Interference of Streptococcus agalactiae Blitz Therapy in Staphylococcus aureus Microbiological Diagnosis in Subclinical Bovine Mastitis
Abstract
Simple Summary
Abstract
1. Introduction
2. Material and Methods
2.1. Ethical Committee for Animal Use
2.2. Characteristics of Studied Dairy Herd
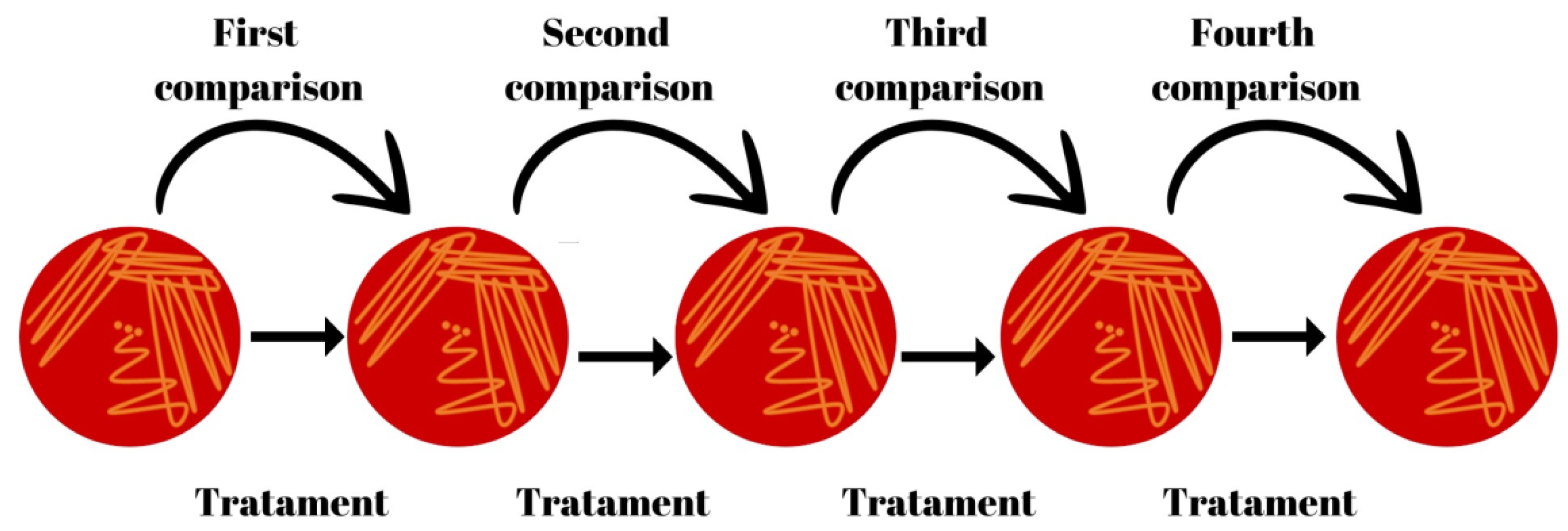
2.3. Frequency and Procedures for Collecting Milk Samples
2.4. Methodology for Somatic Cell Counts (SCC), Total Bacteria Counts (TBC), and Microbiological Diagnosis
2.5. Treatment of Subclinical Mastitis Cases
2.6. Study Design and Statistical Analysis
RP = (AP + SPC − 1)/(SEN + SPC − 1)
3. Results
3.1. Somatic Cell Counts and Total Bacteria Count according to Subclinical Mastitis Pathogens
3.2. Evaluation of the Dynamic of Subclinical Mastitis Infection according to Pathogens
3.3. Variation of Sensitivity, Specificity, Predictive Values, and Accuracy of Microbiological Diagnosis of S. aureus during Blitz Therapy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Heikkila, A.M.; Nousiainen, J.; Pyörälä, S. Costs of clinical mastitis with special reference to premature culling. J. Dairy Sci. 2012, 95, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Souza, F.N.; Cunha, A.F.; Rosa, D.L.; Brito, M.A.V.; Guimarães, A.S.; Mendonça, L.C.; Souza, G.N.; Lage, A.P.; Blagitz, M.G.; Della Libera, A.M.; et al. Somatic cell count and mastitis pathogen detection in composite and single or duplicate quarter milk samples. Pesqui. Veterinária Bras. 2016, 36, 811–818. [Google Scholar] [CrossRef]
- Keefe, G.P. Update on control of Staphylococcus aureus and Streptococcus agalactiae for Management of Mastitis. Vet. Clin. North Am. Food Anim. Pract. 2012, 28, 203–216. [Google Scholar] [CrossRef] [PubMed]
- Mendonça, L.C.; Gentilini, M.B.; Carvalho, N.L.; Malacco, V.R.; Lage, C.A.; Molina, L.R. Blitz therapy in control of Streptococcus agalactiae subclinical mastitis in dairy cows reduces somatic cell count of bulk milk tank in a dairy cattle herd. Acta Vet. Bras. 2017, 11, 1–5. [Google Scholar]
- Carvalho-Castro, G.A.; Silva, J.R.; Paiva, L.V.; Custódio, D.A.; Moreira, R.O.; Mian, G.F.; Prado, I.A.; Chalfun-Junior, A.; Costa, G.M. Molecular epidemiology of Streptococcus agalactiae isolated from mastitis in Brazilian dairy herds. Braz. J. Microbiol. 2017, 48, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.V.; Fonseca, L.F.L. Controle da Mastite e Qualidade do Leite: Desafios e Soluções, 1st ed.; Edição dos Autores: Pirassununga, Brazil, 2019; 301p, ISBN 978-85-915913-1-2. [Google Scholar]
- Svennesen, L.; Lund, T.B.; Skarbye, A.P.; Klaas, I.C.; Nielsen, S.S. Expert evaluation of different infection types in dairy cows quarters naturally infected with Staphylococcus aureus or Streptococcus agalactiae. Prev. Vet. Med. 2019, 167, 16–23. [Google Scholar] [CrossRef] [PubMed]
- National Mastitis Council. Recommended Mastitis Control Program; National Mastitis Council: New Prague, MN, USA, 2000. [Google Scholar]
