Abstract
Recent human-centered developments in the industrial field (Industry 5.0) lead companies and stakeholders to ensure the wellbeing of their workers with assessments of upper limb performance in the workplace, with the aim of reducing work-related diseases and improving awareness of the physical status of workers, by assessing motor performance, fatigue, strain and effort. Such approaches are usually developed in laboratories and only at times they are translated to on-field applications; few studies summarized common practices for the assessments. Therefore, our aim is to review the current state-of-the-art approaches used for the assessment of fatigue, strain and effort in working scenarios and to analyze in detail the differences between studies that take place in the laboratory and in the workplace, in order to give insights on future trends and directions. A systematic review of the studies aimed at evaluating the motor performance, fatigue, strain and effort of the upper limb targeting working scenarios is presented. A total of 1375 articles were found in scientific databases and 288 were analyzed. About half of the scientific articles are focused on laboratory pilot studies investigating effort and fatigue in laboratories, while the other half are set in working places. Our results showed that assessing upper limb biomechanics is quite common in the field, but it is mostly performed with instrumental assessments in laboratory studies, while questionnaires and scales are preferred in working places. Future directions may be oriented towards multi-domain approaches able to exploit the potential of combined analyses, exploitation of instrumental approaches in workplace, targeting a wider range of people and implementing more structured trials to translate pilot studies to real practice.
1. Introduction
The last decade has been characterized by a revolution in the industrial sector that integrates several technologies to achieve high productivity and efficiency (Industry 5.0) [1]. The automatization of processes and the interaction between human and robot, the use of devices, and the burden of work-related diseases lead to an increasing interest in the physical and psychological state of the workers [2]. Moreover, the European Agency for Safety and Health at Work conducts the European Survey of Enterprises on New and Emerging Risks (ESENER) every four years beginning since 2009, highlighting the risks related to the workplace and, also, the psychosocial risks [3]. Industry 5.0 aims at creating a synergy between humans and autonomous machines [4], driving the transition to a human-centered and sustainable industry [1]. These recent human-centered developments in the industrial field lead companies and stakeholders to ensure the wellbeing of the industrial workers, prevent diseases and perform assessments in workplaces, assembly lines and industries, and see this as a fundamental step to improve working conditions and reduce work-related musculoskeletal disorders (WRMSD) [5]. This recent crucial step leads to an investment of resources and research mutating techniques, sensors [6] and findings from the bioengineering field, in order to apply it to the industry to enhance the industrial environments in several ways. Following this line, factors such as upper limb fatigue, strain and effort have been repeatedly measured and assessed for various purposes including, as a main target, the customization of working cells and the design of supportive devices that have effects on mental health protection, load reduction for multiple aims, including the design of supportive devices, [7] and improvements in ergonomics [8], in order to reduce work absenteeism [9] and increased well-being. These scenarios are frequently depicted in recent research projects, where several human factors are involved, including humans interaction with robots, physical and mental health monitoring in order to guarantee workers with improved working conditions and promoting workers’ good mental health, biomechanical parameters assessment [10,11], physiological measures [12], and ergonomics improvement [13]. However, since these practices have been adopted only recently, and not yet in a systematic way, we observed that often there is not a correspondence between tests made in laboratory and those carried out in working environments in real factories, leading to a gap between potential applications and those that are implemented in workplaces. Fatigue, strain and effort are generally used to refer to the physical exertion needed to perform an activity and to the associated perceived weakness and pain. Physical fatigue describes a progressive decrease in physical performance due to a prolonged sustained activity [14]; physical strain indicates an excessive physical workload during an activity that can lead to an injury [15]; physical effort refers to the use of energy needed to perform the activity [16]. Although these terms are distinct and may underlie slightly different assessments, they have a wide area of intersection and, thus, we analyzed them together in this work, referring to them with the acronym FSE (fatigue, strain and effort). Very few comprehensive reviews are available that summarize common good practice and golden standard guidelines to determine and assess workers’ FSE, and they are limited to specific scopes and very targeted fields of research. The available reviews are usually sectorial and have a more focused scope, and describe in detail specific fields, such as exoskeleton-assisted work [17], fatigue monitoring with wearable systems [18] or physical fatigue detection in construction workers [19].
Moreover, considering the large scope of industrial applications, a variety of studies, investigations and setups were implemented, considering different protocols and scenarios, as well as a variety of study designs and assessments, with very non-homogeneous approaches. Previous reviews have already summarized some of the aspects related to biomechanical fatigue in the industrial scenarios, focusing on the studies that investigated the effect of job rotation and work-rest schemes, as well as work pace, cycle time and duty cycle, on the upper limb muscle fatigue [20]. The effects of these work organization factors on subjective fatigue or discomfort were also analyzed. Electromyography (EMG) was the most used measurement, and no consistent results were found related to the effects of job rotation on muscle activity and subjective measurements of fatigue.
This paper presents a systematic review of the studies and setups specifically aimed at evaluating and assessing the motor performance of the upper limb in the industrial field. First of all, the main topics addressed by the screened studies are presented, showing their main focus on upper limb FSE. Then, a comprehensive comparison between laboratory and working settings is reported, based on the systematic screening of many relevant features including the type of enrolled participants, the type of motor task, the use of support and interaction devices and the type of assessment used. Indeed, laboratory settings can reproduce a working scenario in a controlled environment and they can be used for the preliminary testing of devices and new methods of evaluation, allowing for the use of technological instrumentations that provide objective measures to perform the biomedical assessment, such as kinematic parameters and EMG signals. However, real working scenarios are different and the worker can be affected by multiple factors that are not present in the simulated environment. Therefore, it is fundamental to directly assess the workers on the workplace during their usual working activity in order to monitor their physical state, so that the working experience can be improved, work-related musculoskeletal disorders can be prevented, and human compliant working environments can be arranged, improving ergonomics, workloads and sustainability. Therefore, we wanted to analyze in detail the differences between laboratory and workplace studies, and to investigate if the biomechanical assessments used in laboratories are being transferred to real working scenarios. Finally, this review also provides critical comments on the current state-of-the-art approaches and future trends and directions lying at the interdisciplinary intersection between biomechanics, ergonomics and human-centered approaches for the industrial field.
2. Materials and Methods
This research was designed to answer the main research question (RQ 0): “How have biomechanical assessments of the upper limb in an industrial context been implemented for assessing fatigue, strain and effort?”. RQ 0 is further split into the following research questions, addressed for both the laboratory and working settings:
RQ (1) Which topics were addressed and which findings were obtained?
RQ (2) Which kind of setting was used for the studies?
RQ (3) What type and how many participants were targeted and which anatomical target was assessed?
RQ (4) What type of motor tasks and protocol design were studied?
RQ (5) Which analysis techniques were employed?
We thus considered scientific articles that applied a biomechanical analysis, targeting industrial applications, and we provided an overview of the main topics addressed, and the setups considered for applications, exploring the data analysis techniques. The international guidelines established by PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [21,22] were used.
2.1. Bibliographic Research Strategy
With the above-mentioned aims, the following procedure was employed for the literature screening. A collection of articles was obtained by screening Scopus and Web of Science (WOS), using a query based on the keywords: “shoulder”, “elbow”, “wrist”, “upper limb”, “upper extremity”, “arm”, “fatigue”, “effort”, “strain”, “workplace”, “industry”, “industrial”, “assessment”, “index”, “evaluation”, “biomechanics”, “measure”, “measurement” and all possible variants.
The formal logical query was (shoulder OR elbow OR wrist OR upper limb OR upper-limb OR upper extremity OR arm) AND (fatigue OR strain OR effort) AND (worker OR workplace OR industry OR industrial) AND (assessment OR index OR evaluation OR biomechanics OR measure OR measurement).
2.2. Eligibility Criteria and Study Selection
In the eligibility phase, we selected the articles relevant to the aim of this review. Screened articles had to satisfy all the following criteria:
- (A)
- To include the terms selected in the above reported query in the abstract and/or title and/or in the keywords.
- (B)
- To involve applications with biomechanical evaluations (in a broad sense, as this includes biomechanical models, EMG, and others).
- (C)
- To target laboratory or workplace scenarios, with a clear aim at industrial applications.
- (D)
- To be indexed in at least one of the screened databases.
- (E)
- To be a full journal article.
- (F)
- To be available in English.
The eligibility criterium was “criterium A AND criterium B AND criterium C AND criterium D AND criterium E AND criterium F”.
Lastly, some articles were also available before the year 2000. However, most of them regarded the use of obsolete technologies and methods, thus we decided not to include papers published before the year 2000. The screening was updated to the 31st of December 2022.
The selection process was performed with the papers screened one by one for inclusion by two different groups (made of subgroups of the authors of the review) independently. Each paper was screened by two different reviewers who blindly classified it as eligible or non-eligible. This allowed for a reduction in the risk of bias in the selection process. Any disagreement in the classification was settled by discussion between the two groups and a consensus was reached in all cases.
2.3. Data Extraction and Synthesis
Our review of the literature was organized to summarize the state-of-the-art information in the field by detailing the following categories:
2.3.1. Main Topics and Findings
This section aimed to summarize the main topics addressed in the works and in the obtained results, answering the research question: “Which main topics were addressed and which findings were obtained?”. Since the studies were based on specific design and a wide variety of aims, we summarized the results dividing all the studies into categories.
Basic research on biomechanical assessments in physiological conditions of fatigue: includes studies in which physiological effects of fatigue were investigated in order to find fatigue indicators during working activities.
Influence of task conditions on biomechanics: includes studies that investigate how the presence of external loads, and the type and speed of movements can affect the biomechanics.
Musculoskeletal diseases risk assessment: includes studies that performed assessments in a variety of workplaces and jobs, in order to investigate the risk of developing musculoskeletal diseases (MSD).
Effects of ergonomic interventions: includes studies that proposed and evaluated interventions in order to mitigate and prevent pain and musculoskeletal injuries.
Prevention and beneficial effects of exoskeletons/supporting devices: includes studies that examined the effects of the use of exoskeletons or other supporting devices on biomechanics.
Design and validation of assessment methods: includes studies that proposed and validated alternative methods and more objective measures in comparison to the traditional scales and questionnaires.
Protocols: includes studies that proposed some protocols to be implemented in the following years.
2.3.2. Setting
First of all, the studies were subdivided based on the setting, classified into “workplace”, “laboratory”, “simulated” and “protocol”. Then, all further analyses were performed dividing the selected papers in the following two categories: laboratory (that included also simulated and protocol studies that were considered as pilot work not performed on the field) and workplace.
2.3.3. Type of Participants, Number of Participants, Anatomical Target
This section characterized the participants that were enrolled in the studies, answering the research question, “What type and how many participants were targeted and which anatomical target was assessed?”, and it is subdivided into:
Type of participants: this section answered the question: “Which type of participants were enrolled?”. The type of participants enrolled in the studies were divided into “volunteers”, “workers” and “simulated subjects” (by simulated subjects, we mean those made with biomechanical simulations and modelling).
Number of participants: this section specified the number of participants enrolled in each of the studies, answering the question “How many participants were enrolled?”.
Anatomical target: this section answered: “Which upper limb segments were considered in the paper?”, specifying the targeted upper limb segments for functional assessment in “proximal joints” (shoulder and elbow), “distal joints” (wrist and hand) or “both”, in order to better specify which upper limb joints were used in biomechanical evaluations.
2.3.4. Tasks Type, Task Design, Task Support
This section described the design of the studies in terms of the characteristic of the motor tasks that were biomechanically analyzed, answering the research question “What type of motor tasks and protocol design were studied?”. This section was further divided into:
Task type: this section answered, “Which tasks were performed and analyzed?” and described the type of movements that were performed. We classified them into five main categories:
Lifting: studies in which participants were asked to lift weights as a primary task;
Postural: where participants were asked to hold a specific posture or train/test postural capabilities;
Functional: participants were asked to perform functional tasks that allow them to complete very specific goals;
Free: where participants could move freely in the environment, performing numerous tasks, in general and without clear or stringent constrains;
Others: all task types not belonging to the previous groups.
Task design: answered the question, “What was the design of the task and protocol?” and specifies the design of the task/protocol to be performed. We divided this section into three main groups:
Repetitive: participants performed the same task repetitively;
Controlled: participants performed tasks in specific constrained conditions;
Free: participants were not performing tasks with specific constrained conditions.
Task support: answered, “What supports were used to execute the tasks?” and specified which tools and devices were used to support the execution of the task. Supports were classified in 5 groups:
Free: tasks were performed without the use of specific tools;
Tool/handle: tasks required specific tools to be performed;
Exoskeleton/support: participants performed the task wearing exoskeletons or supporting devices;
Robot/end effector: tasks were performed in collaboration with a robotic end effector;
Others: tasks were performed with the use of devices not belonging to the previous categories.
2.3.5. Type of Assessments
This section described which techniques and findings were used for the data analysis, answering the question: “Which analysis techniques have been employed?”. The assessments were classified into:
EMG: the assessment included muscle activity signals measured with EMG;
Kinematics: kinematic parameters, such as articular angles, velocities and accelerations, were used for the assessment;
Biomechanics/kinetics: biomechanical parameters, such as torques, power and energy, were used for the assessment;
Questionnaires/scales: the assessment was done mainly using questionnaires and scales, such as the OCRA Checklist [23], the Nordic Musculoskeletal Questionnaire (NMQ) [24], the Rapid Entire Body Assessment (REBA) [25] and others;
RULA: the Rapid Upper Limb Assessment [26] was used for the assessment; this is a scale method developed for use in ergonomics investigations of workplaces where work-related upper limb disorders are reported [27], and gives quantitative indexes based on directed measurements of articular angles.
Strain index: the Strain Index [28] was used for the assessment. It is a job analysis tool that uses both qualitative and quantitative methods to identify jobs that do and do not expose workers to an increased risk of developing a distal upper extremity (DUE) disorder [27].
Other measurements: other measures not included in the other categories, such as heart rate, Near Infrared Spectroscopy (NIRS) and electroencephalography (EEG).
3. Results
3.1. Study Selection
As a result of the screening, 978 papers were found on Scopus and 930 on Web of Science. The total number of articles was 1908 and, after duplicates removal, the number of screened articles was 1375. Papers that were not in English and conference papers were not considered. Due to non-adherence to the eligibility criteria, 79% of the papers were excluded (n = 1087). Reasons for the exclusion were: the not-targeting of industrial or workplace scenarios, but clinical or merely laboratory applications with not-foreseen further applications in industrial scenarios; the absence of any quantitative method for assessment, or data non-presented; the lack of crucial information, lack of data or evident incompleteness in the data or methodology presentation; non-full-text studies. After the screening phase, the number of papers identified as eligible, meeting all the selection criteria and included in the review, was 288. In the next sections, the results of our research are presented. The PRISMA flow chart summarizing all the steps for screening and inclusion is presented in Figure 1.
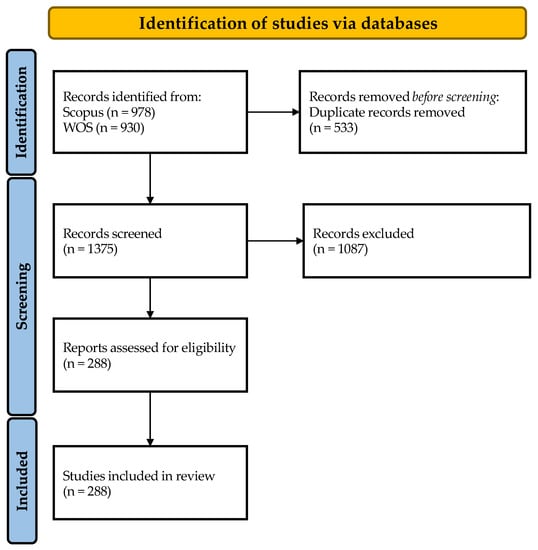
Figure 1.
The PRISMA flow chart for the proposed literature review.
3.2. Assessing FSE: Main Findings
In this section, we briefly report the main findings of the studies screened (see Table 1) in the assessment of fatigue, strain or effort, or a combination of those. Due to their variability in aims and purposes, we reported the main topics of investigation aggregated according to categories that divided studies by topic, summarizing the main findings. The categories were ordered to highlight the specific features of each research aim, from basic research to practical applications, including protocols, application of ergonomic assessments and use of supporting devices.

Table 1.
Summary of the main findings, divided into categories related to the topic of the investigation.
3.2.1. Basic Research on Biomechanical Assessments in Physiological Conditions of Fatigue
The physiological effects of fatigue during repetitive movements, overhead tasks and posture maintenance have been investigated in order to find indicators that can be used to identify fatigue during working activities. Joint angles and torques, especially at shoulder level, significantly reduce with fatigue [29,30]. Moreover, fatigue influences joint coordination that has to compensate for kinematic changes to maintain the trajectory of the end effector [31]. Systematic changes were found also on the power spectrum of the angular velocity and the acceleration of the shoulder and trunk [32]. Muscle fatigue is often detected with EMG signals, since spectral features such as the mean power frequency, the median frequency and the maximum voluntary contraction decrease with fatigue [33,34], clearly allowing the use of EMG as a biomarker for fatigue. Finally, the EMG signal can be associated with the EEG alpha band for the identification of mental and physical fatigue [35,36]. EMG and EEG signal coupling may provide a complete characterization of both the mental and physical state of the worker [317]. Indeed, physical and mental fatigue can be correlated in specific tasks, since the complexity and precision of the task increase fatigue [37].
3.2.2. Influence of Task Conditions on Biomechanics
During working activities, workers usually interact with objects and tools, and perform movement in various directions. The presence of external loads and the direction of movements can affect the biomechanics and, consequently, induce fatigue. Moreover, in industrial assembly lines or interacting with devices, the work pace and movement velocity may be constrained and uncomfortable for the worker. Therefore, some studies investigated how biomechanics is affected by the task conditions, such as the presence of external loads, velocity and direction of movement, in order to provide ergonomic recommendations for new workstations. In general, additional, external loads increase the muscular workload and pain, and decrease the endurance time [81,101], suggesting that light tools should be preferred. The direction and height of the movement have significant effects on the muscular strain and body posture, increasing the overall discomfort, pain and fatigue [82]. Therefore, workstations should be designed in order to improve working postures, maintaining a posture that is as neutral as possible [96]. Finally, the work pace may affect the development of FSE. In fact, fast movements without rest decrease the oxygen saturation and muscle activity [90] and, therefore, a slow pace with rest should be preferred.
