Abstract
Several metal nanoparticles have been developed for medical application. While all have their benefits, gold nanoparticles (AuNPs) are ideal in cancer therapy and diagnosis as they are chemically inert and minimally toxic. Several studies have shown the potential of AuNPs in the therapeutic field, as photosensitizing agents in sonochemical and photothermal therapy and as drug delivery, as well as in diagnostics and theranostics. Although there is a significant number of reviews on the application of AuNPs in cancer medicine, there is no comprehensive review on their application both in therapy and diagnostics. Therefore, considering the high number of studies on AuNPs’ applications, this review summarizes data on the application of AuNPs in cancer therapy and diagnostics. In addition, we looked at the influence of AuNPs’ shape and size on their biological properties. We also present the potential use of hybrid materials based on AuNPs in sonochemical and photothermal therapy and the possibility of their use in diagnostics. Despite their potential, the use of AuNPs and derivatives in cancer medicine still has some limitations. In this review, we provide an overview of the biological, physicochemical, and legal constraints on using AuNPs in cancer medicine.
Keywords:
gold nanoparticles; cancer; diagnosis; therapy; drug delivery; theranostics; hybrid materials 1. Introduction
Cancer is one of the most global and widespread health problems, as it is the second leading cause of death globally [1,2]. However, conventional cancer treatments have severe drawbacks and often fail to provide satisfactory results [3,4,5,6,7,8,9,10]. After traditional cancer therapy, patients usually take a long time to recover from side effects [10,11,12,13,14,15]. Moreover, most methods are not highly effective against cancer cells, and cancer chemotherapy causes disorders in many body organs (heart, kidneys, bladder, nervous system, and lungs) [16,17,18,19].
In recent years, great interest has arisen in applying nanotechnology to diagnose and treat tumor diseases [20,21], mainly because nanotechnology can offer unique methods for the study and control of various biological and medical processes. Therefore, it provides high expectations of creating new techniques with a revolutionary impact on the diagnosis and treatment of cancer [22,23].
Currently, several varieties of nano-objects of biomedical significance are in use, including polymer nanoparticles, metal nanoparticles, liposomes, micelles, quantum dots, dendrimers, and nanoscale assemblies [24,25,26,27,28,29]. Among all of them, the use of nanoparticles offers more potential in different medical applications [30,31], as shown by their successful use as image-enhancing sensors, delivery agents, toxic agents (for example, for the destruction of cancer cells), and diagnostic agents [32,33].
In addition, the use of nanoparticles can enhance the effect of various treatments when used in combination with them [34,35,36]. Moreover, in clinical oncology, there is a new trend of transition from monotherapy towards combination therapy in the presence of valuable nanomaterials [37,38,39], allowing interactions between different types of treatment and leading to a much more potent therapeutic effect than the separate use of the corresponding monotherapies [40,41,42,43,44].
AuNPs have become promising agents for the therapy and diagnosis of diseases [45,46], as they can passively accumulate and retain in the tumor site because of increased permeability and retention (EPR) arising from leaking vascular network and ineffective lymphatic drainage of tumor tissue [47,48].
Further, while many reviews highlight different benefits of AuNPs in cancer medicine, our study presents the recent progress towards the therapeutic and diagnostic application of AuNPs and their derivatives in cancer medicine. However, with the biocompatibility and cytotoxicity of nanoparticles being more or less dependent on their shape and size, we also decided to add an overview of the impact of these two parameters on the applications of AuNPs.
Therefore, the present review is divided into seven sections. The impact of the shape and size of AuNPs on their cytotoxicity and biocompatibility is reviewed in Section 2, “Form and Size Dependence on the Biological Properties of Gold Nanoparticles”. The therapeutic application of AuNPs is highlighted in Section 3 Drug Delivery. In the drug delivery section, we review the use of AuNPs in peptide and nucleic acids’ delivery and the potential of hybrid gold-based materials for drug delivery. We continue the review on recent progress in using AuNPs as photosensitizing agents in Section 4. Photothermal therapy and in Section 5. Sonochemical therapy, we also highlight the efficacity of AuNPs in improving these therapeutic methods. In Section 6. Gold Nanoparticles as a Diagnostic Material, we describe the promising developments in the use of AuNPs in diagnosis and theranostics of oncological diseases. Finally, in Section 7. Current Major Restrictions on the Use of Gold Nanoparticles for Medical Purposes, we reviewed the current major restrictions on the use of gold nanoparticles for medical purposes including highlights of the main problems still to be resolved before the widespread use of AuNPs in cancer medicine.
For this review, electronic scientific databases such as PubMed, Science Direct, Web of Science, Scopus, and Medline were used to analyze studies on AuNPs and their application in cancer medicine using keywords such gold nanoparticles, cancer, drug delivery, cancer therapy, cancer treatment, and diagnostics. Data were sorted from 2010 to provide the latest and most current information, but, when there was a need for more clarification, ulterior data were also used.
2. Form and Size Dependence on the Biological Properties of Gold Nanoparticles
The application of gold nanoparticles (AuNPs) in anti-cancer therapy is influenced by many factors, as reviewed by Singh P. et al., 2018 [49]; among those factors are the preparation methods, the presence of stabilizing agents, surface charge, the presence of hydrophobic/hydrophilic groups on the surface, as well as the size and shape of the AuNPs. Currently, there are several studies on the preparation methods of AuNPs, including those with a modified surface by particular groups; so, in this review, we will not look at those different ways of preparing AuNPs, but will instead focus exclusively on the application of these gold nanoparticle-based materials products [49,50].
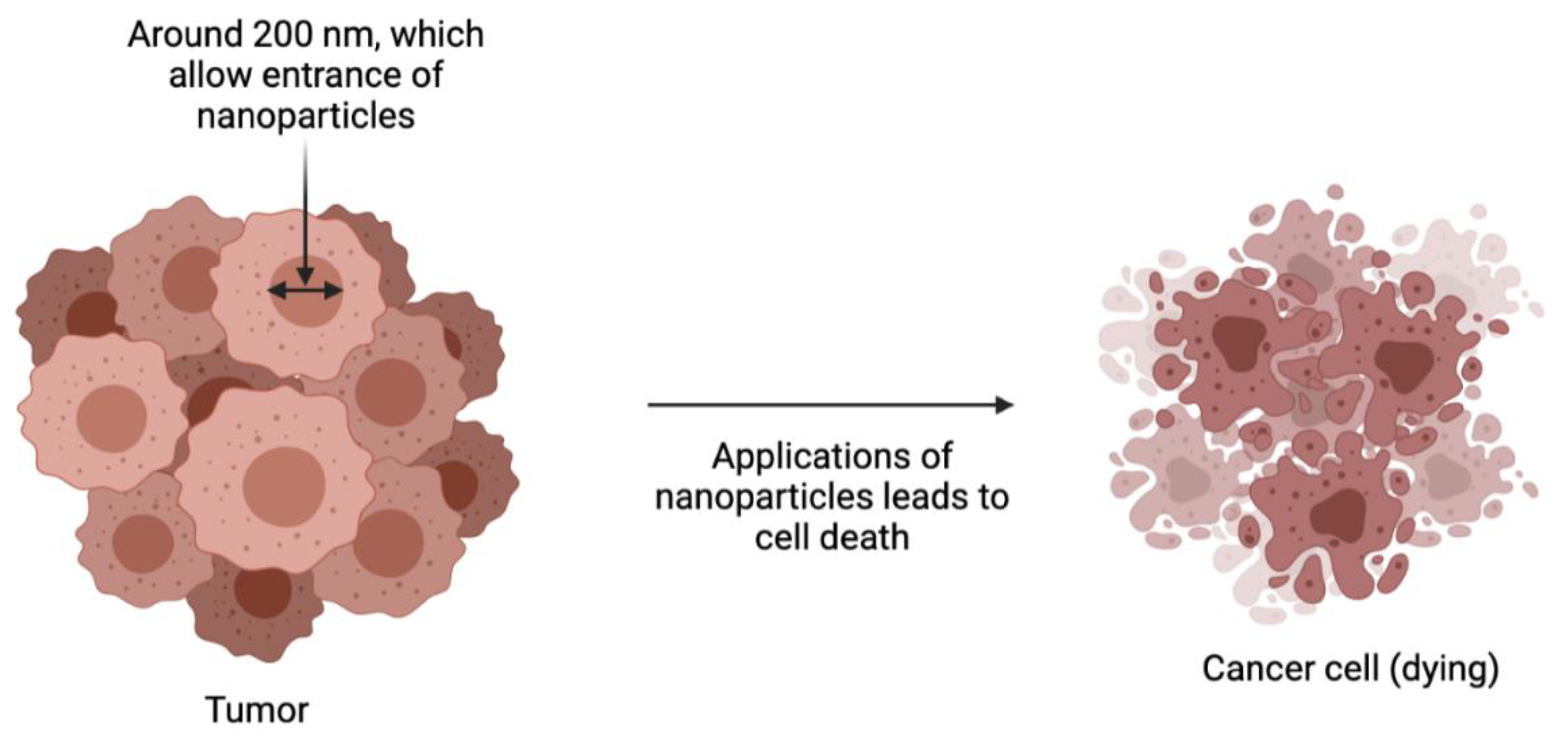
In recent years, studies have shown the impact of both the size and shape of AuNPs on their biological properties, especially their cytotoxicity, and owing to the EPR effect (enhanced permeability and retention effect), nanoparticles smaller than 200 nm can be used (Figure 1). However, particles smaller than 6 nm are quickly excreted by the kidneys, while for those in the region of 10–100 nm, their half-life increases with increasing size [50,51].
