The Use of Virtual-Problem-Based Learning during COVID-19 Pandemic Emergency: Veterinary Students’ Perception
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample Population
2.2. Practical Training Characteristics
2.3. Survey Questionnaire
2.4. Data Management and Statistical Analyses
2.4.1. Inter-Group Comparison
2.4.2. Intra-Group Comparison
2.4.3. Open-Ended Questions
3. Results
3.1. Inter-Group Comparison
3.2. Intra-Group Comparison
3.3. Open-Ended Questions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Survey Questionnaire Given to the Students at the End of the Two Clinical Training (Traditional in Presence and Virtual)
| Question | Type | Answers |
|---|---|---|
| Section-1—Demographic data | ||
| Gender | Male | |
| Female | ||
| Age range | 22–24 years old | |
| 25–27 years old | ||
| 28–30 years old | ||
| >30 years old | ||
| Section-2—Satisfaction | ||
| On a scale of 1 to 5 (with 1 being least satisfied and 5 being most), please rate your overall satisfaction with clinical training | 1 | |
| 2 | ||
| L_Q1 | 3 | |
| 4 | ||
| 5 | ||
| The clinical training was focused on relevant learning objectives. | Strongly agree | |
| Agree | ||
| L-Q2 | Neither agree nor disagree | |
| Disagree | ||
| Strongly disagree | ||
| My tasks during clinical training were clearly explained. | Strongly agree | |
| Agree | ||
| L-Q3 | Neither agree nor disagree | |
| Disagree | ||
| Strongly disagree | ||
| The organization of clinical training was appropriate. | Strongly agree | |
| Agree | ||
| L-Q4 | Neither agree nor disagree | |
| Disagree | ||
| Strongly disagree | ||
| The clinical training meet my expectations. | Strongly agree | |
| Agree | ||
| L-Q5 | Neither agree nor disagree | |
| Disagree | ||
| Strongly disagree | ||
| Describe with 1 or 2 phrases your expectation. | OE-Q1 | Free text |
| Was the duration of clinical training sufficient to ensure adequate competencies? | Yes | |
| Not relevant | ||
| L-Q6 | No, it was too short | |
| No, it was too long | ||
| Section-3—Clinical Skills | ||
| How would you define your clinical experience (for example examination skills, taking a history, deciding investigations and management, seeing a variety of patients in different settings, etc) before this clinical training? | Very poor | |
| Poor | ||
| L-Q7 | Neither good nor poor | |
| Good | ||
| Very good | ||
| How would you define your clinical experience after this clinical training? | Very poor | |
| Poor | ||
| L-Q8 | Neither good nor poor | |
| Good | ||
| Very good | ||
| I had the chance to deepen my knowledge through this clinical training. | Strongly agree | |
| Agree | ||
