Treatment of Lumbar Degenerative Disease with a Novel Interlaminar Screw Elastic Spacer Technique: A Finite Element Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Development and Validation of Intact Lumbar FE Model
2.2. Development of Surgical Lumbar FE Model
2.3. Simulation Analysis
3. Results
3.1. Validation of the Intact Lumbar FE Model
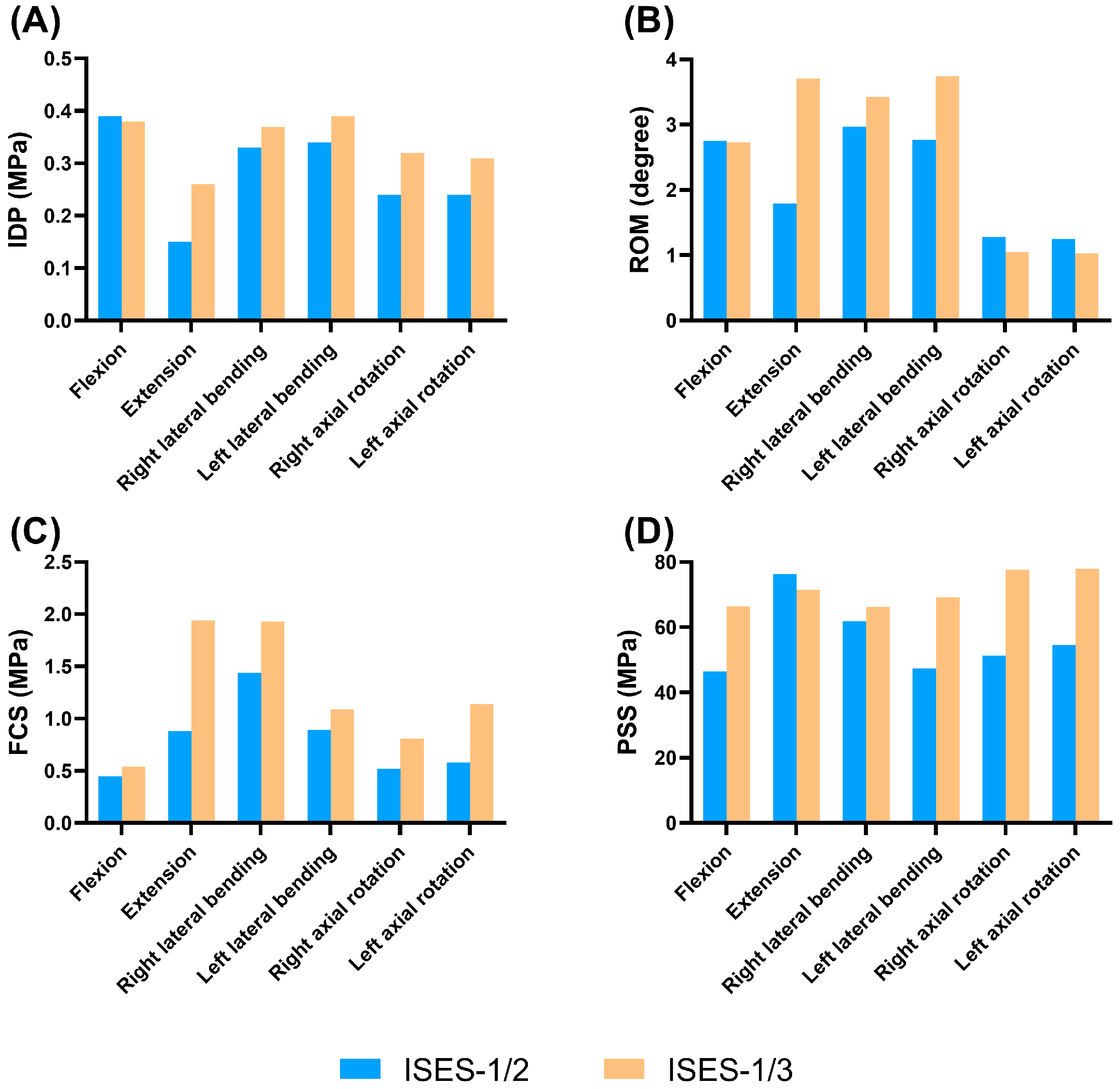
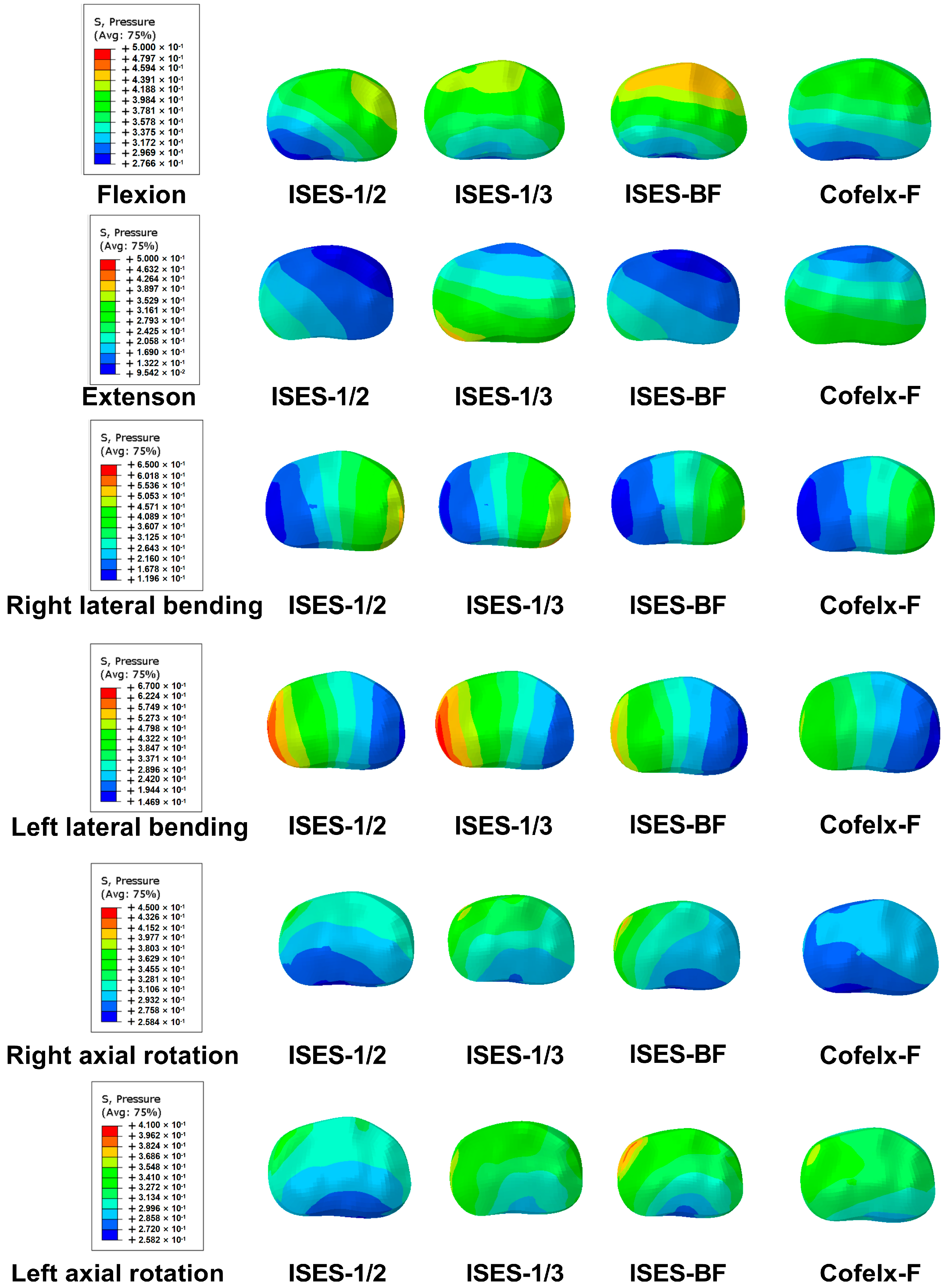
3.2. The Insertion Point of ISES Technique
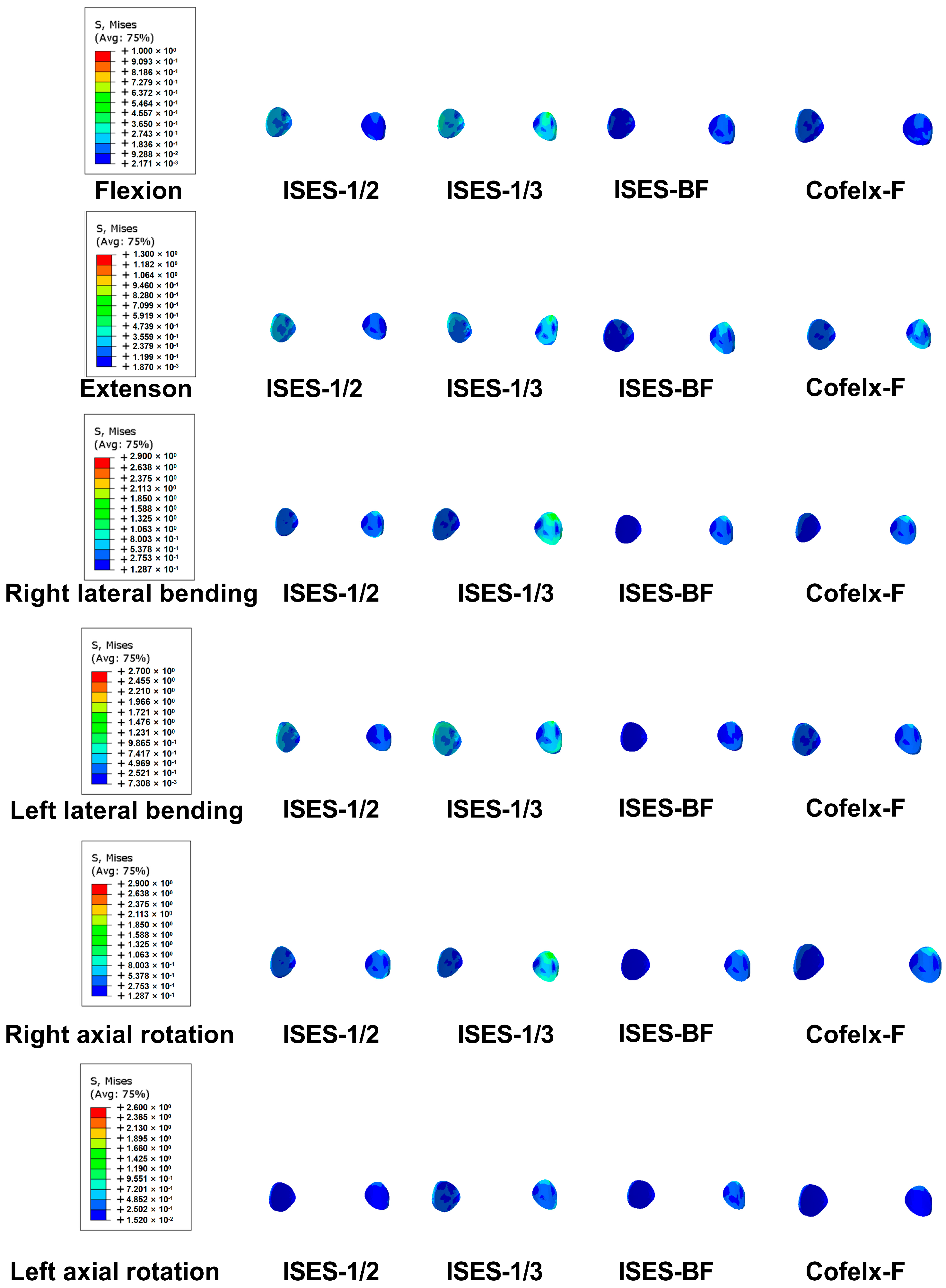
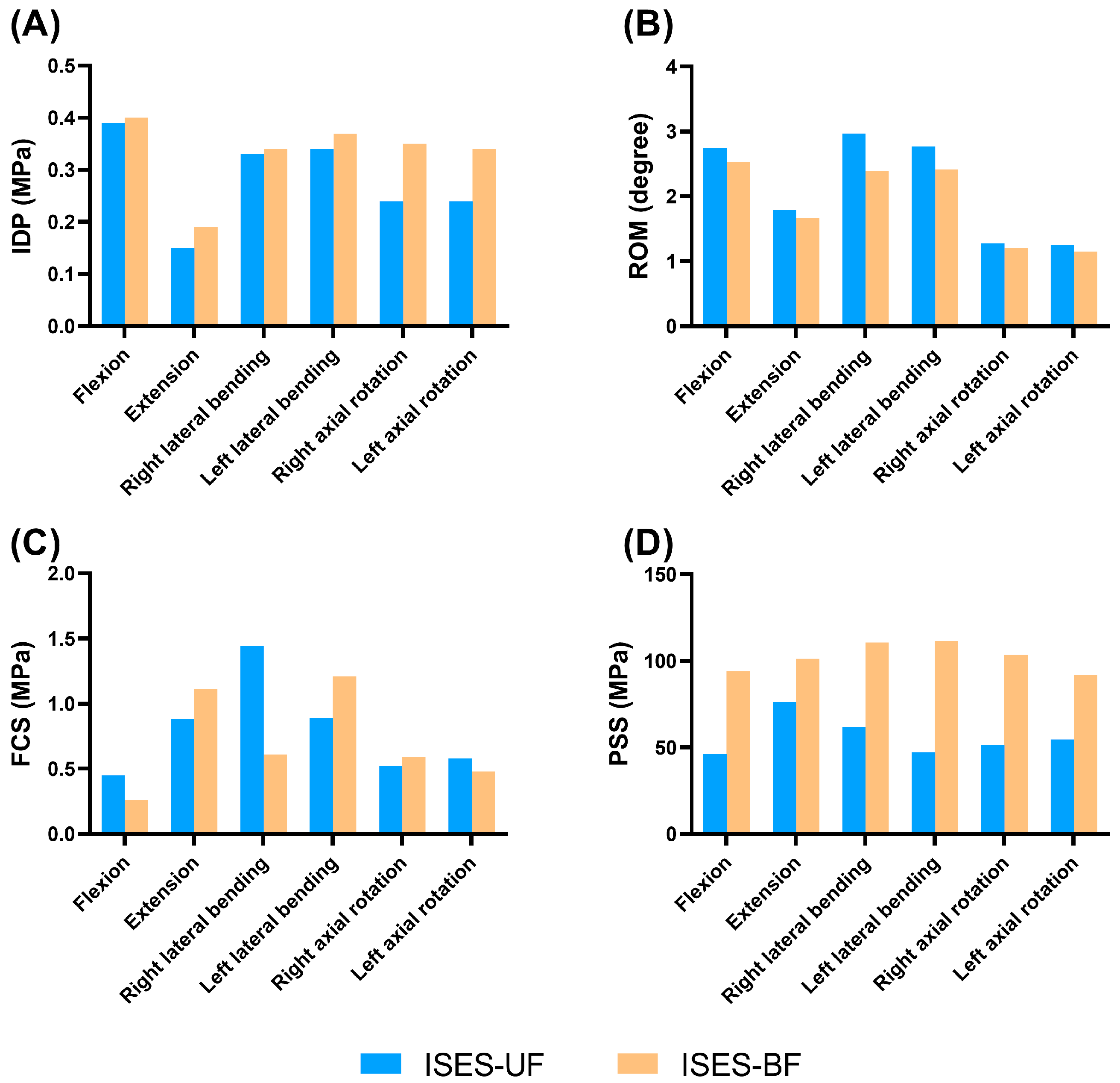
3.3. Feasibility Analysis of the Unilateral Fixation in the ISES Technique
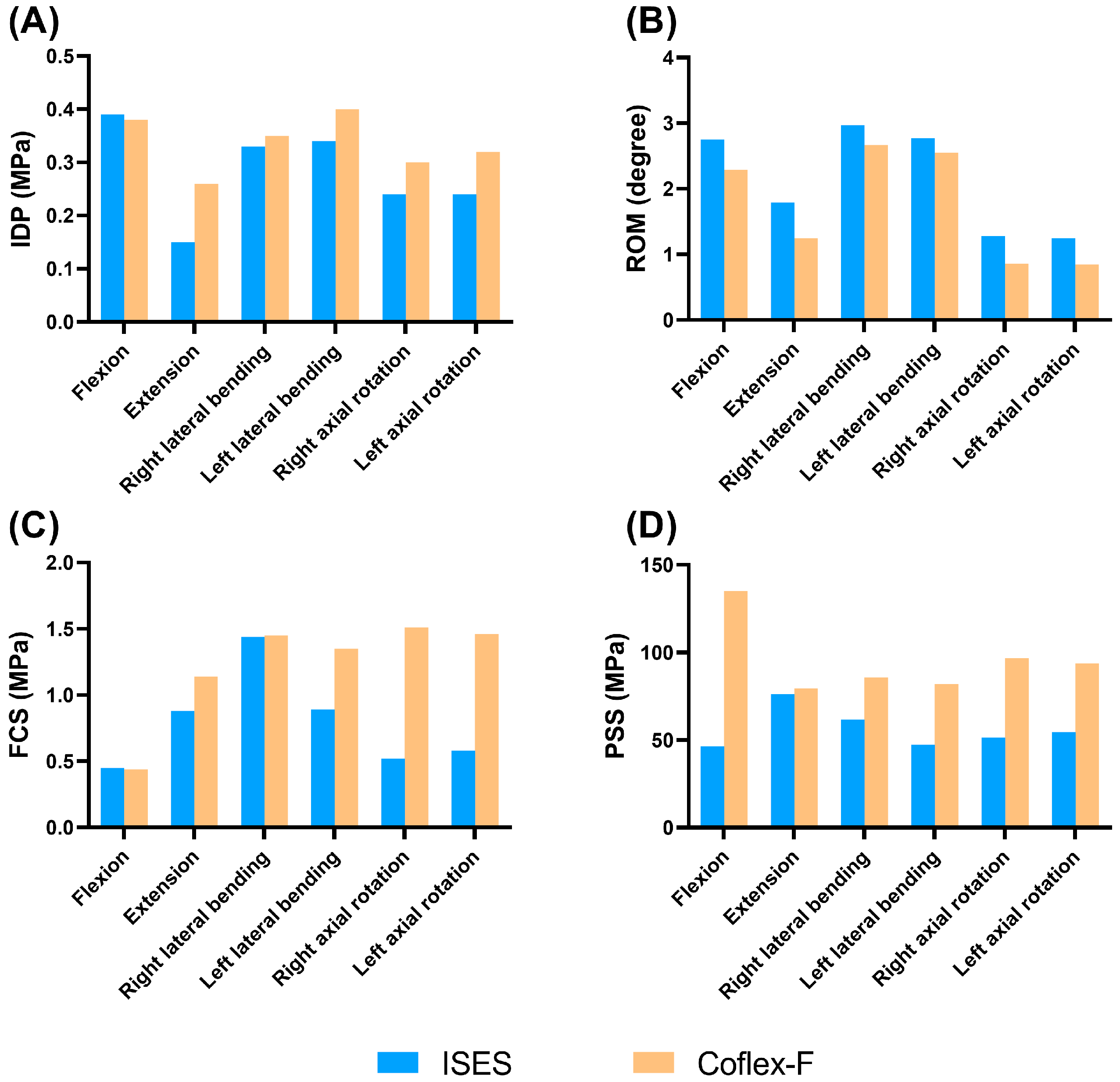
3.4. The Feasibility of ISES Technique
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fatoye, F.; Gebrye, T.; Odeyemi, I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol. Int. 2019, 39, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Bento, T.; Genebra, C.; Maciel, N.; Cornelio, G.; Simeão, S.; Vitta, A. Low back pain and some associated factors: Is there any difference between genders? Braz. J. Phys. Ther. 2020, 24, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Raikar, S.; Patil, A.; Pandey, D.; Kumar, S. Inter Spinal Fixation and Stabilization Device for Lumbar Radiculopathy and Back Pain. Cureus 2021, 13, e19956. [Google Scholar] [CrossRef] [PubMed]
- Faulkner, J.; Khalifeh, K.; Hara, J.; Ozgur, B. Interspinous Process (ISP) Devices in Comparison to the Use of Traditional Posterior Spinal Instrumentation. Cureus 2021, 13, e13886. [Google Scholar] [CrossRef]
- Wei, H.; Tang, H.; Zhang, T.; Chen, H.; Dong, C. Preliminary efficacy of inter-spinal distraction fusion which is a new technique for lumbar disc herniation. Int. Orthop. 2019, 43, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Li, H.; Chen, L.; Xiang, J.; Li, C.; Weng, J.; Tian, N. Complications and radiographic changes after implantation of interspinous process devices: Average eight-year follow-up. BMC Musculoskelet. Disord. 2023, 24, 667. [Google Scholar] [CrossRef]