- Edmondson, P. Blitz therapy for eradication of Streptococcus agalactiae infections in dairy cattle. Farm Anim. Pract. 2011, 33, 33–37. [Google Scholar] [CrossRef]
- Mendonça, J.F.M.; Brito, M.A.V.P.; Lange, C.C.; Silva, M.R.; Ribeiro, J.B.; Mendonca, L.; de Souza, G.N. Prevalence reduction of contagious mastitis pathogens in a Holstein dairy herd under tropical conditions. J. Vet. Sci. Technol. 2018, 9, 1–3. [Google Scholar] [CrossRef]
- Barkema, H.W.; Schukken, Y.H.; Zadoks, R.N. Invited Review: The Role of Cow, Pathogen and Treatment Regimen in the Therapeutic Success of Bovine Staphylococcus aureus Mastitis. J. Dairy Sci. 2006, 89, 1877–1895. [Google Scholar] [CrossRef] [PubMed]
- Adkins, P.R.F.; Middleton, J.R. Methods for diagnosing mastitis. Vet. Clin. Food Anim. Pract. 2018, 34, 479–491. [Google Scholar] [CrossRef] [PubMed]
- Souza, G.N.; Brito, J.; Moreira, E.; Brito, M.; Silva, M. Variação da Contagem de Células somáticas em vacas leiteiras de acordo com patógenos da mastite. Arq. Bras. Med. Vet. Zootec. 2009, 61, 1015–1020. [Google Scholar] [CrossRef]
- Analkip, M.E.; Quintela-Baluja, M.; Bohme, K.; Fernandez-No, I.; Caamano-Antelo, S.; Calo-Mata, P.; Barros-Velazquez, J. The Immunology of Mammary Gland of Dairy Ruminants between Healthy and Inflammatory Conditions. J. Vet. Med. 2014, 2014, 659801. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, R.M.; Schwertz, C.I.; de Cecco, B.S.; Panziera, W.; De Lorenzo, C.; Heck, L.C.; Snel, G.G.M.; Lopes, B.C.; da Silva, F.S.; Pavarini, S.P.; et al. Pathological and microbiological characterization of mastitis in dairy cows. Trop. Anim. Health Prod. 2019, 51, 2057–2066. [Google Scholar] [CrossRef] [PubMed]
- Lopes, J.E.F., Jr.; Lange, C.C.; Brito, M.A.V.P.; Santos, F.R.; Silva, M.A.S.; de Moraes, L.C.D.; de Souza, G.N. Relationship between total bacteria counts and somatic cell counts from mammary quarters infected by mastitis pathogens. Ciência Rural. 2012, 42, 691–696. [Google Scholar] [CrossRef]
- Britten, A.M. The Role of Diagnostic Microbiology in Mastitis Control Programs. Vet. Clin. N. Am. Food Anim. Pract. 2012, 28, 187–202. [Google Scholar] [CrossRef] [PubMed]
- Sears, P.M.; Smith, B.; English, P.; Herer, P.; Gonzalez, R.N. Shedding pattern of Staphylococcus aureus from bovine intramammary infections. J. Dairy Sci. 1990, 73, 2785–2789. [Google Scholar] [CrossRef] [PubMed]
- National Mastitis Council. Laboratory Handbook on Bovine Mastitis, 3rd ed.; National Mastitis Council: New Prague, MN, USA, 2017; 47p. [Google Scholar]
- Habibzadeh, F.; Habibzadeh, P.; Yadollahie, M. The apparent prevalence, the true prevalence. Biochem. Medica 2022, 32, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Keefe, G.P. Streptococcus agalactiae mastitis: A review. Can. Vet. J. 1997, 38, 429–437. [Google Scholar] [PubMed]
