Porcine Reproductive and Respiratory Syndrome Virus Engineered by Serine Substitution on the 44th Amino Acid of GP5 Resulted in a Potential Vaccine Candidate with the Ability to Produce High Levels of Neutralizing Antibody
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells, Viruses and Plasmids
2.2. Generation of the Tentative Hypoglycosylated Mutant Virus
2.3. Indirect Immunofluorescence Assay (IFA)
2.4. Growth Kinetics
2.5. Animal Experiments
2.6. RT-PCR and Sequencing Analysis
2.7. RNA Extraction and RT-qPCR
2.8. ELISA
2.9. Pathological Analysis
2.10. Serum Neutralization Test
2.11. Statistical Analysis
3. Results
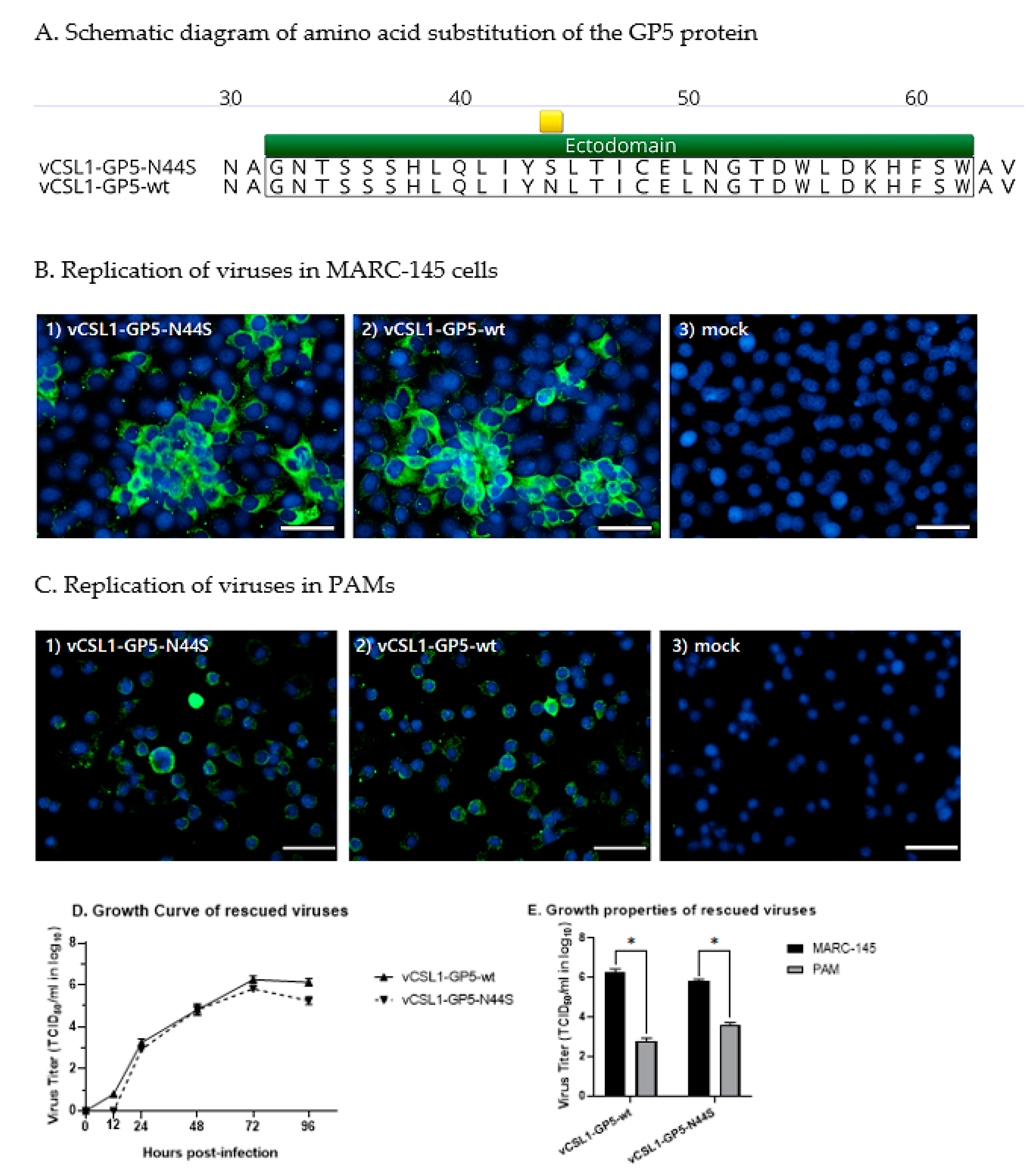
3.1. Tentative Hypoglycosylated Mutations and Virus Rescue
3.2. Characteristics of Tentative Hypoglycosylated Viruses
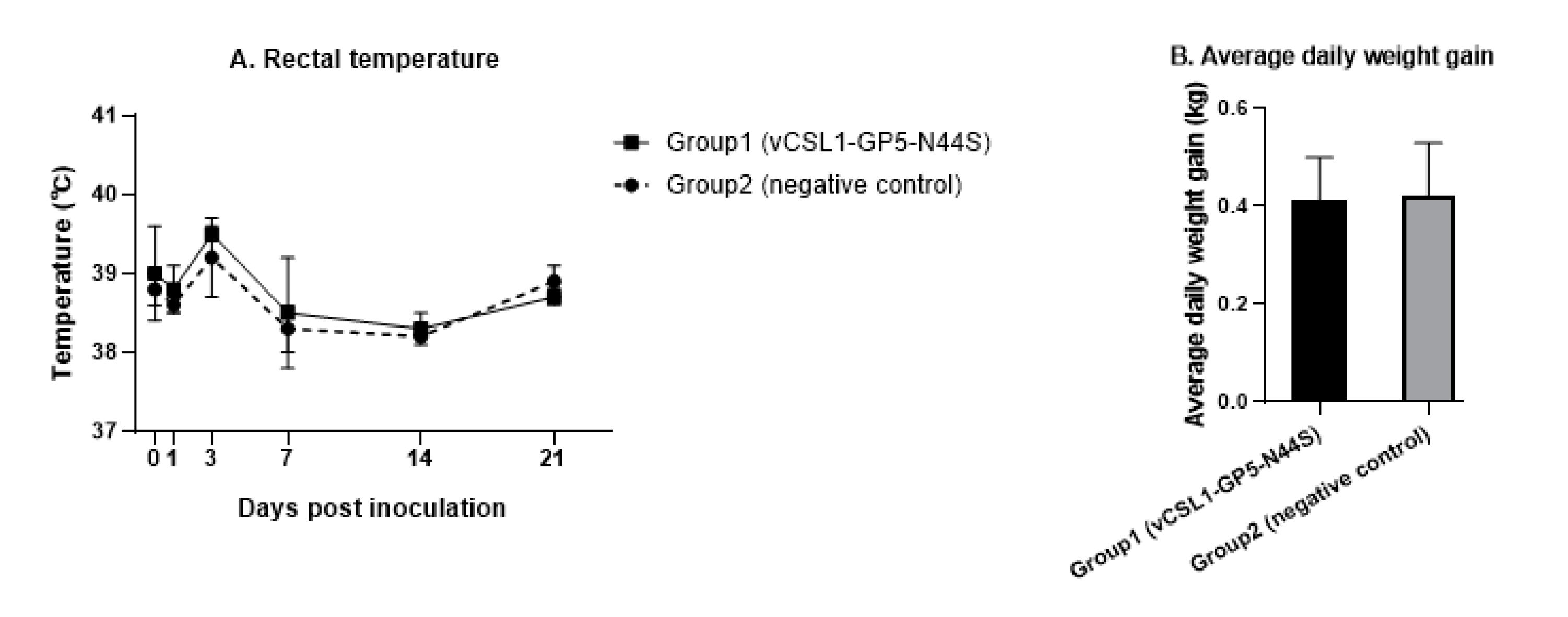
3.3. Pathogenicity and Safety Assessment of Tentative Hypoglycosylated Viruses
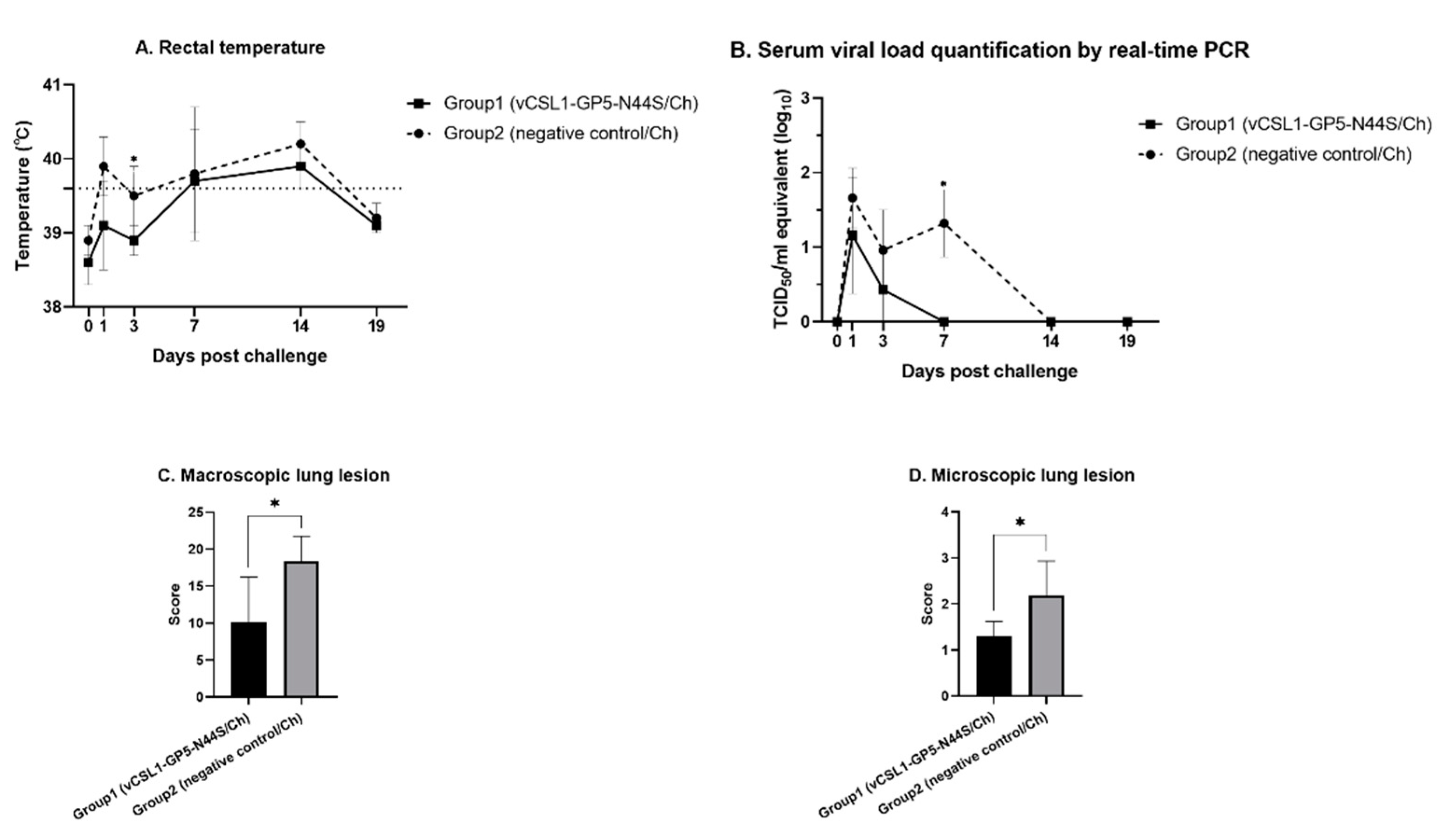
3.4. Evaluation of the Protective Efficacy of Tentative Hypoglycosylated Viruses
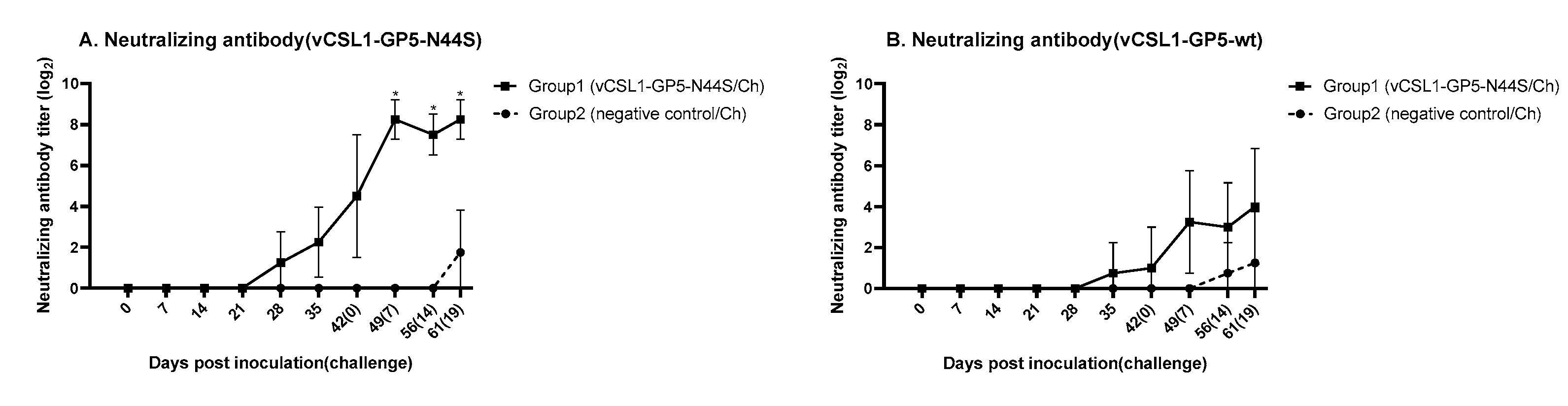
3.5. Neutralizing Antibody Measurement
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mardassi, H.; Mounir, S.; Dea, S. Identification of major differences in the nucleocapsid protein genes of a Quebec strain and European strains of porcine reproductive and respiratory syndrome virus. J. Gen. Virol. 1994, 75, 681–685. [Google Scholar] [CrossRef]
- Beura, L.K.; Sarkar, S.N.; Kwon, B.; Subramaniam, S.; Jones, C.; Pattnaik, A.K.; Osorio, F.A. Porcine Reproductive and Respiratory Syndrome Virus Nonstructural Protein 1β Modulates Host Innate Immune Response by Antagonizing IRF3 Activation. J. Virol. 2010, 84, 1574–1584. [Google Scholar] [CrossRef]
- Holtkamp, D.J.; Kliebenstein, J.B.; Neumann, E.J.; Zimmerman, J.J.; Rotto, H.F.; Yoder, T.K.; Wang, C.; Yeske, P.E.; Mowrer, C.L.; Haley, C.A. Assessment of the Economic Impact of Porcine Reproductive and Respiratory Syndrome Virus on United States Pork Producers. J. Swine Health Prod. 2013, 21, 72–84. [Google Scholar]
