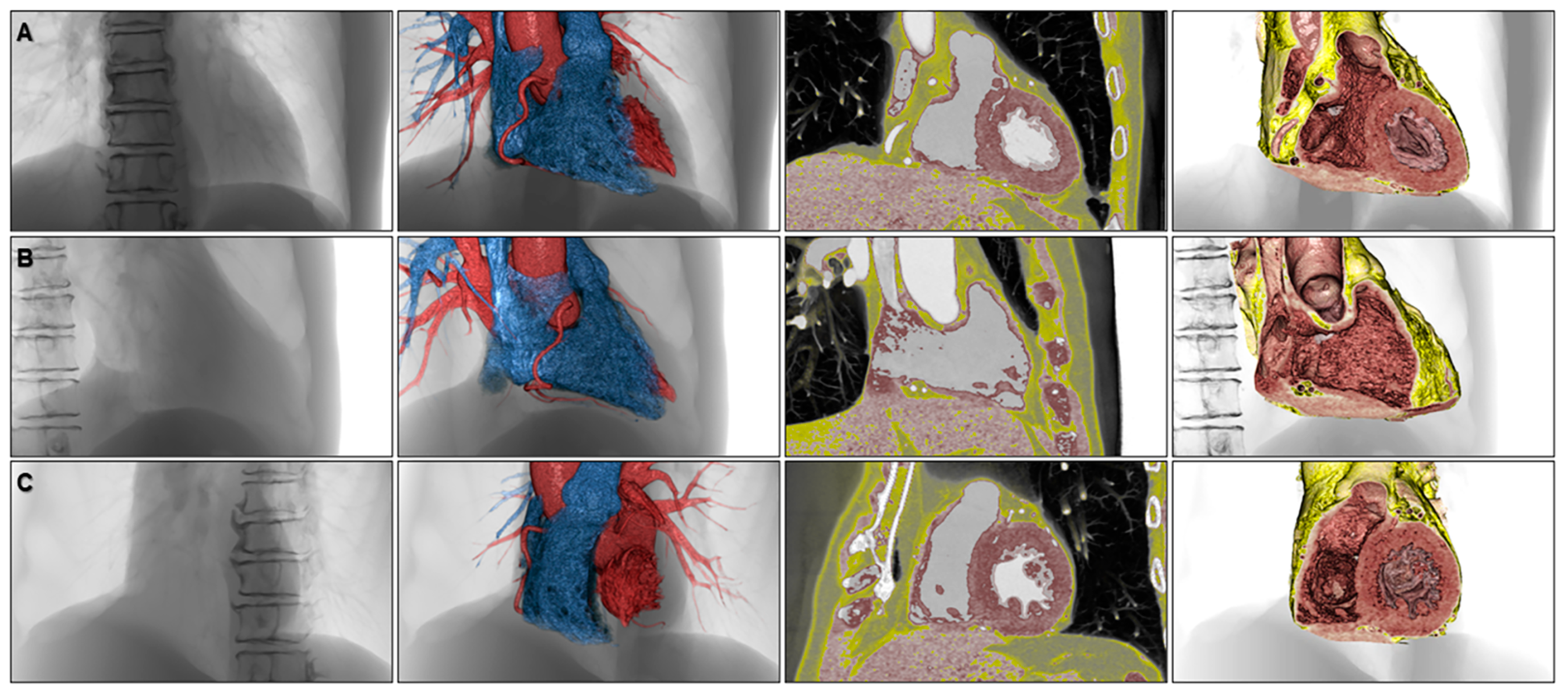
2. The Concept of Three-Dimensional Imaging Using the Volume-Rendering Method
3. The Advantage of the Virtual Dissection Compared to Conventional Real Dissection
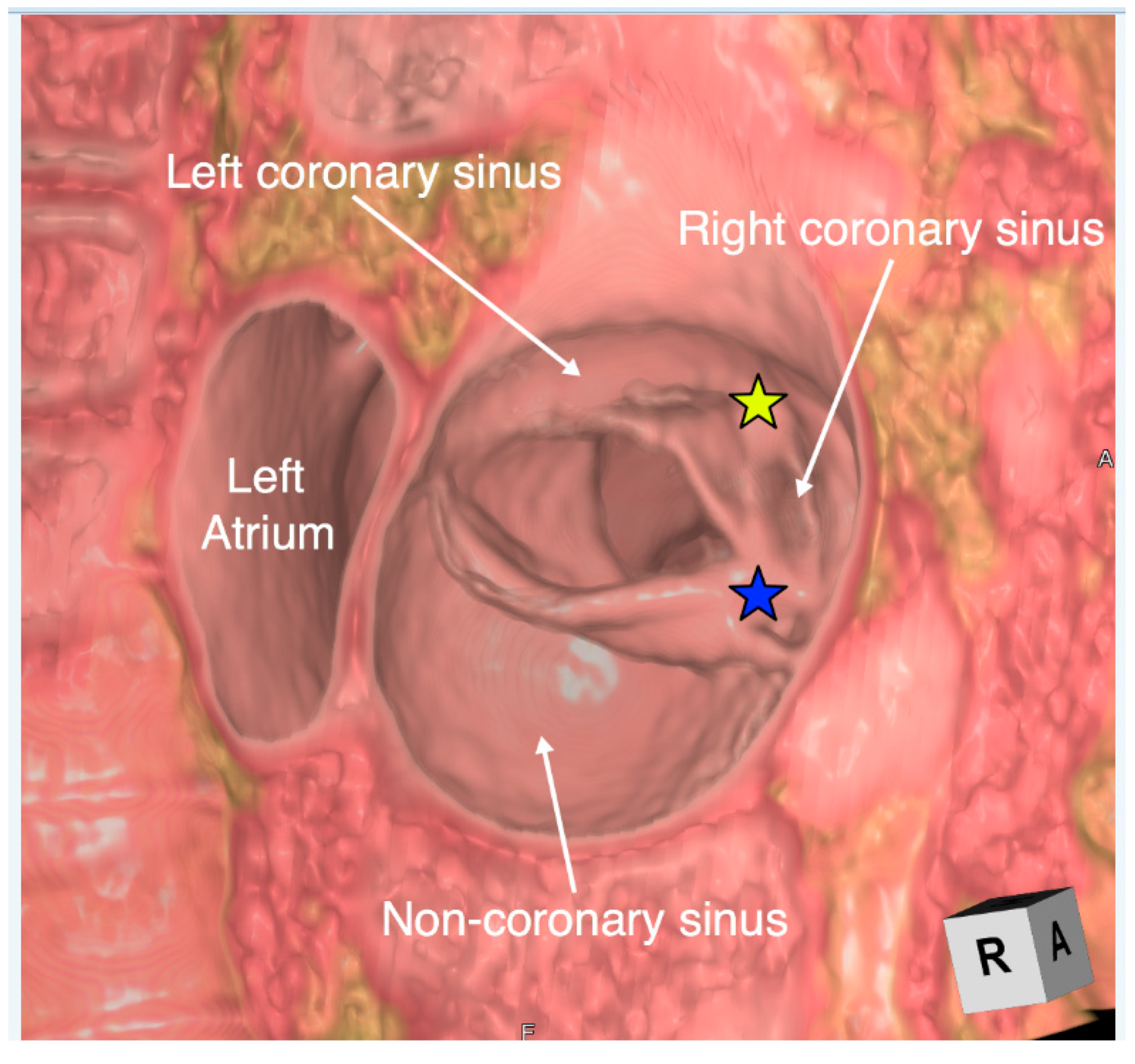
4. Educational Implication of the Three-Dimensional Living Heart Anatomy
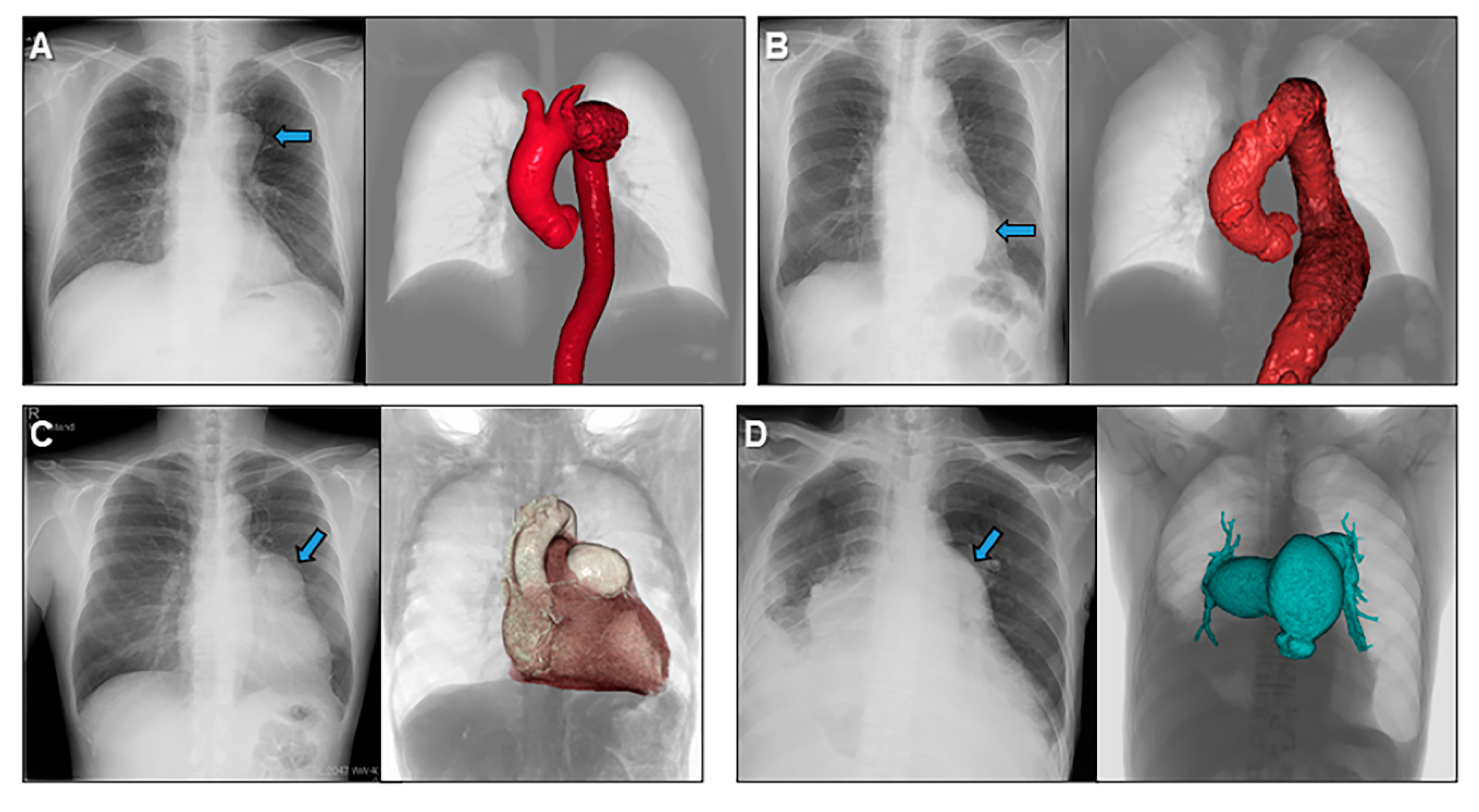
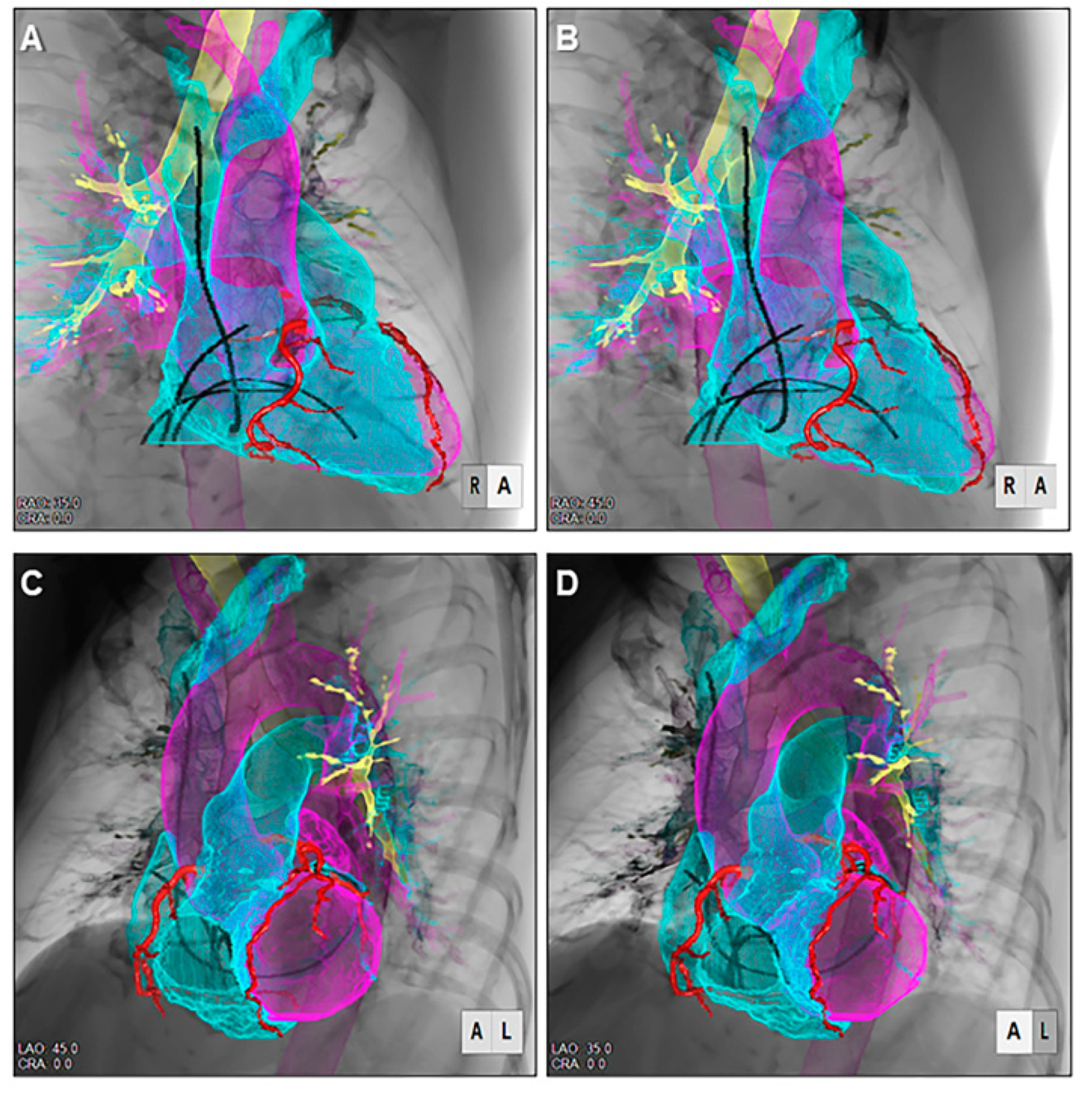
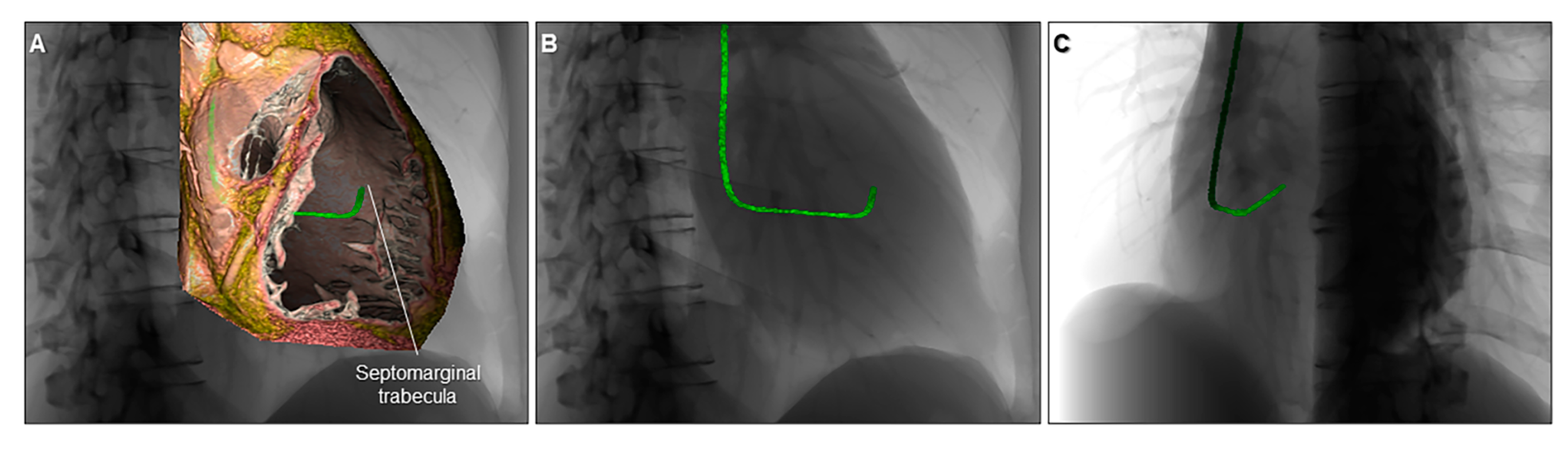
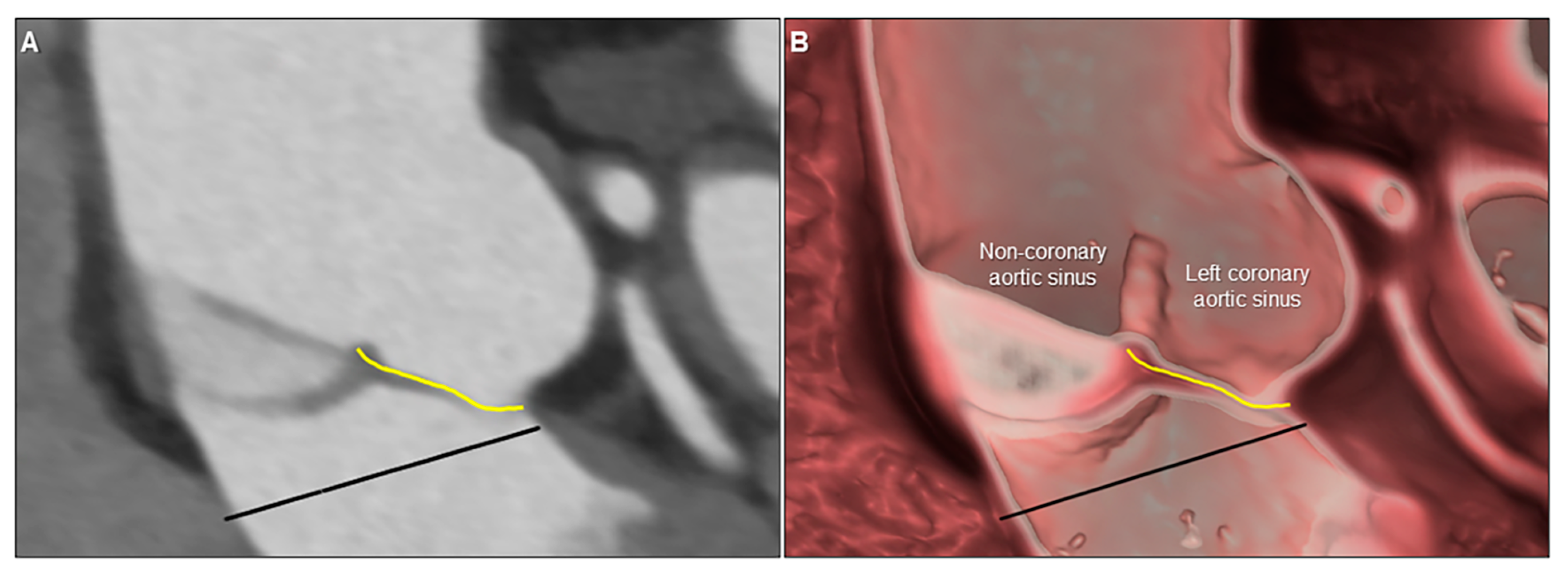
5. Clinical Implication in Acquired Heart Disease with Representative Cases
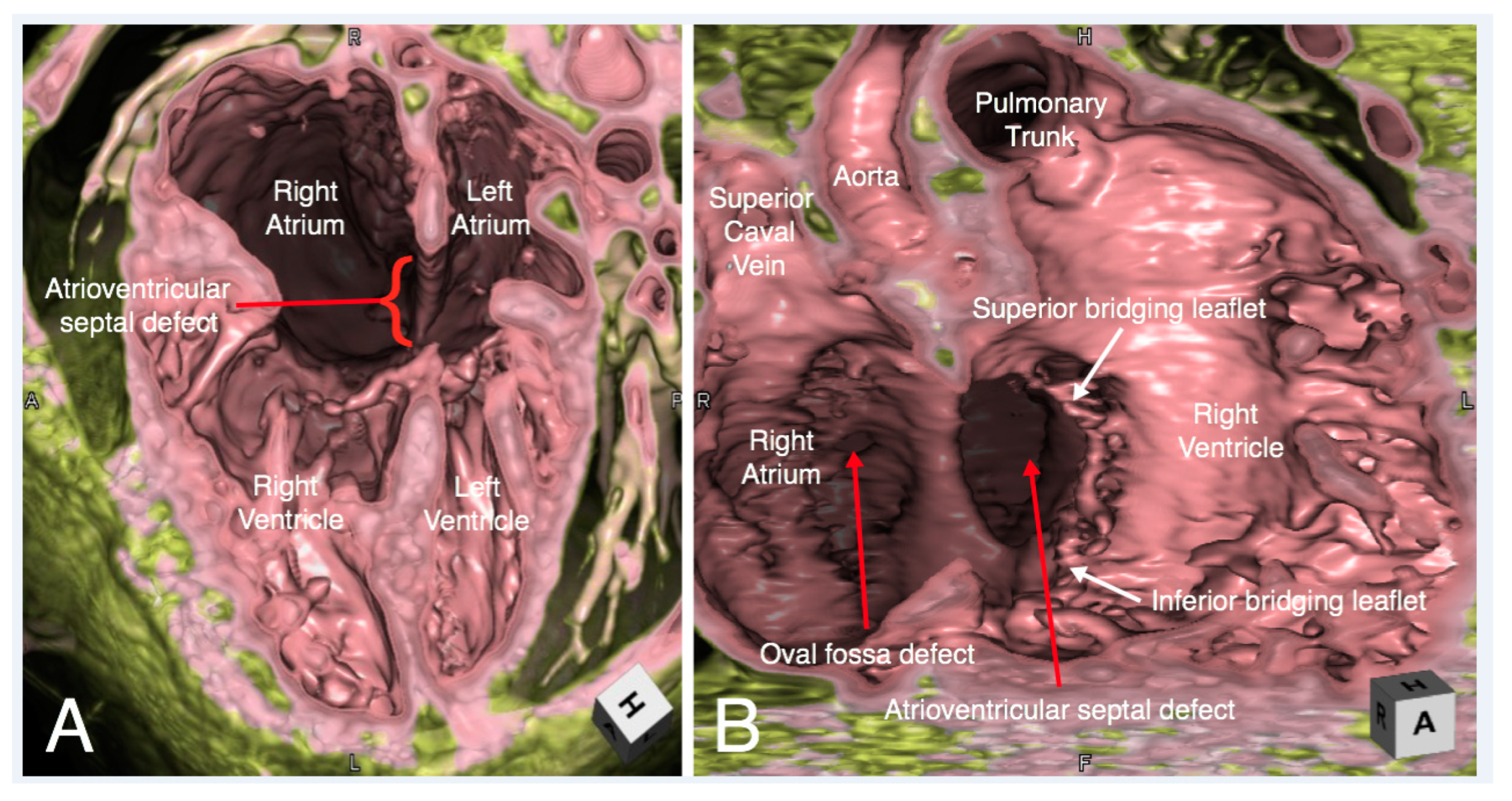
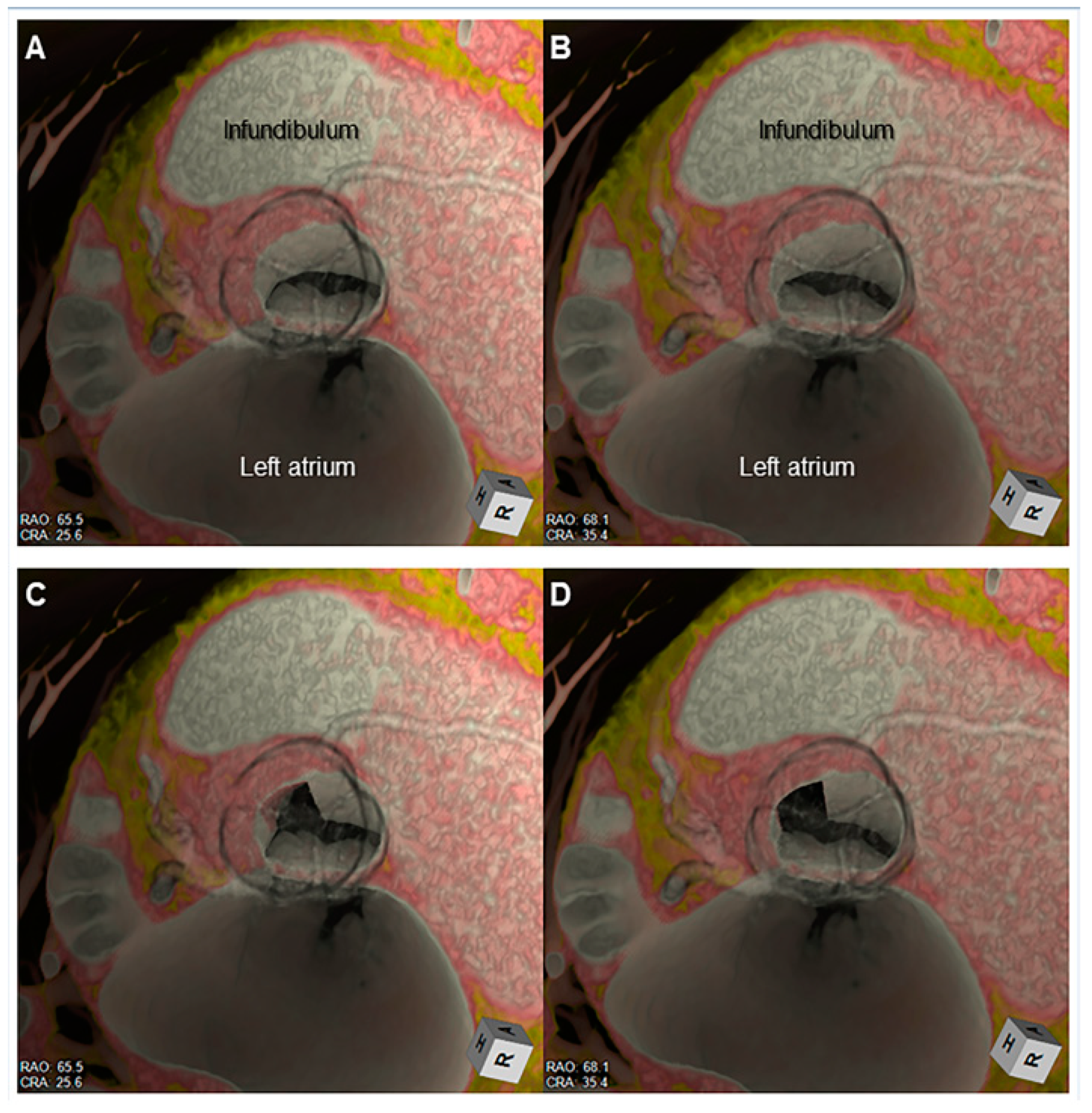
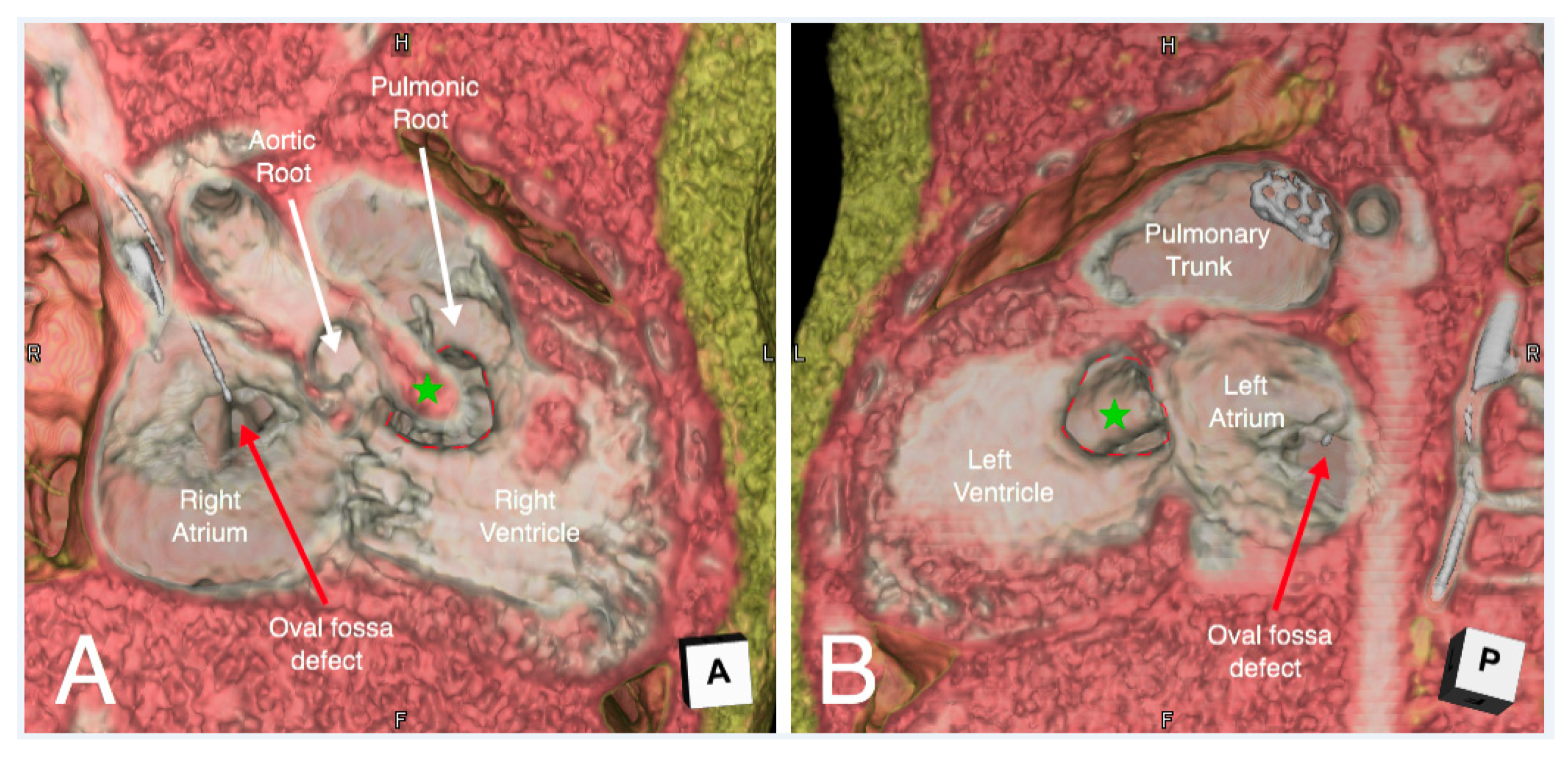
6. Clinical Implication in Congenital Heart Disease with Representative Cases
- Relationship of the great arteries to an interventricular communication in the setting of double outlet right ventricle for surgical planning (Figure 13);
- Unicuspid aortic valve for surgical repair planning (Figure 14, Supplementary Movie 2);
- Right ventricular outflow tract obstruction in repaired tetralogy of Fallot to guide transcatheter pulmonary valve replacement (Figure 16).
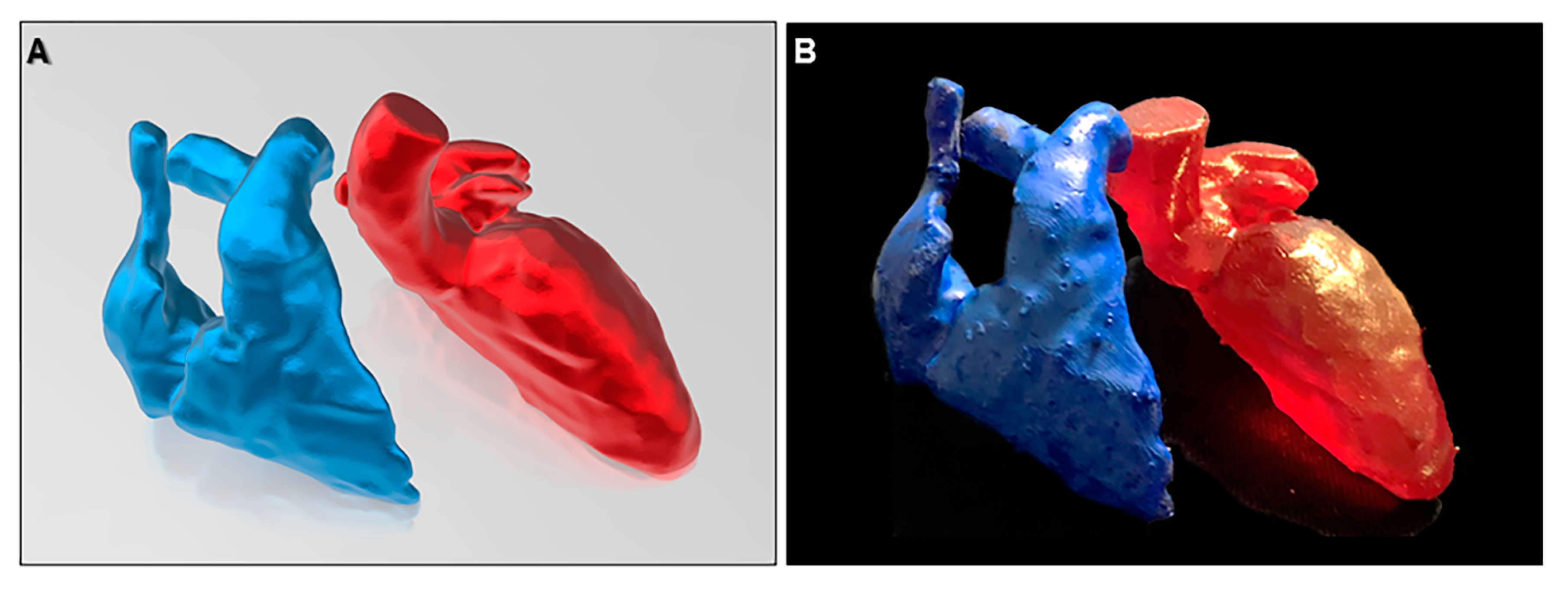
7. Advanced Application of the Three-Dimensional Imaging
8. Limitations of Three-Dimensional Imaging and Importance of Basic Anatomical Knowledge and Multidisciplinary Relationship
9. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Mori, S.; Tretter, J.T.; Spicer, D.E.; Bolender, D.L.; Anderson, R.H. What is the real cardiac anatomy? Clin. Anat. 2019, 32, 288–309. [Google Scholar] [CrossRef]
- Anderson, R.H. Re-Setting the Gold Standard. J. Cardiovasc. Electrophysiol. 2015, 26, 713–714. [Google Scholar] [CrossRef]
- Lin, E.; Alessio, A. What are the basic concepts of temporal, contrast, and spatial resolution in cardiac CT? J. Cardiovasc. Comput. Tomogr. 2009, 3, 403–408. [Google Scholar] [CrossRef]
- Gupta, S.K.; Spicer, D.E.; Anderson, R.H. A new low-cost method of virtual cardiac dissection of computed tomographic datasets. Ann. Pediatr. Cardiol. 2019, 12, 110–116. [Google Scholar] [CrossRef]