3.2.3. Musculoskeletal Diseases Risk Assessment
Assessments during working activities were performed in a variety of workplaces and jobs, in order to investigate the risk of developing musculoskeletal diseases (MSD). In fact, physical risk factors at work and musculoskeletal disorders are associated with the increase of MSD [141]. The characterization of physical risk exposures of workers is needed in order to design tools and interventions capable of mitigating and, especially, preventing the development of MSD. Usually, scales and questionnaires such as REBA, RULA, SI and the OCRA checklist are used for risk evaluations since they can be administrated quickly on a large cohort of participants and they do not need specific architectures and equipment. However, some studies employed instrumental techniques, such as EMG, for the evaluation of the muscle activity during work and its correlation with MSD development [185]. Almost all the working activities analyzed resulted in having a high risk of MSD development, from industry and manual workers to office works, since these activities lead to high effort and strain. Moreover, repetitive activities [142] and high workloads [187] increase the risks of MSD. Therefore, ergonomic interventions are needed in order to correct working postures and to reduce pain and the risk of MSD [149].
3.2.4. Effects of Ergonomic Interventions
Since most of the working activities are classified as being at high risk for MSD development, ergonomic interventions are needed in order to mitigate and prevent pain and musculoskeletal injuries. Some studies investigate if and how ergonomic tools and workstations can improve working postures and decrease the risk of MSD with respect to commercial and traditional ones, which are not tailored for specific needs. In general, ergonomic tools and workstations improved postures and comfort and reduced the strain, effort and, consequently, the risk of MSD occurrence and musculoskeletal complaints [243,251]. Better working conditions also resulted in increased productivity and quality [253]. However, workers may need time to familiarize with the new tools [249]. Moreover, ergonomic educational training making the worker aware of the risks and physical exercise programs showed improved working postures, reducing muscle activity and musculoskeletal complaints [214,239]. These interventions improve both physical and mental health [250] and are thus beneficial for workers [318].
3.2.5. Prevention and Beneficial Effects of Exoskeletons/Supporting Devices
Repetitive tasks and posture maintenance (especially in overhead tasks) are one of the main causes of neck and back pain, and of joint load. Several exoskeletons and supportive devices, generally not actuated, have been developed to assist movements and postures during working activities. Exoskeletons reduce the muscles’ effort and joint load in the shoulder, arm and lower back [273,278], and this effect was proven in laboratory scenarios [258,272] and in preliminary campaigns conducted on field workers [263,265]. Thus, supporting devices reduce the EMG activity and fatigue, limiting the effects on joint torques and kinematics [270]. Moreover, the onset of muscular fatigue is delayed [280] and the oxygen consumption and heart rate are reduced [256]. Finally, the perceived effort and physical pain is reduced, improving the overall comfort of the worker [266,276].
3.2.6. Design and Validation of Assessment Methods
A variety of assessment methods can be used for the evaluation of fatigue and strain during work. The most employed methods are scales, but other alternative methods and more objective measures are proposed and validated with comparisons to the traditional scales and questionnaires. The reliability of scales and the accordance between different methods were assessed, finding that the Strain Index is more specific for the distal upper limb evaluation, while the OCRA checklist allows for the assessment of the whole upper limb [308]. SI was also found to be more effective than RULA and REBA in non-fixed tasks [309]. Furthermore, the usability and reliability of technologies that allow for quantitative assessments were tested. The use of inertial measurement units (IMU) or Kinect cameras for fatigue assessments allow for the detection of kinematic changes in long-duration manual tasks [286]. These methods are easy-to-use in real time and could assist ergonomists in risk evaluations on site [306]. Moreover, the EMG signal can provide measures for detecting muscular fatigue and they can be correlated to kinematic and kinetic parameters to evaluate the global fatigue [293].
3.2.7. Protocols
Some studies proposed protocols to be implemented in following studies. Three studies proposed new ergonomic intervention programs whose validity and efficacy will be tested with questionnaires and scales. Mathiassen et al. [313], instead, described an on-site biomechanical assessment, based on questionnaires and measurements of postures, movements and heart rate.
3.2.8. Fatigue, Strain and Effort of the Upper Limb in Industrial Applications: Main Findings
We divided the papers into three groups depending on the main design and findings related to the assessment of fatigue, strain and effort. It is documented that FSE are a burden for the industrial field and for workers, as it was reported that three out of five workers in the European Union had MSD complaints due to their working activity [319]. On the basis of such epidemiologic data, some studies assumed that the effects of FSE are in most of the cases present and they are working to reduce such effects [258,273]. FSE are not directly measured, but rather technologies, protocols, devices, exoskeletons, methods, ergonomic platforms or interventions aim at reducing or preventing the effects of FSE. Therefore, often the assessments are based on differential measures and the main focus is on the reduction in the effects of FSE. Some studies, instead, directly measure when FSE are found. Most of the studies reported that fatigue is found in industrial tasks in working places [150,167] but also in simulated environments [29,32]. In a limited number of studies, the effects of FSE were not observed or they were under the limit for high risk of MSD development [117,136]. All the effects are summarized in Figure 2 of each of the categories of the study.
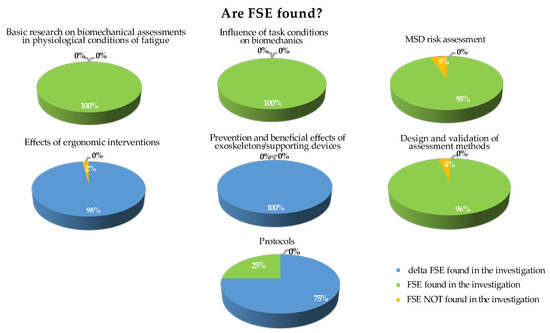
Figure 2.
Main findings on FSE. For each category, papers were classified based on the main findings related to FSE. Papers showing differential effects of ergonomic interventions or supporting devices on FSE were classified in blue; papers that found FSE were classified in green; papers that measured but did not find FSE were classified in yellow.
FSE are present in almost all the working activities, and represent a burden in the working scenario. Therefore, the assessment of FSE is important for preserving and improving workers’ health.
3.3. Setting
The setting categories used in this review paper were: workplace, laboratory, simulated and protocol studies. A total of 50% of the works were performed in a laboratory environment; 47% of the works were performed directly in the workplace (or considering data relative to the workplace). Few studies were suggested/approved protocols (not yet implemented) or simulated studies. A visual representation of the settings is reported in Figure 3. The selected studies split almost equally into two groups: those made in laboratory environments, and those performed in working places. All the following assessments are based on the separation and comparison of these two groups clearly identified in the setting section. Simulated and protocol studies were considered as laboratory studies, since they do not involve workers and/or volunteers directly in the workplace.
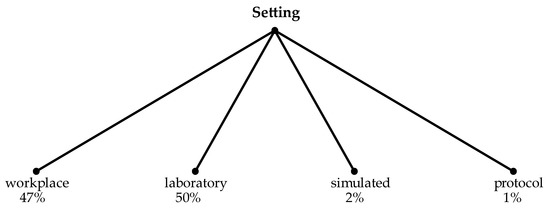
Figure 3.
Distribution of settings in the screened articles.
As shown in Figure 4, studies based on human-centered approaches for biomechanics of the upper limb in the industrial field are not new, even if the trend shows an increase in the papers published in the field in the last years (the screened papers are updated until the 31st of December 2022, with few papers already available and scheduled for publication for the year 2023). Interestingly, more recently, there has been an increase in the works based on laboratory settings, while the number of on-site works has stabilized. This trend could suggest that the interest is more focused on laboratory research activity than the translation of the assessments in the workplace. However, this finding should be commented in light of the fact that in the last three years, the restrictions due to COVID-19 may have impacted the on-field research.
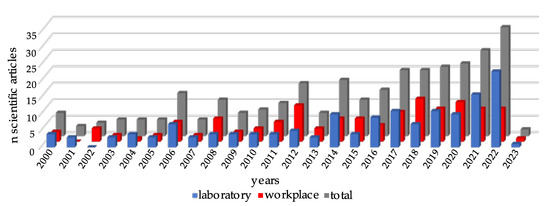
Figure 4.
Temporal distribution (number of scientific articles published per year) of the screened scientific articles from the year 2000 to December 2022, for laboratory settings (blue), working places (red) and overall (grey). Some scientific articles that were already accepted and will be published in 2023 are available.
3.4. Type of Participants, Number of Participants, Anatomical Target
3.4.1. Type of Participants
In the papers analyzed in this review, the cohorts of participants involved during the experimental sessions could be divided into 3 macro-categories: (i) volunteers, (ii) on-field workers and (iii) simulated subjects. In particular, 71% of the laboratory studies enrolled volunteers that did not have working experience related to the topic of the study and only 23% enrolled workers. In a minor number of laboratory studies (6%), the data were simulated starting from real recordings with biomechanical models (as in Brambilla et al. [109]) or completely simulated. Conversely, 99% of the workplace papers had enrolled workers. The categories of participants are graphically summarized in Figure 5. These results validate the choice to separate the laboratory and working places as they enrolled participants from different cohorts.
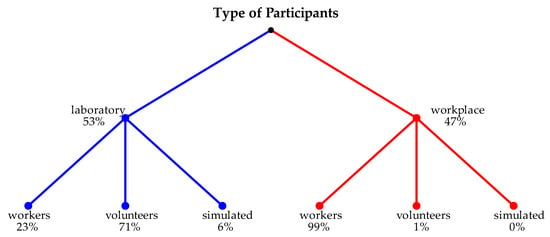
Figure 5.
Distribution of selected papers based on the cohort of participants enrolled in the laboratory setting (on the left) and in the workplace setting (on the right). Participants were classified as workers, volunteers and simulated.
3.4.2. Number of Participants
Considering the sample size, most of the laboratory studies involved less than 20 participants and only 10 papers involved more than 50 participants; the median number of participants was 14 and the 95th percentile was 68. In the workplace setting, most of the studies involved a high number of participants (>50) and 16 papers included more than 500 participants, with a maximum of 3141; the median number of participants was 62 and the 95th percentile was 560. Eight studies did not clearly declare the number of participants or presented protocols in which no participants were involved. A summary of the number of involved participants described in this section is reported in Figure 6.
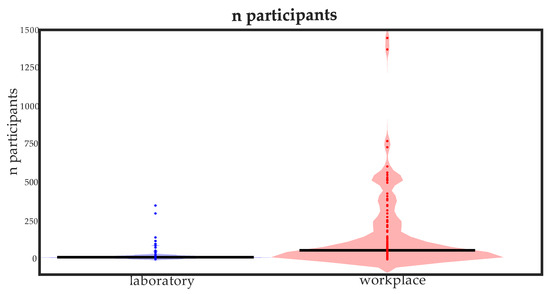
Figure 6.
Distribution of the number of participants for a laboratory setting (blue) and for a workplace setting (red). The points indicate the value for each article and the black line is the median value. The number of participants (3141) of one workplace study is not shown in the figure for visualization purposes.
Figure 7 summarizes the sample size for both the laboratory and workplace papers. In a laboratory setting, most of papers included less than 20 participants (31% of the papers had less than 10 participants, 45% had a number of participants between 10 and 20); 18% of the studies included between 20 and 50 participants, while only 6% included more than 50 participants and none considered more than 500. The workplace design, instead, included various numbers of participants, uniformly distributed. The participants were less than 10 in 13% of the papers, between 10 and 20 in 17% of the cases and between 20 and 50 in 14% of the papers. About 56% of the studies included more than 50 participants, in particular: 18% involved between 50 and 100 participants, 26% between 100 and 500 participants, and 12% more than 500 participants.
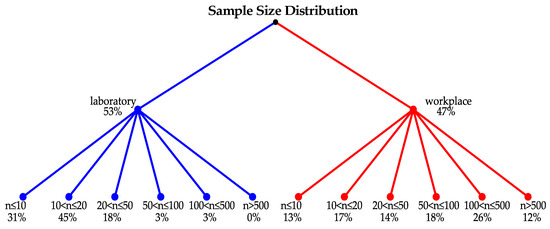
Figure 7.
Sample size distribution in the laboratory setting (on the left) and in the workplace setting (on the right). The sample size was divided in six groups: n ≤ 10, 10 < n ≤ 20, 20 < n ≤ 50, 50 < n ≤ 100, 100 < n ≤ 500 and n > 500.
3.4.3. Anatomical Target
In Figure 8, a detailed representation of the anatomical targets for the considered studies were reported. In the laboratory studies, 35% reported an analysis in proximal joints, 10% reported an analysis mainly on distal joints, while most of the studies (55%) reported an analysis on both the anatomical targets. In the workplace studies, 17% reported a proximal analysis, 10% reported a distal analysis, and the majority (73%) reported an analysis on both the proximal and distal targets. There was a tendency toward extending the analyses to the whole upper limb in the workplace studies in order to perform a comprehensive assessment of the workers, while the laboratory studies showed more targeted investigations.
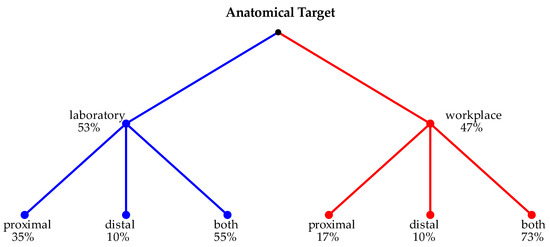
Figure 8.
Anatomical targets considered in the laboratory setting (on the left) and in the workplace setting (on the right).
3.5. Task Type, Task Design, Task Support
3.5.1. Task Type
Task type is reported in Figure 9. In the laboratory papers, most of the studies analyzed functional tasks (52%), followed by lifting tasks (20%) and postural tasks (14%); only 3% of the laboratory studies reported free movements. On the contrary, 38% of the workplace studies reported free movements and 43% functional movements. Only 3% of these papers regarded lifting tasks and 13% postural ones. In laboratory scenarios, the tasks generally reproduce specific movements of the working activities and, therefore, they could be precisely classified into categories. In workplace settings, instead, the tasks are functional movements when the participant performs only a specific task, while in the other cases, the workers perform multiple activities that are a combination of different functional subtasks.
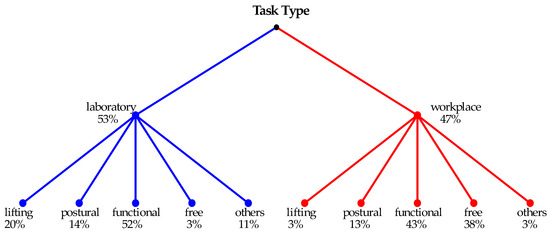
Figure 9.
Percentage of the task types for the laboratory setting (on the left) and for the workplace setting (on the right).
3.5.2. Task Design
Partially correlated with the task type, the task design showed that the laboratory studies were equally divided into repetitive (49%) and controlled (49%) movements that are by nature subject to experimental limitations, and only 2% of them considered unconstrained movements that represent more realistic working conditions in most of the cases. In the workplace studies, most of the studies (55%) considered unconstrained movements, 38% of the studies were based on a controlled design, and only 7% were conducted in repetitive conditions. The task design is reported in Figure 10.
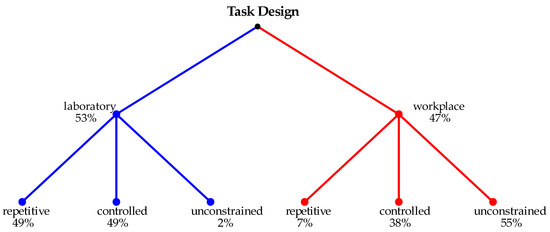
Figure 10.
Percentage of the task design for the laboratory setting (on the left) and for the workplace setting (on the right).
3.5.3. Task Support
Supports are intended in a broad sense and they include devices and robots, but also tools and handles. Various kinds of task support were employed in the screened studies. Since most of the laboratory studies regarded the interaction with the environment and simulation of controlled tasks, 42% of them required tools and handles, including screwdrivers, hand supports, and others; 38% were based on free movements, while other supports (3%), end effector (EE) robots (1%) and exoskeletons (16%) were found in the other cases. In the workplace studies, participants usually performed their work during the entire workday, therefore the majority of them (75%) reported free movements, 20% used tools, while only 3% employed exoskeletons. The task support is reported in Figure 11. In the laboratory setting, there is a higher employment of tools and exoskeletons since new technologies, as new specific tools or supporting devices, are tested in a controlled environment, while in workplace scenarios, movements are generally free (as described in the task type), representing the whole working activity with multiple and various tasks.
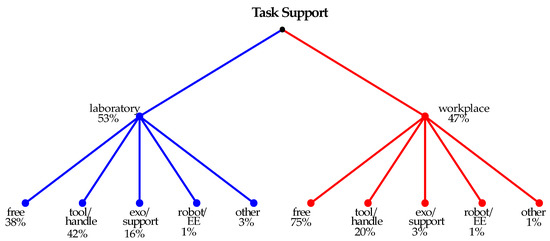
Figure 11.
Percentage of the task supports employed for the laboratory setting (on the left) and for the workplace setting (on the right).
3.6. Measurements and Data Analysis
Several approaches were employed in the screened studies as shown in Figure 12. Some instrumental approaches were based on the EMG and kinematics, but also model-based approaches often included biomechanics and kinetics, with human models or recorded forces. Other approaches were based on scales and questionnaires. Some papers merged two or more of these approaches, even though usually sensors-based measures are used together as well as scales/questionnaires methods. Interestingly, the type of assessment differs consistently between the laboratory and workplace settings. In laboratories, EMG and kinematics are the most used methods to assess the biomechanics, effort, fatigue and strain, employed in more than 50% of the studies; on the contrary, in workplace settings, questionnaires and scales are by far the most employed ones (more than 80% of the studies).
