Preliminary Bioequivalence of an Oral Pimobendan Solution Formulation with Reference Solution Formulation in Beagle Dogs
Abstract
:1. Introduction
2. Materials and Methods
2.1. Pimobendan Oral Solution Formulation
2.2. Animals
2.3. Drug Administration and Blood Sample Acquisition
2.4. Drug Analysis by Liquid Chromatography Tandem Mass Spectrometry
2.5. Pharmacokinetics
2.6. Effects of Drugs on Cardiac Function
2.7. Bioequivalence and Data Analysis
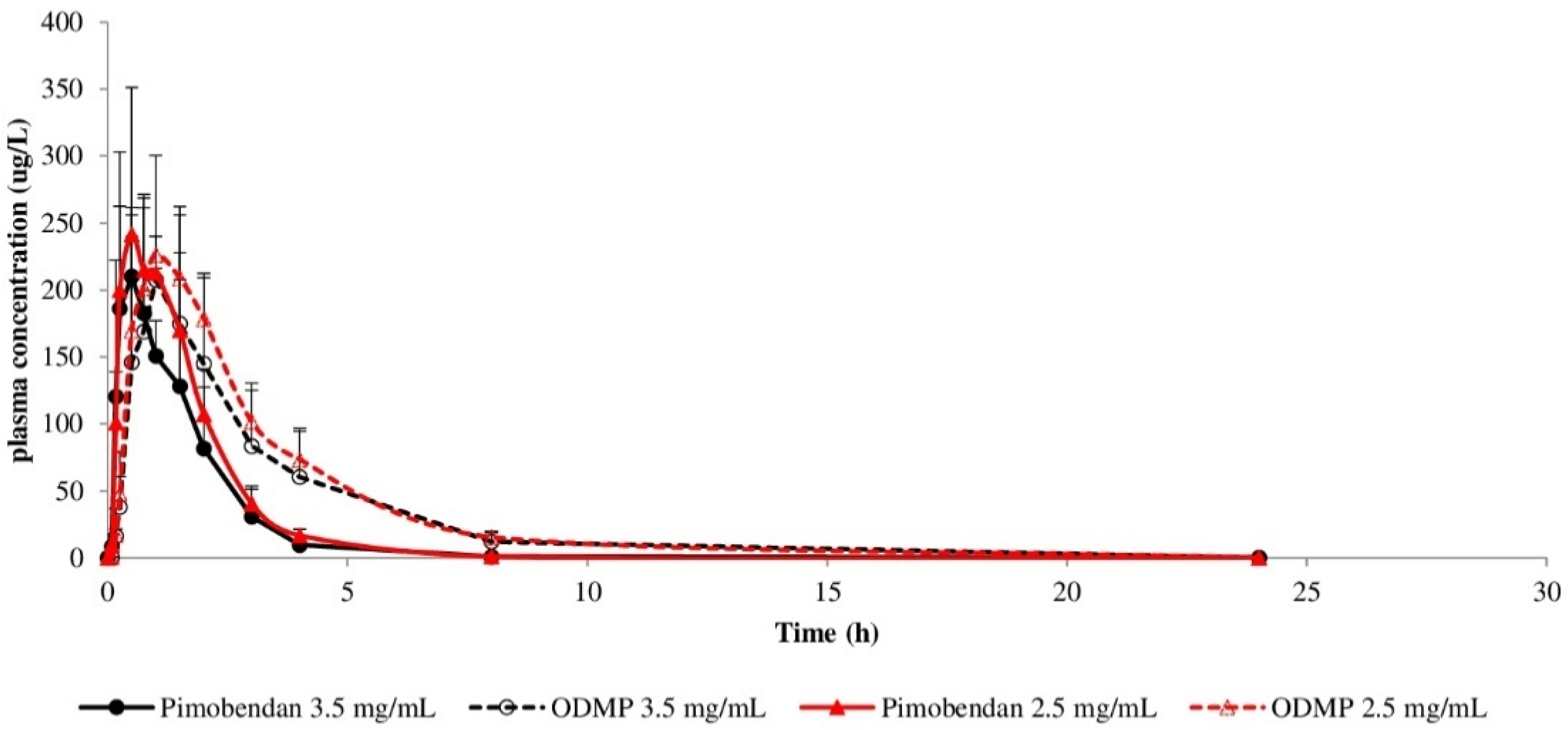
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bell, E.T.; Devi, J.L.; Chiu, S.; Zahra, P.; Whittem, T. The pharmacokinetics of pimobendan enantiomers after oral and intravenous administration of racemate pimobendan formulations in healthy dogs. J. Vet. Pharmacol. Ther. 2016, 39, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Lombard, C.W.; Jons, O.; Bussadori, C.M. Clinical efficacy of pimobendan versus benazepril for the treatment of acquired atrioventricular valvular disease in dogs. J. Am. Anim. Hosp. Assoc. 2006, 42, 249–261. [Google Scholar] [CrossRef]
- Atkins, C.E.; Haggstrom, J. Pharmacologic management of myxomatous mitral valve disease in dogs. J. Vet. Cardiol. 2012, 14, 165–184. [Google Scholar] [CrossRef] [PubMed]
- Boswood, A.; Gordon, S.G.; Haggstrom, J.; Wess, G.; Stepien, R.L.; Oyama, M.A.; Keene, B.W.; Bonagura, J.; MacDonald, K.A.; Patteson, M.; et al. Longitudinal Analysis of Quality of Life, Clinical, Radiographic, Echocardiographic, and Laboratory Variables in Dogs with Preclinical Myxomatous Mitral Valve Disease Receiving Pimobendan or Placebo: The EPIC Study. J. Vet. Intern. Med. 2018, 32, 72–85. [Google Scholar] [CrossRef] [PubMed]