| Microbiological Results of the Previous Month | Microbiological Results for Next Month | |
|---|---|---|
| Positive | Negative | |
| Positive | a | b |
| Negative | c | d |
| Microbiological Result | N | Mean of SCC (×1000 Cells/mL) 1 | Median of TBC (×1000 cfu/mL) 2 |
|---|---|---|---|
| No growth | 21 | 139 a | 27 a |
| Corynebacterium bovis | 14 | 134 a | 27 a |
| Coagulase-negative staphylococci | 12 | 151 a | 27 a |
| Staphylococcus aureus | 11 | 730 b | 41 ab |
| Streptococcus uberis | 12 | 1.318 b | 100 b |
| Streptococcus agalactiae | 50 | 1.658 b | 93 b |
| Month | S. agalactiae | S. aureus | S. agalactiae | S. aureus | ||||
|---|---|---|---|---|---|---|---|---|
| AP (%) | RP (%) | AP (%) | RP (%) | Incidence | Elimination | Incidence | CI | |
| 1 | 61.0 | 61.6 | 28.3 | 25.2 | 5.6 | 40.3 | 19.4 | 19.4 |
| 2 | 18.8 | 17.1 | 38.9 | 25.5 | 1.5 | 7.6 | 3.1 | 26.7 |
| 3 | 3.8 | 1.4 | 29.8 | 38.5 | 2.7 | 2.1 | 10.3 | 19.9 |
| 4 | 4.8 | 2.4 | 33.6 | 36.9 | 1.3 | 1.9 | 8.9 | 28.7 |
| 5 | 3.8 | 1.4 | 35.0 | 39.0 | - | - | - | - |
| Months | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) |
|---|---|---|---|---|---|
| (Kappa Index) | |||||
| 1 | 50.0 | 79.0 | 62.2 | 69.5 | 67.1 |
| 2 | 89.7 | 78.5 | 62.5 | 95.0 | 81.7 |
| 3 | 59.1 | 88.6 | 74.3 | 79.5 | 78.1 |
| 4 | 76.3 | 91.4 | 85.7 | 85.2 | 85.4 |
| Mean | 68.8 | 84.4 | 71.2 | 82.3 | 78.1 |
| SD | 17.7 | 6.6 | 11.2 | 10.7 | 7.9 |
| MCI 95% | 34.1–100.0 | 71.4–97.3 | 49.2–93.1 | 61.4–100.0 | 62.6–93.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gomes, A.F.N.; de Castro, F.d.F.A.; Silva, M.R.; Lange, C.C.; Ribeiro, J.B.; Guimarães, A.d.S.; de Souza, G.N. Interference of Streptococcus agalactiae Blitz Therapy in Staphylococcus aureus Microbiological Diagnosis in Subclinical Bovine Mastitis. Vet. Sci. 2024, 11, 233. https://doi.org/10.3390/vetsci11060233
Gomes AFN, de Castro FdFA, Silva MR, Lange CC, Ribeiro JB, Guimarães AdS, de Souza GN. Interference of Streptococcus agalactiae Blitz Therapy in Staphylococcus aureus Microbiological Diagnosis in Subclinical Bovine Mastitis. Veterinary Sciences. 2024; 11(6):233. https://doi.org/10.3390/vetsci11060233
Chicago/Turabian StyleGomes, Ana Flávia Novaes, Fúlvia de Fátima Almeida de Castro, Márcio Roberto Silva, Carla Christine Lange, João Batista Ribeiro, Alessandro de Sá Guimarães, and Guilherme Nunes de Souza. 2024. "Interference of Streptococcus agalactiae Blitz Therapy in Staphylococcus aureus Microbiological Diagnosis in Subclinical Bovine Mastitis" Veterinary Sciences 11, no. 6: 233. https://doi.org/10.3390/vetsci11060233
APA StyleGomes, A. F. N., de Castro, F. d. F. A., Silva, M. R., Lange, C. C., Ribeiro, J. B., Guimarães, A. d. S., & de Souza, G. N. (2024). Interference of Streptococcus agalactiae Blitz Therapy in Staphylococcus aureus Microbiological Diagnosis in Subclinical Bovine Mastitis. Veterinary Sciences, 11(6), 233. https://doi.org/10.3390/vetsci11060233