- Nagata, K.; Endo, S.; Honda, T.; Yasuda, T.; Hirayama, M.; Takahashi, S.; Kato, T.; Horita, S.; Furuya, K.; Kasai, K.; et al. Accuracy of CT Colonography for Detection of Polypoid and Nonpolypoid Neoplasia by Gastroenterologists and Radiologists: A Nationwide Multicenter Study in Japan. Am. J. Gastroenterol. 2017, 112, 163–171. [Google Scholar] [CrossRef]
- Matsumoto, Y.; Izumo, T.; Sasada, S.; Tsuchida, T.; Ohe, Y. Diagnostic utility of endobronchial ultrasound with a guide sheath under the computed tomography workstation (ziostation) for small peripheral pulmonary lesions. Clin. Respir. J. 2017, 11, 185–192. [Google Scholar] [CrossRef]
- Xu, X.; Zheng, Y.; Yao, S.; Sun, G.; Xu, B.; Chen, X. A low-cost multimodal head-mounted display system for neuroendoscopic surgery. Brain Behav. 2018, 8. [Google Scholar] [CrossRef] [PubMed]
- Clifton, W.; Damon, A.; Valero-Moreno, F.; Nottmeier, E.; Pichelmann, M. The SpineBox: A Freely Available, Open-access, 3D-printed Simulator Design for Lumbar Pedicle Screw Placement. Cureus 2020, 12. [Google Scholar] [CrossRef]
- Wada, K.; Arimoto, H.; Ohkawa, H.; Shirotani, T.; Matsushita, Y.; Takahara, T. Usefulness of preoperative three-dimensional computed tomographic angiography with two-dimensional computed tomographic imaging for rupture point detection of middle cerebral artery aneurysms. Neurosurgery 2008, 62, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Fukuzawa, K.; Nagamatsu, Y.; Mori, S.; Kiuchi, K.; Takami, M.; Izawa, Y.; Konishi, H.; Ichibori, H.; Imada, H.; Hyogo, K.; et al. Percutaneous Pericardiocentesis With the Anterior Approach: Demonstration of the Precise Course with Computed Tomography. JACC Clin. Electrophysiol. 2019, 5, 730–741. [Google Scholar] [CrossRef]
- Steele, J.; Alsaied, T.; Crotty, E.J.; Tretter, J.T. Computed Tomographic 3-Dimensional Virtual Dissection Aiding Surgical Planning in a Rare Pediatric Case of Bicuspid Aortic Valve with Ascending Aorta Pseudoaneurysm. Circ. Cardiovasc. Imaging 2020, 13. [Google Scholar] [CrossRef] [PubMed]
- McGovern, E.M.; Tretter, J.T.; Moore, R.A.; Goldstein, B.H. Simulation to Success: Treatment of a 3D printed heart before complex systemic venous baffle intervention. JACC Case Rep. 2020, 2, 486–487. [Google Scholar] [CrossRef]
