A Comparative Pharmacokinetic Analysis of Oral and Subcutaneous Meloxicam Administered to Postpartum Dairy Cows
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Study Herd and Treatment Protocol
2.3. Laboratory Analysis for Meloxicam Quantitation in Plasma
2.4. Data Collection and Analysis
3. Results and Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Von Keyserlingk, M.; Martin, N.; Kebreab, E.; Knowlton, K.; Grant, R.; Stephenson, M.; Sniffen, C.; Harner, J.; Wright, A.; Smith, S. Invited review: Sustainability of the US dairy industry. J. Dairy Sci. 2013, 96, 5405–5425. [Google Scholar] [CrossRef]
- Barkema, H.; Von Keyserlingk, M.; Kastelic, J.; Lam, T.; Luby, C.; Roy, J.-P.; Leblanc, S.; Keefe, G.; Kelton, D.; Barkema, H. Invited review: Changes in the dairy industry affecting dairy cattle health and welfare. J. Dairy Sci. 2015, 98, 7426–7445. [Google Scholar] [CrossRef] [PubMed]
- Davies, N.M.; Skjodt, N.M. Clinical Pharmacokintics of Meloxicam: A cyclo-oxygenase-2 preferential nonsteroidal anti-inflammatory drug. Clin. Pharmacokinet. 1999, 36, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Olson, M.E.; Ralston, B.; Burwash, L.; Matheson-Bird, H.; Allan, N.D. Efficacy of oral meloxicam suspension for prevention of pain and inflammation following band and surgical castration in calves. BMC Vet. Res. 2016, 12, 279. [Google Scholar] [CrossRef] [PubMed]
- Heinrich, A.; Duffield, T.; Lissemore, K.; Millman, S.; Millman, S. The effect of meloxicam on behavior and pain sensitivity of dairy calves following cautery dehorning with a local anesthetic. J. Dairy Sci. 2010, 93, 2450–2457. [Google Scholar] [CrossRef]
- Allen, K.; Coetzee, J.; Edwards-Callaway, L.; Glynn, H.; Dockweiler, J.; KuKanich, B.; Lin, H.; Wang, C.; Fraccaro, E.; Jones, M.; et al. The effect of timing of oral meloxicam administration on physiological responses in calves after cautery dehorning with local anesthesia. J. Dairy Sci. 2013, 96, 5194–5205. [Google Scholar] [CrossRef]
- Newby, N.C.; Tucker, C.B.; Pearl, D.L.; Leblanc, S.J.; Leslie, K.E.; Von Keyserlingk, M.A.; Duffield, T.F. Short communication: A comparison of 2 nonsteroidal antiinflammatory drugs following the first stage of a 2-stage fistulation surgery in dry dairy cows. J. Dairy Sci. 2013, 96, 6514–6519. [Google Scholar] [CrossRef]
- Fitzpatrick, C.; Chapinal, N.; Petersson-Wolfe, C.; Devries, T.; Kelton, D.; Duffield, T.; Leslie, K. The effect of meloxicam on pain sensitivity, rumination time, and clinical signs in dairy cows with endotoxin-induced clinical mastitis. J. Dairy Sci. 2013, 96, 2847–2856. [Google Scholar] [CrossRef]
- Newby, N.C.; Pearl, D.L.; Leblanc, S.J.; Leslie, K.E.; Von Keyserlingk, M.A.; Duffield, T.F. Effects of meloxicam on milk production, behavior, and feed intake in dairy cows following assisted calving. J. Dairy Sci. 2013, 96, 3682–3688. [Google Scholar] [CrossRef]