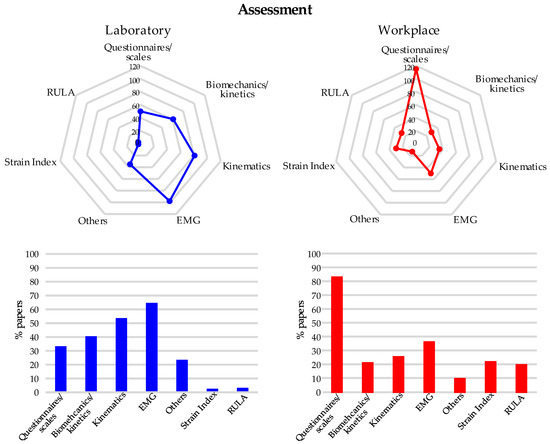
Figure 12.
Assessment methods used in the considered studies. Some studies used more than one assessment (overall percentage could exceed 100%). In the upper panel, the number of studies that employed the considered assessment methods is reported for both laboratory ((left panel), in blue) and workplace settings ((right panel), in red). In the lower panel, the percentages of papers employing the assessment methods are shown in blue for laboratory and in red for workplace scenarios.
4. Discussion
4.1. Summary of the Main Results
In this systematic review, we screened a large number of studies that performed biomechanical assessments to identify FSE in a working scenario. First, we found that a wide variety of topics were addressed by the screened studies: from the identification of physiological markers of fatigue, to the influence of task conditions on the biomechanics; from the MSD risk assessment during working activities to the design and definition of ergonomic interventions and to the testing of the effects of supporting devices, such as exoskeletons. In most of the studies, the working activities had high risk of MSD development and ergonomic interventions were needed. However, few works proposed practical solutions to solve such issues and concentrate more on assessment, while recent literature is leveraging on the validation of novel technologies. Moreover, several differences between studies taking place in laboratories and in workplaces were found. In a laboratory setting, healthy volunteers were principally included, performing movements in a controlled environment. In a workplace setting, instead, workers performing their usual working activities were analyzed, allowing for a more realistic assessment. However, this scenario limited the application of technologies that could provide the quantitative assessment of fatigue, and, therefore, scales and questionnaires were the most employed methods. In the laboratories, instead, EMG and kinematic measures were used for the assessment.
4.2. Rationale for a Top-Down Large Scope Screening on Fatigue, Strain and Effort
In this systematic review, we analyzed papers in which biomechanical assessments were used or analyzed for evaluating or assessing motor performance, fatigue, effort and strain in applications aimed at industrial scenarios, separating laboratory studies from those performed in the workplace. The integration of biomechanical assessments and physiological signals can be useful for the evaluation of fatigue, effort and strain in industrial scenarios, allowing for the investigation of the motor system, ergonomics and of mental health in their complexity, configuring a multi-disciplinary field of research at the intersection between several fields such as industry, biomechanics, ergonomic assessment, and medicine [320]. In our sample of articles, a wide variety of scenarios and assessments were found. The range of applications was very wide and non-homogeneous; while on one hand this variability complicated our analysis, on the other hand it allowed to perform a wide summary that allows for the generalization of trends in the field, and provide a comprehensive top-down view of the assessments available. Our large screening provides a comprehensive view of the actual context in which biomechanical assessments are performed in working applications and which are the following advancements that are needed for monitoring workers’ states during working activities. We summarized the results achieved so far, with an attempt to coordinate the available achievements and findings into homogeneous groups.
4.3. A Transition to a Human-Centered Perspective
From the distribution of selected papers over the years, 288 related studies emerged in our screening and they are in a growing trend, suggesting that the topic will expand further in the next years. Indeed, most studies were published in the last decade with a remarkable increase in number in the last 10 years. Increasing the mental health and the wellbeing of workers is becoming more and more of an emerging topic to improve the industrial field in a human-centered perspective [11]. The recent human-centered developments in the industrial field lead to a high level of automatization in order to increase the productivity and efficiency. In this way, human operators may face an increased complexity in their daily tasks with a higher physical and mental demand [321]. Therefore, the physical safety of workers is of primary importance [322] and the wellbeing of the industrial workers and the prevention of diseases with biomechanical assessments are a fundamental step to improve working conditions and reduce work-related musculoskeletal disorders [5]. This recent crucial step leads towards the investment of resources and research results mutating techniques, sensors and findings from the bioengineering field, in order to apply them to the industry to enhance the industrial environments in several ways.
These aspects can explain why the use of biomechanical analyses, or biomechanical-related measurements are rapidly becoming an emerging topic even outside of the medical field. This finding may also indicate that the human factor requires strong theoretical and technological improvements for adapting methods and technologies from bioengineering and mechanical engineering for use in the industrial field, thus fostering laboratory investigations. This human-centered revolution includes the introduction of assistive devices and exoskeletons that are topical for many applications in the field [17]; at the moment, it is limited mainly to devices but is growing also in the direction of employment of techniques for motor control [323,324], bio-signal analysis with advanced techniques from bioengineering [325], bio-inspired control [326], fatigue detection and others.
4.4. Main Findings on FSE of the Upper Limb
Given the high variability in the aims, the studies were divided based on the main topic of their findings. One category included all the papers that investigated the physiological effects of FSE during the simulated and constrained movements. They found that the presence of FSE can be detected by changes in the kinematics [32], dynamics [30] and also in the EMG signal [33]. Papers that analyzed the influence of the movement conditions, such as the presence of external loads [101], velocity and direction of movement [82], on biomechanics providing ergonomic recommendations for preventing fatigue, strain and effort were grouped in another category. As in the previous category, these articles directly measured and detected FSE and provided recommendations that could be used for improving the workstation design. The largest category consisted of papers that assessed the risk of MSD development, identifying most of the working activities as having a high risk, since the FSE exceeded the recommended threshold limits. These assessments were performed mainly with scales and questionnaires [193,202], but in some cases also kinematics and EMG signals were used [135,167]. Very few studies did not find FSE in the working tasks [117,136]. Another group of studies identified ergonomic interventions, such as new ergonomic workstations [243], tools [229] or training programs [239] that could be implemented in order to improve the working postures and reduce FSE. Other studies proposed exoskeletons or supporting devices in order to reduce the FSE, especially in prolonged posture maintenance and overhead working tasks [259,263] that require high loads on the neck, back and shoulder [261]. Another category included papers that design and validate alternative methods for assessing FSE during working activities, such as marker-less systems [286,306] or EMG measures [293]. Finally, few papers described new protocols for assessing FSE or for implementing intervention programs.
From this analysis, two research lines emerged: one consisted of the investigation of FSE from a physiological point of view and in their identification during working activities; the other one proposed and tested technologies and instruments aimed at reducing and preventing FSE. It is important to foster the research on mechanisms and factors influencing the development of FSE. However, since the majority of the working activity resulted in tasks with the presence of fatigue and at high risk of MSD development, the development of new ergonomic solutions to be actuated in order to reduce and prevent FSE should become of primary interest. Moreover, in the human-centered perspective of Industry 5.0, the safety and physical state of the worker has become a primary driver for future developments in the field [5]. In this scenario, new methods and technologies need to be implemented with practical applications [8]. Moreover, raising awareness and promoting education among workers on the risks of MSDs is an important element for improving their physical health [327]. Studies demonstrated that educational training reduced the biomechanical exposure and the musculoskeletal symptoms in the neck and upper limbs [328,329]. Finally, early ergonomic interventions may prevent the development of MSDs and pain in workers [330].
4.5. Laboratory vs. Working Setting
We found that studies in laboratories and workplaces are about of the same number, with an unexpected recent trend promoting laboratory investigations. This result could indicate a higher interest in the research activity or in testing new devices and methods instead of assessments in the workplaces, and a consequent push toward novel technological innovation. Another factor that may explain the increase in laboratory studies in recent years is related to the restrictions due to COVID-19 pandemics, that limited the working activities and also on-site assessments. Moreover, we found that many studies taking place in laboratories were observational or pilot studies—mainly focused on preliminary works in which novel experimental setups or concept designs were tested on a limited number of participants. Only some papers presented structured, comprehensive investigations that evaluated the fatigue, effort and strain in detail in large cohorts of people with the aim of extracting results that could be generalized to a large sample of people. On the contrary, in workplace settings many more studies assessed large cohorts of participants, but they employed fairly rapid and subject-dependent assessments (such as questionnaires or scales). One study could screen the impressive number of 3141 participants [181]. In particular, the studies taking place in the laboratory included principally only healthy participants performing constrained movements in order to examine the physiological effects of fatigue or to test new devices. This partially limits the range of application of the results, since the assessments are not fully adherent to real workers’ activities; on the contrary, they show a major technological push to introduce new techniques and technologies to comply to the requirements of the field. In workplace settings, only workers were recruited and they performed their usual working activity. However, the real working scenario reduced the availability of a detailed biomechanical assessment since some technologies cannot be easily used in uncontrolled environments. In fact, ~80% of the studies in the workplace setting employed scales and questionnaires for the assessment. However, these kinds of assessment are not completely objective since they may depend on the subjective sensations of the worker and also on the rater that administers the scale. Detailed instrumental analyses were instead performed mainly in the studies with participants. The high number of the pilot and observational studies indicated that the use of complex approaches and techniques was found mainly in the studies that aimed at exploring novel research purposes rather than deepening topics in detail with generalization objectives. This is understandable considering the feasibility of some approaches that require complex setups for data gathering, which are not always compatible with working activities, high costs, invasive setups or time-consuming procedures. Consequently, it arose from the literature that there is a relevant trade-off between the papers that deal with a large number of workers, and especially working scenarios, and the assessments that were performed. It followed that more time-consuming techniques were mostly employed in preliminary studies for evaluating how some protocols or assessments are accepted by workers or are useful to determine their level of FSE.
4.6. Translating Biomechanical Assessments from Laboratory to the Workplace
From the screening of the papers, the studies taking place in laboratories were principally observational or were pilot studies in which new tools and supporting devices were tested or some biomarkers for FSE were identified [29,32,33]. Future directions should foresee more structured and comprehensive studies involving large cohorts of participants, developed starting from pilot studies already available so that more reliable conclusions can be drawn. The laboratory studies enrolling healthy participants should be used as a benchmark for assessing the physical state of the worker and for identifying the pathological changes occurring in disorders that may occur for workers [93]. Moreover, we foresee for future developments that the environment will be less and less controlled, focusing in more detail on the real interaction of workers with their workplaces. This should be mixed with detailed biomechanical assessments also including kinematic, EMG, kinetic and dynamic measurements that can better complement and specify with more detail—and continuously monitor—the findings of the scales/questionnaire’s assessments. Indeed, the laboratory research should be translated into the real working scenario, using objective measures for the assessments, instead of scales only [307].
Another relevant issue not always reported in the studies is how the findings and the assessments can relevantly enter into the working practice. In laboratory settings, the proposed tools and experimentations show some biomarkers for fatigue and strain; there should be suggested methods and devices for reducing the workload in simulated working tasks or in quasi-static postures [272]. However, the application to the real working scenario may show different results and, therefore, it is necessary to apply the new technologies in the workplace to assess the real efficacy [331]. In the workplace setting, instead, lots of studies showed that many activities performed during work required high strain and effort and workers might develop musculoskeletal disorders related to their job. However, very few works suggest how these situations can be changed and how the effects of ergonomic interventions are generally verified with scales. Future directions should design solutions for improving the worker’s wellbeing and validate their efficacy not only in a controlled laboratory environment but also in the real workplace.
5. Conclusions
In this systematic review, we provided a wide screening of studies that performed biomechanical assessments in order to identify fatigue, strain and effort during work. First of all, we found that a wide variety of topics are addressed when performing biomechanical assessments in industrial scenarios. The studies suggested that most of the working activities are at high risk of MSD development and that ergonomic interventions are needed. However, few works proposed changes that can be done with ergonomic workstations and the use of supporting devices. Moreover, we found that in laboratory settings, the studies included principally healthy volunteers that performed movements in a controlled environment that replicated the workplace. In workplace settings, instead, workers were recruited and assessed during their usual working activity. This allows for a real assessment but limits the application of technologies that provide a quantitative assessment of fatigue. Therefore, in a human-centered perspective, the translation of new technological assessments into the real practice is needed to improve the comprehension and devise new ways to protect the physical and mental health of the worker.
Author Contributions
Conceptualization, A.S.; methodology, A.S. and C.B.; formal analysis, A.S. and C.B.; investigation, A.S., C.B., M.L.N. and F.S.; resources, A.S.; writing—original draft preparation, A.S. and C.B.; writing—review and editing, A.S., C.B., M.L.N., F.S., G.R. and M.M.; visualization, A.S. and C.B.; supervision, A.S.; funding acquisition, A.S., G.R. and M.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement No. 847926. The APC received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement No. 847926.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Xu, X.; Lu, Y.; Vogel-Heuser, B.; Wang, L. Industry 4.0 and Industry 5.0—Inception, conception and perception. J. Manuf. Syst. 2021, 61, 530–535. [Google Scholar] [CrossRef]
- Brocal, F.; González, C.; Komljenovic, D.; Katina, P.F.; Sebastián, M.A.; Garciá-Alcaraz, J.L. Emerging risk management in industry 4.0: An approach to improve organizational and human performance in the complex systems. Complexity 2019, 2019, 2089763. [Google Scholar] [CrossRef]
- van den Heuvel, S.G.; Bakhuys Roozebom, M.C.; Eekhout, I.; Venema, A. Management of Psychosocial Risks in European Workplaces—Evidence from the Second European Survey of Enterprises on New and Emerging Risks (ESENER-2); Publications Office of the European Union: Luxembourg, 2018; Available online: https://osha.europa.eu/en/publications/management-psychosocial-risks-european-workplaces-evidence-second-european-survey (accessed on 1 March 2023).
