Investigation of Genes and Proteins Expression Associating Serotonin Signaling Pathway in Lung and Pulmonary Artery Tissues of Dogs with Pulmonary Hypertension Secondary to Degenerative Mitral Valve Disease: The Preliminary Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Investigation of Genes Related to 5-HT Signaling Pathway
2.3. Investigation of the Downstream Effectors in 5-HT Signaling Pathway by Western Blot Analysis
2.4. Investigation of the Downstream Effectors in 5-HT Signaling Pathway by Immunohistochemistry
2.5. Statistical Analysis
3. Results
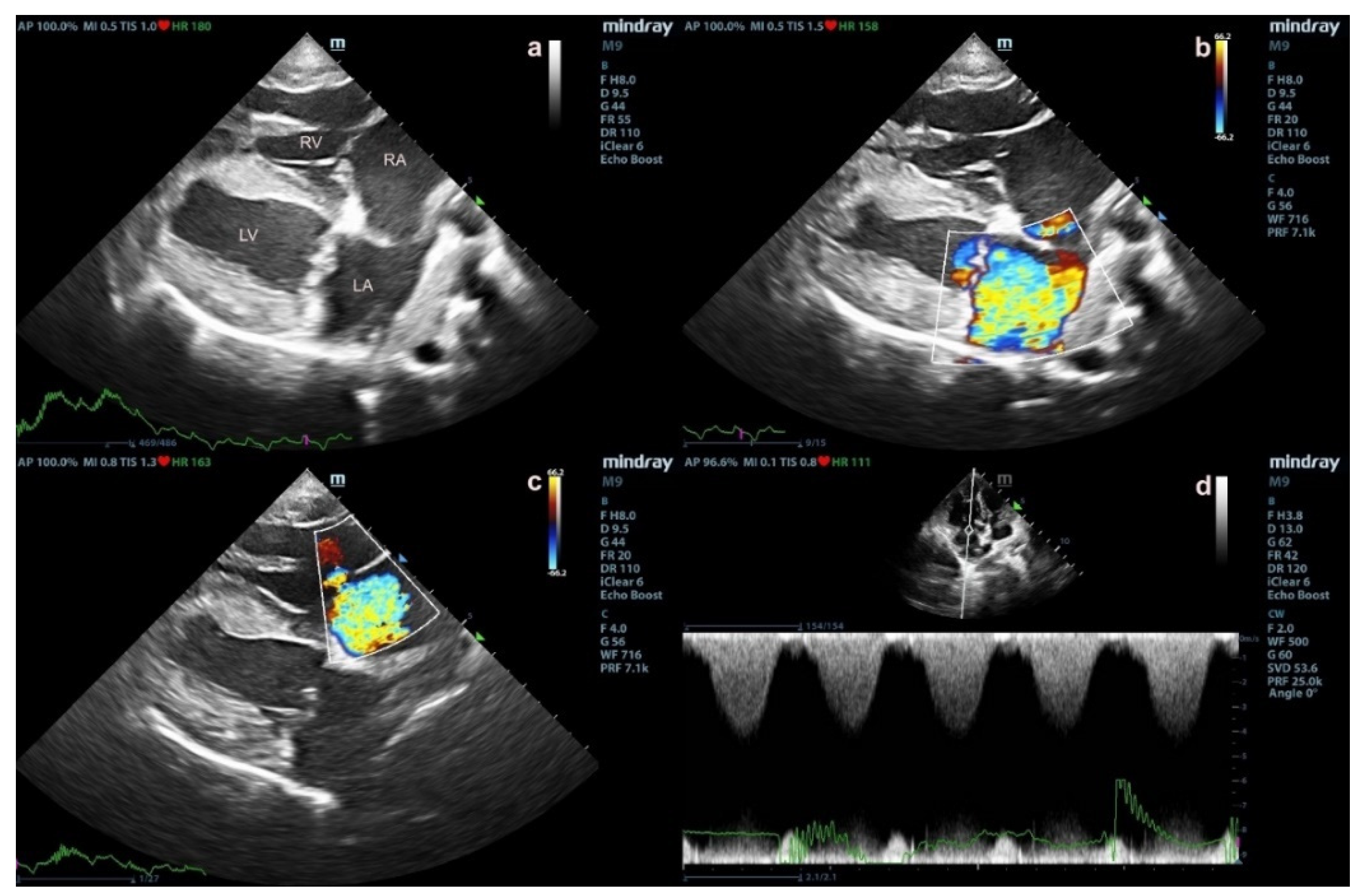
3.1. Animals
3.2. Investigation of Genes Associating 5-HT Signaling Pathway
3.3. Investigation of Proteins Associating 5-HT Signaling Pathway
3.3.1. Western Blot Analysis
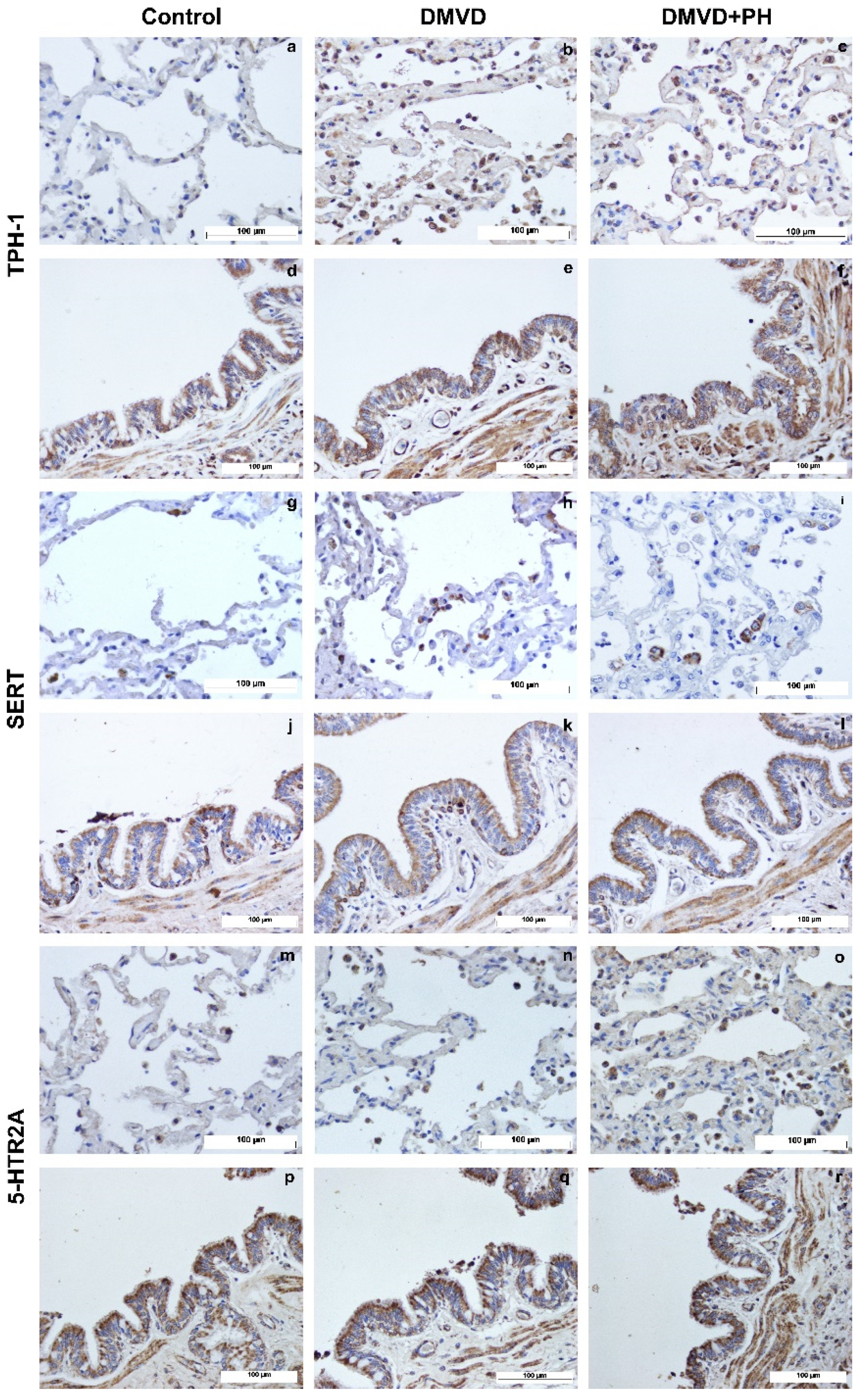
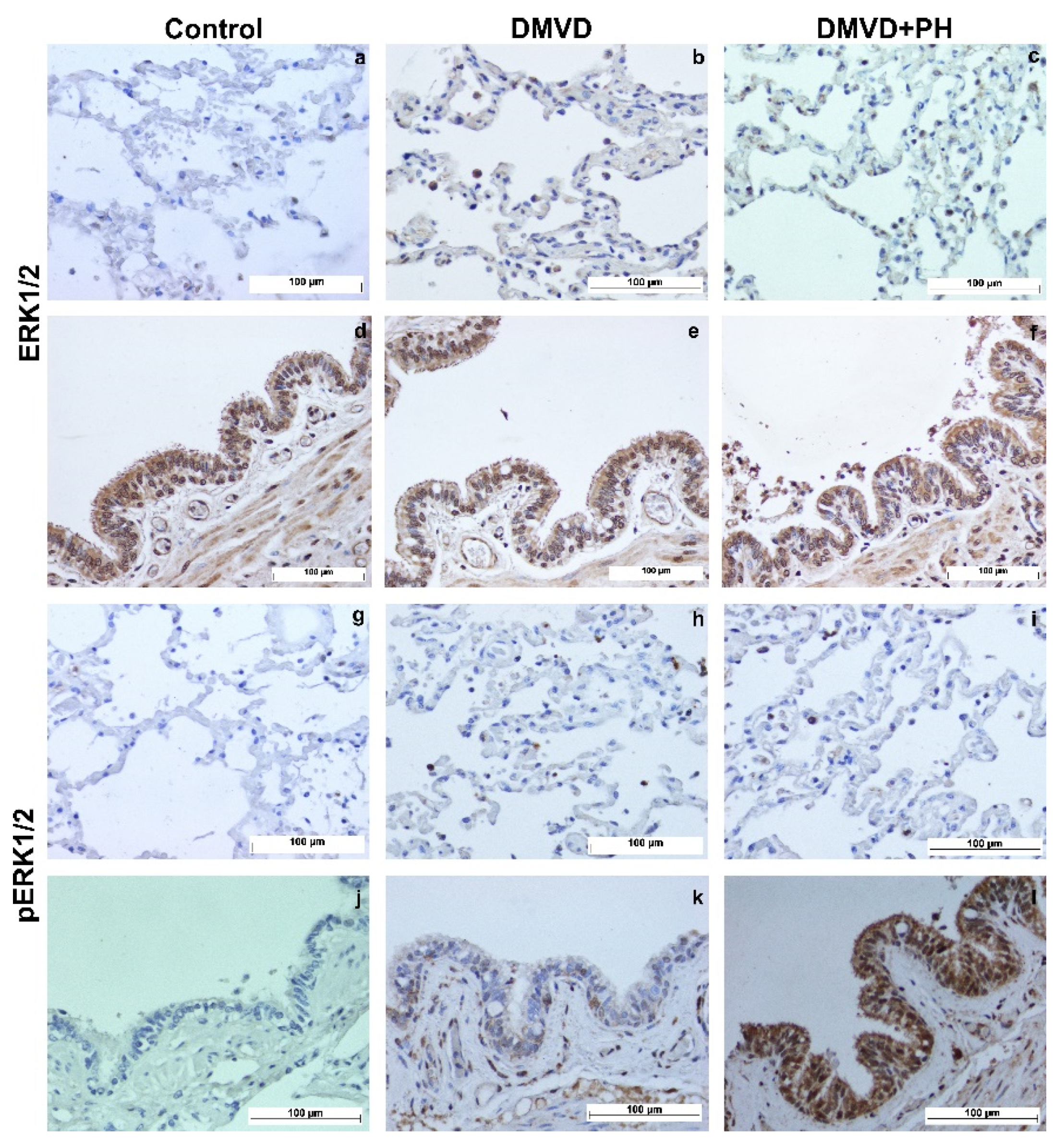
3.3.2. Immunohistochemical Study
3.4. The Correlation between the Relative Expression and Echocardiographic Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hatano, S.; Strasser, T.; World Health Organization. Primary Pulmonary Hypertension: Report on a WHO Meeting, Geneva, 15–17 October 1973; World Health Organization: Geneva, Switzerland, 1975. [Google Scholar]
- Reinero, C.; Visser, L.C.; Kellihan, H.B.; Masseau, I.; Rozanski, E.; Clercx, C.; Williams, K.; Abbott, J.; Borgarelli, M.; Scansen, B.A. ACVIM consensus statement guidelines for the diagnosis, classification, treatment, and monitoring of pulmonary hypertension in dogs. J. Vet. Intern. Med. 2020, 34, 549–573. [Google Scholar] [CrossRef] [PubMed]
- Pyle, R.L.; Abbott, J.; MacLean, H. Pulmonary hypertension and cardiovascular sequelae in 54 dogs. Intern. J. Appl. Res. Vet. Med. 2004, 2, 99–109. [Google Scholar]
- Delgado, J.F.; Conde, E.; Sanchez, V.; Lopez-Rios, F.; Gomez-Sanchez, M.A.; Escribano, P.; Sotelo, T.; de la Camara, A.G.; Cortina, J.; de la Calzada, C.S. Pulmonary vascular remodeling in pulmonary hypertension due to chronic heart failure. Eur. J. Heart Fail. 2005, 7, 1011–1016. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.; Desai, M.; Tuzcu, E.M.; Griffin, B.; Kapadia, S. Pulmonary hypertension in mitral regurgitation. J. Am. Heart Assoc. 2014, 3, e000748. [Google Scholar] [CrossRef] [PubMed]
- Borgarelli, M.; Abbott, J.; Braz-Ruivo, L.; Chiavegato, D.; Crosara, S.; Lamb, K.; Ljungvall, I.; Poggi, M.; Santilli, R.A.; Haggstrom, J. Prevalence and prognostic importance of pulmonary hypertension in dogs with myxomatous mitral valve disease. J. Vet. Intern. Med. 2015, 29, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Borgarelli, M.; Zini, E.; D’Agnolo, G.; Tarducci, A.; Santilli, R.A.; Chiavegato, D.; Tursi, M.; Prunotto, M.; Haggstrom, J. Comparison of primary mitral valve disease in German Shepherd dogs and in small breeds. J. Vet. Cardiol. 2004, 6, 27–34. [Google Scholar] [CrossRef]
- Guglielmini, C.; Civitella, C.; Diana, A.; Di Tommaso, M.; Cipone, M.; Luciani, A. Serum cardiac troponin I concentration in dogs with precapillary and postcapillary pulmonary hypertension. J. Vet. Intern. Med. 2010, 24, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Schober, K.E.; Hart, T.M.; Stern, J.A.; Li, X.; Samii, V.F.; Zekas, L.J.; Scansen, B.A.; Bonagura, J.D. Detection of congestive heart failure in dogs by Doppler echocardiography. J. Vet. Intern. Med. 2010, 24, 1358–1368. [Google Scholar] [CrossRef]
- Serres, F.J.; Chetboul, V.; Tissier, R.; Sampedrano, C.C.; Gouni, V.; Nicolle, A.P.; Pouchelon, J.-L. Doppler echocardiography–derived evidence of pulmonary arterial hypertension in dogs with degenerative mitral valve disease: 86 cases (2001–2005). J. Am. Vet. Med. Assoc. 2006, 229, 1772–1778. [Google Scholar] [CrossRef]