- Boswood, A.; Haggstrom, J.; Gordon, S.G.; Wess, G.; Stepien, R.L.; Oyama, M.A.; Keene, B.W.; Bonagura, J.; MacDonald, K.A.; Patteson, M.; et al. Effect of Pimobendan in Dogs with Preclinical Myxomatous Mitral Valve Disease and Cardiomegaly: The EPIC Study-A Randomized Clinical Trial. J. Vet. Intern. Med. 2016, 30, 1765–1779. [Google Scholar] [CrossRef] [PubMed]
- Keene, B.W.; Atkins, C.E.; Bonagura, J.D.; Fox, P.R.; Haggstrom, J.; Fuentes, V.L.; Oyama, M.A.; Rush, J.E.; Stepien, R.; Uechi, M. ACVIM consensus guidelines for the diagnosis and treatment of myxomatous mitral valve disease in dogs. J. Vet. Intern. Med. 2019, 33, 1127–1140. [Google Scholar] [CrossRef] [PubMed]
- Yata, M.; McLachlan, A.J.; Foster, D.J.; Page, S.W.; Beijerink, N.J. Pharmacokinetics and cardiovascular effects following a single oral administration of a nonaqueous pimobendan solution in healthy dogs. J. Vet. Pharmacol. Ther. 2016, 39, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Boehringer Ingelheim. Vetmedin (Pimobendan) Chewable Tablets [Package Insert]; Boehringer Ingelheim: St. Joseph, MO, USA, 2012. [Google Scholar]
- Papich, M.G. Pimobendan. In Saunders Handbook of Veterinary Drugs, 4th ed.; Papich, M.G., Ed.; W.B. Saunders: London, UK, 2016; pp. 638–640. [Google Scholar]
- Yata, M.; McLachlan, A.J.; Foster, D.J.; Hanzlicek, A.S.; Beijerink, N.J. Single-dose pharmacokinetics and cardiovascular effects of oral pimobendan in healthy cats. J. Vet. Cardiol. 2016, 18, 310–325. [Google Scholar] [CrossRef] [PubMed]
- NRC. Guide for the Care and Use of Laboratory Animals, 8th ed.; National Academies Press (US): Washington, DC, USA, 2011. [Google Scholar]
- EMEA. Guideline on the Investigatin of Bioequivalence. 2010. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-investigation-bioequivalence-rev1_en.pdf (accessed on 14 February 2022).