- Renken, C.; Nathues, C.; Swam, H.; Fiebig, K.; Weiss, C.; Eddicks, M.; Ritzmann, M.; Nathues, H. Application of an economic calculator to determine the cost of porcine reproductive and respiratory syndrome at farm-level in 21 pig herds in Germany. Porc. Health Manag. 2021, 7, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Charerntantanakul, W. Porcine reproductive and respiratory syndrome virus vaccines: Immunogenicity, efficacy and safety aspects. World J. Virol. 2012, 1, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Vu, H.L.; Pattnaik, A.K.; Osorio, F.A. Strategies to broaden the cross-protective efficacy of vaccines against porcine reproductive and respiratory syndrome virus. Vet. Microbiol. 2017, 206, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Zuckermann, F.A.; Garcia, E.A.; Luque, I.D.; Christopher-Hennings, J.; Doster, A.; Brito, M.; Osorio, F. Assessment of the efficacy of commercial porcine reproductive and respiratory syndrome virus (PRRSV) vaccines based on measurement of serologic response, frequency of gamma-IFN-producing cells and virological parameters of protection upon challenge. Vet. Microbiol. 2007, 123, 69–85. [Google Scholar] [CrossRef]
- Choi, H.-Y.; Kim, M.-S.; Kang, Y.-L.; Choi, J.-C.; Choi, I.-Y.; Jung, S.-W.; Jeong, J.-Y.; Kim, M.-C.; Hwang, S.-S.; Lee, S.-W.; et al. Development of a Chimeric Porcine Reproductive and Respiratory Syndrome Virus (PRRSV)-2 Vaccine Candidate Expressing Hypo-Glycosylated Glycoprotein-5 Ectodomain of Korean Lineage-1 Strain. Vet. Sci. 2022, 9, 165. [Google Scholar] [CrossRef]
- Wang, X.; Marthaler, D.; Rovira, A.; Rossow, S.; Murtaugh, M.P. Emergence of a virulent porcine reproductive and respiratory syndrome virus in vaccinated herds in the United States. Virus Res. 2015, 210, 34–41. [Google Scholar] [CrossRef]
- Rock, D.L. Report: Colloquium on Prospects for Development of an Effective PRRS Virus Vaccine; American Association of Swine Veterinarians: Perry, IA, USA, 2007. [Google Scholar]
- Kang, H.; Yu, J.E.; Shin, J.-E.; Kang, A.; Kim, W.-I.; Lee, C.; Lee, J.; Cho, I.-S.; Choe, S.-E.; Cha, S.-H. Geographic distribution and molecular analysis of porcine reproductive and respiratory syndrome viruses circulating in swine farms in the Republic of Korea between 2013 and 2016. BMC Vet. Res. 2018, 14, 160. [Google Scholar] [CrossRef]
