Immunohistochemical Studies of Cytokeratins and Differentiation Markers in Bovine Ocular Squamous Cell Carcinoma
Abstract
1. Introduction
2. Materials and Methods
2.1. Samples
2.2. Histopathology
2.3. Immunohistochemistry (IHC)
2.4. Statistical Analysis
2.5. Ethics
3. Results
3.1. Clinical Data
3.2. Histopathological Diagnosis
3.3. Immunohistochemistry
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fornazari, G.A.; Kravetz, J. Ocular squamous cell carcinoma in Holstein cows from the South of Brazil. Vet. World 2017, 10, 1413–1420. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hamir, A.N.; Parry, O.B. An abattoir study of bovine neoplasms with particular reference to ocular squamous cell carcinoma in Canada. Vet. Rec. 1980, 106, 551–553. [Google Scholar] [CrossRef]
- Dennis, M.W.; Lueker, D.C. Host response to bovine ocular squamous cell carcinoma. Am. J. Vet. Res. 1985, 46, 1975–1979. [Google Scholar] [PubMed]
- Heeney, J.L.; Valli, V.E.O. Bovine ocular squamous cell carcinoma: An epidemiological perspective. Can. J. Comp. Med. 1985, 49, 21–26. [Google Scholar] [PubMed]
- Stewart, R.J.; Masztalerz, A. Local interleukin-2 and interleukin-12 therapy of bovine ocular squamous cell carcinomas. Vet. Immunol. Immunopathol. 2005, 106, 277–284. [Google Scholar] [CrossRef]
- Stewart, R.J.; Hill, F.W. Treatment of ocular squamous cell carcinomas in cattle with interleukin-2. Vet. Rec. 2006, 159, 668–672. [Google Scholar] [CrossRef]
- Wilcock, B.P. The eye and ear. In Pathology of Domestic Animals, 7th ed.; Jubb, K.V.F., Kennedy, P.C., Eds.; Academic Press, Inc.: San Diego, CA, USA, 2007; Volume 1, pp. 534–536. [Google Scholar]
- Tsujita, H.; Plummer, C.E. Bovine Ocular Squamous Cell Carcinoma. Vet. Clin. N. Am. Food Anim. Pract. 2010, 26, 511–529. [Google Scholar] [CrossRef]
- Pinto, C.; Medeiros, F. Cattle neoplasias in S. Miguel–Açores. A retrospective study and actual situation. Vet. Téc. 1996, 6, 30–37. [Google Scholar]
