Investigation on the Effect of Dose, Frequency and Duration of Allergen Exposure on Development of Staphylococcal Infections in a Chronic Model of Canine Atopic Dermatitis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Dogs
2.2. Protocols for Allergen Challenges
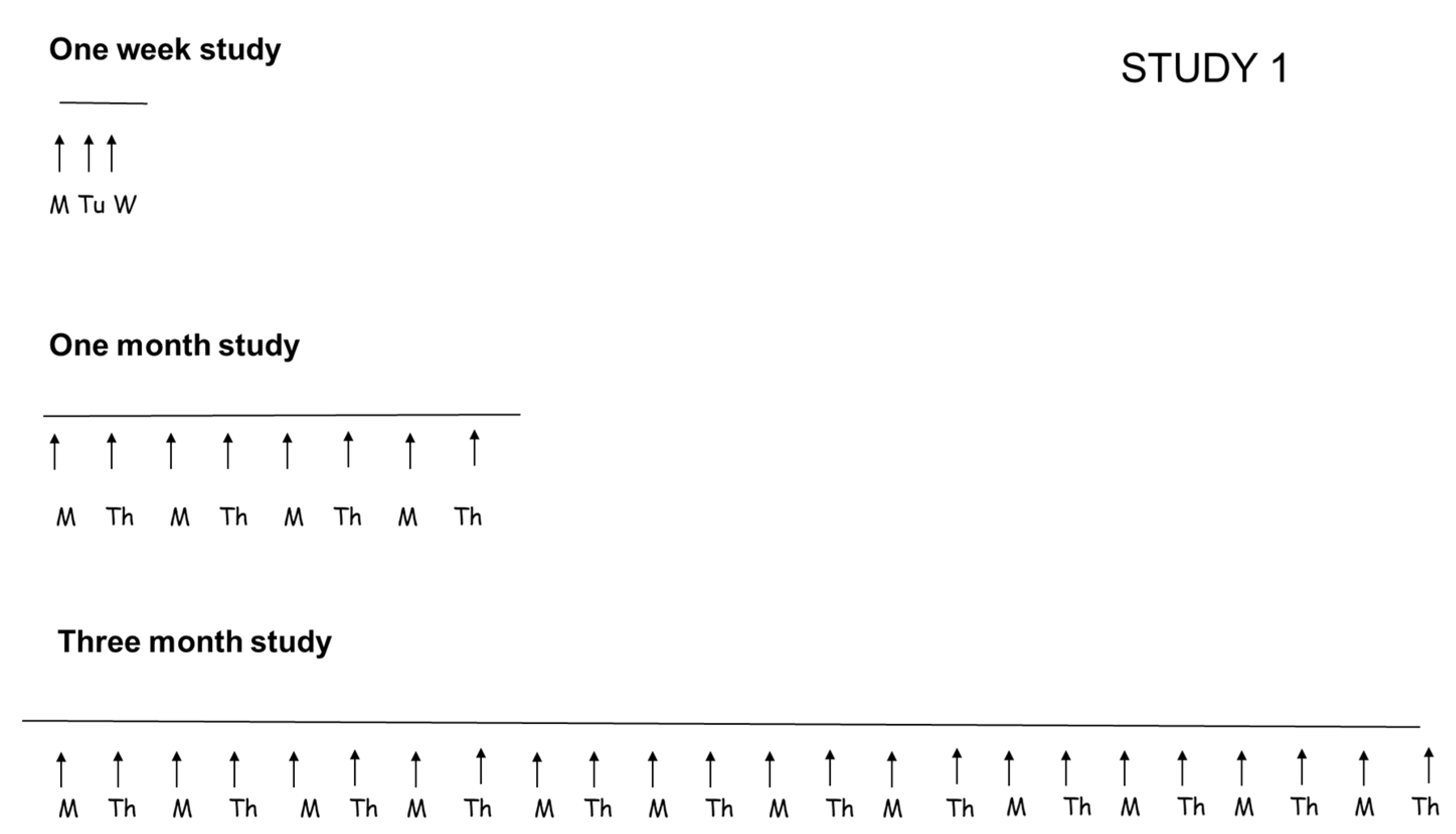
2.2.1. Study 1: Evaluation of Duration of Allergen Exposure
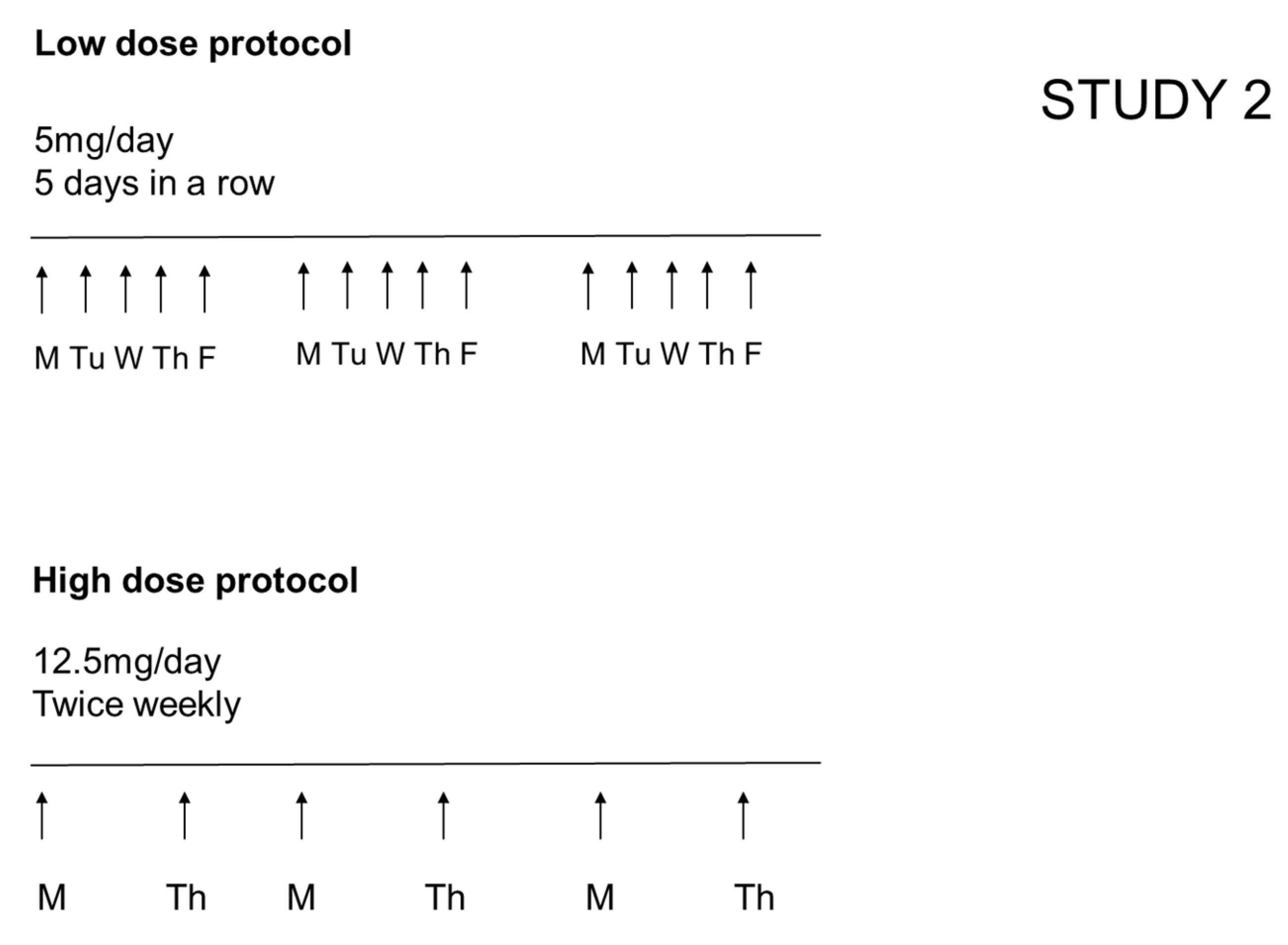
2.2.2. Study 2: Evaluation of the Effect of Different Daily Doses (While Keeping Constant the Total Weekly Dose of Allergen and the Overall Duration of the Study)
2.3. Clinical Assessment of Severity of Dermatitis and Development of Pyoderma
2.4. Statistical Analysis
3. Results
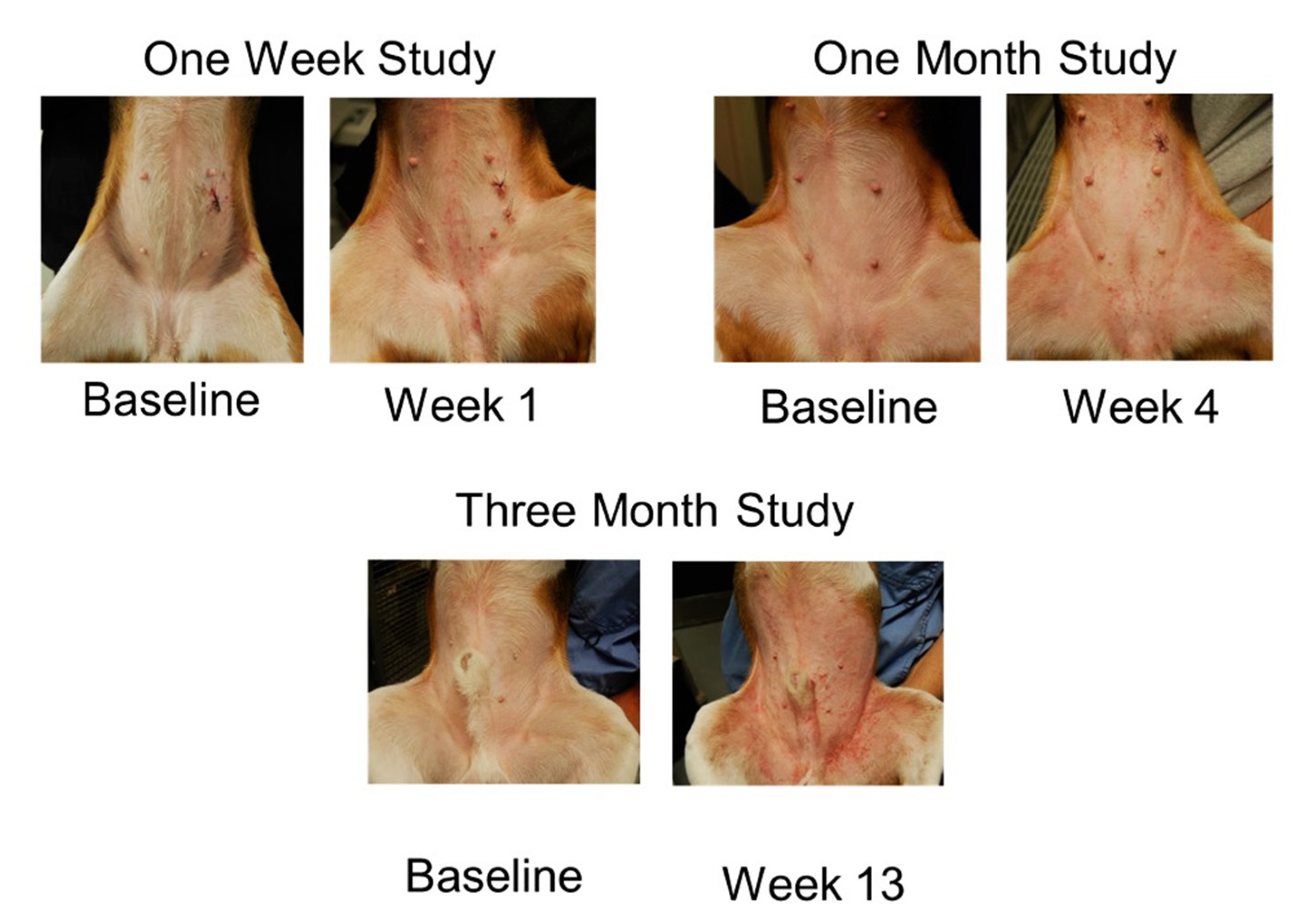
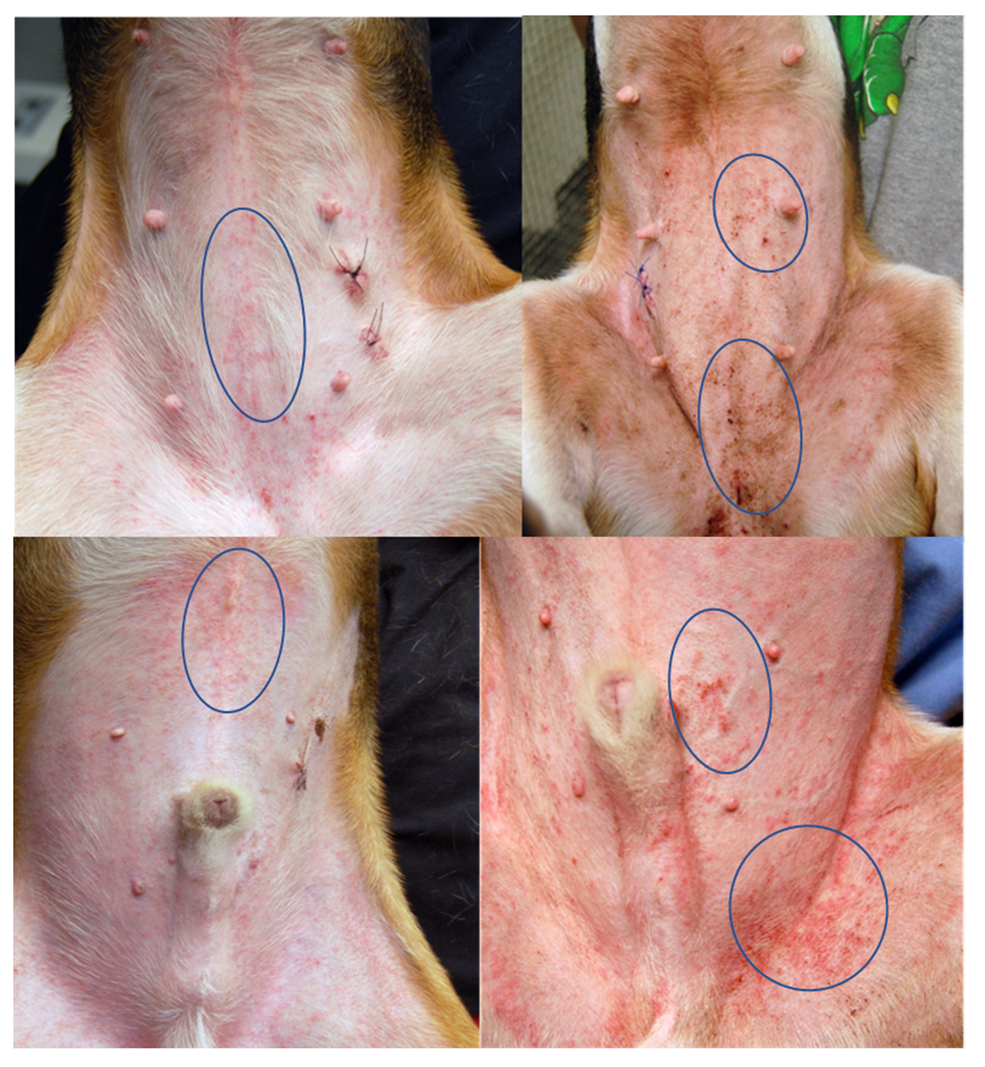
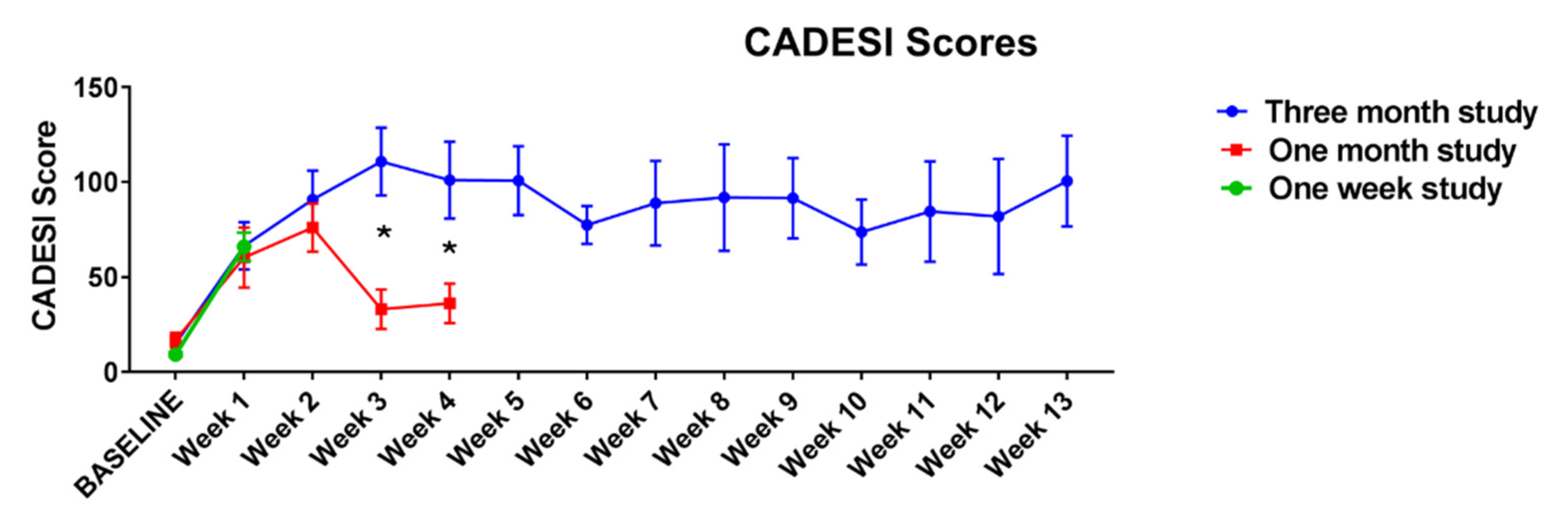
3.1. Study 1. Evaluation of Duration of Allergen Exposure (While Keeping the Dose of the Allergen Challenge the Same)
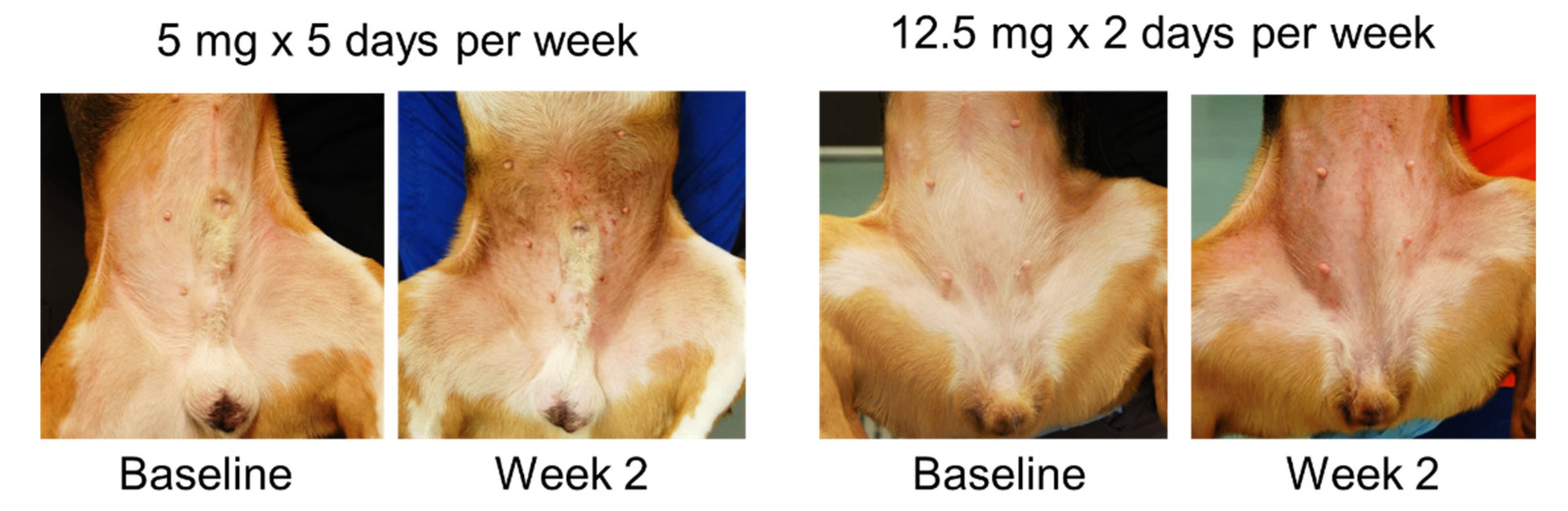
