Hydrogels for Liver Tissue Engineering
Abstract
1. Introduction
2. Liver and LTE
2.1. Liver Functions and LTE
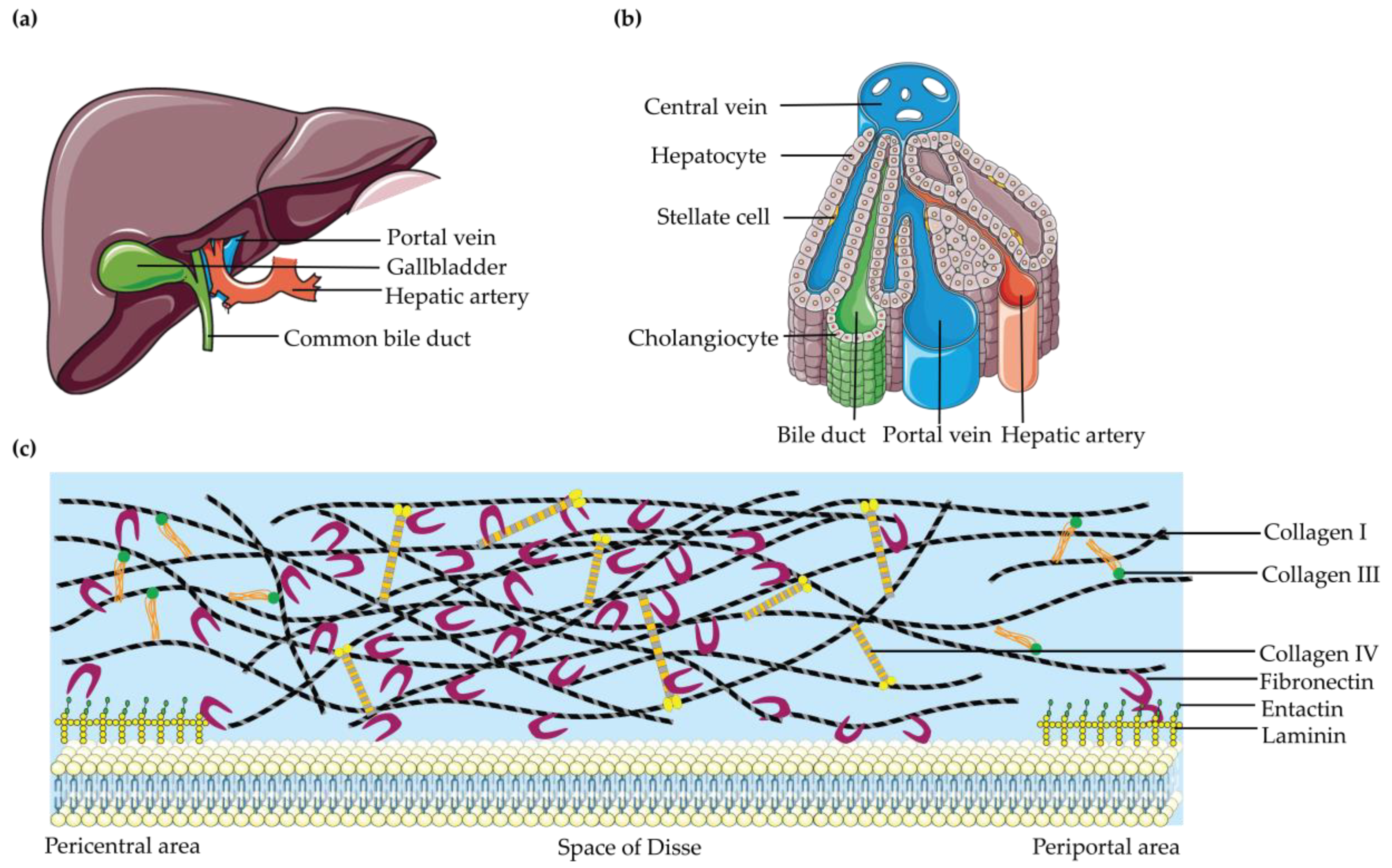
2.2. Liver Histology and LTE
2.3. Liver ECM and LTE
3. Hydrogels for LTE
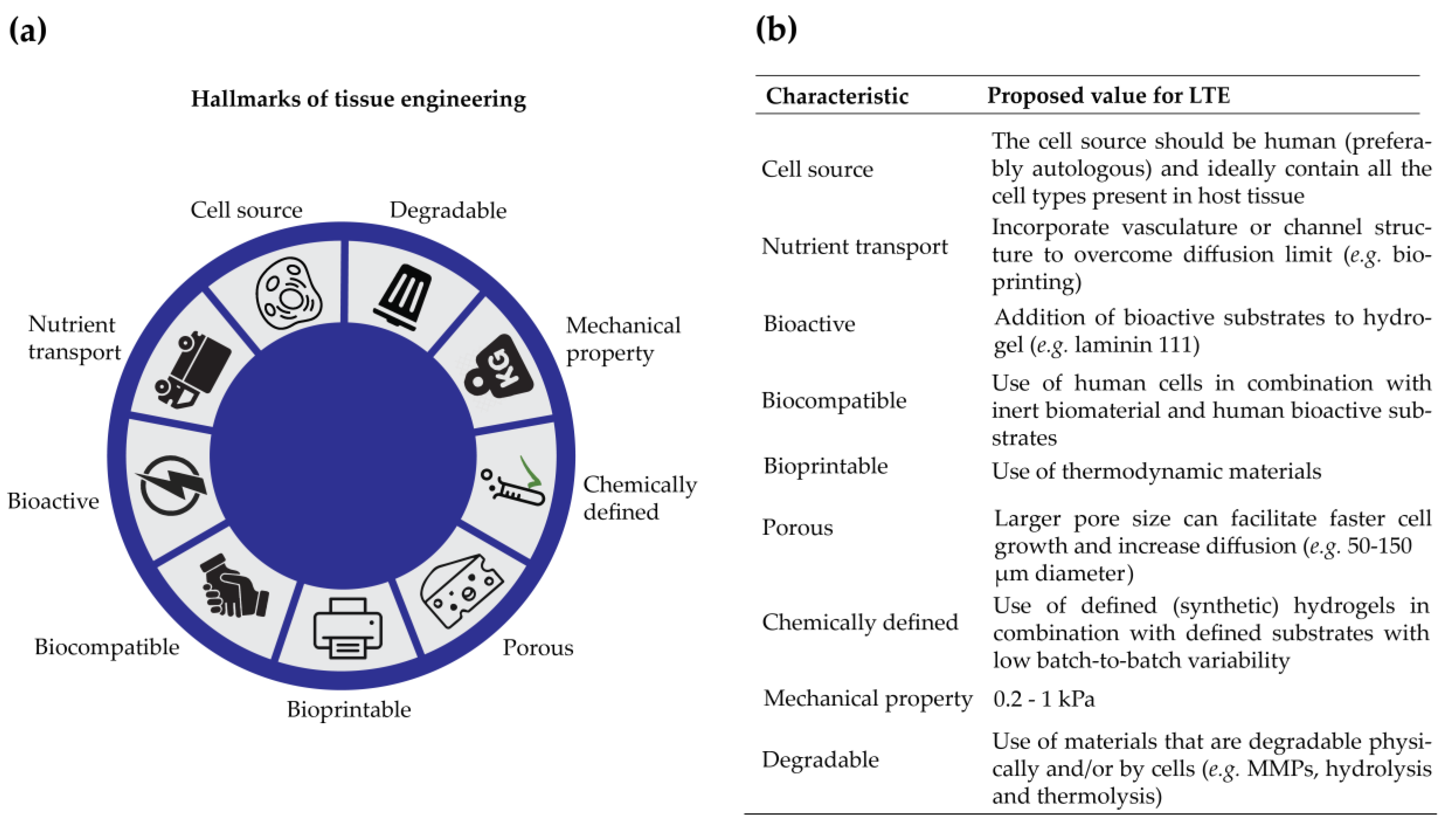
3.1. Properties Significant for LTE
3.1.1. Biological Properties
3.1.2. Physicochemical Properties
3.2. Categories of Hydrogels
3.2.1. Natural Hydrogels
3.2.2. Synthetic Hydrogels
3.3. Progress in Hydrogel Techniques
4. Conclusions
5. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Ananthanarayanan, A.; Narmada, B.C.; Mo, X.; McMillian, M.; Yu, H. Purpose-driven biomaterials research in liver-tissue engineering. Trends Biotechnol. 2011, 29, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Han, R.; Ng, S.; Ni, J.; Sun, W.; Wohland, T.; Ong, S.H.; Kuleshova, L.; Yu, H. Identification and characterization of a novel prespheroid 3-dimensional hepatocyte monolayer on galactosylated substratum. Tissue Eng. 2007, 13, 1455–1468. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.; Han, R.; Chang, S.; Ni, J.; Hunziker, W.; Goryachev, A.B.; Ong, S.H.; Yu, H. Improved Hepatocyte Excretory Function by Immediate Presentation of Polarity Cues. Tissue Eng. 2006, 12, 2181–2191. [Google Scholar] [CrossRef] [PubMed]
- Dash, A.; Inman, W.; Hoffmaster, K.; Sevidal, S.; Kelly, J.; Obach, R.S.; Griffith, L.G.; Tannenbaum, S.R. Liver tissue engineering in the evaluation of drug safety. Expert Opin. Drug Metab. Toxicol. 2009, 5, 1159–1174. [Google Scholar] [CrossRef] [PubMed]
- Palakkan, A.A.; Hay, D.C.; Anil Kumar, P.R.; Kumary, T.V.; Ross, J.A. Liver tissue engineering and cell sources: Issues and challenges. Liver Int. 2013, 33, 666–676. [Google Scholar] [CrossRef] [PubMed]
- Uygun, B.E.; Uygun, K.; Yarmush, M.L. 5.541—Liver Tissue Engineering. Compr. Biomater. 2011, 575–585. [Google Scholar] [CrossRef]
- Lee, J.S.; Cho, S.-W. Liver tissue engineering: Recent advances in the development of a bio-artificial liver. Biotechnol. Bioprocess Eng. 2012, 17, 427–438. [Google Scholar] [CrossRef]
- Bhatia, S.N.; Underhill, G.H.; Zaret, K.S.; Fox, I.J. Cell and tissue engineering for liver disease. Sci. Transl. Med. 2014, 6, 1–21. [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, X.; Liang, L.; Li, J.; Demirci, U.; Wang, S. A decade of progress in liver regenerative medicine. Biomaterials 2018, 157, 161–176. [Google Scholar] [CrossRef]
- Duan, B.-W.; Lu, S.-C.; Wang, M.-L.; Liu, J.-N.; Chi, P.; Lai, W.; Wu, J.-S.; Guo, Q.-L.; Lin, D.-D.; Liu, Y.; et al. Liver transplantation in acute-on-chronic liver failure patients with high model for end-stage liver disease (MELD) scores-a single center experience of 100 consecutive cases. J. Surg. Res. 2013, 18, 936–943. [Google Scholar] [CrossRef]
- Kidambi, S.; Yarmush, R.S.; Novik, E.; Chao, P.; Yarmush, M.L.; Nahmias, Y. Oxygen-mediated enhancement of primary hepatocyte metabolism, functional polarization, gene expression, and drug clearance. Proc. Natl. Acad Sci. USA 2009, 106, 15714–15719. [Google Scholar] [CrossRef] [PubMed]
- Habibullah, C.M.; Syed, I.H.; Qamar, A.; Taher-Uz, Z. Human fetal hepatocyte transplantation in patients with fulminant hepatic failure. Transplantation 1994, 58, 951–952. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, N.; Noguchi, H.; Matsumura, T.; Watanabe, T.; Totsugawa, T.; Fujiwara, T.; Tanaka, N. Establishment of a tightly regulated immortalized human hepatocyte cell line for the development of bioartificial liver. Hepatology 2000, 32, 611a. [Google Scholar]
- Mito, M.; Kusano, M. Hepatocyte Transplantation in Man. Cell Transpl. 1993, 2, 65–74. [Google Scholar] [CrossRef]
- Strom, S.C.; Fisher, R.A.; Thompson, M.T.; Sanyal, A.J.; Cole, P.E.; Ham, J.M.; Posner, M.P. Hepatocyte transplantation as a bridge to orthotopic liver transplantation in terminal liver failure. Transplantation 1997, 63, 559–569. [Google Scholar] [CrossRef]
- Kisseleva, T.; Gigante, E.; Brenner, D.A. Recent advances in liver stem cell therapy. Curr. Opin. Gastroenterol. 2010, 26, 395–402. [Google Scholar] [CrossRef]
- Zhang, W.; Tucker-Kellogg, L.; Narmada, B.C.; Venkatraman, L.; Chang, S.; Lu, Y.; Tan, N.; White, J.K.; Jia, R.; Bhowmick, S.S.; et al. Cell-delivery therapeutics for liver regeneration. Adv. Drug Deliv. Rev. 2010, 62, 814–826. [Google Scholar] [CrossRef]
- Khan, A.A.; Shaik, M.V.; Parveen, N.; Rajendraprasad, A.; Aleem, M.A.; Habeeb, M.A.; Srinivas, G.; Raj, T.A.; Tiwari, S.K.; Kumaresan, K.; et al. Human Fetal Liver-Derived Stem Cell Transplantation as Supportive Modality in the Management of End-Stage Decompensated Liver Cirrhosis. Cell Transpl. 2010, 19, 409–418. [Google Scholar] [CrossRef]
- Cai, J.; Zhao, Y.; Liu, Y.; Ye, F.; Song, Z.; Qin, H.; Meng, S.; Chen, Y.; Zhou, R.; Song, X.; et al. Directed differentiation of human embryonic stem cells into functional hepatic cells. Hepatology 2007, 45, 1229–1239. [Google Scholar] [CrossRef]
- Huch, M.; Dorrell, C.; Boj, S.F.; van Es, J.H.; Li, V.S.; van de Wetering, M.; Sato, T.; Hamer, K.; Sasaki, N.; Finegold, M.J.; et al. In vitro expansion of single Lgr5+ liver stem cells induced by Wnt-driven regeneration. Nature 2013, 494, 247–250. [Google Scholar] [CrossRef]
- Si-Tayeb, K.; Noto, F.K.; Nagaoka, M.; Li, J.; Battle, M.A.; Duris, C.; North, P.E.; Dalton, S.; Duncan, S.A. Highly efficient generation of human hepatocyte-like cells from induced pluripotent stem cells. Hepatology 2010, 51, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Stock, P.; Bruckner, S.; Ebensing, S.; Hempel, M.; Dollinger, M.M.; Christ, B. The generation of hepatocytes from mesenchymal stem cells and engraftment into murine liver. Nat. Protoc. 2010, 5, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Huch, M.; Gehart, H.; van Boxtel, R.; Hamer, K.; Blokzijl, F.; Verstegen, M.M.; Ellis, E.; van Wenum, M.; Fuchs, S.A.; de Ligt, J.; et al. Long-term culture of genome-stable bipotent stem cells from adult human liver. Cell 2015, 160, 299–312. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Soto-Gutierrez, A.; Baptista, P.M.; Spee, B. Biotechnology Challenges to In Vitro Maturation of Hepatic Stem Cells. Gastroenterology 2018, 154, 1258–1272. [Google Scholar] [CrossRef] [PubMed]
- Levy, G.; Bomze, D.; Heinz, S.; Ramachandran, S.D.; Noerenberg, A.; Cohen, M.; Shibolet, O.; Sklan, E.; Braspenning, J.; Nahmias, Y. Long-term culture and expansion of primary human hepatocytes. Nat. Biotechnol. 2015, 33, 1264–1271. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Zhang, L.; Liu, W.; Ma, X.; Cen, J.; Sun, Z.; Wang, C.; Feng, S.; Zhang, Z.; Yue, L.; et al. In Vitro Expansion of Primary Human Hepatocytes with Efficient Liver Repopulation Capacity. Cell Stem Cell 2018. [Google Scholar] [CrossRef]
- Hu, H.; Gehart, H.; Artegiani, B.; LÖpez-Iglesias, C.; Dekkers, F.; Basak, O.; van Es, J.; Chuva de Sousa Lopes, S.M.; Begthel, H.; Korving, J.; et al. Long-Term Expansion of Functional Mouse and Human Hepatocytes as 3D Organoids. Cell 2018, 175, 1591–1606. [Google Scholar] [CrossRef] [PubMed]
- Sivashanmugam, A.; Arun Kumar, R.; Vishnu Priya, M.; Nair, S.V.; Jayakumar, R. An overview of injectable polymeric hydrogels for tissue engineering. Eur. Polym. J. 2015, 72, 543–565. [Google Scholar] [CrossRef]
- Bedian, L.; Villalba-Rodriguez, A.M.; Hernandez-Vargas, G.; Parra-Saldivar, R.; Iqbal, H.M. Bio-based materials with novel characteristics for tissue engineering applications-A review. Int. J. Biol. Macromol. 2017, 98, 837–846. [Google Scholar] [CrossRef]
- Bahram, M.; Mohseni, N.; Moghtader, M. An Introduction to Hydrogels and Some Recent Applications. In Emerging Concepts in Analysis and Applications of Hydrogels; InTech: London, UK, 2016; ISBN 978-953-51-2510-5. [Google Scholar]
- Lee, K.Y.; Mooney, D.J. Hydrogels for Tissue Engineering. Chem. Rev. 2001, 101. [Google Scholar] [CrossRef]
