Effect of Yoga versus Light Exercise to Improve Well-Being and Promote Healthy Aging among Older Adults in Central India: A Study Protocol for a Randomized Controlled Trial
Abstract
:1. Introduction
1.1. Rationale
1.2. Study Objective
1.3. Specific Objectives
- Subjective well-being;
- Prevalent multiple health outcomes such as poor sleep quality, pain, depression anxiety, mood and stress;
- Balance and fear of falling and physical activity levels;
- Cognitive function;
- Cardio-metabolic measures such as blood pressure, blood glucose and blood lipids and on cortisol and other inflammatory markers.
1.4. Hypotheses
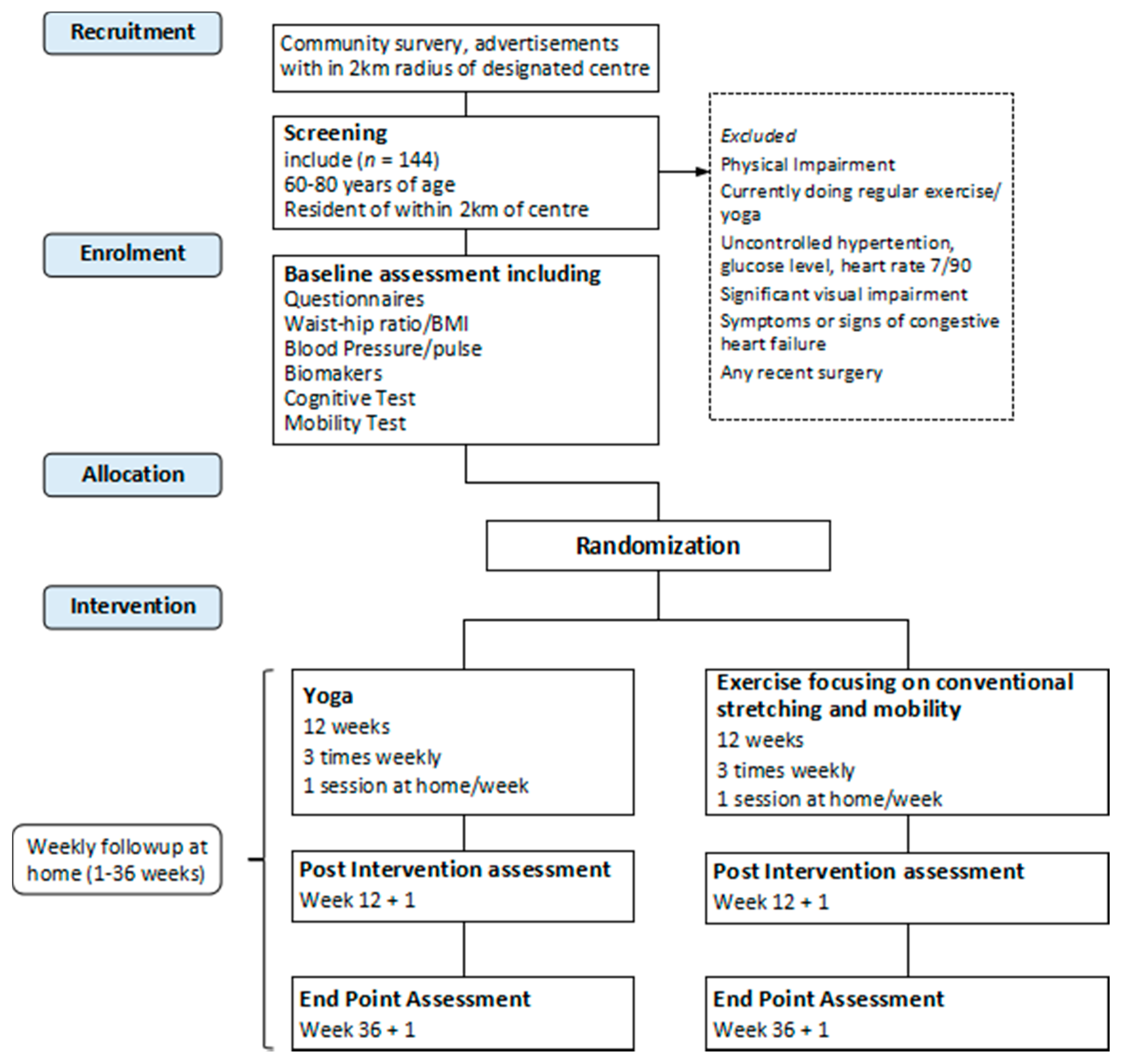
1.5. Trial Design
2. Methods
2.1. Study Setting
2.2. Inclusion Criteria
2.3. Exclusion Criteria
- Individuals currently enrolled in any other research study;
- Individuals advised by doctors to not perform exercises;
- Individuals involved in current or recent (last two months) practice of yoga or those with regular (three times per week or more) participation in other planned exercises, such as aerobics or strength training;
- Individuals with health or mobility problems that would interfere with yoga training such as paralysis or inability to sit, stand, walk and severe pain;
- Individuals having evidence of liver or kidney dysfunction, significant lung diseases, symptoms or signs of congestive heart failure, ischemic heart disease or significant valvar disease and significant visual impairment;