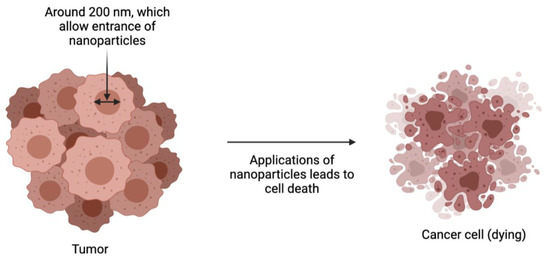
Figure 1.
Owing to the EPR effect (enhanced permeability and retention effect), nanoparticles up to 200 nm can enter and accumulate in the tumor cells, and cause tumor cell death (created with BioRender.com).
In addition, studies show that, with inflammation, the endothelial lining of the blood vessel wall is more permeable than in normal conditions, so particles of 10 to 200 nm in size can leave the bloodstream and accumulate inside the interstitial tissues.
Moreover, different organs accumulate particles of a particular shape; for example, the preferred localization of irregularly shaped nanoparticles is the spleen and the lungs for rod-shaped particles, but the exact mechanism of this preference is still unknown [52,53]. Finally, the impact of their shape is also closely related to their movement in the bloodstream.
From studies on the effect of size and shape on the biodistribution of AuNPs after intravenous administration, we note the following:
- (a)
- The size and shape strongly affect the kinetics of accumulation and excretion of AuNPs in filtering organs;
- (b)
- Spherical and star-shaped AuNPs showed the same percentage of accumulation, but others localize in the liver;
- (c)
- Only stellate (or star-shaped) AuNPs can accumulate in the lungs;
- (d)
- Changes in geometry did not improve the passage of the blood–brain barrier. Overall, the study is a reliable starting point for the synthesis and functionalization of potential candidates for theranostic purposes in many research areas [54].
In addition to the accumulation and distribution of gold nanoparticles within the body, their cytotoxicity is assessed depending on their shape and size. Studies show that cytotoxicity also depends on these parameters. For example, the toxicity tests on three different forms of chitosan-coated gold nanoparticles (nanospheres, nanostars, and nanorods) showed that, even at low concentrations, like 8 μM Au, nanorods exhibited cytotoxicity [55]. Moreover, the IC50 value was 127.1 μM Au for nanospheres against HepG2 cells, 81.8 μM Au for nanostars, and 22.7 μM Au for nanorods, thus showing that nanorods are the most cytotoxic, followed by nanostars, and nanospheres—the least cytotoxic to HepG2 cells [56].
In addition, analysis on cellular uptake of nanoparticles showed that it is also dependent on the shape, with a study of the absorption of AuNPs (5 μM Au—a non-toxic concentration in four types of cancer cells) showing the highest absorption for nanospheres (58.0%), followed by nanorods (52.7%) and nanostars (41.5%). Therefore, not only cytotoxicity (nanorods > nanostars > nanospheres), but also the level of cellular absorption (nanospheres > nanorods > nanostars) depend on the shape of the particles [57].
The cytotoxicity of different shapes of AuNPs (rods, stars, and spheres) have also been analyzed on human cells using in vitro model cells—hFOB 1.19, 143B, MG63, and hTERT-HPNE. The results showed that the IC50 values were the lowest in 143B cell compared with hFOB 1.19 and MG63 cell lines. AuNPs induced apoptosis in human osteosarcoma in both 143B and MG63, and AuNPs of all types penetrated the cell membrane and caused ultrastructural changes. AuNPs-nanostars were more cytotoxic to 143B, while hFOB 1.19 cells were more resistant to AuNPs-nanostars (2.5 and 5 μg/mL). After exposure to a low concentration of AuNPs-nanostars (0.3 and 0.6 μg/mL), hFOB 1.19 and MG63 cells had a similar survival rate. In the MTT test, AuNPs significantly reduced the viability of hFOB 1.19, MG63, and 143B cells. The neutral-red uptake analysis (NR analysis) showed that hFOB 1.19 are resistant to the cytotoxic effect of AuNPs-rods at concentrations of 0.3 to 2.5 μg/mL, MG63 to AuNPs-rods at the concentration of 0.3 to 0.6 μg/mL, and 143B cells to AuNPs-rods at the concentration of 0.3–1.2 µg/mL. The AuNPs-spheres were the least cytotoxic compared with the other nanoparticles. MTT tests showed that AuNPs-spheres did not reduce the viability of hFOB1.19 and MG-63 cells. In contrast, the NR assay showed no statistically significant effect of AuNPs-spheres on the viability of hFOB1.19, MG63, and 143B cells over the analyzed concentration range. Thus, AuNPs-nanostars were the most cytotoxic, and thus have the highest anti-cancer potential, while AuNPs-spheres have the lowest anti-cancer potential [58].
An analysis of the catalytic activity of AuNPs showed that it is dependent on their size, as Suchomel P. et al. found that decreasing the size causes an increase in the catalytic activity of AuNPs obtained by the reduction of HAuCl4 with maltose in the presence of Tween 80 [59].
Other properties of AuNPs have also been studied, such as their biological properties based on in vivo and in vitro results. It has been shown that their physicochemical properties can be explained by their hydrodynamic diameter and their zeta potential [60]. However, in an analysis of multidimensional set, no direct relationship between physicochemical parameters and biological properties was established [61,62], which is most likely because of a large number of parameters that are difficult to take into account and makes it difficult to predict the biological effect of AuNPs in the case of a simultaneous change in several physicochemical properties [63,64].
The results of several studies show that the shape, size, surface charge, and presence of special groups have an impact on the potential and effectivity of AuNPs, so it should be recommended that nano-objects are specially developed for the intended application taking into account all its subtleties, as it would increase the efficiency of AuNPs in therapy or diagnosis of the disease.
3. Drug Delivery
The ability to customize AuNPs makes it possible to create particles of various core diameters with complete control over size dispersion [65]. Owing to the high surface area to volume ratio, dense loading of ligands with multiple functions involved in therapy, diagnosis, and targeting can be anchored to the surface of AuNPs [66]. There are two main types of anchoring of drugs to the surface of nanoparticles:
- Conjugation (attachment to the surface of a nanoparticle through linker molecules);
- Sorption (fixation on the surface due to non-covalent bonds and the developed surface of nanoparticles).
Hostetler et al. demonstrated the covalent conjugation of almost 100 molecules with one AuNP with a core diameter of 2 nm [67]. In addition, the delicate surface treatment of AuNPs with different multifunctional monolayers provides ideal functional diversity, making them a versatile platform for drug delivery [68].
The most efficient cellular uptake occurs for particles ranging in size from 25 to 50 nm. In addition, a study on in vivo uptake of AuNPs and their passive accumulation in the tumor showed that the penetration of nanoparticles through the interstitial space of a tumor is highly size-dependent. While the larger AuNPs accumulate near the vasculature, the smaller AuNPs rapidly diffuse from the vasculature and are distributed throughout the tumor matrix [69].
There are two main types of targeted drug delivery:
- Passive transfer (delivery is carried out in areas of increased permeability, which cancer cells often have);
- Active transfer (accumulation in the tumor due to the binding of a specific ligand and a damage marker).
A critical factor in drug delivery is the EPR effect, which occurs because of the extravasation of macromolecules or nanoparticles through the tumor’s blood vessels. Nanoprobe delivery based on the EPR effect is also helpful for tumor imaging agents using fluorescent or radio nuclei in nanoprobes [70].
Several researchers have confirmed that extravasation through EPR does not have a reverse mechanism, so an object penetrating inside is delayed for a long time [45,46]. Currently, there are some mechanisms aimed at improving the EPR effect and the treatment’s effectiveness; one of them is a combination of pharmacological and physical methods of treatment [48,71].
3.1. Peptide Delivery
Given the potential of peptides as drugs, nanoparticles of different sizes from 1 to 100 nm have been used to deliver peptides into cells to improve their therapeutic effect. Pérez-Ortiz M. et al. showed that AuNPs synthesized by reducing HAuCl4 with sodium citrate could serve as a basis for creating a glucagon-like peptide from conjugates, which can be used as a drug. This method helps increase the peptide half-life and drug stability. They found that the complex of nanoparticles and peptides had no effect on the integrity of tight junctions and had no adverse impact on the metabolic activity (viability) of intestinal epithelial cells after 2 and 20 months. Their study also showed that the modification with polyethylene glycol improves biocompatibility with biological barriers and increases the efficiency of the conjugate absorption, which indicates that AuNPs are highly promising for delivering peptide drugs [72]. Other researchers have also shown the potential of AuNPs in peptide delivery, as they synthesized AuNPs by reduction with tannin and sodium citrate, after which they functionalized PEG together with peptides PFV (CALNNPFVYLI) or R8 (CALRRRRRRRR) [73].
