Tobacco Smoke Exposure in Pregnant Dogs: Maternal and Newborn Cotinine Levels: A Pilot Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Samples Collection
2.3. Cotinine Assay
2.4. Statistical Analysis
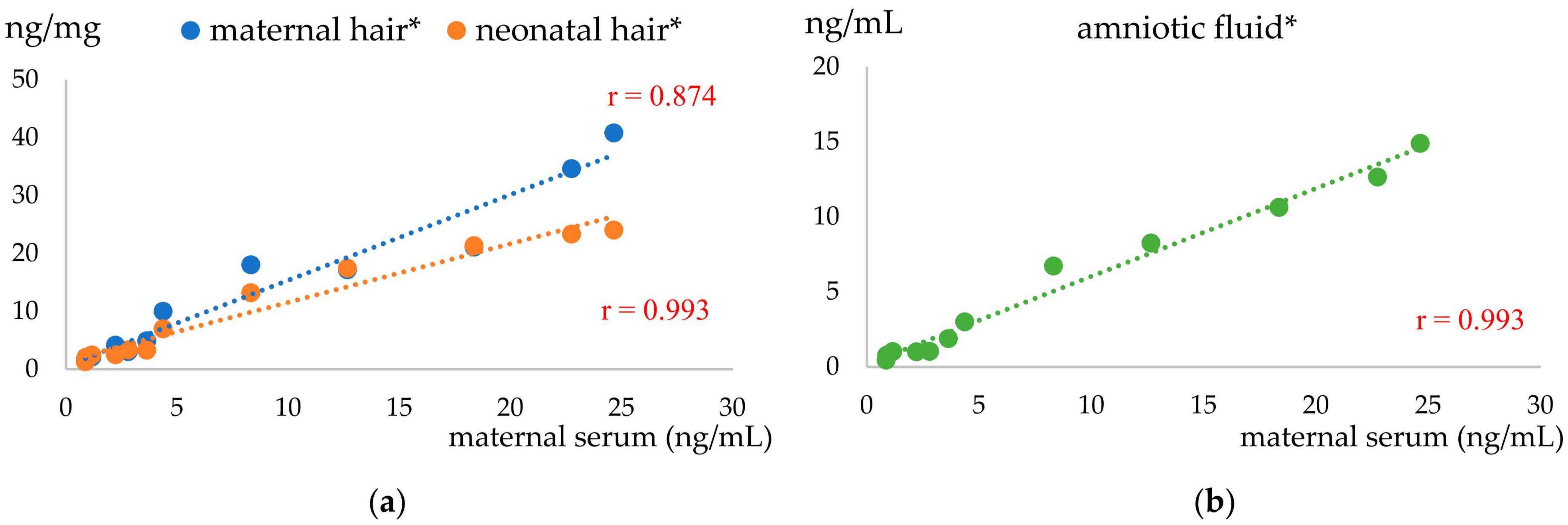
3. Results
3.1. Clinical Outcomes
3.2. Cotinine Detection
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cao, S.; Yang, C.; Gan, Y.; Lu, Z. The health effects of passive smoking: An overview of systematic re-views based on observational epidemiological evidence. PLoS ONE 2015, 10, e0139907. [Google Scholar] [CrossRef] [PubMed]
- Jacob, P.; Benowitz, N.L.; Destaillats, H.; Gundel, L.; Hang, B.; Martins-Green, M.; Matt, G.E.; Quintana, P.J.E.; Samet, J.M.; Schick, S.F.; et al. Thirdhand smoke: New evidence, challenges, and future directions. Chem. Res. Toxicol. 2017, 30, 270–294. [Google Scholar] [CrossRef] [PubMed]
- Pineles, B.L.; Park, E.; Samet, J.M. Systematic review and meta-analysis of miscarriage and maternal exposure to tobacco smoke during pregnancy. Am. J. Epidemiol. 2014, 179, 807–823. [Google Scholar] [CrossRef] [PubMed]
- Pineles, B.L.; Hsu, S.; Park, E.; Samet, J.M. Systematic Review and Meta-Analyses of Perinatal Death and Maternal Exposure to Tobacco Smoke During Pregnancy. Am. J. Epidemiol. 2016, 184, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Abraham, M.; Alramadhan, S.; Iniguez, C.; Duijts, L.; Jaddoe, V.W.; Den Dekker, H.T.; Crozier, S.; Godfrey, K.M.; Hindmarsh, P.; Vik, T.; et al. A systematic review of maternal smoking during pregnancy and fetal measurements with meta-analysis. PLoS ONE 2017, 12, e0170946. [Google Scholar] [CrossRef]
- Bublitz, M.H.; Stroud, L.R. Maternal smoking during pregnancy and offspring brain structure and function: Review and agenda for future research. Nicotine Tob. Res. 2012, 14, 388–397. [Google Scholar] [CrossRef]
- Weitzman, M.; Byrd, R.S.; Aligne, C.A.; Moss, M. The effects of tobacco exposure on children’s behavioral and cognitive functioning: Implications for clinical and public health policy and future research. Neurotoxicol. Teratol. 2002, 24, 397–406. [Google Scholar] [CrossRef]
- Yu, C.; Wei, Y.; Tang, X.; Liu, B.; Shen, L.; Long, C.; Lin, T.; He, D.; Wu, S.; Wei, G. Maternal smoking during pregnancy and risk of cryptorchidism: A systematic review and meta-analysis. Eur. J. Pediatr. 2019, 178, 287–297. [Google Scholar] [CrossRef]
- Holloway, A.C.; Salomon, A.; Soares, M.J.; Garnier, V.; Raha, S.; Sergent, F.; Nicholson, C.J.; Feige, J.J.; Benharouga, M.; Alfaidy, N. Characterization of the adverse effects of nicotine on placental development: In vivo and in vitro studies. Am. J. Physiol. Endocrinol. Metab. 2014, 306, E443–E456. [Google Scholar] [CrossRef]
