Mice Treated Subcutaneously with Mouse LPS-Converted PrPres or LPS Alone Showed Brain Gene Expression Profiles Characteristic of Prion Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals and Experimental Design
2.2. Euthanasia at 11 Weeks Post-Inoculation and Terminal Stage
2.3. Total RNA Isolation
2.4. Custom-Made PCR Array
2.5. First Strand cDNA Synthesis and Quantitative PCR (qPCR) Assay
2.6. Protein Expression and Purification
2.7. Statistical Analysis
3. Results and Discussion
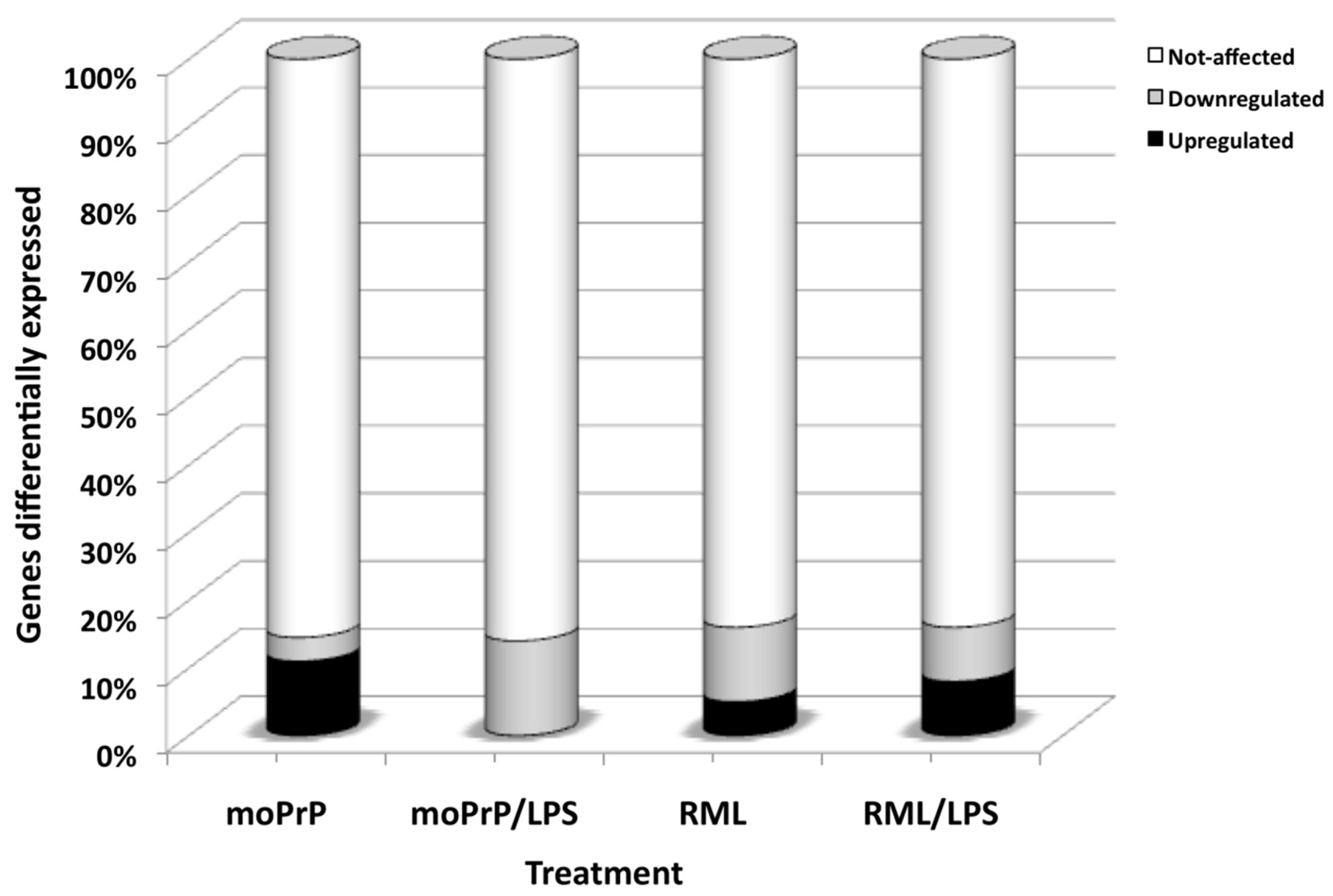
3.1. Subcutaneous Injection of LPS, moPrPres, RML and Combinations of LPS Altered Gene Expression in the Brains of Mice at 11 Weeks Post-Infection
3.2. Reduction of Sprn mRNA Expression at Terminal Stage
3.3. Decreased Expression of ApoE and Bax in moPrPres, moPrPres/LPS, and LPS Treatments
3.4. Atp1b1, Prkaca, Ncam1, and Sod1 Down-Regulated in all the Treatments Except moPrPres
3.5. Down-Regulation of SOD1 in moPrPres, RML, and RML/LPS Treatments
3.6. Up-Regulation of Immune Response Genes by moPrPres Treatment
3.7. Immune Response Genes Uniquely Regulated by LPS Treatment
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Prusiner, S.B. Prions. Proc. Nat. Acad. Sci. USA 1998, 95, 13363–13383. [Google Scholar] [CrossRef]
- Legname, G.; Baskakov, I.V.; Nguyen, H.O.; Riesner, D.; Cohen, F.E.; DeArmond, S.J.; Prusiner, S.B. Synthetic mammalian prions. Science 2004, 305, 673–676. [Google Scholar] [CrossRef]
- Deleault, N.R.; Harris, B.T.; Rees, J.R.; Supattapone, S. Formation of native prions from minimal components in vitro. Proc. Nat. Acad. Sci. USA 2007, 104, 9741–9746. [Google Scholar] [CrossRef] [PubMed]
- Barria, M.A.; Mukherjee, A.; Gonzalez-Romero, D.; Morales, R.; Soto, C. De novo generation of infectious prions in vitro produces a new disease phenotype. PLoS Pathog. 2009, 5, e1000421. [Google Scholar] [CrossRef] [PubMed]
- Makarava, N.; Kovacs, G.G.; Bocharova, O.; Savtchenko, R.; Alexeeva, I.; Budka, H.; Rohwer, R.G.; Baskakov, I.V. Recombinant prion protein induces a new transmissible prion disease in wild-type animals. Acta Neuropathol. 2010, 119, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Wangm, F.; Wangm, X.; Yuan, C.G.; Ma, J. Generating a prion with bacterially expressed recombinant prion protein. Science 2010, 327, 1132–1135. [Google Scholar] [CrossRef] [PubMed]
- Castilla, J.; Saa, P.; Hetz, C.; Soto, C. In vitro generation of infectious scrapie prions. Cell 2005, 121, 195–206. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, Z.; Wang, X.; Li, J.; Zha, L.; Yuan, C.G.; Weissmann, C.; Ma, J. Genetic informational RNA is not required for recombinant prion infectivity. J. Virol. 2012, 86, 1874–1876. [Google Scholar] [CrossRef]
- Riemer, C.; Queck, I.; Simon, D.; Kurth, R.; Baier, M. Identification of upregulated genes in scrapie-infected brain tissue. J. Virol. 2000, 74, 10245–10248. [Google Scholar] [CrossRef] [PubMed]
- Xiang, W.; Windl, O.; Wunsch, G.; Dugas, M.; Kohlmann, A.; Dierkes, N.; Westner, I.M.; Kretzschmar, H.A. Identification of differentially expressed genes in scrapie-infected mouse brains by using global gene expression technology. J. Virol. 2004, 78, 11051–11060. [Google Scholar] [CrossRef]
- Booth, S.; Bowman, C.; Baumgartner, R.; Sorensen, G.; Robertson, C.; Coulthart, M.; Phillipson, C.; Somorjai, R.L. Identification of central nervous system genes involved in the host response to the scrapie agent during preclinical and clinical infection. J. Gen. Virol. 2004, 85, 3459–3471. [Google Scholar] [CrossRef]
- Skinner, P.J.; Abbassi, H.; Chesebro, B.; Race, R.E.; Reilly, C.; Haase, A.T. Gene expression alterations in brains of mice infected with three strains of scrapie. BMC Genom. 2006, 7, 114. [Google Scholar] [CrossRef]