Data on cellular uptake at 4 °C show that nanoparticles enter cells through energy-dependent endocytosis, which has been studied on nanoparticles of 10 to 100 nm in size [74]. In addition, nanoparticles with peptides can inhibit macropinocytosis by blocking the sodium–proton exchange. Most nanoparticles with peptides are absorbed by cells in the pathways of clathrin-mediated endocytosis and micropinocytosis, and it was revealed that they had increased cellular uptake in comparison with conventional nanoparticles, which should undoubtedly be used in the design of various delivery systems for the treatment of multiple diseases [75,76,77].
Kapur A. et al. used the complexes of peptides with gold nanoparticles and nanorods for direct translocation across the plasma membrane [78], showing that those peptides could help avoid the limitations currently encountered during the delivery of nano-objects into tumor cells. In addition, the complex of AuNPs and peptides can also be used as a biosensor inside the cell, thanks to the high electronic contrast provided by AuNPs [79,80].
3.2. Nucleic Acid Delivery
Another class of compounds that are promising in treating various diseases, including cancer diseases, is nucleic acids. To attach oligonucleotides to gold nanoparticles, covalent functionalization with thiol-modified oligonucleotides is used [81,82]. A layer of nucleic acids on the surface of gold nanoparticles inhibits the action of nucleases, and thus preserves the payload. The non-covalent interaction of nucleic acids and gold nanoparticles is used to deliver unmodified nucleic acids useful for gene therapy [83,84]. For the successful application of this method, it is important to consider several factors, such as carrier/nucleotide size, surface charge, and surface hydrophobicity [85].
Kunoh T. et al. showed in their green biosynthesis of AuNPs using Leptothrix cells (iron-oxidizing bacteria) that nucleic acids bind to ready-made gold nanoparticles and participate in the formation of nanoparticles, acting as a reducing agent and a coating agent [86]. Furthermore, they showed that fine-grained spherical AuNPs could be formed owing to the oxidation of the guanine fragment without the need for any reducing agents or physical modifications, which makes this material very promising for medical applications [87,88].
AuNPs can also be obtained by reduction with chitosan combined with siRNA STAT3 on its surface (sense sequence: 5′AAAUGAAGGUGGUGGAGAAUU3′; antisense sequence: 5′UUCUCCACCACCUUCAUUUUU3′) and imatinib for one hour [87]. Intratumoral delivery of siRNA STAT3 and imatinib with AuNPs showed a decrease in tumor weight by 45% and in intramuscular load by 30% [88]. In vitro studies have demonstrated that co-delivery of the two drugs (siRNA STAT3 and imatinib) significantly reduces cell viability compared with siRNA STAT3 or imatinib alone. In the absence of a nucleotide portion, there was no effect on tumors. Therefore, the created complex hybrid material shows high efficiency in suppressing melanoma cancer [89].
Several researchers have developed AuNPs by reducing sodium citrate and functionalizing them through thiol modifications at the 5′-end of anti-221 nucleotides, miR-221 inhibitor, and AS1411 aptamer, a guanine-rich oligonucleotide that can form stable G-quadruplex structures for specific targeting of nucleolin, which is overexpressed on the surface of leukemic cells [90,91,92]. Such AuNPs were modified with PEG and loaded with doxorubicin. This hybrid material counteracts miR-221/p-glycoprotein-dependent multidrug resistance in leukemia and sensitizes primary blasts in leukemic patients with a chemoresistant relapse to doxorubicin [93,94,95,96]. This method for oligonucleotide drug delivery in combination with doxorubicin is a unique antileukemic strategy that induces apoptosis of cancer cells and leads to the restoration of the expression of tumor suppressors p27kip1 and p15ink4b, as well as to a miR-221-mediated decrease in the expression of P-glycoprotein [97].
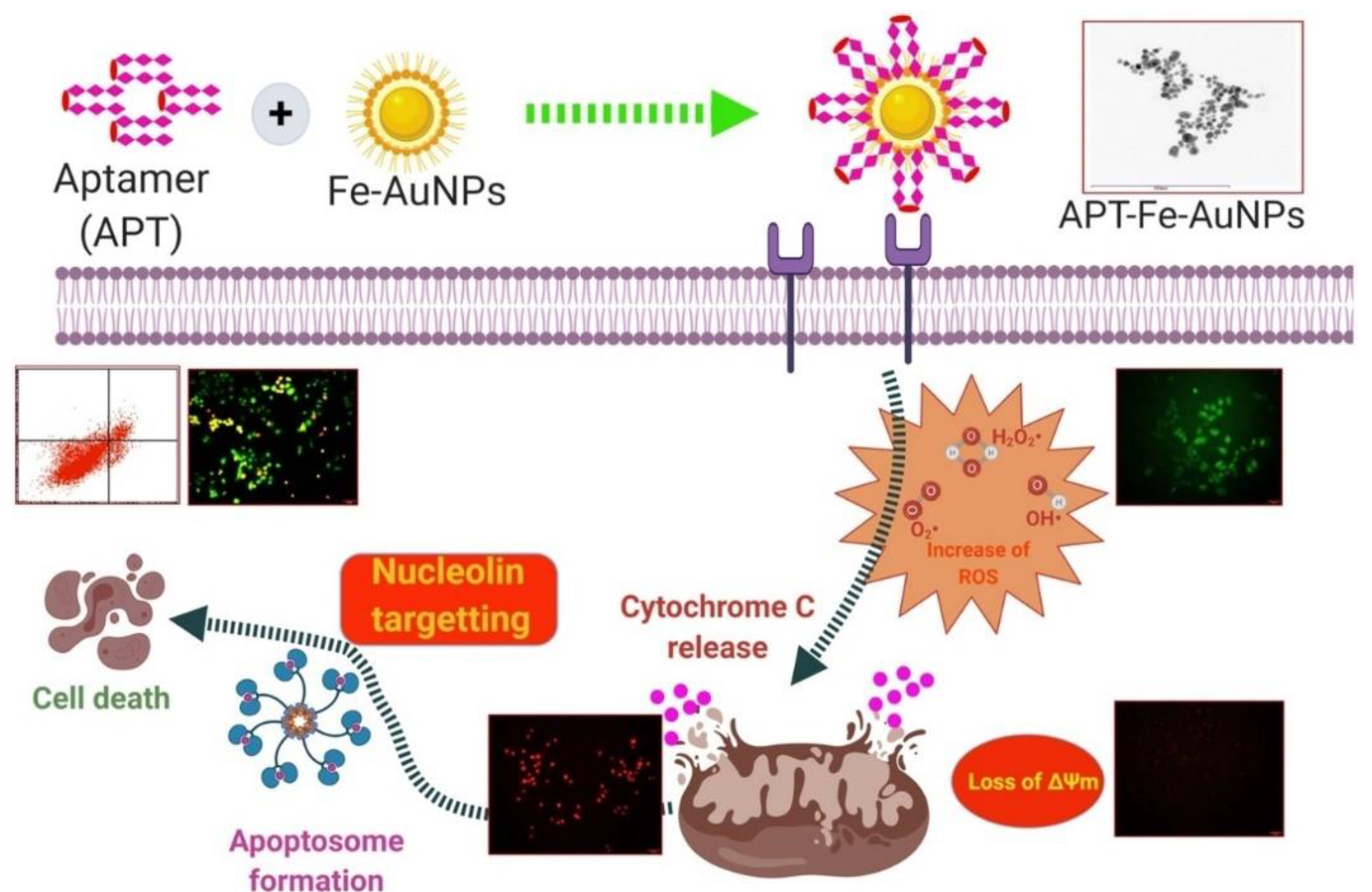
In a recent study, Saravanakumar K. et al. used AuNPs of 50 nm in size and spherical and hexagonal shape, obtained by incubation with the protein extract of the fungi Trichoderma harzianum. They modified them using the APT aptamer (AS1411). Cytotoxicity analysis showed that the modification with APT aptamer increased cytotoxicity in lung cancer and human brain tumor cell lines compared with normal cells NIH3T3 because of a lower expression of nucleolin in the plasma membrane of normal cells NIH3T3 and higher expression of nucleolin in cancer cells. In addition, the crude protein content of Trichoderma was also associated with the toxicity of AuNPs to malignant cells. In addition, their results show that, during the action of AuNPs on cells, an excessive amount of ROS is released, causing damage to the nucleus and cell death and that fungal crude protein-coated gold nanoparticles functionalized with aptamer (APT-FE-AuNPs) bind to nucleolin in the plasma membrane of cancer cells and trigger apoptosis and necrosis (Figure 2) [98].