- Curvello, R.; Raghuwanshi, V.S.; Garnier, G. Engineering nanocellulose hydrogels for biomedical applications. Adv. Colloid Interface Sci. 2019, 267, 47–61. [Google Scholar] [CrossRef] [PubMed]
- Chiti, M.C.; Dolmans, M.M.; Donnez, J.; Amorim, C.A. Fibrin in Reproductive Tissue Engineering: A Review on Its Application as a Biomaterial for Fertility Preservation. Ann. Biomed Eng. 2017, 45, 1650–1663. [Google Scholar] [CrossRef] [PubMed]
- Dong, C.; Lv, Y. Application of Collagen Scaffold in Tissue Engineering: Recent Advances and New Perspectives. Polymers 2016, 8, 42. [Google Scholar] [CrossRef] [PubMed]
- Dash, T.K.; Konkimalla, V.B. Poly-small je, Ukrainian-caprolactone based formulations for drug delivery and tissue engineering: A review. J. Control. Release 2012, 158, 15–33. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Han, S.S. PVA-based hydrogels for tissue engineering A review. Int. J. Polym. Mater. Polym. Biomater. 2017, 66, 159–182. [Google Scholar] [CrossRef]
- Annabi, N.; Tamayol, A.; Uquillas, J.A.; Akbari, M.; Bertassoni, L.E.; Cha, C.; Camci-Unal, G.; Dokmeci, M.R.; Peppas, N.A.; Khademhosseini, A. 25th Anniversary Article: Rational Design and Applications of Hydrogels in Regenerative Medicine. Adv. Mater. 2014, 26, 85–124. [Google Scholar] [CrossRef] [PubMed]
- Drury, J.L.; Mooney, D.J. Hydrogels for tissue engineering: Scaffold design variables and applications. Biomaterials 2003, 24, 4337–4351. [Google Scholar] [CrossRef]
- Khorshidi, S.; Karkhaneh, A. A review on gradient hydrogel/fiber scaffolds for osteochondral regeneration. J. Tissue Eng. Regen. Med. 2018, 12, e1974–e1990. [Google Scholar] [CrossRef] [PubMed]
- Gradinaru, V.; Treweek, J.; Overton, K.; Deisseroth, K. Hydrogel-Tissue Chemistry: Principles and Applications. Annu. Rev. Biophys. 2018, 47, 355–376. [Google Scholar] [CrossRef] [PubMed]
- Jung, J. Initiation of Mammalian Liver Development from Endoderm by Fibroblast Growth Factors. Science 1999, 284, 1998–2003. [Google Scholar] [CrossRef]
- Bohm, F.; Kohler, U.A.; Speicher, T.; Werner, S. Regulation of liver regeneration by growth factors and cytokines. EMBO Mol. Med. 2010, 2, 294–305. [Google Scholar] [CrossRef] [PubMed]
- Bosch, F.X.; Ribes, J.; Díaz, M.; Cléries, R. Primary liver cancer: Worldwide incidence and trends. Gastroenterology 2004, 127, S5–S16. [Google Scholar] [CrossRef] [PubMed]
- Rebecca, T. Liver regeneration: from myth to mechanism. Nat. Rev. Mol. Cell Biol. 2004, 5, 836–847. [Google Scholar]
- Court, F.G.; Wemyss-Holden, S.A.; Dennison, A.R.; Maddern, G.J. The mystery of liver regeneration. Br. J. Surg. 2002, 89, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, Y.; Nagino, M.; Nimura, Y. Mechanisms of Hepatic Regeneration Following Portal Vein Embolization and Partial Hepatectomy: A Review. World J. Surg. 2007, 31, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Fausto, N.; Riehle, K.J. Mechanisms of liver regeneration and their clinical implications. J. Hepatobiliary Pancreat. Surg. 2005, 12, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Fausto, N.; Campbell, J.S.; Riehle, K.J. Liver regeneration. Hepatology 2006, 43, S45–S53. [Google Scholar] [CrossRef] [PubMed]
- Michalopoulos, G.K. Liver regeneration. J. Cell Physiol. 2007, 213, 286–300. [Google Scholar] [CrossRef]
- Duncan, A.W.; Dorrell, C.; Grompe, M. Stem cells and liver regeneration. Gastroenterology 2009, 137, 466–481. [Google Scholar] [CrossRef]
- Riehle, K.J.; Dan, Y.Y.; Campbell, J.S.; Fausto, N. New concepts in liver regeneration. J. Gastroenterol. Hepatol. 2011, 26 (Suppl. 1), 203–212. [Google Scholar] [CrossRef]
- DeLeve, L.D. Liver sinusoidal endothelial cells and liver regeneration. J. Clin. Investig. 2013, 123, 1861–1866. [Google Scholar] [CrossRef] [PubMed]
- Forbes, S.J.; Newsome, P.N. Liver regeneration-mechanisms and models to clinical application. Nat. Rev. Gastroenterol Hepatol 2016, 13, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Timchenko, N.A. Aging and liver regeneration. Trends Endocrinol. Metab. 2009, 20, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Li, L.; Li, J. Stem cells with decellularized liver scaffolds in liver regeneration and their potential clinical applications. Liver Int. 2015, 35, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Souza, F.S.D.; Botelho, M.C.S.N.; Lisbôa, R.S. Hepatology: Hepatology Principles and Practice: History, Morphology, Biochemistry, Diagnostics, Clinic, Therapy. J. Am. Med Assoc. 2002, 288, 1–15. [Google Scholar]
- Willemse, J.; Lieshout, R.; van der Laan, L.J.W.; Verstegen, M.M.A. From organoids to organs: Bioengineering liver grafts from hepatic stem cells and matrix. Best Pract. Res. Clin. Gastroenterol. 2017, 31, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Gordillo, M.; Evans, T.; Gouon-Evans, V. Orchestrating liver development. Development 2015, 142, 2094–2108. [Google Scholar] [CrossRef]
- Racanelli, V.; Rehermann, B. The liver as an immunological organ. Hepatology 2006, 43, S54–S62. [Google Scholar] [CrossRef]
- Lin, X.; Horng, M.; Sun, Y.; Shiesh, S.C.; Chow, N.H.; Guo, X.Z. Computer morphometry for quantitative measurement of liver fibrosis: Comparison with Knodell’s score, colorimetry and conventional description reports. J. Gastroenterol. Hepatol. 2010, 13, 75–80. [Google Scholar] [CrossRef]
- Martinez-Hernandez, A.; Amenta, P.S. The hepatic extracellular matrix. Virchows Arch. A 1993, 423, 77–84. [Google Scholar] [CrossRef]
- Thiery, J.P.; Duband, J.L.; Tucker, G.C. Cell Migration in the Vertebrate Embryo: Role of Cell Adhesion and Tissue Environment in Pattern Formation. Annu. Rev. Cell Biol. 1985, 1, 91–113. [Google Scholar] [CrossRef] [PubMed]
- Kleinman, H.K.; Philp, D.; Hoffman, M.P. Role of the extracellular matrix in morphogenesis. Curr. Opin. Biotechnol. 2003, 14, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Bedossa, P.; Paradis, V. Liver extracellular matrix in health and disease. J. Pathol. 2003, 200, 504–515. [Google Scholar] [CrossRef] [PubMed]
- Hynes, R.O. The extracellular matrix: Not just pretty fibrils. Science 2009, 326, 1216–1219. [Google Scholar] [CrossRef] [PubMed]
- Baiocchini, A.; Montaldo, C.; Conigliaro, A.; Grimaldi, A.; Correani, V.; Mura, F.; Ciccosanti, F.; Rotiroti, N.; Brenna, A.; Montalbano, M.; et al. Extracellular Matrix Molecular Remodeling in Human Liver Fibrosis Evolution. PLoS ONE 2016, 11, e0151736. [Google Scholar] [CrossRef]
- Martinez-Hernandez, A. The hepatic extracellular matrix. I. Electron immunohistochemical studies in normal rat liver. Lab. Investig. 1984, 51, 57–74. [Google Scholar]
- Rojkind, M.; Ponce-Noyola, P. The Extracellular Matrix of the Liver. Collagen Relat. Res. 1982, 2, 151–175. [Google Scholar] [CrossRef]
- Marrone, G.; Shah, V.H.; Gracia-Sancho, J. Sinusoidal communication in liver fibrosis and regeneration. J. Hepatol. 2016, 65, 608–617. [Google Scholar] [CrossRef]
- Zhu, C.; Coombe, D.R.; Zheng, M.H.; Yeoh, G.C.; Li, L. Liver progenitor cell interactions with the extracellular matrix. J. Tissue Eng. Regen. Med. 2013, 7, 757–766. [Google Scholar] [CrossRef]
- Klaas, M.; Kangur, T.; Viil, J.; Maemets-Allas, K.; Minajeva, A.; Vadi, K.; Antsov, M.; Lapidus, N.; Jarvekulg, M.; Jaks, V. The alterations in the extracellular matrix composition guide the repair of damaged liver tissue. Sci. Rep. 2016, 6, 27398. [Google Scholar] [CrossRef]
- Bemmelen, J.M.V. Der Hydrogel und das kristallinische Hydrat des Kupferoxydes. Z. Anorg. Chem. 1894, 5, 466. [Google Scholar] [CrossRef]
- Danno, A. Gel Formation of Aqueous Solution of Polyvinyl Alcohol Irradiated by Gamma Rays from Cobalt-60. J. Phys. Soc. Jpn. 1958, 13, 722–727. [Google Scholar] [CrossRef]
- Wichterle, O.; Lim, D. Hydrophilic Gels for Biological Use. Nature 1960, 185, 117–118. [Google Scholar] [CrossRef]