- Nahavandi, S. Industry 5.0—A human-centric solution. Sustainability 2019, 11, 4371. [Google Scholar] [CrossRef]
- Sorensen, G.; Peters, S.; Nielsen, K.; Nagler, E.; Karapanos, M.; Wallace, L.; Burke, L.; Dennerlein, J.; Wagner, G. Improving working conditions to promote worker safety, health, and wellbeing for low-wage workers: The workplace organizational health study. Int. J. Environ. Res. Public Health 2019, 16, 1449. [Google Scholar] [CrossRef]
- Scano, A.; Mira, R.M.; Cerveri, P.; Tosatti, L.M.; Sacco, M. Analysis of upper-limb and trunk kinematic variability: Accuracy and reliability of an RGB-D sensor. Multimodal Technol. Interact. 2020, 4, 14. [Google Scholar] [CrossRef]
- de Looze, M.P.; Bosch, T.; Krause, F.; Stadler, K.S.; O’Sullivan, L.W. Exoskeletons for industrial application and their potential effects on physical work load. Ergonomics 2016, 59, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Kadir, B.A.; Broberg, O.; da Conceição, C.S. Current research and future perspectives on human factors and ergonomics in Industry 4.0. Comput. Ind. Eng. 2019, 137, 106004. [Google Scholar] [CrossRef]
- Brunner, B.; Igic, I.; Keller, A.C.; Wieser, S. Who gains the most from improving working conditions? Health-related absenteeism and presenteeism due to stress at work. Eur. J. Health Econ. 2019, 20, 1165–1180. [Google Scholar] [CrossRef]
- Ranavolo, A.; Chini, G.; Draicchio, F.; Silvetti, A.; Varrecchia, T.; Fiori, L.; Tatarelli, A.; Rosen, P.H.; Wischniewski, S.; Albrecht, P.; et al. Human-Robot Collaboration (HRC) Technologies for Reducing Work-Related Musculoskeletal Diseases in Industry 4.0. In Lecture Notes in Networks and Systems; Springer Science and Business Media Deutschland GmbH: Berlin, Germany, 2022; Volume 223, pp. 335–342. [Google Scholar]
- Lavit Nicora, M.; Andre, E.; Berkmans, D.; Carissoli, C.; D’Orazio, T.; Fave, A.D.; Gebhard, P.; Marani, R.; Mira, R.M.; Negri, L.; et al. A human-driven control architecture for promoting good mental health in collaborative robot scenarios. In Proceedings of the 2021 30th IEEE International Conference on Robot and Human Interactive Communication, RO-MAN 2021, Vancouver, BC, Canada, 8–12 August 2021; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2021; pp. 285–291. [Google Scholar]
- Argyle, E.M.; Marinescu, A.; Wilson, M.L.; Lawson, G.; Sharples, S. Physiological indicators of task demand, fatigue, and cognition in future digital manufacturing environments. Int. J. Hum. Comput. Stud. 2021, 145, 102522. [Google Scholar] [CrossRef]
- Gualtieri, L.; Palomba, I.; Merati, F.A.; Rauch, E.; Vidoni, R. Design of human-centered collaborative assembly workstations for the improvement of operators’ physical ergonomics and production efficiency: A case study. Sustainability 2020, 12, 3606. [Google Scholar] [CrossRef]
- Abd-Elfattah, H.M.; Abdelazeim, F.H.; Elshennawy, S. Physical and cognitive consequences of fatigue: A review. J. Adv. Res. 2015, 6, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Argubi-Wollesen, A.; Wollesen, B.; Leitner, M.; Mattes, K. Human Body Mechanics of Pushing and Pulling: Analyzing the Factors of Task-related Strain on the Musculoskeletal System. Saf. Health Work 2017, 8, 11–18. [Google Scholar] [CrossRef]
- Morel, P.; Ulbrich, P.; Gail, A. What makes a reach movement effortful? Physical effort discounting supports common minimization principles in decision making and motor control. PLoS Biol. 2017, 15, e2001323. [Google Scholar] [CrossRef] [PubMed]
- Crea, S.; Beckerle, P.; De Looze, M.; De Pauw, K.; Grazi, L.; Kermavnar, T.; Masood, J.; O’Sullivan, L.W.; Pacifico, I.; Rodriguez-Guerrero, C.; et al. Occupational exoskeletons: A roadmap toward large-scale adoption. Methodology and challenges of bringing exoskeletons to workplaces. Wearable Technol. 2021, 2, e11. [Google Scholar] [CrossRef]
- Moshawrab, M.; Adda, M.; Bouzouane, A.; Ibrahim, H.; Raad, A. Smart Wearables for the Detection of Occupational Physical Fatigue: A Literature Review. Sensors 2022, 22, 7472. [Google Scholar] [CrossRef]
- Anwer, S.; Li, H.; Antwi-Afari, M.F.; Umer, W.; Wong, A.Y.L. Evaluation of Physiological Metrics as Real-Time Measurement of Physical Fatigue in Construction Workers: State-of-the-Art Review. J. Constr. Eng. Manag. 2021, 147, 03121001. [Google Scholar] [CrossRef]
- Santos, J.; Baptista, J.S.; Monteiro, P.R.R.; Miguel, A.S.; Santos, R.; Vaz, M.A.P. The influence of task design on upper limb muscles fatigue during low-load repetitive work: A systematic review. Int. J. Ind. Ergon. 2014, 52, 78–91. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Occhipinti, E. OCRA: A concise index for the assessment of exposure to repetitive movements of the upper limbs. Ergonomics 1998, 41, 1290–1311. [Google Scholar] [CrossRef]
- Crawford, J.O. The Nordic Musculoskeletal Questionnaire. Occup. Med. 2007, 57, 300–301. [Google Scholar] [CrossRef]
- Hignett, S.; McAtamney, L. Rapid Entire Body Assessment (REBA). Appl. Ergon. 2000, 31, 201–205. [Google Scholar] [CrossRef]
- McAtamney, L.; Nigel Corlett, E. RULA: A survey method for the investigation of work-related upper limb disorders. Appl. Ergon. 1993, 24, 91–99. [Google Scholar] [CrossRef]
- Stephens, J.P.; Vos, G.A.; Stevens, E.M.; Steven Moore, J. Test-retest repeatability of the Strain Index. Appl. Ergon. 2006, 37, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.S.; Garg, A. The strain index: A proposed method to analyze jobs for risk of distal upper extremity disorders. Am. Ind. Hyg. Assoc. J. 1995, 56, 443–458. [Google Scholar] [CrossRef]
- Lamooki, S.R.; Cavuoto, L.A.; Kang, J. Adjustments in Shoulder and Back Kinematics during Repetitive Palletizing Tasks. Sensors 2022, 22, 5655. [Google Scholar] [CrossRef] [PubMed]
- Qin, J.; Lin, J.H.; Faber, G.S.; Buchholz, B.; Xu, X. Upper extremity kinematic and kinetic adaptations during a fatiguing repetitive task. J. Electromyogr. Kinesiol. 2014, 24, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Anwer, S.; Li, H.; Antwi-Afari, M.F.; Umer, W.; Wong, A.Y.L. Cardiorespiratory and thermoregulatory parameters are good surrogates for measuring physical fatigue during a simulated construction task. Int. J. Environ. Res. Public Health 2020, 17, 5418. [Google Scholar] [CrossRef]
- Boubaker, K.; Colantoni, A.; Allegrini, E.; Longo, L.; Di Giacinto, S.; Monarca, D.; Cecchini, M. A model for musculoskeletal disorder-related fatigue in upper limb manipulation during industrial vegetables sorting. Int. J. Ind. Ergon. 2014, 44, 601–605. [Google Scholar] [CrossRef]
- Brandt, M.; Andersen, L.L.; Samani, A.; Jakobsen, M.D.; Madeleine, P. Inter-day reliability of surface electromyography recordings of the lumbar part of erector spinae longissimus and trapezius descendens during box lifting. BMC Musculoskelet. Disord. 2017, 18, 519. [Google Scholar] [CrossRef]
- Cè, E.; Doria, C.; Roveda, E.; Montaruli, A.; Galasso, L.; Castelli, L.; Mulè, A.; Longo, S.; Coratella, G.; D’Aloia, P.; et al. Reduced Neuromuscular Performance in Night Shift Orthopedic Nurses: New Insights From a Combined Electromyographic and Force Signals Approach. Front. Physiol. 2020, 11, 693. [Google Scholar] [CrossRef]
- Cudlip, A.C.; Holmes, M.W.R.; Callaghan, J.P.; Dickerson, C.R. The effects of shoulder abduction angle and wrist angle on upper extremity muscle activity in unilateral right handed push/pull tasks. Int. J. Ind. Ergon. 2018, 64, 102–107. [Google Scholar] [CrossRef]
- Dennerlein, J.T.; Ciriello, V.M.; Kerin, K.J.; Johnson, P.W. Fatigue in the Forearm Resulting From Low-Level Repetitive Ulnar Deviation. AIHA J. 2003, 64, 799. [Google Scholar] [CrossRef]
- Earle-Richardson, G.; Jenkins, P.L.; Strogatz, D.; Bell, E.M.; May, J.J. Development and initial assessment of objective fatigue measures for apple harvest work. Appl. Ergon. 2006, 37, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Fang, N.; Zhang, C.; Lv, J. Effects of vertical lifting distance on upper-body muscle fatigue. Int. J. Environ. Res. Public Health 2021, 18, 5468. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, S.A.; Allread, W.G.; Le, P.; Rose, J.; Marras, W.S. Shoulder muscle fatigue during repetitive tasks as measured by electromyography and near-infrared spectroscopy. Hum. Factors 2013, 55, 1077–1087. [Google Scholar] [CrossRef] [PubMed]
- Fifolato, T.M.; Nardim, H.C.B.; do Carmo Lopes, E.R.; Suzuki, K.A.K.; da Silva, N.C.; de Souza Serenza, F.; Fonseca, M.C.R. Association between muscle strength, upper extremity fatigue resistance, work ability and upper extremity dysfunction in a sample of workers at a tertiary hospital. BMC Musculoskelet. Disord. 2021, 22, 508. [Google Scholar] [CrossRef]
- Côté, J.N.; Feldman, A.G.; Mathieu, P.A.; Levin, M.F. Effects of fatigue on intermuscular coordination during repetitive hammering. Motor Control 2008, 12, 79–92. [Google Scholar] [CrossRef]
- Hostler, D.; Schwob, J.; Schlader, Z.J.; Cavuoto, L. Heat Stress Increases Movement Jerk During Physical Exertion. Front. Physiol. 2021, 12, 1750. [Google Scholar] [CrossRef]
- Hsieh, Y.J.; Cho, C.Y. Using risk factors, myoelectric signal, and finger tremor to distinguish computer users with and without musculoskeletal symptoms. Eur. J. Appl. Physiol. 2008, 104, 9–17. [Google Scholar] [CrossRef]
- Huang, C.K.; Siu, K.C.; Lien, H.Y.; Lee, Y.J.; Lin, Y.H. Scapular kinematics and muscle activities during pushing tasks. J. Occup. Health 2013, 55, 259–266. [Google Scholar] [CrossRef]
- Iridiastadi, H.; Nussbaum, M.A. Muscle fatigue and endurance during repetitive intermittent static efforts: Development of prediction models. Ergonomics 2006, 49, 344–360. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Park, J.S.; Kim, D.J.; Im, S. Evaluation of fatigue patterns in individual shoulder muscles under various external conditions. Appl. Ergon. 2021, 91, 103280. [Google Scholar] [CrossRef] [PubMed]
- Li, K.W.; Li, W.; Yi, C. Muscular fatigue measurements for push-down tasks in ground demolitions. Hum. Factors Ergon. Manuf. Serv. Ind. 2021, 31, 76–85. [Google Scholar] [CrossRef]
- Luger, T.; Seibt, R.; Rieger, M.A.; Steinhilber, B. The role of motor learning on measures of physical requirements and motor variability during repetitive screwing. Int. J. Environ. Res. Public Health 2019, 16, 1231. [Google Scholar] [CrossRef]
- Madeleine, P. On functional motor adaptations: From the quantification of motor strategies to the prevention of musculoskeletal disorders in the neck-shoulder region. Acta Physiol. 2010, 199, 1–46. [Google Scholar] [CrossRef]
- Maikala, R.V.; Bhambhani, Y.N. Comparisons of physiological and perceptual responses in healthy men and women during standardized arm cranking and task-specific pushing-pulling. Int. Arch. Occup. Environ. Health 2006, 79, 509–520. [Google Scholar] [CrossRef]
- Maiti, R.; Bagchi, T.P. Effect of different multipliers and their interactions during manual lifting operations. Int. J. Ind. Ergon. 2006, 36, 991–1004. [Google Scholar] [CrossRef]
- Moyen-Sylvestre, B.; Goubault, É.; Begon, M.; Côté, J.N.; Bouffard, J.; Dal Maso, F. Power Spectrum of Acceleration and Angular Velocity Signals as Indicators of Muscle Fatigue during Upper Limb Low-Load Repetitive Tasks. Sensors 2022, 22, 8008. [Google Scholar] [CrossRef]
- McDonald, A.C.; Mulla, D.M.; Keir, P.J. Muscular and kinematic adaptations to fatiguing repetitive upper extremity work. Appl. Ergon. 2019, 75, 250–256. [Google Scholar] [CrossRef] [PubMed]
- McDonald, A.C.; Mulla, D.M.; Keir, P.J. Using EMG Amplitude and Frequency to Calculate a Multimuscle Fatigue Score and Evaluate Global Shoulder Fatigue. Hum. Factors 2019, 61, 526–536. [Google Scholar] [CrossRef] [PubMed]
- McDonald, A.C.; Tse, C.T.F.; Keir, P.J. Adaptations to isolated shoulder fatigue during simulated repetitive work. Part II: Recovery. J. Electromyogr. Kinesiol. 2016, 29, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.K.; Agnew, M.J. Analysis of individual and occupational risk factors on task performance and biomechanical demands for a simulated drilling task. Int. J. Ind. Ergon. 2010, 40, 584–591. [Google Scholar] [CrossRef]
- Merino, G.; da Silva, L.; Mattos, D.; Guimarães, B.; Merino, E. Ergonomic evaluation of the musculoskeletal risks in a banana harvesting activity through qualitative and quantitative measures, with emphasis on motion capture (Xsens) and EMG. Int. J. Ind. Ergon. 2019, 69, 80–89. [Google Scholar] [CrossRef]
- Ohashi, J.Y.; Blangsted, A.K.; Nielsen, P.K.; Jørgensen, K. The assessment of muscle strain with surface electromyograms during simulated mushroom picking. J. Hum. Ergol. 2008, 37, 13–22. [Google Scholar] [CrossRef]
- Renberg, J.; Nordrum Wiggen, Ø.; Stranna Tvetene, P.Ø.; Færevik, H.; Van Beekvelt, M.; Roeleveld, K. Effect of working position and cold environment on muscle activation level and fatigue in the upper limb during manual work tasks. Int. J. Ind. Ergon. 2020, 80, 103035. [Google Scholar] [CrossRef]
- Roquelaure, Y.; Dano, C.; Dusolier, G.; Fanello, S.; Penneau-Fontbonne, D. Biomechanical strains on the hand-wrist system during grapevine pruning. Int. Arch. Occup. Environ. Health 2002, 75, 591–595. [Google Scholar] [CrossRef]
- Salmanzadeh, H.; Doroodi, M. Analyzing surface electromyography signals to predict fatigue in Longissimus thoracis and Iliocostalis Cervicis muscles: A statistical model. Hum. Factors Ergon. Manuf. 2022, 32, 335–344. [Google Scholar] [CrossRef]
- Silva, L.; Dias, M.; Folgado, D.; Nunes, M.; Namburi, P.; Anthony, B.; Carvalho, D.; Carvalho, M.; Edelman, E.; Gamboa, H. Respiratory Inductance Plethysmography to Assess Fatigability during Repetitive Work. Sensors 2022, 22, 4247. [Google Scholar] [CrossRef]
- Goubault, E.; Martinez, R.; Bouffard, J.; Dowling-Medley, J.; Begon, M.; Dal Maso, F. Shoulder electromyography-based indicators to assess manifestation of muscle fatigue during laboratory-simulated manual handling task. Ergonomics 2022, 65, 118–133. [Google Scholar] [CrossRef]
- Sormunen, E.; Oksa, J.; Pienimäki, T.; Rissanen, S.; Rintamäki, H. Muscular and cold strain of female workers in meatpacking work. Int. J. Ind. Ergon. 2006, 36, 713–720. [Google Scholar] [CrossRef]
- Sormunen, E.; Rissanen, S.; Oksa, J.; Pienimaki, T.; Remes, J.; Rintamaki, H. Muscular activity and thermal responses in men and women during repetitive work in cold environments. Ergonomics 2009, 52, 964–976. [Google Scholar] [CrossRef] [PubMed]
- Spyropoulos, E.; Chroni, E.; Katsakiori, P.; Athanassiou, G. A quantitative approach to assess upper limb fatigue in the work field. Occup. Ergon. 2013, 11, 45–57. [Google Scholar] [CrossRef]
- Strøm, V.; Knardahl, S.; Stanghelle, J.K.; Røe, C. Pain induced by a single simulated office-work session: Time course and association with muscle blood flux and muscle activity. Eur. J. Pain 2009, 13, 843–852. [Google Scholar] [CrossRef] [PubMed]
- Tse, C.T.F.; McDonald, A.C.; Keir, P.J. Adaptations to isolated shoulder fatigue during simulated repetitive work. Part I: Fatigue. J. Electromyogr. Kinesiol. 2016, 29, 34–41. [Google Scholar] [CrossRef]
- Widia, M.; Dawal, S.Z.M. The effect of hand-held vibrating tools on muscle activity and grip strength. Aust. J. Basic Appl. Sci. 2011, 5, 198–211. [Google Scholar]
- Yung, M.; Bigelow, P.L.; Hastings, D.M.; Wells, R.P. Detecting within- and between-day manifestations of neuromuscular fatigue at work: An exploratory study. Ergonomics 2014, 57, 1562–1573. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, K.W.; Zhang, W.; Ma, L.; Chen, Z. Muscular fatigue and maximum endurance time assessment for male and female industrial workers. Int. J. Ind. Ergon. 2014, 44, 292–297. [Google Scholar] [CrossRef]
- Chihara, T.; Nozawa, A.; Seo, A. Formulation of perceived muscle fatigue based on elbow flexion task. Mech. Eng. J. 2016, 3, 15-00740. [Google Scholar] [CrossRef]