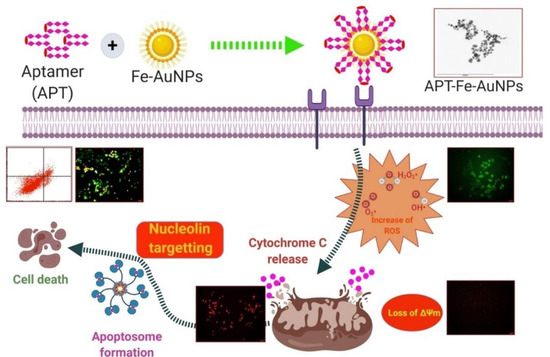
Figure 2.
Schematic illustration of nucleolin targeted delivery of APT-FE-AuNPs to improve cytotoxicity in cancer cells [98].
AuNPs have also been used in combination with biopolymers, capable of being incorporated into the human body and metabolized to deliver nucleic acids. A recent study shows the process of assembling a hybrid material based on AuNPs by reducing HAuCl4 in the presence of chitosan, which acts as a capping agent, thus obtaining chitosan-coated AuNPs of 20 nm on average. Those nanoparticles were used to deliver siRNA. The results show that, in addition to the high stability of the obtained particles in biological systems, there is increased efficiency in releasing the therapeutic agent and high absorption by cells owing to endocytosis. Cytotoxicity relative to lung epithelial cells H1299-eGFP, as well as suppression of biomarker signals, indicated a high efficiency of siRNA delivery using the developed system (Figure 3) [99].
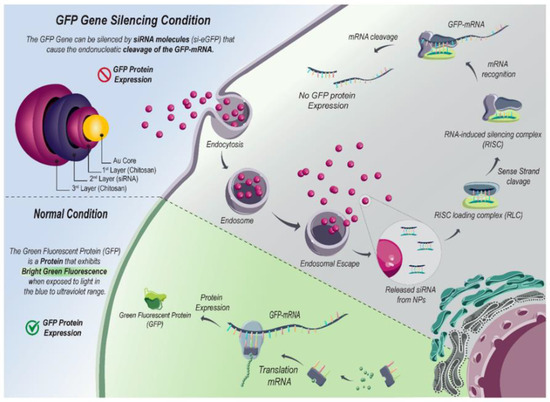
Figure 3.
Schematic representation of the chitosan-coated AuNPs for siRNA delivery [99].
3.3. Hybrid Gold-Based Materials for Drug Delivery
Recently, hybrid materials based on AuNPs have become more promising for anti-cancer drug delivery, as an example of the complex of AuNPs with gallauseite nanotubes. This complex is prepared with biological methods, giving it a tremendous advantage for biomedical purposes [100,101,102,103].
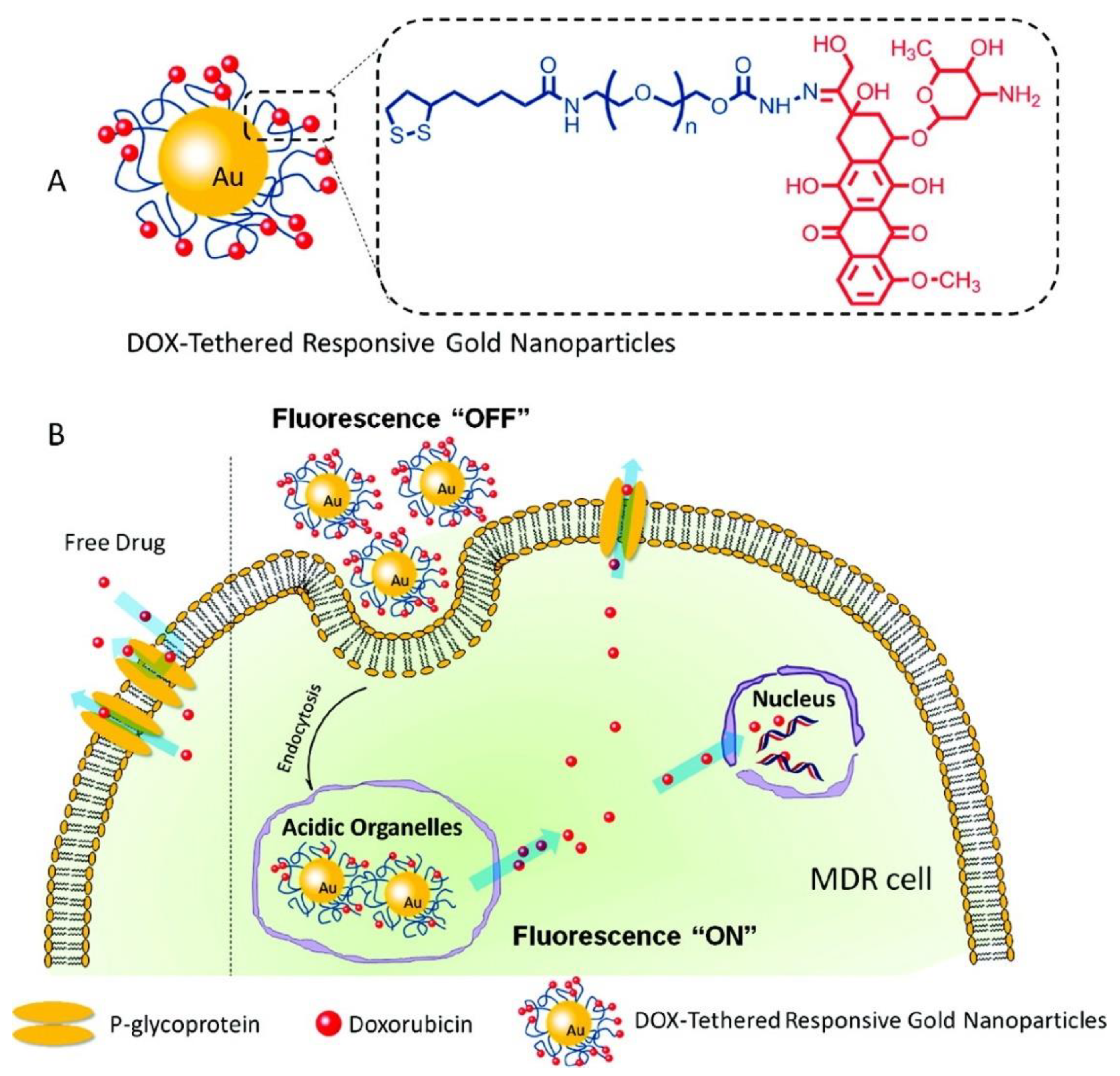
Several methods can be used to attach AuNPs to a drug-using particular group, such as a pH-sensitive linker. Such a type of attachment of the drug to AuNPs allows the intracellular release of the drug from the nanoparticle to be triggered when they enter the acidic organelles (Figure 4) [104]. AuNPs, developed through a modification with polyethylene glycol and conjugated with doxorubicin using a hydrazine linker, were used to release a model drug (doxorubicin). The drug release was found to be dependent on the pH of the medium, as at pH 7.4, after incubation for 48 h, only 20% of the drug was released, and at pH 5, more than 80% was released.
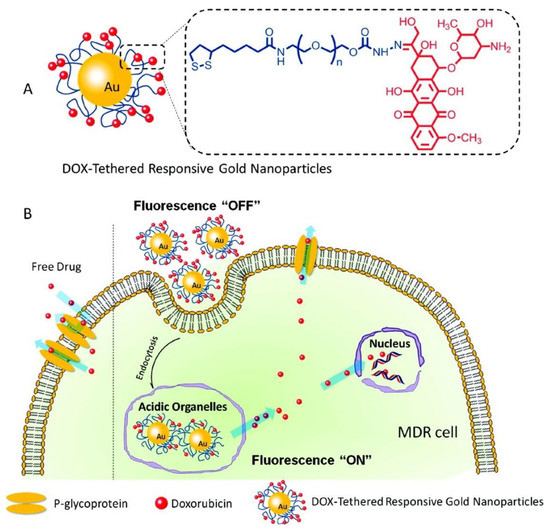
Figure 4.
(A) Schematic illustration of doxorubicin (DOX)-tethered responsive gold nanoparticles and (B) their cooperation between enhanced doxorubicin cellular entry and a responsive intracellular release of doxorubicin into the cells to overcome drug resistance [104].
The attachment of doxorubicin to the surface of AuNPs protects it from P-gp efflux, thus increasing the retention of doxorubicin in cells [105,106], and that combined with high drug loading capacity and effective drug release under pH control combined with the advantage of multimodal visualization inside cells show the high potential of this delivery system in medicine [107]. Furthermore, drug delivery systems, by binding cytotoxic drugs to the surface of AuNPs through an acid–labile bond, have demonstrated their potential to inhibit the growth of cancer cells (for instance, MCF-7/ADR) owing to the high efficiency of cellular uptake through endocytosis and subsequent acid-dependent release in cells [108].
