Effect of Injectable Platelet-Rich Fibrin with a Nano-Hydroxyapatite Bone Graft on the Treatment of a Grade II Furcation Defect
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
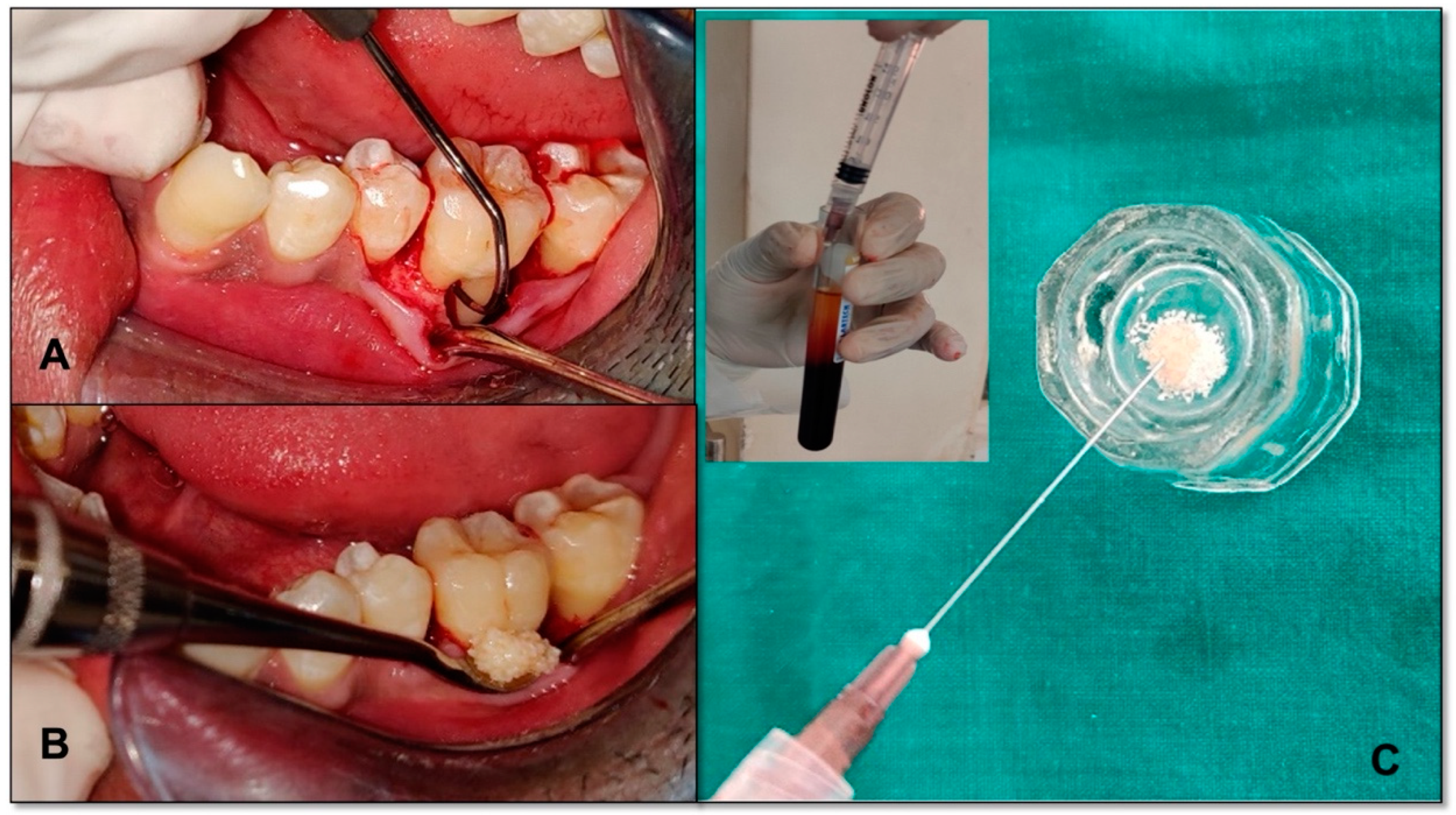
2.2. I-Prf Preparation Method
2.3. Surgical Procedure
2.4. Statistical Analysis
3. Results
3.1. Plaque Index (Pi)
3.2. Gingival Index
3.3. Pocket Probing Depth
3.4. Clinical Attachment Level
3.5. Horizontal Probing Depth
3.6. Vertical Probing Depth
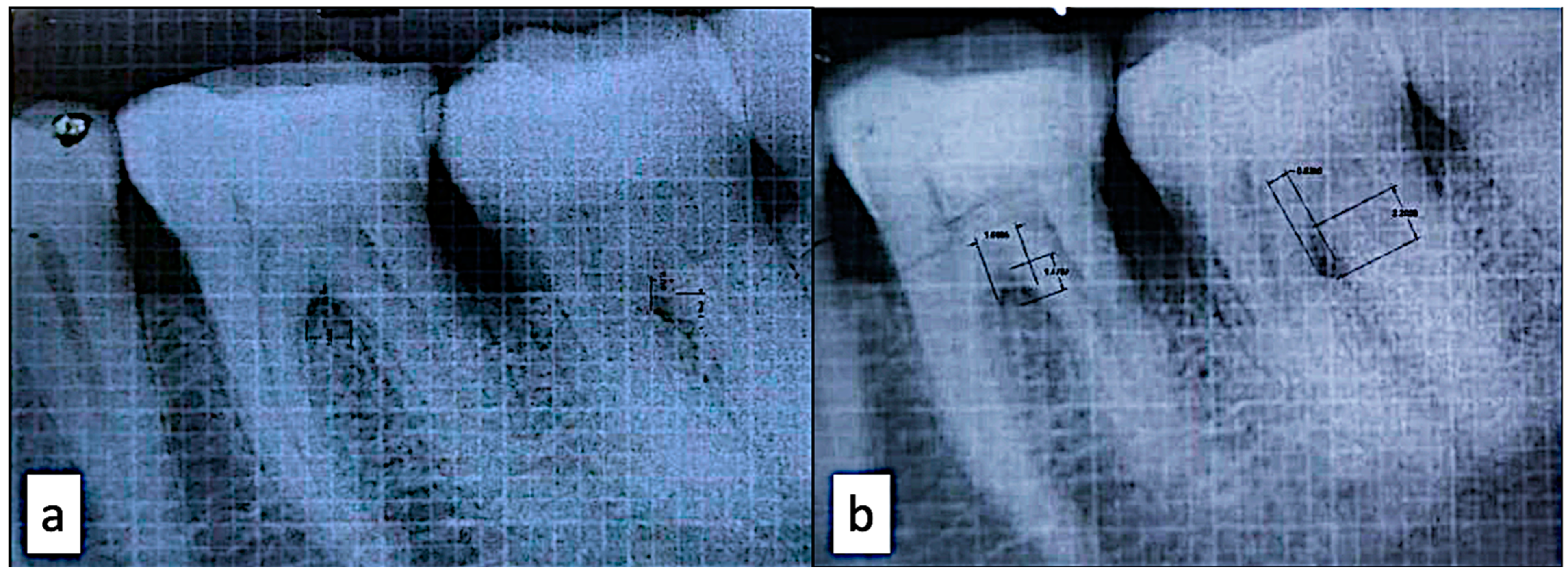
3.7. Bone Area Fill
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Panda, S.; Karanxha, L.; Goker, F.; Satpathy, A.; Taschieri, S.; Francetti, L.; Das, A.C.; Kumar, M.; Panda, S.; Del Fabbro, M. Autologous Platelet Concentrates in Treatment of Furcation Defects—A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2019, 20, 1347. [Google Scholar] [CrossRef] [PubMed]
- Dahiya, P.; Kamal, R.; Gupta, R.; Bhardwaj, R.; Chaudhary, K.; Kaur, S. Reactive oxygen species in periodontitis. J. Indian Soc. Periodontol. 2013, 17, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Martu, M.-A.; Surlin, P.; Lazar, L.; Maftei, G.; Luchian, I.; Gheorghe, D.-N.; Rezus, E.; Toma, V.; Foia, L.-G. Evaluation of Oxidative Stress before and after Using Laser and Photoactivation Therapy as Adjuvant of Non-Surgical Periodontal Treatment in Patients with Rheumatoid Arthritis. Antioxidants 2021, 10, 226. [Google Scholar] [CrossRef] [PubMed]
- Anton, D.-M.; Martu, M.-A.; Maris, M.; Maftei, G.-A.; Sufaru, I.-G.; Tatarciuc, D.; Luchian, I.; Ioanid, N.; Martu, S. Study on the Effects of Melatonin on Glycemic Control and Periodontal Parameters in Patients with Type II Diabetes Mellitus and Periodontal Disease. Medicina 2021, 57, 140. [Google Scholar] [CrossRef]
- Cianetti, S.; Abraha, I.; Pagano, S.; Lupatelli, E.; Lombardo, G. Sonic and ultrasonic oscillating devices for the management of pain and dental fear in children or adolescents that require caries removal: A systematic review. BMJ Open 2018, 8, e020840. [Google Scholar] [CrossRef]
- Chitsazi, M.T.; Shirmohammadi, A.; Faramarzie, M.; Pourabbas, R.; Rostamzadeh, A.n. A clinical comparison of nano-crystalline hydroxyapatite (Ostim) and autogenous bone graft in the treatment of periodontal intrabony defects. Med. Oral Patol. Oral Cir. Bucal 2011, 16, e448–e453. [Google Scholar] [CrossRef]