- Zadry, H.R.; Dawal, S.Z.M.; Taha, Z. Development of statistical models for predicting muscle and mental activities during repetitive precision tasks. Int. J. Occup. Saf. Ergon. 2016, 22, 374–383. [Google Scholar] [CrossRef]
- Zadry, H.R.; Md Dawal, S.Z.; Taha, Z. Combination of electromyography and electroencephalography measurements in designing repetitive task in industry. Adv. Sci. Lett. 2011, 4, 2498–2502. [Google Scholar] [CrossRef]
- Collier, B.R.; Holland, L.; McGhee, D.; Sampson, J.A.; Bell, A.; Stapley, P.J.; Groeller, H. Precision markedly attenuates repetitive lift capacity. Ergonomics 2014, 57, 1427–1439. [Google Scholar] [CrossRef]
- Alhaag, M.H.; Ramadan, M.Z.; Al-harkan, I.M.; Alessa, F.M.; Alkhalefah, H.; Abidi, M.H.; Sayed, A.E. Determining the fatigue associated with different task complexity during maintenance operations in males using electromyography features. Int. J. Ind. Ergon. 2022, 88, 103273. [Google Scholar] [CrossRef]
- Yu, N.; Hong, L.; Guo, J. Analysis of upper-limb muscle fatigue in the process of rotary handling. Int. J. Ind. Ergon. 2021, 83, 103109. [Google Scholar] [CrossRef]
- Werner, R.A.; Franzblau, A.; Gell, N.; Ulin, S.S.; Armstrong, T.J. Predictors of upper extremity discomfort: A longitudinal study of industrial and clerical workers. J. Occup. Rehabil. 2005, 15, 27–35. [Google Scholar] [CrossRef]
- Maiti, R.; Ray, G.G. Manual lifting load limit equation for adult Indian women workers based on physiological criteria. Ergonomics 2004, 47, 59–74. [Google Scholar] [CrossRef] [PubMed]
- Maciukiewicz, J.M.; Cudlip, A.C.; Chopp-Hurley, J.N.; Dickerson, C.R. Effects of overhead work configuration on muscle activity during a simulated drilling task. Appl. Ergon. 2016, 53, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.H.; McGorry, R.W.; Banks, J.J. Exposures and physiological responses in power tool operations: Fastening vs. Unfastening threaded hardware. J. Occup. Environ. Hyg. 2010, 7, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.H.; Maikala, R.V.; McGorry, R.; Brunette, C. NIRS application in evaluating threaded-fastener driving assembly tasks. Int. J. Ind. Ergon. 2010, 40, 146–152. [Google Scholar] [CrossRef]
- Li, K.W.; Yu, R.F.; Han, X.L. Physiological and psychophysical responses in handling maximum acceptable weights under different footwear-floor friction conditions. Appl. Ergon. 2007, 38, 259–265. [Google Scholar] [CrossRef]
- Lee, T.H. Static lifting strengths at different exertion heights. Int. J. Ind. Ergon. 2004, 34, 263–269. [Google Scholar] [CrossRef]
- Lee, C.L.; Lu, S.Y.; Wu, C.Y. Rest period and object load effects on upper limb muscle strength recovery for manual load transfer. Int. J. Ind. Ergon. 2022, 89, 103274. [Google Scholar] [CrossRef]
- Lee, C.L.; Lu, S.Y.; Sung, P.C.; Liao, H.Y. Working height and parts bin position effects on upper limb muscular strain for repetitive hand transfer. Int. J. Ind. Ergon. 2015, 50, 178–185. [Google Scholar] [CrossRef]
- Kothiyal, K.; Kayis, B. Workplace layout for seated manual handling tasks: An electromyography study. Int. J. Ind. Ergon. 2001, 27, 19–32. [Google Scholar] [CrossRef]
- Jakob, M.; Liebers, F.; Behrendt, S. The effects of working height and manipulated weights on subjective strain, body posture and muscular activity of milking parlor operatives—Laboratory study. Appl. Ergon. 2012, 43, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Strasser, H.; Mueller, K.-W. Electromyographically Determined Muscle Strain Associated with the Direction of Manual Movements in the Horizontal Reach. In Assessement of the Ergonomic Quality of Hand-Held Tools and Computer Input Devices; IOS Press: Amsterdam, The Netherlands, 2007; Volume 1, pp. 57–65. ISBN 978-1-58603-788-8. [Google Scholar]
- Hattori, Y.; Ono, Y.; Shimaoka, M.; Hiruta, S.; Shibata, E.; Ando, S.; Hori, F.; Takeuchi, Y. Effects of box weight, vertical location and symmetry on lifting capacities and ratings on category scale in Japanese female workers. Ergonomics 2000, 43, 2031–2042. [Google Scholar] [CrossRef] [PubMed]
- Han, W.; Gao, L.; Wu, J.; Pelowski, M.; Liu, T. Assessing the brain ‘on the line’: An ecologically-valid assessment of the impact of repetitive assembly line work on hemodynamic response and fine motor control using fNIRS. Brain Cogn. 2019, 136, 103613. [Google Scholar] [CrossRef] [PubMed]
- Gooyers, C.E.; Stevenson, J.M. The impact of an increase in work rate on task demands for a simulated industrial hand tool assembly task. Int. J. Ind. Ergon. 2012, 42, 80–89. [Google Scholar] [CrossRef]
- Girish, N.; Iqbal, R.; Khanzode, V. Liftig capacity among indian manual materials handlers using progressive isoinertial lifting evaluation. J. Musculoskelet. Res. 2017, 20, 1750004. [Google Scholar] [CrossRef]
- Garg, A.; Hegmann, K.; Kapellusch, J. Short-cycle overhead work and shoulder girdle muscle fatigue. Int. J. Ind. Ergon. 2006, 36, 581–597. [Google Scholar] [CrossRef]
- Gagnon, M.; Larrivé, A.; Desjardins, P. Strategies of load tilts and shoulders positioning in asymmetrical lifting. A concomitant evaluation of the reference systems of axes. Clin. Biomech. 2000, 15, 478–488. [Google Scholar] [CrossRef]
- Eddy, M.; Moore, C.; Nimbarte, A. Evaluation of shoulder strain during multidirectional forceful arm exertions. Occup. Ergon. 2016, 13, 131–138. [Google Scholar] [CrossRef]
- Cort, J.A.; Stephens, A.; Potvin, J.R. A biomechanical and psychophysical examination of fastener initiations in automotive assembly. Int. J. Ind. Ergon. 2006, 36, 837–845. [Google Scholar] [CrossRef]
- Christensen, H.; Søgaard, K.; Pilegaard, M.; Olsen Engineer, H.B. The importance of the work/rest pattern as a risk factor in repetitive monotonous work. Int. J. Ind. Ergon. 2000, 25, 367–373. [Google Scholar] [CrossRef]
- Choi, H.S.; In, H. The effects of operating height and the passage of time on the end-point performance of fine manipulative tasks that require high accuracy. Front. Physiol. 2022, 13, 1628. [Google Scholar] [CrossRef] [PubMed]
- Southard, S.A.; Mirka, G.A. An evaluation of backpack harness systems in non-neutral torso postures. Appl. Ergon. 2007, 38, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Cavuoto, L.A.; Nussbaum, M.A. The influences of obesity and age on functional performance during intermittent upper extremity tasks. J. Occup. Environ. Hyg. 2014, 11, 583–590. [Google Scholar] [CrossRef]
- Bulbrook, B.D.; La Delfa, N.J.; McDonald, A.C.; Liang, C.; Callaghan, J.P.; Dickerson, C.R. Higher body mass index and body fat percentage correlate to lower joint and functional strength in working age adults. Appl. Ergon. 2021, 95, 103453. [Google Scholar] [CrossRef]
- Brambilla, C.; Malosio, M.; Reni, G.; Scano, A. Optimal Biomechanical Performance in Upper-Limb Gestures Depends on Velocity and Carried Load. Biology 2022, 11, 391. [Google Scholar] [CrossRef]
- Bosch, T.; Mathiassen, S.E.; Visser, B.; de Looze, M.D.; van Dieën, J.V. The effect of work pace on workload, motor variability and fatigue during simulated light assembly work. Ergonomics 2011, 54, 154–168. [Google Scholar] [CrossRef] [PubMed]
- Babski-Reeves, K.; Calhoun, A. Muscle Activity and Posture Differences in the Sit and Stand Phases of Sit-to-Stand Workstation Use: A Comparison of Computer Configurations. IIE Trans. Occup. Ergon. Hum. Factors 2016, 4, 236–246. [Google Scholar] [CrossRef]
- Anton, D.; Shibley, L.D.; Fethke, N.B.; Hess, J.; Cook, T.M.; Rosecrance, J. The effect of overhead drilling position on shoulder moment and electromyography. Ergonomics 2001, 44, 489–501. [Google Scholar] [CrossRef]
- Al-Qaisi, S.; Aghazadeh, F. The effects of valve-handwheel height and angle on neck, shoulder, and back muscle loading. Int. J. Ind. Ergon. 2018, 64, 69–78. [Google Scholar] [CrossRef]
- Allen, J.L.; James, C.; Snodgrass, S.J. The effect of load on biomechanics during an overhead lift in the WorkHab Functional Capacity Evaluation. Work 2012, 43, 487–496. [Google Scholar] [CrossRef]
- Anwer, S.; Li, H.; Antwi-Afari, M.F.; Umer, W.; Mehmood, I.; Wong, A.Y.L. Effects of load carrying techniques on gait parameters, dynamic balance, and physiological parameters during a manual material handling task. Eng. Constr. Archit. Manag. 2022, 29, 3415–3438. [Google Scholar] [CrossRef]
- Skovlund, S.V.; Bláfoss, R.; Skals, S.; Jakobsen, M.D.; Andersen, L.L. The Importance of Lifting Height and Load Mass for Muscular Workload during Supermarket Stocking: Cross-Sectional Field Study. Int. J. Environ. Res. Public Health 2022, 19, 3030. [Google Scholar] [CrossRef] [PubMed]
- Silvetti, A.; Mari, S.; Ranavolo, A.; Forzano, F.; Iavicoli, S.; Conte, C.; Draicchio, F. Kinematic and electromyographic assessment of manual handling on a supermarket greengrocery shelf. Work 2015, 51, 261–271. [Google Scholar] [CrossRef]
- Shin, S.J.; Yoo, W.G.; Kim, T.Y. Effects of different overhead work conditions on the neck and shoulder muscles. J. Phys. Ther. Sci. 2012, 24, 197–199. [Google Scholar] [CrossRef]
- Roman-Liu, D.; Tokarski, T. Upper limb strength in relation to upper limb posture. Int. J. Ind. Ergon. 2005, 35, 19–31. [Google Scholar] [CrossRef]
- Potvin, J.R.; Christy Calder, I.; Cort, J.A.; Agnew, M.J.; Stephens, A. Maximal acceptable forces for manual insertions using a pulp pinch, oblique grasp and finger press. Int. J. Ind. Ergon. 2006, 36, 779–787. [Google Scholar] [CrossRef]
- Oyewole, S.A. Enhancing ergonomic safety effectiveness of repetitive job activities: Prediction of muscle fatigue in dominant and nondominant arms of industrial workers. Hum. Factors Ergon. Manuf. 2014, 24, 585–600. [Google Scholar] [CrossRef]
- Akanmu, A.; Olayiwola, J.; Olatunji, O.A. Musculoskeletal disorders within the carpentry trade: Analysis of timber flooring subtasks. Eng. Constr. Archit. Manag. 2020, 27, 2577–2590. [Google Scholar] [CrossRef]
- Allahyari, T.; Mortazavi, N.; Khalkhali, H.R.; Sanjari, M.A. Shoulder girdle muscle activity and fatigue in traditional and improved design carpet weaving workstations. Int. J. Occup. Med. Environ. Health 2016, 29, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Buchholz, B.; Park, J.S.; Gold, J.; Punnett, L. Subjective ratings of upper extremity exposures: Inter-method agreement with direct measurement of exposures. Ergonomics 2008, 51, 1064–1077. [Google Scholar] [CrossRef]
- Cabeças, J.M. The risk of distal upper limb disorder in cleaners: A modified application of the Strain Index method. Int. J. Ind. Ergon. 2007, 37, 563–571. [Google Scholar] [CrossRef]
- Chaiklieng, S. Health risk assessment on musculoskeletal disorders among potato-chip processing workers. PLoS ONE 2019, 14, e0224980. [Google Scholar] [CrossRef]
- Chiasson, M.È; Imbeau, D.; Aubry, K.; Delisle, A. Comparing the results of eight methods used to evaluate risk factors associated with musculoskeletal disorders. Int. J. Ind. Ergon. 2012, 42, 478–488. [Google Scholar] [CrossRef]
- Coury, H.J.C.G.; Alfredo Léo, J.; Kumar, S. Effects of progressive levels of industrial automation on force and repetitive movements of the wrist. Int. J. Ind. Ergon. 2000, 25, 587–595. [Google Scholar] [CrossRef]
- Das, B.; Ghosh, T.; Gangopadhyay, S. Child work in agriculture in West Bengal, India: Assessment of musculoskeletal disorders and occupational health problems. J. Occup. Health 2013, 55, 244–258. [Google Scholar] [CrossRef]
- De Souza, J.A.C.; Filho, M.L.M. Ergonomics posture and movement analyses of supermarket checkout operators in the city of Cataguases, MG. Gest. Prod. 2017, 24, 123–135. [Google Scholar] [CrossRef]
- Denbeigh, K.; Slot, T.R.; Dumas, G.A. Wrist postures and forces in tree planters during three tree unloading conditions. Ergonomics 2013, 56, 1599–1607. [Google Scholar] [CrossRef]
- Douphrate, D.I.; Fethke, N.B.; Nonnenmann, M.W.; Rodriguez, A.; Hagevoort, R.; Gimeno Ruiz de Porras, D. Full-shift and task-specific upper extremity muscle activity among US large-herd dairy parlour workers. Ergonomics 2017, 60, 1042–1054. [Google Scholar] [CrossRef]
- Douphrate, D.I.; Gimeno Ruiz de Porras, D.; Nonnenmann, M.W.; Hagevoort, R.; Reynolds, S.J.; Rodriguez, A.; Fethke, N.B. Effects of milking unit design on upper extremity muscle activity during attachment among U.S. large-herd parlor workers. Appl. Ergon. 2017, 58, 482–490. [Google Scholar] [CrossRef]
- Anand, M.V.; Vijayakumar, K.C.K.; Mohanraj, T. Evaluation of Shoulder Pain Among the Workers Involved in Ironing Process Using Surface Electromyography. J. Med. Imaging Health Inform. 2019, 10, 86–92. [Google Scholar] [CrossRef]
- Forcella, L.; Bonfiglioli, R.; Cutilli, P.; Antonucci, A.; Di Donato, A.; Siciliano, E.; Cortini, M.; Violante, F.S.; Boscolo, P. Occupational stress and biomechanical risk in a high fashion clothing company. Work 2012, 41, 2966–2970. [Google Scholar] [CrossRef]
- Forcella, L.; Bonfiglioli, R.; Cutilli, P.; Siciliano, E.; Di Donato, A.; Di Nicola, M.; Antonucci, A.; Di Giampaolo, L.; Boscolo, P.; Violante, F.S. Analysis of occupational stress in a high fashion clothing factory with upper limb biomechanical overload. Int. Arch. Occup. Environ. Health 2012, 85, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Gardner, B.T.; Lombardi, D.A.; Dale, A.M.; Franzblau, A.; Evanoff, B.A. Reliability of job-title based physical work exposures for the upper extremity: Comparison to self-reported and observed exposure estimates. Occup. Environ. Med. 2010, 67, 538–547. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.; Kapellusch, J.; Hegmann, K.; Wertsch, J.; Merryweather, A.; Deckow-Schaefer, G.; Malloy, E.J. The Strain Index (SI) and Threshold Limit Value (TLV) for Hand Activity Level (HAL): Risk of carpal tunnel syndrome (CTS) in a prospective cohort. Ergonomics 2012, 55, 396–414. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.; Kapellusch, J.M.; Hegmann, K.T.; Thiese, M.S.; Merryweather, A.S.; Wang, Y.C.; Malloy, E.J. The Strain Index and TLV for HAL: Risk of lateral epicondylitis in a prospective cohort. Am. J. Ind. Med. 2014, 57, 286–302. [Google Scholar] [CrossRef]
- Gerr, F.; Fethke, N.B.; Merlino, L.; Anton, D.; Rosecrance, J.; Jones, M.P.; Marcus, M.; Meyers, A.R. A prospective study of musculoskeletal outcomes among manufacturing workers: I. effects of physical risk factors. Hum. Factors 2014, 56, 112–130. [Google Scholar] [CrossRef]
- Glenday, J.D.; Steinhilber, B.; Jung, F.; Haeufle, D.F.B. Development of a musculoskeletal model of the wrist to predict frictional work dissipated due to tendon gliding resistance in the carpal tunnel. Comput. Methods Biomech. Biomed. Engin. 2021, 24, 973–984. [Google Scholar] [CrossRef]
- Granzow, R.F.; Schall, M.C.; Smidt, M.F.; Chen, H.; Fethke, N.B.; Huangfu, R. Characterizing exposure to physical risk factors among reforestation hand planters in the Southeastern United States. Appl. Ergon. 2018, 66, 1–8. [Google Scholar] [CrossRef]
- Gruevski, K.M.; Hodder, J.N.; Keir, P.J. Upper Extremity Muscle Activity during In-Phase and Anti-Phase Continuous Pushing Tasks. Hum. Factors 2017, 59, 1066–1077. [Google Scholar] [CrossRef]
- Gupta, A.D.; Mahalanabis, D. Study of hand function in a group of shoe factory workers engaged in repetitive work. J. Occup. Rehabil. 2006, 16, 675–684. [Google Scholar] [CrossRef]
- Andriani, P.; Tejamaya, M.; Widanarko, B.; Putri, A.A. Ergonomic assessment in metal-based small industries in Bogor Regency, Indonesia, 2019. Gac. Sanit. 2021, 35, S360–S363. [Google Scholar] [CrossRef]
- Harris, C.; Eisen, E.A.; Goldberg, R.; Krause, N.; Rempel, D. 1st place, PREMUS best paper competition: Workplace and individual factors in wrist tendinosis among blue-collar workers—The San Francisco study. Scand. J. Work. Environ. Health 2011, 37, 85–98. [Google Scholar] [CrossRef] [PubMed]