- Individuals having a resting heart rate >100 beats/min, uncontrolled diabetes mellitus with blood glucose measuring greater than or equal to 400 mg/dL and blood pressure >160 mmHg systolic, >100 mm Hg diastolic;
- Individuals having major surgery in the last year or planning to undergo future surgeries.
2.4. Interventions
2.4.1. Yoga
2.4.2. Light Exercise Focusing on Conventional Stretching
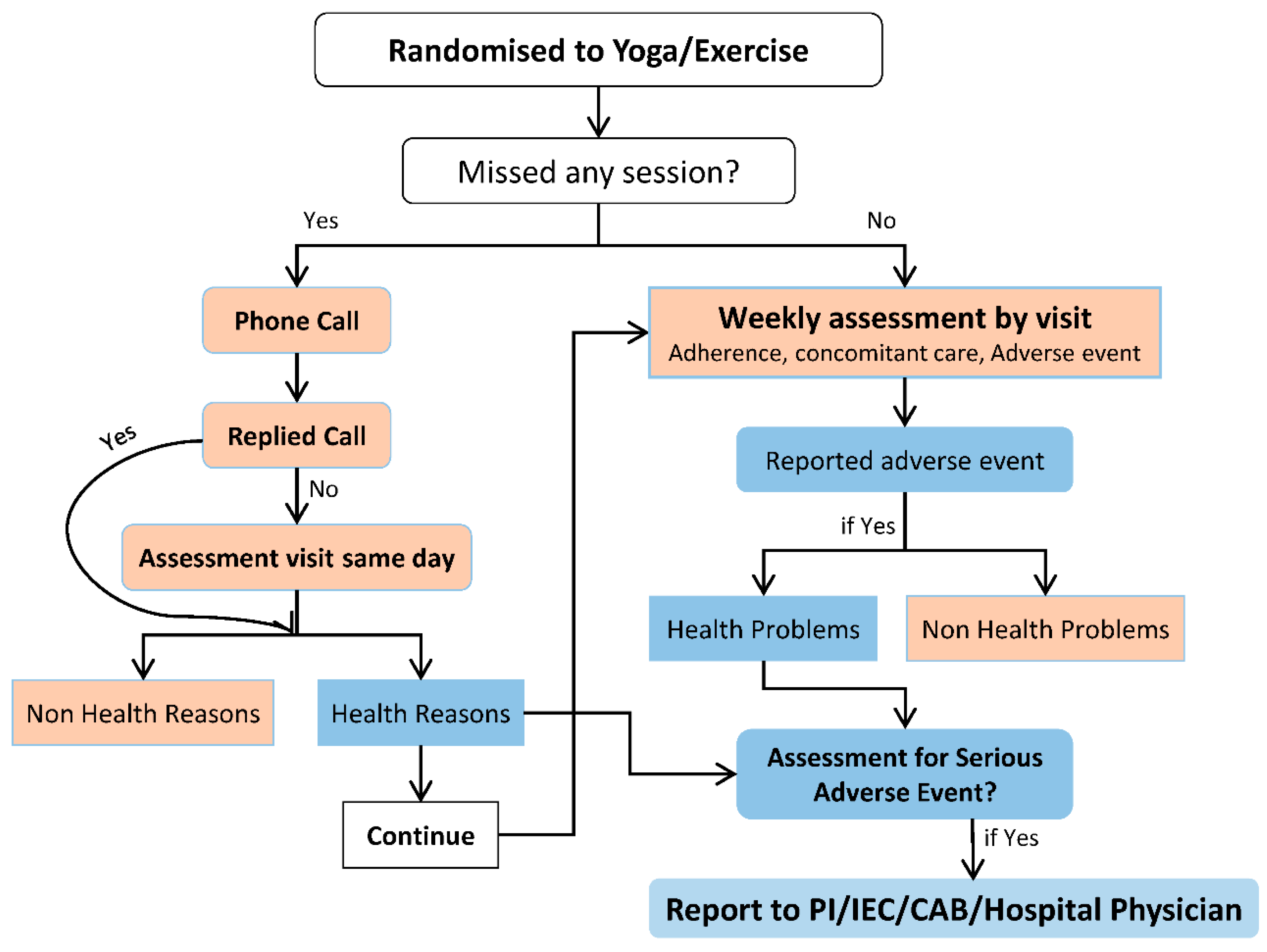
2.5. Follow-Up Visits
2.6. Strategies to Maintain Adherence
2.7. Outcomes Variables
2.7.1. Primary
2.7.2. Secondary
- The Berg balance scale, a 14-item objective measure that assesses static balance and fall risks in adults [57,58,59] and modified falls efficacy scale (MFES) [60,61], a 14-item activity questionnaire, which assesses the fear of falling among older adults in various indoor and outdoor activity, will be used to measure mobility and falls.
- Self-reported anxiety will be assessed using the geriatric anxiety inventory (GAI) scale.
- Mood states and psychological distress will be assessed using the profile of mood state questionnaire (POMS) [64].
- The perceived stress scale (PSS) will be used to assess pass month subjective stress [65].
- Body mass index (BMI), resting heart rate, blood pressure, waist–hip ratio (WHR), blood glucose, blood lipids and cortisol will be collected to assess cardio metabolic risk factors. Interleukin-6, and tumor necrosis factor-alpha will also be also examined.
2.7.3. Sample Size
2.7.4. Recruitment
2.7.5. Randomization and Blinding
2.8. Data Collection
2.8.1. Time Points