- Murphy, K.G.; Gunsolley, J.C. Guided tissue regeneration for the treatment of periodontal intrabony and furcation defects. A systematic review. Ann. Periodontol. 2003, 8, 266–302. [Google Scholar] [CrossRef]
- Machtei, E.E.; Oettinger-Barak, O.; Peled, M. Guided tissue regeneration in smokers: Effect of aggressive anti-infective therapy in Class II furcation defects. J Periodontol. 2003, 74, 579–584. [Google Scholar] [CrossRef]
- Mlachkova, A.; Panova, V.D.; Popova, C. Application of PRP (platelet-rich plasma) in surgical periodontal therapy: Overview. Biotechnol. Biotechnol. Equip. 2021, 35, 586–592. [Google Scholar] [CrossRef]
- Mohan, S.P.; Jaishangar, N.; Devy, S.; Narayanan, A.; Cherian, D.; Madhavan, S.S. Platelet-Rich Plasma and Platelet-Rich Fibrin in Periodontal Regeneration: A Review. J. Pharm. Bioallied Sci. 2019, 11, S126–S130. [Google Scholar] [CrossRef]
- Feigin, K.; Shope, B. Use of Platelet-Rich Plasma and Platelet-Rich Fibrin in Dentistry and Oral Surgery: Introduction and Review of the Literature. J. Vet. Dent. 2019, 36, 109–123. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.A. Evolution, current status and advances in application of platelet concentrate in periodontics and implantology. World J. Clin. Cases 2017, 5, 159–171. [Google Scholar] [CrossRef]
- Mourão, C.F.; Valiense, H.; Melo, E.R.; Mourão, N.B.; Maia, M.D. Obtention of injectable platelets rich-fibrin (i-PRF) and its polymerization with bone graft: Technical note. Rev. Col. Bras. Cir. 2015, 42, 421–423. [Google Scholar] [CrossRef]
- Agarwal, A.; Gupta, N.D.; Jain, A. Platelet rich fibrin combined with decalcified freeze-dried bone allograft for the treatment of human intrabony periodontal defects: A randomized split mouth clinical trail. Acta Odontol. Scand. 2016, 74, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Glickman, I. Clinical Periodontology: Prevention, Diagnosis, and Treatment of Periodontal Disease in the Practice of General Dentistry, 4th ed.; Saunders: Philadelphia, PA, USA, 1972; pp. 242–245. [Google Scholar]
- Tarnow, D.; Fletcher, P. Classification of the vertical component of furcation involvement. J. Periodontol. 1984, 55, 283–284. [Google Scholar] [CrossRef] [PubMed]