- Nishimori, M.; Kiuchi, K.; Mori, S.; Kurose, J.; Izawa, Y.; Kouno, S.; Nakagawa, H.; Shimoyama, S.; Fukuzawa, K.; Hirata, K.I. Atypical inferoseptal accessory pathway connection associated with an aneurysm of the coronary sinus: Insight from a three-dimensional combined image of electroanatomic mapping and computed tomography. HeartRhythm Case Rep. 2018, 4, 389–392. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vukicevic, M.; Mosadegh, B.; Min, J.K.; Little, S.H. Cardiac 3D Printing and its Future Directions. JACC Cardiovasc. Imaging 2017, 10, 171–184. [Google Scholar] [CrossRef] [PubMed]
- Silva, J.N.A.; Southworth, M.; Raptis, C.; Silva, J. Emerging Applications of Virtual Reality in Cardiovascular Medicine. JACC Basic Transl. Sci. 2018, 3, 420–430. [Google Scholar] [CrossRef] [PubMed]
- Schneider, K.; Ghaleb, S.; Morales, D.L.S.; Tretter, J.T. Virtual dissection and endocast three-dimensional reconstructions: Maximizing computed tomographic data for procedural planning of an obstructed pulmonary venous baffle. Cardiol. Young 2019, 29, 1104–1106. [Google Scholar] [CrossRef]
- Mori, S.; Spicer, D.E.; Anderson, R.H. Revisiting the Anatomy of the Living Heart. Circ. J. 2016, 80, 24–33. [Google Scholar] [CrossRef]
- Anderson, R.H.; Razavi, R.; Taylor, A.M. Cardiac anatomy revisited. J. Anat. 2004, 205, 159–177. [Google Scholar] [CrossRef]
- Codreanu, A.; Odille, F.; Aliot, E.; Marie, P.Y.; Magnin-Poull, I.; Andronache, M.; Mandry, D.; Djaballah, W.; Régent, D.; Felblinger, J.; et al. Electroanatomic characterization of post-infarct scars comparison with 3-dimensional myocardial scar reconstruction based on magnetic resonance imaging. J. Am. Coll. Cardiol. 2008, 52, 839–842. [Google Scholar] [CrossRef]
- Cochet, H.; Komatsu, Y.; Sacher, F.; Jadidi, A.S.; Scherr, D.; Riffaud, M.; Derval, N.; Shah, A.; Roten, L.; Pascale, P.; et al. Integration of merged delayed-enhanced magnetic resonance imaging and multidetector computed tomography for the guidance of ventricular tachycardia ablation: A pilot study. J. Cardiovasc. Electrophysiol. 2013, 24, 419–426. [Google Scholar] [CrossRef]
- Mori, S.; Nishii, T.; Takaya, T.; Kashio, K.; Kasamatsu, A.; Takamine, S.; Ito, T.; Fujiwara, S.; Kono, A.K.; Hirata, K. Clinical structural anatomy of the inferior pyramidal space reconstructed from the living heart: Three-dimensional visualization using multidetector-row computed tomography. Clin. Anat. 2015, 28, 878–887. [Google Scholar] [CrossRef] [PubMed]