- Sawiris, G.P.; Becker, K.G.; Elliott, E.J.; Moulden, R.; Rohwer, R.G. Molecular analysis of bovine spongiform encephalopathy infection by cDNA arrays. J. Gen. Virol. 2007, 88, 1356–1362. [Google Scholar] [CrossRef]
- Westaway, D.; Daude, N.; Wohlgemuth, S.; Harrison, P. The PrP-like proteins Shadoo and Doppel. Top. Curr. Chem. 2011, 305, 225–256. [Google Scholar] [PubMed]
- Westaway, D.; Genovesi, S.; Daude, N.; Brown, R.; Lau, A.; Lee, I.; Mays, C.E.; Coomaraswamy, J.; Canine, B.; Pitstick, R.; et al. Down-regulation of Shadoo in prion infections traces a pre-clinical event inversely related to PrP(Sc) accumulation. PLoS Pathog. 2011, 7, e1002391. [Google Scholar] [CrossRef]
- Watts, J.C.; Giles, K.; Grillo, S.K.; Lemus, A.; DeArmond, S.J.; Prusiner, S.B. Bioluminescence imaging of Abeta deposition in bigenic mouse models of Alzheimer’s disease. Proc. Nat. Acad. Sci. USA 2011, 108, 2528–2533. [Google Scholar] [CrossRef] [PubMed]
- Saleem, F.; Bjorndahl, T.C.; Ladner, C.L.; Perez-Pineiro, R.; Ametaj, B.N.; Wishart, D.S. Lipopolysaccharide induced conversion of recombinant prion protein. Prion 2014, 8, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Olfert, E.D.; Cross, B.M.; McWilliam, A.A. The Guide to the Care and Use of Experimental Animals. Can. Counc. Anim. Care 1993, 19–22. [Google Scholar]
- Bjorndahl, T.C.; Zhou, G.P.; Liu, X.; Perez-Pineiro, R.; Semenchenko, V.; Saleem, F.; Acharya, S.; Bujold, A.; Sobsey, C.A.; Wishart, D.S. Detailed biophysical characterization of the acid-induced PrP(c) to PrP(beta) conversion process. Biochemistry 2011, 50, 1162–1173. [Google Scholar] [CrossRef]
- Mabbott, N.A.; Bruce, M.E.; Botto, M.; Walport, M.J.; Pepys, M.B. Temporary depletion of complement component C3 or genetic deficiency of C1q significantly delays onset of scrapie. Nat. Med. 2001, 7, 485–487. [Google Scholar] [CrossRef]
- Moncada, S.; Bolanos, J.P. Nitric oxide, cell bioenergetics and neurodegeneration. J. Neurochem. 2006, 97, 1676–1689. [Google Scholar] [CrossRef]
- Bruijn, L.I.; Miller, T.M.; Cleveland, D.W. Unraveling the mechanisms involved in motor neuron degeneration in ALS. Ann. Rev. Neurosci. 2004, 27, 723–749. [Google Scholar] [CrossRef]
- Mogi, M.; Harada, M.; Narabayashi, H.; Inagaki, H.; Minami, M.; Nagatsu, T. Interleukin (IL)-1 beta, IL-2, IL-4, IL-6 and transforming growth factor-alpha levels are elevated in ventricular cerebrospinal fluid in juvenile parkinsonism and Parkinson’s disease. Neurosci. Lett. 1996, 211, 13–16. [Google Scholar] [CrossRef]
- Griffin, W.S.; Stanley, L.C.; Ling, C.; White, L.; MacLeod, V.; Perrot, L.J.; White, C.L., 3rd; Araoz, C. Brain interleukin 1 and S-100 immunoreactivity are elevated in Down syndrome and Alzheimer disease. Proc. Nat. Acad. Sci. USA 1989, 86, 7611–7615. [Google Scholar] [CrossRef]
- Stanley, L.C.; Mrak, R.E.; Woody, R.C.; Perrot, L.J.; Zhang, S.; Marshak, D.R.; Nelson, S.J.; Griffin, W.S. Glial cytokines as neuropathogenic factors in HIV infection: Pathogenic similarities to Alzheimer’s disease. J. Neuropathol. Experim. Neurol. 1994, 53, 231–238. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, M.C.; Powers, J.M.; Bias, W.B.; Schmeckpeper, B.J.; Segal, A.H.; Gowda, V.C.; Wesselingh, S.L.; Berger, J.; Griffin, D.E.; Smith, K.D. Human leukocyte antigens and cytokine expression in cerebral inflammatory demyelinative lesions of X-linked adrenoleukodystrophy and multiple sclerosis. J. Neuroimmunol. 1997, 75, 174–182. [Google Scholar] [CrossRef]