- Holte, K.A.; Westgaard, R.H. Daytime trapezius muscle activity and shoulder-neck pain of service workers with work stress and low biomechanical exposure. Am. J. Ind. Med. 2002, 41, 393–405. [Google Scholar] [CrossRef]
- Holte, K.A.; Westgaard, R.H. Further studies of shoulder and neck pain and exposures in customer service work with low biochemical demands. Ergonomics 2002, 45, 887–909. [Google Scholar] [CrossRef]
- Hong, X.; Lee, Y.C.; Zhou, S. Musculoskeletal symptoms and associated factors among manual porcelain workers at different workstations: A cross-sectional study. Int. Arch. Occup. Environ. Health 2022, 95, 1845–1857. [Google Scholar] [CrossRef]
- Ijaz, M.; Ahmad, S.R.; Akram, M.; Khan, W.U.; Yasin, N.A.; Nadeem, F.A. Quantitative and qualitative assessment of musculoskeletal disorders and socioeconomic issues of workers of brick industry in Pakistan. Int. J. Ind. Ergon. 2020, 76, 102933. [Google Scholar] [CrossRef]
- Intranuovo, G.; De Maria, L.; Facchini, F.; Giustiniano, A.; Caputi, A.; Birtolo, F.; Vimercati, L. Risk assessment of upper limbs repetitive movements in a fish industry. BMC Res. Notes 2019, 12, 354. [Google Scholar] [CrossRef]
- Iram, H.; Kashif, M.; Sattar, M.; Bhatti, Z.M.; Dustgir, A.; Mehdi, Z. Ergonomic risk factors among computer office workers for complaints of arm, neck and shoulder and workstation evaluation. Work 2022, 73, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Jahromy, F.H.; Jahromy, S.A.M. Musculoskeletal Disorders Risk Level among Workers of Jahrom University of Medical Science: An Ergonomic Assessment. Ambient Sci. 2019, 6, 43–46. [Google Scholar] [CrossRef]
- Jain, R.; Meena, M.L.; Dangayach, G.S.; Bhardwaj, A.K. Association of risk factors with musculoskeletal disorders in manual-working farmers. Arch. Environ. Occup. Health 2018, 73, 19–28. [Google Scholar] [CrossRef]
- Jain, R.; Meena, M.L.; Dangayach, G.S.; Bhardwaj, A.K. Risk factors for musculoskeletal disorders in manual harvesting farmers of Rajasthan. Ind. Health 2018, 56, 241–248. [Google Scholar] [CrossRef]
- Asadi, H.; Simons, M.C.; Breur, G.J.; Yu, D. Characterizing Exposure to Physical Risk Factors during Veterinary Surgery with Wearable Sensors: A Pilot Study. IISE Trans. Occup. Ergon. Hum. Factors 2022, 10, 151–160. [Google Scholar] [CrossRef]
- Jansen, K.; Esko, L.; Luik, M.; Viljasoo, V.; Ereline, J.; Gapeyeva, H.; Aibast, H.; Pääsuke, M. Workload assessment and its influence on a male tile layers working ability. Agron. Res. 2011, 9, 299–304. [Google Scholar]
- Jones, T.; Kumar, S. Comparison of ergonomic risk assessment output in a repetitive sawmill occupation: Trim-saw operator. Work 2008, 31, 367–376. [Google Scholar] [PubMed]
- Jones, T.; Kumar, S. Comparison of ergonomic risk assessment output in four sawmill jobs. Int. J. Occup. Saf. Ergon. 2010, 16, 105–111. [Google Scholar] [CrossRef]
- Kallenberg, L.A.C.; Hermens, H.J.; Vollenbroek-Hutten, M.M.R. Distinction between computer workers with and without work-related neck-shoulder complaints based on multiple surface EMG parameters. Int. J. Ind. Ergon. 2006, 36, 921–929. [Google Scholar] [CrossRef]
- Kapellusch, J.M.; Garg, A.; Hegmann, K.T.; Thiese, M.S.; Malloy, E.J. The strain index and ACGIH TLV for HAL: Risk of trigger digit in the WISTAH prospective cohort. Hum. Factors 2014, 56, 98–111. [Google Scholar] [CrossRef]
- Keester, D.L.; Sommerich, C.M. Investigation of musculoskeletal discomfort, work postures, and muscle activation among practicing tattoo artists. Appl. Ergon. 2017, 58, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Banga, H.K.; Kumar, R.; Singh, S.; Singh, S.; Scutaru, M.L.; Pruncu, C.I. Ergonomic evaluation of workstation design using taguchi experimental approach: A case of an automotive industry. Int. J. Interact. Des. Manuf. 2021, 15, 481–498. [Google Scholar] [CrossRef]
- Kuta, Ł.; Ciez, J.; Golab, I. Assessment of workload on musculoskeletal system of milkers in mechanical milking through the use of Job Strain Index method. Sci. Pap. Ser. Manag. Econ. Eng. Agric. Rural Dev. 2015, 15, 251. [Google Scholar]
- Landau, K.; Rademacher, H.; Meschke, H.; Winter, G.; Schaub, K.; Grasmueck, M.; Moelbert, I.; Sommer, M.; Schulze, J. Musculoskeletal disorders in assembly jobs in the automotive industry with special reference to age management aspects. Int. J. Ind. Ergon. 2008, 38, 561–576. [Google Scholar] [CrossRef]
- Macdonald, V.; Keir, P.J. Assessment of Musculoskeletal Disorder Risk with Hand and Syringe use in Chemotherapy Nurses and Pharmacy Assistants. IISE Trans. Occup. Ergon. Hum. Factors 2018, 6, 128–142. [Google Scholar] [CrossRef]
- Bakhsh, H.R.; Bakhsh, H.H.; Alotaibi, S.M.; Abuzaid, M.A.; Aloumi, L.A.; Alorf, S.F. Musculoskeletal disorder symptoms in saudi allied dental professionals: Is there an underestimation of related occupational risk factors? Int. J. Environ. Res. Public Health 2021, 18, 10167. [Google Scholar] [CrossRef]
- Marak, T.; Bhagat, D.; Borah, S. Musculoskeletal disorders of garo women workers engaged in tea-plucking activity: An ergonomic analysis. Indian J. Occup. Environ. Med. 2020, 24, 60–65. [Google Scholar] [CrossRef]
- Masci, F.; Rosecrance, J.; Mixco, A.; Cortinovis, I.; Calcante, A.; Mandic-Rajcevic, S.; Colosio, C. Personal and occupational factors contributing to biomechanical risk of the distal upper limb among dairy workers in the Lombardy region of Italy. Appl. Ergon. 2020, 83, 102796. [Google Scholar] [CrossRef] [PubMed]
- Masci, F.; Mixco, A.; Brents, C.A.; Murgia, L.; Colosio, C.; Rosecrance, J. Comparison of Upper Limb Muscle Activity among Workers in Large-Herd U.S. and Small-Herd Italian Dairies. Front. Public Health 2016, 4, 141. [Google Scholar] [CrossRef]
- Mathiassen, S.E.; Möller, T.; Forsman, M. Variability in mechanical exposure within and between individuals performing a highly constrained industrial work task. Ergonomics 2003, 46, 800–824. [Google Scholar] [CrossRef]
- Meyers, A.R.; Wurzelbacher, S.J.; Krieg, E.F.; Ramsey, J.G.; Crombie, K.; Christianson, A.L.; Luo, L.; Burt, S. Work-Related Risk Factors for Rotator Cuff Syndrome in a Prospective Study of Manufacturing and Healthcare Workers. Hum. Factors 2021, 00187208211022122. [Google Scholar] [CrossRef] [PubMed]
- Mixco, A.; Masci, F.; Brents, C.A.; Rosecrance, J. Upper Limb Muscle Activity among Workers in Large-Herd Industrialized Dairy Operations. Front. Public Health 2016, 4, 134. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, G. Risk factors for the prevalence of the upper limb and neck work-related musculoskeletal disorders among poultry slaughter workers. J. Musculoskelet. Res. 2012, 15, 1250005. [Google Scholar] [CrossRef]
- Mohammadipour, F.; Pourranjbar, M.; Naderi, S.; Rafie, F. Work-related Musculoskeletal Disorders in Iranian Office Workers: Prevalence and Risk Factors. J. Med. Life 2018, 11, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Mohammadpour, H.; Jalali, M.; Moussavi-Najarkola, S.A.; Farhadi, S.; Kangavari, M.; Ghanbari Sartang, A. Ergonomic Risk Assessment of Distal Upper Extremities by Job Strain Index in Carpet Weavers. Health Scope 2018, 7, e64182. [Google Scholar] [CrossRef]
- Mork, P.J.; Westgaard, R.H. The influence of body posture, arm movement, and work stress on trapezius activity during computer work. Eur. J. Appl. Physiol. 2007, 101, 445–456. [Google Scholar] [CrossRef]
- Bergsten, E.L.; Mathiassen, S.E.; Kwak, L.; Vingård, E. Daily shoulder pain among flight baggage handlers and its association with work tasks and upper arm postures on the same day. Ann. Work Expo. Health 2017, 61, 1145–1153. [Google Scholar] [CrossRef]
- Mosaly, P.R. Multifactor association of job, individual and psychosocial factors in prevalence of distal upper extremity disorders and quantification of job physical exposure. Int. J. Ind. Ergon. 2016, 55, 40–45. [Google Scholar] [CrossRef]
- Moussavi-najarkola, S.A. Application of the Strain Index (SI) Method for the Evaluation of Risk Factors Featuring Distal Upper Extremity (DUE) Musculoskeletal Disorders in a Textile Factory. Pakistan J. Med. Health Sci. 2008, 2, 42–45. [Google Scholar]
- Mukhopadhyay, P.; Srivastava, S. Evaluating ergonomic risk factors in non-regulated stone carving units of Jaipur. Work 2010, 35, 87–99. [Google Scholar] [CrossRef]
- Mulla, D.M.; McDonald, A.C.; Keir, P.J. Joint moment trade-offs across the upper extremity and trunk during repetitive work. Appl. Ergon. 2020, 88, 103142. [Google Scholar] [CrossRef]
- Naik, G.; Khan, M.R. Prevalence of MSDs and Postural Risk Assessment in Floor Mopping Activity Through Subjective and Objective Measures. Saf. Health Work 2020, 11, 80–87. [Google Scholar] [CrossRef]
- Nordander, C.; Hansson, G.Å.; Ohlsson, K.; Arvidsson, I.; Balogh, I.; Strömberg, U.; Rittner, R.; Skerfving, S. Exposure-response relationships for work-related neck and shoulder musculoskeletal disorders—Analyses of pooled uniform data sets. Appl. Ergon. 2016, 55, 70–84. [Google Scholar] [CrossRef]
- Nordander, C.; Hansson, G.Å.; Rylander, L.; Asterland, P.; BystrÖm, J.U.; Ohlsson, K.; Balogh, I.; Skerfving, S. Muscular rest and gap frequency as emg measures of physical exposure: The impact of work tasks and individual related factors. Ergonomics 2000, 43, 1904–1919. [Google Scholar] [CrossRef]
- Nwe, Y.Y.; Toyama, S.; Akagawa, M.; Yamada, M.; Sotta, K.; Tanzawa, T.; Kikuchi, C.; Ogiwara, I. Workload assessment with Ovako Working Posture Analysis System (OWAS) in Japanese vineyards with focus on pruning and berry thinning operations. J. Japanese Soc. Hortic. Sci. 2012, 81, 320–326. [Google Scholar] [CrossRef]
- Oksa, J.; Hosio, S.; Mäkinen, T.; Lindholm, H.; Rintamäki, H.; Rissanen, S.; Latvala, J.; Vaara, K.; Oksa, P. Muscular, cardiorespiratory and thermal strain of mast and pole workers. Ergonomics 2014, 57, 669–678. [Google Scholar] [CrossRef]
- Østensvik, T.; Veiersted, K.B.; Nilsen, P. A method to quantify frequency and duration of sustained low-level muscle activity as a risk factor for musculoskeletal discomfort. J. Electromyogr. Kinesiol. 2009, 19, 283–294. [Google Scholar] [CrossRef]
- Bhatt, H.; Sidhu, M.K. Physiological stress assessment of female workers at kitchen workstation. Work 2012, 41, 441–446. [Google Scholar] [CrossRef]
- Østensvik, T.; Veiersted, K.B.; Nilsen, P. Association between numbers of long periods with sustained low-level trapezius muscle activity and neck pain. Ergonomics 2009, 52, 1556–1567. [Google Scholar] [CrossRef]
- Ou, Y.K.; Liu, Y.; Chang, Y.P.; Lee, B.O. Relationship between musculoskeletal disorders and work performance of nursing staff: A comparison of hospital nursing departments. Int. J. Environ. Res. Public Health 2021, 18, 7085. [Google Scholar] [CrossRef]
- Poochada, W.; Chaiklieng, S. Ergonomic Risk Assessment among Call Center Workers. Procedia Manuf. 2015, 3, 4613–4620. [Google Scholar] [CrossRef]
- Pourmahabadian, M.; Saraji, J.N.; Aghabeighi, M.; Saddeghi-Naeeni, H. Risk assessment of developing distal upper extremity disorders by strain index method in an assembling electronic industry. Acta Med. Iran. 2005, 43, 347–354. [Google Scholar]
- Proto, A.R.; Zimbalatti, G. Risk assessment of repetitive movements in olive growing: Analysis of annual exposure level assessment models with the OCRA checklist. J. Agric. Saf. Health 2015, 21, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.N.A.; Razak, N.S.A.; Hassan, M.F.; Adzila, S.; Ngali, M.Z.; Salleh, S.M. Quantifying exposure to risk factors among office workers using ROSA method. Adv. Sci. Lett. 2017, 23, 7597–7600. [Google Scholar] [CrossRef]
- Rodrigues, M.S.A.; Leite, R.D.V.; Lelis, C.M.; Chaves, T.C. Differences in ergonomic and workstation factors between computer office workers with and without reported musculoskeletal pain. Work 2017, 57, 563–572. [Google Scholar] [CrossRef]
- Sanmugum, S.; Karuppiah, K. Sivasankar Ergonomic risk assessment on selected hot-work workers at company XXX. Malaysian J. Public Health Med. 2020, 20, 176–185. [Google Scholar] [CrossRef]
- Sakthi Nagaraj, T.; Jeyapaul, R.; Mathiyazhagan, K. Evaluation of ergonomic working conditions among standing sewing machine operators in Sri Lanka. Int. J. Ind. Ergon. 2019, 70, 70–83. [Google Scholar] [CrossRef]
- Sjøgaard, G.; Søgaard, K.; Hermens, H.J.; Sandsjö, L.; Läubli, T.; Thorn, S.; Vollenbroek-Hutten, M.M.R.; Sell, L.; Christensen, H.; Klipstein, A.; et al. Neuromuscular assessment in elderly workers with and without work related shoulder/neck trouble: The NEW-study design and physiological findings. Eur. J. Appl. Physiol. 2006, 96, 110–121. [Google Scholar] [CrossRef] [PubMed]
- Borah, S. Physiological Workload of Hill Farm Women of Meghalaya, India Involved in Firewood Collection. Procedia Manuf. 2015, 3, 4984–4990. [Google Scholar] [CrossRef]
- Slack, P.S.; Coulson, C.J.; Ma, X.; Webster, K.; Proops, D.W. The effect of operating time on surgeons’ muscular fatigue. Ann. R. Coll. Surg. Engl. 2008, 90, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Spielholz, P.; Bao, S.; Howard, N.; Silverstein, B.; Fan, J.; Smith, C.; Salazar, C. Reliability and validity assessment of the hand activity level threshold limit value and strain index using expert ratings of mono-task jobs. J. Occup. Environ. Hyg. 2008, 5, 250–275. [Google Scholar] [CrossRef]
- Subramaniam, S.; Murugesan, S.; Jayaraman, S. Assessment of shoulder and low back muscle activity of male kitchen workers using surface electromyography. Int. J. Occup. Med. Environ. Health 2018, 31, 81–90. [Google Scholar] [CrossRef]
- Subramaniam, S.; Raju, N.; Jeganathan, K.; Periyasamy, M. Evaluation of vibrant muscles over the shoulder region among workers of the hand screen printing industry. Int. J. Occup. Saf. Ergon. 2018, 24, 278–285. [Google Scholar] [CrossRef]
- Tahernejad, S.; Choobineh, A.; Razeghi, M.; Abdoli-Eramaki, M.; Parsaei, H.; Daneshmandi, H.; Seif, M. Investigation of office workers’ sitting behaviors in an ergonomically adjusted workstation. Int. J. Occup. Saf. Ergon. 2022, 28, 2346–2354. [Google Scholar] [CrossRef]
- Widiyawati, S.; Lukodono, R.P.; Lustyana, A.T.; Pradana, I.A. Investigation of the risk of daily officer work posture based on rapid upper limb assessment (rula) method. Int. J. Hum. Mov. Sport. Sci. 2020, 8, 24–31. [Google Scholar] [CrossRef]
- Yayli, D.; Caliskan, E. Comparison of Ergonomic Risk Analysis Methods for Working Postures of Forest Nursery Workers. Eur. J. For. Eng. 2019, 5, 18–24. [Google Scholar] [CrossRef]
- Yazdanirad, S.; Pourtaghi, G.; Raei, M.; Ghasemi, M. Development of modified rapid entire body assessment (MOREBA) method for predicting the risk of musculoskeletal disorders in the workplaces. BMC Musculoskelet. Disord. 2022, 23, 82. [Google Scholar] [CrossRef] [PubMed]
- Yung, M.; Lang, A.E.; Stobart, J.; Kociolek, A.M.; Milosavljevic, S.; Trask, C. The combined fatigue effects of sequential exposure to seated whole body vibration and physical, mental, or concurrent work demands. PLoS ONE 2017, 12, e0188468. [Google Scholar] [CrossRef]
- Zhang, F.R.; He, L.H.; Wu, S.S.; Li, J.Y.; Ye, K.P.; Wang, S. Quantify work load and muscle functional activation patterns in neck-shoulder muscles of female sewing machine operators using surface electromyogram. Chin. Med. J. 2011, 124, 3731–3737. [Google Scholar] [CrossRef]
- Bruno Garza, J.L.; Eijckelhof, B.H.W.; Johnson, P.W.; Raina, S.M.; Rynell, P.W.; Huysmans, M.A.; van Dieën, J.H.; van der Beek, A.J.; Blatter, B.M.; Dennerlein, J.T. Observed differences in upper extremity forces, muscle efforts, postures, velocities and accelerations across computer activities in a field study of office workers. Ergonomics 2012, 55, 670–681. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wu, X.; Gao, J.; Chen, J.; Xv, X. Simulation and ergonomic evaluation of welders’ standing posture using Jack software. Int. J. Environ. Res. Public Health 2019, 16, 4354. [Google Scholar] [CrossRef]
