A New Simplified Autogenous Sinus Lift Technique
Abstract
1. Introduction
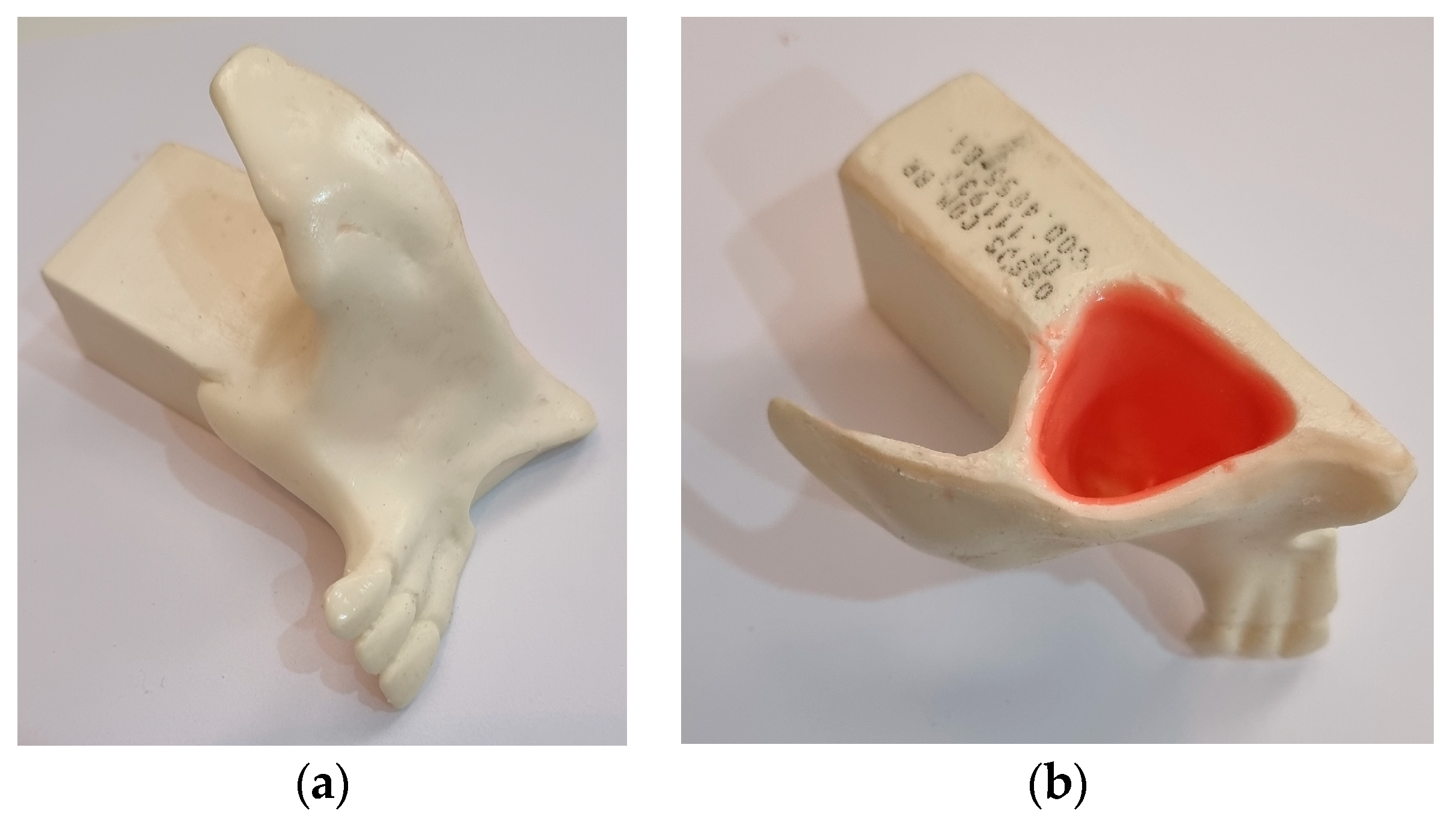
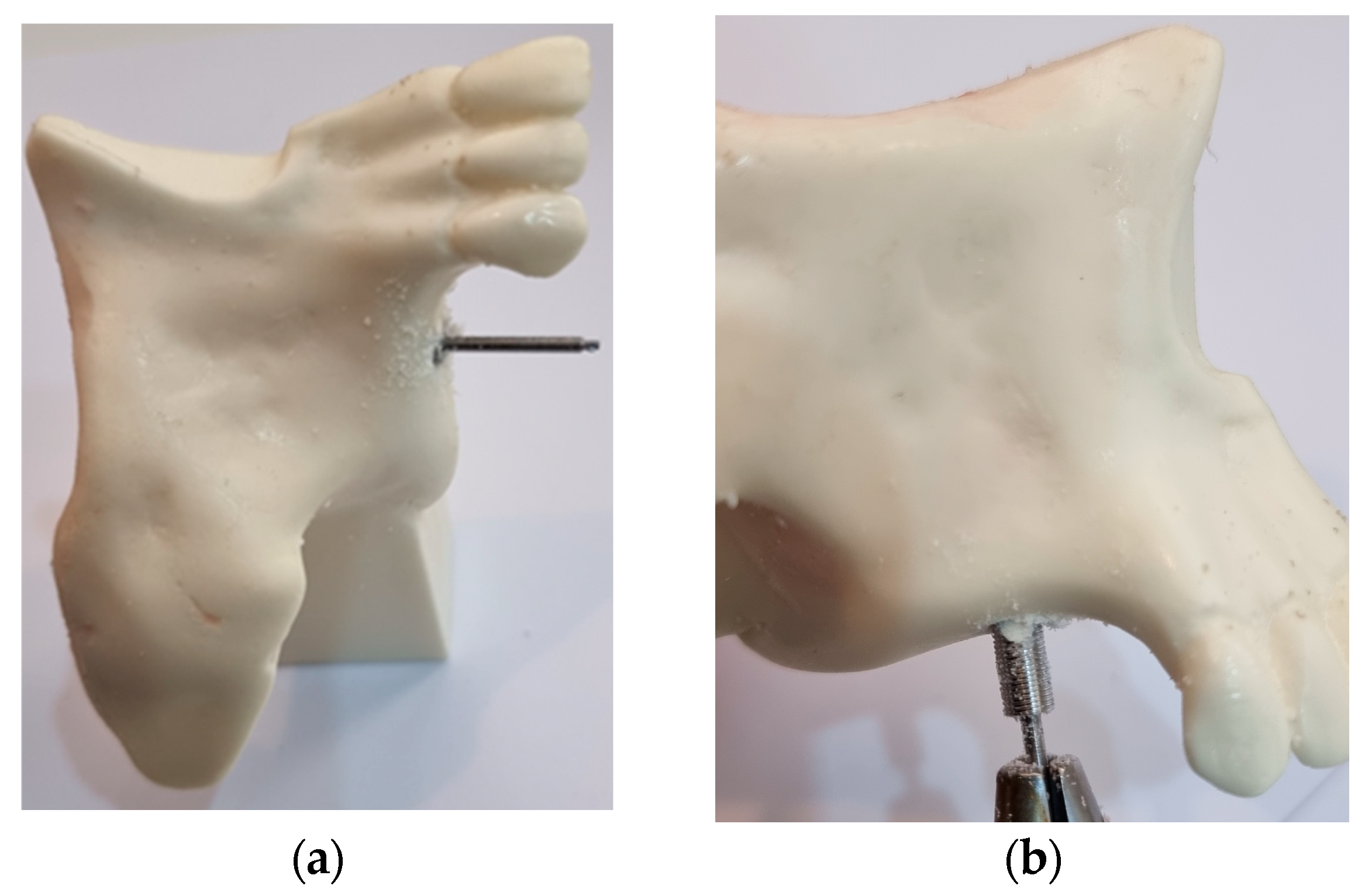
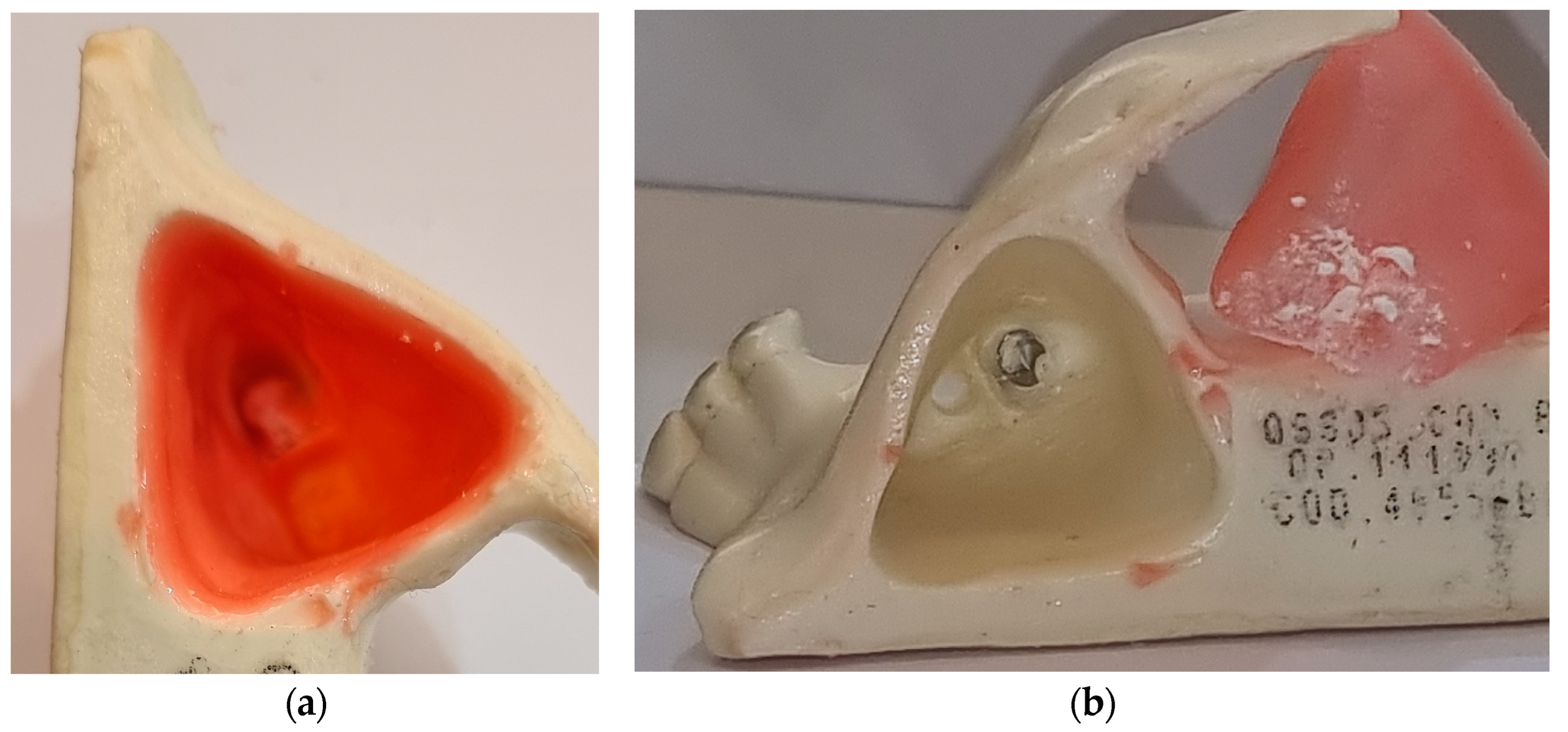
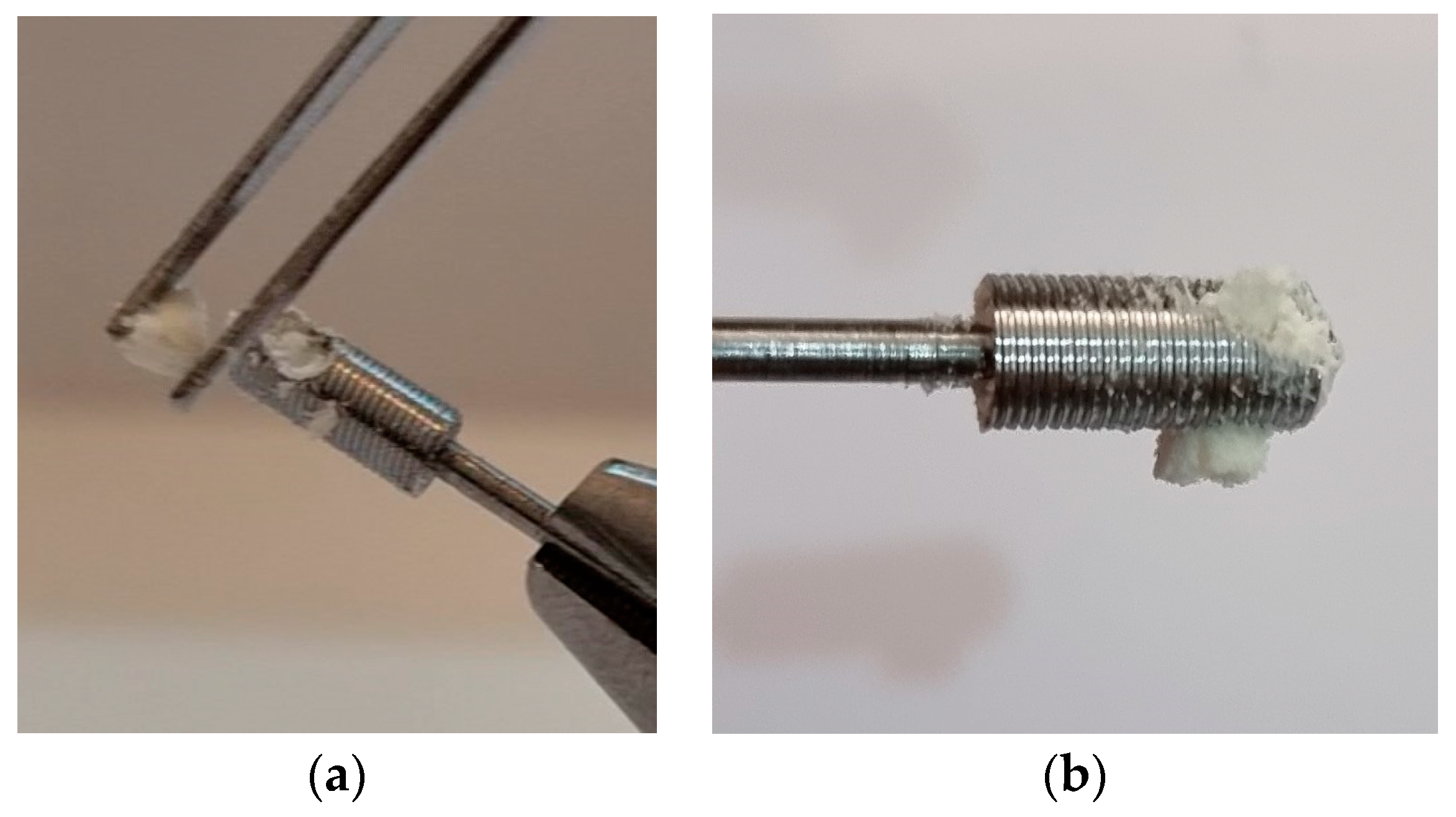
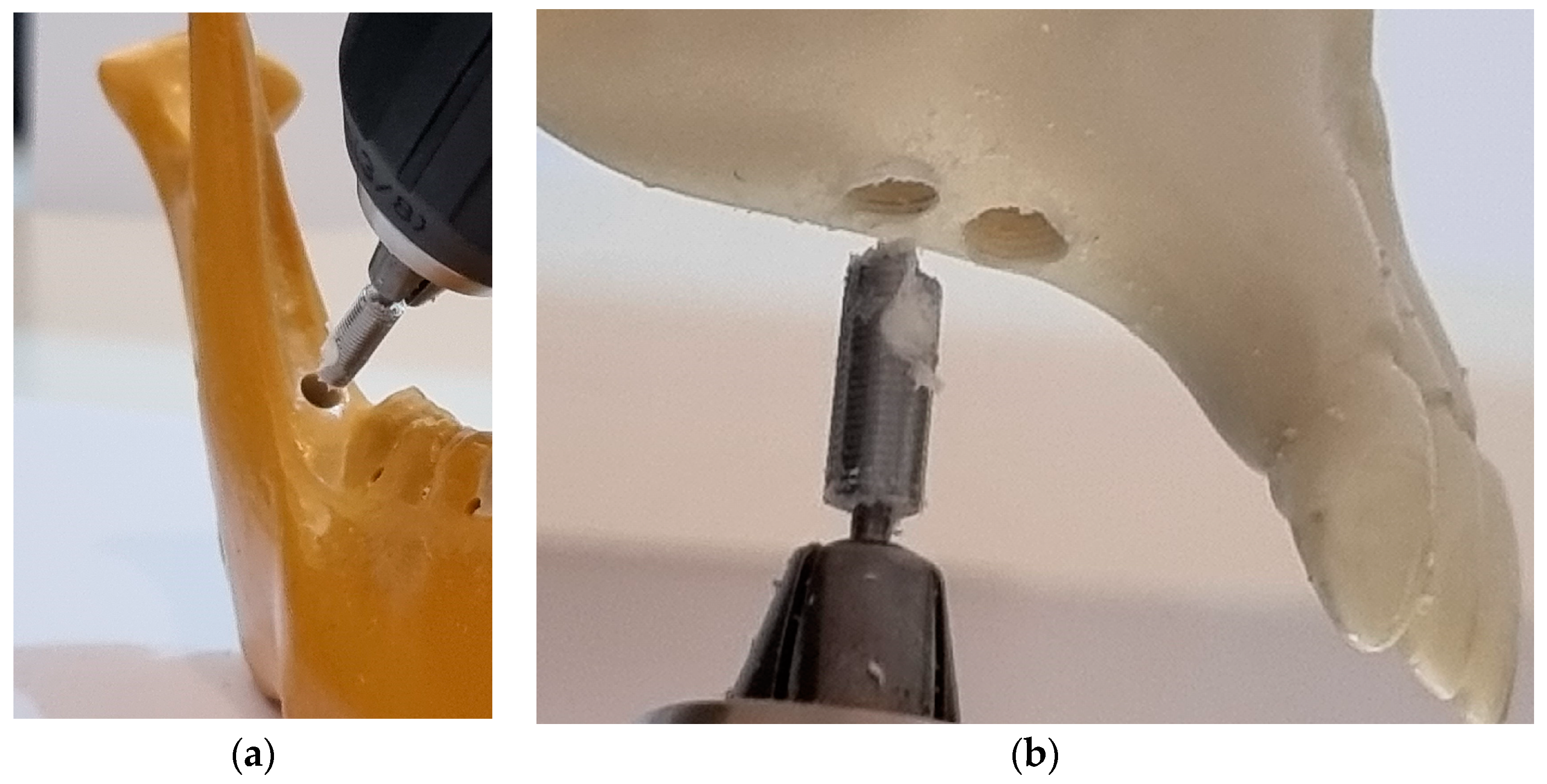
2. Materials and Methods
3. Results
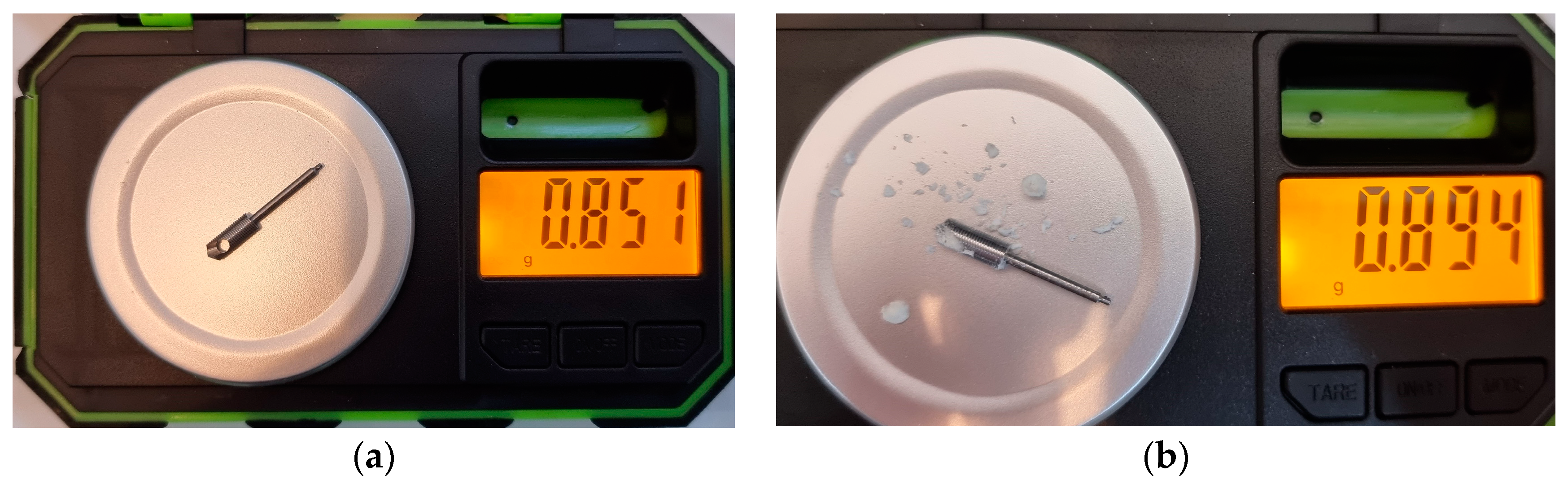
MIT and MRT
Weight Measurement
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raponi, I.; Giovannetti, F.; Buracchi, M.; Priore, P.; Battisti, A.; Scagnet, M.; Genitori, L.; Valentini, V. Management of orbital and brain complications of sinusitis: A practical algorithm. J. Craniomaxillofac. Surg. 2021, 49, 1124–1129. [Google Scholar] [CrossRef] [PubMed]
- Stern, A.; Green, J. Sinus Lift Procedures: An Overview of Current Techniques. Dent. Clin. N. Am. 2012, 56, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Bernardi, S.; Macchiarelli, G.; Bianchi, S. Autologous Materials in Regenerative Dentistry: Harvested Bone, Platelet Concentrates and Dentin Derivates. Molecules 2020, 25, 5330. [Google Scholar] [CrossRef] [PubMed]