- Cui, H.; Gong, T.T.; Liu, C.X.; Wu, Q.J. Associations between Passive Maternal Smoking during Pregnancy and Preterm Birth: Evidence from a Meta-Analysis of Observational Studies. PLoS ONE 2016, 11, e01478482016. [Google Scholar] [CrossRef]
- Salmasi, G.; Grady, R.; Jones, J.; McDonald, S.D. Environmental tobacco smoke exposure and perinatal outcomes: A systematic review and meta-analyses. Acta Obstet. Gynecol. Scand. 2010, 89, 423–441. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Sun, Y.; Duan, W.; Jia, C. Meta-analysis of the association of maternal smoking and passive smoking during pregnancy with neural tube defects. Int. J. Gynaecol. Obstet. 2018, 140, 18–25. [Google Scholar] [CrossRef] [PubMed]
- El-Ardat, M.A.; Izetbegovic, S.; El-Ardat, K.A. Effect of cigarette smoking in pregnancy on infants anthropometric characteristics. Mater. Sociomed. 2014, 26, 186–187. [Google Scholar] [CrossRef] [PubMed]
- Swanson, J.M.; Entringer, S.; Buss, C.; Wadhwa, P.D. Developmental Origins of Health and Disease: Environmental Exposures. Semin. Reprod. Med. 2009, 27, 391–402. [Google Scholar] [CrossRef]
- Tzatzarakis, M.N.; Vardavas, C.I.; Terzi, I.; Kavalakis, M.; Kokkinakis, M.; Liesivuori, J.; Tsatsakis, A.M. Hair nicotine/cotinine concentrations as a method of monitoring exposure to tobacco smoke among infants and adults. Hum. Exp. Toxicol. 2012, 31, 258–265. [Google Scholar] [CrossRef]
- Tan, X.; Vrana, K.; Ding, Z.-M. Cotinine: Pharmacologically Active Metabolite of Nicotine and Neural Mechanisms for Its Actions. Front. Behav. Neurosci. 2021, 15, 758252. [Google Scholar] [CrossRef]
- Benowitz, N.L. Cotinine as a biomarker of environmental tobacco smoke exposure. Epidemiol. Rev. 1996, 18, 188–204. [Google Scholar] [CrossRef]
- Baheiraei, A.; Banihosseini, S.Z.; Heshmat, R.; Mota, A.; Mohsenifar, A. Association of self-reported passive smoking in pregnant women with cotinine level of maternal urine and umbilical cord blood at delivery. Paediatr. Perinat. Epidemiol. 2012, 26, 70–76. [Google Scholar] [CrossRef]
- Sachiyo, K.; Kumiko, A.; Keiko, N.; Kaori, K.; Sonomi, O. Effect of passive smoking using maternal and neonatal salivary cotinine measurements. Nurs. Res. 2012, 61, 140–144. [Google Scholar] [CrossRef]
- Eskenazi, B.; Prehn, A.W.; Christianson, R.E. Passive and active maternal smoking as measured by serum cotinine: The effect on birthweight. Am. J. Public Health 1995, 85, 395–398. [Google Scholar] [CrossRef]
- Eliopoulos, C.; Klein, J.; Phan, M.K.; Knie, B.; Greenwald, M.; Chitayat, D.; Koren, G. Hair concentrations of nicotine and cotinine in women and their newborn infants. JAMA 1994, 271, 621–623. [Google Scholar] [CrossRef]