- Nebigil, C.G.; Choi, D.S.; Dierich, A.; Hickel, P.; Le Meur, M.; Messaddeq, N.; Launay, J.M.; Maroteaux, L. Serotonin 2B receptor is required for heart development. Proc. Natl. Acad. Sci. USA 2000, 97, 9508–9513. [Google Scholar] [CrossRef]
- Berger, G.; Azzam, Z.S.; Hoffman, R.; Yigla, M. Coagulation and anticoagulation in pulmonary arterial hypertension. Isr. Med. Assoc. J. 2009, 11, 376–379. [Google Scholar]
- Adnot, S.; Houssaini, A.; Abid, S.; Marcos, E.; Amsellem, V. Serotonin transporter and serotonin receptors. In Pharmacotherapy of Pulmonary Hypertension; Humbert, M., Evgenov, O.V., Stasch, J.P., Eds.; Springer: Berlin/Heidelberg, Germany, 2013; pp. 365–380. [Google Scholar]
- Bentfeld-Barker, M.E.; Bainton, D.F. Identification of primary lysosomes in human megakaryocytes and platelets. Blood 1982, 59, 472–481. [Google Scholar] [CrossRef] [PubMed]
- Tranzer, J.; Da Prada, M.; Pletscher, A. Ultrastructural localization of 5-hydroxy-tryptamine in blood platelets. Nature 1966, 212, 1574–1575. [Google Scholar] [CrossRef] [PubMed]
- White, J.G. The dense bodies of human platelets: Inherent electron opacity of the serotonin storage particles. Blood 1969, 33, 598–606. [Google Scholar] [CrossRef] [PubMed]
- Egermayer, P.; Town, G.I.; Peacock, A.J. Role of serotonin in the pathogenesis of acute and chronic pulmonary hypertension. Thorax 1999, 54, 161–168. [Google Scholar] [CrossRef]
- Gillis, C.; Pitt, B. The fate of circulating amines within the pulmonary circulation. Annu. Rev. Physiol. 1982, 44, 269–281. [Google Scholar] [CrossRef]
- Fanburg, B.L.; Lee, S.L. A new role for an old molecule: Serotonin as a mitogen. Am. J. Physiol.-Lung Cell. Mol. Physiol. 1997, 272, L795–L806. [Google Scholar] [CrossRef]
- Fukumoto, T.; Kema, I.P.; Levin, M. Serotonin signaling is a very early step in patterning of the left-right axis in chick and frog embryos. Curr. Biol. 2005, 15, 794–803. [Google Scholar] [CrossRef]
- Lauder, J.M. Neurotransmitters as growth regulatory signals: Role of receptors and second messengers. Trends Neurosci. 1993, 16, 233–240. [Google Scholar] [CrossRef]
- Nebigil, C.G.; Hickel, P.; Messaddeq, N.; Vonesch, J.L.; Douchet, M.P.; Monassier, L.; Gyorgy, K.; Matz, R.; Andriantsitohaina, R.; Manivet, P.; et al. Ablation of serotonin 5-HT2B receptors in mice leads to abnormal cardiac structure and function. Circulation 2001, 103, 2973–2979. [Google Scholar] [CrossRef]
- Nebigil, C.G.; Maroteaux, L. A novel role for serotonin in heart. Trends Cardiovasc. Med. 2001, 11, 329–335. [Google Scholar] [CrossRef]
- Kramer, M.S.; Lane, D.A. Aminorex, dexfenfluramine, and primary pulmonary hypertension. J. Clin. Epidemiol. 1998, 51, 361–364. [Google Scholar] [CrossRef]
- Rothman, R.B.; Ayestas, M.A.; Dersch, C.M.; Baumann, M.H. Aminorex, fenfluramine, and chlorphentermine are serotonin transporter substrates. Implications for primary pulmonary hypertension. Circulation 1999, 100, 869–875. [Google Scholar] [CrossRef] [PubMed]
- Gairhe, S.; Bauer, N.N.; Gebb, S.A.; McMurtry, I.F. Serotonin passes through myoendothelial gap junctions to promote pulmonary arterial smooth muscle cell differentiation. Am. J. Physiol.-Lung C 2012, 303, L767–L777. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.L.; Simon, A.R.; Wang, W.W.; Fanburg, B.L. H2O2 signals 5-HT-induced ERK MAP kinase activation and mitogenesis of smooth muscle cells. Am. J. Physiol. Lung Cell Mol. Physiol. 2001, 281, L646–L652. [Google Scholar] [CrossRef]
- Lee, S.L.; Wang, W.W.; Finlay, G.A.; Fanburg, B.L. Serotonin stimulates mitogen-activated protein kinase activity through the formation of superoxide anion. Am. J. Physiol. 1999, 277, L282–L291. [Google Scholar] [CrossRef]