- Pichayapaiboon, P.; Tantisuwat, L.; Boonpala, P.; Saengklub, N.; Boonyarattanasoonthorn, T.; Khemawoot, P.; Kijtawornrat, A. Pharmacodynamics and Pharmacokinetics of Injectable Pimobendan and Its Metabolite, O-Desmethyl-Pimobendan, in Healthy Dogs. Front. Vet. Sci. 2021, 8, 656902. [Google Scholar] [CrossRef] [PubMed]
- Schiller, N.B.; Shah, P.M.; Crawford, M.; DeMaria, A.; Devereux, R.; Feigenbaum, H.; Gutgesell, H.; Reichek, N.; Sahn, D.; Schnittger, I.; et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J. Am. Soc. Echocardiogr. 1989, 2, 358–367. [Google Scholar] [CrossRef]
- Lang, R.M.; Bierig, M.; Devereux, R.B.; Flachskampf, F.A.; Foster, E.; Pellikka, P.A.; Picard, M.H.; Roman, M.J.; Seward, J.; Shanewise, J.S.; et al. Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J. Am. Soc. Echocardiogr. 2005, 18, 1440–1463. [Google Scholar] [CrossRef] [PubMed]
- Saengklub, N.; Pirintr, P.; Nampimoon, T.; Kijtawornrat, A.; Chaiyabutr, N. Short-Term Effects of Sacubitril/valsartan on Echocardiographic Parameters in Dogs with Symptomatic Myxomatous Mitral Valve Disease. Front. Vet. Sci. 2021, 8, 700230. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Kim, S.; Lee, J.; Choi, J.C.; Kim, Y.; Park, C.W.; Lee, S. Preliminary bioequivalence of an oral integrating film formulation containing meloxicam with a suspension formulation in beagle dogs. J. Vet. Pharmacol. Ther. 2021, 44, 342–348. [Google Scholar] [CrossRef] [PubMed]
- FDA. Guidance for Industry: Statistical Approaches to Establishing Bioequivalence. 2001. Available online: https://www.fda.gov/media/70958/download (accessed on 14 February 2022).
- Her, J.; Kuo, K.W.; Winter, R.L.; Cruz-Espindola, C.; Bacek, L.M.; Boothe, D.M. Pharmacokinetics of Pimobendan and Its Metabolite O-Desmethyl-Pimobendan Following Rectal Administration to Healthy Dogs. Front. Vet. Sci. 2020, 7, 423. [Google Scholar] [CrossRef] [PubMed]
- Bohm, M.; Morano, I.; Pieske, B.; Ruegg, J.C.; Wankerl, M.; Zimmermann, R.; Erdmann, E. Contribution of cAMP-phosphodiesterase inhibition and sensitization of the contractile proteins for calcium to the inotropic effect of pimobendan in the failing human myocardium. Circ. Res. 1991, 68, 689–701. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Endoh, M.; Shibasaki, T.; Satoh, H.; Norota, I.; Ishihata, A. Different mechanisms involved in the positive inotropic effects of benzimidazole derivative UD-CG 115 BS (pimobendan) and its demethylated metabolite UD-CG 212 Cl in canine ventricular myocardium. J. Cardiovasc. Pharmacol. 