- Mori, S.; Fukuzawa, K.; Takaya, T.; Takamine, S.; Ito, T.; Fujiwara, S.; Nishii, T.; Kono, A.K.; Yoshida, A.; Hirata, K. Clinical Structural Anatomy of the Inferior Pyramidal Space Reconstructed Within the Cardiac Contour Using Multidetector-Row Computed Tomography. J. Cardiovasc. Electrophysiol. 2015, 26, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Mori, S.; Fukuzawa, K.; Takaya, T.; Takamine, S.; Ito, T.; Fujiwara, S.; Nishii, T.; Kono, A.K.; Yoshida, A.; Hirata, K. Clinical cardiac structural anatomy reconstructed within the cardiac contour using multidetector-row computed tomography: Left ventricular outflow tract. Clin. Anat. 2016, 29, 353–363. [Google Scholar] [CrossRef] [PubMed]
- Mori, S.; Fukuzawa, K.; Takaya, T.; Takamine, S.; Ito, T.; Fujiwara, S.; Nishii, T.; Kono, A.K.; Yoshida, A.; Hirata, K. Clinical cardiac structural anatomy reconstructed within the cardiac contour using multidetector-row computed tomography: Atrial septum and ventricular septum. Clin. Anat. 2016, 29, 342–352. [Google Scholar] [CrossRef]
- Mori, S.; Fukuzawa, K.; Takaya, T.; Takamine, S.; Ito, T.; Fujiwara, S.; Nishii, T.; Kono, A.K.; Yoshida, A.; Hirata, K. Clinical cardiac structural anatomy reconstructed within the cardiac contour using multidetector-row computed tomography: The arrangement and location of the cardiac valves. Clin. Anat. 2016, 29, 364–370. [Google Scholar] [CrossRef]
- Anderson, R.H.; Loukas, M. The importance of attitudinally appropriate description of cardiac anatomy. Clin. Anat. 2009, 22, 47–51. [Google Scholar] [CrossRef]
- De Almeida, M.C.; Spicer, D.E.; Anderson, R.H. Why do we break one of the first rules of anatomy when describing the components of the heart? Clin. Anat. 2019, 32, 585–596. [Google Scholar] [CrossRef]
- Ghosh, S.K. Cadaveric dissection as an educational tool for anatomical sciences in the 21st century. Anat. Sci. Educ. 2017, 10, 286–299. [Google Scholar] [CrossRef]
- Ruzycki, S.M.; Desy, J.R.; Lachman, N.; Wolanskyj-Spinner, A.P. Medical education for millennials: How anatomists are doing it right. Clin. Anat. 2019, 32, 20–25. [Google Scholar] [CrossRef]
