Cat and/or Dog Ownership, Cardiovascular Disease, and Obesity: A Systematic Review
Abstract
:1. Introduction
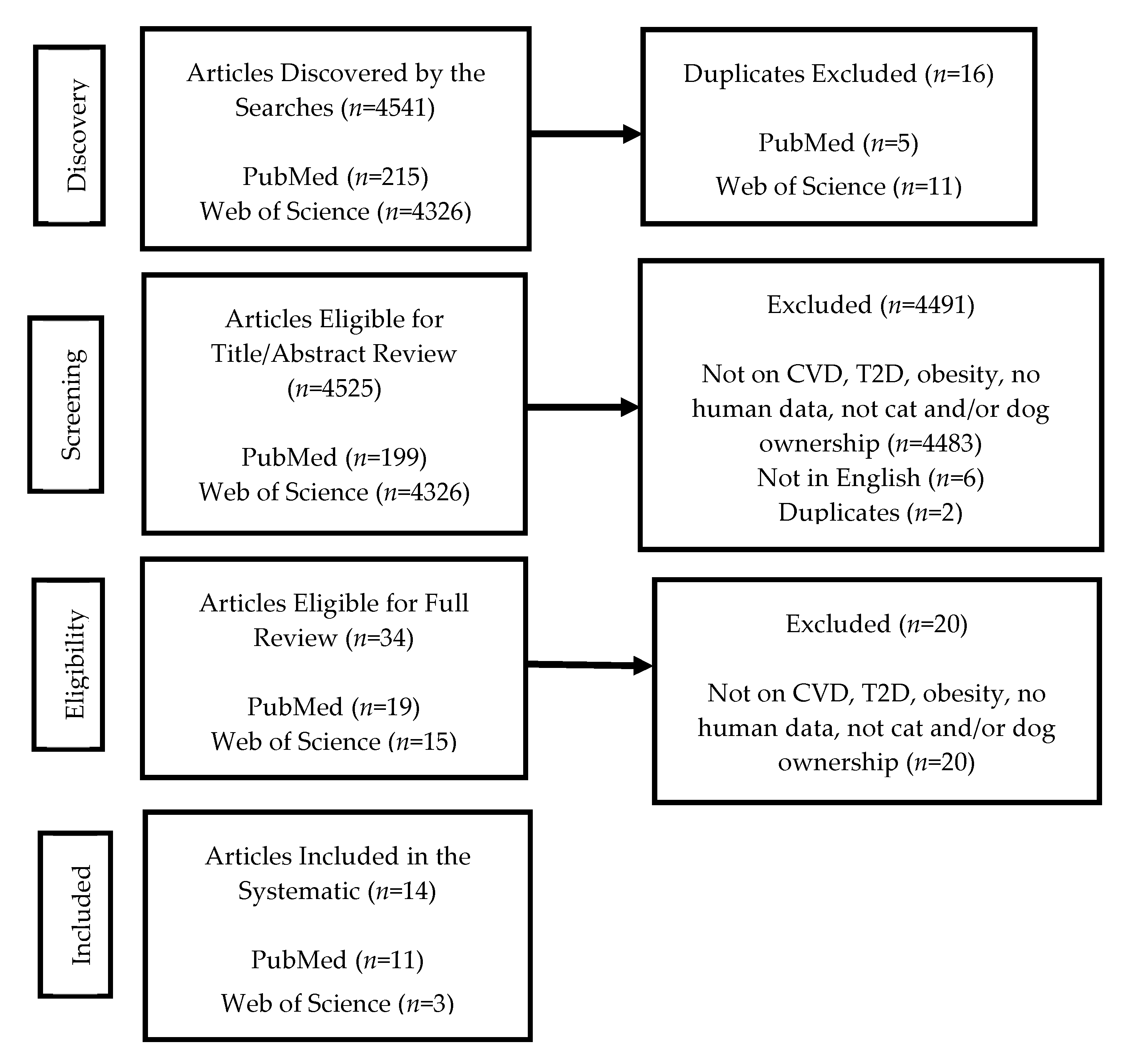
2. Materials and Methods
3. Results
3.1. CVD Studies
3.2. Obesity Studies
3.3. Quality/Bias Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Bernell, S.; Howard, S.W. Use your words carefully: What is a chronic disease? Front. Public Health 2016, 4, 159. [Google Scholar] [CrossRef] [Green Version]
- Buttorff, C.; Ruder, T.; Bauman, M. Multiple Chronic Conditions in the United States; Rand Corporation: Santa Monica, CA, USA, 2017; Available online: https://www.rand.org/pubs/tools/TL221.html (accessed on 23 February 2021).