- Rahate, P.S.; Kolte, R.A.; Kolte, A.P.; Bodhare, G.H.; Lathiya, V.N. Efficacy of simultaneous placement of dental implants in osteotome-mediated sinus floor elevation with and without bone augmentation: A systematic review and meta-analysis. J. Indian Soc. Periodontol. 2023, 27, 31–39. [Google Scholar] [PubMed]
- Nasr, S.; Slot, D.E.; Bahaa, S.; Dörfer, C.E.; Fawzy El-Sayed, K.M. Dental implants combined with sinus augmentation: What is the merit of bone grafting? A systematic review. J. Craniomaxillofac. Surg. 2016, 44, 1607–1617. [Google Scholar] [CrossRef]
- Boyne, P.J.; James, R.A. Grafting of the maxillary sinus floor with autogenous marrow and bone. J. Oral Surg. 1980, 38, 613–616. [Google Scholar]
- Summers, R.B. A new concept in maxillary implant surgery: The osteotome technique. Compendium 1994, 15, 152, 154–156, 158. [Google Scholar]
- Ferrigno, N.; Laureti, M.; Fanali, S. Dental implants placement in conjunction with osteotome sinus floor elevation: A 12-year life-table analysis from a prospective study on 588 ITI implants. Clin. Oral Implant. Res. 2006, 17, 194–205. [Google Scholar] [CrossRef]