- Hołda, M.K.; Stefura, T.; Koziej, M.; Skomarovska, O.; Jasińska, K.A.; Sałabun, W.; Klimek-Piotrowska, W. Alarming decline in recognition of anatomical structures amongst medical students and physicians. Ann. Anat. 2019, 221, 48–56. [Google Scholar] [CrossRef]
- Spitzer, V.M.; Scherzinger, A.L. Virtual anatomy: An anatomist’s playground. Clin. Anat. 2006, 19, 192–203. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, C.G.; Backhaus, M.; Bluemke, D.A.; Britten, R.D.; Chung, J.D.; Cowan, B.R.; Dinov, I.D.; Finn, J.P.; Hunter, P.J.; Kadish, A.H.; et al. The Cardiac Atlas Project—An imaging database for computational modeling and statistical atlases of the heart. Bioinformatics 2011, 27, 2288–2295. [Google Scholar] [CrossRef] [PubMed]
- Maresky, H.S.; Oikonomou, A.; Ali, I.; Ditkofsky, N.; Pakkal, M.; Ballyk, B. Virtual reality and cardiac anatomy: Exploring immersive three-dimensional cardiac imaging, a pilot study in undergraduate medical anatomy education. Clin. Anat. 2019, 32, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Tretter, J.T.; Mori, S. Two-Dimensional Imaging of a Complex Three-Dimensional Structure: Measurements of Aortic Root Dimensions. J. Am. Soc. Echocardiogr. 2019, 32, 792–794. [Google Scholar] [CrossRef] [PubMed]
- Baskar, S.; Gray, S.B.; Del Grippo, E.L.; Osakwe, O.; Powell, A.W.; Tretter, J.T. Cardiac morphology for the millennial cardiology fellow: Nomenclature and advances in morphologic imaging. Congenit. Heart Dis. 2018, 13, 808–810. [Google Scholar] [CrossRef]
- Hasegawa, K.; Takaya, T.; Mori, S.; Ito, T.; Fujiwara, S.; Nishii, T.; Kono, A.K.; Shimoura, H.; Tanaka, H.; Hirata, K.I. Compression of the Right Ventricular Outflow Tract due to Straight Back Syndrome Clarified by Low-dose Dual-source Computed Tomography. Intern. Med. 2016, 55, 3279–3283. [Google Scholar] [CrossRef][Green Version]
- Ichibori, H.; Mori, S.; Takaya, T.; Kiuchi, K.; Ito, T.; Fujiwara, S.; Fukuzawa, K.; Tatsumi, K.; Tanaka, H.; Nishii, T.; et al. Slit-Like Deformation of the Coronary Sinus Orifice due to Compression of the Inferior Pyramidal Space by the Severely Dilated Left Ventricle. Pacing Clin. Electrophysiol. 2016, 39, 1026–1029. [Google Scholar] [CrossRef]