- Liu, Y.; Suzuki, Y.J.; Day, R.M.; Fanburg, B.L. Rho kinase-induced nuclear translocation of ERK1/ERK2 in smooth muscle cell mitogenesis caused by serotonin. Circ. Res. 2004, 95, 579–586. [Google Scholar] [CrossRef]
- Suzuki, Y.J.; Day, R.M.; Tan, C.C.; Sandven, T.H.; Liang, Q.; Molkentin, J.D.; Fanburg, B.L. Activation of GATA-4 by serotonin in pulmonary artery smooth muscle cells. J. Biol. Chem. 2003, 278, 17525–17531. [Google Scholar] [CrossRef]
- Delaney, C.; Gien, J.; Roe, G.; Isenberg, N.; Kailey, J.; Abman, S.H. Serotonin contributes to high pulmonary vascular tone in a sheep model of persistent pulmonary hypertension of the newborn. Am. J. Physiol. Lung Cell Mol. Physiol. 2013, 304, L894–L901. [Google Scholar] [CrossRef]
- MacLean, M.R.; Dempsie, Y. Serotonin and pulmonary hypertension—From bench to bedside? Curr. Opin. Pharmacol. 2009, 9, 281–286. [Google Scholar] [CrossRef]
- Sakarin, S.; Surachetpong, S.D.; Rungsipipat, A. The Expression of Proteins Related to Serotonin Pathway in Pulmonary Arteries of Dogs Affected With Pulmonary Hypertension Secondary to Degenerative Mitral Valve Disease. Front. Vet. Sci. 2020, 7, 612130. [Google Scholar] [CrossRef] [PubMed]
- Keene, B.W.; Atkins, C.E.; Bonagura, J.D.; Fox, P.R.; Haggstrom, J.; Fuentes, V.L.; Oyama, M.A.; Rush, J.E.; Stepien, R.; Uechi, M. ACVIM consensus guidelines for the diagnosis and treatment of myxomatous mitral valve disease in dogs. J. Vet. Intern. Med. 2019, 33, 1127–1140. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Oliva, A.; Casas-Alvarado, A.; Miranda-Cortés, A.E.; Hernández-Avalos, I. Clinical pharmacology of tramadol and tapentadol, and their therapeutic efficacy in different models of acute and chronic pain in dogs and cats. J. Adv. Vet. Anim. Res. 2021, 8, 404–422. [Google Scholar] [CrossRef] [PubMed]
- Tangmahakul, N.; Techangamsuwan, S.; Surachetpong, S.D. Selection of the appropriate reference genes for relative quantitative reverse transcription polymerase chain reaction (qRT-PCR) in canine pulmonary arteries. Thai J. Vet. Med. 2019, 49, 313–318. [Google Scholar]
- Peters, I.R.; Peeters, D.; Helps, C.R.; Day, M.J. Development and application of multiple internal reference (housekeeper) gene assays for accurate normalisation of canine gene expression studies. Vet. Immunol. Immunopathol. 2007, 117, 55–66. [Google Scholar] [CrossRef]
- Schmittgen, T.D.; Livak, K.J. Analyzing real-time PCR data by the comparative C(T) method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef]
- Brinkhof, B.; Spee, B.; Rothuizen, J.; Penning, L.C. Development and evaluation of canine reference genes for accurate quantification of gene expression. Anal. Biochem. 2006, 356, 36–43. [Google Scholar] [CrossRef]
- Kodippili, K.; Thorne, P.K.; Laughlin, M.H.; Duan, D. Dystrophin deficiency impairs vascular structure and function in the canine model of Duchenne muscular dystrophy. J. Pathol. 2021, 254, 589–605. [Google Scholar] [CrossRef]
- Eddahibi, S.; Adnot, S. The Serotonin Pathway in Pulmonary Hypertension. Adv. Pulm. Hypertens. 2005, 4, 20–23. [Google Scholar] [CrossRef]
- Dempsie, Y.; MacLean, M.R. Pulmonary hypertension: Therapeutic targets within the serotonin system. Br. J. Pharmacol. 2008, 155, 455–462. [Google Scholar] [CrossRef]
- MacLean, M.R. Pulmonary hypertension and the serotonin hypothesis: Where are we now? Int. J. Clin. Pract. Suppl. 2007, 156, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Aiello, R.J.; Bourassa, P.-A.; Zhang, Q.; Dubins, J.; Goldberg, D.R.; De Lombaert, S.; Humbert, M.; Guignabert, C.; Cavasin, M.A.; McKinsey, T.A. Tryptophan hydroxylase 1 inhibition impacts pulmonary vascular remodeling in two rat models of pulmonary hypertension. J. Pharmacol. Exp. Ther. 2017, 360, 267–279. [Google Scholar] [CrossRef] [PubMed]