| L-Q9 | Neither agree nor disagree | |
| Disagree | ||
| Strongly disagree | ||
| During this clinical training, I attained the ability to make autonomous clinical decisions | Strongly disagree | |
| Agree | ||
| L-Q10 | Neither agree nor disagree | |
| Disagree | ||
| Strongly disagree | ||
| Section-4—Clinical supervision | ||
| During this clinical training, supervisors supported in managing clinical cases. | Strongly agree | |
| Agree | ||
| L-Q11 | Neither agree nor disagree | |
| Disagree | ||
| Strongly disagree | ||
| Supervisors encouraged students to deepen their knowledge of issues encountered during this clinical training. | Strongly agree | |
| Agree | ||
| L-Q12 | Neither agree nor disagree | |
| Disagree | ||
| Strongly disagree | ||
| During this clinical training, the supervisors’ support meets my expectations. | Strongly agree | |
| Agree | ||
| L-Q13 | Neither agree nor disagree | |
| Disagree | ||
| Strongly disagree | ||
| Section-5—Perceptions of problems | ||
| How would you define the clinical activities of this training? | Very difficult | |
| Difficult | ||
| L-Q14 | Neither Difficult nor Easy | |
| Easy | ||
| Too easy | ||
| Please, describe what should change in this clinical training to “WOW” you | OE-Q2 | Free text |
References
- Nour, A.; Gyorffy, A.; Frenyo, L.V. A Review of Some Innovative Teaching Concepts and Methods Used in the Field of Veterinary Medical Education. J. Dairy Veter-Sci. 2019, 8, 1–9. [Google Scholar]
- De Ponti, R.; Marazzato, J.; Maresca, A.M.; Rovera, F.; Carcano, G.; Ferrario, M.M. Pre-graduation medical training including virtual reality during COVID-19 pandemic: A report on students’ perception. MC Med. Educ. 2020, 20, 1–7. [Google Scholar] [CrossRef]
- Lane, E.A. Problem-based learning in veterinary education. J. Vet. Med. Educ. 2008, 35, 631–636. [Google Scholar] [CrossRef]
- Cooke, M.; Moyle, K. Students’ evaluation of problem-based learning. Nurse Educ. Today 2002, 22, 330–339. [Google Scholar] [CrossRef]
- Ryan, M.T.; Irwin, J.A.; Bannon, F.J.; Mulholland, C.W.; Baird, A.W. Observations of veterinary medicine students’ approaches to study in pre-clinical years. J. Vet. Med. Educ. 2004, 31, 242–254. [Google Scholar] [CrossRef]
- Becker, S.; Viljoen, M.J.; Botma, Y.; Bester, I.J. Integration of study material in the problem-based learning method. Curationis 2003, 26, 57–61. [Google Scholar] [CrossRef][Green Version]
- Whitney, M.S.; Herron, M.A.; Weeks, B.R. Preclinical curricular alternatives-history and rationale of problem-based medical-education. J. Vet. Med. Educ. 1993, 20, 2–8. [Google Scholar]