2.8.2. Baseline Assessment
2.8.3. Post Intervention and End Point Assessments
2.8.4. Biological Sampling
2.9. Follow-Up Visits
2.10. Data Management
2.11. Community Advisory Board
3. Statistical Analyses
3.1. Assessment of Adverse Events
3.2. Ethics Approvals
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Holliday, R. Understanding ageing. Philos. Trans. R. Soc. Lond. B Biol. Sci. 1997, 352, 1793–1797. [Google Scholar] [CrossRef]
- Kirkwood, T.B.L. Why and how are we living longer? Exp. Physiol. 2017, 102, 1067–1074. [Google Scholar] [CrossRef]
- Dziechciaz, M.; Filip, R. Biological psychological and social determinants of old age: Bio-psycho-social aspects of human aging. Ann. Agric. Environ. Med. 2014, 21, 835–838. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Multisectoral Action for a Life Course Approach to Healthy Ageing: DraftGlobal Strategy and Plan of Action on Ageing and Health: Report by the Secretariat. Available online: https://www.who.int/ageing/global-strategy/en/ (accessed on 1 March 2019).
- Zhou, Z.; Fu, J.; Hong, Y.A.; Wang, P.; Fang, Y. Association between exercise and the risk of dementia: Results from a nationwide longitudinal study in China. BMJ Open 2017, 7, e017497. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. PA for Health. More Active People or a Healthier World: Draft Global Action Plan on PA 2018–2030. 2018. Available online: https://apps.who.int/iris/bitstream/handle/10665/272722/9789241514187-eng.pdf?ua=1 (accessed on 1 March 2019).