- Buwalda, S.J.; Boere, K.W.; Dijkstra, P.J.; Feijen, J.; Vermonden, T.; Hennink, W.E. Hydrogels in a historical perspective: From simple networks to smart materials. J. Control. Release 2014, 190, 254–273. [Google Scholar] [CrossRef] [PubMed]
- Vishwakarma, S.K.; Bardia, A.; Lakkireddy, C.; Raju, N.; Paspala, S.A.B.; Habeeb, M.A.; Khan, A.A. Intraperitoneal transplantation of bioengineered humanized liver grafts supports failing liver in acute condition. Mater. Sci. Eng. C Mater Biol. Appl. 2019, 98, 861–873. [Google Scholar] [CrossRef] [PubMed]
- Vasanthan, K.S.; Subramanian, A.; Krishnan, U.M.; Sethuraman, S. Role of biomaterials, therapeutic molecules and cells for hepatic tissue engineering. Biotechnol. Adv. 2012, 30, 742–752. [Google Scholar] [CrossRef]
- Barbucci, R. Hydrogels: Biological Properties and Applications; Springer: Milan, Italy, 2009; pp. 1–179. [Google Scholar]
- Wang, X.H.; Li, D.P.; Wang, W.J.; Feng, Q.L.; Cui, F.Z.; Xu, Y.X.; Song, X.H.; van der Werf, M. Crosslinked collagen/chitosan matrix for artificial livers. Biomaterials 2003, 24, 3213–3220. [Google Scholar] [CrossRef]
- Yu, X.; Bichtelen, A.; Wang, X.; Yan, Y.; Lin, F.; Xiong, Z.; Wu, R.; Zhang, R.; Lu, Q. Collagen/Chitosan/Heparin Complex with Improved Biocompatibility for Hepatic Tissue Engineering. J. Bioact. Compat. Polym. 2016, 20, 15–28. [Google Scholar] [CrossRef]
- Nair, L.S.; Laurencin, C.T. Biodegradable polymers as biomaterials. Prog. Polym. Sci. 2007, 32, 762–798. [Google Scholar] [CrossRef]
- Bhattacharya, M.; Malinen, M.M.; Lauren, P.; Lou, Y.R.; Kuisma, S.W.; Kanninen, L.; Lille, M.; Corlu, A.; GuGuen-Guillouzo, C.; Ikkala, O.; et al. Nanofibrillar cellulose hydrogel promotes three-dimensional liver cell culture. J. Control. Release 2012, 164, 291–298. [Google Scholar] [CrossRef]
- Park, U.J.; Jeong, W.; Kwon, S.Y.; Kim, Y.; Choi, K.; Kim, H.T.; Son, D. Fabrication of a Novel Absorbable Vascular Anastomosis Device and Testing in a Pig Liver Transplantation Model. Ann. Biomed. Eng. 2019, 47, 1063–1077. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Tao, R.; Wu, W.; Cao, H.; Xin, J.; Li, J.; Guo, J.; Jiang, L.; Gao, C.; Demetriou, A.A.; et al. 3D PLGA scaffolds improve differentiation and function of bone marrow mesenchymal stem cell-derived hepatocytes. Stem Cells Dev. 2010, 19, 1427–1436. [Google Scholar] [CrossRef] [PubMed]
- Brandl, F.; Sommer, F.; Goepferich, A. Rational design of hydrogels for tissue engineering: Impact of physical factors on cell behavior. Biomaterials 2007, 28, 134–146. [Google Scholar] [CrossRef] [PubMed]
- Bomo, J.; Ezan, F.; Tiaho, F.; Bellamri, M.; Langouet, S.; Theret, N.; Baffet, G. Increasing 3D Matrix Rigidity Strengthens Proliferation and Spheroid Development of Human Liver Cells in a Constant Growth Factor Environment. J. Cell Biochem. 2016, 117, 708–720. [Google Scholar] [CrossRef] [PubMed]
- Desai, S.S.; Tung, J.C.; Zhou, V.X.; Grenert, J.P.; Malato, Y.; Rezvani, M.; Espanol-Suner, R.; Willenbring, H.; Weaver, V.M.; Chang, T.T. Physiological ranges of matrix rigidity modulate primary mouse hepatocyte function in part through hepatocyte nuclear factor 4 alpha. Hepatology 2016, 64, 261–275. [Google Scholar] [CrossRef] [PubMed]
- Wells, R.G. The role of matrix stiffness in regulating cell behavior. Hepatology 2008, 47, 1394–1400. [Google Scholar] [CrossRef] [PubMed]
- Gong, H.; Agustin, J.; Wootton, D.; Zhou, J.G. Biomimetic design and fabrication of porous chitosan-gelatin liver scaffolds with hierarchical channel network. J. Mater. Sci. Mater. Med. 2014, 25, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Capone, S.H.; Dufresne, M.; Rechel, M.; Fleury, M.J.; Salsac, A.V.; Paullier, P.; Daujat-Chavanieu, M.; Legallais, C. Impact of alginate composition: From bead mechanical properties to encapsulated HepG2/C3A cell activities for in vivo implantation. PLoS ONE 2013, 8, e62032. [Google Scholar] [CrossRef] [PubMed]
- Annabi, N.; Nichol, J.W.; Zhong, X.; Ji, C.; Koshy, S.; Khademhosseini, A.; Dehghani, F. Controlling the Porosity and Microarchitecture of Hydrogels for Tissue Engineering. Tissue Eng. Part B Rev. 2010, 16, 371–383. [Google Scholar] [CrossRef]
- Zhao, H.; Xu, K.; Zhu, P.; Wang, C.; Chi, Q. Smart hydrogels with high tunability of stiffness as a biomimetic cell carrier. Cell Biol. Int. 2019, 43, 84–97. [Google Scholar] [CrossRef]
- Park, T.G. Perfusion culture of hepatocytes within galactose-derivatized biodegradable poly(lactide-co-glycolide) scaffolds prepared by gas foaming of effervescent salts. J. Biomed. Mater. Res. Part B Appl. Biomater. 2010, 59, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Park, K.H.; Bae, Y.H. Phenotype of Hepatocyte Spheroids in Arg-Gly-Asp (RGD) Containing a Thermo-Reversible Extracellular Matrix. Biosci. Biotechnol. Biochem. 2002, 66, 1473–1478. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.Y.J.; Kumar, R.; Xu, X.Y.; Mantalaris, A. A combined fluid dynamics, mass transport and cell growth model for a three-dimensional perfused biorector for tissue engineering of haematopoietic cells. Biochem. Eng. J. 2007, 35, 1–11. [Google Scholar] [CrossRef]
- Wu, C.; Pan, J.; Bao, Z.; Yu, Y. Fabrication and characterization of chitosan microcarrier for hepatocyte culture. J. Mater. Sci. Mater. Med. 2007, 18, 2211–2214. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, A.; Melo, J.S. Preparation of a sponge-like biocomposite agarose–chitosan scaffold with primary hepatocytes for establishing an in vitro 3D liver tissue model. RSC Adv. 2015, 5, 30701–30710. [Google Scholar] [CrossRef]
- Jaspers, M.; Dennison, M.; Mabesoone, M.F.; MacKintosh, F.C.; Rowan, A.E.; Kouwer, P.H. Ultra-responsive soft matter from strain-stiffening hydrogels. Nat. Commun. 2014, 5, 5808. [Google Scholar] [CrossRef] [PubMed]
- Necas, J.; Brauner, P.; Kolar, J.; Bartosikova, L. Hyaluronic acid (hyaluronan)—A review. Vet. Med. 2008, 53, 397–411. [Google Scholar] [CrossRef]
- Allison, D.D.; Grande-Allen, K.J. Hyaluronan: A powerful tissue engineering tool. Tissue Eng. 2006, 12, 2131–2140. [Google Scholar] [CrossRef]
- Augst, A.D.; Kong, H.J.; Mooney, D.J. Alginate hydrogels as biomaterials. Macromol. Biosci. 2006, 6, 623–633. [Google Scholar] [CrossRef]
- Lee, K.Y.; Mooney, D.J. Alginate: Properties and biomedical applications. Prog. Polym. Sci. 2012, 37, 106–126. [Google Scholar] [CrossRef]
- Liu, C.Z.; Xia, Z.D.; Han, Z.W.; Hulley, P.A.; Triffitt, J.T.; Czernuszka, J.T. Novel 3D collagen scaffolds fabricated by indirect printing technique for tissue engineering. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 85, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Van Vlierberghe, S.; Dubruel, P.; Schacht, E. Biopolymer-based hydrogels as scaffolds for tissue engineering applications: A review. Biomacromolecules 2011, 12, 1387–1408. [Google Scholar] [CrossRef]
- Klotz, B.J.; Gawlitta, D.; Rosenberg, A.; Malda, J.; Melchels, F.P.W. Gelatin-Methacryloyl Hydrogels: Towards Biofabrication-Based Tissue Repair. Trends Biotechnol. 2016, 34, 394–407. [Google Scholar] [CrossRef] [PubMed]
- Kleinman, H.K.; Martin, G.R. Matrigel: Basement membrane matrix with biological activity. Semin. Cancer Biol. 2005, 15, 378–386. [Google Scholar] [CrossRef] [PubMed]
- Snyder, J.E.; Hamid, Q.; Wang, C.; Chang, R.; Emami, K.; Wu, H.; Sun, W. Bioprinting cell-laden matrigel for radioprotection study of liver by pro-drug conversion in a dual-tissue microfluidic chip. Biofabrication 2011, 3, 034112. [Google Scholar] [CrossRef]
- Hughes, C.S.; Postovit, L.M.; Lajoie, G.A. Matrigel: A complex protein mixture required for optimal growth of cell culture. Proteomics 2010, 10, 1886–1890. [Google Scholar] [CrossRef]
- Currie, L.J.; Sharpe, J.R.; Martin, R. The use of fibrin glue in skin grafts and tissue-engineered skin replacements: A review. Plast. Reconstr. Surg. 2001, 108, 1713–1726. [Google Scholar] [CrossRef]