- Pinto, C.; Medeiros, F. Cattle neoplasias in S. Miguel–Açores. Anatomohistopathological study. Vet. Téc. 2001, 11, 44–48. [Google Scholar]
- Carvalho, T.; Vala, H. Immunohistochemical Studies of Epithelial Cell Proliferation and p53 Mutation in Bovine Ocular Squamous Cell Carcinoma. Vet. Pathol. 2005, 42, 66–73. [Google Scholar] [CrossRef]
- Rice, R.H.; Qin, Q. Keratinocyte differentiation markers: Involucrin, transglutaminase, and toxicity. J. Natl. Cancer Inst. Monogr. 1992, 13, 87–91. [Google Scholar]
- Livasy, C.A.; Karaca, G. Phenotipic evaluation of the basal-like subtype of invasive breast carcinoma. Mod. Pathol. 2006, 19, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Prince, M.E.; Sivanandan, R. Identification of a subpopulation of cells with cancer stem cell properties in head and neck squamous cell carcinoma. Proc. Natl. Acad. Sci. USA 2007, 16, 973–978. [Google Scholar] [CrossRef] [PubMed]
- Fillies, T.; Jogschies, M. Cytokeratin alteration in oral leukoplakia and oral squamous cell carcinoma. Oncol. Rep. 2007, 18, 639–643. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhong, L.P.; Chen, W.T. Increased CK19 expression correlated with pathologic differentiation grade and prognosis in oral squamous cell carcinoma patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 104, 377–384. [Google Scholar] [CrossRef]
- Hohl, D. Cornified cell envelope. Dermatologica 1990, 180, 201–211. [Google Scholar] [CrossRef]
- Steven, A.C.; Steinert, P.M. Protein composition of cornified cell envelopes of epidermal keratinocytes. J. Cell Sci. 1994, 107, 693–700. [Google Scholar]
- Caldwell, C.J.; Hobbs, C. The relationship of Ki67 and involucrin expression in proliferative, pre-neoplastic and neoplastic skin. Clin. Exp. Dermatol. 1997, 22, 11–16. [Google Scholar] [CrossRef]