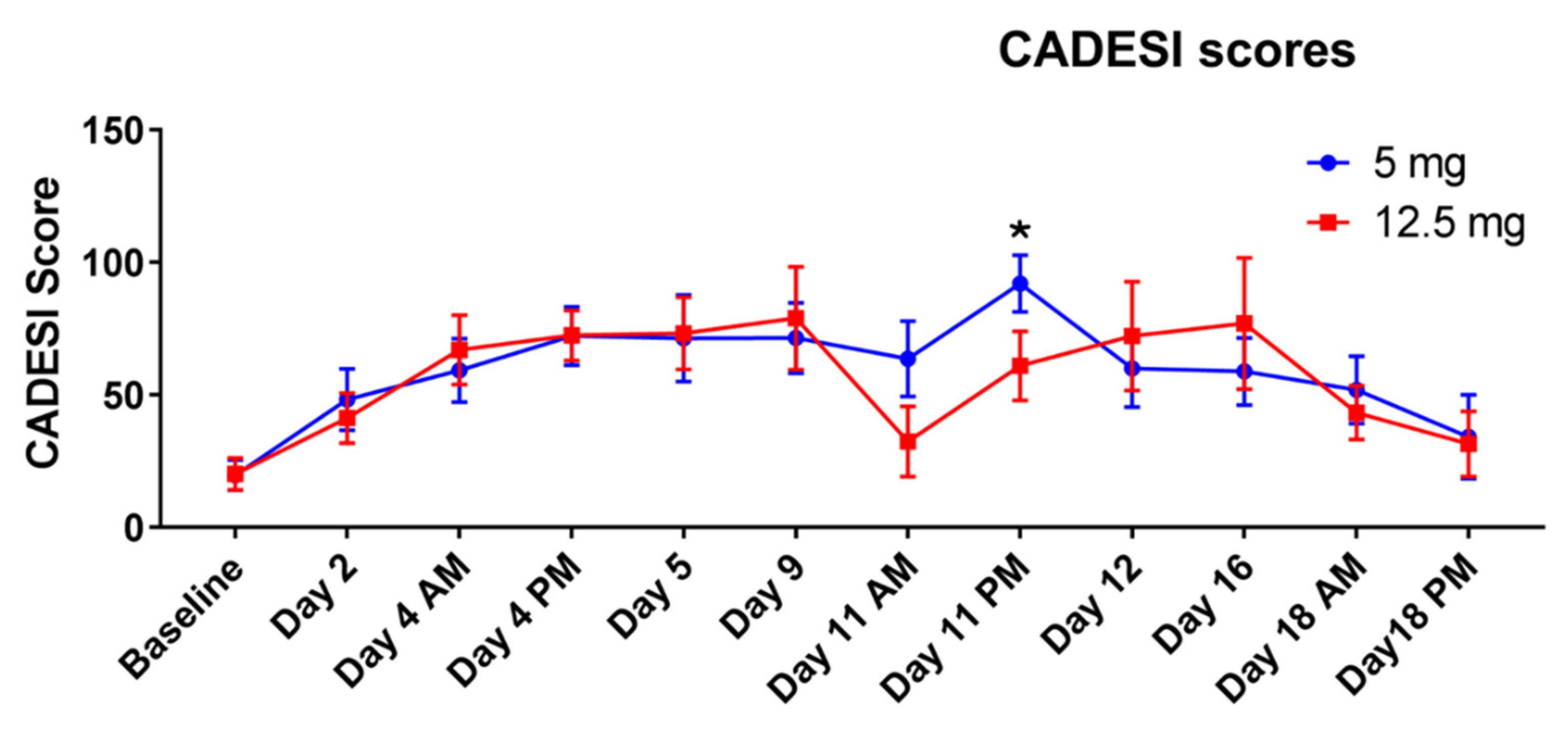
3.2. Study 2. Evaluation of the Effect of Different Daily Doses (While Keeping Constant the Total Weekly Dose of Allergen and the Overall Duration of the Study)
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Olivry, T.; DeBoer, D.J.; Favrot, C.; Jackson, H.A.; Mueller, R.S.; Nuttall, T.; Prélaud, P. International Task Force on Canine Atopic Dermatitis. Treatment of canine atopic dermatitis: 2010 clinical practice guidelines from the International Task Force on Canine Atopic Dermatitis. Vet. Dermatol. 2010, 21, 233–248. [Google Scholar] [CrossRef] [PubMed]
- DeBoer, D.J.; Marsella, R. The ACVD task force on canine atopic dermatitis (XII): The relationship of cutaneous infections to the pathogenesis and clinical course of canine atopic dermatitis. Vet. Immunol. Immunopathol. 2001, 81, 239–249. [Google Scholar] [CrossRef]