- Langhammer, B.; Bergland, A.; Rydwik, E. The Importance of Physical Activity Exercise among Older People. BioMed Res. Int. 2018, 2018, 7856823. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. CMAJ 2006, 174, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Paterson, D.H.; Warburton, D.E. Physical activity and functional limitations in older adults: A systematic review related to Canada’s Physical Activity Guidelines. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 38. [Google Scholar] [CrossRef]
- Yeom, H.A.; Keller, C.; Fleury, J. Interventions for promoting mobility in community-dwelling older adults. J. Am. Acad. Nurse Pract. 2009, 21, 95–100. [Google Scholar] [CrossRef]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U.; Lancet Physical Activity Series Working Group. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Chen, K.M.; Chen, M.H.; Lin, M.H.; Fan, J.T.; Lin, H.S.; Li, C.H. Effects of yoga on sleep quality and depression in elders in assisted living facilities. J. Nurs. Res. 2010, 18, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Hariprasad, V.R.; Varambally, S.; Varambally, P.T.; Thirthalli, J.; Basavaraddi, I.V.; Gangadhar, B.N. Designing, validation and feasibility of a yoga-based intervention for elderly. Indian J. Psychiatry 2013, 55, 344–349. [Google Scholar]
- Jha, P.K. Health and social benefits from improving community hygiene and sanitation: An Indian experience. Int. J. Environ. Health Res. 2003, 13, S133–S140. [Google Scholar] [CrossRef] [PubMed]
- Youkhana, S.; Dean, C.M.; Wolff, M.; Sherrington, C.; Tiedemann, A. Yoga-based exercise improves balance and mobility in people aged 60 and over: A systematic review and meta-analysis. Age Ageing 2016, 45, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Barrows, J.L.; Fleury, J. Systematic Review of Yoga Interventions to Promote Cardiovascular Health in Older Adults. West J. Nurs. Res. 2016, 38, 753–781. [Google Scholar] [CrossRef] [PubMed]
- CDC. 2016. Available online: https://www.cdc.gov/hrqol/wellbeing.htm (accessed on 1 March 2019).
- Freedman, V.A.; Carr, D.; Cornman, J.C.; Lucas, R.E. Aging, mobility impairments and subjective wellbeing. Disabil. Health J. 2017, 10, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Deaton, A.; Stone, A.A. Subjective wellbeing, health, and ageing. Lancet 2015, 385, 640–648. [Google Scholar] [CrossRef]
- Sathyanarayanan, G.; Vengadavaradan, A.; Bharadwaj, B. Role of Yoga and Mindfulness in Severe Mental Illnesses: A Narrative Review. Int. J. Yoga 2019, 12, 3–28. [Google Scholar] [CrossRef]
- Cramer, H.; Lauche, R.; Dobos, G. Characteristics of randomized controlled trials of yoga: A bibliometric analysis. BMC Complement. Altern. Med. 2014, 14, 328. [Google Scholar] [CrossRef]
- Gothe, N.P.; McAuley, E. Yoga Is as Good as Stretching-Strengthening Exercises in Improving Functional Fitness Outcomes: Results From a Randomized Controlled Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 406–411. [Google Scholar] [CrossRef]
- Krishnamurthy, M.N.; Telles, S. Assessing depression following two ancient Indian interventions: Effects of yoga and ayurveda on older adults in a residential home. J. Gerontol. Nurs. 2007, 33, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, M.; Bhavanani, A.B.; Trakroo, M. Effect of a 12-week yoga therapy program on mental health status in elderly women inmates of a hospice. Int. J. Yoga 2017, 10, 24–28. [Google Scholar] [PubMed]
- Sivaramakrishnan, D.; Fitzsimons, C.; Kelly, P.; Ludwig, K.; Mutrie, N.; Saunders, D.H.; Baker, G. The effects of yoga compared to active and inactive controls on physical function and health related quality of life in older adults—Systematic review and meta-analysis of randomised controlled trials. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 33. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.Y.; Chang, H.Y.; Lin, C.Y. Systematic review of yoga for depression and quality of sleep in the elderly. Hu Li Za Zhi. 2014, 61, 85–92. [Google Scholar] [PubMed]