- Doherty, M.L.; Jones, B.R. Undergraduate veterinary education at University College Dublin: A time of change. J. Vet. Med. Educ. 2006, 33, 214–219. [Google Scholar] [CrossRef]
- Howell, N.E.; Lane, I.F.; Brace, J.J.; Shull, R.M. Integration of problem-based learning in a veterinary medical curriculum: First-year experiences with Application-Based Learning Exercises at the University of Tennessee College of Veterinary Medicine. J. Vet. Med. Educ. 2002, 29, 169–175. [Google Scholar] [CrossRef]
- Nandi, P.L.; Chan, J.N.; Chan, C.P.; Chan, P.; Chan, L.P. Undergraduate medical education: Comparison of problem-based learning and conventional teaching. Hong Kong Med. J. 2000, 6, 301–306. [Google Scholar]
- Williams, A.F. An antipodean evaluation of problem-based learning by clinical educators. Nurse Educ. Today 1999, 19, 659–667. [Google Scholar] [CrossRef]
- Popovic, C. Teaching for Quality Learning at University, 2nd ed.; Innovations in Education and Teaching International Routledge/Taylor & Francis: Oxfordshire, UK, 2013; Volume 5, pp. 422–423. [Google Scholar]
- Monitor, C. Guides Ultimate Email Marketing Benchmarks for 2020: By Industry and Day; CM Group: Nashville, TN, USA, 2020. [Google Scholar]
- Abbamonte, K. Customer Satisfaction Surveys: A Comprehensive Guide; Help Scout-Software Company: Boston, MA, USA, 2020. [Google Scholar]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Anderson, H.M.; Cain, J.; Bird, E. Online Student Course Evaluations: Review of Literature and a Pilot Study. Am. J. Pharm Educ. 2005, 69, 34–43. [Google Scholar] [CrossRef]
- Norman, G.R.; van der Vleuten, C.P.; Newble, D.I. (Eds.) International Handbook of Research in Medical Education; Springer Science & Business Media: Berlin, Germany, 2012; Volume 7. [Google Scholar]
- Lowenthal, P.; Bauer, C.; Chen, K.Z. Student perceptions of online learning: An analysis of online course evaluations. Am. J. Distance Educ. 2015, 29, 85–97. [Google Scholar] [CrossRef][Green Version]
- Hung, W.; Harpole Bailey, J.; Jonassen, D.H. Exploring the tensions of problem-based learning: Insights from research. New Dir. Teach. Learn. 2003, 95, 13–23. [Google Scholar] [CrossRef]
- Curtin, R.; Presser, S.; Singer, E. Changes in telephone survey nonresponse over the past quarter century. Public Opin. Q. 2005, 69, 87–98. [Google Scholar]
- Keusch, F. Why do people participate in Web surveys? Applying survey participation theory to Internet survey data collection. Manag Rev. Q. 2015, 65, 183–216. [Google Scholar] [CrossRef]
- Porter, S.R.; Whitcomb, M.E. Non-response in student surveys: The role of demographics, engagement and personality. Res. High. Educ. 2005, 46, 127–152. [Google Scholar] [CrossRef]