- Bradley, C.W.; Morris, D.O.; Rankin, S.C.; Cain, C.L.; Misic, A.M.; Houser, T.; Mauldin, E.A.; Grice, E.A. Longitudinal Evaluation of the Skin Microbiome and Association with Microenvironment and Treatment in Canine Atopic Dermatitis. J. Investig. Dermatol. 2016, 136, 1182–1190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loeffler, A.; Lloyd, D.H. What has changed in canine pyoderma? A narrative review. Vet. J. 2018, 235, 73–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Damme, C.M.M.; Broens, E.M.; Auxilia, S.T.; Schlotter, Y.M. Clindamycin resistance of skin derived Staphylococcus pseudintermedius is higher in dogs with a history of antimicrobial therapy. Vet. Dermatol. 2020, 31, 305-e75. [Google Scholar] [CrossRef] [PubMed]
- Elnageh, H.R.; Hiblu, M.A.; Abbassi, M.S.; Abouzeed, Y.M.; Ahmed, M.O. Prevalence and antimicrobial resistance of Staphylococcus species isolated from cats and dogs. Open Vet. J. 2021, 10, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.; Ahrens, K.; Devalaraja, M.; Dymond, M.; Fagura, M.; Hargreaves, A.; Holt, A.; Peers, I.; Price, S.; Reens, J.; et al. Use of a Canine Model of Atopic Dermatitis to Investigate the Efficacy of a CCR4 Antagonist in Allergen-Induced Skin Inflammation in a Randomized Study. J. Investig. Dermatol. 2016, 136, 665–671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marsella, R.; Olivry, T.; Nicklin, C.; Lopez, J. Pilot investigation of a model for canine atopic dermatitis: Environmental house dust mite challenge of high-IgE-producing beagles, mite hypersensitive dogs with atopic dermatitis and normal dogs. Vet. Dermatol. 2006, 17, 24–35. [Google Scholar] [CrossRef] [PubMed]
- Bäumer, W.; Stahl, J.; Sander, K.; Petersen, L.J.; Paps, J.; Stark, H.; Kietzmann, M.; Olivry, T. Lack of preventing effect of systemically and topically administered histamine H(1) or H(4) receptor antagonists in a dog model of acute atopic dermatitis. Exp. Dermatol. 