- Trautwein, F.; Lowery, G.; Wharton, N.; Hipp, J.; Chomiak, R. Determination of the in vivo posterior loading environment of the Coflex interlaminar-interspinous implant. Spine J. 2010, 10, 244–251. [Google Scholar] [CrossRef]
- Magerl, F. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin. Orthop. Relat. Res. 1984, 125–141. [Google Scholar] [CrossRef]
- Mulholland, R.; Sengupta, D. Rationale, principles and experimental evaluation of the concept of soft stabilization. Eur. Spine J. 2002, S198–S205. [Google Scholar] [CrossRef]
- Jia, L.; Yu, Y.; Khan, K.; Li, F.; Zhu, R.; Zeng, Z.; Cheng, L. Superior Facet Joint Violations during Single Level Minimally Invasive Transforaminal Lumbar Interbody Fusion: A Preliminary Retrospective Clinical Study. BioMed Res. Int. 2018, 2018, 6152769. [Google Scholar] [CrossRef]
- Oh, H.; Seo, H. The Relationship between Adjacent Segment Pathology and Facet Joint Violation by Pedicle Screw after Posterior Lumbar Instrumentation Surgery. J. Clin. Med. 2021, 10, 2911. [Google Scholar] [CrossRef]
- Singhatanadgige, W.; Songthong, K.; Pholprajug, P.; Yingsakmongkol, W.; Kotheeranurak, V.; Limthongkul, W. Trajectory of Lumbar Translaminar Facet Screw Under Navigation: A Cadaveric Study. Glob. Spine J. 2022, 12, 765–771. [Google Scholar] [CrossRef]
- Lu, J.; Ebraheim, N.; Yeasting, R. Translaminar facet screw placement: An anatomic study. Am. J. Orthop. 1998, 27, 550–555. [Google Scholar] [PubMed]