- Del Fabbro, M.; Corbella, S.; Weinstein, T.; Ceresoli, V.; Taschieri, S. Implant survival rates after osteotome-mediated maxillary sinus augmentation: A systematic review. Clin. Implant Dent. Relat. Res. 2012, 14 (Suppl. 1), e159–e168. [Google Scholar] [CrossRef]
- Gu, Y.X.; Shi, J.Y.; Zhuang, L.F.; Qian, S.J.; Mo, J.J.; Lai, H.C. Transalveolar sinus floor elevation using osteotomes without grafting in severely atrophic maxilla: A 5-year prospective study. Clin. Oral Implants Res. 2016, 27, 120–125. [Google Scholar] [CrossRef]
- Krennmair, S.; Hunger, S.; Forstner, T.; Malek, M.; Krennmair, G.; Stimmelmayr, M. Implant health and factors affecting peri-implant marginal bone alteration for implants placed in staged maxillary sinus augmentation: A 5-year prospective study. Clin. Implant Dent. Relat. Res. 2019, 21, 32–41. [Google Scholar] [CrossRef]
- Giovannetti, F.; Raponi, I.; Priore, P.; Macciocchi, A.; Barbera, G.; Valentini, V. Minimally-Invasive Endoscopic-Assisted Sinus Augmentation. J. Craniofac. Surg. 2019, 30, e359–e362. [Google Scholar] [CrossRef]