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart disease and stroke statistics—2020 update: A report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. About Chronic Diseases. 2019. Available online: https://www.cdc.gov/chronicdisease/about/index.htm (accessed on 23 February 2021).
- Centers for Medicare & Medicaid Services. National Health Expenditures Data. National Health Expenditure Fact Sheet: Historical National Health Expenditures. 2018. Available online: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet (accessed on 25 February 2021).
- American Pet Products Association. 2019–2020 National Pet Owner’s Survey; American Pet Products Association: Stamford, CT, USA, 2020. [Google Scholar]
- Headey, B. Health benefits and health cost savings due to pets: Preliminary estimates from an Australian national survey. Soc. Indic. Res. 1998, 47, 233–243. [Google Scholar] [CrossRef]
- McNicholas, J.; Gilbey, A.; Rennie, A.; Ahmedzai, S.; Dono, J.-A.; Ormerod, E. Pet ownership and human health: A brief review of evidence and issues. BMJ 2005, 331, 1252–1254. [Google Scholar] [CrossRef] [Green Version]
- Anderson, W.P.; Reid, C.M.; Jennings, G.L. Pet ownership and risk factors for cardiovascular disease. Med. J. Aust. 1992, 157, 298–301. [Google Scholar] [CrossRef]
- Wright, J.D.; Kritz-Silverstein, D.; Morton, D.J.; Wingard, D.L.; Barrett-Connor, E. Pet ownership and blood pressure in old age. Epidemiology 2007, 18, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Levine, G.N.; Allen, K.; Braun, L.T.; Christian, H.E.; Friedmann, E.; Taubert, K.A.; Thomas, S.A.; Wells, D.L.; Lange, R.A. Pet ownership and cardiovascular risk: A scientific statement from the American Heart Association. Circulation 2013, 127, 2353–2363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kramer, C.K.; Mehmood, S.; Suen, R.S. Dog ownership and survival: A systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005554. [Google Scholar] [CrossRef]
- Parslow, R.A.; Jorm, A.F. Pet ownership and risk factors for cardiovascular disease: Another look. Med. J. Aust. 2003, 179, 466–468. [Google Scholar] [CrossRef]
- Gillum, R.F.; Obisesan, T.O. Living with companion animals, physical activity and mortality in a U.S. national cohort. Int. J. Environ. Res. Public Health 2010, 7, 2452–2459. [Google Scholar] [CrossRef]
- Miyake, K.; Kito, K.; Kotemori, A.; Sasaki, K.; Yamamoto, J.; Otagiri, Y.; Nagasawa, M.; Kuze-Arata, S.; Mogi, K.; Kikusui, T.; et al. Association between pet ownership and obesity: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 3498. [Google Scholar] [CrossRef]
- Lentino, C.; Visek, A.J.; McDonnell, K.; DiPietro, L. Dog walking is associated with a favorable risk profile independent of moderate to high volume of physical activity. J. Phys. Act. Health 2012, 9, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Dembicki, D.; Anderson, J. Pet ownership may be a factor in improved health of the elderly. J. Nutr. Elder. 1996, 15, 15–31. [Google Scholar] [CrossRef] [PubMed]
- Friedmann, E.; Thomas, S.A. Pet ownership, social support, and one-year survival after acute myocardial infarction in the Cardiac Arrhythmia Suppression Trial (CAST). Am. J. Cardiol. 1995, 76, 1213–1217. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef] [Green Version]
- Chowdury, E.K.; Nelson, M.R.; Jennings, G.L.R.; Wing, L.M.H.; Reid, C.M. Pet ownership and survival in the elderly hypertensive population. J. Hyperten. 2017, 35, 769–775. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Bauman, A.E.; Sherrington, C.; McGreevy, P.D.; Edwards, K.M.; Stamatakis, E. Dog ownership and mortality in England: A pooled analysis of six population-based cohorts. Am. J. Prev. Med. 2018, 54, 289–293. [Google Scholar] [CrossRef]
- Krittanawong, C.; Kumar, A.; Wang, Z.; Jneid, H.; Virani, S.S.; Levine, G.N. Pet ownership and cardiovascular health in the U.S. general population. Am. J. Cardiol. 2020, 125, 1158–1161. [Google Scholar] [CrossRef]
