Using a 3D Navigation Template to Increase the Accuracy of Thoracic Pedicle Screws in Patients with Scoliosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Ethics and Patients’ Section
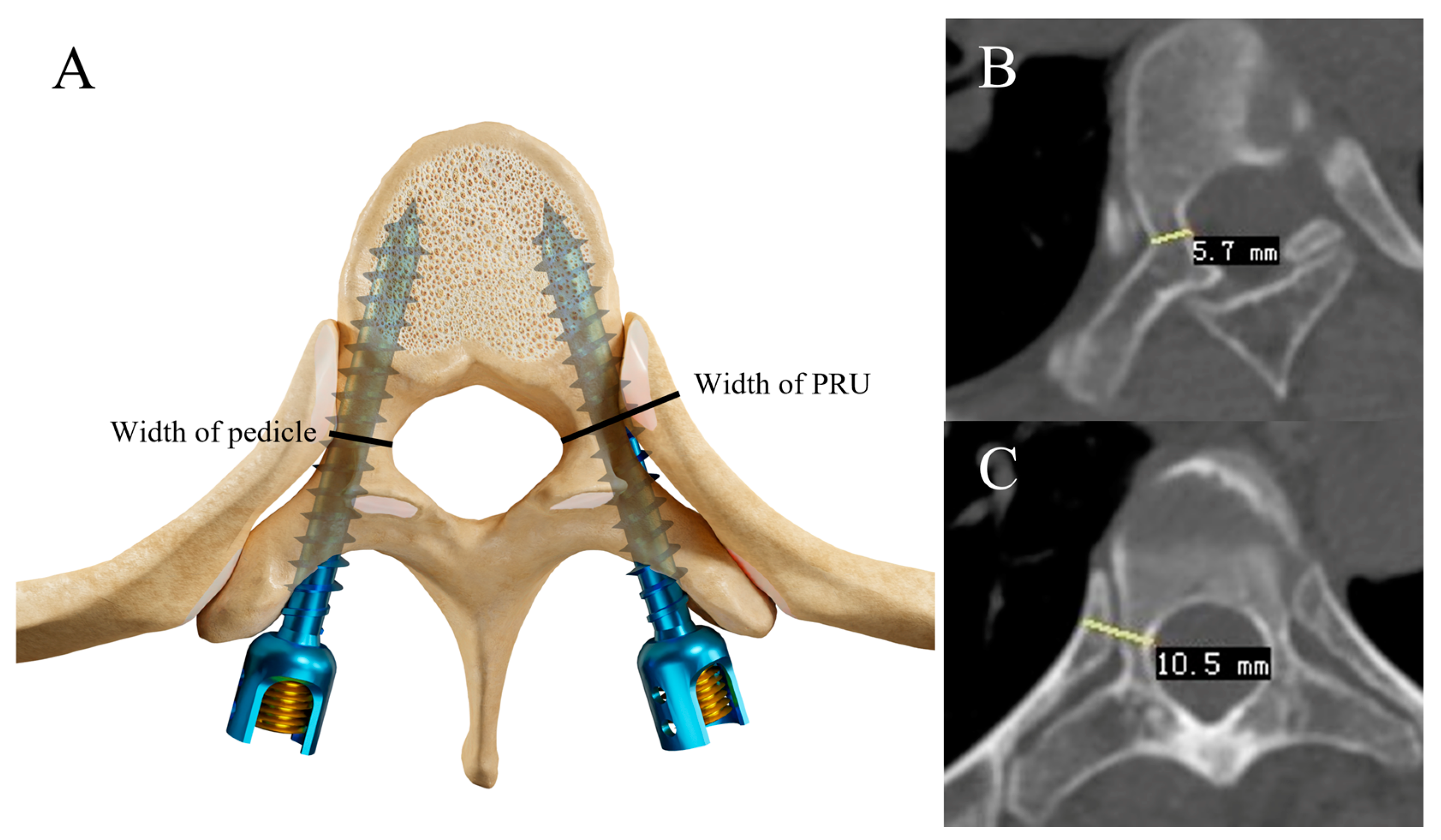
2.2. Preoperative Measurements
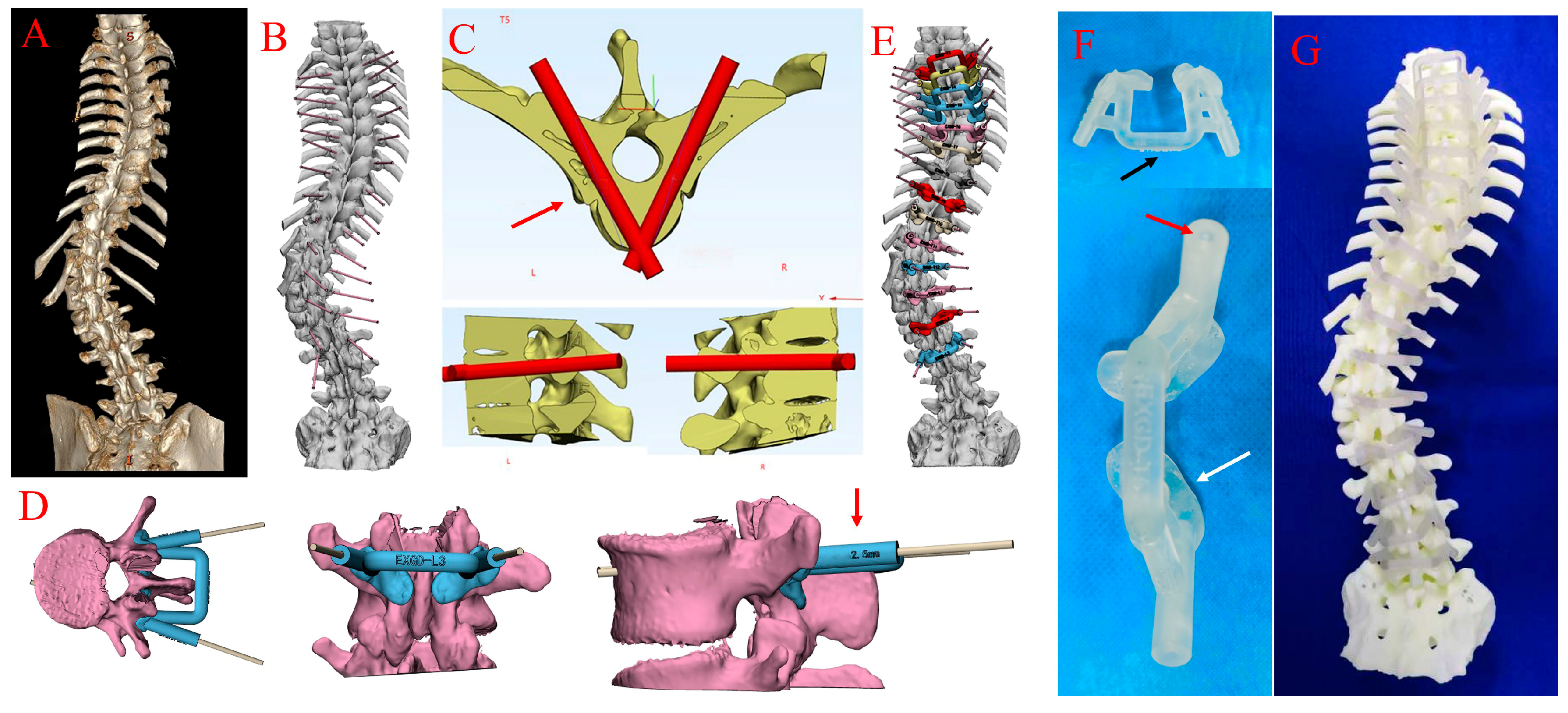
2.3. Fabrication of the Spine Model and 3D Navigation Templates
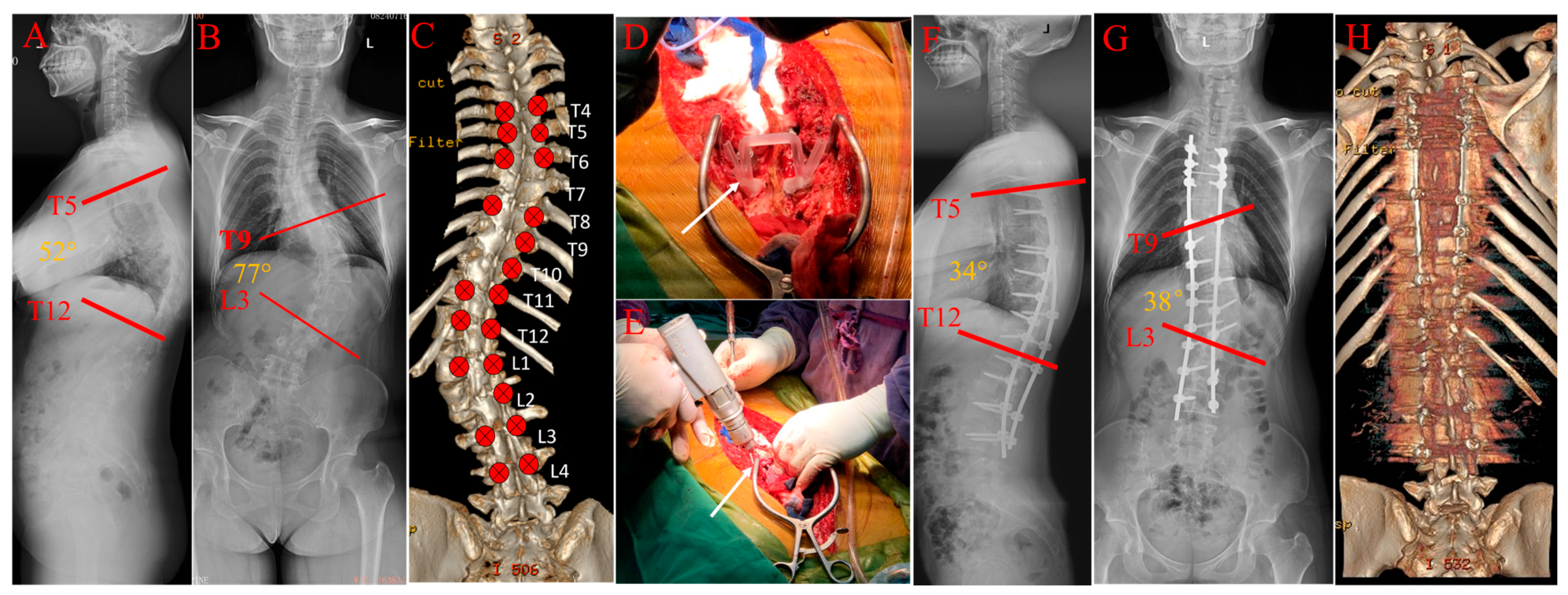
2.4. Surgical Procedures and the Use of 3D Navigation Templates
2.5. Methods of Pedicle Screw Grading
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Trial Registration
Data Availability Statement
Conflicts of Interest
References
- Miyazaki, M.; Ishihara, T.; Kanezaki, S.; Notani, N.; Abe, T.; Tsumura, H. Relationship between vertebral morphology and the potential risk of spinal cord injury by pedicle screw in adolescent idiopathic scoliosis. Clin. Neurol. Neurosurg. 2018, 172, 143–150. [Google Scholar] [CrossRef]
- Behensky, H.; Cole, A.A.; Freeman, B.J.; Grevitt, M.P.; Mehdian, H.S.; Webb, J.K. Fixed lumbar apical vertebral rotation predicts spinal decompensation in Lenke type 3C adolescent idiopathic scoliosis after selective posterior thoracic correction and fusion. Eur. Spine J. 2007, 16, 1570–1578. [Google Scholar] [CrossRef]
- Lenke, L.G.; Kuklo, T.R.; Ondra, S.; Polly, D.W., Jr. Rationale behind the current state-of-the-art treatment of scoliosis (in the pedicle screw era). Spine 2008, 33, 1051–1054. [Google Scholar] [CrossRef]
- Halm, H.; Niemeyer, T.; Link, T.; Liljenqvist, U. Segmental pedicle screw instrumentation in idiopathic thoracolumbar and lumbar scoliosis. Eur. Spine J. 2000, 9, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Ferlic, P.W.; Hauser, L.; Götzen, M.; Lindtner, R.A.; Fischler, S.; Krismer, M. Correction of adolescent idiopathic scoliosis using a convex pedicle screw technique with low implant density. Bone. Joint. J. 2021, 103, 536–541. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Yuan, S.; Tian, Y.; Wang, L.; Liu, X. Uniplanar Cannulated Pedicle Screws in the Correction of Lenke Type 1 Adolescent Idiopathic Scoliosis. World Neurosurg. 2021, 149, e785–e793. [Google Scholar] [CrossRef] [PubMed]
