Visual Blood, Visualisation of Blood Gas Analysis in Virtual Reality, Leads to More Correct Diagnoses: A Computer-Based, Multicentre, Simulation Study
Abstract
1. Introduction
2. Materials and Methods
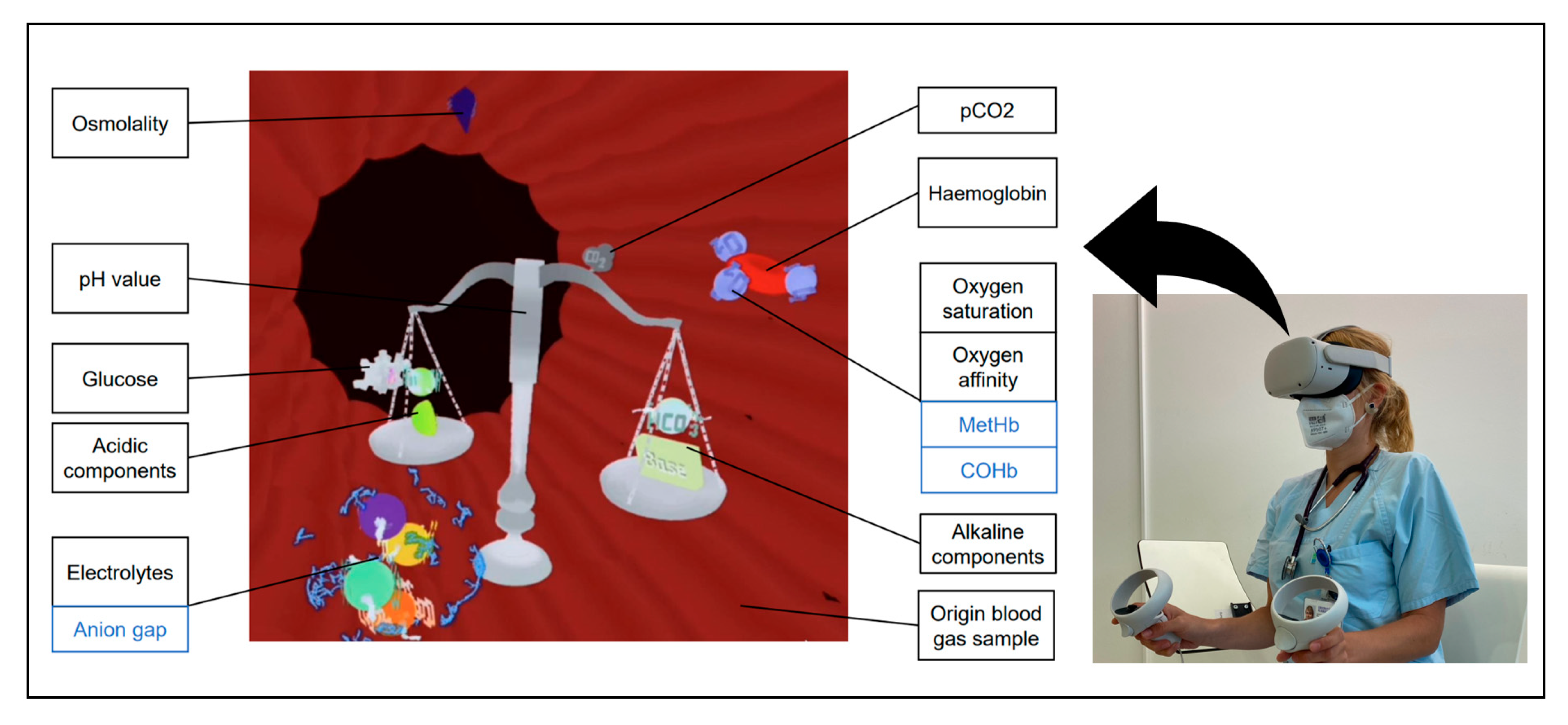
2.1. Visual Blood
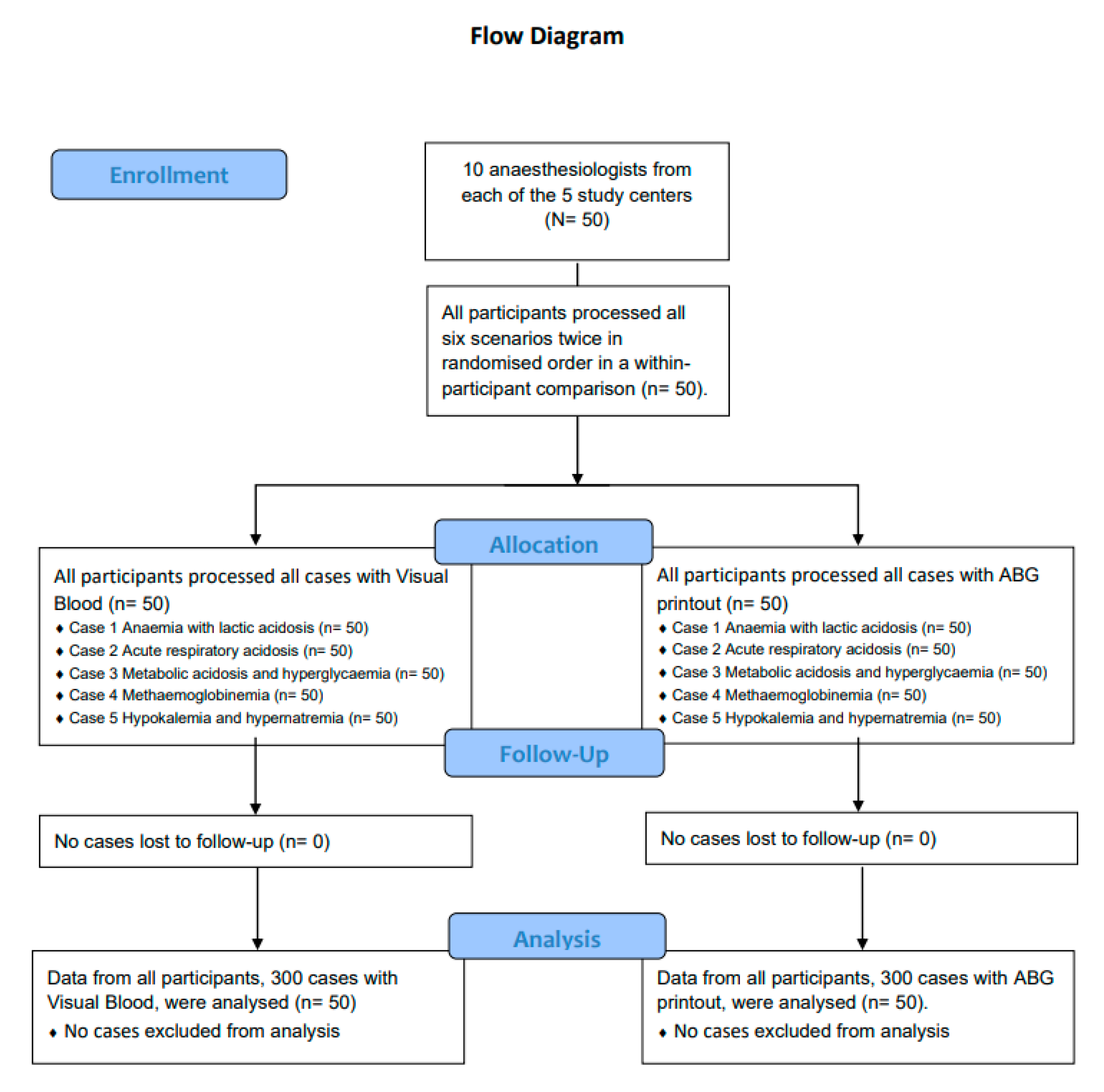
2.2. Study Design and Participants
2.3. Study Procedure
2.4. Outcome Measures
2.5. Statistical Analysis
3. Results
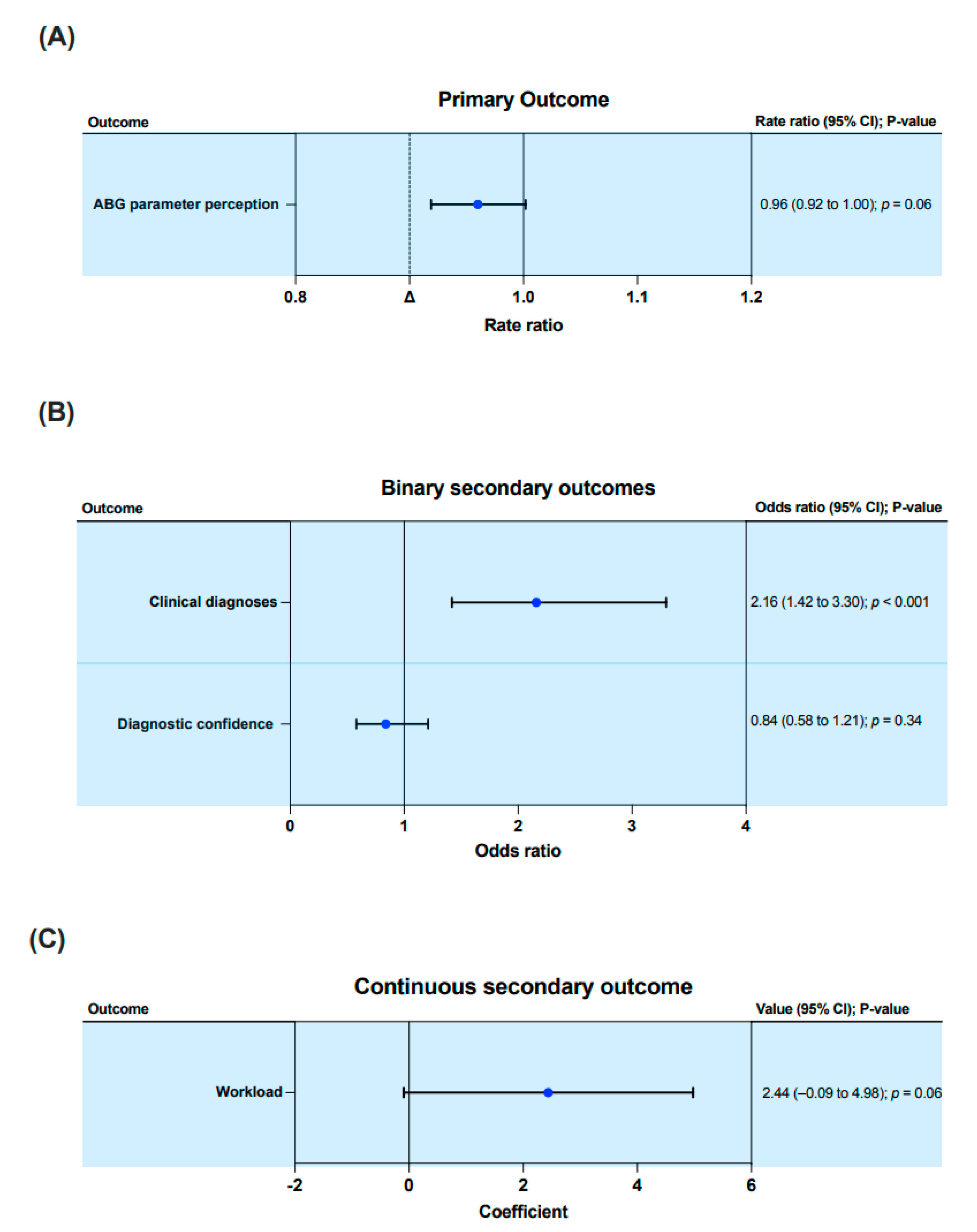
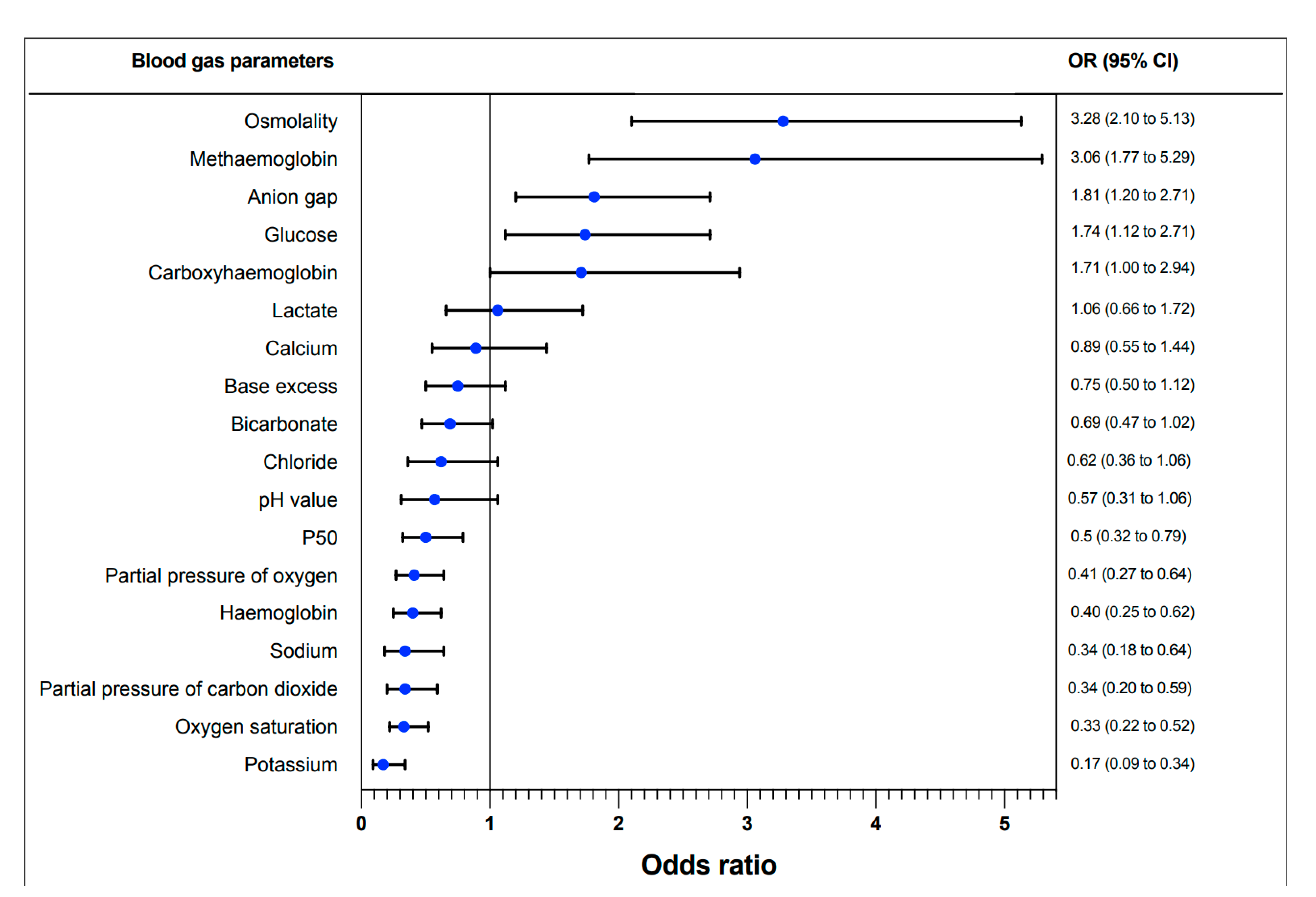
3.1. Correct ABG Parameter Perception
3.2. Correct Clinical Diagnoses
3.3. Perceived Diagnostic Confidence
3.4. Perceived Workload
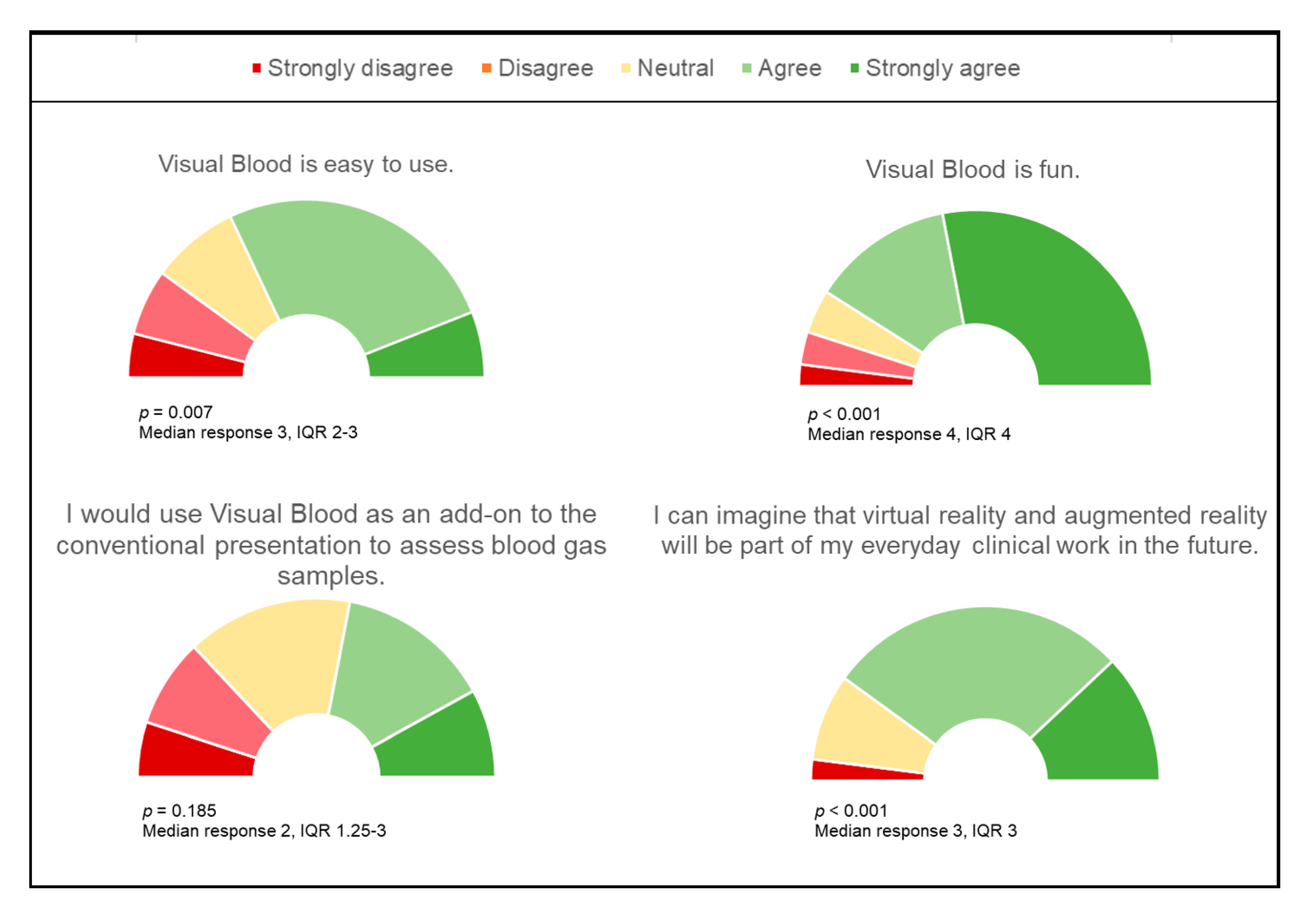
3.5. Participant Opinions on Visual Blood and Virtual Reality in Clinical Practice
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Astrup, P.; Jorgensen, K.; Andersen, O.S.; Engel, K. The acid-base metabolism. A new approach. Lancet 1960, 1, 1035–1039. [Google Scholar] [CrossRef] [PubMed]
- Campbell, E.J. Blood gas measurements in clinical practice. Postgrad. Med. J. 1961, 37, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Pesenti, A.; Matthay, M. Understanding blood gas analysis. Intensive Care Med. 2018, 44, 91–93. [Google Scholar] [CrossRef] [PubMed]