- Starkweather, A.R. The effects of exercise on perceived stress and IL-6 levels among older adults. Biol. Res. Nurs. 2007, 8, 186–194. [Google Scholar] [CrossRef]
- Groessl, E.J.; Schmalzl, L.; Maiya, M.; Liu, L.; Goodman, D.; Chang, D.G.; Wetherell, J.L.; Bormann, J.E.; Atkinson, J.H.; Baxi, S. Yoga for veterans with chronic low back pain: Design and methods of a randomized clinical trial. Contemp. Clin. Trials 2016, 48, 110–118. [Google Scholar] [CrossRef]
- Woodyard, C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int. J. Yoga 2011, 4, 49–54. [Google Scholar] [CrossRef]
- Hariprasad, V.R.; Sivakumar, P.T.; Koparde, V.; Varambally, S.; Thirthalli, J.; Varghese, M.; Basavaraddi, I.V.; Gangadhar, B.N. Effects of yoga intervention on sleep and quality-of-life in elderly: A randomized controlled trial. Indian J. Psychiatry 2013, 55, S364–S368. [Google Scholar]
- Groessl, E.J.; Maiya, M.; Schmalzl, L.; Wing, D.; Jeste, D.V. Yoga to prevent mobility limitations in older adults: Feasibility of a randomized controlled trial. BMC Geriatr. 2018, 18, 306. [Google Scholar] [CrossRef]
- Zettergren, K.K.; Lubeski, J.M.; Viverito, J.M. Effects of a yoga program on postural control, mobility, and gait speed in community-living older adults: A pilot study. J. Geriatr. Phys. Ther. 2011, 34, 88–94. [Google Scholar] [CrossRef]
- Brunner, D.; Abramovitch, A.; Etherton, J. A yoga program for cognitive enhancement. PLoS ONE 2017, 12, e0182366. [Google Scholar] [CrossRef] [PubMed]
- Chu, P.; Gotink, R.A.; Yeh, G.Y.; Goldie, S.J.; Hunink, M.G. The effectiveness of yoga in modifying risk factors for cardiovascular disease and metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Prev. Cardiol. 2016, 23, 291–307. [Google Scholar] [CrossRef] [PubMed]
- Paikkatt, B.; Singh, A.R.; Singh, P.K.; Jahan, M. Efficacy of yoga therapy on subjective well-being and basic living skills of patients having chronic schizophrenia. Indian Psychiatry J. 2012, 21, 109–114. [Google Scholar]
- Tulloch, A.; Bombell, H.; Dean, C.; Tiedemann, A. Yoga-based exercise improves health-related quality of life and mental well-being in older people: A systematic review of randomised controlled trials. Age Ageing 2018, 47, 537–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Djalilova, D.M.; Schulz, P.S.; Berger, A.M.; Case, A.J.; Kupzyk, K.A.; Ross, A.C. Impact of Yoga on Inflammatory Biomarkers: A Systematic Review. Biol. Res. Nurs. 2019, 21, 198–209. [Google Scholar] [CrossRef] [PubMed]
- Harkess, K.N.; Ryan, J.; Delfabbro, P.H.; Cohen-Woods, S. Preliminary indications of the effect of a brief yoga intervention on markers of inflammation and DNA methylation in chronically stressed women. Transl. Psychiatry 2016, 6, e965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, K.M.; Chen, M.H.; Hong, S.M.; Chao, H.C.; Lin, H.S.; Li, C.H. Physical fitness of older adults in senior activity centres after 24-week silver yoga exercises. J. Clin. Nurs. 2008, 17, 2634–2646. [Google Scholar] [CrossRef]
- Gothe, N.P.; Kramer, A.F.; McAuley, E. Hatha Yoga Practice Improves Attention and Processing Speed in Older Adults: Results from an 8-Week Randomized Control Trial. J. Altern. Complement. Med. 2017, 23, 35–40. [Google Scholar] [CrossRef]
- Oken, B.S.; Zajdel, D.; Kishiyama, S.; Flegal, K.; Dehen, C.; Haas, M.; Kraemer, D.F.; Lawrence, J.; Leyva, J. Randomized, controlled, six-month trial of yoga in healthy seniors: Effects on cognition and quality of life. Altern. Ther. Health Med. 2006, 12, 40–47. [Google Scholar]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Picorelli, A.M.; Pereira, D.S.; Felicio, D.C.; Dos Anjos, D.M.; Pereira, D.A.; Dias, R.C.; Assis, M.G.; Pereira, L.S. Adherence of older women with strength training and aerobic exercise. Clin. Interv. Aging 2014, 9, 323–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Govindaraj, R.; Karmani, S.; Varambally, S.; Gangadhar, B.N. Yoga