- Neumann, E.J.; Kliebenstein, J.B.; Johnson, C.D.; Mabry, J.W.; Bush, E.J.; Seitzinger, A.H.; Green, A.L.; Zimmerman, J.J. Assessment of the economic impact of porcine reproductive and respiratory syndrome on swine production in the United States. J. Am. Vet. Med. Assoc. 2005, 227, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Allende, R.; Kutish, G.F.; Laegreid, W.; Lu, Z.; Lewis, T.L.; Rock, D.L.; Friesen, J.; Galeota, J.A.; Doster, A.R.; Osorio, F.A. Mutations in the genome of porcine reproductive and respiratory syndrome virus responsible for the attenuation phenotype. Arch. Virol. 2000, 145, 1149–1161. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Choi, S.; Jeon, J.H.; Lee, K.-W.; Lee, C. Novel lineage 1 recombinants of porcine reproductive and respiratory syndrome virus isolated from vaccinated herds: Genome sequences and cytokine production profiles. Arch. Virol. 2020, 165, 2259–2277. [Google Scholar] [CrossRef]
- Mateu, E.; Diaz, I. The challenge of PRRS immunology. Vet. J. 2008, 177, 345–351. [Google Scholar] [CrossRef]
- Lunney, J.K.; Fang, Y.; Ladinig, A.; Chen, N.; Li, Y.; Rowland, B.; Renukaradhya, G.J. Porcine Reproductive and Respiratory Syndrome Virus (PRRSV): Pathogenesis and Interaction with the Immune System. Annu. Rev. Anim. Biosci. 2016, 4, 129–154. [Google Scholar] [CrossRef] [PubMed]
- Das, P.B.; Dinh, P.X.; Ansari, I.H.; de Lima, M.; Osorio, F.A.; Pattnaik, A.K. The Minor Envelope Glycoproteins GP2a and GP4 of Porcine Reproductive and Respiratory Syndrome Virus Interact with the Receptor CD163. J. Virol. 2010, 84, 1731–1740. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, S.; Qiu, M.; Li, X.; Li, C.; Feng, B.; Lin, H.; Zheng, W.; Zhu, J.; Chen, N. Minor and major envelope proteins of PRRSV play synergistic roles in inducing heterologous neutralizing antibodies and conferring cross protection. Virus Res. 2022, 315, 198789. [Google Scholar] [CrossRef]
- Dokland, T. The structural biology of PRRSV. Virus Res. 2010, 154, 86–97. [Google Scholar] [CrossRef]
- Ansari, I.H.; Kwon, B.; Osorio, F.A.; Pattnaik, A.K. Influence of N-Linked Glycosylation of Porcine Reproductive and Respiratory Syndrome Virus GP5 on Virus Infectivity, Antigenicity, and Ability To Induce Neutralizing Antibodies. J. Virol. 2006, 80, 3994–4004. [Google Scholar] [CrossRef]