- Ahmed, T.A.; Griffith, M.; Hincke, M. Characterization and inhibition of fibrin hydrogel-degrading enzymes during development of tissue engineering scaffolds. Tissue Eng. 2007, 13, 1469–1477. [Google Scholar] [CrossRef]
- Kalia, V.C.; Ray, S.; Patel, S.K.S.; Singh, M.; Singh, G.P. The Dawn of Novel Biotechnological Applications of Polyhydroxyalkanoates. In Biotechnological Applications of Polyhydroxyalkanoates; Kalia, V., Ed.; Springer: Singapore, 2019. [Google Scholar]
- Zhang, Y.S.; Yue, K.; Aleman, J.; Moghaddam, K.M.; Bakht, S.M.; Yang, J.; Jia, W.; Dell’Erba, V.; Assawes, P.; Shin, S.R.; et al. 3D Bioprinting for Tissue and Organ Fabrication. Ann. Biomed. Eng. 2017, 45, 148–163. [Google Scholar] [CrossRef]
- Mazzocchi, A.; Devarasetty, M.; Huntwork, R.; Soker, S.; Skardal, A. Optimization of collagen type I-hyaluronan hybrid bioink for 3D bioprinted liver microenvironments. Biofabrication 2018, 11, 015003. [Google Scholar] [CrossRef]
- Wang, X.; Yan, Y.; Xiong, Z.; Lin, F.; Wu, R.; Zhang, R.; Lu, Q. Preparation and evaluation of ammonia-treated collagen/chitosan matrices for liver tissue engineering. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 75, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Yan, Y.; Lin, F.; Xiong, Z.; Wu, R.; Zhang, R.; Lu, Q. Preparation and characterization of a collagen/chitosan/heparin matrix for an implantable bioartificial liver. J. Biomater. Sci. Polym. Ed. 2012, 16, 1063–1080. [Google Scholar] [CrossRef]
- Wang, X.; Yan, Y.; Pan, Y.; Xiong, Z.; Liu, H.; Cheng, J.; Liu, F.; Lin, F.; Wu, R.; Zhang, R.; et al. Generation of Three-Dimensional Hepatocyte-Gelatin Structures with Rapid Prototyping System. Tissue Eng. 2006, 12, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Hussein, K.H.; Park, K.M.; Kang, K.S.; Woo, H.M. Heparin-gelatin mixture improves vascular reconstruction efficiency and hepatic function in bioengineered livers. Acta Biomater. 2016, 38, 82–93. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.; Xiaohong, W.; Yongnian, Y.; Renji, Z. A Polyurethane-Gelatin Hybrid Construct for Manufacturing Implantable Bioartificial Livers. J. Bioact. Compat. Polym. 2008, 23, 409–422. [Google Scholar] [CrossRef]
- Rozario, T.; DeSimone, D.W. The extracellular matrix in development and morphogenesis: A dynamic view. Dev. Biol. 2010, 341, 126–140. [Google Scholar] [CrossRef] [PubMed]
- Suri, S.; Han, L.H.; Zhang, W.; Singh, A.; Chen, S.; Schmidt, C.E. Solid freeform fabrication of designer scaffolds of hyaluronic acid for nerve tissue engineering. Biomed. Microdevices 2011, 13, 983–993. [Google Scholar] [CrossRef] [PubMed]
- Turner, W.S.; Schmelzer, E.; McClelland, R.; Wauthier, E.; Chen, W.; Reid, L.M. Human hepatoblast phenotype maintained by hyaluronan hydrogels. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 82, 156–168. [Google Scholar] [CrossRef]
- Christoffersson, J.; Aronsson, C.; Jury, M.; Selegard, R.; Aili, D.; Mandenius, C.F. Fabrication of modular hyaluronan-PEG hydrogels to support 3D cultures of hepatocytes in a perfused liver-on-a-chip device. Biofabrication 2018. [Google Scholar] [CrossRef]
- Bruns, H.; Kneser, U.; Holzhüter, S.; Roth, B.; Kluth, J.; Kaufmann, P.M.; Kluth, D.; Fiegel, H.C. Injectable Liver A Novel Approach Using Fibrin Gel as a Matrix for Culture and Intrahepatic Transplantation of Hepatocytes. Tissue Eng. 2005, 11, 1718–1726. [Google Scholar] [CrossRef]
- Wang, X.; Liu, C. Fibrin Hydrogels for Endothelialized Liver Tissue Engineering with a Predesigned Vascular Network. Polymers 2018, 10, 48. [Google Scholar] [CrossRef] [PubMed]
- Hickey, R.D.; Naugler, W.E. Ectopic expansion of engineered human liver tissue seeds using mature cell populations. Hepatology 2018, 67, 2465–2467. [Google Scholar] [CrossRef]
- Jammalamadaka, U.; Tappa, K. Recent Advances in Biomaterials for 3D Printing and Tissue Engineering. J. Funct. Biomater. 2018, 9, 22. [Google Scholar] [CrossRef]
- Kim, Y.; Kang, K.; Jeong, J.; Paik, S.S.; Kim, J.S.; Park, S.A.; Kim, W.D.; Park, J.; Choi, D. Three-dimensional (3D) printing of mouse primary hepatocytes to generate 3D hepatic structure. Ann. Surg. Treat. Res. 2017, 92, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Tong, X.F.; Zhao, F.Q.; Ren, Y.Z.; Zhang, Y.; Cui, Y.L.; Wang, Q.S. Injectable hydrogels based on glycyrrhizin, alginate, and calcium for three-dimensional cell culture in liver tissue engineering. J. Biomed. Mater. Res. A 2018, 106, 3292–3302. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.H.; Shin, S.J.; Kim, C.B.; Kim, J.K.; Cho, Y.W.; Chung, B.G.; Lee, S.H. Microfluidic synthesis of pure chitosan microfibers for bio-artificial liver chip. Lab. Chip. 2010, 10, 1328–1334. [Google Scholar] [CrossRef] [PubMed]
- Jiankang, H.; Dichen, L.; Yaxiong, L.; Bo, Y.; Hanxiang, Z.; Qin, L.; Bingheng, L.; Yi, L. Preparation of chitosan-gelatin hybrid scaffolds with well-organized microstructures for hepatic tissue engineering. Acta Biomater. 2009, 5, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Rajendran, D.; Hussain, A.; Yip, D.; Parekh, A.; Shrirao, A.; Cho, C.H. Long-term liver-specific functions of hepatocytes in electrospun chitosan nanofiber scaffolds coated with fibronectin. J. Biomed. Mater. Res. A 2017, 105, 2119–2128. [Google Scholar] [CrossRef]
- Su, Z.; Li, P.; Wu, B.; Ma, H.; Wang, Y.; Liu, G.; Zeng, H.; Li, Z.; Wei, X. PHBVHHx scaffolds loaded with umbilical cord-derived mesenchymal stem cells or hepatocyte-like cells differentiated from these cells for liver tissue engineering. Mater. Sci. Eng. C Mater. Biol. Appl. 2014, 45, 374–382. [Google Scholar] [CrossRef]
- Li, P.; Zhang, J.; Liu, J.; Ma, H.; Liu, J.; Lie, P.; Wang, Y.; Liu, G.; Zeng, H.; Li, Z.; et al. Promoting the recovery of injured liver with poly (3-hydroxybutyrate-co-3-hydroxyvalerate-co-3-hydroxyhexanoate) scaffolds loaded with umbilical cord-derived mesenchymal stem cells. Tissue Eng. Part A 2015, 21, 603–615. [Google Scholar] [CrossRef] [PubMed]
- Markstedt, K.; Mantas, A.; Tournier, I.; Martinez Avila, H.; Hagg, D.; Gatenholm, P. 3D Bioprinting Human Chondrocytes with Nanocellulose-Alginate Bioink for Cartilage Tissue Engineering Applications. Biomacromolecules 2015, 16, 1489–1496. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Lin, Z.Y.; Wenger, A.C.; Tam, K.C.; Tang, X. 3D bioprinting of liver-mimetic construct with alginate/cellulose nanocrystal hybrid bioink. Bioprinting 2018, 9, 1–6. [Google Scholar] [CrossRef]
- Malinen, M.M.; Kanninen, L.K.; Corlu, A.; Isoniemi, H.M.; Lou, Y.R.; Yliperttula, M.L.; Urtti, A.O. Differentiation of liver progenitor cell line to functional organotypic cultures in 3D nanofibrillar cellulose and hyaluronan-gelatin hydrogels. Biomaterials 2014, 35, 5110–5121. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Liu, S.; Feng, W. PVA hydrogel properties for biomedical application. J. Mech. Behav. Biomed. Mater. 2011, 4, 1228–1233. [Google Scholar] [CrossRef] [PubMed]
- Kouwer, P.H.; Koepf, M.; Le Sage, V.A.; Jaspers, M.; van Buul, A.M.; Eksteen-Akeroyd, Z.H.; Woltinge, T.; Schwartz, E.; Kitto, H.J.; Hoogenboom, R.; et al. Responsive biomimetic networks from polyisocyanopeptide hydrogels. Nature 2013, 493, 651–655. [Google Scholar] [CrossRef] [PubMed]
- Hammink, R.; Eggermont, L.J.; Zisis, T.; Tel, J.; Figdor, C.G.; Rowan, A.E.; Blank, K.G. Affinity-Based Purification of Polyisocyanopeptide Bioconjugates. Bioconjug. Chem. 2017, 28, 2560–2568. [Google Scholar] [CrossRef] [PubMed]
- Utech, S.; Boccaccini, A.R. A review of hydrogel-based composites for biomedical applications: enhancement of hydrogel properties by addition of rigid inorganic fillers. J. Mater. Sci. 2016, 51, 271–310. [Google Scholar] [CrossRef]