- Marcos, E.; Fadel, E.; Sanchez, O.; Humbert, M.; Dartevelle, P.; Simonneau, G.; Hamon, M.; Adnot, S.; Eddahibi, S. Serotonin-induced smooth muscle hyperplasia in various forms of human pulmonary hypertension. Circ. Res. 2004, 94, 1263–1270. [Google Scholar] [CrossRef] [PubMed]
- De Raaf, M.A.; Kroeze, Y.; Middelman, A.; de Man, F.S.; de Jong, H.; Vonk-Noordegraaf, A.; de Korte, C.; Voelkel, N.F.; Homberg, J.; Bogaard, H.J. Serotonin transporter is not required for the development of severe pulmonary hypertension in the Sugen hypoxia rat model. Am. J. Physiol. Lung Cell Mol. Physiol. 2015, 309, L1164–L1173. [Google Scholar] [CrossRef]
- Delaney, C.; Sherlock, L.; Fisher, S.; Maltzahn, J.; Wright, C.; Nozik-Grayck, E. Serotonin 2A receptor inhibition protects against the development of pulmonary hypertension and pulmonary vascular remodeling in neonatal mice. Am. J. Physiol. Lung Cell Mol. Physiol. 2018, 314, L871–L881. [Google Scholar] [CrossRef]
- Delgado, J.F. The right heart and pulmonary circulation (III). The pulmonary circulation in heart failure. Rev. Esp. Cardiol. 2010, 63, 334–345. [Google Scholar] [CrossRef]
- Bai, Y.; Wang, H.M.; Liu, M.; Wang, Y.; Lian, G.C.; Zhang, X.H.; Kang, J.; Wang, H.L. 4-Chloro-DL-phenylalanine protects against monocrotaline-induced pulmonary vascular remodeling and lung inflammation. Int. J. Mol. Med. 2014, 33, 373–382. [Google Scholar] [CrossRef]
- Morecroft, I.; Dempsie, Y.; Bader, M.; Walther, D.J.; Kotnik, K.; Loughlin, L.; Nilsen, M.; MacLean, M.R. Effect of tryptophan hydroxylase 1 deficiency on the development of hypoxia-induced pulmonary hypertension. Hypertension 2007, 49, 232–236. [Google Scholar] [CrossRef]
- Welford, R.W.D.; Vercauteren, M.; Trébaul, A.; Cattaneo, C.; Eckert, D.; Garzotti, M.; Sieber, P.; Segrestaa, J.; Studer, R.; Groenen, P.M.A.; et al. Serotonin biosynthesis as a predictive marker of serotonin pharmacodynamics and disease-induced dysregulation. Sci. Rep. 2016, 6, 30059. [Google Scholar] [CrossRef]
- Matthes, S.; Bader, M. Peripheral Serotonin Synthesis as a New Drug Target. Trends Pharmacol. Sci. 2018, 39, 560–572. [Google Scholar] [CrossRef]
- Morecroft, I.; White, K.; Caruso, P.; Nilsen, M.; Loughlin, L.; Alba, R.; Reynolds, P.N.; Danilov, S.M.; Baker, A.H.; MacLean, M.R. Gene Therapy by Targeted Adenovirus-mediated Knockdown of Pulmonary Endothelial Tph1 Attenuates Hypoxia-induced Pulmonary Hypertension. Mol. Ther. 2012, 20, 1516–1528. [Google Scholar] [CrossRef] [PubMed]
- Ni, W.; Watts, S.W. 5-hydroxytryptamine in the cardiovascular system: Focus on the serotonin transporter (SERT). Clin. Exp. Pharmacol. Physiol. 2006, 33, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Wang, Y.; Wang, H.M.; Bai, Y.; Zhang, X.H.; Sun, Y.X.; Wang, H.L. Fluoxetine attenuates chronic methamphetamine-induced pulmonary arterial remodelling: Possible involvement of serotonin transporter and serotonin 1B receptor. Basic Clin. Pharmacol. Toxicol. 2013, 112, 77–82. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, M.; Wang, H.M.; Bai, Y.; Zhang, X.H.; Sun, Y.X.; Wang, H.L. Involvement of serotonin mechanism in methamphetamine-induced chronic pulmonary toxicity in rats. Hum. Exp. Toxicol. 2013, 32, 736–746. [Google Scholar] [CrossRef]
- MacLean, M.M.R. The serotonin hypothesis in pulmonary hypertension revisited: Targets for novel therapies (2017 Grover Conference Series). Pulm. Circ. 2018, 8, 2045894018759125. [Google Scholar] [CrossRef] [PubMed]