- Konishi, H.; Mori, S.; Nishii, T.; Izawa, Y.; Tamada, N.; Tanaka, H.; Kiuchi, K.; Fukuzawa, K.; Hirata, K.I. Extracardiac compression of the inferolateral branch of the coronary vein by the descending aorta in a patient with dilated cardiomyopathy. J. Arrhythm. 2017, 33, 646–648. [Google Scholar] [CrossRef]
- Izawa, Y.; Mori, S.; Nishii, T.; Matsuzoe, H.; Imada, H.; Suehiro, H.; Nakayama, K.; Matsumoto, K.; Tanaka, H.; Fujiwara, S.; et al. Optimal image reconstruction using multidetector-row computed tomography to facilitate cardiac resynchronization therapy. Echocardiography 2017, 34, 1073–1076. [Google Scholar] [CrossRef]
- Toh, H.; Mori, S.; Shimoyama, S.; Izawa, Y.; Yokota, S.; Shinkura, Y.; Takeshige, R.; Nagasawa, A.; Soga, F.; Tanaka, H.; et al. Optimal reconstruction of left ventricular outflow tract obstruction before surgical myectomy in a case with hypertrophic obstructive cardiomyopathy. Echocardiography 2018, 35, 537–540. [Google Scholar] [CrossRef]
- Burchill, L.J.; Huang, J.; Tretter, J.T.; Khan, A.M.; Crean, A.M.; Veldtman, G.R.; Kaul, S.; Broberg, C.S. Noninvasive Imaging in Adult Congenital Heart Disease. Circ. Res. 2017, 120, 995–1014. [Google Scholar] [CrossRef] [PubMed]
- Costello, J.P.; Olivieri, L.J.; Krieger, A.; Thabit, O.; Marshall, M.B.; Yoo, S.J.; Kim, P.C.; Jonas, R.A.; Nath, D.S. Utilizing Three-Dimensional Printing Technology to Assess the Feasibility of High-Fidelity Synthetic Ventricular Septal Defect Models for Simulation in Medical Education. World J. Pediatr. Congenit. Heart Surg. 2014, 5, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Bhatla, P.; Tretter, J.T.; Ludomirsky, A.; Argilla, M.; Latson, L.A.; Chakravarti, S., Jr.; Barker, P.C.; Yoo, S.J.; McElhinney, D.B.; Wake, N.; et al. Utility and Scope of Rapid Prototyping in Patients with Complex Muscular Ventricular Septal Defects or Double-Outlet Right Ventricle: Does it Alter Management Decisions? Pediatr. Cardiol. 2017, 38, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Bhatla, P.; Tretter, J.T.; Chikkabyrappa, S.; Chakravarti, S.; Mosca, R.S. Surgical planning for a complex double-outlet right ventricle using 3D printing. Echocardiography 2017, 34, 802–804. [Google Scholar] [CrossRef]