- Nibali, L.; Sun, C.; Akcalı, A.; Yeh, Y.C.; Tu, Y.K.; Donos, N. The effect of horizontal and vertical furcation involvement on molar survival: A retrospective study. J. Clin. Periodontol. 2018, 45, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Martu, M.A.; Maftei, G.A.; Luchian, I.; Popa, C.; Filioreanu, A.M.; Tatarciuc, D.; Nichitean, G.; Hurjui, L.L.; Foia, L.G. Wound healing of periodontal and oral tissues: Part II—Patho-phisiological conditions and metabolic diseases. Rom. J. Oral Rehabil. 2020, 12, 30–40. [Google Scholar]
- Maftei, G.A.; Martu, C.M.; Popa, C.; Geletu, G.; Danila, V.; Jelihovschi, I.; Foia, L. The biomechanical properties of suture materials and their relationship to bacterial adherence. Mater. Plast. 2019, 56, 980–985. [Google Scholar] [CrossRef]
- Bordea, I.R.; Candrea, S.; Alexescu, G.T.; Bran, S.; Băciuț, M.; Băciuț, G.; Lucaciu, O.; Dinu, C.M.; Todea, D.A. Nano-hydroxyapatite use in dentistry: A systematic review. Drug Metab. Rev. 2020, 52, 319–332. [Google Scholar] [CrossRef]
- Singh, V.P.; Nayak, D.G.; Uppoor, A.S.; Shah, D. Clinical and radiographic evaluation of Nano-crystalline hydroxyapatite bone graft (Sybograf) in combination with bioresorbable collagen membrane (Periocol) in periodontal intrabony defects. Dent. Res. J. 2012, 9, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Sadowska, J.M.; Wei, F.; Guo, J.; Guillem-Marti, J.; Ginebra, M.P.; Xiao, Y. Effect of nano-structural properties of biomimetic hydroxyapatite on osteoimmunomodulation. Biomaterials 2018, 181, 318–332. [Google Scholar] [CrossRef] [PubMed]
- Mathur, A.; Bains, V.K.; Gupta, V.; Jhingran, R.; Singh, G.P. Evaluation of intrabony defects treated with platelet-rich fibrin or autogenous bone graft: A comparative analysis. Eur. J. Dent. 2015, 9, 100–108. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Edrees, M.; Maher, M.; Hassan, K. Platelet Rich Fibrin Combined with Nano Crystalline Hydroxyappatite in Treatment of Grade II Mandibular Furcation Defect. Al-Azhar Assiut Dent. J. 2019, 2, 85–91. [Google Scholar] [CrossRef]
- Pradeep, A.R.; Sharma, A. Autologous platelet rich fibrin in the treatment of mandibular Degree II furcation defects: A randomized clinical trial. J. Periodontol. 2011, 82, 1396–1403. [Google Scholar]
- Attia, A. Platelet-rich fibrin and nanocrystalline hydroxyapatite in treatment of periodontal class ii furcation defects: Clinical and radiographic study. Egypt. Dent. J. 2015, 61, 5049–5063. [Google Scholar]