- Steinert, P.M.; Marekov, L.N. Initiation of assembly of the cell envelope barrier structure of stratified squamous epithelia. Mol. Biol. Cell 1999, 10, 4247–4261. [Google Scholar] [CrossRef]
- Park, G.T.; Kim, H.Y. Autocrine extracellular signal-regulated kinase activation in normal human keratinocytes is not interrupted by calcium triggering and is involved in the control of the cell cycle at the early stage of calcium-induced differentiation. J. Korean Med. Sci. 2007, 22, 290–297. [Google Scholar] [CrossRef][Green Version]
- Ivanova, P.; Atanasova, G. Knockdown of PKD1 in normal human epidermal keratinocytes increases mRNA expression of keratin 10 and involucrin: Early markers of keratinocyte differenciation. Arch. Dermatol. Res. 2008, 300, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.E.; Leung, D.Y.M. Loricrin and involucrin expression is down-regulated by Th2 cytokines through STAT-6. Clin. Immunol. 2008, 126, 332–337. [Google Scholar] [CrossRef] [PubMed]
- Murphy, G.F.; Flynn, T.C. Involucrin expression in normal and neoplastic human skin: A marker for keratinocyte differentiation. J. Investig. Dermatol. 1984, 82, 453–457. [Google Scholar] [CrossRef]
- Smoller, B.R.; Kwan, T.H. Keratoacanthoma and squamous cell carcinoma of the skin: Immunohistochemical localization of involucrin and keratin proteins. J. Am. Acad. Dermatol. 1986, 14, 226–234. [Google Scholar] [CrossRef]
- Markova, N.G.; Marekov, L.N. Profilaggrin is a major epidermal calcium-Binding protein. Mol. Cell. Biol. 1993, 13, 613–625. [Google Scholar] [CrossRef][Green Version]
- Resing, K.A.; Johnson, R.S. Mass spectrometric analysis of 21 phosphorylation sites in the internal repeat of rat profilaggrin, precursor of an intermediate filament associated protein. Biochemistry 1995, 34, 9477–9487. [Google Scholar] [CrossRef]
- King, K.E.; Ponnamperuma, R.M. Unique domain functions of p63 isotypes that differentially regulate distinct aspects of epidermal homeostasis. Carcinogenesis 2006, 27, 53–63. [Google Scholar] [CrossRef]