- Zolfaghari Nejhad, N.; Khavanin, A.; Vosoughi, S. The Effect of Simultaneous Postural Stress and Noise Exposure on Strain Index Number Among the Machinery Women Aged 25–30 Years old in Gas Supply Parts Manufactories. Health Scope 2015, 4, 23602. [Google Scholar] [CrossRef]
- Yoon, T.L.; Min, J.H.; Kim, H.N. Effect of using an 8-figure shoulder brace on posture and muscle activities during the performance of dental hygiene procedures. Int. J. Environ. Res. Public Health 2020, 17, 8494. [Google Scholar] [CrossRef]
- Wolf, P.; Rausch, J.; Hennes, N.; Potthast, W. The effects of joint angle variability and different driving load scenarios on maximum muscle activity—A driving posture simulation study. Int. J. Ind. Ergon. 2021, 84, 103161. [Google Scholar] [CrossRef]
- Nelson, J.E.; Treaster, D.E.; Marras, W.S. Finger motion, wrist motion and tendon travel as a function of keyboard angles. Clin. Biomech. 2000, 15, 489–498. [Google Scholar] [CrossRef]
- Motamedzadeh, M.; Jalali, M.; Golmohammadi, R.; Faradmal, J.; Zakeri, H.R.; Nasiri, I. Ergonomic risk factors and musculoskeletal disorders in bank staff: An interventional follow-up study in Iran. J. Egypt. Public Health Assoc. 2021, 96, 34. [Google Scholar] [CrossRef] [PubMed]
- Motamedzade, M.; Mohseni, M.; Golmohammadi, R.; Mahjoob, H. Ergonomics intervention in an Iranian television manufacturing industry. Work 2011, 38, 257–263. [Google Scholar] [CrossRef] [PubMed]
- McGorry, R.W.; Maikala, R.V.; Lin, J.H.; Rivard, A. Oxygenation kinetics of forearm muscles as a function of handle diameter during a repetitive power grip force task. Int. J. Ind. Ergon. 2009, 39, 465–470. [Google Scholar] [CrossRef]
- Lowe, B.D.; Shaw, P.B.; Wilson, S.R.; Whitaker, J.R.; Witherspoon, G.J.; Hudock, S.D.; Barrero, M.; Ray, T.K.; Wurzelbacher, S.J. Evaluation of a Workplace Exercise Program for Control of Shoulder Disorders in Overhead Assembly Work. J. Occup. Environ. Med. 2017, 59, 563–570. [Google Scholar] [CrossRef]
- Lowe, B.D.; Albers, J.; Hudock, S.D. A biomechanical assessment of hand/arm force with pneumatic nail gun actuation systems. Int. J. Ind. Ergon. 2014, 44, 715–722. [Google Scholar] [CrossRef]
- Kumar, S.; Muralidhar, M. Analysis for prevalence of carpal tunnel syndrome in shocker manufacturing workers. Adv. Prod. Eng. Manag. 2016, 11, 126–140. [Google Scholar] [CrossRef]
- Krüger, K.; Petermann, C.; Pilat, C.; Schubert, E.; Pons-Kühnemann, J.; Mooren, F.C. Preventive strength training improves working ergonomics during welding. Int. J. Occup. Saf. Ergon. 2015, 21, 150–157. [Google Scholar] [CrossRef]
- Koleini Mamaghani, N.; Shimomura, Y.; Iwanaga, K.; Katsuura, T. Effects of strap support in a hand-held device on the muscular activity in female workers assessed by electromyography and subjective rating. Ergonomics 2009, 52, 848–859. [Google Scholar] [CrossRef] [PubMed]
- Johnson, B.; Otieno, W.; Campbell-Kyureghyan, N. Influence of Jackhammer Weight on Grip Pressure, Muscle Activity, and Hand–Arm Vibration of the Operator. IISE Trans. Occup. Ergon. Hum. Factors 2017, 5, 12–22. [Google Scholar] [CrossRef]
- Stenlund, B.; Lindbeck, L.; Karlsson, D. Significance of house painters’ work techniques on shoulder muscle strain during overhead work. Ergonomics 2002, 45, 455–468. [Google Scholar] [CrossRef]
- Hess, J.A.; Kincl, L.D.; Davis, K. The impact of drywall handling tools on the low back. Appl. Ergon. 2010, 41, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Hedegaard, M.; Støttrup, N.; Sørensen, F.F.; Langer, T.H.; Samani, A. Evaluation of five steering input devices in terms of muscle activity, upper body kinematics and steering performance during heavy machine simulator driving. Int. J. Ind. Ergon. 2019, 72, 137–145. [Google Scholar] [CrossRef]
- Harris-Adamson, C.; Chen, B.; Janowitz, I.; Rempel, D.M. Ergonomic evaluation of an alternative tool for cake decorating. Int. J. Ind. Ergon. 2017, 57, 63–67. [Google Scholar] [CrossRef]
- Gaudez, C.; Wild, P.; Aublet-Cuvelier, A. A better way of fitting clips? A comparative study with respect to physical workload. Appl. Ergon. 2015, 51, 236–243. [Google Scholar] [CrossRef]
- Gagnon, M.; Delisle, A.; Desjardins, P. Biomechanical differences between best and worst performances in repeated free asymmetrical lifts. Int. J. Ind. Ergon. 2002, 29, 73–83. [Google Scholar] [CrossRef]
- Gagnon, M. The efficacy of training for three manual handling strategies based on the observation of expert and novice workers. Clin. Biomech. 2003, 18, 601–611. [Google Scholar] [CrossRef]
- Fischer, S.L.; Dickerson, C.R. Applying psychophysics to prevent overexposure: On the relationships between acceptable manual force, joint loading, and perception. Int. J. Ind. Ergon. 2014, 44, 266–274. [Google Scholar] [CrossRef]
- Earle-Richardson, G.; Jenkins, P.L.; Strogatz, D.; Bell, E.M.; Sorensen, J.A.; May, J.J. Orchard evaluation of ergonomically modified apple bucket. J. Agromed. 2006, 11, 95–105. [Google Scholar] [CrossRef]
- Earle-Richardson, G.; Jenkins, P.L.; Strogatz, D.; Bell, E.M.; Freivalds, A.; Sorensen, J.A.; May, J.J. Electromyographic assessment of apple bucket intervention designed to reduce back strain. Ergonomics 2008, 51, 902–919. [Google Scholar] [CrossRef]
- Drinkaus, P.; Sesek, R.; Bloswick, D.; Bernard, T.; Walton, B.; Joseph, B.; Reeve, G.; Counts, J.H. Comparison of ergonomic risk assessment outputs from Rapid Upper Limb Assessment and the Strain Index for tasks in automotive assembly plants. Work 2003, 21, 165–172. [Google Scholar]
- Singh, A.K.; Meena, M.L.; Chaudhary, H. Assessment of low-cost tool intervention among carpet alignment workers exposed to hand-arm vibration and shift in hearing threshold. Int. J. Hum. Factors Ergon. 2018, 5, 189. [Google Scholar] [CrossRef]
- Ding, Y.; Cao, Y.; Duffy, V.G.; Zhang, X. It is Time to Have Rest: How do Break Types Affect Muscular Activity and Perceived Discomfort During Prolonged Sitting Work. Saf. Health Work 2020, 11, 207–214. [Google Scholar] [CrossRef]
- Denadai, M.S.; Alouche, S.R.; Valentim, D.P.; Padula, R.S. An ergonomics educational training program to prevent work-related musculoskeletal disorders to novice and experienced workers in the poultry processing industry: A quasi-experimental study. Appl. Ergon. 2021, 90, 103234. [Google Scholar] [CrossRef]
- Dempsey, P.G.; McGorry, R.W.; O’Brien, N.V. The effects of work height, workpiece orientation, gender, and screwdriver type on productivity and wrist deviation. Int. J. Ind. Ergon. 2004, 33, 339–346. [Google Scholar] [CrossRef]
- de Barros, F.C.; Moriguchi, C.S.; Chaves, T.C.; Andrews, D.M.; Sonne, M.; de Oliveira Sato, T. Usefulness of the Rapid Office Strain Assessment (ROSA) tool in detecting differences before and after an ergonomics intervention. BMC Musculoskelet. Disord. 2022, 23, 526. [Google Scholar] [CrossRef]
- Da Col, S.; Kim, E.; Sanna, A. Human performance and mental workload in augmented reality: Brain computer interface advantages over gestures. Brain-Comput. Interfaces 2022, 9, 211–225. [Google Scholar] [CrossRef]
- Colim, A.; Morgado, R.; Carneiro, P.; Costa, N.; Faria, C.; Sousa, N.; Rocha, L.A.; Arezes, P. Lean manufacturing and ergonomics integration: Defining productivity and wellbeing indicators in a human–robot workstation. Sustainability 2021, 13, 1931. [Google Scholar] [CrossRef]
- Chien, T.I.; Liang, H.W.; Lee, Y.F.; Liu, F.Y.; Hsu, C.K.; Liu, S.T.; Lee, M.S.M.; Wei, P.F. Evaluation of Newly Developed Easy-Open Assistive Devices for Pneumatic Tube System Carriers for the Reduction of Work-Related Musculoskeletal Disorders. Biomed Res. Int. 2021, 2021, 8853602. [Google Scholar] [CrossRef]
- Cabeças, J.M.; Milho, R.J. The efforts in the forearm during the use of anti-vibration gloves in simulated work tasks. Int. J. Ind. Ergon. 2011, 41, 289–297. [Google Scholar] [CrossRef]
- Brandt, M.; Madeleine, P.; Samani, A.; Ajslev, J.Z.N.; Jakobsen, M.D.; Sundstrup, E.; Andersen, L.L. Effects of a participatory ergonomics intervention with wearable technical measurements of physical workload in the construction industry: Cluster randomized controlled trial. J. Med. Internet Res. 2018, 20, e10272. [Google Scholar] [CrossRef]
- Bhattacharyya, N.; Chakrabarti, D. Ergonomic basket design to reduce cumulative trauma disorders in tea leaf plucking operation. Work 2012, 41, 1234–1238. [Google Scholar] [CrossRef]
- Sesto, M.E.; Radwin, R.G.; Best, T.M.; Richard, T.G. Upper limb mechanical changes following short duration repetitive eccentric exertions. Clin. Biomech. 2004, 19, 921–928. [Google Scholar] [CrossRef]
- Berrio, S.; Barrero, L.H. Effect of Time Elapsed since Last Pruner Maintenance on Upper-Extremity Biomechanics during Manual Flower Cutting. J. Agromed. 2018, 23, 166–175. [Google Scholar] [CrossRef]
- Berrio, S.; Barrero, L.H.; Quintana, L.A. A field experiment comparing mechanical demands of two pruners for flower cutting. Work 2012, 41, 1342–1345. [Google Scholar] [CrossRef]
- Bazazan, A.; Dianat, I.; Feizollahi, N.; Mombeini, Z.; Shirazi, A.M.; Castellucci, H.I. Effect of a posture correction–based intervention on musculoskeletal symptoms and fatigue among control room operators. Appl. Ergon. 2019, 76, 12–19. [Google Scholar] [CrossRef]
- Ashok, P.; Madhan Mohan, G.; Manojkumar, S. An ergonomic evaluation of workers in the winding section of the pump manufacturing industry. Work 2022, 72, 1455–1467. [Google Scholar] [CrossRef]
- Anton, D.; Rosecrance, J.C.; Gerr, F.; Merlino, L.A.; Cook, T.M. Effect of concrete block weight and wall height on electromyographic activity and heart rate of masons. Ergonomics 2005, 48, 1314–1330. [Google Scholar] [CrossRef]
- Alabdulkarim, S.; Nussbaum, M.A.; Rashedi, E.; Kim, S.; Agnew, M.; Gardner, R. Impact of task design on task performance and injury risk: Case study of a simulated drilling task. Ergonomics 2017, 60, 851–866. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Wang, Y.J.; Zhang, Z.H.; Li, D.P.; Wu, Z.Z.; Bai, R.; Meng, G. Ergonomic and efficiency analysis of conventional apple harvest process. Int. J. Agric. Biol. Eng. 2019, 12, 210–217. [Google Scholar] [CrossRef]
- Santiago, R.J.; Baptista, J.S.; Magalhães, A.; Costa, J.T. Impact of a 10-min typing task in the development of trapezius myalgia: A preliminary observational study. Int. J. Occup. Saf. Ergon. 2022, 29, 115–120. [Google Scholar] [CrossRef]
- Safarian, M.H.; Rahmati-Najarkolaei, F.; Yaghoubi, M. A Comparison of the Effects of Ergonomic, Organization, and Education Interventions on Reducing Musculoskeletal Disorders in Office Workers. Health Scope, 2018; in press. [Google Scholar] [CrossRef]
- Roquelaure, Y.; D’Espagnac, F.; Delamarre, Y.; Penneau-Fontbonne, D. Biomechanical assessment of new hand-powered pruning shears. Appl. Ergon. 2004, 35, 179–182. [Google Scholar] [CrossRef]
- Ozalp, T.; Babalik, F.C. Ergonomic evaluation of screwdriver handles under different working conditions. Occup. Ergon. 2005, 5, 187–203. [Google Scholar] [CrossRef]
- Nogueira, H.C.; Silva, L.C.D.C.B.; Coury, H.J.C.G.; Barbieri, D.F.; Oliveira, A.B. Can experience modulate handler responses to boxes designed to decrease musculoskeletal load? Ergonomics 2017, 60, 867–875. [Google Scholar] [CrossRef] [PubMed]
- Antwi-Afari, M.F.; Li, H.; Anwer, S.; Li, D.; Yu, Y.; Mi, H.Y.; Wuni, I.Y. Assessment of a passive exoskeleton system on spinal biomechanics and subjective responses during manual repetitive handling tasks among construction workers. Saf. Sci. 2021, 142, 105382. [Google Scholar] [CrossRef]
- Blanco, A.; Catalan, J.M.; Martinez, D.; Garcia-Perez, J.V.; Garcia-Aracil, N. The Effect of an Active Upper-Limb Exoskeleton on Metabolic Parameters and Muscle Activity during a Repetitive Industrial Task. IEEE Access 2022, 10, 16479–16488. [Google Scholar] [CrossRef]
- Iranzo, S.; Piedrabuena, A.; Iordanov, D.; Martinez-Iranzo, U.; Belda-Lois, J.M. Ergonomics assessment of passive upper-limb exoskeletons in an automotive assembly plant. Appl. Ergon. 2020, 87, 103120. [Google Scholar] [CrossRef]
- Kim, S.; Nussbaum, M.A. A Follow-Up Study of the Effects of An Arm Support Exoskeleton on Physical Demands and Task Performance During Simulated Overhead Work. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 163–174. [Google Scholar] [CrossRef]
- Latella, C.; Tirupachuri, Y.; Tagliapietra, L.; Rapetti, L.; Schirrmeister, B.; Bornmann, J.; Gorjan, D.; Camernik, J.; Maurice, P.; Fritzsche, L.; et al. Analysis of Human Whole-Body Joint Torques During Overhead Work With a Passive Exoskeleton. IEEE Trans. Human-Mach. Syst. 2022, 52, 1060–1068. [Google Scholar] [CrossRef]
- Lavallée-Bourget, M.H.; Campeau-Lecours, A.; Tittley, J.; Bielmann, M.; Bouyer, L.J.; Roy, J.S. The use of a three-dimensional dynamic arm support prevents the development of muscle fatigue during repetitive manual tasks in healthy individuals. PLoS ONE 2022, 17, e0266390. [Google Scholar] [CrossRef] [PubMed]
- Maurice, P.; Ivaldi, S.; Babic, J.; Camernik, J.; Gorjan, D.; Schirrmeister, B.; Bornmann, J.; Tagliapietra, L.; Latella, C.; Pucci, D.; et al. Objective and Subjective Effects of a Passive Exoskeleton on Overhead Work. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 152–164. [Google Scholar] [CrossRef]
- Missiroli, F.; Lotti, N.; Xiloyannis, M.; Sloot, L.H.; Riener, R.; Masia, L. Relationship Between Muscular Activity and Assistance Magnitude for a Myoelectric Model Based Controlled Exosuit. Front. Robot. AI 2020, 7, 190. [Google Scholar] [CrossRef] [PubMed]
- Pacifico, I.; Aprigliano, F.; Parri, A.; Cannillo, G.; Melandri, I.; Sabatini, A.M.; Violante, F.S.; Molteni, F.; Giovacchini, F.; Vitiello, N.; et al. Evaluation of a spring-loaded upper-limb exoskeleton in cleaning activities. Appl. Ergon. 2023, 106, 103877. [Google Scholar] [CrossRef] [PubMed]
- Pacifico, I.; Molteni, F.; Giovacchini, F.; Vitiello, N.; Crea, S.; Scano, A.; Guanziroli, E.; Moise, M.; Morelli, L.; Chiavenna, A.; et al. An experimental evaluation of the proto-mate: A novel ergonomic upper-limb exoskeleton to reduce workers’ physical strain. IEEE Robot. Autom. Mag. 2020, 27, 54–65. [Google Scholar] [CrossRef]
- Pacifico, I.; Parri, A.; Taglione, S.; Sabatini, A.M.; Violante, F.S.; Molteni, F.; Giovacchini, F.; Vitiello, N.; Crea, S. Exoskeletons for workers: A case series study in an enclosures production line. Appl. Ergon. 2022, 101, 103679. [Google Scholar] [CrossRef] [PubMed]
- Park, D.; Toxiri, S.; Chini, G.; Natali, C.D.; Caldwell, D.G.; Ortiz, J. Shoulder-sideWINDER (Shoulder-side Wearable INDustrial Ergonomic Robot): Design and Evaluation of Shoulder Wearable Robot with Mechanisms to Compensate for Joint Misalignment. IEEE Trans. Robot. 2022, 38, 1460–1471. [Google Scholar] [CrossRef]
- De Bock, S.; Ampe, T.; Rossini, M.; Tassignon, B.; Lefeber, D.; Rodriguez-Guerrero, C.; Roelands, B.; Geeroms, J.; Meeusen, R.; De Pauw, K. Passive shoulder exoskeleton support partially mitigates fatigue-induced effects in overhead work. Appl. Ergon. 2023, 106, 103903. [Google Scholar] [CrossRef] [PubMed]
- Park, K.S.; Hong, G.B.; Lee, S. Fatigue problems in remote pointing and the use of an upper-arm support. Int. J. Ind. Ergon. 2012, 42, 293–303. [Google Scholar] [CrossRef]
- Pinho, J.P.; Forner-Cordero, A. Shoulder muscle activity and perceived comfort of industry workers using a commercial upper limb exoskeleton for simulated tasks. Appl. Ergon. 2022, 101, 103718. [Google Scholar] [CrossRef] [PubMed]
- Tetteh, E.; Hallbeck, M.S.; Mirka, G.A. Effects of passive exoskeleton support on EMG measures of the neck, shoulder and trunk muscles while holding simulated surgical postures and performing a simulated surgical procedure. Appl. Ergon. 2022, 100, 103646. [Google Scholar] [CrossRef]