- Yan, K.; Zhang, Q.; Tian, W. Comparison of accuracy and safety between second-generation TiRobot-assisted and free-hand thoracolumbar pedicle screw placement. BMC Surg. 2022, 22, 275. [Google Scholar] [CrossRef] [PubMed]
- Modi, H.; Suh, S.W.; Song, H.R.; Yang, J.H. Accuracy of thoracic pedicle screw placement in scoliosis using the ideal pedicle entry point during the freehand technique. Int. Orthop. 2009, 33, 469–475. [Google Scholar] [CrossRef]
- Jin, M.; Liu, Z.; Liu, X.; Yan, H.; Han, X.; Qiu, Y.; Zhu, Z. Does intraoperative navigation improve the accuracy of pedicle screw placement in the apical region of dystrophic scoliosis secondary to neurofibromatosis type I: Comparison between O-arm navigation and free-hand technique. Eur. Spine J. 2016, 25, 1729–1737. [Google Scholar] [CrossRef]
- Li, C.; Li, H.; Su, J.; Wang, Z.; Li, D.; Tian, Y.; Yuan, S.; Wang, L.; Liu, X. Comparison of the Accuracy of Pedicle Screw Placement Using a Fluoroscopy-Assisted Free-Hand Technique with Robotic-Assisted Navigation Using an O-Arm or 3D C-Arm in Scoliosis Surgery. Global. Spine J. 2022, 21925682221143076. [Google Scholar] [CrossRef]
- Farshad, M.; Betz, M.; Farshad-Amacker, N.A.; Moser, M. Accuracy of patient-specific template-guided vs. free-hand fluoroscopically controlled pedicle screw placement in the thoracic and lumbar spine: A randomized cadaveric study. Eur. Spine J. 2017, 26, 738–749. [Google Scholar] [CrossRef]
- Guzek, R.H.; Mitchell, S.L.; Krakow, A.R.; Harshavardhana, N.S.; Sarkissian, E.J.; Flynn, J.M. Morphometric analysis of the proximal thoracic pedicles in Lenke II and IV adolescent idiopathic scoliosis: An evaluation of the feasibility for pedicle screw insertion. Spine Deform. 2021, 9, 1541–1548. [Google Scholar] [CrossRef] [PubMed]
- Jeswani, S.; Drazin, D.; Hsieh, J.C.; Shweikeh, F.; Friedman, E.; Pashman, R.; Johnson, J.P.; Kim, T.T. Instrumenting the small thoracic pedicle: The role of intraoperative computed tomography image-guided surgery. Neurosurg. Focus. 2014, 36, E6. [Google Scholar] [CrossRef] [PubMed]