- Berend, K.; de Vries, A.P.; Gans, R.O. Physiological approach to assessment of acid-base disturbances. N. Engl. J. Med. 2014, 371, 1434–1445. [Google Scholar] [CrossRef] [PubMed]
- Berend, K. Acid-base pathophysiology after 130 years: Confusing, irrational and controversial. J. Nephrol. 2013, 26, 254–265. [Google Scholar] [CrossRef]
- Endsley, M.R. Toward a Theory of Situation Awareness in Dynamic Systems. Hum. Factors J. Hum. Factors Ergon. Soc. 1995, 37, 32–64. [Google Scholar] [CrossRef]
- Endsley, M.R. Designing for Situation Awareness: An Approach to User-Centered Design, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2016. [Google Scholar]
- Schulz, C.M.; Krautheim, V.; Hackemann, A.; Kreuzer, M.; Kochs, E.F.; Wagner, K.J. Situation awareness errors in anesthesia and critical care in 200 cases of a critical incident reporting system. BMC Anesthesiol. 2016, 16, 4. [Google Scholar] [CrossRef]
- Marshall, S. The use of cognitive aids during emergencies in anesthesia: A review of the literature. Anesth. Analg. 2013, 117, 1162–1171. [Google Scholar] [CrossRef]
- Drews, F.A.; Westenskow, D.R. The right picture is worth a thousand numbers: Data displays in anesthesia. Hum. Factors 2006, 48, 59–71. [Google Scholar] [CrossRef]