- Hu, Y.; Zhu, B.; Yuan, Z.; Dong, W.; Sun, X.; Xu, J.; Chen, X. Anatomic study of the lumbar lamina for safe and effective placement of lumbar translaminar facet screws. J. Int. Med. Res. 2019, 47, 5082–5093. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Kang, K.; Son, J.; Lee, C.; Chang, B.; Yeom, J. The influence of facet joint orientation and tropism on the stress at the adjacent segment after lumbar fusion surgery: A biomechanical analysis. Spine J. 2015, 15, 1841–1847. [Google Scholar] [CrossRef] [PubMed]
- Dreischarf, M.; Zander, T.; Shirazi-Adl, A.; Puttlitz, C.; Adam, C.; Chen, C.; Goel, V.; Kiapour, A.; Kim, Y.; Labus, K.; et al. Comparison of eight published static finite element models of the intact lumbar spine: Predictive power of models improves when combined together. J. Biomech. 2014, 47, 1757–1766. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.B.; Nie, M.D.; Zhang, N.Z.; Liu, S.; Yuan, J.B.; Lin, X.M.; Cheng, C.K.; Shi, Z.C.; Mao, N.F. Biomechanical evaluation of a short-rod technique for lumbar fixation surgery. Front. Bioeng. Biotechnol. 2022, 10, 959210. [Google Scholar] [CrossRef]
- Goto, K.; Tajima, N.; Chosa, E.; Totoribe, K.; Kuroki, H.; Arizumi, Y.; Arai, T. Mechanical analysis of the lumbar vertebrae in a three-dimensional finite element method model in which intradiscal pressure in the nucleus pulposus was used to establish the model. J. Orthop. Sci. 2002, 7, 243–246. [Google Scholar] [CrossRef]
- Brinckmann, P.; Grootenboer, H. Change of disc height, radial disc bulge, and intradiscal pressure from discectomy. An in vitro investigation on human lumbar discs. Spine 1991, 16, 641–646. [Google Scholar] [CrossRef]
- Goel, V.; Goyal, S.; Clark, C.; Nishiyama, K.; Nye, T. Kinematics of the whole lumbar spine. Effect of discectomy. Spine 1985, 10, 543–554. [Google Scholar] [CrossRef]
- Karahalios, D.; Kaibara, T.; Porter, R.; Kakarla, U.; Reyes, P.; Baaj, A.; Yaqoobi, A.; Crawford, N. Biomechanics of a lumbar interspinous anchor with anterior lumbar interbody fusion. J. Neurosurg. Spine 2010, 12, 372–380. [Google Scholar] [CrossRef]