- Swartz, T.; Schramm, H.; Bewley, J.; Wood, C.; Leslie, K.; Petersson-Wolfe, C. Meloxicam administration either prior to or after parturition: Effects on behavior, health, and production in dairy cows. J. Dairy Sci. 2018, 101, 10151–10167. [Google Scholar] [CrossRef]
- Todd, C.G.; Millman, S.T.; McKnight, D.R.; Duffield, T.F.; Leslie, K.E. Nonsteroidal anti-inflammatory drug therapy for neonatal calf diarrhea complex: Effects on calf performance. J. Anim. Sci. 2010, 88, 2019–2028. [Google Scholar] [CrossRef]
- Coetzee, J.F.; KuKanich, B.; Mosher, R.; Allen, P.S. Pharmacokinetics of intravenous and oral meloxicam in ruminant calves. Vet. Ther. Res. Appl. Vet. Med. 2009, 10, E1–E8. [Google Scholar]
- Mosher, R.A.; Coetzee, J.F.; Cull, C.A.; Gehring, R.; Kukanich, B. Pharmacokinetics of oral meloxicam in ruminant and preruminant calves. J. Vet. Pharmacol. Ther. 2012, 35, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Coetzee, J.F.; Mosher, R.A.; Griffith, G.R.; Gehring, R.; Anderson, D.E.; KuKanich, B.; Miesner, M. Pharmacokinetics and tissue disposition of meloxicam in beef calves after repeated oral administration. J. Vet. Pharmacol. Ther. 2015, 38, 556–562. [Google Scholar] [CrossRef]
- Gorden, P.J.; Burchard, M.; Ydstie, J.A.; Kleinhenz, M.D.; Wulf, L.W.; Rajewski, S.J.; Wang, C.; Gehring, R.; Mochel, J.P.; Coetzee, J.F. Comparison of milk and plasma pharmacokinetics of meloxicam in postpartum versus mid-lactation Holstein cows. J. Vet. Pharmacol. Ther. 2018, 41, 463–468. [Google Scholar] [CrossRef]
- Karademir, U.; Erdogan, H.; Boyacioglu, M.; Kum, C.; Sekkin, S.; Bilgen, M. Pharmacokinetics of meloxicam in adult goats: A comparative study of subcutaneous, oral and intravenous administration. N. Z. Vet. J. 2016, 64, 165–168. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Huo, M.; Zhou, J.; Xie, S. PKSolver: An add-in program for pharmacokinetic and pharmacodynamic data analysis in Microsoft Excel. Comput. Methods Programs Biomed. 2010, 99, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Dohoo, I.; Martin, W.; Stryhn, H. Veterinary Epidemiologic Research, 2nd ed.; VER Inc.: Charlottetown, PE, Canada, 2009. [Google Scholar]
- Meikle, A.; Kulcsár, M.; Chilliard, Y.; Fébel, H.; Delavaud, C.; Cavestany, D.; Chilibroste, P. Effects of parity and body condition at parturition on endocrine and reproductive parameters of the cow. Reproduction 2004, 127, 727–737. [Google Scholar] [CrossRef]
- Coetzee, J.F.; Mosher, R.A.; KuKanich, B.; Gehring, R.; Robert, B.; Reinbold, J.B.; White, B.J. Pharmacokinetics and effect of intravenous meloxicam in weaned Holstein calves following scoop dehorning without local anesthesia. BMC Vet. Res. 2012, 8, 153. [Google Scholar] [CrossRef]