- Welsh, D.J.; Harnett, M.; MacLean, M.; Peacock, A.J. Proliferation and signaling in fibroblasts: Role of 5-hydroxytryptamine2A receptor and transporter. Am. J. Respir. Crit. Care. Med. 2004, 170, 252–259. [Google Scholar] [CrossRef]
- Cogolludo, A.; Moreno, L.; Lodi, F.; Frazziano, G.; Cobeño, L.; Tamargo, J.; Perez-Vizcaino, F. Serotonin inhibits voltage-gated K+ currents in pulmonary artery smooth muscle cells: Role of 5-HT2A receptors, caveolin-1, and KV1.5 channel internalization. Circ. Res. 2006, 98, 931–938. [Google Scholar] [CrossRef]
- Yang, T.; Wang, H.; Li, Y.; Zeng, Z.; Shen, Y.; Wan, C.; Wu, Y.; Dong, J.; Chen, L.; Wen, F. Serotonin receptors 5-HTR2A and 5-HTR2B are involved in cigarette smoke-induced airway inflammation, mucus hypersecretion and airway remodeling in mice. Int. Immunopharmacol. 2020, 81, 106036. [Google Scholar] [CrossRef]
- Fabre, A.; Marchal-Sommé, J.; Marchand-Adam, S.; Quesnel, C.; Borie, R.; Dehoux, M.; Ruffié, C.; Callebert, J.; Launay, J.M.; Hénin, D.; et al. Modulation of bleomycin-induced lung fibrosis by serotonin receptor antagonists in mice. Eur. Respir. J. 2008, 32, 426–436. [Google Scholar] [CrossRef]
- Königshoff, M.; Dumitrascu, R.; Udalov, S.; Amarie, O.V.; Reiter, R.; Grimminger, F.; Seeger, W.; Schermuly, R.T.; Eickelberg, O. Increased expression of 5-hydroxytryptamine2A/B receptors in idiopathic pulmonary fibrosis: A rationale for therapeutic intervention. Thorax 2010, 65, 949–955. [Google Scholar] [CrossRef]
- Guilbert, F.; Lainée, P.; Dubreuil, B.; McCort, G.; O’Connor, S.E.; Janiak, P.; Herbert, J.-M. Serotonin aggravates exercise-induced cardiac ischemia in the dog: Effect of serotonin receptor antagonists. Eur. J. Pharmacol. 2004, 497, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Rondelet, B.; Van Beneden, R.; Kerbaul, F.; Motte, S.; Fesler, P.; McEntee, K.; Brimioulle, S.; Ketelslegers, J.-M.; Naeije, R. Expression of the serotonin 1b receptor in experimental pulmonary hypertension. Eur. Respir. J. 2003, 22, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Keegan, A.; Morecroft, I.; Smillie, D.; Hicks, M.N.; MacLean, M.R. Contribution of the 5-HT1B receptor to hypoxia-induced pulmonary hypertension: Converging evidence using 5-HT1B-receptor knockout mice and the 5-HT1B/1D-receptor antagonist GR127935. Circ. Res. 2001, 89, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Launay, J.-M.; Herve, P.; Peoc’h, K.; Tournois, C.; Callebert, J.; Nebigil, C.G.; Etienne, N.; Drouet, L.; Humbert, M.; Simonneau, G. Function of the serotonin 5-hydroxytryptamine 2B receptor in pulmonary hypertension. Nat. Med. 2002, 8, 1129–1135. [Google Scholar] [CrossRef] [PubMed]
- Bhat, L.; Hawkinson, J.; Cantillon, M.; Reddy, D.G.; Bhat, S.R.; Laurent, C.-E.; Bouchard, A.; Biernat, M.; Salvail, D. Evaluation of the effects of RP5063, a novel, multimodal, serotonin receptor modulator, as single-agent therapy and co-administrated with sildenafil, bosentan, and treprostinil in a monocrotaline-induced pulmonary arterial hypertension rat model. Eur. J. Pharmacol. 2018, 827, 159–166. [Google Scholar] [CrossRef]
- Bhat, L.; Hawkinson, J.; Cantillon, M.; Reddy, D.G.; Bhat, S.R.; Laurent, C.E.; Bouchard, A.; Biernat, M.; Salvail, D. RP5063, a novel, multimodal, serotonin receptor modulator, prevents Sugen 5416-hypoxia–induced pulmonary arterial hypertension in rats. Eur. J. Pharmacol. 2017, 810, 83–91. [Google Scholar] [CrossRef]
- Bhat, L.; Hawkinson, J.; Cantillon, M.; Reddy, D.G.; Bhat, S.R.; Laurent, C.E.; Bouchard, A.; Biernat, M.; Salvail, D. RP5063, a novel, multimodal, serotonin receptor modulator, prevents monocrotaline-induced pulmonary arterial hypertension in rats. Eur. J. Pharmacol. 2017, 810, 92–99. [Google Scholar] [CrossRef]