- Jamcoski, V.H.; Faot, F.; Marcello-Machado, R.M.; Melo, A.C.M.; Fontão, F.N.G.K. 15-Year Retrospective Study on the Success Rate of Maxillary Sinus Augmentation and Implants: Influence of Bone Substitute Type, Presurgical Bone Height, and Membrane Perforation during Sinus Lift. Biomed. Res. Int. 2023, 2023, 9144661. [Google Scholar] [CrossRef]
- Johansson, L.A.; Isaksson, S.; Lindh, C.; Becktor, J.P.; Sennerby, L. Maxillary sinus floor augmentation and simultaneous implant placement using locally harvested autogenous bone chips and bone debris: A prospective clinical study. J. Oral Maxillofac. Surg. 2010, 68, 837–844. [Google Scholar] [CrossRef]
- Beck-Broichsitter, B.E.; Gerle, M.; Wiltfang, J.; Becker, S.T. Perforation of the Schneiderian membrane during sinus floor elevation: A risk factor for long-term success of dental implants? Oral Maxillofac. Surg. 2020, 24, 151–156. [Google Scholar] [CrossRef]
- Khehra, A.; Levin, L. Maxillary sinus augmentation procedures: A narrative clinical review. Quintessence Int. 2020, 51, 578–584. [Google Scholar] [CrossRef]