1991, 17, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Kass, D.A.; Solaro, R.J. Mechanisms and use of calcium-sensitizing agents in the failing heart. Circulation 2006, 113, 305–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pagel, P.S.; Hettrick, D.A.; Warltier, D.C. Influence of levosimendan, pimobendan, and milrinone on the regional distribution of cardiac output in anaesthetized dogs. Br. J. Pharmacol. 1996, 119, 609–615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hori, Y.; Taira, H.; Nakajima, Y.; Ishikawa, Y.; Yumoto, Y.; Maekawa, Y.; Oshiro, A. Inotropic effects of a single intravenous recommended dose of pimobendan in healthy dogs. J. Vet. Med. Sci. 2019, 81, 22–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| PK Parameters | Pimobendan | O-Desmethyl-Pimobendan (ODMP) | ||||||
|---|---|---|---|---|---|---|---|---|
| Reference | PS | Ratio # | 90% CI # | Reference | PS | Ratio # | 90% CI # | |
| Cmax (µg/L) | 240.9 ± 15.6 | 269.6 ± 50.4 | 89.1 | 80.9–97.3 | 241.8 ± 64.4 | 253.3 ± 8.7 | 95.5 | 85.1–107.2 |
| Tmax (h) | 0.67 ± 0.29 | 0.75 ± 0.29 | 88.0 | 66.0–115.2 | 1.10 ± 0.36 | 1.15 ± 0.40 | 95.7 | 75.3–119.6 |
| AUC0–24 (µg.h/L) | 414.4 ± 98.2 | 439.5 ± 55.5 | 95.5 | 83.2–109.7 | 880.3 ± 82.4 | 818.1 ± 79.7 | 107.2 | 97.3–115.5 |
| AUC0–inf (µg.h/L) | 415.5 ± 98.2 | 440.3 ± 55.4 | 95.5 | 82.6–108.9 | 880.6 ± 82.4 | 818.4 ± 79.7 | 107.2 | 98.3–115.5 |
| MRT (h) | 8.27 ± 0.25 | 8.50 ± 0.87 | 97.8 | 93.3–104.7 | 5.07 ± 0.68 | 5.00 ± 0.30 | 100.0 | 93.4–107.2 |
| Vd (L/kg) | 43.9 ± 10.4 | 43.2 ± 9.3 | 100.0 | 82.9–119.9 | 9.23 ± 0.72 | 8.67 ± 1.15 | 107.1 | 97.6–117.5 |
| CL (L/h/kg) | 5.80 ± 1.59 | 5.74 ± 0.71 | 100.0 | 85.9–115.9 | 2.86 ± 0.28 | 2.92 ± 0.39 | 97.6 | 89.2–104.8 |
| Half-life (h) | 4.72 ± 0.19 | 4.68 ± 0.53 | 100.0 | 93.2–107.1 | 2.25 ± 0.22 | 2.21 ± 0.10 | 102.3 | 97.7–125.7 |
| Timepoints | Formulations | LA/Ao | LVIDDN (cm) | LVIDSN (cm) | EDVI | ESVI | EF (%) | SV (mL) | CO (L/min) | HR (bpm) |
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Reference (3.5 mg/mL) | 1.4 ± 0.09 | 1.4 ± 0.04 | 0.9 ± 0.03 | 65.8 ± 4.3 | 22.1 ± 1.8 | 66.6 ± 0.8 | 24.4 ± 1.7 | 2.5 ± 0.44 | 102 ± 14.6 |
| PS (2.5 mg/mL) | 1.3 ± 0.05 | 1.4 ± 0.04 | 0.9 ± 0.03 | 63.4 ± 4.4 | 22.1 ± 1.6 | 64.8 ± 0.5 | 23.0 ± 1.7 | 2.4 ± 0.13 | 107 ± 4.9 | |
| 0.083 h | Reference (3.5 mg/mL) | 1.3 ± 0.04 | 1.4 ± 0.02 | 0.9 ± 0.01 | 60.1 ± 2.1 | 20.6 ± 0.8 | 65.6 ± 0.4 | 22.0 ± 0.7 | 2.2 ± 0.27 | 98 ± 9.3 |