- Jeunesse, E.C.; Bargues, I.A.; Toutain, C.E.; Lacroix, M.Z.; Letellier, I.M.; Giraudel, J.M.; Toutain, P.L. Paw Inflammation Model in Dogs for Preclinical Pharmacokinetic/Pharmacodynamic Investigations of Nonsteroidal Anti-Inflammatory Drugs. J. Pharmacol. Exp. Ther. 2011, 338, 548–558. [Google Scholar] [CrossRef]
- Lees, P.; Toutain, P.-L. The role of pharmacokinetics in veterinary drug residues. Drug Test. Anal. 2012, 4, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Toutain, P.-L.; Cester, C.C. Pharmacokinetic-pharmacodynamic relationships and dose response to meloxicam in horses with induced arthritis in the right carpal joint. Am. J. Vet. Res. 2004, 65, 1533–1541. [Google Scholar] [CrossRef] [PubMed]
- González Canga, A.; Sahagún Prieto, A.M.; José Diez Liébana, M.; Martínez, N.F.; Vega, M.S.; Vieitez, J.J.G. The pharmacokinetics and metabolism of ivermectin in domestic animal species. Vet. J. 2009, 179, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Coetzee, J.F.; Mosher, R.A.; Kohake, L.E.; Cull, C.A.; Kelly, L.L.; Mueting, S.L.; KuKanich, B. Pharmacokinetics of oral gabapentin alone or co-administered with meloxicam in ruminant beef calves. Vet. J. 2011, 190, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Antanaitis, R.; Januskauskas, A.; Rutkauskas, A.; Zilinskas, H. The effect of post-calving pain management with carprofen on stress, reproduction, and milk yield in cattle. Acta Vet. Brno 2018, 87, 115–118. [Google Scholar] [CrossRef]
- Stilwell, G.; Schubert, H.; Broom, D. Short communication: Effects of analgesic use postcalving on cow welfare and production. J. Dairy Sci. 2014, 97, 888–891. [Google Scholar] [CrossRef] [PubMed]
- Newby, N.C.; Renaud, D.; Tremblay, R.; Duffield, T.F. Evaluation of the effects of treating dairy cows with meloxicam at calving on retained fetal membranes risk. Can. Vet. J. 2014, 55, 1196–1199. [Google Scholar] [PubMed]
- Carpenter, A.; Ylioja, C.; Vargas, C.; Mamedova, L.; Mendonça, L.; Coetzee, J.; Hollis, L.; Gehring, R.; Bradford, B. Hot topic: Early postpartum treatment of commercial dairy cows with nonsteroidal antiinflammatory drugs increases whole-lactation milk yield. J. Dairy Sci. 2016, 99, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Shock, D.A.; Renaud, D.L.; Roche, S.M.; Poliquin, R.; Thomson, R.; Olson, M.E. Evaluating the impact of meloxicam oral suspension administered at parturition on subsequent production, health, and culling in dairy cows: A randomized clinical field trial. PLoS ONE 2018, 13, e0209236. [Google Scholar] [CrossRef]
- von Keyserlingk, M.A.G.; Rushen, J.; de Passillé, A.M.; Weary, D.M. Invited review: The welfare of dairy cattle—Key concepts and the role of science. J. Dairy Sci. 2009, 92, 4101–4111. [Google Scholar] [CrossRef]
| Variable | Oral Meloxicam (MOS) | Subcutaneous Meloxicam (MET) | Total |
|---|---|---|---|
| Parity | |||
| # 1st lactation cows | 3 | 2 | 5 |
| # ≥2nd lactation cows | 3 | 4 | 7 |