- Yamamoto, I.; Panjabi, M.; Crisco, T.; Oxland, T. Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine 1989, 14, 1256–1260. [Google Scholar] [CrossRef] [PubMed]
- Lo, C.; Tsai, K.; Chen, S.; Zhong, Z.; Hung, C. Biomechanical effect after Coflex and Coflex rivet implantation for segmental instability at surgical and adjacent segments: A finite element analysis. Comput. Methods Biomech. Biomed. Eng. 2011, 14, 969–978. [Google Scholar] [CrossRef] [PubMed]
- Ballestra, E.; Battaglino, A.; Cotella, D.; Rossettini, G.; Sanchez-Romero, E.A.; Villafane, J.H. Do patients’ expectations influence conservative treatment in Chronic Low Back Pain? A Narrative Review. Retos-Nuevas Tend. Educ. Fis. Deport. Recreacion 2022, 46, 395–403. [Google Scholar] [CrossRef]
- Farì, G.; de Sire, A.; Fallea, C.; Albano, M.; Grossi, G.; Bettoni, E.; Di Paolo, S.; Agostini, F.; Bernetti, A.; Puntillo, F.; et al. Efficacy of Radiofrequency as Therapy and Diagnostic Support in the Management of Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Diagnostics 2022, 12, 600. [Google Scholar] [CrossRef] [PubMed]
- Giglio, M.; Farì, G.; Preziosa, A.; Corriero, A.; Grasso, S.; Varrassi, G.; Puntillo, F. Low Back Pain and Radiofrequency Denervation of Facet Joint: Beyond Pain Control-A Video Recording. Pain Ther. 2023, 12, 879–884. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, F.M.; Urrutia, G.; Arana, E.; Alvarez-Galovich, L.; Olabe, J. Re: Lumbar spine fusion for chronic low back pain due to degenerative disc disease. A systematic review. Spine 2013, 38, 1901. [Google Scholar] [CrossRef]
- Guan, J.; Liu, T.; Li, W.; Zhao, H.; Yang, K.; Li, C.; Feng, N.; Jiang, G.; Yang, Y.; Yu, X. Effects of posterior lumbar nonfusion surgery with isobar devices versus posterior lumbar interbody fusion surgery on clinical and radiological features in patients with lumbar degenerative diseases: A meta-analysis. J. Orthop. Surg. Res. 2022, 17, 116. [Google Scholar] [CrossRef]