- Jenkins, B. Cognitive aids: Time for a change? Anaesthesia 2014, 69, 660–664. [Google Scholar] [CrossRef]
- Kataife, E.D.; Said, S.; Braun, J.; Roche, T.R.; Rössler, J.; Kaserer, A.; Spahn, D.R.; Mileo, F.G.; Tscholl, D.W. The Haemostasis Traffic Light, a user-centred coagulation management tool for acute bleeding situations: A simulation-based randomised dual-centre trial. Anaesthesia 2021, 76, 902–910. [Google Scholar] [CrossRef]
- Wachter, S.B.; Agutter, J.; Syroid, N.; Drews, F.; Weinger, M.B.; Westenskow, D. The employment of an iterative design process to develop a pulmonary graphical display. J. Am. Med. Inform. Assoc. JAMIA 2003, 10, 363–372. [Google Scholar] [CrossRef]
- Wachter, S.B.; Johnson, K.; Albert, R.; Syroid, N.; Drews, F.; Westenskow, D. The evaluation of a pulmonary display to detect adverse respiratory events using high resolution human simulator. J. Am. Med. Inform. Assoc. JAMIA 2006, 13, 635–642. [Google Scholar] [CrossRef]
- Tscholl, D.W.; Rossler, J.; Said, S.; Kaserer, A.; Spahn, D.R.; Nothiger, C.B. Situation Awareness-Oriented Patient Monitoring with Visual Patient Technology: A Qualitative Review of the Primary Research. Sensors 2020, 20, 2112. [Google Scholar] [CrossRef]