- Moore, R.A.; Riggs, K.W.; Kourtidou, S.; Schneider, K.; Szugye, N.; Troja, W.; D’Souza, G.; Rattan, M.; Bryant, R.; Taylor, M.D., III; et al. Three-dimensional printing and virtual surgery for congenital heart procedural planning. Birth Defects Res. 2018, 110, 1082–1090. [Google Scholar] [CrossRef]
- Yoo, S.J.; Spray, T.; Austin, E.H.; Yun, T.J., III; van Arsdell, G.S. Hands-on surgical training of congenital heart surgery using 3-dimensional print models. J. Thorac. Cardiovasc. Surg. 2017, 153, 1530–1540. [Google Scholar] [CrossRef]
- Jud, L.; Fotouhi, J.; Andronic, O.; Aichmair, A.; Osgood, G.; Navab, N.; Farshad, M. Applicability of augmented reality in orthopedic surgery—A systematic review. BMC Musculoskelet. Disord. 2020, 21, 103. [Google Scholar] [CrossRef]
- Elmi-Terander, A.; Burström, G.; Nachabé, R.; Fagerlund, M.; Ståhl, F.; Charalampidis, A.; Edström, E.; Gerdhem, P. Augmented reality navigation with intraoperative 3D imaging vs. fluoroscopy-assisted free-hand surgery for spine fixation surgery: A matched-control study comparing accuracy. Sci. Rep. 2020, 10, 707. [Google Scholar] [CrossRef]
- Kasamatsu, A.; Takaya, T.; Mori, S.; Kashio, K.; Takahashi, H.; Ito, T.; Takamine, S.; Fujiwara, S.; Nishii, T.; Kono, A.K.; et al. Reconstruction of an extracardiac aortocoronary collateral and simulation of selective angiography with multidetector-row computed tomography. Circulation 2015, 131, 476–479. [Google Scholar] [CrossRef]
- Gupta, S.K.; Anderson, R.H. Virtual dissection: An alternative to surface-rendered virtual three-dimensional cardiac model. Ann. Pediatr. Cardiol. 2020, 13, 102–103. [Google Scholar] [CrossRef]
- Sachdeva, S.; Gupta, S.K. Imaging Modalities in Congenital Heart Disease. Indian J. Pediatr. 2020, 87, 385–397. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, R.S.; Agger, P.; Omann, C.; Sanchez-Quintana, D.; Jarvis, J.C.; Anderson, R.H. Resolving the True Ventricular Mural Architecture. J. Cardiovasc. Dev. Dis. 2018, 5, 34. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, R.S.; Atkinson, A.; Kottas, P.; Perde, F.; Jafarzadeh, F.; Bateman, M.; Iaizzo, P.A.; Zhao, J.; Zhang, H.; Anderson, R.H.; et al. High resolution 3-Dimensional imaging of the human cardiac conduction system from microanatomy to mathematical modeling. Sci. Rep. 2017, 7, 7188. [Google Scholar] [CrossRef] [PubMed]