- Elgendy, E.A.; Abo Shady, T.E. Clinical and radiographic evaluation of nanocrystalline hydroxyapatite with or without platelet-rich fibrin membrane in the treatment of periodontal intrabony defects. J. Indian Soc. Periodontol. 2015, 19, 61–65. [Google Scholar] [CrossRef]
- Siddiqui, Z.R.; Jhingran, R.; Bains, V.K.; Srivastava, R.; Madan, R.; Rizvi, I. Comparative evaluation of platelet-rich fibrin versus beta-tri-calcium phosphate in the treatment of Grade II mandibular furcation defects using cone-beam computed tomography. Eur. J. Dent. 2016, 10, 496–506. [Google Scholar] [CrossRef]
- Miron, R.J.; Fujioka-Kobayashi, M.; Hernandez, M.; Kandalam, U.; Zhang, Y.; Ghanaati, S.; Choukroun, J. Injectable platelet rich fibrin (i-PRF): Opportunities in regenerative dentistry? Clin. Oral Investig. 2017, 21, 2619–2627. [Google Scholar] [CrossRef]
- Drago, L.; Bortolin, M.; Vassena, C.; Taschieri, S.; Del Fabbro, M. Antimicrobial activity of pure platelet-rich plasma against microorganisms isolated from oral cavity. BMC Microbiol. 2013, 13, 47. [Google Scholar] [CrossRef]
- Blair, P.; Flaumenhaft, R. Platelet alpha-granules: Basic biology and clinical correlates. Blood Rev. 2009, 23, 177–189. [Google Scholar] [CrossRef]
- Ozsagir, Z.B.; Saglam, E.; Sen Yilmaz, B.; Choukroun, J.; Tunali, M. Injectable platelet-rich fibrin and microneedling for gingival augmentation in thin periodontal phenotype: A randomized controlled clinical trial. J. Clin. Periodontol. 2020, 47, 489–499. [Google Scholar] [CrossRef] [PubMed]
- Fotani, S.; Shiggaon, L.B.; Waghmare, A.; Kulkarni, G.; Agrawal, A.; Tekwani, R. Effect of injectable platelet rich fibrin (i-PRF) on thin gingival biotype: A clinical trial. J. Appl. Dent. Med. Sci. 2019, 5, 10–16. [Google Scholar]
- İzol, B.S.; Üner, D.D. A New Approach for Root Surface Biomodification Using Injectable Platelet-Rich Fibrin (i-PRF). Med. Sci. Monit. 2019, 25, 4744. [Google Scholar] [CrossRef] [PubMed]
- Vikhe, D.M.; Shah, S.V.; Carrion, J.B.; Palekar, U.G. Innovative method “DV-PIMS” technique and dental implant design for grafting injectable platelet-rich fibrin around the dental implant—Goat jaw cadaver study. Indian J. Dent. Res. 2019, 30, 450–454. [Google Scholar] [CrossRef]