- Hicks, J.M.; Singla, A.; Shen, F.H.; Arlet, V. Complications of pedicle screw fixation in scoliosis surgery: A systematic review. Spine 2010, 35, E465–E470. [Google Scholar] [CrossRef]
- Smith, J.S.; Klineberg, E.; Lafage, V.; Shaffrey, C.I.; Schwab, F.; Lafage, R.; Hostin, R.; Mundis, G.M., Jr.; Errico, T.J.; Kim, H.J.; et al. Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. J. Neurosurg. Spine 2016, 25, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Di Silvestre, M.; Parisini, P.; Lolli, F.; Bakaloudis, G. Complications of thoracic pedicle screws in scoliosis treatment. Spine 2007, 32, 1655–1661. [Google Scholar] [CrossRef]
- Kwan, M.K.; Loh, K.W.; Chung, W.H.; Chiu, C.K.; Hasan, M.S.; Chan, C.Y.W. Perioperative outcome and complications following single-staged Posterior Spinal Fusion (PSF) using pedicle screw instrumentation in Adolescent Idiopathic Scoliosis (AIS): A review of 1057 cases from a single centre. BMC Musculoskelet. Disord. 2021, 22, 413. [Google Scholar] [CrossRef] [PubMed]
- Radermacher, K.; Portheine, F.; Anton, M.; Zimolong, A.; Kaspers, G.; Rau, G.; Staudte, H.W. Computer assisted orthopaedic surgery with image based individual templates. Clin. Orthop. Relat. Res. 1998, 354, 28–38. [Google Scholar] [CrossRef]
- Fan, Y.; Du, J.P.; Wu, Q.N.; Zhang, J.N.; Hao, D.J. Accuracy of a patient-specific template for pedicle screw placement compared with a conventional method: A meta-analysis. Arch. Orthop. Trauma. Surg. 2017, 137, 1641–1649. [Google Scholar] [CrossRef]
- Cecchinato, R.; Berjano, P.; Zerbi, A.; Damilano, M.; Redaelli, A.; Lamartina, C. Pedicle screw insertion with patient-specific 3D-printed guides based on low-dose CT scan is more accurate than free-hand technique in spine deformity patients: A prospective, randomized clinical trial. Eur. Spine J. 2019, 28, 1712–1723. [Google Scholar] [CrossRef]