- Jordanov, J.S. Cotinine concentrations in amniotic fluid and urine of smoking, passive smoking and non-smoking pregnant women at term and in the urine of their neonates on 1st day of life. Eur. J. Pediatr. 1990, 149, 734–737. [Google Scholar] [CrossRef] [PubMed]
- Dhar, P. Measuring Tobacco Smoke Exposure: Quantifying nicotine/cotinine concentration in biologi-cal samples by colorimetry, chromatography and immunoassay methods. J. Pharm. Biomed. Anal. 2004, 35, 155–168. [Google Scholar] [CrossRef] [PubMed]
- Gunay, F.; Ilarslan, N.E.C.; Bakar-Ates, F.; Deniz, K.; Kadioglu, Y.K.; Kiran, S.; Bakirarar, B.; Cobanoglu, N. Evaluation of Hair Cotinine and Toxic Metal Levels in Children Who Were Exposed to Tobacco Smoke. Pediatr. Pulmonol. 2020, 55, 1012–1019. [Google Scholar] [CrossRef] [PubMed]
- Groppetti, D.; Pizzi, G.; Pecile, A.; Bronzo, V.; Mazzola, S. Cotinine as a sentinel of canine exposure to tobacco smoke. Animals 2023, 13, 693. [Google Scholar] [CrossRef]
- Coussons-Read, M.E. Effects of prenatal stress on pregnancy and human development: Mechanisms and pathways. Obstet. Med. 2013, 6, 52–57. [Google Scholar] [CrossRef]
- Gaccioli, F.; Lager, S. Placental Nutrient Transport and Intrauterine Growth Restriction. Front. Physiol. 2016, 7, 40. [Google Scholar] [CrossRef]
- Bertone-Johnson, E.R.; Procter-Gray, E.; Gollenberg, A.L.; Ryan, M.B.; Barber, L.G. Environmental tobacco smoke and canine urinary cotinine level. Environ. Res. 2008, 106, 361–364. [Google Scholar] [CrossRef]
- Al-Delaimy, W.K. Hair as a biomarker for exposure to tobacco smoke. Tob. Control. 2002, 11, 176–182. [Google Scholar] [CrossRef]
- Luck, W.; Nau, H.; Hansen, R.; Steldinger, R. Extent of nicotine and cotinine transfer to the human fetus, placenta and amniotic fluid of smoking mothers. Dev. Pharmacol. Ther. 1985, 8, 384–395. [Google Scholar] [CrossRef]
- Jauniaux, E.; Gulbis, B.; Acharya, G.; Thiry, P.; Rodeck, C. Maternal tobacco exposure and cotinine levels in fetal fluids in the first half of pregnancy. Obstet. Gynecol. 1999, 93, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Terzioglu, F.; Boztepe, H.; Erkekoglu, P.; Korucu, A.E.; Kocer-Gumusel, B.; Kandemir, O. The effects of amniotic fluid and foetal cord blood cotinine concentrations on pregnancy complications and the anthropometric measurements of newborns. J. Obestetrics Gynaecol. 2019, 39, 952–958. [Google Scholar] [CrossRef] [PubMed]
- Machado, J.d.B.; Chatkin, J.M.; Zimmer, A.R.; Goulart, A.P.S.; Thiesen, F.V. Cotinine and Polycyclic Aromatic Hydrocarbons Levels in the Amniotic Fluid and Fetal Cord at Birth and in the Urine from Pregnant Smokers. PLoS ONE 2014, 9, e116293. [Google Scholar] [CrossRef] [PubMed]