- Adams, M.J.; Umbach, P.D. Nonresponse and online student evaluations of teaching: Understanding the influence of salience, fatigue, and academic environments. Res. High. Educ. 2012, 53, 576–591. [Google Scholar] [CrossRef]
- Park, K.; Park, N.; Heo, W.; Gustafson, K. What prompts college students to participate in online surveys? Int Educ. Stud. 2018, 12, 69. [Google Scholar] [CrossRef]
- Das Carlo, M.; Swadi, H.; Mpofu, D. Medical student perceptions of factors affecting productivity of problem-based learning tutorial groups: Does culture influence the outcome? Teach. Learn. Med. 2003, 15, 59–64. [Google Scholar] [CrossRef]
- Hendry, G.D.; Ryan, G.; Harris, J. Group problems in problem-based learning. Med. Teac. 2003, 25, 609–616. [Google Scholar] [CrossRef]
- Dost, S.; Hossain, A.; Shehab, M.; Abdelwahed, A.; Al-Nusair, L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: A national cross-sectional survey of 2721 UK medical students. BMJ Open 2020, 10, e042378. [Google Scholar] [CrossRef]
- Huddart, D.; Hirniak, J.; Sethi, R.; Hayer, G.; Dibblin, C.; Rao, B.M.; Sethi, S. # MedStudentCovid: How social media is supporting students during COVID-19. Med. Educ. 2020, 54, 951. [Google Scholar] [CrossRef]
- Spencer, J.A.; Jordan, R.K. Learner centred approaches in medical education. BMJ 1999, 318, 1280–1283. [Google Scholar]
- Morgado, M.; Mendes, J.J.; Proença, L. Online Problem-Based Learning in Clinical Dental Education: Students’ Self-Perception and Motivation. Healthcare 2021, 9, 420. [Google Scholar] [CrossRef]
- Rand, J.S.; Baglioni Jr, A.J. Subject-based problem-based learning in the veterinary science course at the University of Queensland. Aust Vet. J. 1997, 75, 120–125. [Google Scholar] [CrossRef]
- Haynes, J.S.; Myers, R.K. A case-based, cooperative learning approach to teaching veterinary systemic pathology. J. Vet. Med. Educ. 1998, 25, 12–16. [Google Scholar]
- Haidet, P.; Stein, H.F. The role of the student-teacher relationship in the formation of physicians. J. Gen. Intern. Med. 2006, 21, 16–20. [Google Scholar] [CrossRef]
- Plaut, S.M.; Baker, D. Teacher–student relationships in medical education: Boundary considerations. Med. Teach. 2011, 33, 828–833. [Google Scholar] [CrossRef]
- Hrastinski, S. Asynchronous and synchronous e-learning. Educ. Q. 2008, 31, 51–55. [Google Scholar]
- Cranfield, D.J.; Tick, A.; Venter, I.M.; Blignaut, R.J.; Renaud, K. Higher Education Students’ Perceptions of Online Learning during COVID-19—A Comparative Study. Educ. Sci. 2021, 11, 403. [Google Scholar] [CrossRef]