- Roche, T.R.; Said, S.; Braun, J.; Maas, E.J.C.; Machado, C.; Grande, B.; Kolbe, M.; Spahn, D.R.; Nöthiger, C.B.; Tscholl, D.W. Avatar-based patient monitoring in critical anaesthesia events: A randomised high-fidelity simulation study. Br. J. Anaesth. 2021, 126, 1046–1054. [Google Scholar] [CrossRef]
- Alam, F.; Matava, C. A New Virtual World? The Future of Immersive Environments in Anesthesiology. Anesth. Analg. 2022, 135, 230–238. [Google Scholar] [CrossRef]
- Wolf, J.; Wolfer, V.; Halbe, M.; Maisano, F.; Lohmeyer, Q.; Meboldt, M. Comparing the effectiveness of augmented reality-based and conventional instructions during single ECMO cannulation training. Int. J. Comput. Assist. Radiol. Surg. 2021, 16, 1171–1180. [Google Scholar] [CrossRef]
- Vávra, P.; Roman, J.; Zonča, P.; Ihnát, P.; Němec, M.; Kumar, J.; Habib, N.; El-Gendi, A. Recent Development of Augmented Reality in Surgery: A Review. J. Healthc. Eng. 2017, 2017, 4574172. [Google Scholar] [CrossRef]
- Piaggio, G.; Elbourne, D.R.; Pocock, S.J.; Evans, S.J.; Altman, D.G. Reporting of noninferiority and equivalence randomized trials: Extension of the CONSORT 2010 statement. JAMA 2012, 308, 2594–2604. [Google Scholar] [CrossRef]