- Saito, E.; Kang, H.; Taboas, J.M.; Diggs, A.; Flanagan, C.L.; Hollister, S.J. Experimental and computational characterization of designed and fabricated 50:50 PLGA porous scaffolds for human trabecular bone applications. J. Mater. Sci. Mater. Med. 2010, 21, 2371–2383. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, M.H.; Shea, L.D.; Peters, M.C.; Mooney, D.J. Bioabsorbable polymer scaffolds for tissue engineering capable. J. Control. Release 2000, 64, 91–102. [Google Scholar] [CrossRef]
- Middleton, J.C.; Tipton, A.J. Synthetic biodegradable polymers as orthopedic devices. Biomaterials 2000, 21, 2335–2346. [Google Scholar] [CrossRef]
- Lv, Q.; Hu, K.; Feng, Q.; Cui, F.; Cao, C. Preparation and characterization of PLA/fibroin composite and culture of HepG2 (human hepatocellular liver carcinoma cell line) cells. Compos. Sci. Technol. 2007, 67, 3023–3030. [Google Scholar] [CrossRef]
- Siddiqui, N.; Asawa, S.; Birru, B.; Baadhe, R.; Rao, S. PCL-Based Composite Scaffold Matrices for Tissue Engineering Applications. Mol. Biotechnol. 2018, 60, 506–532. [Google Scholar] [CrossRef] [PubMed]
- JANG, T.-S.; Jung, H.-D.; Pan, H.M.; Han, W.T. 3D printing of hydrogel composite systems: Recent advances in technology for tissue engineering. Int. J. Bioprinting 2018. [Google Scholar] [CrossRef]
- Yoon No, D.; Lee, K.H.; Lee, J.; Lee, S.H. 3D liver models on a microplatform: Well-defined culture, engineering of liver tissue and liver-on-a-chip. Lab. Chip. 2015, 15, 3822–3837. [Google Scholar] [CrossRef] [PubMed]
- Perez, R.A.; Jung, C.R.; Kim, H.W. Biomaterials and Culture Technologies for Regenerative Therapy of Liver Tissue. Adv. Healthc. Mater. 2017, 6. [Google Scholar] [CrossRef]
- Schepers, A.; Li, C.; Chhabra, A.; Seney, B.T.; Bhatia, S. Engineering a perfusable 3D human liver platform from iPS cells. Lab. Chip. 2016, 16, 2644–2653. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.S.; Xiong, A.; Nguyen, K.; Masek, M.; No, D.Y.; Elazar, M.; Shteyer, E.; Winters, M.A.; Voedisch, A.; Shaw, K.; et al. Long-term culture of human liver tissue with advanced hepatic functions. JCI Insight. 2017, 2. [Google Scholar] [CrossRef]
- Celikkin, N.; Simó Padial, J.; Costantini, M.; Hendrikse, H.; Cohn, R.; Wilson, C.; Rowan, A.; Święszkowski, W. 3D Printing of Thermoresponsive Polyisocyanide (PIC) Hydrogels as Bioink and Fugitive Material for Tissue Engineering. Polymers 2018, 10, 555. [Google Scholar] [CrossRef]
- Liu, Y.; Geever, L.M.; Kennedy, J.E.; Higginbotham, C.L.; Cahill, P.A.; McGuinness, G.B. Thermal behavior and mechanical properties of physically crosslinked PVA/Gelatin hydrogels. J. Mech. Behav. Biomed. Mater. 2010, 3, 203–209. [Google Scholar] [CrossRef]
- Moscato, S.; Ronca, F.; Campani, D.; Danti, S. Poly(vinyl alcohol)/gelatin Hydrogels Cultured with HepG2 Cells as a 3D Model of Hepatocellular Carcinoma: A Morphological Study. J. Funct. Biomater. 2015, 6, 16–32. [Google Scholar] [CrossRef]
- Kim, S.S.; Utsunomiya, H.; Koski, J.A.; Wu, B.M.; Cima, M.J.; Sohn, J.; Mukai, K.; Griffith, L.G.; Vacanti, J.P. Survival and function of hepatocytes on a novel three-dimensional synthetic biodegradable polymer scaffold with an intrinsic network of channels. Ann. Surg. 1998, 228, 8–13. [Google Scholar] [CrossRef]
- Kasuya, J.; Sudo, R.; Tamogami, R.; Masuda, G.; Mitaka, T.; Ikeda, M.; Tanishita, K. Reconstruction of 3D stacked hepatocyte tissues using degradable, microporous poly(d,l-lactide-co-glycolide) membranes. Biomaterials 2012, 33, 2693–2700. [Google Scholar] [CrossRef]
- Kobayashi, S.; Nagano, H.; Marubashi, S.; Wada, H.; Eguchi, H.; Takeda, Y.; Tanemura, M.; Doki, Y.; Mori, M. Fibrin sealant with PGA felt for prevention of bile leakage after liver resection. Hepatogastroenterology 2012, 59, 2564–2568. [Google Scholar] [CrossRef]
- Riccalton-Banks, L.; Liew, C.; Bhandari, R.; Fry, J.; Shakesheff, K. Long-Term Culture of Functional Liver Tissue Three-Dimensional Coculture of Primary Hepatocytes and Stellate Cells. Tissue Eng. 2003, 9, 401–410. [Google Scholar] [CrossRef]
- Davis, M.W.; Vacanti, J.P. Toward development of an implantable tissue engineered liver. Biomaterials 1996, 17, 365–372. [Google Scholar] [CrossRef]
- Feng, Z.Q.; Chu, X.H.; Huang, N.P.; Leach, M.K.; Wang, G.; Wang, Y.C.; Ding, Y.T.; Gu, Z.Z. Rat hepatocyte aggregate formation on discrete aligned nanofibers of type-I collagen-coated poly(L-lactic acid). Biomaterials 2010, 31, 3604–3612. [Google Scholar] [CrossRef]
- Lee, J.W.; Choi, Y.J.; Yong, W.J.; Pati, F.; Shim, J.H.; Kang, K.S.; Kang, I.H.; Park, J.; Cho, D.W. Development of a 3D cell printed construct considering angiogenesis for liver tissue engineering. Biofabrication 2016, 8, 015007. [Google Scholar] [CrossRef]
- Grant, R.; Hay, D.C.; Callanan, A. A Drug-Induced Hybrid Electrospun Poly-Capro-Lactone: Cell-Derived Extracellular Matrix Scaffold for Liver Tissue Engineering. Tissue Eng. Part A 2017, 23, 650–662. [Google Scholar] [CrossRef]
- Hashemi, S.M.; Soleimani, M.; Zargarian, S.S.; Haddadi-Asl, V.; Ahmadbeigi, N.; Soudi, S.; Gheisari, Y.; Hajarizadeh, A.; Mohammadi, Y. In vitro differentiation of human cord blood-derived unrestricted somatic stem cells into hepatocyte-like cells on poly(epsilon-caprolactone) nanofiber scaffolds. Cells Tissues Organs 2009, 190, 135–149. [Google Scholar] [CrossRef]
- Semnani, D.; Naghashzargar, E.; Hadjianfar, M.; Dehghan Manshadi, F.; Mohammadi, S.; Karbasi, S.; Effaty, F. Evaluation of PCL/chitosan electrospun nanofibers for liver tissue engineering. Int. J. Polym. Mater. Polym. Biomater. 2016, 66, 149–157. [Google Scholar] [CrossRef]
- Tan, W.J.; Teo, G.P.; Liao, K.; Leong, K.W.; Mao, H.Q.; Chan, V. Adhesion contact dynamics of primary hepatocytes on poly(ethylene terephthalate) surface. Biomaterials 2005, 26, 891–898. [Google Scholar] [CrossRef]
- Janorkar, A.V.; Rajagopalan, P.; Yarmush, M.L.; Megeed, Z. The use of elastin-like polypeptide-polyelectrolyte complexes to control hepatocyte morphology and function in vitro. Biomaterials 2008, 29, 625–632. [Google Scholar] [CrossRef]
- Cho, C.S.; Seo, S.J.; Park, I.K.; Kim, S.H.; Kim, T.H.; Hoshiba, T.; Harada, I.; Akaike, T. Galactose-carrying polymers as extracellular matrices for liver tissue engineering. Biomaterials 2006, 27, 576–585. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, Q.S.; Yan, K.; Qi, Y.; Wang, G.F.; Cui, Y.L. Preparation, characterization, and evaluation of genipin crosslinked chitosan/gelatin three-dimensional scaffolds for liver tissue engineering applications. J. Biomed. Mater. Res. A 2016, 104, 1863–1870. [Google Scholar] [CrossRef]
- Yan, Y.; Wang, X.; Pan, Y.; Liu, H.; Cheng, J.; Xiong, Z.; Lin, F.; Wu, R.; Zhang, R.; Lu, Q. Fabrication of viable tissue-engineered constructs with 3D cell-assembly technique. Biomaterials 2005, 26, 5864–5871. [Google Scholar] [CrossRef]
- Jiankang, H.; Dichen, L.; Yaxiong, L.; Bo, Y.; Bingheng, L.; Qin, L. Fabrication and characterization of chitosan/gelatin porous scaffolds with predefined internal microstructures. Polymer 2007, 48, 4578–4588. [Google Scholar] [CrossRef]
- Yang, Z.; Xu, L.S.; Yin, F.; Shi, Y.Q.; Han, Y.; Zhang, L.; Jin, H.F.; Nie, Y.Z.; Wang, J.B.; Hao, X.; et al. In vitro and in vivo characterization of silk fibroin/gelatin composite scaffolds for liver tissue engineering. J. Dig. Dis. 2012, 13, 168–178. [Google Scholar] [CrossRef]
- Fan, J.; Shang, Y.; Yuan, Y.; Yang, J. Preparation and characterization of chitosan/galactosylated hyaluronic acid scaffolds for primary hepatocytes culture. J. Mater. Sci. Mater. Med. 2010, 21, 319–327. [Google Scholar] [CrossRef]
- Turner, R.A.; Wauthier, E.; Lozoya, O.; McClelland, R.; Bowsher, J.E.; Barbier, C.; Prestwich, G.; Hsu, E.; Gerber, D.A.; Reid, L.M. Successful transplantation of human hepatic stem cells with restricted localization to liver using hyaluronan grafts. Hepatology 2013, 57, 775–784. [Google Scholar] [CrossRef]