and physical exercise—A review and comparison. Int. Rev. Psychiatry 2016, 28, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Park, C.L.; Groessl, E.; Maiya, M.; Sarkin, A.; Eisen, S.V.; Riley, K.; Elwy, A.R. Comparison groups in yoga research: A systematic review and critical evaluation of the literature. Complement. Ther. Med. 2014, 22, 920–929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lau, C.; Yu, R.; Woo, J. Effects of a 12-Week Hatha Yoga Intervention on Metabolic Risk and Quality of Life in Hong Kong Chinese Adults with and without Metabolic Syndrome. PLoS ONE 2015, 10, e0130731. [Google Scholar] [CrossRef] [PubMed]
- Greendale, G.A.K.L.; Mazdyasni, S.; Ramirez, E.; Wang, M.Y.; Yu, S.S.; Salem, G. Yoga Empowers Seniors Study (YESS): Design and Asana Series. J. Yoga Phys. Ther. 2012, 2, 107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keadle, S.K.; McKinnon, R.; Graubard, B.I.; Troiano, R.P. Prevalence and trends in physical activity among older adults in the United States: A comparison across three national surveys. Prev. Med. 2016, 89, 37–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borg, C.; Hallberg, I.R.; Blomqvist, K. Life satisfaction among older people (65+) with reduced self-care capacity: The relationship to social, health and financial aspects. J. Clin. Nurs. 2006, 15, 607–618. [Google Scholar] [CrossRef]
- Wood, V.; Wylie, M.L.; Sheafor, B. An analysis of a short self-report measure of life satisfaction: Correlation with rater judgments. J. Gerontol. 1969, 24, 465–469. [Google Scholar] [CrossRef]
- Adams, D.L. Analysis of a life satisfaction index. J. Gerontol. 1969, 24, 470–474. [Google Scholar] [CrossRef]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The Satisfaction with Life Scale. J. Personal. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Misra, P.; Upadhyay, R.P.; Krishnan, A.; Sharma, N.; Kapoor, S.K. A community based study to test the reliability and validity of physical activity measurement techniques. Int. J. Prev. Med. 2014, 5, 952–959. [Google Scholar] [PubMed]
- Rosenbaum, S.; Ward, P.B.; International Working, G. The Simple Physical Activity Questionnaire. Lancet Psychiatry 2016, 3, e1. [Google Scholar] [CrossRef] [Green Version]
- Berg, K.W.-D.S.; Williams, J.I.; Maki, B. Measuring balance in the elderly: Validation of an instrument. Can. J. Public Health 1992, 83, S7–S11. [Google Scholar] [PubMed]
- Berg, K.W.-D.S.; Williams, J.I.; Gayton, D. Measuring balance in the elderly: Priliminary development of an instrument. Physiotherpy Can. 1989, 41, 304–311. [Google Scholar] [CrossRef]
- Berg, K.W.-D.S.; Williams, J.I. The balance sacle: Reliability assessment with elderly residents and patient with an acute stroke. Scand. J. Rehabil. Med. 1995, 27, 27–36. [Google Scholar]
- Joshi, S.K.G. Validation of the Gujarati and Hindi Versions of Modified Falls Efficacy Scale. Ann. Physiother. Occup. Ther. 2018, 1, 2294–2303. [Google Scholar]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef] [Green Version]
- Ganguli, M.; Dube, S.; Johnston, J.M.; Pandav, R.; Chandra, V.; Dodge, H.H. Depressive symptoms, cognitive impairment and functional impairment in a rural elderly population in India: A Hindi version of the geriatric depression scale (GDS-H). Int. J. Geriatr. Psychiatry 1999, 14, 807–820. [Google Scholar] [CrossRef]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiatr. Res. 1982, 17, 37–49. [Google Scholar] [CrossRef]
- Berger, B.G.; Motl, P.W. Exercise and mood: A selective review and synthesis of research employing the profile of mood states. J. Appl. Sport Psychol. 2000, 12, 69–92. [Google Scholar] [CrossRef]
- Cohen SKamarck, T.; Mermeistein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Cleeland, C.S.R.K. The Brief Pain Inventory; Pain Research Group: 1991. The University of Texas M. D. Anderson Cancer Center, Houston. Available online: http://www.npcrc.org/files/news/briefpain_long.pdf (accessed on 27 April 2019).