- Schulz, C.M.; Endsley, M.R.; Kochs, E.F.; Gelb, A.W.; Wagner, K.J. Situation awareness in anesthesia: Concept and research. Anesthesiology 2013, 118, 729–742. [Google Scholar] [CrossRef]
- Hart, S.G.; Staveland, L.E. Development of NASA-TLX (Task Load Index): Results of Empirical and Theoretical Research. In Advances in Psychology; Hancock, P.A., Meshkati, N., Eds.; North-Holland: Amsterdam, The Netherlands, 1988; Volume 52, pp. 139–183. [Google Scholar]
- Lowndes, B.R.; Forsyth, K.L.; Blocker, R.C.; Dean, P.G.; Truty, M.J.; Heller, S.F.; Blackmon, S.; Hallbeck, M.S.; Nelson, H. NASA-TLX Assessment of Surgeon Workload Variation Across Specialties. Ann. Surg. 2020, 271, 686–692. [Google Scholar] [CrossRef]
- Said, S.; Gozdzik, M.; Roche, T.R.; Braun, J.; Rössler, J.; Kaserer, A.; Spahn, D.R.; Nöthiger, C.B.; Tscholl, D.W. Validation of the Raw National Aeronautics and Space Administration Task Load Index (NASA-TLX) Questionnaire to Assess Perceived Workload in Patient Monitoring Tasks: Pooled Analysis Study Using Mixed Models. J. Med. Internet Res. 2020, 22, e19472. [Google Scholar] [CrossRef] [PubMed]