Our literature analysis also showed another hybrid system—a complex of AuNPs with dendrimer G5-FD conjugated with doxorubicin [109,110,111]. Further, it has been demonstrated that such a complex has a therapeutic effect and provides targeted inhibition of FAR-expressing cancer cells [112,113].
AuNPs (20–25 nm) modified with PEG and carboxylated dendrimer PAMAM G4 have also been used to deliver doxorubicin [114]. While nanoparticles have shown high stability over a wide pH range [115,116], Wang F. et al. in their work established a relationship between drug release at different pH, with more than 50% of doxorubicin released in an acidic medium (pH 4), thus suggesting a high efficiency against cancer cells [104].
Apart from doxorubicin, the drug delivery ability of AuNP-based hybrid materials was tested by loading it with the model drug, curcumin; it was found that, at pH 5.5, about 95% of curcumin was released within 48 h, and at pH 7.4, only 10% was released. Thus, confirming that hybrid nanoparticles have a pH-dependent drug delivery process and are more efficient in the acidic medium [117,118,119,120,121].
Drug release from nanosystems is controlled; first, it enters the cytoplasm, accumulates in the lysosomes, and then, after 24 h, the drug is released from the lysosomes going into the cell nucleus [45]. Thus, the new multifunctional nanosystem based on AuNPs may provide a unique platform for intracellularly releasing an anti-cancer drug at tumor sites.
AuNPs coated with a platinum layer and modified with the cRGD peptide of various sizes were loaded with doxorubicin. Yang Q. et al. showed in their in vivo experiments the effectiveness of the complex AuNPs-DOX comparison with free doxorubicin [122]. The antitumor properties of the complex were additionally confirmed by immunohistochemical/immunofluorescence analysis of tumor tissues during various treatments. Furthermore, the complex showed high absorption in the near-infrared range, which was used for photothermal therapy and showed a high degree of inhibition of MDA-MB-231 tumor with a low level of laser radiation (1.5 W/cm2 for 5 min) and a low dose of medication. This complex has combined therapeutic functions, including an antioxidant effect on injuries caused by oxidative stress. It may be an ideal candidate for maximizing the results of chemothermal therapy, compensating for their adverse effects [122].
4. Photothermal Therapy
Photothermal therapy (PTT) is one of the non-surgical methods based on the use of particular photosensitizing substances, which selectively accumulate in pathologic cells and increase their sensitivity to light. Photothermal therapy has several advantages over other methods, for example, high efficiency in the treatment of skin cancer, the absence of complicated procedures in preparation for treatment, and the possibility of using it in hard-to-reach places [123].
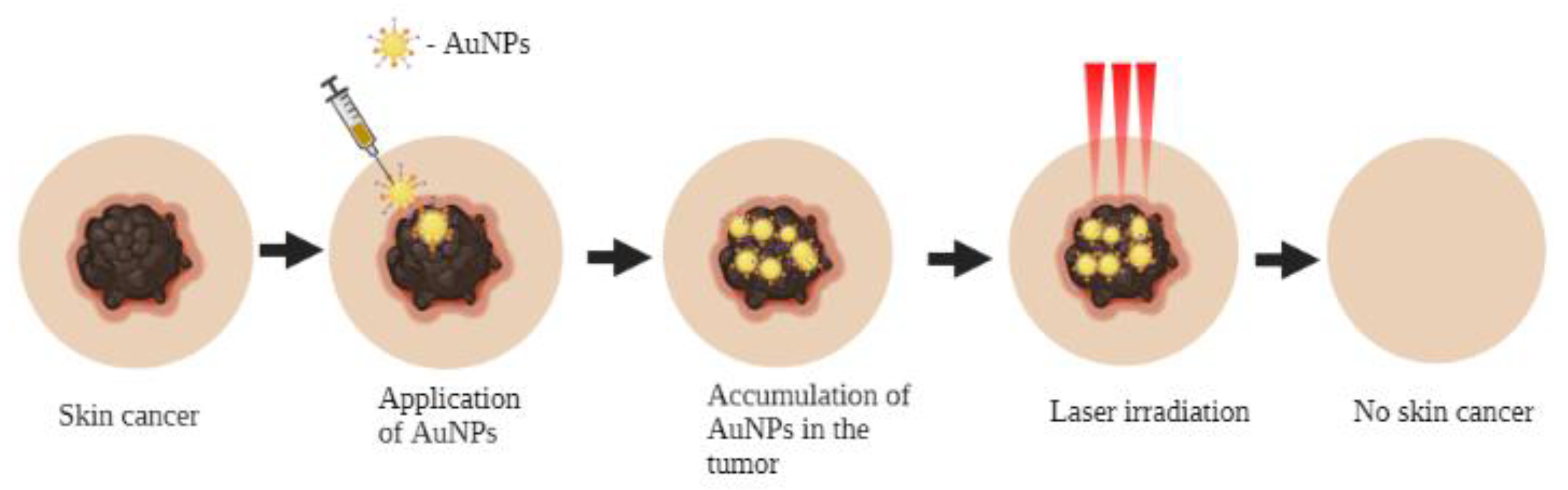
Usually, PTT is carried out in two stages (Figure 5): the introduction of a photosensitizer drug into the tumor area (or vein) and its accumulation in cancer cells, after which the tumor area is irradiated with a laser with a specific wavelength [124].
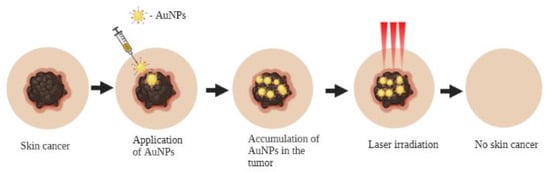
Figure 5.
Schematic illustration of PTT on skin cancer (created with BioRender.com).
AuNPs actively absorb radiation in the near-infrared range owing to the relative transparency of the human body and its large surface area, and these properties are the reason for the use of AuNPs in PTT [125,126]. Upon absorption of light energy, the photosensitizer excites the surrounding oxygen molecules into the singlet state, destroying cells by oxidation. Thus, for AuNPs, there is intense heating of cells, followed by their death. The depth of light penetration increases as its spectrum shifts to the red region, so the development of photosensitizers based on metal NPs, including AuNPs, activated by infrared radiation, should increase the depth of the photodynamic effect by several times [127,128].
An ideal candidate for a photothermal therapy role requires several conditions [129,130,131,132,133]:
- (i)
- nanoparticles of suitable size and uniform shape;
- (ii)
- possessing a good dispersibility in aqueous solutions;
- (iii)
- respond to near-infrared light in range (650–950 nm) to prevent damage to surrounding healthy tissue, to ensure sufficient photothermal efficiency, and to ensure enough penetration depth;
- (iv)
- sufficiently photostable to allow adequate diffusion time to reach tumors before losing their light sensitivity;
- (v)
- exhibit low or no cytotoxicity in living systems.
Gold is already used as a therapeutic method in nanomedicine, with colloidal gold, covalently linked to adenovirus vectors, used to selectively target cancer and induce hyperthermia by near-infrared (NIR) laser radiation. Moreover, gold nanoparticles have several advantages that make them suitable for photothermal cancer treatments [134,135]:
- (1)
- The ability to focus on the local region of the tumor while minimizing non-specific distribution;
- (2)
- They can be activated through near-infrared (NIR) laser light, creating the ability to penetrate deep into biological tissues;
- (3)
- They can be modulated to create multifaceted drug delivery systems and cancer photothermal therapy.
Several studies have proposed a unique hybrid material based on AuNPs and black phosphorus. Black phosphorus (BP), a new type of two-dimensional nanomaterial, has received serious attention in recent years thanks to its excellent properties and enormous potential in various chemical, physical, and biological fields [136,137]. The hybrid material is obtained by sonicating black phosphorus suspension, mixing it in boiling water with a HAuCl4 solution for 2 min. Finally, the solution is centrifuged to obtain gold nanoparticles in black phosphorus (BP-AuNPs). To assess the potential of BP-AuNPs, both in vivo and in vitro experiments showed encouraging results, with BP-AuNPs for 4 h inducing a more severe photothermal damage and 75% of cancer cells being destroyed after incubation with 30 μg/mL. Furthermore, the in vivo experiment with 4T1 mammary tumors in mice showed that photothermal treatment of tumors with BP-AuNPs provides high therapeutic efficacy without obvious neoplasms. Thus, the BP-AuNPs have an excellent photothermal effect and high antitumor activity, indicating their promising biomedicine potential [138].
AuNPs can also be used to increase the sensitivity of tumor cells to hyperthermia treatment, as proven by the work of Moradi S. et al. They analyzed the viability of Y79 cells 48 h after 0.5–11 min hyperthermia with and without AuNPs using MTT analysis and found that the percentage of cell viability was 50% after hyperthermia with AuNPs for 4.5 min; to achieve a similar effect without nanoparticles, it took 9 min. Thus, proving that AuNPs help increase tumor cells’ sensitivity to hyperthermia treatment [139].