- Dvir-Ginzberg, M.; Gamlieli-Bonshtein, I.; Agbaria, R.; Cohen, S. Liver Tissue Engineering within Alginate Scaffolds Effects of Cell-Seeding Density on Hepatocyte Viability, Morphology, and Function. Tissue Eng. 2003, 9, 757–766. [Google Scholar] [CrossRef]
- Kilbride, P.; Mahbubani, K.T.; Saeb-Parsy, K.; Morris, G.J. Engaging Cold to Upregulate Cell Proliferation in Alginate-Encapsulated Liver Spheroids. Tissue Eng. Part C Methods 2017, 23, 455–464. [Google Scholar] [CrossRef]
- Glicklis, R.; Shapiro, L.; Agbaria, R.; Merchuk, J.C.; Cohen, S. Hepatocyte behavior within three-dimensional porous alginate scaffolds. Biotechnol. Bioeng. 2000, 67, 344–353. [Google Scholar] [CrossRef]
- Yang, J.; Chung, T.W.; Nagaoka, M.; Goto, M.; Cho, C.-S.; Akaike, T. Hepatocyte-specific porous polymer-scaffolds of alginate-galactosylated chitosan sponge for liver-tissue engineering. Biotechnol. Lett. 2001, 23, 1385–1389. [Google Scholar] [CrossRef]
- Wang, B.; Hu, Q.; Wan, T.; Yang, F.; Cui, L.; Hu, S.; Gong, B.; Li, M.; Zheng, Q.C. Porous Lactose-Modified Chitosan Scaffold for Liver Tissue Engineering: Influence of Galactose Moieties on Cell Attachment and Mechanical Stability. Int. J. Polym. Sci. 2016, 2016, 1–8. [Google Scholar] [CrossRef]
- She, Z.; Jin, C.; Huang, Z.; Zhang, B.; Feng, Q.; Xu, Y. Silk fibroin/chitosan scaffold: Preparation, characterization, and culture with HepG2 cell. J. Mater. Sci. Mater. Med. 2008, 19, 3545–3553. [Google Scholar] [CrossRef]
- She, Z.; Zhang, B.; Jin, C.; Feng, Q.; Xu, Y. Preparation and in vitro degradation of porous three-dimensional silk fibroin/chitosan scaffold. Polym. Degrad. Stab. 2008, 93, 1316–1322. [Google Scholar] [CrossRef]
- Lewis, P.L.; Shah, R.N. 3D Printing for Liver Tissue Engineering: Current Approaches and Future Challenges. Curr. Transplant. Rep. 2016, 3, 100–108. [Google Scholar] [CrossRef]
- Miller, J.S.; Stevens, K.R.; Yang, M.T.; Baker, B.M.; Nguyen, D.H.; Cohen, D.M.; Toro, E.; Chen, A.A.; Galie, P.A.; Yu, X.; et al. Rapid casting of patterned vascular networks for perfusable engineered three-dimensional tissues. Nat. Mater. 2012, 11, 768–774. [Google Scholar] [CrossRef]
- Gou, M.; Qu, X.; Zhu, W.; Xiang, M.; Yang, J.; Zhang, K.; Wei, Y.; Chen, S. Bio-inspired detoxification using 3D-printed hydrogel nanocomposites. Nat. Commun. 2014, 5, 3774. [Google Scholar] [CrossRef]
- Underhill, G.H.; Chen, A.A.; Albrecht, D.R.; Bhatia, S.N. Assessment of hepatocellular function within PEG hydrogels. Biomaterials 2007, 28, 256–270. [Google Scholar] [CrossRef]
- Hammond, J.S.; Gilbert, T.W.; Howard, D.; Zaitoun, A.; Michalopoulos, G.; Shakesheff, K.M.; Beckingham, I.J.; Badylak, S.F. Scaffolds containing growth factors and extracellular matrix induce hepatocyte proliferation and cell migration in normal and regenerating rat liver. J. Hepatol. 2011, 54, 279–287. [Google Scholar] [CrossRef]
- Stevens, K.R.; Miller, J.S.; Blakely, B.L.; Chen, C.S.; Bhatia, S.N. Degradable hydrogels derived from PEG-diacrylamide for hepatic tissue engineering. J. Biomed. Mater. Res. A 2015, 103, 3331–3338. [Google Scholar] [CrossRef]
- Zimoch, J.; Padial, J.S.; Klar, A.S.; Vallmajo-Martin, Q.; Meuli, M.; Biedermann, T.; Wilson, C.J.; Rowan, A.; Reichmann, E. Polyisocyanopeptide hydrogels: A novel thermo-responsive hydrogel supporting pre-vascularization and the development of organotypic structures. Acta Biomater. 2018, 70, 129–139. [Google Scholar] [CrossRef]
- Hasirci, V.; Berthiaume, F.; Bondre, S.P.; Gresser, J.D.; Trantolo, D.J.; Toner, M.; Wise, D.L. Expression of Liver-Specific Functions by Rat Hepatocytes Seeded in Treated Poly(Lactic-co-Glycolic) Acid Biodegradable Foams. Tissue Eng. 2001, 7, 385–394. [Google Scholar] [CrossRef]
- Wang, X.; Rijff, B.L.; Khang, G. A building-block approach to 3D printing a multichannel, organ-regenerative scaffold. J. Tissue Eng. Regen. Med. 2017, 11, 1403–1411. [Google Scholar] [CrossRef]
- Bishi, D.K.; Mathapati, S.; Venugopal, J.R.; Guhathakurta, S.; Cherian, K.M.; Verma, R.S.; Ramakrishna, S. A Patient-Inspired Ex Vivo Liver Tissue Engineering Approach with Autologous Mesenchymal Stem Cells and Hepatogenic Serum. Adv. Healthc. Mater. 2016, 5, 1058–1070. [Google Scholar] [CrossRef]
- Huang, H.; Oizumi, S.; Kojima, N.; Niino, T.; Sakai, Y. Avidin-biotin binding-based cell seeding and perfusion culture of liver-derived cells in a porous scaffold with a three-dimensional interconnected flow-channel network. Biomaterials 2007, 28, 3815–3823. [Google Scholar] [CrossRef]
- Rad, A.T.; Ali, N.; Kotturi, H.S.; Yazdimamaghani, M.; Smay, J.; Vashaee, D.; Tayebi, L. Conducting scaffolds for liver tissue engineering. J. Biomed. Mater. Res. A 2014, 102, 4169–4181. [Google Scholar] [CrossRef]
- Blouin, A.; Bolender, R.P.; Weibel, E.R. Distribution of organelles and membranes between hepatocytes and nonhepatocytes in the rat liver parenchyma. A stereological study. J. Cell Biol. 1977, 72, 441–455. [Google Scholar] [CrossRef]
- Page, D.T.; Garvey, J.S. Isolation and characterization of hepatocytes and Kupffer cells. J. Immunol. Methods 1979, 27, 159–173. [Google Scholar] [CrossRef]
- Lee, H.; Han, W.; Kim, H.; Ha, D.H.; Jang, J.; Kim, B.S.; Cho, D.W. Development of Liver Decellularized Extracellular Matrix Bioink for Three-Dimensional Cell Printing-Based Liver Tissue Engineering. Biomacromolecules 2017, 18, 1229–1237. [Google Scholar] [CrossRef]
- Mazza, G.; Al-Akkad, W.; Rombouts, K.; Pinzani, M. Liver tissue engineering: From implantable tissue to whole organ engineering. Hepatol. Commun. 2018, 2, 131–141. [Google Scholar] [CrossRef]
- Ambekar, R.S.; Kandasubramanian, B. Progress in the Advancement of Porous Biopolymer Scaffold: Tissue Engineering Application. Ind. Eng. Chem. Res. 2019, 58, 6163–6194. [Google Scholar] [CrossRef]
- Lewis, P.L.; Green, R.M.; Shah, R.N. 3D-printed gelatin scaffolds of differing pore geometry modulate hepatocyte function and gene expression. Acta Biomater. 2018, 69, 63–70. [Google Scholar] [CrossRef]
| Natural Materials | Major Concerned Properties | Applications | References | |||||
|---|---|---|---|---|---|---|---|---|
| Biocompatible | Biodegradable | Hydrophilic | Thermal-Responsible | FDA | Other Characteristics | |||
| HA | Yes | Yes, hyaluronidases | Yes | Yes | Approved | Nonimmunogenic, non-adhesive, good swelling and creep compliance properties, photopolymerizable, promote cell mortality and proliferation, reduces long-term inflammation, hepatic elimination | Tissue engineering, wound healing, angiogenesis, etc. | [99,100] |
| Alginate | Yes | Yes, controllable | Yes | Yes | Approved | Nonimmunogenic, bioactive, ease of gelation, suitable for in situ injection; poor elasticity, poor cell adhesion, mechanical weakness, difficulties in handling and sterilization | Tissue engineering and regeneration, as model ECMs, drug delivery | [101,102] |
| Collagen | Yes | Yes | Yes | Yes | Approved | Good permeability, low immunogenicity, poor mechanical properties | Tissue engineering (including cartilage, ligament, vessel etc.) | [34,103] |
| Gelatin | Yes | Yes, very fast | Yes | Yes | Approved | Ease of manipulation, high mechanical properties, easy to form films and matrix hydrogels, very viscous polymer, low thermal stability, low cost | Tissue engineering, drug discovery | [104,105] |
| Cellulose | Yes | Yes | Yes | Yes | Approved | Noncytotoxic, good thermal and mechanical properties, hydrogels with a high water content | Various derivatives in biomedical field | [32] |
| Matrigel | Yes | Yes | Yes | Yes | No | Bioactive, mechanical weakness, batch-to-batch variation, undefined composition | 3D models, cell culture, mimic ECMs | [106,107,108] |