- Dziadzko, M.A.; Herasevich, V.; Sen, A.; Pickering, B.W.; Knight, A.M.; Moreno Franco, P. User perception and experience of the introduction of a novel critical care patient viewer in the ICU setting. Int. J. Med. Inform. 2016, 88, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Carne, B.; Kennedy, M.; Gray, T. Review article: Crisis resource management in emergency medicine. Emerg. Med. Australas. 2012, 24, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Tscholl, D.W.; Handschin, L.; Neubauer, P.; Weiss, M.; Seifert, B.; Spahn, D.R.; Noethiger, C.B. Using an animated patient avatar to improve perception of vital sign information by anaesthesia professionals. Br. J. Anaesth. 2018, 121, 662–671. [Google Scholar] [CrossRef] [PubMed]
- Rossler, J.; Meybohm, P.; Spahn, D.R.; Zacharowski, K.; Braun, J.; Nothiger, C.B.; Tscholl, D.W. Improving decision making through presentation of viscoelastic tests as a 3D animated blood clot: The Visual Clot. Anaesthesia 2020, 75, 1059–1069. [Google Scholar] [CrossRef]
- Roche, T.R.; Braun, J.; Ganter, M.T.; Meybohm, P.; Herrmann, J.; Zacharowski, K.; Raimann, F.J.; Piekarski, F.; Spahn, D.R.; Nöthiger, C.B.; et al. Voice alerting as a medical alarm modality for next-generation patient monitoring: A randomised international multicentre trial. Br. J. Anaesth. 2021, 127, 769–777. [Google Scholar] [CrossRef]