- Vigneswaran, N.; Peters, K.P. Comparison of cytokeratin, filaggrin and involucrin profiles in oral leukoplakias and squamous carcinomas. J. Oral Pathol. Med. 1989, 18, 377–390. [Google Scholar] [CrossRef]
- Nozoe, T.; Oyama. T. Significance of immunohistochemical expression of p27 and involucrin as the marker of cellular differentiation of squamous cell carcinoma of the esophagus. Oncology 2006, 71, 402–410. [Google Scholar] [CrossRef]
- Kurokawa, I.; Nishimura, K. Cytokeratin expression in squamous cell carcinoma arising from hidradenitis suppurativa (acne inversa). J. Cutan. Pathol. 2007, 34, 675–678. [Google Scholar] [CrossRef]
- Karatzanis, A.D.; Fragkiadakis, G.M. Basaloid squamous cell carcinoma of the soft palate. Case report. Auris Nasus Larynx 2008, 35, 592–596. [Google Scholar] [CrossRef]
- Mikaelian, I.; Wong, V. Follicular stem cell carcinoma: Histologic, immunohistochemical, ultrastructural, and clinical characterization in 30 days. Vet. Pathol. 2004, 41, 302. [Google Scholar] [CrossRef]
- Martín de Las Mulas, J.; Molina, A.M. Spontaneous trichoepithelioma in a laboratory mouse: Gross, microscopic and immunohistochemical findings. Lab. Anim. 2007, 41, 136–140. [Google Scholar] [PubMed]
- Kato, K.; Uchida, K. Immunohistochemical studies on cytokeratin 8 and 18 expressions in canine cutaneous adnexus and their tumors. Vet. Med. Sci. 2007, 69, 233–239. [Google Scholar] [CrossRef]
- Perez, J.; Mendez, A. Ovine squamous cell carcinoma: Immunocharacterisation of neoplastic cells and peritumoural cellular infiltrate. Res. Vet. Sci. 1997, 63, 43–47. [Google Scholar] [CrossRef]
- Neves Ada, C.; Mesquita, R.A. Comparison between immunohistochemical expression of cyclin D1 and p21 and histological malignancy graduation of oral squamous cell carcinomas. Braz. Dent. J. 2004, 15, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Goldschmidt, M.H.; Dunstan, R.W. Histological Classification of Epithelial and Melanocytic Tumors of the Skin of Domestic Animals, 2nd ed.; World Health Organization: Geneva, Switzerland, 1998; pp. 20–21. [Google Scholar]