- Fan, W.; Guo, L. The effect of non-fusion dynamic stabilization on biomechanical responses of the implanted lumbar spine during whole-body vibration. Comput. Methods Programs Biomed. 2020, 192, 105441. [Google Scholar] [CrossRef]
- Gomleksiz, C.; Sasani, M.; Oktenoglu, T.; Ozer, A.F. A short history of posterior dynamic stabilization. Adv. Orthop. 2012, 2012, 629698. [Google Scholar] [CrossRef]
- Anekstein, Y.; Floman, Y.; Smorgick, Y.; Rand, N.; Millgram, M.; Mirovsky, Y. Seven years follow-up for total lumbar facet joint replacement (TOPS) in the management of lumbar spinal stenosis and degenerative spondylolisthesis. Eur. Spine J. 2015, 24, 2306–2314. [Google Scholar] [CrossRef] [PubMed]
- Mo, Z.; Li, D.; Zhang, R.; Chang, M.; Yang, B.; Tang, S. Comparative effectiveness and safety of posterior lumbar interbody fusion, Coflex, Wallis, and X-stop for lumbar degenerative diseases: A systematic review and network meta-analysis. Clin. Neurol. Neurosurg. 2018, 172, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Spallone, A. Long term results of the use of a fusion-promoting, new generation interspinous processes device (IPD), Bacfuse (R): A monocentric prospective study. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 7561–7565. [Google Scholar]
- Epari, D.; Kandziora, F.; Duda, G. Stress shielding in box and cylinder cervical interbody fusion cage designs. Spine 2005, 30, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Sasso, R.; Best, N.; Potts, E. Percutaneous computer-assisted translaminar facet screw: An initial human cadaveric study. Spine J. 2005, 5, 515–519. [Google Scholar] [CrossRef]