- Kour, P.; Pudakalkatti, P.S.; Vas, A.M.; Das, S.; Padmanabhan, S. Comparative Evaluation of Antimicrobial Efficacy of Platelet-rich Plasma, Platelet-rich Fibrin, and Injectable Platelet-rich Fibrin on the Standard Strains of Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans. Contemp. Clin. Dent. 2018, 9, S325–S330. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, Y.; Choukroun, J.; Ghanaati, S.; Miron, R.J. Effects of an injectable platelet-rich fibrin on osteoblast behavior and bone tissue formation in comparison to platelet-rich plasma. Platelets 2018, 29, 48–55. [Google Scholar] [CrossRef]
- Kyyak, S.; Blatt, S.; Pabst, A.; Thiem, D.; Al-Nawas, B.; Kämmerer, P.W. Combination of an allogenic and a xenogenic bone substitute material with injectable platelet-rich fibrin—A comparative in vitro study. J. Biomater. Appl. 2020, 35, 83–96. [Google Scholar] [CrossRef]
- Raj, R.; Gayathri, G.V.; Shejali, J.; Vinayaka, A.M. Injectable platelet-rich fibrin-“a quicker therapeutic aid” in the treatment of combined endo-perio lesion: A case report. Int. J. Med. Dent. Case Rep. 2020, 7, 1–4. [Google Scholar] [CrossRef]
- Vučković, M.; Nikolić, N.; MilaКin, J.; Djordjević, V.; Milinković, I.; Asotić, J.; Jezdić, Z.; Janković, S.; Aleksić, Z. The effect of injectable platelet-rich fibrin uses in the initial treatment of chronic periodontitis. Srp. Arh. Celok. Lek. 2020, 148, 280–285. [Google Scholar] [CrossRef]
- Zhang, J.; Yin, C.; Zhao, Q.; Zhao, Z.; Wang, J.; Miron, R.J.; Zhang, Y. Anti-inflammation effects of injectable platelet-rich fibrin via macrophages and dendritic cells. J. Biomed. Mater. Res. A 2020, 108, 61–68. [Google Scholar] [CrossRef]
- Abd El Raouf, M.; Wang, X.; Miusi, S.; Chai, J.; Mohamed AbdEl-Aal, A.B.; Nefissa Helmy, M.M.; Ghanaati, S.; Choukroun, J.; Choukroun, E.; Zhang, Y.; et al. Injectable-platelet rich fibrin using the low speed centrifugation concept improves cartilage regeneration when compared to platelet-rich plasma. Platelets 2019, 30, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Han, T.; Zhu, H.; Tang, J.; Guo, Y.; Jin, Y.; Wang, Y.; Chen, G.; Gu, N.; Wang, C. Potential Osteoinductive Effects of Hydroxyapatite Nanoparticles on Mesenchymal Stem Cells by Endothelial Cell Interaction. Nanoscale Res. Lett. 2021, 16, 67. [Google Scholar] [CrossRef] [PubMed]
- Mu, Z.; He, Q.; Xin, L.; Li, Y.; Yuan, S.; Zou, H.; Shu, L.; Song, J.; Huang, Y.; Chen, T. Effects of injectable platelet rich fibrin on bone remodeling in combination with DBBM in maxillary sinus elevation: A randomized preclinical study. Am. J. Transl. Res. 2020, 12, 7312–7325. [Google Scholar] [PubMed]