Another latest advancement in the hyperthermal treatment of tumor diseases was Fe3O4 nanoparticles coated with gold and silver shells. Colloidal solutions of magnetite nanoparticles coated with gold and silver with 10–20 nm had a cytotoxic effect on HCT116 cells. Concentrations of 400 μg/mL and 600 μg/mL of the Fe3O4 core with a shell of AuNPs led to a decrease in the viability by about 40% and 55%, respectively [140].
5. Sonochemical Therapy
In recent years, scientists have widely explored various approaches in cancer therapy based on the action of ultrasound waves on the tumor [141]. There are a few studies on the use of ultrasound techniques in cancer control [142,143]. The therapeutic effect of ultrasound is based on its interaction with tissues, causing some biological effects [142].
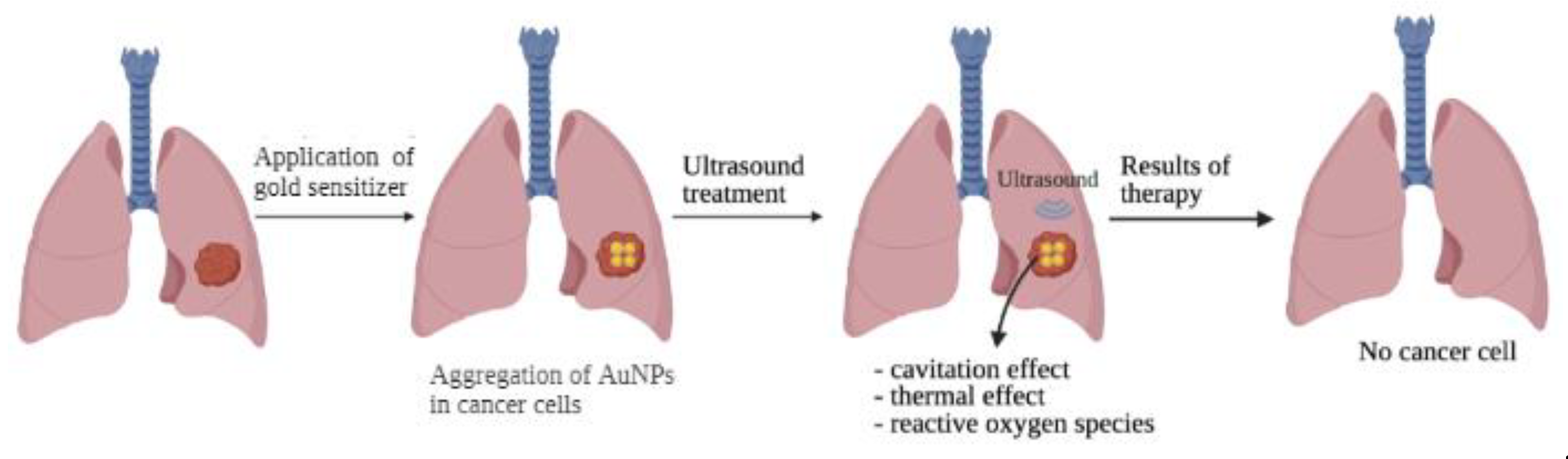
There are three main methods of ultrasound therapy for tumor diseases (Table 1): high intensity focused ultrasound (HIFU), low-intensity ultrasound (LIU), and sonodynamic therapy (SDT) [144,145,146,147]. The biological effects of ultrasound are mainly caused by heat, mechanical stress, and cavitation (Figure 6) [148]. Inertial cavitation is considered a more promising method of using ultrasound therapy as it does not cause thermal effects [149,150,151].

Table 1.
Main methods of ultrasound therapy for cancer.
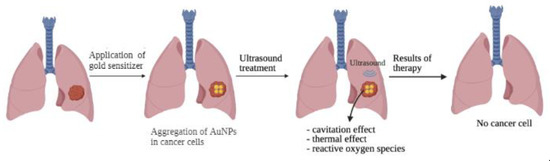
Figure 6.
Schematic illustration of sonochemical therapy (created with BioRender.com).
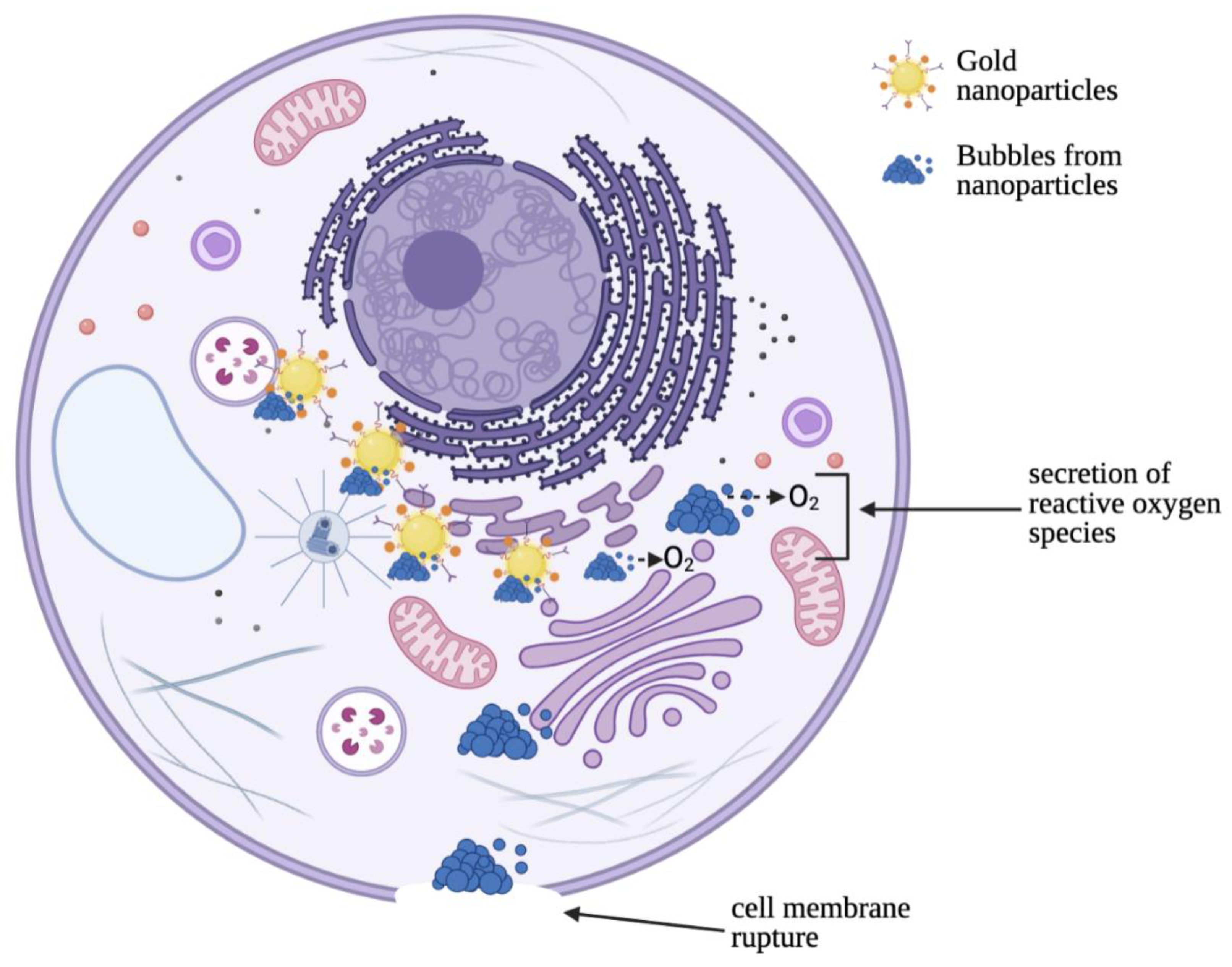
The main application of nanoparticles in ultrasound therapy for cancer is reduced to the formation of bubbles on their rough surface, which causes evaporation in the environment and, thereby, vapor cavities (Figure 7). The method of sonodynamic therapy seems to be very attractive because, owing to the high penetrating ability of ultrasound (up to tens of centimeters, depending on the frequency), it allows acting on intensely localized tumors that are inaccessible for photodynamic therapy [152,153].
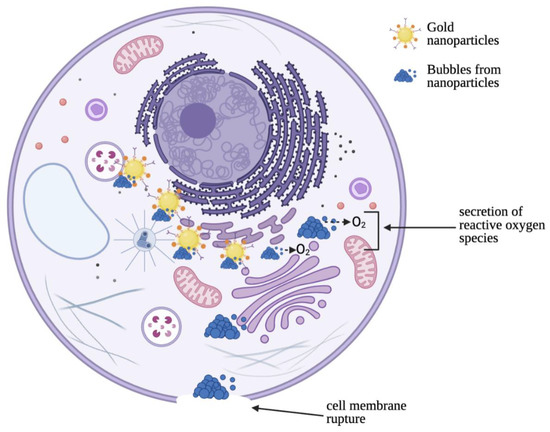
Figure 7.