- Grantcharov, T.P.; Reznick, R.K. Teaching procedural skills. BMJ 2008, 336, 1129–1131. [Google Scholar] [CrossRef]
- Moorthy, K.; Vincent, C.; Darzi, A. Simulation based training. BMJ (Clin. Res. Ed.) 2005, 330, 493–494. [Google Scholar] [CrossRef]
| Study centres, n | 5 |
| Participants per study centre, n | 10 |
| Age in years, median (IQR 25/75, (range)) | 31.0 (28/40.8 (25–56)) |
| Work experience in years, median (IQR 25/75, (range)) | 5.0 (2/10 (1–30)) |
| Gender female, n (%) | 31 (62%) |
| Resident physician, n (%) | 28 (56%) |
| Self-rated theoretical ABG skills (0 = novice, 100 = expert), median (IQR 25/75, (range)) | 70.5 (60/83 (31–100)) |
| Self-rated frequency of playing video games (0 = never, 100 = very often), median (IQR 25/75, (range)) | 6.0 (0/30.8 (0–87)) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bergauer, L.; Akbas, S.; Braun, J.; Ganter, M.T.; Meybohm, P.; Hottenrott, S.; Zacharowski, K.; Raimann, F.J.; Rivas, E.; López-Baamonde, M.; et al. Visual Blood, Visualisation of Blood Gas Analysis in Virtual Reality, Leads to More Correct Diagnoses: A Computer-Based, Multicentre, Simulation Study. Bioengineering 2023, 10, 340. https://doi.org/10.3390/bioengineering10030340