- Goldschmidt, M.H.; Hendrick, M.S. Tumors of the skin and soft tissues. In Tumors in Domestic Animals, 4th ed.; Meuten, D.J., Ed.; Iowa State Press: Iowa, IA, USA, 2002; pp. 51–52. [Google Scholar]
- Sözmen, M.; Devrim, A.K. Significance of Angiogenic Growth Factors in Bovine Ocular Squamous Cell Carcinoma. J. Comp. Pathol. 2019, 170, 60–69. [Google Scholar] [CrossRef]
- Mendez, A.; Perez, J. Clinicopathological study of an outbreak of squamous cell carcinoma in sheep. Vet. Rec. 1997, 141, 597–600. [Google Scholar]
- Young, A.R. Cumulative effects of ultraviolet radiation on the skin: Cancer and photoaging. Semin. Dermatol. 1990, 9, 25–31. [Google Scholar]
- Gross, T.L.; Ihrke, P.J. Veterinary Dermatopathology, 1st ed.; Mosby–Year Book, Inc.: Missouri, MS, USA, 1992; pp. 336–340. [Google Scholar]
- Garma-Aviña, A. The cytology of squamous cell carcinomas in domestic animals. J. Vet. Diagn. Investig. 1994, 6, 238–246. [Google Scholar]
- Gin, P.E.; Mansell, J.E.K.L. Skin and appendages. In Pathology of Domestic Animals, 5th ed.; Jubb, K.V.F., Kennedy, P.C., Eds.; Academic Press, Inc.: San Diego, CA, USA, 2007; Volume 1, pp. 751–753. [Google Scholar]
- Kartasova, T.; Roop, D.R. Mouse differentiation-specific keratins 1 and 10 require a preexisting keratin scaffold to form a filament network. J. Cell Biol. 1993, 120, 1251–1261. [Google Scholar] [PubMed]
- Smack, D.P.; Korge, B.P. Keratin and keratinisation. J. Am. Acad. Dermatol. 1994, 30, 85–102. [Google Scholar] [CrossRef]
- Watanabe, S.; Ichikawa, E. Changes of cytokeratin and involucrin expression in squamous cell carcinomas of the skin during progression to malignancy. Br. J. Dermatol. 1995, 132, 730–739. [Google Scholar] [PubMed]