| Chitosan | Yes | Yes, lysozyme | Yes | Yes | Approved | Nonimmunogenic, good host response, high antimicrobial activity, very viscous polymer solution and pH-responsive, sufficient mechanical properties | Tissue engineering, e.g., liver, bone, skin, vessels | [31,89] |
| Agarose | Yes | Yes | Yes | Yes | No | High mechanical strength, ability to maintain the cellular phenotype | Mimics the microenvironment for hepatocytes | [97] |
| Fibrin | Yes | Yes | No | Yes | Approved | Easily autologous isolation, uniform cell distribution, limited mechanical strength, inflammatory response | Tissue engineering scaffolds, blood blotting, fertility preservation | [33,109,110] |
| PHAs | Yes | Yes | No | Yes | No | Non-toxic, piezoelectric properties, brittleness, tendency to crystallize | Tissue engineering including LTE, drug carrier, would healing | [29,111] |
| Synthetic Materials | Major Concerned Properties | Applications | References | |||||
|---|---|---|---|---|---|---|---|---|
| Biocompatible | Biodegradable | Hydrophilic | Thermal-Responsive | FDA | Other Characteristics | |||
| PAA | Yes | No | Yes | No | Approved | Various derivatives, excellent optical transparency and stability in water | Degradable or thermal-responsive derivatives for drug delivery | [31] |
| PVA | Yes | No | Yes | Yes | Approved | Inefficient elasticity, stiff membrane, lack of cell adhesion, ease of fabrication and sterilization | Tissue engineering, both medical and nonmedical devices | [36,137] |
| PIC | Yes | No | Yes | Yes | No | Semiflexible properties, strain stiffening | Tissue engineering and cancer immunotherapy | [138,139] |
| PEG | Yes | No | Yes | No | Approved | Hydrolytically bioactive, photocrosslinkable, easily modifiable | Widely used in for chemical, biological, and commercial purposes, and also in tissue engineering | [31,140] |
| PLGA | Yes | Yes, controlled | No | Yes | Approved | Poor load-bearing properties, hydrolytically unstable; good cell adhesion and proliferation | Medical devices, drug delivery, fabrication of tissue engineering matrices, suture reinforcements | [141,142] |
| PGA | Yes | Yes | Yes | No | Approved | Highly crystalline, high melting point, lacks elasticity, not soluble in most organic solvents, tends to lose mechanical strength | Absorbable sutures, orthopedic devices, scaffolding matrices for tissue regeneration | [81,143] |
| PLA | Yes | Yes, slow | No | No | Approved | Lacks elasticity, high tensile strength, hydrolytically unstable | Orthopedic fixation devices | [143,144] |
| PCL | Yes, less | Yes. Low rate | No | Yes | Approved | Limited elasticity, tunable mechanical properties | Tissue engineering, long-term drug/vaccine delivery vehicle | [35,145] |
| Composition | Cell Source | Crosslinking Method | Output | Reference |
|---|---|---|---|---|
| Collagen, chitosan | Platelet and rat hepatocyte; rat hepatocyte | Chemical crosslinking; noncovalently linked | The matrix has excellent blood and cell compatibility; hepatocytes exhibited relatively high glutamate-oxaloacetate transaminase and glucose secretion functions | [79,114] |
| Collagen, chitosan, heparin | Platelet and rat hepatocyte | Chemical and physical crosslinking | Improved the blood compatability and maintained hepatocyte viability and function; exhibited high urea and triglyceride secretion functions | [80,113,115] |
| Collagen I, HA | Primary human hepatocytes and liver stellate cells | Physical crosslinking, UV crosslinker | Bioprinted 3D liver tissue constructs maintained liver functions including urea and albumin production | [113] |
| Gelatin, chitosan | Human HepG2; primary rat hepatocyte | Crosslinked with 1% genipin; crosslinked by glutaraldehyde solution | Cells cultured in 3D scaffolds preformed better on the structural characteristics, cell viability, growth and liver specific functions; supply living cells with nutrients and allow removing the cell metabolite; hepatocytes perform better in the well-defined scaffold | [167,168,169] |
| Gelatin, silk fibroin (SF) | Human normal hepatic QZG cell line | Use of glutaraldehyde solution to produce cross-linked gelatin solution and then mix with SF | Achieved better biocompatibility, controlled degradation, and good for the attachment and proliferation of cells | [170] |
| Gelatin | Primary rat hepatocytes | Gelatin is dissolved in hot NaCl and Tris-HCl | Rapid prototypedg hepatocytes remained viable and performed biological functions for more than 2 months | [116] |
| Gelatin, heparin | Human endothelial cells and HepG2 cells | Physical mixture | Helped cells to reconstruct a patent vascular tree within the decellularized porcine liver scaffold | [117] |
| Gelatin, polyurethane | Hepatocyte | Cross-linked with glutaraldehyde, enhanced by the addition of lysine | Generation of a hydrogel with controlled pore size and interconnectivity | [118] |
| GelMA | Human HepG2/C3A cells | Photocrosslinked | Bioprinted liver spheroids exhibited long-term functionality | [112] |
| HA, PEG | Human HepG2 cells, hiPS-HEPs | Bioorthogonal SPAAC crosslinked, modified with cyclic RGD peptides | hiPS-HEPs migrated and grew in 3D and showed an increased viability and higher albumin production compared to ctrols | [122] |
| HA, moieties; collagen III, laminin | Primary rat hepatocytes; hHpSCs | Galactose moieties were covalently coupled with HA through ethylenediamine; the is initiated by a PEGDA cross-linker | Formation of cellular aggregates with enhanced liver specific metabolic activities and improved cell density; permissive for survival and phenotypic stability of human hepatic stem cells and hepatoblasts | [171,172] |
| Fibrin | Rat hepatocyte; human hepatocytes, dermal fibroblasts, and UVECs | Human fibrinogen was applied with the thrombin solution to make the fibrin matrix | Supported engraftment and specific differentiation of viable hepatocytes; stimulated hepatocytes for the ectopic expansion of engineered human liver tissue seeds; in vitro-generated liver tissues can expand and function in vivo | [110,123,125] |
| Fibrin, PLGA | Rat hepatocytes and ADSCs | Formed by the pollymerization of fibrinogen acted by protease thrombin | Assembled to be an implantable endothelialized liver tissue, along with a hierarchical vascular network | [124] |
| Alginate | Mouse primary hepatocytes; HepG2 cells | Freezedry technique; crosslinked in CaCl2 solution | Maintained hepatocyte genotype, produced hepatic-specific proteins for two weeks; liver spheroids displayed an enhanced cell proliferation; importance of cell density within weakly adhesive alginate scaffolds; a cold reduction in temperature display an enhanced cell proliferation | [101,126,127,173,174] |
| Alginate, galactosylated chitosan | Primary hepatocytes | Calcium crosslinked; lyophilization | Enhanced hepatocyte aggregation; improved cell attachment and viability | [175,176] |
| Alginate (Alg), glycyrrhizin (GL), calcium (Ca) | HepG2 cells | Calcium crosslinked equal volume mixture of GL, nano-CaCO3 and Alg | GL–Alg–Ca hydrogel was homogenous complex with stable structure and well viscoelasticity, and cells showed good biocompatibility, and maintained the viability, proliferation and liver function | [128] |
| Chitosan | HepG2 cells | The microfluidic fabrication process for pure chitosan microfibers | HepG2 cells were self-aggregated with a spheroid shape, showing a higher liver specific function (albumin secretion and urea synthesis). | [129] |
| Lactose-modified chitosan (Lact-CTS) | Normal liver cell | Coupling of lactose with chitosan was carried out by the reducing agent, addition of NaBH4 | Lact-CTS with 48.62% of galactose moieties could facilitate the cell attachment and possess great biocompatibility and mechanical stability | [177] |