- Llaquet, H.; Pichini, S.; Joya, X.; Papaseit, E.; Vall, O.; Klein, J.; Garcia-Algar, O. Biological matrices for the evaluation of exposure to environmental tobacco smoke during prenatal life and childhood. Anal. Bioanal. Chem. 2010, 396, 379–399. [Google Scholar] [CrossRef] [PubMed]
- Yurdakok-Dikmen, B.; Kuzukiran, O.; Uyar, R.; Gulsum Boztepe, U.; Çelik, H.T.; Ozyuncu, O.; Turgut, Y.; Kanca, H.; Karakas-Alkan, K.; Filazi, A. Live in same region, respond differently: Canine and human response to pollutants in placental accumulation. Chemosphere 2022, 301, 134470. [Google Scholar] [CrossRef]
- Walker, N.; Filis, P.; Soffientini, U.; Bellingham, M.; O’Shaughnessy, P.J.; Fowler, P.A. Placental transporter localization and expression in the Human: The importance of species, sex, and gestational age differences. Biol. Reprod. 2017, 96, 733–742. [Google Scholar] [CrossRef]
- Dockery, P.; Bermingham, J.; Jenkins, D. Structure-function relations in the human placenta. Biochem. Soc. Trans. 2000, 28, 202–208. [Google Scholar] [CrossRef]
- Kowalewski, M.P.; Kazemian, A.; Klisch, K.; Gysin, T.; Tavares Pereira, M.; Gram, A. Canine Endotheliochorial Placenta: Morpho-Functional Aspects. Adv. Anat. Embryol. Cell. Biol. 2021, 234, 155–179. [Google Scholar] [CrossRef]
- Florescu, A.; Ferrence, R.; Einarson, T.R.; Selby, P.; Kramer, M.; Woodruff, S.; Grossman, L.; Rankin, A.; Jacqz-Aigrain, E.; Koren, G. Reference values for hair cotinine as a biomarker of active and passive smoking in women of reproductive age, pregnant women, children, and neonates: Systematic review and meta-analysis. Ther. Drug Monit. 2007, 29, 437–446. [Google Scholar] [CrossRef]
- Bowker, K.; Lewis, S.; Coleman, T.; Cooper, S. Changes in the rate of nicotine metabolism across pregnancy: A longitudinal study. Addiction 2015, 110, 1827–1832. [Google Scholar] [CrossRef]
- Dempsey, D.; Jacob, P., 3rd; Benowitz, N.L. Accelerated metabolism of nicotine and cotinine in pregnant smokers. J. Pharmacol. Exp. Ther. 2002, 301, 594–859. [Google Scholar] [CrossRef] [PubMed]
- Isoherranen, N.; Thummel, K.E. Drug Metabolism and Transport during Pregnancy: How Does Drug Disposition Change during Pregnancy and What Are the Mechanisms that Cause Such Changes? Drug Metab. Dispos. 2013, 41, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H. Altered drug metabolism during pregnancy: Hormonal regulation of drug-metabolizing enzymes. Expert Opin. Drug Metab. Toxicol. 2010, 6, 689–699. [Google Scholar] [CrossRef] [PubMed]
- Fallatah, A.A.; Hanafi, R.; Afifi, I. Comparison of cotinine salivary levels between smokers, smokers and non-smokers passive. Egypt. J. Hosp. Med. 2018, 70, 982–989. [Google Scholar] [CrossRef]