- Shah, A.A.; Ravana, S.D.; Hamid, S.; Ismail, M.A. Accuracy evaluation of methods and techniques in Web-based question answering systems: A survey. Knowl. Inf. Syst. 2019, 58, 611–650. [Google Scholar] [CrossRef]
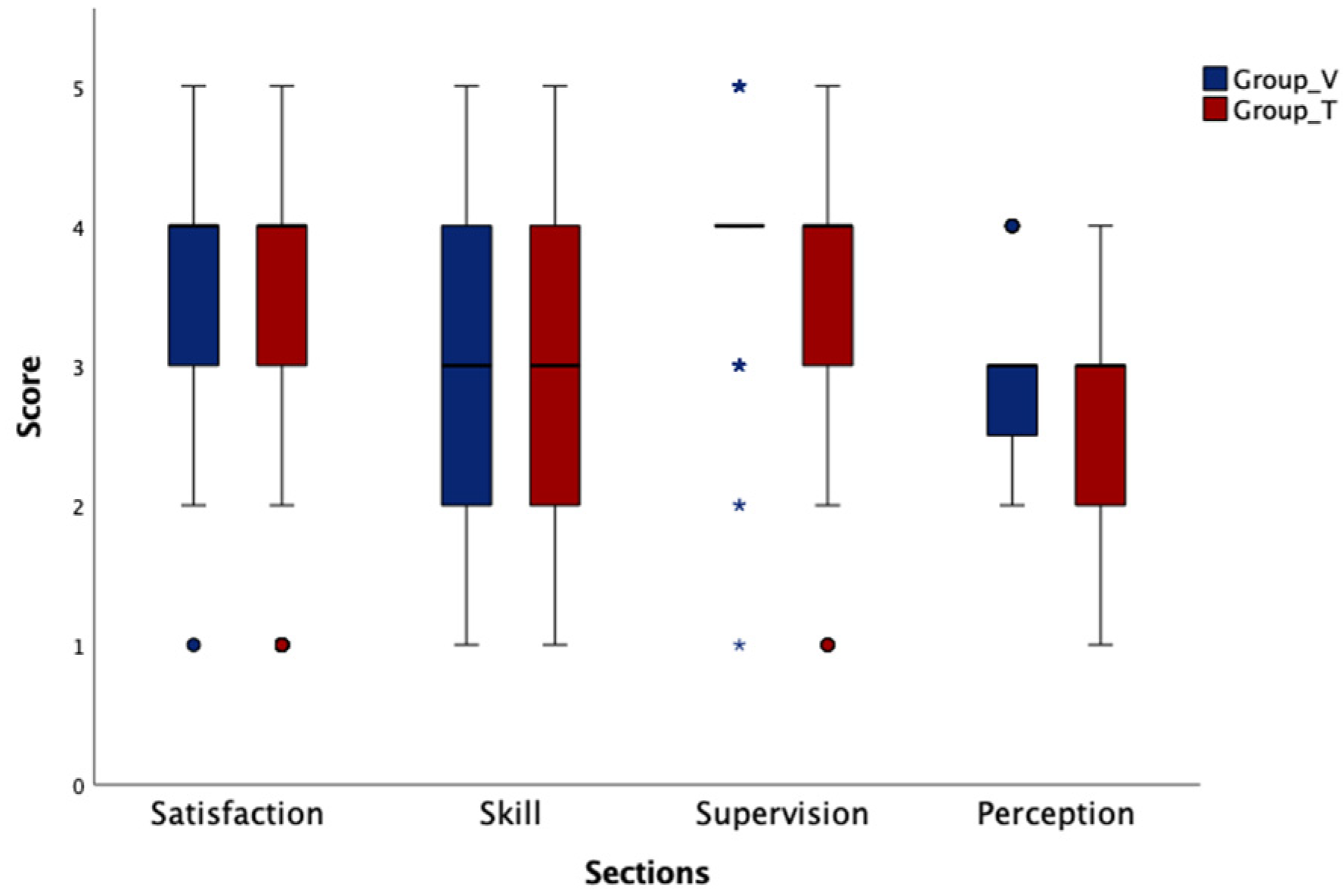
| Likert Question (L-Q) | Question | Group | Response Value | H0 | Median (Q1, Q3) | p | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||||||
| Satisfaction | ||||||||||
| L-Q1 | On a scale of 1 to 5 (with 1 being least satisfied and 5 being most), please rate your overall satisfaction with clinical training. | T | 2 (7.1%) | 3 (10.7%) | 3 (10.7%) | 15 (53.6%) | 3 (10.7%) | 0.004 | 3 (3, 4) | 0.100 |
| V | 0 (0%) | 4 (12.5%) | 15 (46.9%) | 10 (31.2%) | 3 (9.4%) | 0.008 | 4 (3, 4) | |||
| L-Q2 | The clinical training was focused on relevant learning objectives. | T | 0 (0%) | 4 (14.3%) | 2 (7.1%) | 18 (64.3%) | 4 (14.3%) | 0.000 | 4 (4, 4) | 0.361 |
| V | 0 (0%) | 2 (6.2%) | 3 (9.4%) | 20 (62.5%) | 7 (21.9%) | 0.000 | 4 (4, 4) | |||
| L-Q3 | My tasks during clinical training were clearly explained. | T | 2 (7.1%) | 6 (21.4%) | 3 (10.7%) | 16 (57.1%) | 1 (3.6%) | 0.000 | 4 (4, 5) | 0.710 |
| V | 0 (0%) | 1 (3.1%) | 2 (6.2%) | 22 (68.7%) | 7 (21.9%) | 0.000 | 5 (4, 5) | |||
| L-Q4 | The organization of clinical training was appropriate. | T | 4 (14.3%) | 6 (21.4%) | 5 (17.8%) | 13 (46.4%) | 0 (0%) | 0.067 | 4 (4, 4) | 0.001 |
| V | 1 (3.1%) | 5 (15.6%) | 8 (25%) | 15 (46.9%) | 3 (9.4%) | 0.001 | 4 (2, 4) | |||
| L-Q5 | The clinical training meet my expectations. | T | 1 (3.6%) | 8 (28.5%) | 2 (7.1%) | 13 (46.4%) | 4 (14.3%) | 0.002 | 4 (3, 4) | 0.132 |
| V | 0 (0%) | 10 (31.2%) | 7 (21.9%) | 11 (34.4%) | 4 (12.5%) | 0.290 | 3 (2, 4) | |||
| L-Q6 | Was the duration of clinical training sufficient to ensure adequate competencies? | T | - | 4 (14.3%) | 6 (21.4%) | 2 (7.1%) | 16 (57.1%) | 0.001 | 3 (2, 4) | 0.623 |
| V | - | 0 (0%) | 10 (31.2%) | 7 (21.9%) | 15 (46.9%) | 0.216 | 4 (2, 4) | |||
| Clinical Skills | ||||||||||
| L-Q7 | How would you define your clinical experience before this clinical training? | T | 0 (0%) | 1 (3.6%) | 9 (32.1%) | 11 (39.3%) | 7 (25%) | 0.046 | 3 (2, 3) | 0.034 |
| V | 0 (0%) | 6 (18.7%) | 13 (40.6%) | 9 (28.1%) | 4 (12.5%) | 0.124 | 2 (1.7, 3) | |||
| L-Q8 | How would you define your clinical experience after this clinical training? | T | 0 (0%) | 7 (25%) | 8 (28.5%) | 9 (32.1%) | 4 (14.3%) | 0.572 | 3 (2, 4) | 0.158 |
| V | 1 (3.1%) | 14 (43.7%) | 7 (21.9%) | 7 (21.9%) | 3 (9.4%) | 0.000 | 3 (2, 3.2) | |||
| L-Q9 | I had the chance to deepen my knowledge through this clinical training. | T | 2 (7.1%) | 1 (3.6%) | 4 (14.3%) | 19 (67.8%) | 2 (7.1%) | 0.000 | 4 (4, 4) | 0.124 |