- Liu, Y.; Tian, H.; Yan, X.; Fan, F.; Wang, W.; Han, J. Serotonin inhibits apoptosis of pulmonary artery smooth muscle cells through 5-HT2A receptors involved in the pulmonary artery remodeling of pulmonary artery hypertension. Exp. Lung Res. 2013, 39, 70–79. [Google Scholar] [CrossRef]
- Kim, J.; Kim, B.; Kim, S.M.; Yang, C.E.; Song, S.Y.; Lee, W.J.; Lee, J.H. Hypoxia-Induced Epithelial-To-Mesenchymal Transition Mediates Fibroblast Abnormalities via ERK Activation in Cutaneous Wound Healing. Int. J. Mol. Sci. 2019, 20, 2546. [Google Scholar] [CrossRef]
- Jiang, R.; Shi, Y.; Zeng, C.; Yu, W.; Zhang, A.; Du, Y. Protein kinase Cα stimulates hypoxia-induced pulmonary artery smooth muscle cell proliferation in rats through activating the extracellular signal-regulated kinase 1/2 pathway. Mol. Med. Rep. 2017, 16, 6814–6820. [Google Scholar] [CrossRef]
- Kakudo, N.; Morimoto, N.; Ogawa, T.; Taketani, S.; Kusumoto, K. Hypoxia Enhances Proliferation of Human Adipose-Derived Stem Cells via HIF-1α Activation. PLoS ONE 2015, 10, e0139890. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Yang, L.; Shen, J.; Wang, C.; Jiang, Z. The antiproliferative effect of sildenafil on pulmonary artery smooth muscle cells is mediated via upregulation of mitogen-activated protein kinase phosphatase-1 and degradation of extracellular signal-regulated kinase 1/2 phosphorylation. Anesth. Analg. 2007, 105, 1034–1041. [Google Scholar] [CrossRef] [PubMed]
- Lewis, G.D.; Shah, R.; Shahzad, K.; Camuso, J.M.; Pappagianopoulos, P.P.; Hung, J.; Tawakol, A.; Gerszten, R.E.; Systrom, D.M.; Bloch, K.D.; et al. Sildenafil improves exercise capacity and quality of life in patients with systolic heart failure and secondary pulmonary hypertension. Circulation 2007, 116, 1555–1562. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Samaja, M.; Arena, R.; Vicenzi, M.; Guazzi, M.D. Long-term use of sildenafil in the therapeutic management of heart failure. J. Am. Coll. Cardiol. 2007, 50, 2136–2144. [Google Scholar] [CrossRef] [PubMed]
- Dumitrescu, D.; Seck, C.; Möhle, L.; Erdmann, E.; Rosenkranz, S. Therapeutic potential of sildenafil in patients with heart failure and reactive pulmonary hypertension. Int. J. Cardiol. 2012, 154, 205–206. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Vicenzi, M.; Arena, R. Phosphodiesterase 5 inhibition with sildenafil reverses exercise oscillatory breathing in chronic heart failure: A long-term cardiopulmonary exercise testing placebo-controlled study. Eur. J. Heart Fail. 2012, 14, 82–90. [Google Scholar] [CrossRef]
- Behling, A.; Rohde, L.E.; Colombo, F.C.; Goldraich, L.A.; Stein, R.; Clausell, N. Effects of 5′-phosphodiesterase four-week long inhibition with sildenafil in patients with chronic heart failure: A double-blind, placebo-controlled clinical trial. J. Card. Fail. 2008, 14, 189–197. [Google Scholar] [CrossRef]
- Guglin, M.; Rajagopalan, N.; Anaya, P.; Charnigo, R. Sildenafil in heart failure with reactive pulmonary hypertension (Sildenafil HF) clinical trial (rationale and design). Pulm. Circ. 2016, 6, 161–167. [Google Scholar] [CrossRef]
- Kellihan, H.B.; Waller, K.R.; Pinkos, A.; Steinberg, H.; Bates, M.L. Acute resolution of pulmonary alveolar infiltrates in 10 dogs with pulmonary hypertension treated with sildenafil citrate: 2005–2014. J. Vet. Cardiol. 2015, 17, 182–191. [Google Scholar] [CrossRef]
- Marcos, E.; Adnot, S.; Pham, M.H.; Nosjean, A.; Raffestin, B.; Hamon, M.; Eddahibi, S. Serotonin transporter inhibitors protect against hypoxic pulmonary hypertension. Am. J. Respir. Crit. Care Med. 2003, 168, 487–493. [Google Scholar] [CrossRef]