- Mourino, N.; Ruano-Raviña, A.; Varela Lema, L.; Fernández, E.; López, M.J.; Santiago-Pérez, M.I.; Rey-Brandariz, J.; Giraldo-Osorio, A.; Pérez-Ríos, M. Serum cotinine cut-points for secondhand smoke exposure assessment in children under 5 years: A systemic review. PLoS ONE 2022, 17, e0267319. [Google Scholar] [CrossRef] [PubMed]
- Fu, M.; Fernandez, E.; Martínez-Sánchez, J.M.; Pascual, J.A.; Schiaffino, A.; Agudo, A.; Ariza, C.; Borràs, J.M.; Samet, J.M.; The DCOT Study Investigators. Salivary cotinine concentrations in daily smokers in Barcelona, Spain: A cross-sectional study. BMC Public Health 2009, 9, 320. [Google Scholar] [CrossRef]
- von Chamier, M.; Reyes, L.; Hayward, L.F.; Brown, M.B. Nicotine induces maternal and fetal inflammatory responses which predispose intrauterine infection risk in a rat model. Nicotine Tob. Res. 2021, 23, 1763–1770. [Google Scholar] [CrossRef] [PubMed]
- Breit, K.R.; Rodriguez, C.G.; Hussain, S.; Thomas, K.J.; Zeigler, M.; Gerasimidis, I.; Thomas, J.D. A model of combined exposure to nicotine and tetrahydrocannabinol via electronic cigarettes in pregnant rats. Front. Neurosci. 2022, 16, 866722. [Google Scholar] [CrossRef]
- Baba, S.; Wikström, A.K.; Stephansson, O.; Cnattingius, S. Influence of snuff and smoking habits in early pregnancy on risks for stillbirth and early neonatal mortality. Nicotine Tob. Res. 2014, 16, 78–83. [Google Scholar] [CrossRef]
- Wilson, S.E.; Kahn, R.S.; Khoury, J.; Lanphear, B.P. Racial differences in exposure to environmental tobacco smoke among children. Environ. Health Perspect. 2005, 113, 362–367. [Google Scholar] [CrossRef]
- Sabbagh, H.J.; Hassan, M.H.; Innes, N.P.; Elkodary, H.M.; Little, J.; Mossey, P.A. Passive smoking in the etiology of non-syndromic orofacial clefts: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0116963. [Google Scholar] [CrossRef] [PubMed]
- Lammer, E.J.; Shaw, G.M.; Iovannisci, D.M.; Finnell, R.H. Maternal smoking, genetic variation of glutathione s-transferases, and risk for orofacial clefts. Epidemiology 2005, 16, 698–701. [Google Scholar] [CrossRef] [PubMed]
- García-Villarino, M.; Fernández-Iglesias, R.; Riaño-Galán, I.; Rodríguez-Dehli, C.; Babarro, I.; Fernández-Somoano, A.; Tardón, A. Prenatal Exposure to Cigarette Smoke and Anogenital Distance at 4 Years in the INMA-Asturias Cohort. Int. J. Environ. Res. Public Health 2021, 18, 4774. [Google Scholar] [CrossRef] [PubMed]
- Kızılay, D.Ö.; Aydın, C.; Aygün, A.P.; Tuhan, H.Ü.; Olukman, Ö. Prenatal smoke exposure is associated with increased anogenital distance in female infants: A prospective case-control study. J. Pediatr. Endocrinol. Metab. 2020, 34, 79–88. [Google Scholar] [CrossRef]