Bergauer L, Akbas S, Braun J, Ganter MT, Meybohm P, Hottenrott S, Zacharowski K, Raimann FJ, Rivas E, López-Baamonde M, et al. Visual Blood, Visualisation of Blood Gas Analysis in Virtual Reality, Leads to More Correct Diagnoses: A Computer-Based, Multicentre, Simulation Study. Bioengineering. 2023; 10(3):340. https://doi.org/10.3390/bioengineering10030340
Chicago/Turabian StyleBergauer, Lisa, Samira Akbas, Julia Braun, Michael T. Ganter, Patrick Meybohm, Sebastian Hottenrott, Kai Zacharowski, Florian J. Raimann, Eva Rivas, Manuel López-Baamonde, and et al. 2023. "Visual Blood, Visualisation of Blood Gas Analysis in Virtual Reality, Leads to More Correct Diagnoses: A Computer-Based, Multicentre, Simulation Study" Bioengineering 10, no. 3: 340. https://doi.org/10.3390/bioengineering10030340
APA StyleBergauer, L., Akbas, S., Braun, J., Ganter, M. T., Meybohm, P., Hottenrott, S., Zacharowski, K., Raimann, F. J., Rivas, E., López-Baamonde, M., Spahn, D. R., Noethiger, C. B., Tscholl, D. W., & Roche, T. R. (2023). Visual Blood, Visualisation of Blood Gas Analysis in Virtual Reality, Leads to More Correct Diagnoses: A Computer-Based, Multicentre, Simulation Study. Bioengineering, 10(3), 340. https://doi.org/10.3390/bioengineering10030340