| Kg milk production (Std. Dev.) at first test | 39 (8.6) | 43 (12.5) | 41 (10.9) |
| MOS 1 | MET 2 | |||
|---|---|---|---|---|
| Mean (SE 9) | Range | Mean (SE) | Range | |
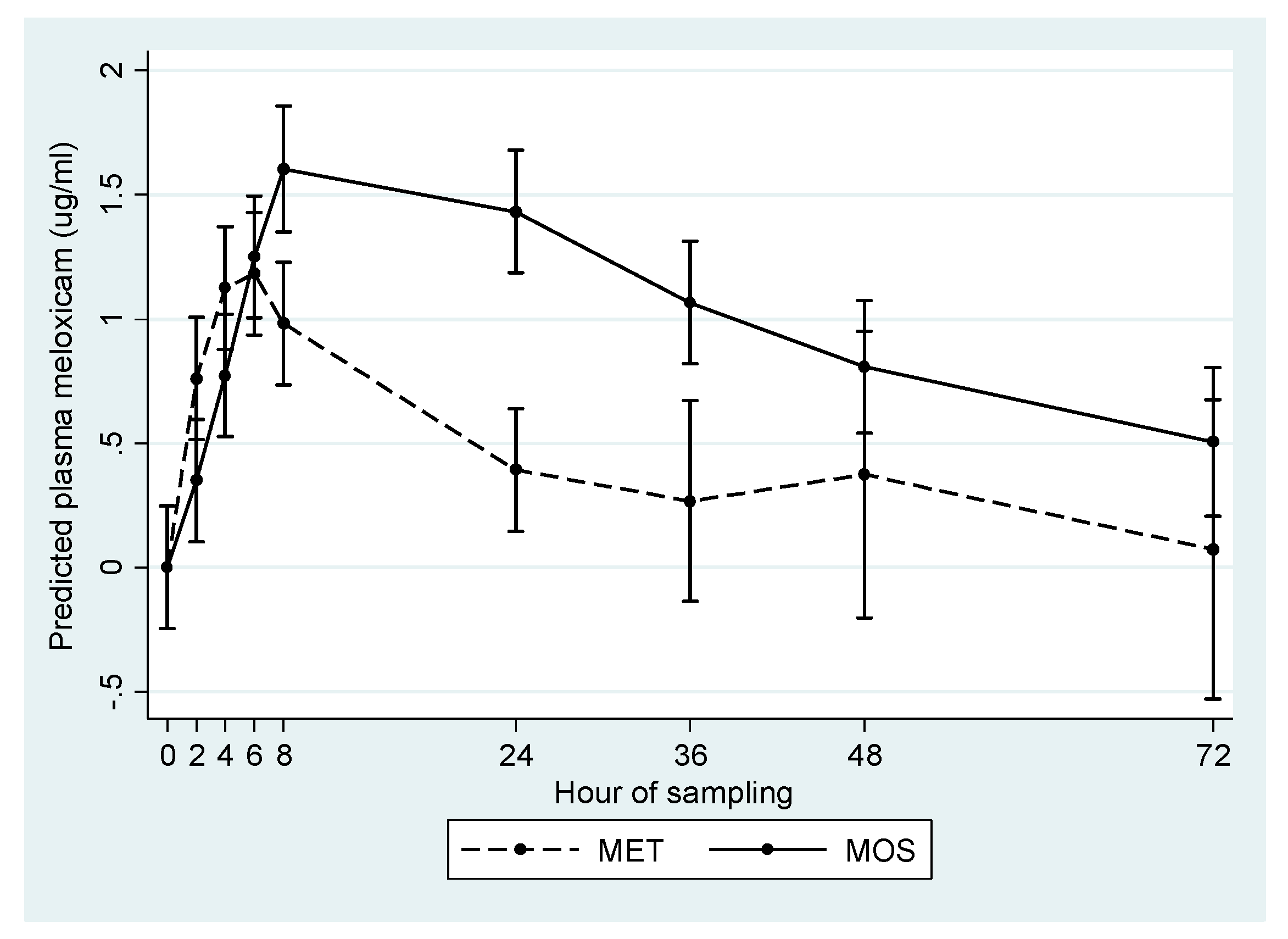
| Half Life 3 | 25.71 a (1.39) | 18.57–32.68 | 8.95 b (1.85) | 4.11–12.37 |
| AUC0-t 4 | 67.46 a (14.25) | 25.52–113.26 | 22.26 b (4.70) | 14.84–45.04 |
| AUC0-∞ 5 | 86.13 a (17.46) | 39.89–150.05 | 25.53 b (5.11) | 15.31–46.65 |
| Cmax 6 | 1.68 a (0.20) | 1.08–2.30 | 1.22 a (0.10) | 0.76–1.47 |
| Tmax 7 | 13.33 a (3.37) | 8–24 | 5.33 b (0.42) | 4–6 |
| KE 8 | 0.03 a (0.001) | 0.02–0.04 | 0.09 b (0.02) | 0.05–0.17 |
| Variable | Estimate | SE 1 | 95% CI 2 | p-Value |
|---|---|---|---|---|
| Treatment: | ||||
| MET 3 | Referent | |||
| MOS 4 | 16.15 | 2.65 | 10.16–22.15 | <0.0001 |
| Lactation Group: | ||||
| 1st | Referent | |||
| 2nd and greater | −3.68 | 2.1 | −12.16 | 0.2 |
| Constant | 11.41 | 2.57 | 5.87–17.22 | 0.002 |
| Variable | Estimate 1 | SE 2 | 95% CI 3 | p-Value |
|---|---|---|---|---|
| Treatment: | ||||
| MET 4 | Referent | |||
| MOS 5 | 1.06 | 0.15 | 0.73–1.40 | <0.0001 |
| Lactation Group: | ||||
| 1 st | Referent | |||
| 2 nd and greater | −0.8 | 0.15 | −1.13–(−0.46) | <0.0001 |
| Constant | 3.68 | 0.14 | 3.35–4.00 | <0.0001 |
| Variable | Estimate | SE 1 | 95% CI 2 | p-Value |
|---|---|---|---|---|
| Treatment: | ||||
| MET 3 | Referent | |||
| MOS 4 | 0.37 | 0.16 | 0.01–0.72 | 0.04 |
| Lactation Group: | ||||
| 1 st | Referent | |||
| 2 nd and greater | −0.56 | 0.16 | −0.92–[−0.20] | 0.007 |
| Constant | 1.59 | 0.15 | 1.24–1.94 | <0.0001 |
| Meloxicam Plasma Concentration Threshold (µg/mL) | Mean (h) | Std. Dev. (h) | Min (h) | Max (h) | |
|---|---|---|---|---|---|
| MET | 0.7 | 13.5 | 6.8 | 7.0 | 21.0 |
| 0.2 | 45.8 | 25.0 | 25.0 | 78.0 | |
| MOS | 0.7 | 30.3 | 14.9 | 15.0 | 47.0 |
| 0.2 | 93.0 | 23.7 | 70.0 | 134.0 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shock, D.; Roche, S.; Olson, M. A Comparative Pharmacokinetic Analysis of Oral and Subcutaneous Meloxicam Administered to Postpartum Dairy Cows. Vet. Sci. 2019, 6, 73. https://doi.org/10.3390/vetsci6030073
Shock D, Roche S, Olson M. A Comparative Pharmacokinetic Analysis of Oral and Subcutaneous Meloxicam Administered to Postpartum Dairy Cows. Veterinary Sciences. 2019; 6(3):73. https://doi.org/10.3390/vetsci6030073
Chicago/Turabian StyleShock, Daniel, Steven Roche, and Merle Olson. 2019. "A Comparative Pharmacokinetic Analysis of Oral and Subcutaneous Meloxicam Administered to Postpartum Dairy Cows" Veterinary Sciences 6, no. 3: 73. https://doi.org/10.3390/vetsci6030073
APA StyleShock, D., Roche, S., & Olson, M. (2019). A Comparative Pharmacokinetic Analysis of Oral and Subcutaneous Meloxicam Administered to Postpartum Dairy Cows. Veterinary Sciences, 6(3), 73. https://doi.org/10.3390/vetsci6030073