- De Rooster, H.; Vercauteren, G.; Görtz, K.; Saunders, J.; Polis, I.; Rijsselaere, T. True hermaphroditism in six female littermates after administration of synthetic androgens to a pregnant bitch. Reprod. Domest. Anim. 2006, 41, 22–26. [Google Scholar] [CrossRef]
- Kobayashi, K.; Tsugami, Y.; Suzuki, N.; Suzuki, T.; Nishimura, T. Nicotine directly affects milk production in lactating mammary epithelial cells concurrently with inactivation of STAT5 and glucocorticoid receptor in vitro. Toxicol. In Vitro 2020, 63, 104741. [Google Scholar] [CrossRef]


| Breed | Age (ys) | BW (kg) | Smoke Exposure | Intensity | Pregnant | Litter Size |
|---|---|---|---|---|---|---|
| Ambully | 2 | 28.3 | NEp | yes | 5 | |
| Bouledogue | 2 | 17.65 | NEp | yes | 8 | |
| Bernese Mountain D. | 4.5 | 63.6 | NEp | yes | 3 | |
| German Shepherd | 8 | 30.5 | NEp | yes | 4 | |
| Kurzhaar | 5 | 33 | NEp | yes | 2 | |
| Staffordshire Bull T. | 2 | 14 | NEp | yes | 6 | |
| Bernese Mountain D. | 2 | 45.9 | EXp | + | yes | 8 |
| Basset-hound | 2 | 31.5 | EXp | ++ | yes | 8 |
| Basset-hound | 4.5 | 32.3 | EXp | ++ | yes | 3 |
| Entlebucher Mountain D. | 4.5 | 27.5 | EXp | + | yes | 3 |
| Bernese Mountain D. | 3.5 | 48 | EXp | + | yes | 8 |
| Bernese Mountain D. | 3 | 54.7 | EXp | + | yes | 3 |
| Basset-hound | 6 | 23 | EXnp | ++ | no | |
| Basset-hound | 3.5 | 24 | EXnp | ++ | no | |
| Basset-hound | 1.5 | 21 | EXnp | ++ | no | |
| Basset-hound | 2 | 28 | EXnp | + | no | |
| Mongrel | 12 | 15 | EXnp | ++ | no | |
| Mongrel | 11 | 30 | EXnp | ++ | no |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pizzi, G.; Mazzola, S.M.; Pecile, A.; Bronzo, V.; Groppetti, D. Tobacco Smoke Exposure in Pregnant Dogs: Maternal and Newborn Cotinine Levels: A Pilot Study. Vet. Sci. 2023, 10, 321. https://doi.org/10.3390/vetsci10050321
Pizzi G, Mazzola SM, Pecile A, Bronzo V, Groppetti D. Tobacco Smoke Exposure in Pregnant Dogs: Maternal and Newborn Cotinine Levels: A Pilot Study. Veterinary Sciences. 2023; 10(5):321. https://doi.org/10.3390/vetsci10050321
Chicago/Turabian StylePizzi, Giulia, Silvia Michela Mazzola, Alessandro Pecile, Valerio Bronzo, and Debora Groppetti. 2023. "Tobacco Smoke Exposure in Pregnant Dogs: Maternal and Newborn Cotinine Levels: A Pilot Study" Veterinary Sciences 10, no. 5: 321. https://doi.org/10.3390/vetsci10050321
APA StylePizzi, G., Mazzola, S. M., Pecile, A., Bronzo, V., & Groppetti, D. (2023). Tobacco Smoke Exposure in Pregnant Dogs: Maternal and Newborn Cotinine Levels: A Pilot Study. Veterinary Sciences, 10(5), 321. https://doi.org/10.3390/vetsci10050321