- Hauser, S.L.; Doolittle, T.H.; Lincoln, R.; Brown, R.H.; Dinarello, C.A. Cytokine accumulations in CSF of multiple sclerosis patients: Frequent detection of interleukin-1 and tumor necrosis factor but not interleukin-6. Neurology 1990, 40, 1735–1739. [Google Scholar] [CrossRef] [PubMed]
- Van Everbroeck, B.; Dewulf, E.; Pals, P.; Lubke, U.; Martin, J.J.; Cras, P. The role of cytokines, astrocytes, microglia and apoptosis in Creutzfeldt-Jakob disease. Neurobiol. Aging 2002, 23, 59–64. [Google Scholar] [CrossRef]
- Premzl, M.; Sangiorgio, L.; Strumbo, B.; Marshall Graves, J.A.; Simonic, T.; Gready, J.E. Shadoo, a new protein highly conserved from fish to mammals and with similarity to prion protein. Gene 2003, 314, 89–102. [Google Scholar] [CrossRef]
- Watts, J.C.; Drisaldi, B.; Ng, V.; Yang, J.; Strome, B.; Horne, P.; Sy, M.S.; Yoong, L.; Young, R.; Mastrangelo, P.; et al. The CNS glycoprotein Shadoo has PrP(C)-like protective properties and displays reduced levels in prion infections. EMBO J. 2007, 26, 4038–4050. [Google Scholar] [CrossRef]
- Daude, N.; Westaway, D. Biological properties of the PrP-like Shadoo protein. Front. Biosci. (Landmark Ed.) 2011, 16, 1505–1516. [Google Scholar] [CrossRef]
- Murakami, T.; Paitel, E.; Kawarabayashi, T.; Ikeda, M.; Chishti, M.A.; Janus, C.; Matsubara, E.; Sasaki, A.; Kawarai, T.; Phinney, A.L.; et al. Cortical neuronal and glial pathology in TgTauP301L transgenic mice: Neuronal degeneration, memory disturbance, and phenotypic variation. Am. J. Pathol. 2006, 169, 1365–1375. [Google Scholar] [CrossRef] [PubMed]
- Chishti, M.A.; Yang, D.S.; Janus, C.; Phinney, A.L.; Horne, P.; Pearson, J.; Strome, R.; Zuker, N.; Loukides, J.; French, J.; et al. Early-onset amyloid deposition and cognitive deficits in transgenic mice expressing a double mutant form of amyloid precursor protein 695. J. Biol. Chem. 2001, 276, 21562–21570. [Google Scholar] [CrossRef]
- Watts, J.C.; Huo, H.; Bai, Y.; Ehsani, S.; Jeon, A.H.; Shi, T.; Daude, N.; Lau, A.; Young, R.; Xu, L.; et al. Interactome analyses identify ties of PrP and its mammalian paralogs to oligomannosidic N-glycans and endoplasmic reticulum-derived chaperones. PLoS Pathog. 2009, 5, e1000608. [Google Scholar] [CrossRef]
- Coomaraswamy, J.; Kilger, E.; Wolfing, H.; Schafer, C.; Kaeser, S.A.; Wegenast-Braun, B.M.; Hefendehl, J.K.; Wolburg, H.; Mazzella, M.; Ghiso, J.; et al. Modeling familial Danish dementia in mice supports the concept of the amyloid hypothesis of Alzheimer’s disease. Proc. Nat. Acad. Sci. USA 2010, 107, 7969–7974. [Google Scholar] [CrossRef] [PubMed]
- Horsburgh, K.; Kelly, S.; McCulloch, J.; Higgins, G.A.; Roses, A.D.; Nicoll, J.A. Increased neuronal damage in apolipoprotein E-deficient mice following global ischaemia. Neuroreport 1999, 10, 837–841. [Google Scholar] [CrossRef] [PubMed]
- White, F.; Nicoll, J.A.; Roses, A.D.; Horsburgh, K. Impaired neuronal plasticity in transgenic mice expressing human apolipoprotein E4 compared to E3 in a model of entorhinal cortex lesion. Neurobiol. Dis. 2001, 8, 611–625. [Google Scholar] [CrossRef]
- Krugers, H.J.; Mulder, M.; Korf, J.; Havekes, L.; de Kloet, E.R.; Joels, M. Altered synaptic plasticity in hippocampal CA1 area of apolipoprotein E deficient mice. Neuroreport 1997, 8, 2505–2510. [Google Scholar] [CrossRef] [PubMed]
- Gong, J.; Jellali, A.; Forster, V.; Mutterer, J.; Dubus, E.; Altrock, W.D.; Sahel, J.A.; Rendon, A.; Picaud, S. The toxicity of the PrP106-126 prion peptide on cultured photoreceptors correlates with the prion protein distribution in the mammalian and human retina. Am. J. Pathol. 2007, 170, 1314–1324. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wolter, K.G.; Hsu, Y.T.; Smith, C.L.; Nechushtan, A.; Xi, X.G.; Youle, R.J. Movement of Bax from the cytosol to mitochondria during apoptosis. J. Cell Biol. 1997, 139, 1281–1292. [Google Scholar] [CrossRef] [PubMed]