- Garg, B.; Gupta, M.; Singh, M.; Kalyanasundaram, D. Outcome and safety analysis of 3D-printed patient-specific pedicle screw jigs for complex spinal deformities: A comparative study. Spine J. 2019, 19, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Luo, M.; Wang, W.; Yang, N.; Xia, L. Does Three-dimensional Printing Plus Pedicle Guider Technology in Severe Congenital Scoliosis Facilitate Accurate and Efficient Pedicle Screw Placement? Clin. Orthop. Relat. Res. 2019, 477, 1904–1912. [Google Scholar] [CrossRef]
- Chen, Y.; Zeng, J.; Guan, J.; Guo, Y.; Wang, X.; Yao, G.; Wang, W.; Qi, W.; Kong, K. Reformatted computed tomographic evaluation of the thoracic pedicle in a Chinese population for the surgical application of transpedicular screw placement. Surg. Radiol. Anat. 2010, 32, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Soh, T.L.T.; Kho, K.C.; Lim, Z.K.; Tandon, A.A.; Kaliya-Perumal, A.K.; Oh, J.Y. Morphological Parameters of the Thoracic Pedicle in an Asian Population: A Magnetic Resonance Imaging-Based Study of 3324 Pedicles. Global. Spine J. 2021, 11, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Catan, H.; Buluç, L.; Anik, Y.; Ayyildiz, E.; Sarlak, A.Y. Pedicle morphology of the thoracic spine in preadolescent idiopathic scoliosis: Magnetic resonance supported analysis. Eur. Spine J. 2007, 16, 1203–1208. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, S.P.; Pai Kanhangad, M.; Gullia, A. Curve severity and apical vertebral rotation and their association with curve flexibility in adolescent idiopathic scoliosis. Musculoskelet. Surg. 2021, 105, 303–308. [Google Scholar] [CrossRef]
- Hwang, S.W.; Samdani, A.F.; Lonner, B.; Miyanji, F.; Stanton, P.; Marks, M.C.; Bastrom, T.; Newton, P.O.; Betz, R.R.; Cahill, P.J. Impact of direct vertebral body derotation on rib prominence: Are preoperative factors predictive of changes in rib prominence? Spine 2012, 37, E86–E89. [Google Scholar] [CrossRef]
- Lenke, L.G.; Bridwell, K.H.; Baldus, C.; Blanke, K. Analysis of pulmonary function and axis rotation in adolescent and young adult idiopathic scoliosis patients treated with Cotrel-Dubousset instrumentation. J. Spinal. Disord. 1992, 5, 16–25. [Google Scholar] [CrossRef]