- Nishii, T.; Watanabe, Y.; Shimoyama, S.; Kono, A.K.; Sofue, K.; Mori, S.; Takahashi, S.; Sugimura, K. Tailored Duration of Contrast Material Injection in High-Pitch Computed Tomographic Aortography With a Double-Level Test Bolus Method. Invest. Radiol. 2017, 52, 274–280. [Google Scholar] [CrossRef]
- Han, B.K.; Rigsby, C.K.; Hlavacek, A.; Leipsic, J.; Nicol, E.D.; Siegel, M.J.; Bardo, D.; Abbara, S.; Ghoshhajra, B.; Lesser, J.R.; et al. Computed Tomography Imaging in Patients with Congenital Heart Disease Part I: Rationale and Utility. An Expert Consensus Document of the Society of Cardiovascular Computed Tomography (SCCT): Endorsed by the Society of Pediatric Radiology (SPR) and the North American Society of Cardiac Imaging (NASCI). J. Cardiovasc. Comput. Tomogr. 2015, 9, 475–492. [Google Scholar]
- Anderson, R.H.; Bolender, D.; Mori, S.; Tretter, J.T. Virtual Reality Perhaps, but Is this Real Cardiac Anatomy? Clin. Anat. 2019, 32, 468. [Google Scholar] [CrossRef]
- Bradfield, J.S.; Fujimura, O.; Boyle, N.G.; Shivkumar, K. Catheter ablation in the vicinity of the proximal conduction system: Your eyes cannot see what your mind does not know. Heart Rhythm 2019, 16, 378–379. [Google Scholar] [CrossRef]







© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tretter, J.T.; Gupta, S.K.; Izawa, Y.; Nishii, T.; Mori, S. Virtual Dissection: Emerging as the Gold Standard of Analyzing Living Heart Anatomy. J. Cardiovasc. Dev. Dis. 2020, 7, 30. https://doi.org/10.3390/jcdd7030030
Tretter JT, Gupta SK, Izawa Y, Nishii T, Mori S. Virtual Dissection: Emerging as the Gold Standard of Analyzing Living Heart Anatomy. Journal of Cardiovascular Development and Disease. 2020; 7(3):30. https://doi.org/10.3390/jcdd7030030
Chicago/Turabian StyleTretter, Justin T., Saurabh Kumar Gupta, Yu Izawa, Tatsuya Nishii, and Shumpei Mori. 2020. "Virtual Dissection: Emerging as the Gold Standard of Analyzing Living Heart Anatomy" Journal of Cardiovascular Development and Disease 7, no. 3: 30. https://doi.org/10.3390/jcdd7030030
APA StyleTretter, J. T., Gupta, S. K., Izawa, Y., Nishii, T., & Mori, S. (2020). Virtual Dissection: Emerging as the Gold Standard of Analyzing Living Heart Anatomy. Journal of Cardiovascular Development and Disease, 7(3), 30. https://doi.org/10.3390/jcdd7030030