- Jurgensmeier, J.M.; Xie, Z.; Deveraux, Q.; Ellerby, L.; Bredesen, D.; Reed, J.C. Bax directly induces release of cytochrome c from isolated mitochondria. Proc. Nat. Acad. Sci. USA 1998, 95, 4997–5002. [Google Scholar] [CrossRef]
- Bounhar, Y.; Zhang, Y.; Goodyer, C.G.; LeBlanc, A. Prion protein protects human neurons against Bax-mediated apoptosis. J. Biol. Chem. 2001, 276, 39145–39149. [Google Scholar] [CrossRef]
- Manczak, M.; Anekonda, T.S.; Henson, E.; Park, B.S.; Quinn, J.; Reddy, P.H. Mitochondria are a direct site of A beta accumulation in Alzheimer’s disease neurons: Implications for free radical generation and oxidative damage in disease progression. Hum. Mol. Gen. 2006, 15, 1437–1449. [Google Scholar] [CrossRef]
- Wong-Riley, M.T.T. Bigenomic Regulation of Cytochrome C Oxidase in Neurons and the Tight Coupling between Neuronal Activity and Energy Metabolism. Adv. Exp. Med. Biol. 2012, 748, 283–304. [Google Scholar]
- Edelman, G.M. Cell adhesion molecules in the regulation of animal form and tissue pattern. Annu. Rev. Cell Biol. 1986, 2, 81–116. [Google Scholar] [CrossRef]
- Ronn, L.C.; Hartz, B.P.; Bock, E. The neural cell adhesion molecule (NCAM) in development and plasticity of the nervous system. Exp. Gerontol. 1998, 33, 853–864. [Google Scholar] [CrossRef]
- Nait Oumesmar, B.; Vignais, L.; Duhamel-Clerin, E.; Avellana-Adalid, V.; Rougon, G.; Baron-Van Evercooren, A. Expression of the highly polysialylated neural cell adhesion molecule during postnatal myelination and following chemically induced demyelination of the adult mouse spinal cord. Europ. J. Neurosci. 1995, 7, 480–491. [Google Scholar] [CrossRef]
- Pedersen, W.A.; McCullers, D.; Culmsee, C.; Haughey, N.J.; Herman, J.P.; Mattson, M.P. Corticotropin-releasing hormone protects neurons against insults relevant to the pathogenesis of Alzheimer’s disease. Neurobiol. Dis. 2001, 8, 492–503. [Google Scholar] [CrossRef]
- Pedersen, W.A.; Wan, R.; Zhang, P.; Mattson, M.P. Urocortin, but not urocortin II, protects cultured hippocampal neurons from oxidative and excitotoxic cell death via corticotropin-releasing hormone receptor type I. J. Neurosci. 2002, 22, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.R.; Schulz-Schaeffer, W.J.; Schmidt, B.; Kretzschmar, H.A. Prion protein-deficient cells show altered response to oxidative stress due to decreased SOD-1 activity. Exp. Neur. 1997, 146, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.R.; Besinger, A. Prion protein expression and superoxide dismutase activity. Biochem. J. 1998, 334, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Klamt, F.; Dal-Pizzol, F.; Conte da Frota, M.L., Jr.; Walz, R.; Andrades, M.E.; da Silva, E.G.; Brentani, R.R.; Izquierdo, I.; Fonseca Moreira, J.C. Imbalance of antioxidant defense in mice lacking cellular prion protein. Free Rad. Biol. Med. 2001, 30, 1137–1144. [Google Scholar] [CrossRef]
- Sakudo, A.; Lee, D.C.; Li, S.; Nakamura, T.; Matsumoto, Y.; Saeki, K.; Itohara, S.; Ikuta, K.; Onodera, T. PrP cooperates with STI1 to regulate SOD activity in PrP-deficient neuronal cell line. Biochem. Biophys. Res. Commun. 2005, 328, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Carri, M.T.; Cozzolino, M. SOD1 and mitochondria in ALS: A dangerous liaison. J. Bioenerg. Biomembr. 2011, 43, 593–599. [Google Scholar] [CrossRef]
- Jóhannesson, T.; Kristinsson, J.; Snædal, J. Neurodegenerative diseases, antioxidative enzymes and copper. A review of experimental research. Laeknabladid 2003, 89, 659–671. [Google Scholar] [PubMed]