- Shu, S.; Bao, H.; Zhang, Y.; Gu, Q.; Zhang, T.; Jing, W.; Liu, Z.; Qiu, Y.; Zhu, Z. Selection of Distal Fusion Level for Lenke 5 Curve: Does the Rotation of the Presumed Lower Instrumented Vertebra Matter? Spine 2020, 45, E688–E693. [Google Scholar] [CrossRef]
- O’Brien, M.F.; Lenke, L.G.; Mardjetko, S.; Lowe, T.G.; Kong, Y.; Eck, K.; Smith, D. Pedicle morphology in thoracic adolescent idiopathic scoliosis: Is pedicle fixation an anatomically viable technique? Spine 2000, 25, 2285–2293. [Google Scholar] [CrossRef]
- Nash, C.L., Jr.; Moe, J.H. A study of vertebral rotation. J. Bone. Joint. Surg. Am. 1969, 51, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Husted, D.S.; Haims, A.H.; Fairchild, T.A.; Kershaw, T.S.; Yue, J.J. Morphometric comparison of the pedicle rib unit to pedicles in the thoracic spine. Spine 2004, 29, 139–146. [Google Scholar] [CrossRef] [PubMed]
- White, K.K.; Oka, R.; Mahar, A.T.; Lowry, A.; Garfin, S.R. Pullout strength of thoracic pedicle screw instrumentation: Comparison of the transpedicular and extrapedicular techniques. Spine 2006, 31, E355–E358. [Google Scholar] [CrossRef] [PubMed]
- Raley, D.A.; Mobbs, R.J. Retrospective computed tomography scan analysis of percutaneously inserted pedicle screws for posterior transpedicular stabilization of the thoracic and lumbar spine: Accuracy and complication rates. Spine 2012, 37, 1092–1100. [Google Scholar] [CrossRef]
- Aoude, A.A.; Fortin, M.; Figueiredo, R.; Jarzem, P.; Ouellet, J.; Weber, M.H. Methods to determine pedicle screw placement accuracy in spine surgery: A systematic review. Eur. Spine J. 2015, 24, 990–1004. [Google Scholar] [CrossRef]
- Bridwell, K.H.; Shufflebarger, H.L.; Lenke, L.G.; Lowe, T.G.; Betz, R.R.; Bassett, G.S. Parents’ and patients’ preferences and concerns in idiopathic adolescent scoliosis: A cross-sectional preoperative analysis. Spine 2000, 25, 2392–2399. [Google Scholar] [CrossRef]
- Rivkin, M.A.; Yocom, S.S. Thoracolumbar instrumentation with CT-guided navigation (O-arm) in 270 consecutive patients: Accuracy rates and lessons learned. Neurosurg. Focus. 2014, 36, E7. [Google Scholar] [CrossRef]