- Mubanga, M.; Byberg, L.; Nowak, C.; Egenvall, A.; Magnusson, P.K.; Ingelsson, E.; Fall, T. Dog ownership and the risk of cardiovascular disease and death—A nationwide cohort study. Sci. Rep. 2017, 7, 15821. [Google Scholar] [CrossRef] [Green Version]
- Mubanga, M.; Byberg, L.; Egenvall, A.; Ingelsson, E.; Fall, T. Dog ownership and survival after a major cardiovascular event: A register-based prospective study. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005342. [Google Scholar] [CrossRef]
- Ogechi, I.; Snook, K.; Davis, B.M.; Hansen, A.R.; Liu, F.; Zhang, J. Pet ownership and the risk of dying from cardiovascular disease among adults without major chronic medical conditions. High Blood Press. Cardiovasc. Prev. 2016, 23, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Parker, G.B.; Gayed, A.; Owen, C.A.; Hyett, M.P.; Hilton, T.M.; Heruc, G. Survival following an acute coronary syndrome: A pet theory to put to the test. Acta Psychiatr. Scand. 2010, 121, 65–70. [Google Scholar] [CrossRef]
- Qureshi, A.I.; Zeeshan Memon, M.; Vazquez, G.; Suri, M.F.K. Cat ownership and the risk of fatal cardiovascular diseases. Results from the second National Health and Nutrition Examination Study Mortality Follow-up Study. J. Vasc. Interven. Neurol. 2009, 2, 132–135. [Google Scholar]
- Ružić, A.; Miletić, B.; Ružić, T.; Persić, V.; Laskarin, G. Regular dog-walking improves physical capacity in elderly patients after myocardial infarction. Coll. Antropol. 2011, 35, 73–75. [Google Scholar]
- Xie, Z.Y.; Zhao, D.; Chen, B.R.; Wang, Y.-N.; Ma, Y.; Shi, H.-J.; Yang, Y.; Wang, Z.-M.; Wang, L.-S. Association between pet ownership and coronary artery disease in a Chinese population. Medicine (Baltimore) 2017, 96, e6466. [Google Scholar] [CrossRef]
- Heuberger, R.; Wakshlag, J. Characteristics of ageing pets and their owners: Dogs v. cats. Brit. J. Nutr. 2011, 106, S150–S153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kushner, R.F.; Jackson Blatner, D.; Jewell, D.E.; Rudloff, K. The PPET Study: People and pets exercising together. Obesity 2006, 14, 1762–1770. [Google Scholar] [CrossRef] [Green Version]
- Niese, J.R.; Mepham, T.; Nielen, M.; Monninkhof, E.M.; Kroese, F.M.; de Ridder, D.T.D.; Corbee, R.J. Evaluating the potential benefit of a combined weight loss program in dogs and their owners. Front. Vet. Sci. 2021, 8, 653920. [Google Scholar] [CrossRef] [PubMed]
- Stephens, M.B.; Wilson, C.C.; Goodie, J.L.; Netting, F.E.; Olsen, C.H.; Byers, C.G. Health perceptions and levels of attachment: Owners and pets exercising together. J. Am. Board Fam. Med. 2012, 25, 923–926. [Google Scholar] [CrossRef] [Green Version]
- Chur-Hansen, A.; Stern, C.; Winefield, H. Gaps in the evidence about companion animals and human health: Some suggestions for progress. Int. J. Evid. Based Healthc. 2010, 8, 140–146. [Google Scholar] [CrossRef] [PubMed]
- El-Qushayri, A.E.; Kamel, A.M.A.; Faraj, H.A.; Vuong, N.L.; Diab, O.M.; Istanbuly, S.; Elshafei, T.A.; Makram, O.M.; Sattar, Z.; Istanbuly, O.; et al. Association between pet ownership and cardiovascular risks and mortality: A systematic review and meta-analysis. Cardiovasc. Med. 2020, 21, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Yeh, T.L.; Lei, W.T.; Liu, S.J.; Chien, K.-L. A modest protective association between pet ownership and cardiovascular diseases: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0216231. [Google Scholar] [CrossRef] [PubMed]
- Deem, S.L.; Lane-deGraaf, K.E.; Rayhel, E.A. Introduction to One Health: An Interdisciplinary Approach to Planetary Health; ProQuest Ebook Central; John Wiley & Sons: Hoboken, NJ, USA, 2019; Available online: https://ebookcentral-proquest-com.proxy.lib.utk.edu/lib/utk/detail.action?docID=5572466 (accessed on 1 April 2021).
