Suspected Cerebral Salt Wasting Syndrome with Cervical Spinal Lesion in a Domestic Shorthair Cat
Abstract
Simple Summary
Abstract
1. Introduction
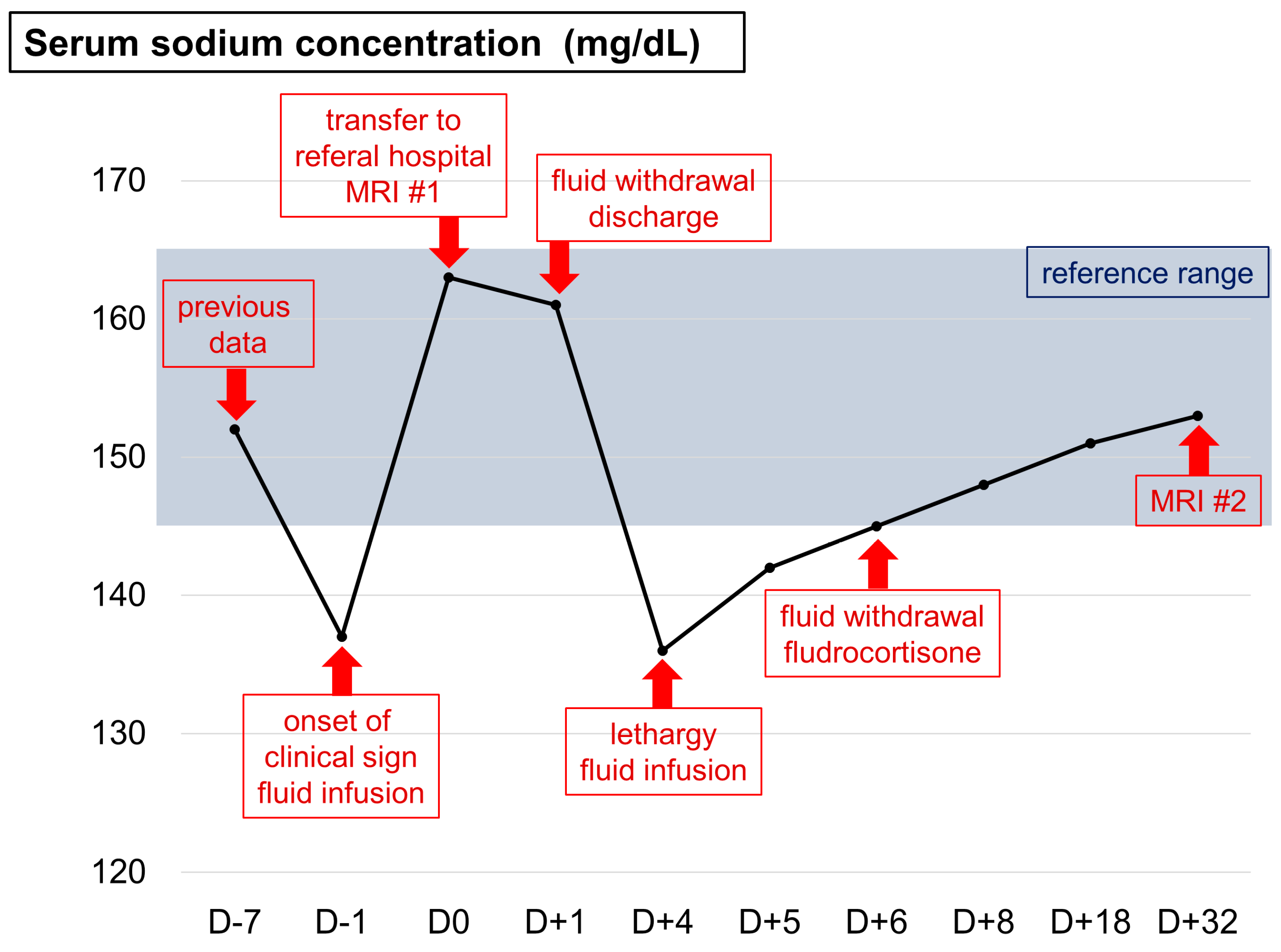
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Burton, A.G.; Hopper, K. Hyponatremia in dogs and cats. J. Vet. Emerg. Crit. Care 2019, 29, 461–471. [Google Scholar] [CrossRef] [PubMed]
- Dibartola, S.P. Hyponatremia. Vet. Clin. N. Am. Small Anim. Pract. 1998, 28, 515–532. [Google Scholar] [CrossRef] [PubMed]
- Harrigan, M. Cerebral salt wasting syndrome. Crit. Care Clin. 2001, 17, 125–138. [Google Scholar] [CrossRef] [PubMed]
- Isotani, E.; Suzuki, R.; Tomita, K.; Hokari, M.; Monma, S.; Marumo, F.; Hirakawa, K. Alterations in plasma concentrations of natriuretic peptides and antidiuretic hormone after subarachnoid hemorrhage. Stroke 1994, 25, 2198–2203. [Google Scholar] [CrossRef] [PubMed]
- Cerdà-Esteve, M.; Cuadrado-Godia, E.; Chillaron, J.J.; Pont-Sunyer, C.; Cucurella, G.; Fernández, M.; Goday, A.; Cano Pèrez, J.F.; Rodrìguez-Campello, A.; Roquer, J. Cerebral salt wasting syndrome: Review. Eur. J. Intern. Med. 2008, 19, 149–254. [Google Scholar] [CrossRef]
- Sakarcan, A.; Bocchini, J. The role of fludrocortisone in a child with cerebral salt wasting. Pediatr. Nephrol. 1998, 12, 769–771. [Google Scholar] [CrossRef]
- Nakamoto, Y.; Ozawa, T.; Mashita, T.; Mitsuda, M.; Katakabe, K.; Nakaichi, M. Clinical outcomes of suspected ischemic myelopathy in cats. J. Vet. Med. 2010, 72, 1657–1660. [Google Scholar] [CrossRef]
- Albanese, A.; Hindmarsh, P.; Stanhope, R. Management of hyponaetremia in patients with acute cerebral insults. Arch. Dis. Child 2001, 85, 246–251. [Google Scholar] [CrossRef]
- Simpson, K.M.; Risio, L.D.; Theobald, A.; Garosi, L.; Lowrie, M. Feline ischaemic myelopathy with a predilection for the cranial cervical spinal cord in older cats. J. Feline Med. Surg. 2014, 16, 1001–1006. [Google Scholar] [CrossRef]
- Fortgens, P.; Pillay, T.S. Pseudohyponatremia revisited: A modern-day pitfall. Arch. Pathol. Lab. Med. 2011, 135, 516–519. [Google Scholar] [CrossRef]
- Fried, L.F.; Palevsky, P. Hyponatremia and hypernatremia. Med. Clin. North. Am. M. 1997, 81, 585–609. [Google Scholar] [CrossRef]
- Brady, C.A.; Hughes, D.; Drobatz, K.J. Association of hyponatremia and hyperglycemia with outcome in dogs with congestive heart failure. J. Vet. Emerg. Crit. Care 2004, 14, 177–182. [Google Scholar] [CrossRef]
- Cameron, K.; Gallagher, A. Inappropriate antidiuretic hormone secretion in a cat. J. Am. Anim. Hosp. Assoc. 2010, 46, 425–432. [Google Scholar] [CrossRef]