- Barzilay, Y.; Schroeder, J.E.; Hiller, N.; Singer, G.; Hasharoni, A.; Safran, O.; Liebergall, M.; Itshayek, E.; Kaplan, L. Robot-assisted vertebral body augmentation: A radiation reduction tool. Spine 2014, 39, 153–157. [Google Scholar] [CrossRef]
- Alaid, A.; von Eckardstein, K.; Smoll, N.R.; Solomiichuk, V.; Rohde, V.; Martinez, R.; Schatlo, B. Robot guidance for percutaneous minimally invasive placement of pedicle screws for pyogenic spondylodiscitis is associated with lower rates of wound breakdown compared to conventional fluoroscopy-guided instrumentation. Neurosurg. Rev. 2018, 41, 489–496. [Google Scholar] [CrossRef]
- Liu, K.; Zhang, Q.; Li, X.; Zhao, C.; Quan, X.; Zhao, R.; Chen, Z.; Li, Y. Preliminary application of a multi-level 3D printing drill guide template for pedicle screw placement in severe and rigid scoliosis. Eur. Spine J. 2017, 26, 1684–1689. [Google Scholar] [CrossRef]
- Pan, Y.; Lü, G.H.; Kuang, L.; Wang, B. Accuracy of thoracic pedicle screw placement in adolescent patients with severe spinal deformities: A retrospective study comparing drill guide template with free-hand technique. Eur. Spine J. 2018, 27, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Zhang, X.; Liu, H.; Yao, Z.; Bai, Y.; Guo, D.; Feng, L. 3D printed templates improve the accuracy and safety of pedicle screw placement in the treatment of pediatric congenital scoliosis. BMC Musculoskelet. Disord. 2021, 22, 1014. [Google Scholar] [CrossRef]
- Tian, W.; Lang, Z. Placement of pedicle screws using three-dimensional fluoroscopy-based navigation in lumbar vertebrae with axial rotation. Eur. Spine J. 2010, 19, 1928–1935. [Google Scholar] [CrossRef] [PubMed]
- Ho, E.K.; Upadhyay, S.S.; Ferris, L.; Chan, F.L.; Bacon-Shone, J.; Hsu, L.C.; Leong, J.C. A comparative study of computed tomographic and plain radiographic methods to measure vertebral rotation in adolescent idiopathic scoliosis. Spine 1992, 17, 771–774. [Google Scholar] [CrossRef]