- Gandhi, Y. Sinus Grafts: Science and Techniques—Then and Now. J. Maxillofac. Oral Surg. 2017, 16, 135–144. [Google Scholar] [CrossRef]
- Tatum, H. Maxillary and sinus implant reconstruction. Dent. Clin. N. Am. 1986, 30, 207–229. [Google Scholar] [CrossRef]
- Chen, L.; Cha, J. An 8-year retrospective study: 1100 patients receiving 1557 implants using the minimally invasive hydraulic sinus condensing technique. J. Periodontol. 2005, 76, 482–491. [Google Scholar] [CrossRef]
- Browaeys, H.; Bouvry, P.; De Bruyn, H. A literature review on biomaterials in sinus augmentation procedures. Clin. Implant Dent. Relat. Res. 2007, 9, 166–177. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Natal, R.M.J. Structural analysis of the new Bioactive Kinetic Screw in titanium alloy vs. commercially pure titanium. J. Comp. Art. Int. Mec. Biomec. 2022, 2, 35–43. [Google Scholar]
- Andreucci, C.A.; Alshaya, A.; Fonseca, E.M.M.; Jorge, R.N. Proposal for a New Bioactive Kinetic Screw in an Implant, Using a Numerical Model. Appl. Sci. 2022, 12, 779. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. 3D Printing as an Efficient Way to Prototype and Develop Dental Implants. BioMedInformatics 2022, 2, 44. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. Increased Material Density within a New Biomechanism. Math. Comput. Appl. 2022, 27, 90. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. Bio-lubricant Properties Analysis of Drilling an Innovative Design of Bioactive Kinetic Screw into Bone. Designs 2023, 7, 21. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. Immediate Autogenous Bone Transplantation Using a Novel Kinetic Bioactive Screw 3D Design as a Dental Implant. BioMedInformatics 2023, 3, 299–305. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; Romasco, T.; Petrini, M.; Afrashtehfar, K.I.; Inchingolo, F.; Piattelli, A.; Di Pietro, N. Insertion Torque, Removal Torque, and Resonance Frequency Analysis Values of Ultrashort, Short, and Standard Dental Implants: An In Vitro Study on Polyurethane Foam Sheets. J. Funct. Biomater. 2023, 14, 10. [Google Scholar] [CrossRef]
- Ravidà, A.; Wang, I.C.; Sammartino, G.; Barootchi, S.; Tattan, M.; Troiano, G.; Laino, L.; Marenzi, G.; Covani, U.; Wang, H.L. Prosthetic Rehabilitation of the Posterior Atrophic Maxilla, Short (≤6 mm) or Long (≥10 mm) Dental Implants? A Systematic Review, Meta-analysis, and Trial Sequential Analysis: Naples Consensus Report Working Group A. Implant Dent. 2019, 28, 590–602. [Google Scholar] [CrossRef]
- Pierfelice, T.V.; D’Amico, E.; Iezzi, G.; Piattelli, A.; Di Pietro, N.; D’Arcangelo, C.; Comuzzi, L.; Petrini, M. Nanoporous Titanium Enriched with Calcium and Phosphorus Promotes Human Oral Osteoblast Bioactivity. Int. J. Environ. Res. Public Health 2022, 19, 6212. [Google Scholar] [CrossRef]
- Shockey, J.S.; von Fraunhofer, J.A.; Seligson, D. A measurement of the coefficient of static friction of human long bones. Surf. Technol. 1985, 25, 167–173. [Google Scholar] [CrossRef]
- Rosenholm, J.B.; Peiponen, K.P.; Gornov, E. Materials cohesion and interaction forces. Adv. Colloid Interf. Sci. 2008, 141, 48–65. [Google Scholar] [CrossRef]