| PS (2.5 mg/mL) | 1.3 ± 0.09 | 1.4 ± 0.05 | 0.8 ± 0.03 | 59.6 ± 5.7 | 19.9 ± 1.8 | 66.6 ± 0.3 | 22.0 ± 2.0 | 2.1 ± 0.14 | 96 ± 4.4 | |
| 0.167 h | Reference (3.5 mg/mL) | 1.3 ± 0.04 | 1.4 ± 0.05 | 0.8 ± 0.05 | 63.9 ± 5.6 | 19.7 ± 2.5 | 69.3 ± 1.9 | 24.1 ± 1.9 | 2.4 ± 0.18 | 97 ± 9.0 |
| PS (2.5 mg/mL) | 1.3 ± 0.07 | 1.4 ± 0.03 | 0.9 ± 0.02 | 60.8 ± 3.4 | 19.9 ± 1.0 | 67.2 ± 0.5 | 22.7 ± 1.2 | 1.9 ± 0.12 | 83 ± 4.1 | |
| 0.25 h | Reference (3.5 mg/mL) | 1.3 ± 0.05 | 1.4 ± 0.05 | 0.8 ± 0.02 | 57.7 ± 5.8 | 17.1 ± 1.1 * | 70.0 ± 1.1 * | 22.5 ± 2.4 | 1.8 ± 0.31 | 91 ± 13.4 |
| PS (2.5 mg/mL) | 1.2 ± 0.05 | 1.4 ± 0.03 | 0.8 ± 0.01 | 60.7 ± 3.2 | 17.9 ± 0.7 * | 70.4 ± 1.4 | 23.8 ± 1.3 | 1.9 ± 0.20 | 82 ± 8.9 | |
| 0.50 h | Reference (3.5 mg/mL) | 1.2 ± 0.06 | 1.4 ± 0.07 | 0.7 ± 0.03 * | 61.9 ± 7.4 | 12.6 ± 1.4 * | 79.2 ± 1.9 * | 27.2 ± 3.1 | 2.6 ± 0.45 | 97 ± 14.5 |
| PS (2.5 mg/mL) | 1.3 ± 0.05 | 1.4 ± 0.06 | 0.7 ± 0.04 * | 58.1 ± 6.0 | 13.3 ± 1.9 * | 77.0 ± 2.4 * | 24.7 ± 2.4 | 2.3 ± 0.24 | 95 ± 9.1 | |
| 0.75 h | Reference (3.5 mg/mL) | 1.3 ± 0.05 | 1.4 ± 0.04 | 0.7 ± 0.03 * | 59.7 ± 3.8 | 11.3 ± 1.4 * | 81.3 ± 1.8 * | 26.9 ± 1.6 | 2.5 ± 0.19 | 95 ± 6.6 |
| PS (2.5 mg/mL) | 1.3 ± 0.03 | 1.3 ± 0.03 | 0.7 ± 0.03 * | 55.2 ± 2.9 | 10.8 ± 1.1 * | 80.3 ± 2.5 * | 24.6 ± 1.6 | 2.2 ± 0.11 | 92 ± 7.6 | |
| 1 h | Reference (3.5 mg/mL) | 1.2 ± 0.06 | 1.3 ± 0.05 | 0.6 ± 0.02 * | 53.7 ± 4.8 | 7.5 ± 0.6 * | 86.0 ± 1.0 * | 25.6 ± 2.1 | 2.4 ± 0.15 | 98 ± 13.0 |
| PS (2.5 mg/mL) | 1.2 ± 0.03 | 1.3 ± 0.07 | 0.6 ± 0.05 * | 55.1 ± 7.2 | 8.1 ± 1.7 * | 85.7 ± 1.5 * | 26.0 ± 2.8 | 2.6 ± 0.25 | 103 ± 11.7 | |
| 1.5 h | Reference (3.5 mg/mL) | 1.2 ± 0.05 | 1.3 ± 0.04 | 0.5 ± 0.01 * | 53.6 ± 3.7 | 5.8 ± 0.3 * | 89.0 ± 0.3 * | 26.5 ± 1.6 * | 3.0 ± 0.22 | 114 ± 11.9 |
| PS (2.5 mg/mL) | 1.3 ± 0.04 | 1.4 ± 0.04 | 0.5 ± 0.01 * | 57.3 ± 4.2 | 6.0 ± 0.3 * | 89.5 ± 0.4 * | 29.2 ± 1.3 * | 2.7 ± 0.41 | 97 ± 12.6 | |
| 2 h | Reference (3.5 mg/mL) | 1.3 ± 0.10 | 1.4 ± 0.05 | 0.5 ± 0.02 * | 56.7 ± 5.4 | 4.9 ± 0.6 * | 91.3 ± 0.4 * | 28.6 ± 2.1 * | 2.7 ± 0.29 | 108 ± 18.4 |
| PS (2.5 mg/mL) | 1.2 ± 0.05 | 1.4 ± 0.05 | 0.5 ± 0.03 * | 58.5 ± 5.1 | 4.8 ± 0.7 * | 91.9 ± 0.5 * | 29.8 ± 2.1 * | 2.9 ± 0.31 | 100 ± 12.7 | |
| 3 h | Reference (3.5 mg/mL) | 1.2 ± 0.04 | 1.4 ± 0.05 | 0.6 ± 0.04 * | 55.1 ± 5.7 | 7.6 ± 1.4 * | 86.4 ± 1.1 * | 26.4 ± 2.3 * | 2.5 ± 0.25 | 99 ± 14.1 |