- Tissier, R.; Chetboul, V.; Moraillon, R.; Nicolle, A.; Carlos, C.; Enriquez, B.; Pouchelon, J.L. Increased mitral valve regurgitation and myocardial hypertrophy in two dogs with long-term pimobendan therapy. Cardiovasc. Toxicol. 2005, 5, 43–51. [Google Scholar] [CrossRef]

| Genes | Accession No. | Forward Primer (5′ to 3′) | Reverse Primer (5′ to 3′) | Product Size (bp) | Tm (°C) | Reference of Primers |
|---|---|---|---|---|---|---|
| tph1 | NM_001197191.1 | CTGTGGAGTTTGGTCTCTGTAAG | TGTGATGAGACACTCCTGTTTG | 158 | 82.77 | This study |
| slc6a4 | NM_001110771.1 | GGCTGAGATGAGGAACGAAG | TTGGACCAGATGTGTGGAAA | 222 | 84.43 | This study |
| htr2a | NM_001005869.1 | TCTTTCAGCTTCCTCCCTCA | TCCTCGTTGCAGGACTCTTT | 227 | 84.70 | This study |
| RPS19 | XM_005616513.3 | CCTTCCTCAAAAAGTCTGGG | GTTCTCATCGTAGGGAGCAAG | 95 | 80.69 | Brinkhof et al. [39] |
| RPL32 | XM_022406256.1 | TGGTTACAGGAGCAACAAGAAA | GCACATCAGCAGCACTTCA | 100 | 81.54 | Peters, Peeters, Helps and Day [37] |
| Normal (n = 4) | DMVD (n = 5) | DMVD with PH (n = 5) | p-Value | |
|---|---|---|---|---|
| Sex (male/female) | 3/1 | 1/4 | 3/2 | - |
| Age (years) | 8 (7.8–10.0) | 15 (14–15) | 14 (13–15) | |
| Weight (kg) | 5.6 (5.28–6.93) | 3.92 (3.7–4.14) | 4.3 (2.8–6.9) | |
| Breed | Shih-Tzu (n = 2) Cocker Spaniel (n = 1) Mixed breed (n = 1) | Poodle (n = 3) Shih-Tzu (n = 1) Pomeranian (n = 1) | Chihuahua (n = 2) Poodle (n = 2) Pomeranian (n = 1) | - |
| Stage (C/D) | - | 2/3 | 1/4 | - |
| Medication | - | ACEIs (n = 5) Furosemide (n = 5) Pimobendane (n = 5) Spironolactone (n = 2) Moduretic (n = 1) | ACEIs (n = 5) Furosemide (n = 5) Pimobendane (n = 5) Spironolactone (n = 2) Moduretic (n = 2) Sildenafil (n = 1) | - |
| DMVD (n = 5) | DMVD with PH (n = 5) | p-Value | |
|---|---|---|---|
| LA index (cm/kg) | 1.67 ± 0.28 | 1.83 ± 0.72 | 0.642 |
| Ao index (cm/kg) | 1.01 ± 0.42 | 1.02 ± 0.28 | 0.952 |
| LA/Ao | 1.80 ± 0.56 | 1.75 ± 0.38 | 0.862 |
| IVSdN index (cm/kg) | 0.59 ± 0.13 | 0.56 ± 0.14 | 0.663 |
| LVIDdN index (cm/kg) | 2.84 ± 0.87 | 1.66 ± 0.62 | 0.038 |
| LVPWdN index (cm/kg) | 0.55 ± 0.24 | 0.48 ± 0.17 | 0.621 |
| IVSsN index (cm/kg) | 0.92 ± 0.30 | 0.84 ± 0.29 | 0.707 |
| LVIDsN index (cm/kg) | 1.59 ± 0.50 | 0.72 ± 0.30 | 0.010 |
| LVPWsN index (cm/kg) | 0.85 ± 0.33 | 0.71 ± 0.10 | 0.407 |
| %FS | 42.14 ± 5.82 | 55.16 ± 7.91 | 0.018 |
| PAP (mmHg) | - | 72.03 ± 25.96 | - |
| Gene | Normal (n = 4) | DMVD (n = 5) | DMVD with PH (n = 5) | p-Value |
|---|---|---|---|---|
| Lung tissues (×10−3) | ||||
| tph1 | 0.61 (0.04–3.29) | 0.24 (0.06–4.21) | 0.13 (0.07–0.53) | 0.680 |
| slc6a4 | 3.32 (0.19–6.23) | 1.11 (0.58–3.03) | 0.27 (0.13–1.03) | 0.081 |
| htr2a | 0.33 (0.23–0.68) | 0.10 (0.09–0.55) | 0.33 (0.29–0.34) | 0.154 |
| PA tissues (×10−3) | ||||
| tph1 | 0.20 (0.04–3.89) | 1.89 (0.58–6.58) | 1.01 (0.45–1.71) | 0.117 |
| slc6a4 | 1.60 (0.08–5.89) | 11.03 (10.66–11.40) | 0.74 (0.12–14.94) | 0.252 |
| htr2a | 14.46 (0.85–20.05) | 2.00 (0.43–3.22) | 5.79 (0.41–19.19) | 0.270 |
| Proteins | Normal (n = 4) | DMVD (n = 5) | DMVD with PH (n = 5) | p-Value |
|---|---|---|---|---|
| Lung tissues | ||||
| TPH-1 | 2.33 (0.58–4.09) | 1.59 (0.52–5.43) | 1.56 (0.68–5.08) | 0.362 |
| SERT | 1.14 (0.09–3.10) | 0.46 (0.04–1.00) | 1.49 (0.24–1.69) | 0.373 |
| 5-HTR2A | 4.40 (0.97–10.75) | 2.59 (1.12–9.46) | 3.15 (2.36–8.88) | 0.656 |
| ERK1/2 | 1.74 (0.68–6.37) | 1.41 (0.72–5.38) | 2.16 (1.04–4.29) | 0.680 |
| pERK1/2 | 0.72 (0.13–2.01) | 1.02 (0.35–4.09) | 0.21 (0.07–2.59) | 0.284 |
| PA tissues | ||||
| TPH-1 | 0.65 (0.49–1.12) | 0.81 (0.29–4.09) | 1.85 (0.51–2.95) | 0.401 |
| SERT | 0.23 (0.14–0.39) | 0.14 (0.04–0.63) | 0.40 (0.04–0.74) | 0.761 |
| 5-HTR2A | 0.68 (0.44–1.00) | 0.99 (0.37–4.67) | 1.58 (0.50–2.57) | 0.350 |