2011, 20, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Olivry, T.; Dunston, S.M. Expression patterns of superficial epidermal adhesion molecules in an experimental dog model of acute atopic dermatitis skin lesions. Vet. Dermatol. 2015, 26, 53–56. [Google Scholar] [CrossRef] [PubMed]
- Olivry, T.; Mayhew, D.; Paps, J.S.; Linder, K.E.; Peredo, C.; Rajpal, D.; Hofland, H.; Cote-Sierra, J. Early Activation of Th2/Th22 Inflammatory and Pruritogenic Pathways in Acute Canine Atopic Dermatitis Skin Lesions. J. Investig. Dermatol. 2016, 136, 1961–1969. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blubaugh, A.; Denley, T.; Banovic, F. Characterization of a chloroquine-induced canine model of pruritus and skin inflammation. Vet. Dermatol. 2020, 31, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Olivry, T.; Wofford, J.; Paps, J.S.; Dunston, S.M. Stratum corneum removal facilitates experimental sensitization to mite allergens in atopic dogs. Vet. Dermatol. 2011, 22, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Olivry, T.; Marsella, R.; Iwasaki, T.; Mueller, R. International Task Force On Canine Atopic Dermatitis. Validation of CADESI-03, a severity scale for clinical trials enrolling dogs with atopic dermatitis. Vet. Dermatol. 2007, 18, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Cork, M.J.; Robinson, D.A.; Vasilopoulos, Y.; Ferguson, A.; Moustafa, M.; MacGowan, A.; Duff, G.W.; Ward, S.J.; Tazi-Ahnini, R. New perspectives on epidermal barrier dysfunction in atopic dermatitis: Gene-environment interactions. J. Allergy Clin. Immunol. 2006, 118, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Pierezan, F.; Olivry, T.; Paps, J.S.; Lawhon, S.D.; Wu, J.; Steiner, J.M.; Suchodolski, J.S.; Rodrigues Hoffmann, A. The skin microbiome in allergen-induced canine atopic dermatitis. Vet. Dermatol. 2016, 27, 332-e82. [Google Scholar] [CrossRef] [PubMed]