Schematic illustration of the cavitation effect in the eukaryotic cell, with a demonstration of ROS secretion and cell membrane rupture (created with BioRender.com).
Sonodynamic therapy uses the synergistic effect of a non-toxic and selective agent (sensitizer). AuNPs can have tremendous therapeutic effects, together with SDT, through biocompatibility, selectivity, and biodistribution [142]. An example of ultrasound therapy and AuNPs is the recovery after anti-cancer therapy involving active forms of oxygen-ROS. Victor et al. demonstrated that nanoparticles and therapeutic pulsed ultrasound reduce the content of pro-inflammatory cytokines in tissues [154]. During the inflammatory phase of the healing process, ultrasound can activate immune cells to migrate to the injury site [155,156]. At the same time, gold compounds can suppress the expression of NF-κB and other inflammatory responses [157]. AuNPs can play a positive role after therapy with ROS participation, because, in combination with pulsed ultrasound, they reduce the effect of reactive oxidative forms on damaged tissues, thereby reducing the structural damage caused by this effect.
Beik et al. compared the pine-sensitizing effect of nanographene oxide and AuNPs. They noted that the ultrasound-induced heating of AuNPs was much higher than that of nanographene, which, in combination with vectors that can direct the nanoparticle to the tumor (for example, folic acid and peptide vectors), are promising for targeted sonodynamic therapy [158].
6. Gold Nanoparticles as a Diagnostic Material
One of the promising areas of application of gold nanoparticles is the diagnosis and theranostics of oncological diseases. Furthermore, AuNPs are a practical choice for biosensors and bioimaging applications because of their unique light absorption and scattering properties. In addition, the electrochemical response of AuNPs can be used as a detection signal [159].
Raman imaging, the technique that uses non-emitting electromagnetic waves (near-IR spectrum) to obtain a chemical composition from the Raman spectrum of a sample [159], is used to assess the chemical composition of cells and tissues in the body and, therefore, is used to track any change in the chemical structure due to tumor formation. AuNPs are used to diagnose cancer owing to their surface-enhanced Raman scattering (SERS) effect [160,161]. They can also be used for rapid intracellular Raman imaging, increasing the sensitivity and selectivity of the method and monitoring changes in cell morphology during toxic-induced cell death [162].
While Raman imaging methods are already successfully used in cancer diagnosis [163,164,165,166], Raman imaging diagnostics using AuNPs allow noticing specific differences related to specific components, reflecting different levels of nucleic acids, proteins, and lipids in cancers and normal serum [167]. For example, in a study with people with various oral cavity diseases, AuNPs allowed obtaining high-quality SERS-spectra of oral squamous cell carcinoma (OSCC) proteins, thus showing their efficiency in the diagnostics of OSCC. Thus, the Raman imaging method with AuNPs allows accurately determining the chemical composition of tissues and, therefore, diagnosing diseases and their localization with a high degree of probability. However, the methods’ sensitivity and effectiveness still depend on many factors, such as stage of the disease, localization of the disease, and the use or absence of additional agents.
Moreover, AuNPs used in combination with graphene oxide can be the next generation of nanotherapeutics, with the SERS signal from graphene oxide wrapped gold nanoparticles being used for intracellular Raman imaging in cancer cells, while an anti-cancer drug, attached to the nanoparticle, is being delivered into the cells [168].
Photoacoustic imaging (PAI), a biomedical analysis technique that provides practical information about the molecular characteristics of tissue, is a newly developed hybrid method of biomedical imaging for monitoring tumor angiogenesis and detecting skin melanoma, as well as monitoring and diagnosing other various neoplasms. Gold nanoparticles of different shapes are used in PAI, a method based on the absorption of waves and the subsequent generation of ultrasonic signals. Gold nanoparticles have great potential for use as biocompatible contrast agents, as reviewed in the work of Li W. and Chen, X. They suggest that the potential of AuNPs is due to their inherent and geometrically induced optical properties [169]. Moreover, as AuNPs are responsive to acidic environments, they can be used as imaging agents. Furthermore, they have a cancer-specific accumulation at the cellular level, and can thus provide an amplified signal for imaging cancer cells [170]. Another critical step is diagnosing metastasis, and biocompatible gold nanoparticles can be used as a contrast agent in diagnosing lymph-node-related diseases and metastasis, as they usually spread through the lymphatic system [171].
Dark-field microscopy, the type of microscopy in which the image contrast is increased by registering only the light scattered by the studied sample, provides a unique opportunity to research living and unstained biological samples in detail. Gold is one of the best markers for dark-field microscopy, which, combined with the properties of nanoparticles, can be a unique system for diagnosing tumor markers and a detailed study of tumor cells. Gold nanoparticles can be used as non-bleaching markers in dark-field microscopy. They are also used to analyze carbohydrate–protein interaction, correlated with biological processes, such as cancer metastasis, in a method based on a single plasmonic nanoparticle by conventional dark field microscopy [172]. Qian W. et al. showed that peptide conjugated AuNPs could be delivered to the cytoplasmic or nuclear region of a cell and used as light scattering contrast agents, thus enabling to track the complete cycle of cancer cells from birth to division [173].
Moreover, AuNPs have been used as an internal reference to reduce the deviations and fluctuations from the dark-field microscopy technique and improve the precision of the acquired data through post-data analysis [174].
Computed tomography (CT), the non-destructive layer-by-layer examination of the internal structure of tissue using X-ray radiation, is used for cell imaging. However, a more accurate image is obtained by injecting a contrast agent intravenously in the diagnosis of tumor diseases. Cao Y. et al. showed that gold nanoparticles could be used as a nanoscale contrast agent, as they used their dendrimer-entrapped AuNPs for targeted CT imaging of hepatocellular carcinoma (HCC), and their flow cytometry results revealed that dendrimer-entrapped gold nanoparticles modified with lactobionic acid could specifically target HepG2 cells [175]. Furthermore, an in vivo cell tracking method using gold nanoparticles was developed and tested using a melanoma-specific T-cell receptor labeled with AuNPs. The AuNPs-labeled T-cells were injected intravenously into mice and, with CT imaging, they were able to study the distribution, migration, and kinetics of T-cells [176]. Apart from CT, other molecular imaging techniques used in cancer diagnostics, such as magnetic resonance imaging (MRI), have also benefited from the development of targeted contrast agents, such as gold nanoparticles, which enables targeted imaging via site-specific accumulation of nanoparticles in the cells of interest [177,178].
In addition to the traditional diagnostic methods, various diagnostic and theranostics systems based on gold nanoparticles are currently being created, like a highly sensitive method for amplifying an enzyme signal using gold nanoparticles to detect a specific antigen in human serum. In addition, a smartphone application was developed for quick analysis of the results within 15 min, displaying them on the smartphone screen [179]. In addition, AuNPs are also used as carriers of the biorecognition of antibody aKLK3 and HRP-streptavidin/biotinylated poly-A-ssDNA sequences for the specific and sensitive analysis of KLK3, an important marker for the diagnosis of prostate cancer [180,181,182].