- Vu, H.L.X.; Kwon, B.; Yoon, K.-J.; Laegreid, W.W.; Pattnaik, A.K.; Osorio, F.A. Immune Evasion of Porcine Reproductive and Respiratory Syndrome Virus through Glycan Shielding Involves both Glycoprotein 5 as Well as Glycoprotein 3. J. Virol. 2011, 85, 5555–5564. [Google Scholar] [CrossRef]
- Kappes, M.A.; Faaberg, K.S. PRRSV structure, replication and recombination: Origin of phenotype and genotype diversity. Virology 2015, 479-480, 475–486. [Google Scholar] [CrossRef]
- Kim, J.-J.; Lee, J.-A.; Choi, H.-Y.; Han, J.-H.; Huh, W.; Pi, J.-H.; Park, S.; Cho, K.-H.; Lee, J.-B. In vitro and in vivo studies of deglycosylated chimeric porcine reproductive and respiratory syndrome virus as a vaccine candidate and its realistic revenue impact at commercial pig production level. Vaccine 2017, 35, 4966–4973. [Google Scholar] [CrossRef] [PubMed]
- Wei, Z.; Lin, T.; Sun, L.; Li, Y.; Wang, X.; Gao, F.; Liu, R.; Chen, C.; Tong, G.; Yuan, S. N-Linked Glycosylation of GP5 of Porcine Reproductive and Respiratory Syndrome Virus Is Critically Important for Virus Replication In Vivo. J. Virol. 2012, 86, 9941–9951. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.-Y.; Lee, S.-H.; Ahn, S.-H.; Choi, J.-C.; Jeong, J.-Y.; Lee, B.-J.; Kang, Y.-L.; Hwang, S.-S.; Lee, J.-K.; Lee, S.-W.; et al. A chimeric porcine reproductive and respiratory syndrome virus (PRRSV)-2 vaccine is safe under international guidelines and effective both in experimental and field conditions. Res. Vet. Sci. 2021, 135, 143–152. [Google Scholar] [CrossRef]
- Lee, J.-A.; Lee, N.-H.; Lee, J.-B.; Park, S.-Y.; Song, C.-S.; Choi, I.-S.; Lee, S.-W. Augmented immune responses in pigs immunized with an inactivated porcine reproductive and respiratory syndrome virus containing the deglycosylated glycoprotein 5 under field conditions. Clin. Exp. Vaccine Res. 2016, 5, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Kwang, J.; Yoon, I.J.; Joo, H.S.; Frey, M.L. Enhanced replication of porcine reproductive and respiratory syndrome (PRRS) virus in a homogeneous subpopulation of MA-104 cell line. Arch. Virol. 1993, 133, 477–483. [Google Scholar] [CrossRef]