- Maesaka, J.K.; Gupta, S.; Fishbane, S. Cerebral salt-wasting syndrome: Does it exist? Nephron 1999, 82, 100–109. [Google Scholar] [CrossRef]
- Uygun, M.A.; Özkal, E.; Acar, O.; Erongun, U. Cerebral salt wasting syndrome. Neurosurg. Rev. 1996, 19, 193–196. [Google Scholar] [CrossRef]
- Leonard, J.; Garrett, R.E.; Salottolo, K.; Slone, D.S.; Mains, C.W.; Carrick, M.M.; Bar-Or, D. Cerebral salt wasting after traumatic brain injury: A review of the literature. Scand. J. Trauma Resusc. Emerg. Med. 2015, 23, 98. [Google Scholar] [CrossRef]
- Sterns, R.H.; Silver, S.M. Cerebral salt wasting versus SIADH: What difference? J. Am. Soc. Nephrol. 2008, 19, 194–196. [Google Scholar] [CrossRef]
- Schrier, R.W.; Gross, P.; Gheorghiade, M.; Berl, T.; Verbalis, J.G.; Czerwiec, F.S.; Orlandi, C. Tolvaptan, a selective oral vasopressin V2-reveptor antagonist, for hyponatremia. N. Engl. J. Med. 2006, 355, 2099–2112. [Google Scholar] [CrossRef]
- Hasan, D.; Lindsay, K.W.; Wijdicks, E.F.M.; Murray, G.D.; Brouwers, P.J.; Bakker, W.H.; Fign, J.V.; Vermeulen, M. Effect of fludrocortisone acetate in patients with subarachnoid hemorrhage. Stroke 1989, 20, 1156–1161. [Google Scholar] [CrossRef]
- Steele, A.; Deveber, H.; Quaggin, S.E.; Scheich, J.E.; Halperin, M.L. What is responsible for the diurnal variation in potassium excretion? Am. J. Physiol. Regul. Integr. Comp. Physiol. 1994, 267, R554–R560. [Google Scholar] [CrossRef]
- Lathan, P.; Thompson, A.L. Management of hypoadrenocorticism (Addison’s disease) in dogs. Res. Vet. Sci. 2018, 9, 1–10. [Google Scholar]
- Theobald, A.; Volk, H.A.; Dennis, R.; Berlato, D.; Risio, L.D. Clinical outcome in 19 cats with clinical and magnetic resonanace imaging diagnosis of ischaemic myelopathy (2000–2011). J. Feline Med. Surg. 2013, 15, 132–141. [Google Scholar] [CrossRef]
- Silvestrini, P.; Piviani, M.; Masian, D.S. Ischaemic myelopathy in a cat with chronic kidney disease, hyperthyroidism, and hyperaldosteronism. Vet. Rec. Case Rep. 2021, 9, e11. [Google Scholar] [CrossRef]
- Cui, H.; He, G.; Yang, S.; Lv, Y.; Jiang, Z.; Gang, X.; Wang, G. Inappropriate antidiuretic hormone secretion and cerebral salt-wasting syndromes in neurological patients. Front. Neurosci. 2019, 13, 1170. [Google Scholar] [CrossRef] [PubMed]
- Bouchlarhem, A.; Haddar, L.; Berrichi, H.; Jabri, M.; Lachhab, A.; Lamassab, N.E.; Bekkaoui, S.; Mamoun, I.B.E.; Berramdane, O.; Oulali, N. Cerebral Salt Wasting Syndrome (CSW): An unusual cause of hypovolemia after spontaneous cerebral hemorrhage successfully treated with fludrocortisone. Radiol. Case Rep. 2022, 17, 106–110. [Google Scholar] [CrossRef]