- Moll, R.; Schiller, D.L. The catalog of human cytokeratins: Patterns of expression in normal epithelia, tumors and cultured cells. Cell 1982, 31, 11–24. [Google Scholar] [CrossRef]
- Ramírez, A.; Vidal, M. Analysis of sequences controlling tissue-specific and hyperproliferation-related keratin 6 gene expression in transgenic mice. DNA Cell Boil. 1998, 17, 177–185. [Google Scholar] [CrossRef]
- Fillies, T.; Werkmeister, R. Cytokeratin 8/18 expression indicates a poor prognosis in squamous cell carcinoma of the oral cavity. BMC Cancer 2006, 6, 10–18. [Google Scholar] [CrossRef]
- Rabban, J.T.; Koerner, F.C. Solid papillary ductal carcinoma in situ versus usual ductal hyperplasia in the breast: A potentially difficult distinction resolved by cytokeratin 5/6. Hum. Pathol. 2006, 37, 787–793. [Google Scholar]
- Gusterson, B.A.; Ross, D.T. Basal cytokeratins and their relationship to the cellular origin and functional classification of breast cancer. Breast Cancer Res. 2005, 7, 143–148. [Google Scholar] [CrossRef]
- Itoiz, M.E.; Conti, C.J. Immunodetection of involucrin in lesions of the oral mucosa. J. Oral Pathol. 1986, 15, 205–208. [Google Scholar] [CrossRef]
- Li, E.R.; Owens, D.M. Expression of involucrin in normal, hyperproliferative and neoplastic mouse keratinocytes. Exp. Dermatol. 2000, 9, 431–438. [Google Scholar]
- Klein-Szanto, A.J.P.; Walts, A.E. Involucrin [letter]. Arch. Pathol. Lab. Med. 1988, 112, 578. [Google Scholar]
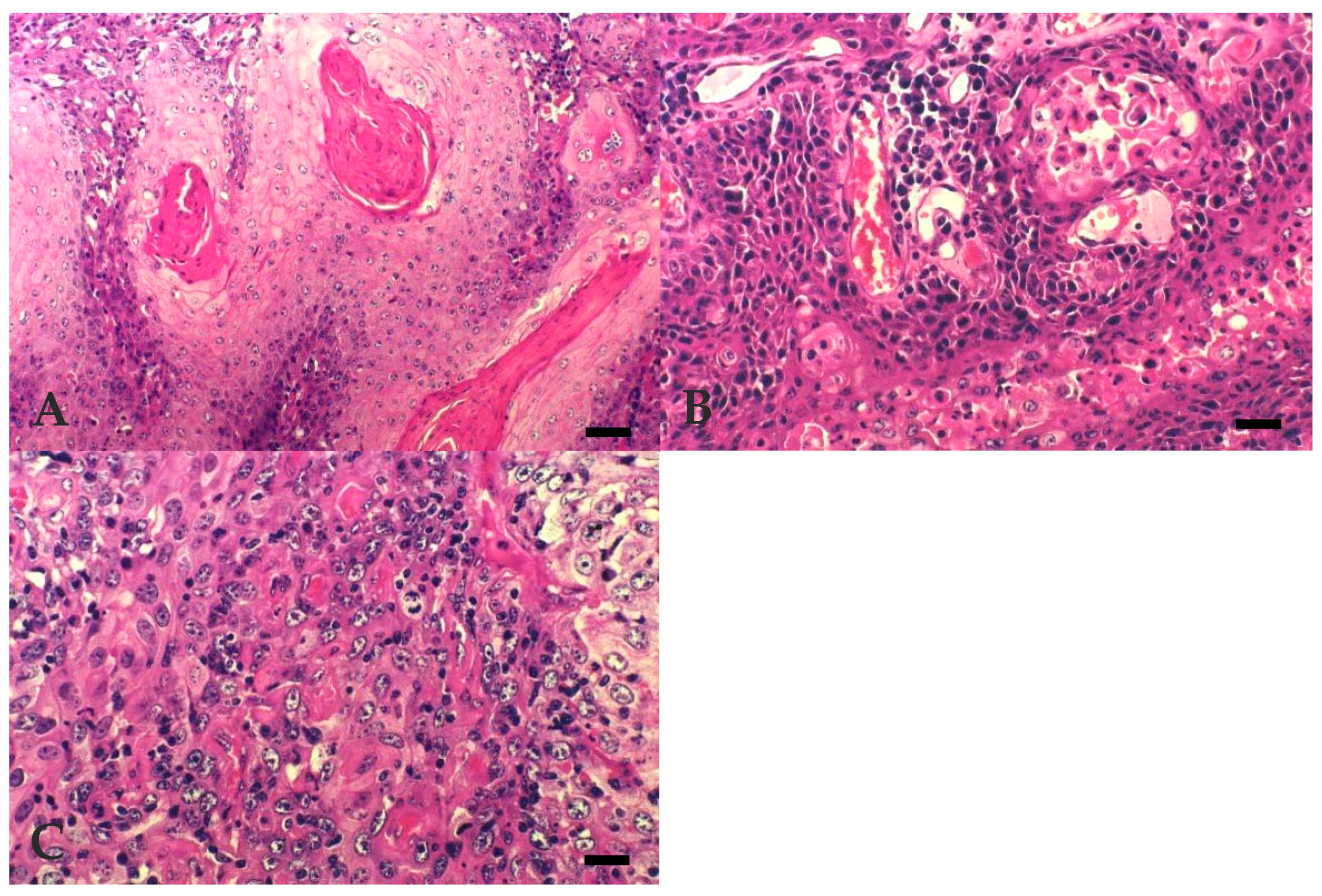
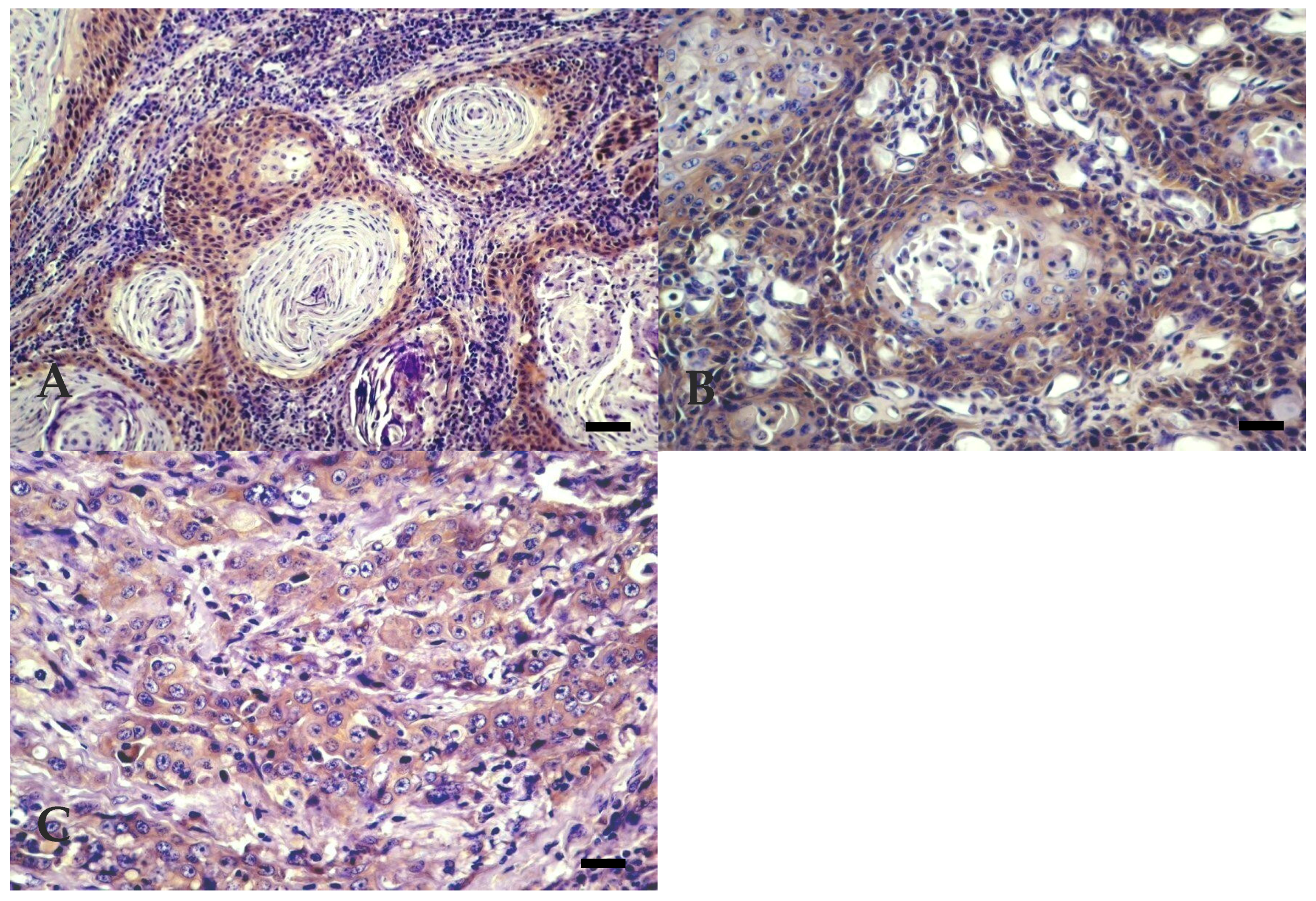
| Degree of Differentiation | |||
| Keratinisation Degree | Pattern | Cellular Phenotype | |
| Well Differentiated | Numerous large keratin pearls | Large islands, trabeculae or cords formation, with central squamous differentiation | Small basal-like cells at the periphery and well-differentiated keratinocytes, with homogenous eosinophilic cytoplasm and clear intercellular bridges in the central areas |