- Van Engelhoven, L.; Poon, N.; Kazerooni, H.; Rempel, D.; Barr, A.; Harris-Adamson, C. Experimental Evaluation of a Shoulder-Support Exoskeleton for Overhead Work: Influences of Peak Torque Amplitude, Task, and Tool Mass. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 250–263. [Google Scholar] [CrossRef]
- Visser, B.; De Korte, E.; Van Der Kraan, I.; Kuijer, P. The effect of arm and wrist supports on the load of the upper extremity during VDU work. Clin. Biomech. 2000, 15, S34–S38. [Google Scholar] [CrossRef]
- Xiloyannis, M.; Chiaradia, D.; Frisoli, A.; Masia, L. Physiological and kinematic effects of a soft exosuit on arm movements. J. Neuroeng. Rehabil. 2019, 16, 29. [Google Scholar] [CrossRef]
- Yin, P.; Yang, L.; Qu, S. Development of an ergonomic wearable robotic device for assisting manual workers. Int. J. Adv. Robot. Syst. 2021, 18, 17298814211046745. [Google Scholar] [CrossRef]
- Yoo, I.G.; Yoo, W.G. The effect of a new neck support tying method using Thera-Band on cervical ROM and shoulder muscle pain after overhead work. J. Phys. Ther. Sci. 2013, 25, 843–844. [Google Scholar] [CrossRef]
- Ziaei, M.; Choobineh, A.; Ghaem, H.; Abdoli-Eramaki, M. Evaluation of a passive low-back support exoskeleton (Ergo-Vest) for manual waste collection. Ergonomics 2021, 64, 1255–1270. [Google Scholar] [CrossRef] [PubMed]
- Luger, T.; Seibt, R.; Cobb, T.J.; Rieger, M.A.; Steinhilber, B. Influence of a passive lower-limb exoskeleton during simulated industrial work tasks on physical load, upper body posture, postural control and discomfort. Appl. Ergon. 2019, 80, 152–160. [Google Scholar] [CrossRef] [PubMed]
- De Bock, S.; Rossini, M.; Lefeber, D.; Rodriguez-Guerrero, C.; Geeroms, J.; Meeusen, R.; De Pauw, K. An Occupational Shoulder Exoskeleton Reduces Muscle Activity and Fatigue During Overhead Work. IEEE Trans. Biomed. Eng. 2022, 69, 3008–3020. [Google Scholar] [CrossRef]
- Du, Z.; Yan, Z.; Huang, T.; Bai, O.; Huang, Q.; Zhang, T.; Han, B. Development and Experimental Validation of a Passive Exoskeletal Vest. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 1941–1950. [Google Scholar] [CrossRef]
- Eilertsen, M.; Merryweather, A.; Roundy, S. Characterization of load reduction while lifting drywall using an unpowered drywall lifting device. Work 2018, 60, 661–671. [Google Scholar] [CrossRef]
- Garosi, E.; Mazloumi, A.; Jafari, A.H.; Keihani, A.; Shamsipour, M.; Kordi, R.; Kazemi, Z. Design and ergonomic assessment of a passive head/neck supporting exoskeleton for overhead work use. Appl. Ergon. 2022, 101, 103699. [Google Scholar] [CrossRef]
- Gillette, J.C.; Stephenson, M.L. Electromyographic Assessment of a Shoulder Support Exoskeleton During on-Site Job Tasks. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 302–310. [Google Scholar] [CrossRef]
- Grazi, L.; Trigili, E.; Proface, G.; Giovacchini, F.; Crea, S.; Vitiello, N. Design and Experimental Evaluation of a Semi-Passive Upper-Limb Exoskeleton for Workers with Motorized Tuning of Assistance. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 2276–2285. [Google Scholar] [CrossRef] [PubMed]
- Huysamen, K.; de Looze, M.; Bosch, T.; Ortiz, J.; Toxiri, S.; O’Sullivan, L.W. Assessment of an active industrial exoskeleton to aid dynamic lifting and lowering manual handling tasks. Appl. Ergon. 2018, 68, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Bao, S.; Spielholz, P.; Howard, N.; Silverstein, B. Quantifying repetitive hand activity for epidemiological research on musculoskeletal disorders—Part I: Individual exposure assessment. Ergonomics 2006, 49, 361–380. [Google Scholar] [CrossRef]
- Beltran Martinez, K.; Nazarahari, M.; Rouhani, H. K-score: A novel scoring system to quantify fatigue-related ergonomic risk based on joint angle measurements via wearable inertial measurement units. Appl. Ergon. 2022, 102, 103757. [Google Scholar] [CrossRef] [PubMed]
- Kiermayer, C.; Hoehne-Hückstädt, U.M.; Brielmeier, M.; Brütting, M.; Ellegast, R.; Schmidt, J. Musculoskeletal load in and highly repetitive actions of animal facility washroom employees. J. Am. Assoc. Lab. Anim. Sci. 2011, 50, 665–674. [Google Scholar] [PubMed]
- Kim, J.H.; Vaughan, A.; Kincl, L. Characterization of Musculoskeletal Injury Risk in Dungeness Crab Fishing. J. Agromedicine 2022, 28, 309–320. [Google Scholar] [CrossRef]
- Klussmann, A.; Liebers, F.; Gebhardt, H.; Rieger, M.A.; Latza, U.; Steinberg, U. Risk assessment of manual handling operations at work with the key indicator method (KIM-MHO)—Determination of criterion validity regarding the prevalence of musculoskeletal symptoms and clinical conditions within a cross-sectional study. BMC Musculoskelet. Disord. 2017, 18, 184. [Google Scholar] [CrossRef] [PubMed]
- Kong, Y.K.; Lee, S.J.; Lee, K.S.; Kim, G.R.; Kim, D.M. Development of an ergonomics checklist for investigation of work-related whole-body disorders in farming—AWBA: Agricultural whole-body assessment. J. Agric. Saf. Health 2015, 21, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.; Lin, J.H.; Bao, S. Inter-rater reliability of an inertial measurement unit sensor-based posture-matching method: A pilot study. Int. J. Ind. Ergon. 2020, 80, 259–265. [Google Scholar] [CrossRef]
- McKinnon, C.D.; Ehmke, S.; Kociolek, A.M.; Callaghan, J.P.; Keir, P.J. Wrist Posture Estimation Differences and Reliability Between Video Analysis and Electrogoniometer Methods. Hum. Factors 2021, 63, 1284–1294. [Google Scholar] [CrossRef]
- Menychtas, D.; Glushkova, A.; Manitsaris, S. Analyzing the kinematic and kinetic contributions of the human upper body’s joints for ergonomics assessment. J. Ambient Intell. Humaniz. Comput. 2020, 11, 6093–6105. [Google Scholar] [CrossRef]
- Nath, N.D.; Akhavian, R.; Behzadan, A.H. Ergonomic analysis of construction worker’s body postures using wearable mobile sensors. Appl. Ergon. 2017, 62, 107–117. [Google Scholar] [CrossRef]
- Park, J.K.; Boyer, J.; Tessler, J.; Casey, J.; Schemm, L.; Gore, R.; Punnett, L. Inter-rater reliability of PATH observations for assessment of ergonomic risk factors in hospital work. Ergonomics 2009, 52, 820–829. [Google Scholar] [CrossRef]
- Peppoloni, L.; Filippeschi, A.; Ruffaldi, E.; Avizzano, C.A. A novel wearable system for the online assessment of risk for biomechanical load in repetitive efforts. Int. J. Ind. Ergon. 2016, 52, 1–11. [Google Scholar] [CrossRef]
- Chen, J.; Mitrouchev, P.; Coquillart, S.; Quaine, F. Disassembly task evaluation by muscle fatigue estimation in a virtual reality environment. Int. J. Adv. Manuf. Technol. 2017, 88, 1523–1533. [Google Scholar] [CrossRef]
- Peternel, L.; Schøn, D.T.; Fang, C. Binary and Hybrid Work-Condition Maps for Interactive Exploration of Ergonomic Human Arm Postures. Front. Neurorobot. 2021, 14, 114. [Google Scholar] [CrossRef] [PubMed]
- Plantard, P.; Muller, A.; Pontonnier, C.; Dumont, G.; Shum, H.P.H.; Multon, F. Inverse dynamics based on occlusion-resistant Kinect data: Is it usable for ergonomics? Int. J. Ind. Ergon. 2017, 61, 71–80. [Google Scholar] [CrossRef]
- Poitras, I.; Bielmann, M.; Campeau-Lecours, A.; Mercier, C.; Bouyer, L.J.; Roy, J.S. Validity of wearable sensors at the shoulder joint: Combining wireless electromyography sensors and inertial measurement units to perform physical workplace assessments. Sensors 2019, 19, 1885. [Google Scholar] [CrossRef]
- Rosecrance, J.; Paulsen, R.; Murgia, L. Risk assessment of cheese processing tasks using the Strain Index and OCRA Checklist. Int. J. Ind. Ergon. 2017, 61, 142–148. [Google Scholar] [CrossRef]
- Shanahan, C.J.; Vi, P.; Salas, E.A.; Reider, V.L.; Hochman, L.M.L.; Moore, A.E. A comparison of RULA, REBA and Strain Index to four psychophysical scales in the assessment of non-fixed work. Work 2013, 45, 367–378. [Google Scholar] [CrossRef] [PubMed]
- Sharotry, A.; Jimenez, J.A.; Mediavilla, F.A.M.; Wierschem, D.; Koldenhoven, R.M.; Valles, D. Manufacturing Operator Ergonomics: A Conceptual Digital Twin Approach to Detect Biomechanical Fatigue. IEEE Access 2022, 10, 12774–12791. [Google Scholar] [CrossRef]
- Waddell, D.E.; Wyvill, C.; Gregor, R.J. Upper extremity kinetics in poultry processing: A comparison between two different cutting tasks. J. Appl. Biomech. 2003, 19, 169–177. [Google Scholar] [CrossRef]
- Cann, A.P.; Connolly, M.; Ruuska, R.; MacNeil, M.; Birmingham, T.B.; Vandervoort, A.A.; Callaghan, J.P. Inter-rater reliability of output measures for a posture matching assessment approach: A pilot study with food service workers. Ergonomics 2008, 51, 556–572. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.K.; Nimbarte, A.D.; Hsiao, H.; Gopalakrishnan, B.; Jaridi, M. A biomechanical shoulder strain index based on stabilizing demand of shoulder joint. Ergonomics 2018, 61, 1657–1670. [Google Scholar] [CrossRef] [PubMed]
- Douwes, M.; Boocock, M.; Coenen, P.; van den Heuvel, S.; Bosch, T. Predictive validity of the Hand Arm Risk assessment Method (HARM). Int. J. Ind. Ergon. 2014, 44, 328–334. [Google Scholar] [CrossRef]
- Fan, Z.J.; Bao, S.; Silverstein, B.A.; Howard, N.L.; Smith, C.K.; Bonauto, D.K. Predicting work-related incidence of lateral and medial epicondylitis using the strain index. Am. J. Ind. Med. 2014, 57, 1319–1330. [Google Scholar] [CrossRef] [PubMed]
- Ghaneh-Ezabadi, S.; Abdoli-Eramaki, M.; Arjmand, N.; Abouhossein, A.; Zakerian, S.A. The Validity and Inter-Rater Reliability of a Video-Based Posture-Matching Tool to Estimate Cumulative Loads on the Lower Back. J. Biomed. Phys. Eng. 2022, 12, 417–430. [Google Scholar] [CrossRef] [PubMed]
- Hellig, T.; Mertens, A.; Brandl, C. The interaction effect of working postures on muscle activity and subjective discomfort during static working postures and its correlation with OWAS. Int. J. Ind. Ergon. 2018, 68, 25–33. [Google Scholar] [CrossRef]
- Hubaut, R.; Guichard, R.; Greenfield, J.; Blandeau, M. Validation of an Embedded Motion-Capture and EMG Setup for the Analysis of Musculoskeletal Disorder Risks during Manhole Cover Handling. Sensors 2022, 22, 436. [Google Scholar] [CrossRef]
- Kapellusch, J.M.; Bao, S.S.; Malloy, E.J.; Thiese, M.S.; Merryweather, A.S.; Hegmann, K.T. Validation of the Revised Strain Index for Predicting Risk of Incident Carpal Tunnel Syndrome in a Prospective Cohort. Ergonomics 2021, 64, 1369–1378. [Google Scholar] [CrossRef]
- Mathiassen, S.E.; Bolin, M.; Olofsdotter, G.; Johansson, E. Equal health at work? Protocol for an observational study of work organisation, workload and musculoskeletal complaints among women and men in grocery retail. BMJ Open 2020, 10, e032409. [Google Scholar] [CrossRef]
- Santos, H.G.; Chiavegato, L.D.; Valentim, D.P.; Da Silva, P.R.; Padula, R.S. Resistance training program for fatigue management in the workplace: Exercise protocol in a cluster randomized controlled trial. BMC Public Health 2016, 16, 1218. [Google Scholar] [CrossRef]
- Shaw, W.S.; Besen, E.; Pransky, G.; Boot, C.R.L.; Nicholas, M.K.; McLellan, R.K.; Tveito, T.H. Manage at work: A randomized, controlled trial of a self-management group intervention to overcome workplace challenges associated with chronic physical health conditions. BMC Public Health 2014, 14, 515. [Google Scholar] [CrossRef]
- Trøstrup, J.; Mikkelsen, L.R.; Frost, P.; Dalbøge, A.; Høybye, M.T.; Casper, S.D.; Jørgensen, L.B.; Klebe, T.M.; Svendsen, S.W. Reducing shoulder complaints in employees with high occupational shoulder exposures: Study protocol for a cluster-randomised controlled study (The Shoulder-Café Study). Trials 2019, 20, 627. [Google Scholar] [CrossRef] [PubMed]
- Brambilla, C.; Pirovano, I.; Mira, R.M.; Rizzo, G.; Scano, A.; Mastropietro, A. Combined use of emg and eeg techniques for neuromotor assessment in rehabilitative applications: A systematic review. Sensors 2021, 21, 7014. [Google Scholar] [CrossRef] [PubMed]
- Leijten, F.R.M.; van den Heuvel, S.G.; van der Beek, A.J.; Ybema, J.F.; Robroek, S.J.W.; Burdorf, A. Associations of Work-Related Factors and Work Engagement with Mental and Physical Health: A 1-Year Follow-up Study Among Older Workers. J. Occup. Rehabil. 2015, 25, 86–95. [Google Scholar] [CrossRef] [PubMed]
- De Kok, J.; Vroonhof, P.; Snijders, J.; Roullis, G.; Clarke, M.; Peereboom, K.; van Dorst, P.; Isusi, I. Work-Related Musculoskeletal Disorders: Prevalence, Costs and Demographics in the EU; Publications Office of the European Union: Luxembourg, 2019; Available online: https://osha.europa.eu/en/publications/msds-facts-and-figures-overview-prevalence-costs-and-demographics-msds-europe (accessed on 1 March 2023).
- Koenig, A.C.; Riener, R. The human in the loop. In Neurorehabilitation Technology, 2nd ed.; Springer International Publishing: New York, NY, USA, 2016; pp. 161–181. ISBN 9783319286037. [Google Scholar]
- Longo, F.; Nicoletti, L.; Padovano, A. Smart operators in industry 4.0: A human-centered approach to enhance operators’ capabilities and competencies within the new smart factory context. Comput. Ind. Eng. 2017, 113, 144–159. [Google Scholar] [CrossRef]
- Pedrocchi, N.; Vicentini, F.; Malosio, M.; Tosatti, L.M. Safe human-robot cooperation in an industrial environment. Int. J. Adv. Robot. Syst. 2013, 10, 27. [Google Scholar] [CrossRef]
- Caporaso, T.; Grazioso, S.; Panariello, D.; Di Gironimo, G.; Lanzotti, A. Understanding the Human Motor Control for User-Centered Design of Custom Wearable Systems: Case Studies in Sports, Industry, Rehabilitation. In Proceedings of the Lecture Notes in Mechanical Engineering, Modena, Italy, 9–10 September 2019; Springer Science and Business Media Deutschland GmbH, 2020; pp. 753–764. Available online: https://link.springer.com/chapter/10.1007/978-3-030-31154-4_64 (accessed on 1 March 2023).
- Grazioso, S.; Caporaso, T.; Palomba, A.; Nardella, S.; Ostuni, B.; Panariello, D.; Di Gironimo, G.; Lanzotti, A. Assessment of upper limb muscle synergies for industrial overhead tasks: A preliminary study. In Proceedings of the 2019 IEEE International Workshop on Metrology for Industry 4.0 and IoT, MetroInd 4.0 and IoT 2019—Proceedings, Naples, Italy, 4–6 June 2019; Institute of Electrical and Electronics Engineers Inc.: New York, NY, USA, 2019; pp. 89–92. [Google Scholar]
- Scano, A.; Mira, R.M.; D’Avella, A. Mixed matrix factorization: A novel algorithm for the extraction of kinematic-muscular synergies. J. Neurophysiol. 2022, 127, 529–547. [Google Scholar] [CrossRef]
- Kim, S.; Laschi, C.; Trimmer, B. Soft robotics: A bioinspired evolution in robotics. Trends Biotechnol. 2013, 31, 287–294. [Google Scholar] [CrossRef]
- McKay, J.; Pickup, L.; Atkinson, S.; McNab, D.; Bowie, P. Human factors in general practice—Early thoughts on the educational focus for specialty training and beyond. Educ. Prim. Care 2016, 27, 162–171. [Google Scholar] [CrossRef]
- Bassey Etuknwa, A.; Humpheries, S. A Systematic Review on the Effectiveness of Ergonomic Training Intervention in Reducing the Risk of Musculoskeletal Disorder. J. Nurs. Health Stud. 2018, 3. [Google Scholar] [CrossRef]
- Faucett, J.; Garry, M.; Nadler, D.; Ettare, D. A test of two training interventions to prevent work-related musculoskeletal disorders of the upper extremity. Appl. Ergon. 2002, 33, 337–347. [Google Scholar] [CrossRef]
- Turja, J.; Kaleva, S.; Kivistö, M.; Seitsamo, J. Effects of early support intervention on workplace ergonomics—A two-year followup study. Work 2012, 41, 809–811. [Google Scholar] [CrossRef] [PubMed]
- McFarland, T.; Fischer, S. Considerations for Industrial Use: A Systematic Review of the Impact of Active and Passive Upper Limb Exoskeletons on Physical Exposures. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 322–347. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).