| Groups * | N | Mean | Std. Deviation | Median | Male | Female |
|---|---|---|---|---|---|---|
| I | 12 | 37.5 | 9.62 | 34 | 6 | 6 |
| II | 12 | 33 | 4.20 | 33.5 | 6 | 6 |
| N | Mean | SD | p-Value | ||
|---|---|---|---|---|---|
| PI | Baseline–Test | 12 | 1.4050 | 0.2813 | 0.3899 |
| Baseline–Control | 12 | 1.2917 | 0.1275 | ||
| GI | Baseline–Test | 12 | 1.4550 | 0.2591 | 0.1595 |
| Baseline–Control | 12 | 1.2717 | 0.1419 | ||
| PPD | Baseline–Test | 12 | 6.0000 | 0.8944 | 0.4388 |
| Baseline–Control | 12 | 5.5000 | 1.2247 | ||
| CAL | Baseline–Test | 12 | 5.1667 | 0.7528 | 0.1306 |
| Baseline–Control | 12 | 3.8333 | 1.8349 | ||
| HPD | Baseline–Test | 12 | 4.0000 | 1.2649 | 0.6372 |
| Baseline–Control | 12 | 4.3333 | 1.0328 | ||
| VPD | Baseline–Test | 12 | 3.5000 | 0.5477 | 0.8339 |
| Baseline–Control | 12 | 3.3333 | 0.8165 |
| Group | Mean | Std. Deviation | N | Sig. | |
|---|---|---|---|---|---|
| PI_base | Test | 1.4050 | 0.28126 | 12 | 0.334 |
| Control | 1.2917 | 0.12750 | 12 | ||
| PI_3mon | Test | 1.0400 | 0.27554 | 12 | |
| Control | 1.0550 | 0.27304 | 12 | ||
| PI_6mon | Test | 0.6783 | 0.22912 | 12 | |
| Control | 0.8217 | 0.35005 | 12 | ||
| PI_9mon | Test | 0.4400 | 0.16982 | 12 | |
| Control | 0.5483 | 0.22807 | 12 | ||
| GI_base | Test | 1.4550 | 0.25906 | 12 | 0.140 |
| Control | 1.2717 | 0.14190 | 12 | ||
| GI_3mon | Test | 1.0983 | 0.19062 | 12 | |
| Control | 1.0433 | 0.27732 | 12 | ||
| GI_6mon | Test | 0.7633 | 0.14348 | 12 | |
| Control | 0.7950 | 0.32415 | 12 | ||
| GI_9mon | Test | 0.3233 | 0.15042 | 12 | |
| Control | 0.5783 | 0.32109 | 12 | ||
| PPD_base | Test | 6.0000 | 0.89443 | 12 | 0.008 * |
| Control | 5.5000 | 1.22474 | 12 | ||
| PPD_3mon | Test | 4.0000 | 1.09545 | 12 | |
| Control | 3.8333 | 1.32916 | 12 | ||
| PPD_6mon | Test | 2.0000 | 0.00000 | 12 | |
| Control | 3.0000 | 0.89443 | 12 | ||
| PPD_9mon | Test | 1.3333 | 0.51640 | 12 | |
| Control | 2.1667 | 0.40825 | 12 | ||
| CAL_base | Test | 5.1667 | 0.75277 | 12 | 0.001 * |
| Control | 3.8333 | 1.83485 | 12 | ||
| CAL_3mon | Test | 3.1667 | 0.98319 | 12 | |
| Control | 3.1667 | 1.32916 | 12 | ||
| CAL_6mon | Test | 1.0000 | 0.00000 | 12 | |
| Control | 2.3333 | 0.81650 | 12 | ||
| CAL_9mon | Test | 1.0000 | 0.00000 | 12 | |
| Control | 1.3333 | 0.51640 | 12 | ||