| Moderately Differentiated | Small to medium sized keratin pearls | Smaller islands and squamous differentiation, acantolytic cysts | Increased number of poorly differentiated cells |
| Poorly Differentiated | Individual cell keratinisation | Few small sized islands, poor cellular differentiation | Predominance of areas with more pleomorphic and atypical cells |
| Degree of Invasiveness | |||
| Non-Invasive | Moderately Invasive | Very Invasive | |
| Minimal signs of invasion of the surrounding tissues | Small independent islands of neoplastic tissue surrounding the main tumour | Invasion of the deepest skin layers, far from the main tumour | |
| Antibody | Clone | Pre-Treatment | Dilution | Incubation Time |
|---|---|---|---|---|
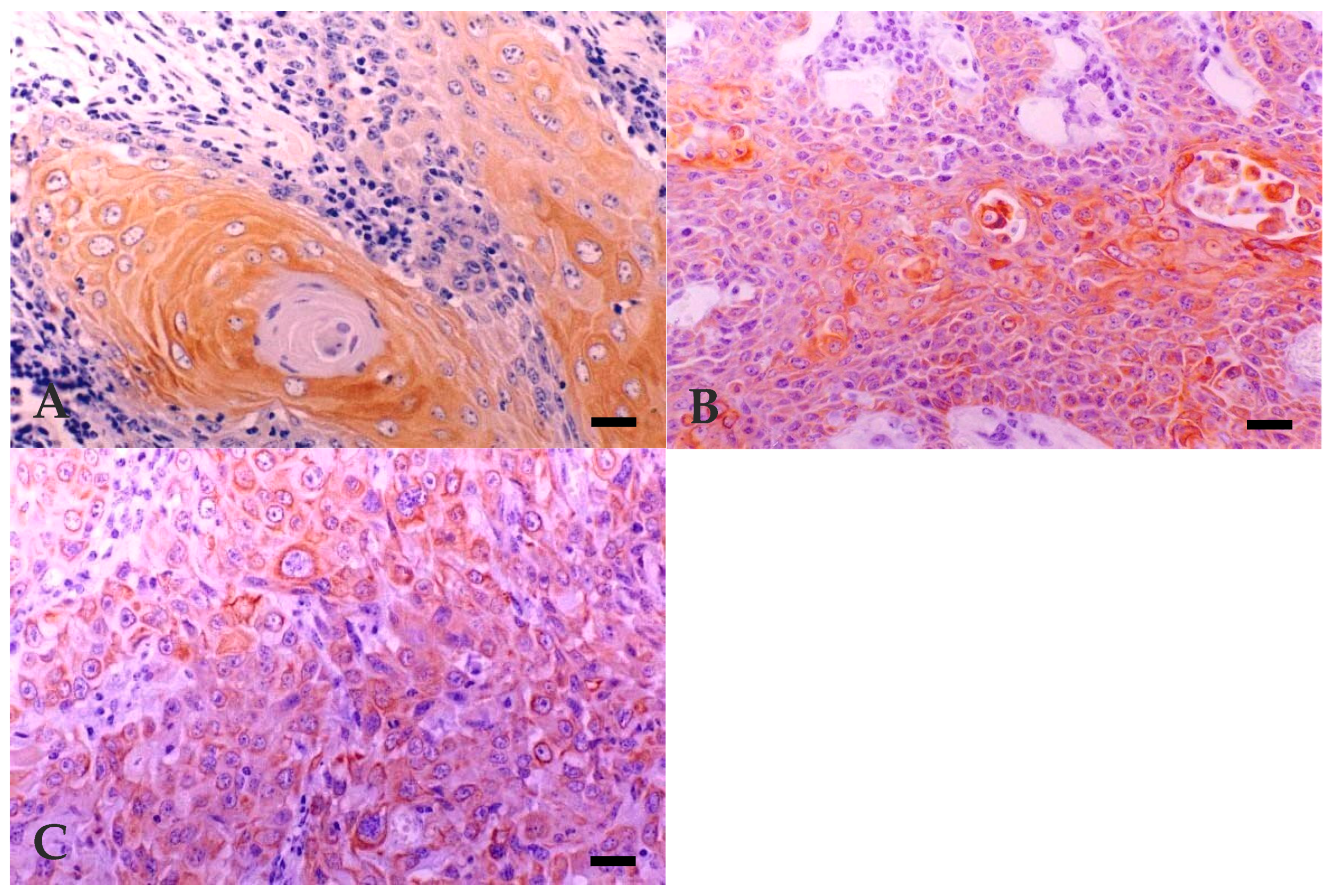
| Cytokeratins 5, 6, 8, 17, and 19 | MNF116 (DAKO) | Tripsin to 0.1% 20′, 37 °C | 1:50 | Overnight Room temperature |
| Cytokeratins 5, 6, and 18 | LP34 (DAKO) | 1:100 | ||
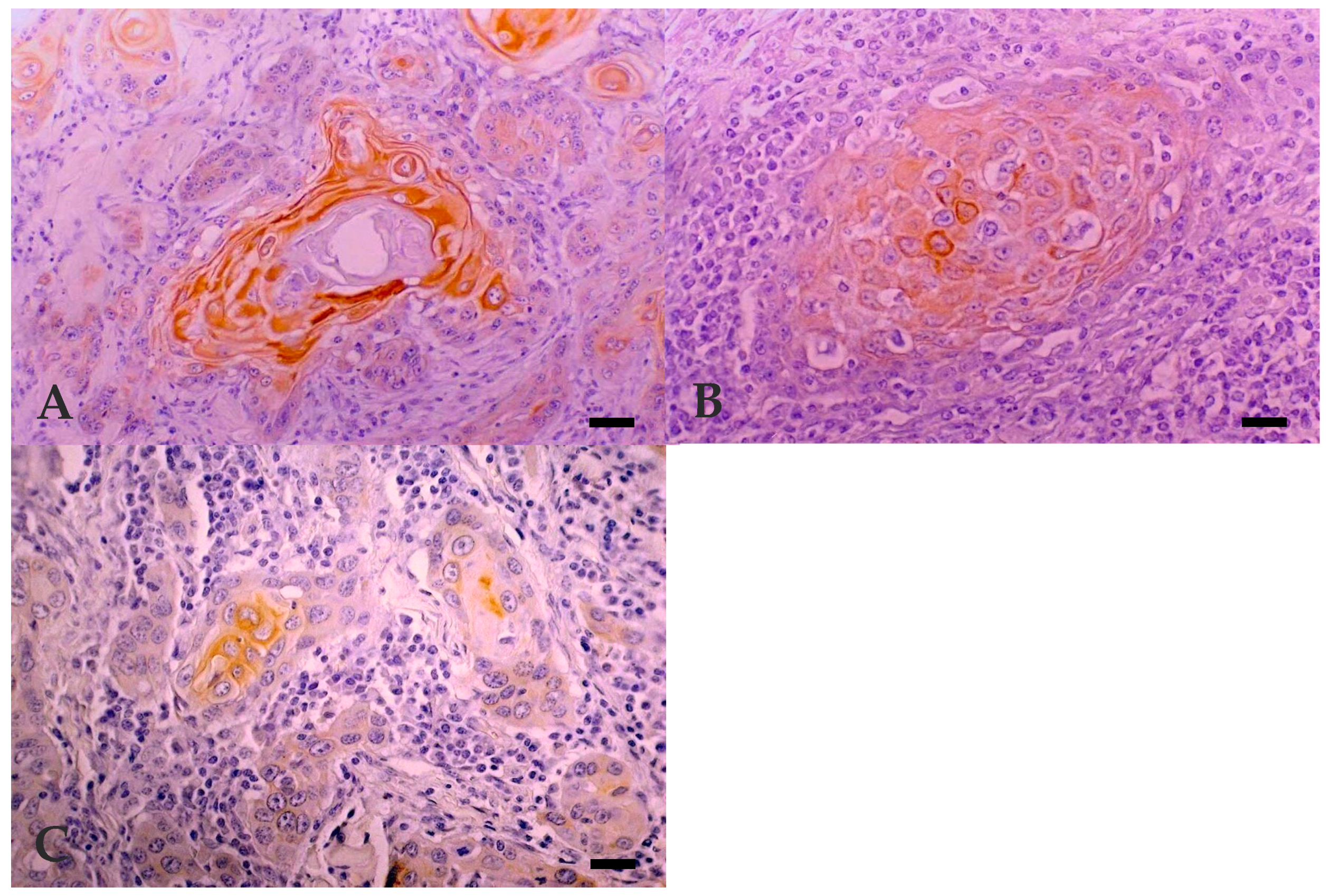
| Profilaggrin | Policlonal (ZYMED) | 1:150 | ||
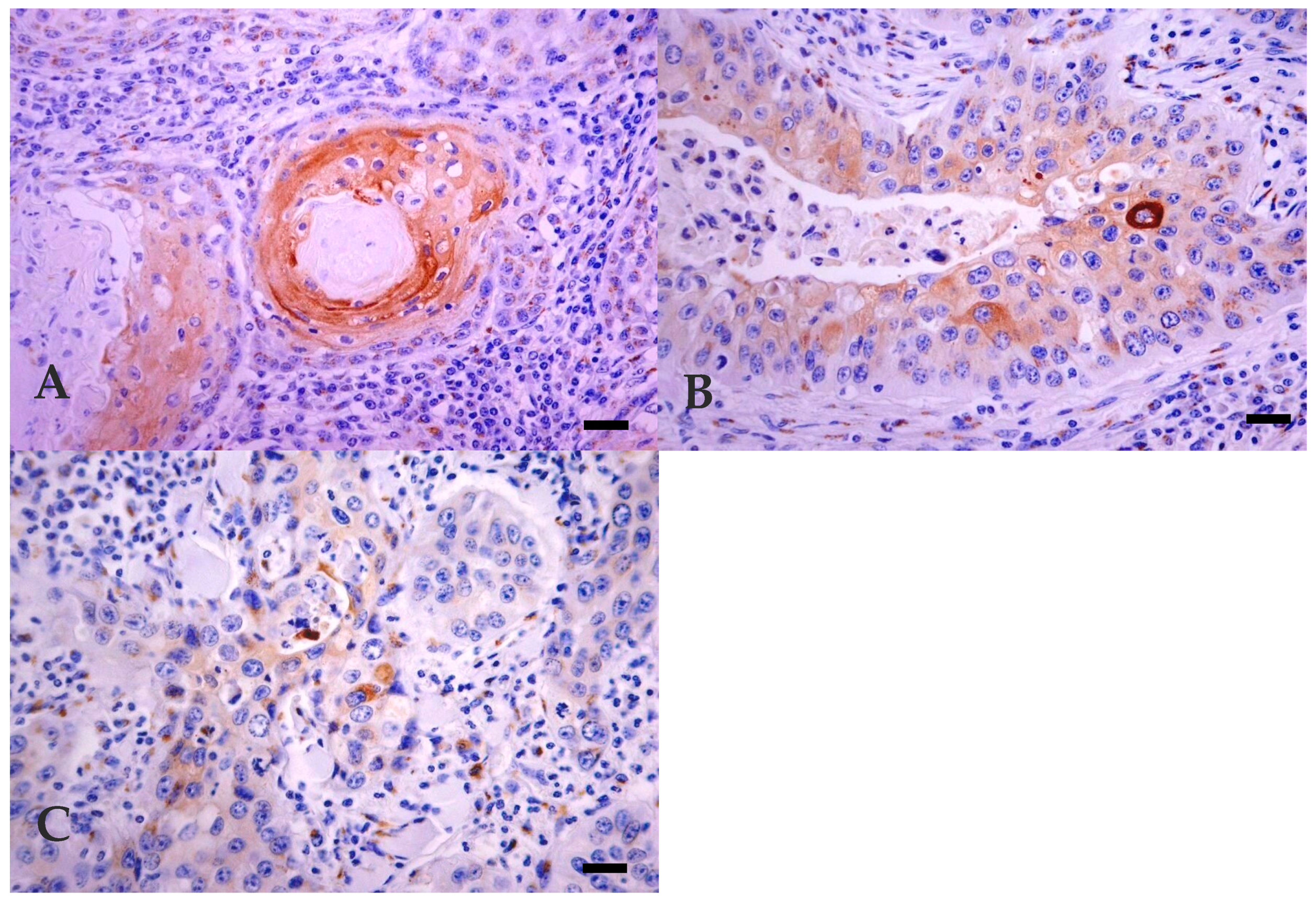
| Involucrin | SY5 (NOVOCASTRA) | 10′, 98 °C in 10 mM citrate buffer (pH 6.0) | 1:20 |
| Animal * | Age (Year) | Localization of Tumour | Histological Classification ** | Invasiveness ‡ | Mitosis § | Immunohistochemistry † | |||
|---|---|---|---|---|---|---|---|---|---|
| MNF 116 | LP 34 | Involucrin | Filaggrin | ||||||
| 1 | 6 | Third eyelid | WD | MI | 0–20 | +++ | +++ | + | +++ |
| 2 | 5 | Eyelid | WD | MI | 0-20 | +++ | ++ | + | ++++ |
| 3 | 8 | Third eyelid | WD | NI | >60 | ++++ | + | + | ++++ |
| 4 | 4 | Eyelid | WD | NI | 30–60 | ++++ | ++ | + | ++++ |
| 5 | 10 | Third eyelid | WD | VI | 0–20 | ++++ | ++++ | + | ++ |
| 6 | 10 | Whole ocular region | WD | VI | 0–20 | +++ | − | + | − |
| 7 | 8 | Eyelid | WD | VI | 0–20 | ++++ | ++ | + | + |
| 8 | 8 | Eyelid | WD | NI | 0–20 | ++++ | + | + | + |
| 9 | 7 | Third eyelid | WD | VI | 0–20 | ++++ | +++ | + | +++ |