| PS (2.5 mg/mL) | 1.3 ± 0.02 | 1.4 ± 0.03 | 0.6 ± 0.02 * | 59.6 ± 3.1 | 8.5 ± 0.6 * | 85.6 ± 1.3 * | 28.4 ± 1.6 * | 2.6 ± 0.16 | 93 ± 9.7 | |
| 4 h | Reference (3.5 mg/mL) | 1.2 ± 0.05 | 1.3 ± 0.05 | 0.7 ± 0.09 * | 52.0 ± 5.0 | 9.0 ± 1.2 * | 82.8 ± 0.6 * | 23.8 ± 1.6 | 2.4 ± 0.43 | 117 ± 18.7 |
| PS (2.5 mg/mL) | 1.2 ± 0.03 | 1.4 ± 0.03 | 0.7 ± 0.02 * | 57.7 ± 2.8 | 10.6 ± 0.9 * | 81.6 ± 0.8 * | 26.2 ± 1.1 | 2.6 ± 0.21 | 98 ± 6.2 | |
| 6 h | Reference (3.5 mg/mL) | 1.3 ± 0.14 | 1.4 ± 0.04 | 0.8 ± 0.03 * | 59.7 ± 4.5 | 15.3 ± 1.5 * | 74.4 ± 0.8 * | 24.7 ± 1.5 | 2.5 ± 0.39 | 101 ± 13.2 |
| PS (2.5 mg/mL) | 1.2 ± 0.09 | 1.3 ± 0.06 | 0.7 ± 0.03 * | 56.0 ± 6.1 | 13.3 ± 1.4 * | 76.0 ± 1.9 * | 23.7 ± 2.6 | 2.2 ± 0.31 | 94 ± 12.7 | |
| 8 h | Reference (3.5 mg/mL) | 1.3 ± 0.04 | 1.4 ± 0.03 | 0.9 ± 0.03 | 62.0 ± 3.0 | 20.2 ± 1.4 | 67.5 ± 1.2 | 23.2 ± 1.0 | 2.3 ± 0.19 | 98 ± 8.3 |
| PS (2.5 mg/mL) | 1.3 ± 0.07 | 1.4 ± 0.04 | 0.8 ± 0.02 | 60.2 ± 4.5 | 19.9 ± 1.4 | 66.9 ± 0.4 | 22.4 ± 1.5 | 2.0 ± 0.13 | 89 ± 3.6 | |
| 12 h | Reference (3.5 mg/mL) | 1.3 ± 0.06 | 1.4 ± 0.03 | 0.9 ± 0.02 | 63.0 ± 3.0 | 21.4 ± 1.3 | 66.1 ± 0.5 | 23.2 ± 1.1 | 2.3 ± 0.35 | 100 ± 11.5 |
| PS (2.5 mg/mL) | 1.3 ± 0.07 | 1.4 ± 0.04 | 0.9 ± 0.03 | 61.5 ± 5.0 | 21.0 ± 1.6 | 65.7 ± 0.4 | 22.5 ± 1.8 | 2.3 ± 0.14 | 101 ± 4.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saengklub, N.; Boonyarattanasoonthorn, T.; Kijtawornrat, A.; Chantasart, D. Preliminary Bioequivalence of an Oral Pimobendan Solution Formulation with Reference Solution Formulation in Beagle Dogs. Vet. Sci. 2022, 9, 141. https://doi.org/10.3390/vetsci9030141
Saengklub N, Boonyarattanasoonthorn T, Kijtawornrat A, Chantasart D. Preliminary Bioequivalence of an Oral Pimobendan Solution Formulation with Reference Solution Formulation in Beagle Dogs. Veterinary Sciences. 2022; 9(3):141. https://doi.org/10.3390/vetsci9030141
Chicago/Turabian StyleSaengklub, Nakkawee, Tussapon Boonyarattanasoonthorn, Anusak Kijtawornrat, and Doungdaw Chantasart. 2022. "Preliminary Bioequivalence of an Oral Pimobendan Solution Formulation with Reference Solution Formulation in Beagle Dogs" Veterinary Sciences 9, no. 3: 141. https://doi.org/10.3390/vetsci9030141
APA StyleSaengklub, N., Boonyarattanasoonthorn, T., Kijtawornrat, A., & Chantasart, D. (2022). Preliminary Bioequivalence of an Oral Pimobendan Solution Formulation with Reference Solution Formulation in Beagle Dogs. Veterinary Sciences, 9(3), 141. https://doi.org/10.3390/vetsci9030141