| Study | Study Sample | Pet Ownership | Outcome Measure(s) | Reported Effect |
|---|---|---|---|---|
| CVD | ||||
| Chowdhury et al., 2017 [20] | older adults (65–84 years old) n = 4039 (never owners = 549, current owners = 1456, previous owners = 2034) | cat, dog | all-cause mortality, CVD 1 mortality | positive |
| Ding et al., 2018 [21] | adults (≥16 years old) n = 59,352 (dog owners = 17,071, non-owners = 42,281) | dog | all-cause mortality, CVD mortality | no effect |
| Krittanawong et al., 2020 [22] | adults n = 10,905 (dog owners = 4577, cat owners = 6328) | cat, dog | CAD 2, heart failure, DM 3, stroke, systemic hypertension | mixed |
| Mubanga et al., 2017 [23] | adults (40–80 years old) n = 3432,153 | dog | all-cause mortality, CVD mortality, acute MI 4 | positive |
| Mubanga et al., 2019 [24] | adults (40–85 years old) cute MI: n = 181,696 ischemic stroke: n = 154,617 | dog | acute MI, ischemic stroke | positive |
| Ogechi et al., 2016 [25] | adults (≥16 years old) n = 3964 | cat, dog | CVD mortality, stroke mortality | positive |
| Parker et al., 2010 [26] | patients hospitalized with ACS 5 n = 424 (12 withdrew/unable to contact) | cat, dog | ACS readmission, CVD mortality | negative |
| Qureshi et al., 2009 [27] | adults (18–74 years old) n = 4435 | cat, dog | MI mortality, CVD mortality | mixed |
| Ruzic et al., 2011 [28] | older adults n = 59 males (owners = 29, non-owners = 30) | dog | physical capacity maximal workload, heart rate, BP 6 | positive |
| Xie et al., 2017 [29] | adults (30–89 years old) n = 561 | cat, dog | CAD | positive |
| Obesity | ||||
| Heuberger and Wakshlag, 2011 [30] | adults (≥17 years old) n = 473 | cat, dog | BMI, dietary intake | negative |
| Kushner et al., 2006 [31] | adults (21–65 years old) n = 92 | dog | BMI 7, PA 8 | no effect |
| Niese et al., 2021 [32] | adults with BMI ≥ 25 n = 60 (owner-dog: n = 29, owner only: n = 31) | dog | weight loss | no effect |
| Stephens et al., 2012 [33] | adults (≥18 years old) n = 75 | dog | BMI, PA, stress, social support | negative |
| Study | Degree of Pertinence (Fitness) | Quality of Study Outcomes | Instrument Validity | Generalizability | Summary Score (Range: 4–12) |
|---|---|---|---|---|---|
| Cardiovascular Disease | |||||
| Chowdhury et al. 2017 [20] | 2 | 3 | 1 | 2 | 8 |
| Ding et al. 2018 [21] | 3 | 3 | 2 | 3 | 11 |
| Krittanawong et al. 2020 [22] | 3 | 3 | 3 | 3 | 12 |
| Mubanga et al. 2017 [23] | 3 | 3 | 3 | 3 | 12 |
| Mubanga et al. 2019 [24] | 3 | 3 | 3 | 3 | 12 |
| Ogechi et al. 2016 [25] | 3 | 3 | 2 | 3 | 11 |
| Parker et al. 2010 [26] | 3 | 3 | 3 | 2 | 11 |
| Qureshi et al. 2009 [27] | 3 | 3 | 3 | 2 | 11 |
| Ruzic et al. 2011 [28] | 1 | 1 | 1 | 1 | 4 |
| Xie et al. 2017 [29] | 3 | 3 | 1 | 1 | 8 |
| Obesity | |||||
| Heuberger et al. 2011 [30] | 1 | 1 | 1 | 1 | 4 |
| Kushner et al. 2006 [31] | 3 | 3 | 2 | 1 | 9 |
| Niese et al. 2021 [32] | 2 | 3 | 2 | 1 | 8 |
| Stephens et al. 2012 [33] | 2 | 3 | 2 | 1 | 8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barroso, C.S.; Brown, K.C.; Laubach, D.; Souza, M.; Daugherty, L.M.; Dixson, M. Cat and/or Dog Ownership, Cardiovascular Disease, and Obesity: A Systematic Review. Vet. Sci. 2021, 8, 333. https://doi.org/10.3390/vetsci8120333
Barroso CS, Brown KC, Laubach D, Souza M, Daugherty LM, Dixson M. Cat and/or Dog Ownership, Cardiovascular Disease, and Obesity: A Systematic Review. Veterinary Sciences. 2021; 8(12):333. https://doi.org/10.3390/vetsci8120333
Chicago/Turabian StyleBarroso, Cristina S., Kathleen C. Brown, David Laubach, Marcy Souza, Linda M. Daugherty, and Melanie Dixson. 2021. "Cat and/or Dog Ownership, Cardiovascular Disease, and Obesity: A Systematic Review" Veterinary Sciences 8, no. 12: 333. https://doi.org/10.3390/vetsci8120333
APA StyleBarroso, C. S., Brown, K. C., Laubach, D., Souza, M., Daugherty, L. M., & Dixson, M. (2021). Cat and/or Dog Ownership, Cardiovascular Disease, and Obesity: A Systematic Review. Veterinary Sciences, 8(12), 333. https://doi.org/10.3390/vetsci8120333