- Spinner, D.S.; Cho, I.S.; Park, S.Y.; Kim, J.I.; Meeker, H.C.; Ye, X.; Lafauci, G.; Kerr, D.J.; Flory, M.J.; Kim, B.S.; et al. Accelerated prion disease pathogenesis in Toll-like receptor 4 signaling-mutant mice. J. Virol. 2008, 82, 10701–10708. [Google Scholar] [CrossRef] [PubMed]
- Prinz, M.; Heikenwalder, M.; Schwarz, P.; Takeda, K.; Akira, S.; Aguzzi, A. Prion pathogenesis in the absence of Toll-like receptor signalling. EMBO Rep. 2003, 4, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Muzio, M.; Ni, J.; Feng, P.; Dixit, V.M. IRAK (Pelle) family member IRAK-2 and MyD88 as proximal mediators of IL-1 signaling. Science 1997, 278, 1612–1615. [Google Scholar] [CrossRef]
- Medzhitov, R.; Preston-Hurlburt, P.; Kopp, E.; Stadlen, A.; Chen, C.; Ghosh, S.; Janeway, C.A., Jr. MyD88 is an adaptor protein in the hToll/IL-1 receptor family signaling pathways. Mol. Cell 1998, 2, 253–258. [Google Scholar] [CrossRef]
- Sakudo, A.; Lee, D.C.; Saeki, K.; Matsumoto, Y.; Itohara, S.; Onodera, T. Tumor necrosis factor attenuates prion protein-deficient neuronal cell death by increases in anti-apoptotic Bcl-2 family proteins. Biochem. Biophys. Chem. Comm. 2003, 310, 725–729. [Google Scholar] [CrossRef]
- Takeuchi, H.; Jin, S.; Wang, J.; Zhang, G.; Kawanokuchi, J.; Kuno, R.; Sonobe, Y.; Mizuno, T.; Suzumura, A. Tumor necrosis factor-alpha induces neurotoxicity via glutamate release from hemichannels of activated microglia in an autocrine manner. J. Biol. Chem. 2006, 281, 21362–21368. [Google Scholar] [CrossRef]
- Lumpkins, K.; Bochicchio, G.V.; Zagol, B.; Ulloa, K.; Simard, J.M.; Schaub, S.; Meyer, W.; Scalea, T. Plasma levels of the beta chemokine regulated upon activation, normal T cell expressed, and secreted (RANTES) correlate with severe brain injury. J. Trauma 2008, 64, 358–361. [Google Scholar] [CrossRef]
- Skuljec, J.; Sun, H.; Pul, R.; Benardais, K.; Ragancokova, D.; Moharregh-Khiabani, D.; Kotsiari, A.; Trebst, C.; Stangel, M. CCL5 induces a pro-inflammatory profile in microglia in vitro. Cell. Immunol. 2011, 270, 164–171. [Google Scholar] [CrossRef]
- Lee, J.K.; Schuchman, E.H.; Jin, H.K.; Bae, J.S. Soluble CCL5 derived from bone marrow-derived mesenchymal stem cells and activated by amyloid beta ameliorates Alzheimer’s disease in mice by recruiting bone marrow-induced microglia immune responses. Stem Cells 2012, 30, 1544–1555. [Google Scholar] [CrossRef]
- Sato, W.; Kadomatsu, K.; Yuzawa, Y.; Muramatsu, H.; Hotta, N.; Matsuo, S.; Muramatsu, T. Midkine is involved in neutrophil infiltration into the tubulointerstitium in ischemic renal injury. J. Immunol. 2001, 167, 3463–3469. [Google Scholar] [CrossRef] [PubMed]
- Horiba, M.; Kadomatsu, K.; Nakamura, E.; Muramatsu, H.; Ikematsu, S.; Sakuma, S.; Hayashi, K.; Yuzawa, Y.; Matsuo, S.; Kuzuya, M.; et al. Neointima formation in a restenosis model is suppressed in midkine-deficient mice. J. Clin. Investig. 2000, 105, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Warmlander, S.K.; Graslund, A.; Abrahams, J.P. Human lysozyme inhibits the in vitro aggregation of Abeta peptides, which in vivo are associated with Alzheimer’s disease. Chem. Commun. (Camb.) 2013, 49, 6507–6509. [Google Scholar] [CrossRef] [PubMed]
- Manuelidis, L.; Tesin, D.M.; Sklaviadis, T.; Manuelidis, E.E. Astrocyte gene expression in Creutzfeldt-Jakob disease. Proc. Nat. Acad. Sci. USA 1987, 84, 5937–5941. [Google Scholar] [CrossRef] [PubMed]
- Nimmerjahn, F.; Ravetch, J.V. Fcgamma receptors as regulators of immune responses. Nat. Rev. Immunol. 2008, 8, 34–47. [Google Scholar] [CrossRef]