- Saxena, A.; Mendoza, T.; Cleeland, C.S. The assessment of cancer pain in north India: The validation of the Hindi Brief Pain Inventory—BPI-H. J. Pain Symptom Manag. 1999, 17, 27–41. [Google Scholar] [CrossRef]
- Lahan, V.; Gupta, R. Translation and validation of the Insomnia Seveity Index in Hindi Language. Indian J. Psycological Med. 2011, 33, 172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morin, C.M.; Belleville, G.; Belanger, L.; Ivers, H. The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011, 34, 601–608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. ‘Mini-Mentle State’ A practical method for grading the congnitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Ganguli, M.; Ratcliff, G.; Chandra, V.; Sharma, S.; Gilby, J.; Pandav, R.; Belle, S.; Ryan, C.; Baker, C.; Seaberg, E.; et al. A Hindi Version of The MMSE: The development of a cognitive screening instrument for a largely illiterate rural elderly population in india. Int. J. Geristric Psychiatry 1995, 10, 367–377. [Google Scholar] [CrossRef]
- Cramer, H.; Haller, H.; Dobos, G.; Lauche, R. A Systematic Review and Meta-Analysis Estimating the Expected Dropout Rates in Randomized Controlled Trials on Yoga Interventions. Evid.-Based Complement. Altern. Med. 2016, 2016, 5859729. [Google Scholar] [CrossRef] [Green Version]
- Cramer, H.; Ostermann, T.; Dobos, G. Injuries and other adverse events associated with yoga practice: A systematic review of epidemiological studies. J. Sci. Med. Sport 2018, 21, 147–154. [Google Scholar] [CrossRef]
- Bussing, A.; Michalsen, A.; Khalsa, S.B.; Telles, S.; Sherman, K.J. Effects of yoga on mental and physical health: A short summary of reviews. Evid.-Based Complement. Altern. Med. 2012, 2012, 165410. [Google Scholar] [CrossRef] [Green Version]
- Patel, N.K.; Newstead, A.H.; Ferrer, R.L. The effects of yoga on physical functioning and health related quality of life in older adults: A systematic review and meta-analysis. J. Altern. Complement. Med. 2012, 18, 902–917. [Google Scholar] [CrossRef] [PubMed]
- Balasubramaniam, M.; Telles, S.; Doraiswamy, P.M. Yoga on our minds: A systematic review of yoga for neuropsychiatric disorders. Front. Psychiatry 2012, 3, 117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahidi, M.; Mojtahed, A.; Modabbernia, A.; Mojtahed, M.; Shafiabady, A.; Delavar, A.; Delavar, A.; Honari, H. Laughter yoga versus group exercise program in elderly depressed women: A randomized controlled trial. Int. J. Geriatr. Psychiatry 2011, 26, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Beena, R.K.; Sreekumaran, E. Yogic practice and diabetes mellitus in geriatric patients. Int. J. Yoga 2013, 6, 47. [Google Scholar]
- Galantino, M.L.; Green, L.; Decesari, J.A.; Mackain, N.A.; Rinaldi, S.M.; Stevens, M.E.; Wurst, V.R.; Marsico, R.; Nell, M.; Mao, J.J. Safety and feasibility of modified chair-yoga on functional outcome among elderly at risk for falls. Int. J. Yoga 2012, 5, 146–150. [Google Scholar] [CrossRef]
- Saravanakumar, P.; Higgins, I.J.; van der Riet, P.J.; Marquez, J.; Sibbritt, D. The influence of tai chi and yoga on balance and falls in a residential care setting: A randomised controlled trial. Contemp. Nurse 2014, 48, 76–87. [Google Scholar] [CrossRef]
| Study Period | ||||||
|---|---|---|---|---|---|---|