- Chen, D.; Yao, C.; Song, Q.; Tang, B.; Liu, X.; Zhang, B.; Dai, M.; Nie, T.; Wan, Z. Unilateral versus Bilateral Pedicle Screw Fixation Combined with Transforaminal Lumbar Interbody Fusion for the Treatment of Low Lumbar Degenerative Disc Diseases: Analysis of Clinical and Radiographic Results. World Neurosurg. 2018, 115, e516–e522. [Google Scholar] [CrossRef]
- Ambati, D.; Wright, E.; Lehman, R.; Kang, D.; Wagner, S.; Dmitriev, A. Bilateral pedicle screw fixation provides superior biomechanical stability in transforaminal lumbar interbody fusion: A finite element study. Spine J. 2015, 15, 1812–1822. [Google Scholar] [CrossRef]
- Suk, K.; Lee, H.; Kim, N.; Ha, J. Unilateral versus bilateral pedicle screw fixation in lumbar spinal fusion. Spine 2000, 25, 1843–1847. [Google Scholar] [CrossRef]
- Lu, P.; Pan, T.; Dai, T.; Chen, G.; Shi, K. Is unilateral pedicle screw fixation superior than bilateral pedicle screw fixation for lumbar degenerative diseases: A meta-analysis. J. Orthop. Surg. Res. 2018, 13, 296. [Google Scholar] [CrossRef]
- Newell, E.; Driscoll, M. Investigation of physiological stress shielding within lumbar spinal tissue as a contributor to unilateral low back pain: A finite element study. Comput. Biol. Med. 2021, 133, 104351. [Google Scholar] [CrossRef]
- Ortega-Porcayo, L.; Leal-López, A.; Soriano-López, M.; Gutiérrez-Partida, C.; Ramírez-Barrios, L.; Soriano-Solis, S.; Rodríguez-García, M.; Soriano-Solis, H.; Soriano-Sánchez, J. Assessment of Paraspinal Muscle Atrophy Percentage after Minimally Invasive Transforaminal Lumbar Interbody Fusion and Unilateral Instrumentation Using a Novel Contralateral Intact Muscle-Controlled Model. Asian Spine J. 2018, 12, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.H.; King, A.I. Mechanism of facet load transmission as a hypothesis for low-back pain. Spine 1984, 9, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Liu, Z.; Li, C.; Luo, S.; Lai, Q.; Wang, S.; Zhang, B.; Wan, Z. Effect of facet-joint degeneration on the in vivo motion of the lower lumbar spine. J. Orthop. Surg. Res. 2020, 15, 340. [Google Scholar] [CrossRef] [PubMed]