- Coxon, A.; Cullere, X.; Knight, S.; Sethi, S.; Wakelin, M.W.; Stavrakis, G.; Luscinskas, F.W.; Mayadas, T.N. Fc gamma RIII mediates neutrophil recruitment to immune complexes. a mechanism for neutrophil accumulation in immune-mediated inflammation. Immunity 2001, 14, 693–704. [Google Scholar] [CrossRef]
- Tsuboi, N.; Asano, K.; Lauterbach, M.; Mayadas, T.N. Human neutrophil Fcgamma receptors initiate and play specialized nonredundant roles in antibody-mediated inflammatory diseases. Immunity 2008, 28, 833–846. [Google Scholar] [CrossRef]
- Liu, S.; Liu, Y.; Hao, W.; Wolf, L.; Kiliaan, A.J.; Penke, B.; Rube, C.E.; Walter, J.; Heneka, M.T.; Hartmann, T.; et al. TLR2 is a primary receptor for Alzheimer’s amyloid beta peptide to trigger neuroinflammatory activation. J. Immunol. 2012, 188, 1098–1107. [Google Scholar] [CrossRef]
- Craft, J.M.; Watterson, D.M.; Hirsch, E.; Van Eldik, L.J. Interleukin 1 receptor antagonist knockout mice show enhanced microglial activation and neuronal damage induced by intracerebroventricular infusion of human beta-amyloid. J. Neuroinflamm. 2005, 2, 15. [Google Scholar] [CrossRef] [PubMed]
- Kam, T.I.; Song, S.; Gwon, Y.; Park, H.; Yan, J.J.; Im, I.; Choi, J.W.; Choi, T.Y.; Kim, J.; Song, D.K.; et al. FcgammaRIIb mediates amyloid-beta neurotoxicity and memory impairment in Alzheimer’s disease. J. Clin. Investig. 2013, 123, 2791–2802. [Google Scholar] [CrossRef]
- Neitzert, K.; Albayram, O.; Göhrs, R.; Müller, C.; Karaca, I.; Kumar, S.; Cron, M.; Walter, J.; Förster, I.; Bilkei-Gorzo, A.; et al. CCL17 deficiency is associated with beneficial CNS immune responses and prevents cognitive decline in a mouse model of Alzheimer’s disease. Brain Behav. Immun. 2013, 39, S21. [Google Scholar] [CrossRef]
- Meucci, O.; Fatatis, A.; Simen, A.A.; Bushell, T.J.; Gray, P.W.; Miller, R.J. Chemokines regulate hippocampal neuronal signaling and gp120 neurotoxicity. Proc. Nat. Acad. Sci. USA 1998, 95, 14500–14505. [Google Scholar] [CrossRef] [PubMed]
- Almeida, S.; Zhou, L.; Gao, F.B. Progranulin, a glycoprotein deficient in frontotemporal dementia, is a novel substrate of several protein disulfide isomerase family proteins. PLoS ONE 2011, 6, e26454. [Google Scholar] [CrossRef]
- Baker, M.; Mackenzie, I.R.; Pickering-Brown, S.M.; Gass, J.; Rademakers, R.; Lindholm, C.; Snowden, J.; Adamson, J.; Sadovnick, A.D.; Rollinson, S.; et al. Mutations in progranulin cause tau-negative frontotemporal dementia linked to chromosome 17. Nature 2006, 442, 916–919. [Google Scholar] [CrossRef] [PubMed]
- Okura, H.; Yamashita, S.; Ohama, T.; Saga, A.; Yamamoto-Kakuta, A.; Hamada, Y.; Sougawa, N.; Ohyama, R.; Sawa, Y.; Matsuyama, A. HDL/apolipoprotein A-I binds to macrophage-derived progranulin and suppresses its conversion into proinflammatory granulins. J. Atheroscler. Thromb. 2010, 17, 568–577. [Google Scholar] [CrossRef]
- He, Z.; Ong, C.H.; Halper, J.; Bateman, A. Progranulin is a mediator of the wound response. Nature Med. 2003, 9, 225–229. [Google Scholar] [CrossRef]
- Kim, H.O.; Snyder, G.P.; Blazey, T.M.; Race, R.E.; Chesebro, B.; Skinner, P.J. Prion disease induced alterations in gene expression in spleen and brain prior to clinical symptoms. Adv. Applic. Bioinfo. Chem. AABC 2008, 1, 29–50. [Google Scholar]
| Gene Symbol | Gene Name | Fold Change | p-Value |
|---|---|---|---|
| Apoe | Apolipoprotein | −7.6 | 0.001 |
| GbP4 | Guanylate binding protein 4 | −2.4 | 0.02 |
| Grn | Granulin | −2.4 | 0.02 |
| Sod1 | Superoxide dismutase 1, soluble | −3.0 | 0.001 |
| Bax | BCL2-associated X protein | −3.8 | 0.01 |
| Ccl17 | Chemokine (C-C motif) ligand 17 | −1.5 | 0.04 |
| Apoe | Apolipoprotein E | −2.8 | 0.02 |
| Sprn | Shadow of prion protein | −2.2 | 0.01 |