- Qiao, J.; Zhu, F.; Xu, L.; Liu, Z.; Sun, X.; Qian, B.; Jiang, Q.; Zhu, Z.; Qiu, Y. Accuracy of pedicle screw placement in patients with Marfan syndrome. BMC Musculoskelet. Disord. 2017, 18, 123. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Yuan, Z.S.; Spiker, W.R.; Dong, W.X.; Sun, X.Y.; Yuan, J.B.; Zhang, J.; Zhu, B. A comparative study on the accuracy of pedicle screw placement assisted by personalized rapid prototyping template between pre- and post-operation in patients with relatively normal mid-upper thoracic spine. Eur. Spine J. 2016, 25, 1706–1715. [Google Scholar] [CrossRef] [PubMed]
- Ron, E. Let’s not relive the past: A review of cancer risk after diagnostic or therapeutic irradiation. Pediatr. Radiol. 2002, 32, 739–744; discussion 751–754. [Google Scholar] [CrossRef] [PubMed]

| Template Group | Free-Hand Group | |
|---|---|---|
| Number | 8 | 7 |
| Age (Year) | 27.8 ± 12.8 | 29.9 ± 18.4 |
| Gender(M/F) | (0/8) | (1/6) |
| Diagnosis | Idiopathic scoliosis (5 cases) | Idiopathic scoliosis (5 cases) |
| Congenital scoliosis (3 cases) | Degenerative scoliosis (2 cases) | |
| Mean Cobb Angle (°) | 61 ± 11° | 56 ± 17° (* n = 6) |
| Pedicle Number | Mean Pedicle Width (mm) | Mean PRU Width (mm) | ||
|---|---|---|---|---|
| Template | 138 | 6.1 ± 2.6 | - | |
| Free-hand | 126 | 6.2 ± 2.6 | - | |
| Thoracic | Template | 101 | 5.5 ± 2.1 | 12.7 ± 2.1 (* n = 100) |
| Free-hand | 91 | 5.5 ± 2.0 | 12.4 ± 2.3 (n = 91) | |
| Concave | Template | 72 | 6.1 ± 2.5 | 13.0 ± 2.1 |
| Free-hand | 63 | 6.3 ± 2.5 | 12.4 ± 2.3 | |
| Convex | Template | 66 | 6.1 ± 2.6 | 12.4 ± 2.1 |
| Free-hand | 63 | 6.2 ± 2.7 | 11.6 ± 3.3 | |
| Grade 0 | Grade I | Grade II | Grade III | Grade IV | Total | |
|---|---|---|---|---|---|---|
| Free-hand (** n = 6) | 18 | 21 | 15 | 1 | 0 | 55 |
| Template | 20 | 39 | 10 | 4 | 1 | 74 |
| G 0 | G 1 | G 2 | G 3 | Total | Accuracy | Safety | ||
|---|---|---|---|---|---|---|---|---|
| Total | Template | 97 | 27 | 14 | 0 | 138 | 70.3% | 89.9% |
| Free-hand | 78 | 36 | 12 | 0 | 126 | 61.9% | 90.5% | |