- Zhang, H.-L.; Tang, Y.-D.; Liu, C.-X.; Xiang, L.-R.; Zhang, W.-L.; Leng, C.-L.; Wang, Q.; An, T.-Q.; Peng, J.-M.; Tian, Z.-J.; et al. Adaptions of field PRRSVs in Marc-145 cells were determined by variations in the minor envelope proteins GP2a-GP3. Vet. Microbiol. 2018, 222, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Novoradovsky, A.; Zhang, V.; Ghosh, M.; Hogrefe, H.; Sorge, J.A.; Gaasterland, T. Computational Principles of Primer Design for Site Directed Mutagenesis. TechConnect Briefs 2005, 1, 532–535. [Google Scholar]
- Jeeva, S.; Lee, J.-A.; Park, S.-Y.; Song, C.-S.; Choi, I.-S.; Lee, J.-B. Development of porcine respiratory and reproductive syndrome virus replicon vector for foot-and-mouth disease vaccine. Clin. Exp. Vaccine Res. 2014, 3, 100–109. [Google Scholar] [CrossRef]
- Vieyres, G.; Pietschmann, T. Entry and replication of recombinant hepatitis C viruses in cell culture. Methods 2013, 59, 233–248. [Google Scholar] [CrossRef]
- Charan, J.; Kantharia, N.D. How to calculate sample size in animal studies? J. Pharmacol. Pharmacother. 2013, 4, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Choi, K.; Jeong, J.; Chae, C. Cross-protection of a new type 2 porcine reproductive and respiratory syndrome virus (PRRSV) modified live vaccine (Fostera PRRS) against heterologous type 1 PRRSV challenge in growing pigs. Vet. Microbiol. 2015, 177, 87–94. [Google Scholar] [CrossRef]
- Kleiboeker, S.B.; Schommer, S.K.; Lee, S.-M.; Watkins, S.; Chittick, W.; Polson, D. Simultaneous Detection of North American and European Porcine Reproductive and Respiratory Syndrome Virus Using Real-Time Quantitative Reverse Transcriptase–PCR. J. Vet. Diagn. Investig. 2005, 17, 165–170. [Google Scholar] [CrossRef]
- Wernike, K.; Hoffmann, B.; Dauber, M.; Lange, E.; Schirrmeier, H.; Beer, M. Detection and Typing of Highly Pathogenic Porcine Reproductive and Respiratory Syndrome Virus by Multiplex Real-Time RT-PCR. PLoS ONE 2012, 7, e38251. [Google Scholar] [CrossRef] [PubMed]
- Wernike, K.; Bonilauri, P.; Dauber, M.; Errington, J.; Leblanc, N.; Revilla-Fernández, S.; Hjulsager, C.K.; Isaksson, M.; Stadejek, T.; Beer, M.; et al. Porcine Reproductive and Respiratory Syndrome Virus: Interlaboratory Ring Trial to Evaluate Real-Time Reverse Transcription Polymerase Chain Reaction Detection Methods. J. Vet. Diagn. Investig. 2012, 24, 855–866. [Google Scholar] [CrossRef]