| C1qb | Complement component 1, q subcomponent, beta polypeptide | −1.7 | 0.005 |
| Ifi27I2a | Interferon, alpha-inducible protein 27 like 2A | 1.8 | 0.01 |
| Nos2 | Nitric oxide synthase 2, inducible | 1.5 | 0.04 |
| Tlr6 | Toll-like receptor 6 | 2.1 | 0.001 |
| Tlr3 | Toll-like receptor 3 | 2.8 | 0.03 |
| C4b | Complement component 4B (Chido blood group) | −1.9 | 0.07 |
| Nos2 | Nitric oxide synthase 2, inducible | 1.4 | 0.08 |
| Il1a | Interleukin 1 alpha | 2.2 | 0.06 |
| Il1f10 | Interleukin 1 family, member 10 | 1.4 | 0.08 |
| H2-T23 | Histocompatibility 2, T region locus 23 | 1.8 | 0.03 |
| C1qb | Complement component 1, q subcomponent, beta polypeptide | −1.8 | 0.09 |
| Rtp4 | Receptor transporter protein 4 | −2.2 | 0.09 |
| Sod1 | Superoxide dismutase 1, soluble | −1.2 | 0.08 |
| Ccl25 | Chemokine (C-C motif) ligand 25 | 2.3 | 0.01 |
| C1qb | Complement component 1, q subcomponent, beta polypeptide | −1.8 | 0.01 |
| C4b | Complement component 4B (Chido blood group) | −2.2 | 0.08 |
| Grn | Granulin | −1.4 | 0.05 |
| Anp32a | Acidic (leucine-rich) nuclear phosphoprotein 32 family, member | −1.9 | 0.05 |
| Sod1 | Superoxide dismutase 1, soluble | −1.5 | 0.01 |
| Bax | BCL2-associated X protein | −1.9 | 0.05 |
| Gene Symbol | Gene Name | Fold Change | p-Value |
|---|---|---|---|
| Apoe | Apolipoprotein E | −2.53 | 0.003 |
| Ache | Acetylcholinesterase | −3.19 | 0.08 |
| Sprn | Shadow of prion protein | −3.21 | 0.01 |
| Iftm3 | Interferon induced transmembrane protein 3 | 2.50 | 0.09 |
| Fcgr2b | Fc receptor, IgG, low affinity IIb | −2.50 | 0.08 |
| Fcgr3 | Fc receptor, IgG, low affinity III | 1.60 | 0.04 |
| Grn | Granulin | −3.19 | 0.01 |
| H2-T23 | Histocompatibility 2, T region locus 23 | 1.98 | 0.03 |
| Ly86 | Lymphocyte antigen 86 | 1.59 | 0.05 |
| Gfap | Glial fibrillary acidic protein | −2.02 | 0.03 |
| Anp32a | Acidic (leucine-rich) nuclear phosphoprotein 32 family, member A | 1.59 | 0.07 |
| Ncam1 | Neural cell adhesion molecule 1 | 3.10 | 0.07 |
| Bax | BCL2-associated X protein | −2.00 | 0.04 |
| Ccl17 | Chemokine (C-C motif) ligand 17 | −1.97 | 0.04 |
| Ccl19 | Chemokine (C-C motif) ligand 19 | −2.53 | 0.02 |
| Mdk | Midkine | 4.99 | 0.03 |
| Ccl25 | Chemokine (C-C motif) ligand 25 | 2.49 | 0.04 |
| Tlr3 | Toll-like receptor 3 | 2.52 | 0.01 |
| Prnp | Prion protein | 1.27 | 0.55 |
| Prnd | Prion protein dublet | 3.15 | 0.06 |
| Gene | Gene Name | Fold Change | p-Value |
|---|---|---|---|
| DE genes in moPrPres vs. saline | |||
| Apoe | Apolipoprotein E | −3.77 | 0.01 |
| Sprn | Shadow of prion protein | −2.39 | 0.02 |
| Ifitm3 | Interferon induced transmembrane protein 3 | 4.23 | 0.01 |
| Myd88 | Myeloid differentiation primary response gene 88 | 1.70 | 0.02 |
| Bax | Bcl2-associated X protein | −3.78 | 0.01 |
| Fyn | Fyn proto-oncogene | 1.69 | 0.02 |
| Tlr4 | Toll-like receptor 4 | 1.68 | 0.02 |
| Ccl5 | Chemokine (C-C motif) ligand 5 | 3.33 | 0.01 |
| Tnf | Tumor necrosis factor | 1.75 | 0.01 |
| Fcgr3 | Fc receptor, IgG, low affinity III | 2.13 | 0.05 |
| Lyz2 | Lysozyme 2 | 1.68 | 0.09 |
| Mdk | Midkine | 2.11 | 0.08 |
| Tlr1 | Toll-like receptor 1 | 6.99 | 0.05 |
| Il1rn | Interleukin 1 receptor antagonist | 3.48 | 0.09 |
| Prnp | Prion protein | −2.99 | 0.25 |
| Prnd | Prion protein dublet | −1.17 | 0.98 |
| DE genes in moPrPres + LPS vs. saline | |||
| Apoe | Apolipoprotein E | −10.98 | 0.01 |
| Sprn | Shadow of prion protein | −3.46 | 0.01 |
| Gfap | Glial fibrillary acidic protein | −3.45 | 0.03 |
| Atp1b1 | ATPase, Na+/K+ transporting, beta 1 polypeptide | −8.68 | 0.01 |
| Prkaca | Protein kinase, cAMP dependent, catalytic, alpha | −3.42 | 0.03 |