| Thoracic | Template | 76 | 16 | 9 | 0 | 101 | 75.3% | 91.1% |
| Free-hand | 55 | 27 | 9 | 0 | 91 | 60.4% | 90.1% | |
| Concave | Template | 46 | 20 | 6 | 0 | 72 | 63.9% | 91.7% |
| Free-hand | 34 | 19 | 10 | 0 | 63 | 54.0% | 84.1% | |
| Convex | Template | 51 | 7 | 8 | 0 | 65 | 77.3% | 89.2% |
| Free-hand | 44 | 17 | 2 | 0 | 63 | 69.8% | 96.8% | |
| Free-Hand | Template | |||
|---|---|---|---|---|
| Rotation Classification | Grade I | Grade II | Grade I | Grade II |
| Accuracy | 69.2% | 56.0% | 76.1% | 55.0% |
| Template | Free-Hand | |
|---|---|---|
| Number of vertebrae | 74 | 69 |
| Drainage volume (mL) | 1027.9 ± 414.2 | 982.4 ± 225.4 |
| Complications | CSF leak (2 cases) | None |
| Postoperative hospital stay (day) | 15.4 ± 5.1 | 14.1 ± 6.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, C.-H.; Shi, Y.; Sun, Y.-M.; Cai, M.-J.; Wu, H.-L.; Hu, L.-S.; Yu, L.-M.; Wang, P.; Shen, J.; Huang, Y.-C.; et al. Using a 3D Navigation Template to Increase the Accuracy of Thoracic Pedicle Screws in Patients with Scoliosis. Bioengineering 2023, 10, 756. https://doi.org/10.3390/bioengineering10070756
Jiang C-H, Shi Y, Sun Y-M, Cai M-J, Wu H-L, Hu L-S, Yu L-M, Wang P, Shen J, Huang Y-C, et al. Using a 3D Navigation Template to Increase the Accuracy of Thoracic Pedicle Screws in Patients with Scoliosis. Bioengineering. 2023; 10(7):756. https://doi.org/10.3390/bioengineering10070756
Chicago/Turabian StyleJiang, Cheng-Hao, Yan Shi, Yong-Mei Sun, Ming-Jun Cai, Hai-Long Wu, Li-Sheng Hu, Li-Min Yu, Peng Wang, Jie Shen, Yong-Can Huang, and et al. 2023. "Using a 3D Navigation Template to Increase the Accuracy of Thoracic Pedicle Screws in Patients with Scoliosis" Bioengineering 10, no. 7: 756. https://doi.org/10.3390/bioengineering10070756
APA StyleJiang, C.-H., Shi, Y., Sun, Y.-M., Cai, M.-J., Wu, H.-L., Hu, L.-S., Yu, L.-M., Wang, P., Shen, J., Huang, Y.-C., & Yu, B.-S. (2023). Using a 3D Navigation Template to Increase the Accuracy of Thoracic Pedicle Screws in Patients with Scoliosis. Bioengineering, 10(7), 756. https://doi.org/10.3390/bioengineering10070756