- Lewiecki, E.; Ortendahl, J.; Vanderpuye-Orgle, J.; Grauer, A.; Arellano, J.; Lemay, J.; Harmon, A.; Broder, M.; Singer, A. Healthcare Policy Changes in Osteoporosis Can Improve Outcomes and Reduce Costs in the United States. JBMR Plus 2019, 3, e10192. [Google Scholar] [CrossRef] [PubMed]
- Adami, G.; Fassio, A.; Gatti, D.; Viapiana, O.; Benini, C.; Danila, M.I.; Saag, K.G.; Rossini, M. Osteoporosis in 10 years time: A glimpse into the future of osteoporosis. Ther. Adv. Musculoskelet. Dis. 2022, 14, 1759720X221083541. [Google Scholar] [CrossRef] [PubMed]
- Sethi, A.; Lee, S.; Vaidya, R. Transforaminal lumbar interbody fusion using unilateral pedicle screws and a translaminar screw. Eur. Spine J. 2009, 18, 430–434. [Google Scholar] [CrossRef]
- Huang, P.; Wang, Y.; Xu, J.; Xiao, B.; Liu, J.; Che, L.; Mao, K. Minimally invasive unilateral pedicle screws and a translaminar facet screw fixation and interbody fusion for treatment of single-segment lower lumbar vertebral disease: Surgical technique and preliminary clinical results. J. Orthop. Surg. Res. 2017, 12, 117. [Google Scholar] [CrossRef]
- Alonso Pérez, J.; Martín Pérez, S.; Battaglino, A.; Villafañe, J.; Alonso-Sal, A.; Sánchez Romero, E. An Up-Date of the Muscle Strengthening Exercise Effectiveness in Postmenopausal Women with Osteoporosis: A Qualitative Systematic Review. J. Clin. Med. 2021, 10, 2229. [Google Scholar] [CrossRef]

| Components | Young’s Modulus (MPa) | Poisson’s Ratio | Cross-Sectional Area (mm2) | Type Element |
|---|---|---|---|---|
| Cortical bone | 12,000 | 0.3 | - | T3D8 |