- Randall, A.; Hillier, A.; Cole, L.K.; Kwochka, K.W.; Needham, G.; Wassom, D.L. Quantitation of house dust mites and house dust mite allergens in the microenvironment of dogs. Am. J. Vet. Res. 2003, 64, 1580–1588. [Google Scholar] [CrossRef] [PubMed]
- Pucheu-Haston, C.M.; Shuster, D.; Olivry, T.; Brianceau, P.; Lockwood, P.; McClanahan, T.; de Waal Malefyt, R.; Mattson, J.D.; Hammerberg, B. A canine model of cutaneous late-phase reactions: Prednisolone inhibition of cellular and cytokine responses. Immunology 2006, 117, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Olivry, T.; Deangelo, K.B.; Dunston, S.M.; Clarke, K.B.; McCall, C.A. Patch testing of experimentally sensitized beagle dogs: Development of a model for skin lesions of atopic dermatitis. Vet. Dermatol. 2006, 17, 95–102. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marsella, R. Investigation on the Effect of Dose, Frequency and Duration of Allergen Exposure on Development of Staphylococcal Infections in a Chronic Model of Canine Atopic Dermatitis. Vet. Sci. 2022, 9, 8. https://doi.org/10.3390/vetsci9010008
Marsella R. Investigation on the Effect of Dose, Frequency and Duration of Allergen Exposure on Development of Staphylococcal Infections in a Chronic Model of Canine Atopic Dermatitis. Veterinary Sciences. 2022; 9(1):8. https://doi.org/10.3390/vetsci9010008
Chicago/Turabian StyleMarsella, Rosanna. 2022. "Investigation on the Effect of Dose, Frequency and Duration of Allergen Exposure on Development of Staphylococcal Infections in a Chronic Model of Canine Atopic Dermatitis" Veterinary Sciences 9, no. 1: 8. https://doi.org/10.3390/vetsci9010008
APA StyleMarsella, R. (2022). Investigation on the Effect of Dose, Frequency and Duration of Allergen Exposure on Development of Staphylococcal Infections in a Chronic Model of Canine Atopic Dermatitis. Veterinary Sciences, 9(1), 8. https://doi.org/10.3390/vetsci9010008