- Steigenga, J.T.; Al-Shammari, K.F.; Nociti, F.H.; Misch, C.E.; Wang, H. Dental Implant Design and Its Relationship to Long-Term Implant Success. Implant Dent. 2003, 12, 306–317. [Google Scholar] [CrossRef]
- Lu, B.; Zhang, X.; Liu, B. A systematic review and meta-analysis on influencing factors of failure of oral implant restoration treatment. Ann. Palliat. Med. 2021, 10, 12664–12677. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. A New Simplified Autogenous Sinus Lift Technique. Bioengineering 2023, 10, 505. https://doi.org/10.3390/bioengineering10050505
Andreucci CA, Fonseca EMM, Jorge RN. A New Simplified Autogenous Sinus Lift Technique. Bioengineering. 2023; 10(5):505. https://doi.org/10.3390/bioengineering10050505
Chicago/Turabian StyleAndreucci, Carlos Aurelio, Elza M. M. Fonseca, and Renato N. Jorge. 2023. "A New Simplified Autogenous Sinus Lift Technique" Bioengineering 10, no. 5: 505. https://doi.org/10.3390/bioengineering10050505
APA StyleAndreucci, C. A., Fonseca, E. M. M., & Jorge, R. N. (2023). A New Simplified Autogenous Sinus Lift Technique. Bioengineering, 10(5), 505. https://doi.org/10.3390/bioengineering10050505