| Cancellous bone | 100 | 0.2 | - | T3D8 |
| Posterior bone | 3500 | 0.25 | - | T3D4 |
| Endplate | 500 | 0.3 | - | T3D4 |
| Nucleus pulposus | 1 | 0.49 | - | T3D8 |
| Annulus fibrosus | 4.2 | 0.45 | - | T3D8 |
| Annulus fiber layers | 360–550 | - | 0.76 | T3D2 |
| ALL | 15.6–20 | 0.3 | 63.7 | T3D2 |
| PLL | 10–20 | 0.3 | 18 | T3D2 |
| LF | 13–19.5 | 0.3 | 40 | T3D2 |
| CL | 7.5–33 | 0.3 | 32 | T3D2 |
| ITL | 12.0–58.7 | 0.3 | 1.8 | T3D2 |
| ISL | 8.8–15 | 0.3 | 25.2 | T3D2 |
| SSL | 9.8–12 | 0.3 | 35.1 | T3D2 |
| Screw | 113,000 | 0.3 | - | T3D8 |
| The shell of elastic rod | 113,000 | 0.3 | - | T3D4 |
| The ‘cable’ structure | 47,000 | 0.3 | - | T3D4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Z.; Liu, S.; Nie, M.; Yuan, J.; Lin, X.; Chu, X.; Shi, Z. Treatment of Lumbar Degenerative Disease with a Novel Interlaminar Screw Elastic Spacer Technique: A Finite Element Analysis. Bioengineering 2023, 10, 1204. https://doi.org/10.3390/bioengineering10101204
Huang Z, Liu S, Nie M, Yuan J, Lin X, Chu X, Shi Z. Treatment of Lumbar Degenerative Disease with a Novel Interlaminar Screw Elastic Spacer Technique: A Finite Element Analysis. Bioengineering. 2023; 10(10):1204. https://doi.org/10.3390/bioengineering10101204
Chicago/Turabian StyleHuang, Zebin, Shu Liu, Maodan Nie, Jiabin Yuan, Xumiao Lin, Xuerong Chu, and Zhicai Shi. 2023. "Treatment of Lumbar Degenerative Disease with a Novel Interlaminar Screw Elastic Spacer Technique: A Finite Element Analysis" Bioengineering 10, no. 10: 1204. https://doi.org/10.3390/bioengineering10101204
APA StyleHuang, Z., Liu, S., Nie, M., Yuan, J., Lin, X., Chu, X., & Shi, Z. (2023). Treatment of Lumbar Degenerative Disease with a Novel Interlaminar Screw Elastic Spacer Technique: A Finite Element Analysis. Bioengineering, 10(10), 1204. https://doi.org/10.3390/bioengineering10101204