| HPD_base | Test | 4.0000 | 1.26491 | 12 | 0.012 * |
| Control | 4.3333 | 1.03280 | 12 | ||
| HPD_3mon | Test | 3.3333 | 1.50555 | 12 | |
| Control | 4.0000 | 1.26491 | 12 | ||
| HPD_6mon | Test | 1.3333 | 0.81650 | 12 | |
| Control | 3.1667 | 1.32916 | 12 | ||
| HPD_9mon | Test | 0.6667 | 0.51640 | 12 | |
| Control | 2.6667 | 1.21106 | 12 | ||
| VPD_base | Test | 3.5000 | 0.54772 | 12 | 0.000 * |
| Control | 3.3333 | 0.81650 | 12 | ||
| VPD_3mon | Test | 3.1667 | 0.75277 | 12 | |
| Control | 3.0000 | 1.09545 | 12 | ||
| VPD_6mon | Test | 1.1667 | 0.40825 | 12 | |
| Control | 2.5000 | 0.83666 | 12 | ||
| VPD_9mon | Test | 0.6667 | 0.51640 | 12 | |
| Control | 2.0000 | 0.63246 | 12 | ||
| baf_base | Test | 2.9167 | 0.88863 | 12 | 0.000 * |
| Control | 3.4000 | 1.39857 | 12 | ||
| baf_9m | Test | 5.6833 | 1.10529 | 12 | |
| Control | 3.9833 | 1.40060 | 12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nair, U.P.; Shivamurthy, R.; Nagate, R.R.; Chaturvedi, S.; Al-Qahtani, S.M.; Magbol, M.A.; Gokhale, S.T.; Tikare, S.; Chaturvedi, M. Effect of Injectable Platelet-Rich Fibrin with a Nano-Hydroxyapatite Bone Graft on the Treatment of a Grade II Furcation Defect. Bioengineering 2022, 9, 602. https://doi.org/10.3390/bioengineering9110602
Nair UP, Shivamurthy R, Nagate RR, Chaturvedi S, Al-Qahtani SM, Magbol MA, Gokhale ST, Tikare S, Chaturvedi M. Effect of Injectable Platelet-Rich Fibrin with a Nano-Hydroxyapatite Bone Graft on the Treatment of a Grade II Furcation Defect. Bioengineering. 2022; 9(11):602. https://doi.org/10.3390/bioengineering9110602
Chicago/Turabian StyleNair, Uma P., Ravindra Shivamurthy, Raghavendra Reddy Nagate, Saurabh Chaturvedi, Saad M. Al-Qahtani, Mohammad Al Magbol, Shankar T. Gokhale, Shreyas Tikare, and Mudita Chaturvedi. 2022. "Effect of Injectable Platelet-Rich Fibrin with a Nano-Hydroxyapatite Bone Graft on the Treatment of a Grade II Furcation Defect" Bioengineering 9, no. 11: 602. https://doi.org/10.3390/bioengineering9110602
APA StyleNair, U. P., Shivamurthy, R., Nagate, R. R., Chaturvedi, S., Al-Qahtani, S. M., Magbol, M. A., Gokhale, S. T., Tikare, S., & Chaturvedi, M. (2022). Effect of Injectable Platelet-Rich Fibrin with a Nano-Hydroxyapatite Bone Graft on the Treatment of a Grade II Furcation Defect. Bioengineering, 9(11), 602. https://doi.org/10.3390/bioengineering9110602