| Ncam1 | Neural cell adhesion molecule 1 | −4.33 | 0.05 |
| Sod1 | Superoxide dismutase 1, soluble | −3.46 | 0.06 |
| Bax | Bcl2-associated X protein | −2.73 | 0.05 |
| Fyn | Fyn proto-oncogene | −2.75 | 0.05 |
| Il18 | Interleukin 18 | −4.35 | 0.06 |
| Adam9 | A disintegrin and metallopeptidase domain 9 | −3.48 | 0.05 |
| Ache | Acetylcholinesterase | −4.34 | 0.08 |
| Prnp | Prion protein | −2.74 | 0.12 |
| Prnd | Prion protein dublet | 2.36 | 0.39 |
| Gene | Gene Name | Fold Change | p-Value |
|---|---|---|---|
| DE genes in RML vs. saline | |||
| Sprn | Shadow of prion protein | −3.13 | 0.01 |
| Lyz2 | Lysozyme 2 | 4.08 | 0.001 |
| Atp1b1 | ATPase, Na+/K+ transporting, beta 1 polypeptide | −6.20 | 0.01 |
| Ncam1 | Neural cell adhesion molecule 1 | −3.90 | 0.02 |
| Prkaca | Protein kinase, cAMP dependent, catalytic, alpha | −3.89 | 0.01 |
| Egr1 | Early growth response 1 | −6.20 | 0.001 |
| Tlr3 | Toll-like receptor 3 | 2.56 | 0.03 |
| Ache | Acetylcholinesterase | −3.90 | 0.08 |
| Fcgr3 | Fc receptor, IgG, low affinity III | 2.59 | 0.09 |
| Ly86 | Lymphocyte antigen 86 | 4.08 | 0.06 |
| Anp32a | Acidic (leucine-rich) nuclear phosphoprotein 32 family, member A | −1.95 | 0.08 |
| Sod1 | Superoxide dismutase 1, soluble | −3.12 | 0.06 |
| Bax | Bcl2-associated X protein | −2.46 | 0.06 |
| Prnp | Prion protein | −1.93 | 0.18 |
| Prnd | Prion protein dublet | 10.82 | 0.14 |
| DE genes in RML + LPS vs. saline | |||
| Sprn | Shadow of prion protein | −1.94 | 0.01 |
| C1qb | complement component 1, q subcomponent, beta polypeptide | 2.61 | 0.03 |
| Ly86 | Lymphocyte antigen 86 | 2.05 | 0.02 |
| Lyz2 | Lysozyme 2 | 5.18 | 0.01 |
| Atp1b1 | ATPase, Na+/K+ transporting, beta 1 polypeptide | −19.46 | 0.01 |
| Anp32a | Acidic (leucine-rich) nuclear phosphoprotein 32 family, member A | −3.07 | 0.03 |
| Ncam1 | Neural cell adhesion molecule 1 | −7.76 | 0.01 |
| Sod1 | Superoxide dismutase 1, soluble | −4.87 | 0.01 |
| Prkaca | Protein kinase, cAMP dependent, catalytic, alpha | −3.84 | 0.03 |
| Egr1 | Early growth response 1 | −4.85 | 0.001 |
| H2-k1 | Histocompatibility 2, K1, K region | 2.58 | 0.02 |
| C4b | Complement component 4B (Childo blood group) | 6.51 | 0.09 |
| Ifi27i2a | Interferon, alpha-inducible protein 27 like 2A | 8.24 | 0.08 |
| A2m | Alpha-2-macroglobulin | 6.53 | 0.09 |
| Prnp | Prion protein | −2.47 | 0.10 |
| Prnd | Prion protein dublet | 3.29 | 0.38 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hailemariam, D.; Goldansaz, S.A.; Daude, N.; Wishart, D.S.; Ametaj, B.N. Mice Treated Subcutaneously with Mouse LPS-Converted PrPres or LPS Alone Showed Brain Gene Expression Profiles Characteristic of Prion Disease. Vet. Sci. 2021, 8, 200. https://doi.org/10.3390/vetsci8090200
Hailemariam D, Goldansaz SA, Daude N, Wishart DS, Ametaj BN. Mice Treated Subcutaneously with Mouse LPS-Converted PrPres or LPS Alone Showed Brain Gene Expression Profiles Characteristic of Prion Disease. Veterinary Sciences. 2021; 8(9):200. https://doi.org/10.3390/vetsci8090200
Chicago/Turabian StyleHailemariam, Dagnachew, Seyed Ali Goldansaz, Nathalie Daude, David S. Wishart, and Burim N. Ametaj. 2021. "Mice Treated Subcutaneously with Mouse LPS-Converted PrPres or LPS Alone Showed Brain Gene Expression Profiles Characteristic of Prion Disease" Veterinary Sciences 8, no. 9: 200. https://doi.org/10.3390/vetsci8090200
APA StyleHailemariam, D., Goldansaz, S. A., Daude, N., Wishart, D. S., & Ametaj, B. N. (2021). Mice Treated Subcutaneously with Mouse LPS-Converted PrPres or LPS Alone Showed Brain Gene Expression Profiles Characteristic of Prion Disease. Veterinary Sciences, 8(9), 200. https://doi.org/10.3390/vetsci8090200