| ERK1/2 | 0.86 (0.73–1.04) | 0.81 (0.54–4.23) | 1.04 (0.48–4.15) | 0.831 |
| pERK1/2 | 0.61 (0.35–0.89) | 0.45 (0.11–2.26) | 0.56 (0.10–2.87) | 0.990 |
| Proteins | Cells | Normal (n = 4) | DMVD (n = 5) | DMVD with PH (n = 5) | p-Value |
|---|---|---|---|---|---|
| TPH-1 | Pneumocytes | 1.63 ± 0.13 | 2.76 ± 0.57 a,b | 4.90 ± 0.99 a,c | <0.001 |
| PAMs Bronchial epithelial cells | 0.28 ± 0.16 74.84 ± 2.82 | 0.65 ± 0.26 76.62 ± 5.33 | 0.52 ± 0.21 81.83 ± 8.98 | 0.074 0.273 | |
| SERT | Pneumocytes | 1.28 ± 0.24 | 3.50 ± 1.03 a | 4.35 ± 1.11 a | <0.001 |
| PAMs Bronchial epithelial cells | 0.29 ± 0.14 67.59 ± 3.12 | 1.63 ± 0.94 a 69.87 ± 5.09 | 1.23 ± 0.47 a 71.90 ± 4.37 | 0.028 0.371 | |
| 5-HTR2A | Pneumocytes | 3.89 ± 0.48 | 7.36 ± 1.03 a | 7.29 ± 1.24 a | <0.001 |
| PAMs Bronchial epithelial cells | 1.67 ± 0.29 86.52 ± 3.90 | 3.62 ± 1.00 a 84.79 ± 7.24 | 3.73 ± 0.65 a 87.32 ± 6.24 | 0.005 0.804 | |
| ERK1/2 | Pneumocytes | 0.81 ± 0.10 | 2.40 ± 0.25 a,b | 1.54 ± 0.41 a,c | <0.001 |
| PAMs Bronchial epithelial cells | 0.24 ± 0.02 78.84 ± 6.55 | 0.78 ± 0.43 76.82 ± 3.51 | 0.41 ± 0.16 81.01 ± 6.95 | 0.059 0.540 | |
| pERK1/2 | Pneumocytes | 0.86 ± 0.18 | 1.63 ± 0.68 | 1.61 ± 0.43 | 0.243 |
| PAMs Bronchial epithelial cells | 0.00 ± 0.00 0.00 ± 0.00 | 0.49 ± 0.30 26.16 ± 4.39 a,b | 0.53 ± 0.28 92.39 ± 7.19 a,c | 0.108 < 0.001 |
| Organ or Cell | Genes or Proteins | Echo Parameters | r | p-Value |
|---|---|---|---|---|
| Lung | tph1 | LA/Ao | 0.648 | 0.043 |
| pERK1/2 | LA/Ao | 0.758 | 0.011 | |
| pERK1/2 | LVIDsN | 0.721 | 0.019 | |
| PA | slc6a4 | LVIDdN | 0.857 | 0.014 |
| slc6a4 | LVIDsN | 0.857 | 0.014 | |
| 5-HTR2A | PAP | −0.943 | 0.005 | |
| Pneumocyte | TPH-1 | %FS | 0.705 | 0.023 |
| TPH-1 | PAP | 0.829 | 0.042 | |
| 5-HTR2A | IVSdN | −0.693 | 0.026 | |
| pERK1/2 | LVPWsN | 0.638 | 0.047 | |
| PAM | SERT | PAP | 0.829 | 0.042 |
| ERK1/2 | LVPWsN | 0.648 | 0.043 | |
| pERK1/2 | LA | 0.721 | 0.019 | |
| pERK1/2 | LA/Ao | 0.685 | 0.029 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tangmahakul, N.; Sakarin, S.; Techangamsuwan, S.; Rungsipipat, A.; Surachetpong, S.D. Investigation of Genes and Proteins Expression Associating Serotonin Signaling Pathway in Lung and Pulmonary Artery Tissues of Dogs with Pulmonary Hypertension Secondary to Degenerative Mitral Valve Disease: The Preliminary Study. Vet. Sci. 2022, 9, 530. https://doi.org/10.3390/vetsci9100530
Tangmahakul N, Sakarin S, Techangamsuwan S, Rungsipipat A, Surachetpong SD. Investigation of Genes and Proteins Expression Associating Serotonin Signaling Pathway in Lung and Pulmonary Artery Tissues of Dogs with Pulmonary Hypertension Secondary to Degenerative Mitral Valve Disease: The Preliminary Study. Veterinary Sciences. 2022; 9(10):530. https://doi.org/10.3390/vetsci9100530
Chicago/Turabian StyleTangmahakul, Nattawan, Siriwan Sakarin, Somporn Techangamsuwan, Anudep Rungsipipat, and Sirilak Disatian Surachetpong. 2022. "Investigation of Genes and Proteins Expression Associating Serotonin Signaling Pathway in Lung and Pulmonary Artery Tissues of Dogs with Pulmonary Hypertension Secondary to Degenerative Mitral Valve Disease: The Preliminary Study" Veterinary Sciences 9, no. 10: 530. https://doi.org/10.3390/vetsci9100530
APA StyleTangmahakul, N., Sakarin, S., Techangamsuwan, S., Rungsipipat, A., & Surachetpong, S. D. (2022). Investigation of Genes and Proteins Expression Associating Serotonin Signaling Pathway in Lung and Pulmonary Artery Tissues of Dogs with Pulmonary Hypertension Secondary to Degenerative Mitral Valve Disease: The Preliminary Study. Veterinary Sciences, 9(10), 530. https://doi.org/10.3390/vetsci9100530