- Halbur, P.G.; Paul, P.S.; Frey, M.L.; Landgraf, J.; Eernisse, K.; Meng, X.-J.; Lum, M.A.; Andrews, J.J.; Rathje, J.A. Comparison of the Pathogenicity of Two US Porcine Reproductive and Respiratory Syndrome Virus Isolates with that of the Lelystad Virus. Vet. Pathol. 1995, 32, 648–660. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-A.; Lee, N.-H.; Lee, S.-W.; Park, S.-Y.; Song, C.-S.; Choi, I.-S.; Lee, J.-B. Development of a chimeric strain of porcine reproductive and respiratory syndrome virus with an infectious clone and a Korean dominant field strain. J. Microbiol. 2014, 52, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Vu, H.L.X.; Ma, F.; Laegreid, W.W.; Pattnaik, A.K.; Steffen, D.; Doster, A.R.; Osorio, F.A. A Synthetic Porcine Reproductive and Respiratory Syndrome Virus Strain Confers Unprecedented Levels of Heterologous Protection. J. Virol. 2015, 89, 12070–12083. [Google Scholar] [CrossRef]
- Evenson, D.; Gerber, P.; Xiao, C.; Halbur, P.; Wang, C.; Tian, D.; Ni, Y.; Meng, X.; Opriessnig, T. A porcine reproductive and respiratory syndrome virus candidate vaccine based on the synthetic attenuated virus engineering approach is attenuated and effective in protecting against homologous virus challenge. Vaccine 2016, 34, 5546–5553. [Google Scholar] [CrossRef]
- Meier, W.A.; Galeota, J.; Osorio, F.A.; Husmann, R.J.; Schnitzlein, W.M.; Zuckermann, F.A. Gradual development of the interferon-γ response of swine to porcine reproductive and respiratory syndrome virus infection or vaccination. Virology 2003, 309, 18–31. [Google Scholar] [CrossRef]
- Lopez, O.J.; Oliveira, M.F.; Garcia, E.A.; Kwon, B.J.; Doster, A.; Osorio, F.A. Protection against Porcine Reproductive and Respiratory Syndrome Virus (PRRSV) Infection through Passive Transfer of PRRSV-Neutralizing Antibodies Is Dose Dependent. Clin. Vaccine Immunol. 2007, 14, 269–275. [Google Scholar] [CrossRef]
- Jeong, C.-G.; Khatun, A.; Nazki, S.; Kim, S.-C.; Noh, Y.-H.; Kang, S.-C.; Lee, D.-U.; Yang, M.-S.; Shabir, N.; Yoon, I.-J.; et al. Evaluation of the Cross-Protective Efficacy of a Chimeric PRRSV Vaccine against Two Genetically Diverse PRRSV2 Field Strains in a Reproductive Model. Vaccines 2021, 9, 1258. [Google Scholar] [CrossRef]