| 10 | 9 | Third eyelid | MD | MI | >60 | ++++ | + | + | ++++ |
| 11 | 8 | Whole ocular region | MD | VI | 0–20 | ++++ | ++++ | + | + |
| 12 | 8 | Eyelid | MD | VI | 0–20 | ++++ | − | + | − |
| 13 | 4 | Third eyelid | MD | VI | 0–20 | ++++ | +++ | + | − |
| 14 | 9 | Eyelid | MD | VI | 0–20 | ++++ | + | + | − |
| 15 | 6 | Third eyelid | PD | VI | 30–60 | ++++ | − | + | ++++ |
| 16 | 7 | Whole ocular region | PD | VI | 30–60 | ++++ | + | + | + |
| 17 | Eyelid | PD | VI | 0–20 | ++++ | + | − | ++ | |
| 18 | 8 | Eyelid | PD | VI | >60 | ++++ | + | + | + |
| 19 | 10 | Third eyelid | PD | VI | 0–20 | ++++ | ++ | + | − |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vala, H.; Carvalho, T.; Pinto, C.; Pereira, M.A.; Mesquita, J.R.; Peleteiro, M.C.; Ferrer, L.; Fondevila, D. Immunohistochemical Studies of Cytokeratins and Differentiation Markers in Bovine Ocular Squamous Cell Carcinoma. Vet. Sci. 2020, 7, 70. https://doi.org/10.3390/vetsci7020070
Vala H, Carvalho T, Pinto C, Pereira MA, Mesquita JR, Peleteiro MC, Ferrer L, Fondevila D. Immunohistochemical Studies of Cytokeratins and Differentiation Markers in Bovine Ocular Squamous Cell Carcinoma. Veterinary Sciences. 2020; 7(2):70. https://doi.org/10.3390/vetsci7020070
Chicago/Turabian StyleVala, Helena, Tânia Carvalho, Carlos Pinto, Maria A. Pereira, João R. Mesquita, Maria C. Peleteiro, Lluís Ferrer, and Dolores Fondevila. 2020. "Immunohistochemical Studies of Cytokeratins and Differentiation Markers in Bovine Ocular Squamous Cell Carcinoma" Veterinary Sciences 7, no. 2: 70. https://doi.org/10.3390/vetsci7020070
APA StyleVala, H., Carvalho, T., Pinto, C., Pereira, M. A., Mesquita, J. R., Peleteiro, M. C., Ferrer, L., & Fondevila, D. (2020). Immunohistochemical Studies of Cytokeratins and Differentiation Markers in Bovine Ocular Squamous Cell Carcinoma. Veterinary Sciences, 7(2), 70. https://doi.org/10.3390/vetsci7020070