| Time Point | Enrolment | Baseline | Intervention | Post Intervention | Endpoint | |
| week −1 | week 0 | week 1–12 | week 12+1 | week 36+1 | ||
| Eligibility Screen | ✓ | |||||
| Informed Consent | ✓ | |||||
| Allocation | ✓ | |||||
| Intervention | ||||||
| Yoga |  | |||||
| Light Aerobic Exercise |  | |||||
| Study Outcomes | Methods for Assessment | |||||
| Demographic | Socio-economic questionnaire | ✓ | ✓ | ✓ | ||
| Well-being | Life Satisfaction Index Z Satisfaction with Life Scale | ✓ | ✓ | ✓ | ||
| Mobility/fall risk | Modified Falls Efficacy Scale Berg Balance Scale | ✓ | ✓ | ✓ | ||
| Pain | Brief Pain Inventory | ✓ | ✓ | ✓ | ||
| Mood | Profile of Mood Status | ✓ | ✓ | ✓ | ||
| Stress | Perceived Stress Scale | ✓ | ✓ | ✓ | ||
| Anxiety | Geriatric Anxiety Inventory | ✓ | ✓ | ✓ | ||
| Depression | Geriatric Depression Scale | ✓ | ✓ | ✓ | ||
| Physical Activity | International Physical Activity Questionnaire | ✓ | ✓ | ✓ | ||
| Sedentary behavior | Simple Physical Activity Questionnaire | ✓ | ✓ | ✓ | ||
| Sleep quality | Insomnia Severity Index | ✓ | ✓ | ✓ | ||
| Cognition | Mini Mental State Examination | ✓ | ✓ | ✓ | ||
| Cardio Metabolic Risk | Blood pressure, resting heart rate, BMI, WHR | ✓ | ✓ | ✓ | ||
| Blood tests | Complete blood count, Blood glucose, Blood lipids, IL-6, TNF-α, CRP, Cortisol | ✓ | ✓ | ✓ | ||
| Followup | Followup visit to participant’s home to check adherence/modification/adverse events | Weekly home visit from week 1 to week 36 | ||||
| Feedback | Feedback and participants satisfaction | ✓ | ||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choudhary, A.; Pathak, A.; Manickam, P.; Purohit, M.; Rajasekhar, T.D.; Dhoble, P.; Sharma, A.; Suliya, J.; Apsingekar, D.; Patil, V.; et al. Effect of Yoga versus Light Exercise to Improve Well-Being and Promote Healthy Aging among Older Adults in Central India: A Study Protocol for a Randomized Controlled Trial. Geriatrics 2019, 4, 64. https://doi.org/10.3390/geriatrics4040064
Choudhary A, Pathak A, Manickam P, Purohit M, Rajasekhar TD, Dhoble P, Sharma A, Suliya J, Apsingekar D, Patil V, et al. Effect of Yoga versus Light Exercise to Improve Well-Being and Promote Healthy Aging among Older Adults in Central India: A Study Protocol for a Randomized Controlled Trial. Geriatrics. 2019; 4(4):64. https://doi.org/10.3390/geriatrics4040064
Chicago/Turabian StyleChoudhary, Anita, Ashish Pathak, Ponnaiah Manickam, Manju Purohit, Thomas Daniel Rajasekhar, Parag Dhoble, Ashish Sharma, Juhi Suliya, Dhanashree Apsingekar, Vandana Patil, and et al. 2019. "Effect of Yoga versus Light Exercise to Improve Well-Being and Promote Healthy Aging among Older Adults in Central India: A Study Protocol for a Randomized Controlled Trial" Geriatrics 4, no. 4: 64. https://doi.org/10.3390/geriatrics4040064
APA StyleChoudhary, A., Pathak, A., Manickam, P., Purohit, M., Rajasekhar, T. D., Dhoble, P., Sharma, A., Suliya, J., Apsingekar, D., Patil, V., Jaiswal, A., Gwarikar, S., Östh, J., Jirwe, M., Diwan, V. K., Hallgren, M., Mahadik, V., & Diwan, V. (2019). Effect of Yoga versus Light Exercise to Improve Well-Being and Promote Healthy Aging among Older Adults in Central India: A Study Protocol for a Randomized Controlled Trial. Geriatrics, 4(4), 64. https://doi.org/10.3390/geriatrics4040064