- Shabir, N.; Khatun, A.; Nazki, S.; Kim, B.; Choi, E.-J.; Sun, D.; Yoon, K.-J.; Kim, W.-I. Evaluation of the Cross-Protective Efficacy of a Chimeric Porcine Reproductive and Respiratory Syndrome Virus Constructed Based on Two Field Strains. Viruses 2016, 8, 240. [Google Scholar] [CrossRef]
- Park, C.; Baek, J.H.; Cho, S.H.; Jeong, J.; Chae, C.; You, S.-H.; Cha, S.-H. Field porcine reproductive and respiratory syndrome viruses (PRRSV) attenuated by codon pair deoptimization (CPD) in NSP1 protected pigs from heterologous challenge. Virology 2020, 540, 172–183. [Google Scholar] [CrossRef]
- Velazquez-Salinas, L.; Pauszek, S.J.; Holinka, L.G.; Gladue, D.P.; Rekant, S.I.; Bishop, E.A.; Stenfeldt, C.; Verdugo-Rodriguez, A.; Borca, M.V.; Arzt, J.; et al. A Single Amino Acid Substitution in the Matrix Protein (M51R) of Vesicular Stomatitis New Jersey Virus Impairs Replication in Cultured Porcine Macrophages and Results in Significant Attenuation in Pigs. Front. Microbiol. 2020, 11, 1123. [Google Scholar] [CrossRef]
- Rahe, M.C.; Murtaugh, M.P. Mechanisms of Adaptive Immunity to Porcine Reproductive and Respiratory Syndrome Virus. Viruses 2017, 9, 148. [Google Scholar] [CrossRef] [PubMed]
- Razzuoli, E.; Armando, F.; De Paolis, L.; Ciurkiewicz, M.; Amadori, M. The Swine IFN System in Viral Infections: Major Advances and Translational Prospects. Pathogens 2022, 11, 175. [Google Scholar] [CrossRef]
- Fontanella, E.; Ma, Z.; Zhang, Y.; de Castro, A.M.; Shen, H.; Halbur, P.G.; Opriessnig, T. An interferon inducing porcine reproductive and respiratory syndrome virus vaccine candidate elicits protection against challenge with the heterologous virulent type 2 strain VR-2385 in pigs. Vaccine 2017, 35, 125–131. [Google Scholar] [CrossRef]
- Sun, H.; Workman, A.; Osorio, F.A.; Steffen, D.; Vu, H.L. Development of a broadly protective modified-live virus vaccine candidate against porcine reproductive and respiratory syndrome virus. Vaccine 2018, 36, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Fang, L.; Xu, Z.; Liu, S.; Gao, J.; Jiang, Y.; Chen, H.; Xiao, S. Recombination in Vaccine and Circulating Strains of Porcine Reproductive and Respiratory Syndrome Viruses. Emerg. Infect. Dis. 2009, 15, 2032–2035. [Google Scholar] [CrossRef] [PubMed]