| Parameters | Value | Reference Range | Unit |
|---|---|---|---|
| CBC | |||
| RBC | 8.5 | 6.54–12.2 | 1012/L |
| HCT | 34.9 | 30.3–52.3 | % |
| #Reticulocytes | 18.7 | 3–50 | 103/µl |
| WBC | 10.36 | 2.87–17.02 | 109/L |
| PLT | 169 | 151–600 | 109/L |
| Serum chemistry | |||
| Na | 137 | 150–165 | mmol/L |
| K | 2.9 | 3.5–5.8 | mmol/L |
| Total protein | 7.2 | 5.7–8.9 | g/dL |
| BUN | 27 | 16–36 | mg/dL |
| Glucose | 170 | 7–159 | mg/dL |
| SDMA | 10 | 0–14 | µg/dL |
| Total T4 | 0.8 | 0.8–4.7 | µg/dL |
| Basal cortisol | 5.91 | 0.5–10 | µg/dL |
| SAA | 41.5 | 0–5 | µg/dL |
| NT-proBNP | 478 | 0–100 | pmol/L |
| Coagulation | |||
| D-dimer | <0.1 | 0–0.1 | µg/ml |
| Hyperosmolality | Normosmolality | Hyposmolality | ||
|---|---|---|---|---|
| Hypervolemia | Normovolemia | Hypovolemia | ||
| Hyperglycemia | Hyperlipidemia | Liver function loss | Primary polydipsia | Hypo- adrenocorticism |
| Mannitol infusion | Hyperproteinemia | Kidney function loss | Hypothyroidism | Pancreatitis |
| Congestive heart failure | Iatrogenic (Diuretics) | Peritonitis | ||
| Syndrome of inappropriate antidiuretic hormone | Gastrointestinal fluid loss | |||
| Burn | ||||
| Cerebral salt wasting syndrome | ||||
| Parameters | SIADH | CSWS |
|---|---|---|
| Hydration status | Hydrated | Dehydrated |
| Urine volume | Variable | Increased |
| Plasma BNP | Variable | Increased |
| ADH | Increased | Decreased |
| Serum uric acid | Decreased | Increased |
| CVP | Increased | Decreased |
| Management | Fluid restriction | Fluid infusion |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.; Song, W.-J.; Park, J.; Lee, S.; Choen, S.; Kim, M.-C.; Yun, Y. Suspected Cerebral Salt Wasting Syndrome with Cervical Spinal Lesion in a Domestic Shorthair Cat. Vet. Sci. 2023, 10, 385. https://doi.org/10.3390/vetsci10060385
Kim M, Song W-J, Park J, Lee S, Choen S, Kim M-C, Yun Y. Suspected Cerebral Salt Wasting Syndrome with Cervical Spinal Lesion in a Domestic Shorthair Cat. Veterinary Sciences. 2023; 10(6):385. https://doi.org/10.3390/vetsci10060385
Chicago/Turabian StyleKim, Minkun, Woo-Jin Song, Jongjin Park, Saeyoung Lee, Sangkyung Choen, Myung-Chul Kim, and Youngmin Yun. 2023. "Suspected Cerebral Salt Wasting Syndrome with Cervical Spinal Lesion in a Domestic Shorthair Cat" Veterinary Sciences 10, no. 6: 385. https://doi.org/10.3390/vetsci10060385
APA StyleKim, M., Song, W.-J., Park, J., Lee, S., Choen, S., Kim, M.-C., & Yun, Y. (2023). Suspected Cerebral Salt Wasting Syndrome with Cervical Spinal Lesion in a Domestic Shorthair Cat. Veterinary Sciences, 10(6), 385. https://doi.org/10.3390/vetsci10060385