| V | 0 (0%) | 1 (3.1%) | 3 (9.4%) | 23 (71.9%) | 5 (15.6%) | 0.000 | 4 (3.7, 4) | |||
| L-Q10 | During this clinical training, I attained the ability to make autonomous clinical decisions. | T | 4 (14.3%) | 8 (28.5%) | 11 (39.3%) | 5 (17.8%) | 0 (0%) | 0.232 | 3 (2, 4) | 0.193 |
| V | 0 (0%) | 13 (40.6%) | 8 (25%) | 8 (25%) | 3 (9.4%) | 0.013 | 3 (2, 3) | |||
| Clinical supervision | ||||||||||
| L-Q11 | During this clinical training, supervisors supported in managing clinical cases. | T | 1 (3.6%) | 3 (10.7%) | 3 (10.7%) | 17 (60.7%) | 4 (14.3%) | 0.000 | 4 (4, 4.2) | 0.213 |
| V | 1 (3.1%) | 1 (3.1%) | 3 (9.4%) | 19 (59.4%) | 8 (25%) | 0.000 | 4 (3.7, 4) | |||
| L-Q12 | Supervisors encouraged students to deepen their knowledge of issues encountered during this clinical training. | T | 1 (3.6%) | 3 (10.7%) | 6 (21.4%) | 12 (42.8%) | 6 (21.4%) | 0.002 | 4 (4, 4) | 0.233 |
| V | 0 (0%) | 0 (0%) | 5 (15.6%) | 21 (65.6%) | 6 (18.7%) | 0.001 | 4 (3, 4) | |||
| L-Q13 | During this clinical training, the supervisors’ support meets my expectations. | T | 1 (3.6%) | 6 (21.4%) | 3 (10.7%) | 13 (46.4%) | 5 (17.8%) | 0.002 | 4 (3.7, 4.2) | 0.185 |
| V | 0 (0%) | 1 (3.1%) | 7 (21.9%) | 16 (50%) | 8 (25%) | 0.003 | 4 (2.7, 4) | |||
| Student’s perceptions of the training | ||||||||||
| L-Q14 | How would you define the clinical activities of this training? | T | 2 (7.1%) | 9 (32.1%) | 15 (53.6%) | 2 (7.1%) | 0 (0%) | 0.005 | 3 (2.7, 3) | 0.132 |
| V | 0 (0%) | 8 (25%) | 19 (59.4%) | 5 (15.6%) | 0 (0%) | 0.006 | 3 (2, 3) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Micieli, F.; Valle, G.D.; Del Prete, C.; Ciaramella, P.; Guccione, J. The Use of Virtual-Problem-Based Learning during COVID-19 Pandemic Emergency: Veterinary Students’ Perception. Vet. Sci. 2022, 9, 581. https://doi.org/10.3390/vetsci9100581
Micieli F, Valle GD, Del Prete C, Ciaramella P, Guccione J. The Use of Virtual-Problem-Based Learning during COVID-19 Pandemic Emergency: Veterinary Students’ Perception. Veterinary Sciences. 2022; 9(10):581. https://doi.org/10.3390/vetsci9100581
Chicago/Turabian StyleMicieli, Fabiana, Giovanni Della Valle, Chiara Del Prete, Paolo Ciaramella, and Jacopo Guccione. 2022. "The Use of Virtual-Problem-Based Learning during COVID-19 Pandemic Emergency: Veterinary Students’ Perception" Veterinary Sciences 9, no. 10: 581. https://doi.org/10.3390/vetsci9100581
APA StyleMicieli, F., Valle, G. D., Del Prete, C., Ciaramella, P., & Guccione, J. (2022). The Use of Virtual-Problem-Based Learning during COVID-19 Pandemic Emergency: Veterinary Students’ Perception. Veterinary Sciences, 9(10), 581. https://doi.org/10.3390/vetsci9100581