- Prickett, J.; Simer, R.; Christopher-Hennings, J.; Yoon, K.-J.; Evans, R.B.; Zimmerman, J.J. Detection of Porcine Reproductive and Respiratory Syndrome Virus Infection in Porcine Oral Fluid Samples: A Longitudinal Study under Experimental Conditions. J. Vet. Diagn. Investig. 2008, 20, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Pileri, E.; Mateu, E. Review on the transmission porcine reproductive and respiratory syndrome virus between pigs and farms and impact on vaccination. Vet. Res. 2016, 47, 1–13. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.-C.; Kim, M.-S.; Choi, H.-Y.; Kang, Y.-L.; Choi, I.-Y.; Jung, S.-W.; Jeong, J.-Y.; Kim, M.-C.; Cho, A.Y.; Lee, J.-H.; et al. Porcine Reproductive and Respiratory Syndrome Virus Engineered by Serine Substitution on the 44th Amino Acid of GP5 Resulted in a Potential Vaccine Candidate with the Ability to Produce High Levels of Neutralizing Antibody. Vet. Sci. 2023, 10, 191. https://doi.org/10.3390/vetsci10030191
Choi J-C, Kim M-S, Choi H-Y, Kang Y-L, Choi I-Y, Jung S-W, Jeong J-Y, Kim M-C, Cho AY, Lee J-H, et al. Porcine Reproductive and Respiratory Syndrome Virus Engineered by Serine Substitution on the 44th Amino Acid of GP5 Resulted in a Potential Vaccine Candidate with the Ability to Produce High Levels of Neutralizing Antibody. Veterinary Sciences. 2023; 10(3):191. https://doi.org/10.3390/vetsci10030191
Chicago/Turabian StyleChoi, Jong-Chul, Min-Sik Kim, Hwi-Yeon Choi, Yeong-Lim Kang, In-Yeong Choi, Sung-Won Jung, Ji-Yun Jeong, Min-Chul Kim, Andrew Y. Cho, Ji-Ho Lee, and et al. 2023. "Porcine Reproductive and Respiratory Syndrome Virus Engineered by Serine Substitution on the 44th Amino Acid of GP5 Resulted in a Potential Vaccine Candidate with the Ability to Produce High Levels of Neutralizing Antibody" Veterinary Sciences 10, no. 3: 191. https://doi.org/10.3390/vetsci10030191
APA StyleChoi, J.-C., Kim, M.-S., Choi, H.-Y., Kang, Y.-L., Choi, I.-Y., Jung, S.-W., Jeong, J.-Y., Kim, M.-C., Cho, A. Y., Lee, J.-H., Lee, D.-H., Lee, S.-W., Park, S.-Y., Song, C.-S., Choi, I.-S., & Lee, J.-B. (2023). Porcine Reproductive and Respiratory Syndrome Virus Engineered by Serine Substitution on the 44th Amino Acid of GP5 Resulted in a Potential Vaccine Candidate with the Ability to Produce High Levels of Neutralizing Antibody. Veterinary Sciences, 10(3), 191. https://doi.org/10.3390/vetsci10030191