| Chitosan, gelatin | Hepatoytes | Crosslinked by glutaraldehyde solution | Scaffold produced with predefined multilevel internal architectures (a flow-channel network and hepatic chambers) and improved hepatocytes performance greatly in comparison with a porous scaffold | [130] |
| Silk fibroin/chitosan (SFCS) | HepG2 cells | Freezing and lyophilization | Provided a matrix with homogeneous porous structure, controllable pore size and mechanical properties | [178,179] |
| Chitosan nanofibers, fibronectin | Primary rat hepatocytes, endothelial cells | Fabricated by the electrospinning technique | Enhanced cell attachment and maintained their morphologies and functions | [131] |
| PHBVHHx | UC-MSCs, hepatocyte cells | Solid–liquid phase separation method to form scaffolds | Injured mice liver were recovered; generated tissue looked similar to the organ | [132,133] |
| Native nanofibrillar cellulose (NFC) | Human hepatic cell lines HepaRG and HepG2 | Physically crosslinked | Provided mechanical support for cell growth and differentiation, and induced spheroid formation of HepaRG and HepG2 cells. | [82] |
| Cellulose nanocrystral (CNCs), alginate | Human hepatoma cells, fibroblasts | Crosslinked with CaCl2 | The bioink formulation was suitable to print a liver mimetic honeycomb 3D structure containing fibroblast and heptatoma cells | [135] |
| Nanofibrillar cellulose, HA-gelatin | Human HepaRG liver progenitor cells, | HG hydrogel based on thiol-modified HA, thiol-modified gelatin and crosslinker PEGDA | Induced apicobasal polarity and functional bile canaliculi-like structures, expediting the hepatic differentiation of HepaRG liver progenitor cells better than the standard 2D culture | [136] |
| Agarose, carbohydrate glass | Primary rat hepatocytes and fibroblasts | Chain entanglements, physical crosslinking | Primary hepatocytes and fibroblasts were cast | [180,181] |
| Agarose–chitosan (AG–CH) | Primary rat hepatocytes | Crosslinke by glutaraldehyde | The hepatic functions like albumin secretion and urea synthesis were established in the 3D scaffold | [97] |
| PEG, heparin | Primary rat hepatocytes, BMEL; cryopreserved primary human hepatocytes, induced pluripotent stem cells (iPSCs) | UV light polymerization; chemically crosslinked | Demonstrated the importance of cell–cell and cell–matrix interactions in BMEL cell and primary hepatocyte survival. Aggregation and encapsulation of iPS cells during their differentiation towards hepatocytes yielded microtissues that depicted stable albumin production on-chip and inducible CYP activity. The 3D in vitro liver model is capable of sustaining advanced human-specific liver functions | [147,148,149,182,183] |
| PEG, PLGA, liver-derived ECM (L-ECM), growth factors | Rat liver | Physical and thermal crosslinking | L-ECM and growth factors enhanced tissue penetration into intrahepatically implanted biodegradable scaffolds and induced cell proliferation in the parenchyma that surrounds these scaffolds in the normal liver | [184] |
| PEG-DA, PEGDAAm, MMP-sensitive | Primary human fetal liver cells, HUVECs and HepG2 | Chemical crosslinking, photopolymerization | The 3D in vitro liver model is capable of sustaining advanced human-specific liver functions for at least 5 months in culture. Hepatic tissues survived and functioned for over 3 weeks after implantation | [150,185] |
| PIC, GRGDS peptide | Human dermal microvascular endothelial cells and fibroblasts | Polymerization of the corresponding monomers using a nickel perchlorate as a catalyst. | Supported pre-vascularization and the development of organotypic structures | [186] |
| PVA | Physical crosslinking by freeze–thaw cycless | Exhibited similar mechanical properties and morphological characteristics to porcine liver | [137] | |
| PVA, gelatin | HUVECs and HepG2 | Physically crosslinked by freeze–thaw cycles | Hydrogel particles with a well pronounced tendency towards association with hepatocytes and endothelial cells. | [152] |
| PLGA, AVAD; collagen-coated PLGA (C-PLGA); PLGA, gelatin | Pig liver transplantation; rat BMSCs; rat hepatocytes (HCs), nonparenchymal liver cells | Chemical and physical crosslinking | Demonstrated the feasibility of using AVADs in organ transplantation. Proved the superiority of the C-PLGA for hepatocytes differentiation. HCs cocultured with nonparenchymal cells can attach to and survive on the 3D polymer scaffolds. Cells recovered polarity and exhibited improved liver-specific function. Untreated PLGA performed best for supporting liver-specific functions. 3D printing and optimized parameters are applied for liver regeneration. | [83,84,154,155,187,188] |
| PGA, fibrin | Physical crosslinking | Effective in preventing biliary leakage | [156] | |
| PLA | Rat hepatocytes, rat hepatic stellate cells | Dissolved in 2,2,2-trifluoroethanol | Encouraged the rapid self-organization of 3D spheroids and the spheroids formed exhibit hepatocyte-specific functionality | [157] |
| PLAL | Rat hepatocyte | Chemical crosslinking | Contributed to hepatocyte engraftment, function, and expansion | [158] |
| PLA, fibroin; collagen I; discrete aligned nanofibers | HepG2 cells; rat hepatocyte | Chemical and thermal crosslinking | Improved the cell growth, enhancing cells adhesion and proliferation. Hepatocyte aggregates formed on nanofibers displayed excellent cell retention, cell activity and stable functional expression | [144,159] |
| PLLA, gelatin, HGF | BMSCs | Electrospinning, physical and chemical crosslinking | Effectively guide hepatic commitment of patient derived BMSCs | [9,189] |
| PCL, collagen | Primary rat hepatocytes, HUVECs and human lung fibroblasts (HLFs) | Physical and thermal crosslinking, 3D printing | The vascular formation and functional abilities of HCs demonstrated that the heterotypic interaction among HCs and nonparenchymal cells increased the survivability and functionality of HCs | [160] |
| PCL, ECM | HepG2 hepatocytes | Electrospinning, physical and thermal crosslinking | Provided a viable, translatable platform for hepatocytes, supporting in vivo phenotype and function | [161] |
| PCL | Human USSCs, self-renewing pluripotent cells | Physical crosslinking, electrospinning | Differentiation of USSCs demonstrated that this culture system can potentially be used as an alternative to the ECM-based culture for relevant hepatocyte-based applications in LTE | [162] |
| PCL, chitosan | Epithelial liver mouse cells. | Physical crosslinking, electrospinning | The porosity and pore is suitable for epithelial liver mouse cells infiltration, attachment, and material exchange | [163] |
| PAA, PET, collagen | Primary hepatocytes | Chemical an physical crosslinking, UV light induced polymerization | The growth kinetics of adhesion patch at primary hepatocyte cell substrate interface is changed upon PAA grafting | [164] |
| PAA, PEI, ELPs | Primary rat hepatocytes, | Chemical an physical crosslinking | ELP–polyelectrolyte conjugates profoundly influenced the morphology, aggregation and differentiation function of primary rat hepatocytes | [165] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ye, S.; Boeter, J.W.B.; Penning, L.C.; Spee, B.; Schneeberger, K. Hydrogels for Liver Tissue Engineering. Bioengineering 2019, 6, 59. https://doi.org/10.3390/bioengineering6030059
Ye S, Boeter JWB, Penning LC, Spee B, Schneeberger K. Hydrogels for Liver Tissue Engineering. Bioengineering. 2019; 6(3):59. https://doi.org/10.3390/bioengineering6030059
Chicago/Turabian StyleYe, Shicheng, Jochem W.B. Boeter, Louis C. Penning, Bart Spee, and Kerstin Schneeberger. 2019. "Hydrogels for Liver Tissue Engineering" Bioengineering 6, no. 3: 59. https://doi.org/10.3390/bioengineering6030059
APA StyleYe, S., Boeter, J. W. B., Penning, L. C., Spee, B., & Schneeberger, K. (2019). Hydrogels for Liver Tissue Engineering. Bioengineering, 6(3), 59. https://doi.org/10.3390/bioengineering6030059