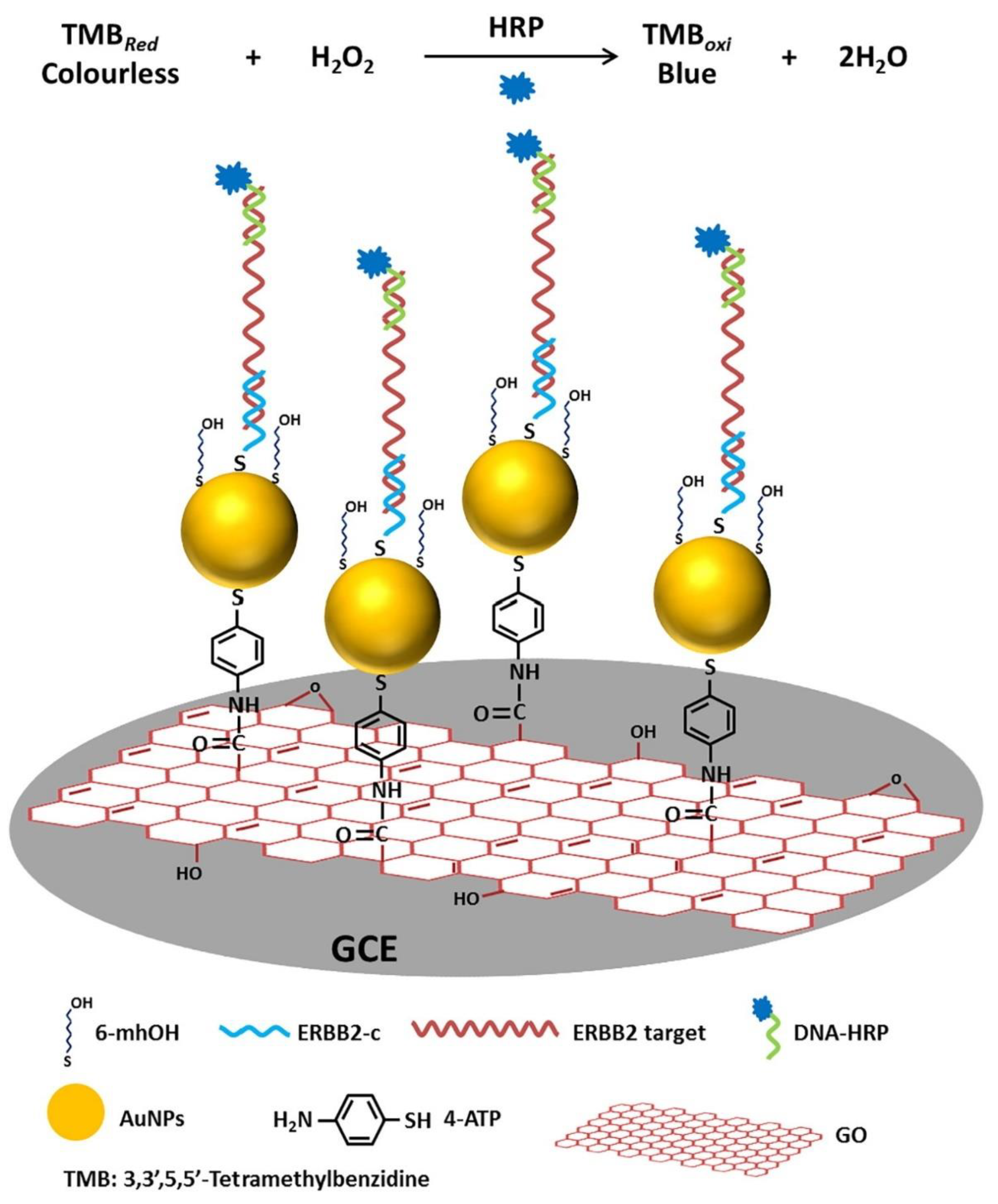
A DNA biosensor based on a hybrid material consisting of graphene oxide and gold nanoparticles (Figure 8) was developed. It uses a sandwich hybridization assay by immobilizing a DNA probe on gold nanoparticles and capturing target DNA biomarkers [183]. The device is based on electrochemical DNA interactions, and its signal is measured by amperometric detection [184,185]. Using amperometric detection, breast cancer biomarkers were obtained with a sensitivity of 378 nA/nM and 219 nA/nM for the target ERBB2 and CD24, respectively, which is several times higher than the target content of these compounds in the tumor [186].
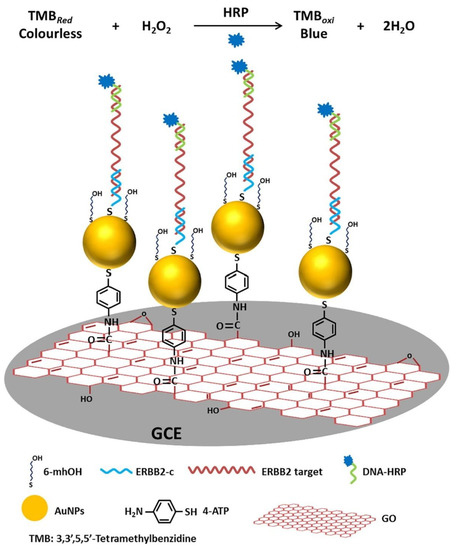
Figure 8.
Schematic illustration of a DNA sensor showing the hybrid material consisting of graphene oxide and gold nanoparticles and the hybridization of target DNA [183].
One of the most challenging tumor diseases to diagnose is brain cancer, but now, diagnostic and theranostic systems based on gold nanoparticles are being actively created, as reviewed by Meola A. et al. [187].
In conclusion, AuNPs possess a unique structure that can be actively used both as a carrier of test systems and as a signal source for the diagnosis of tumor markers and an excellent contrast agent for various diagnostic methods currently used.
7. Current Major Restrictions on the Use of Gold Nanoparticles for Medical Purposes
7.1. Toxicity: Safety Test
Currently, there are several standard methods for assessing the toxicity/safety of nanoparticles in vitro. In addition, researchers have developed recommendations for determining the toxicity of various nanoparticles [188]. However, these techniques are individual for each type of nanoparticle and cannot be applied to more complex or hybrid materials. This leads to uncertain and unpredictable results for real objects, leading to a lack of therapeutic/diagnostic action or being more detrimental to the body.
As mentioned in the section on the effect of shape and size on the biological properties of nanoparticles, there are a considerable number of factors affecting the toxicity of nanoparticles (size, shape, surface charge, and capping agents), and this complicates the possibility of developing an appropriate method for determining toxicity. In addition, it was reported that the toxicity does not depend only on the type of nanoparticles, but also on the target. For different tumor cells, the effect of gold nanoparticles occurs at different concentrations. In this regard, it can be concluded that it is necessary to create several universal procedures (similar to GLP) that allow assessing the safety of nanoparticles in each specific case, which will be used for all similar objects around the world (personalized) [188,189,190].
7.2. Adsorption from Physiological Media
Size, developed surface, shape, and charge contribute to the adsorption of the protein on the surface of nanoparticles. Consequently, this leads to a change in physicochemical parameters and, thereby, worsens the therapeutic properties. Therefore, the development of new agents that would modify the surface could help realistically evaluate the properties of nanoparticles by their physicochemical properties [191]. In addition, several delivery methods that consider the formation of the corona protein and allow it to be used for various purposes are being developed [192,193].
7.3. Pharmacodynamics: Pharmacokinetics
Even though studies on gold nanoparticles are very relevant, there have still not been comprehensive studies on their kinetics, clearance, and biodistribution inside the organism. The lack of studies on the pharmacokinetics of gold nanoparticles inside the human body limits the possibility of the massive use of gold nanoparticles in treating tumor diseases. Analysis of these parameters is complicated by the difficulty of determining nanoparticles’ distribution in the organism, as experiments in vivo and in vitro do not give a complete picture of the biodistribution of nanoparticles within the organism. It is important to note that gold nanoparticles are a convenient object for studying inside the organism, compared with other nano-objects, owing to surface plasma resonance and a high extinction coefficient [194].
7.4. Low Efficiency
Wilhelm S. et al. studied the nanoparticles’ delivery to tumors and found that, on average, only 0.7% of nanoparticles reach the cancer cells, and only in exceptional cases, nanoparticles reach the tumors in more than 5%. Furthermore, when nanoparticles are injected, the mononuclear phagocytic system (MPS) and the renal clearance pathway absorb most of the nanoparticles, drastically reducing the effectiveness and harming the MPS organs [195].
7.5. Lack of Clinical Trials
There are currently few clinical trials using gold nanoparticles (around 15 studies in https://clinicaltrials.gov (accessed on 5 September 2021 )), which do not yet allow comprehensive research on various factors and indicators (clearance, biodistribution, and protein sorption), and thus limit the use of nanoparticles in medical practice. The onset of clinical trials could expand and clarify the therapeutic and diagnostic potential of nanoparticles. Still, they should be carried out after comprehensive safety and toxicity tests of these nanoparticles [196].
8. Conclusions
Cancer remains the most common cause of death currently. Hence, there is a need to develop new and improved cancer treatment and diagnosis, which requires new and modern approaches, and AuNPs can become one of these new approaches. Although there have been several scientific studies on NPs’ application in cancer medicine, studies on AuNPs’ use in cancer therapy and diagnostics are emerging. Therefore, in this review, we analyzed available data on the applications of AuNPs in oncotherapy and cancer diagnostics. Studies have shown that, while shape, size, and charge have a considerable impact on the properties of AuNPs, no direct correlation was found between those parameters and the effectiveness of AuNPs’ use in therapy. Moreover, for each type of tumor disease, a personalized approach is required to establish the optimal physical and chemical parameters of AuNPs that will ensure maximum efficiency and safety.
In therapy, AuNPs can effectively be used as delivery systems for various molecules, including high-molecular compounds. They can also be used as auxiliary agents for sonochemistry and sensitizers for photodynamic therapy. Thanks to their physicochemical properties, they are a very promising sensitizer for these therapeutic methods, which are most relevant for treating skin cancer, as they are highly effective and safe.
In addition, AuNPs play a special role in the diagnosis and theranostics of tumor diseases, with several methods already developed for the diagnosis of diseases successfully using AuNPs as auxiliary agents and sensitizers. AuNPs and their hybrid materials derivatives are very promising components that will soon help in the early diagnosis of tumor markers.
Although the benefits of AuNPs in cancer medicine are visible, there remain several constraints that need to be studied, analyzed, and solved before any large-scale use of gold nanoparticles in the therapy and diagnosis of cancer, along with traditional drugs.
Author Contributions
Methodology, A.A.V.; writing—original draft preparation, A.A.V. and P.K.; writing—review and editing, M.G.H.R., A.A.K. and Y.M.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Acknowledgments
This paper was supported by the RUDN University Strategic Academic Leadership Program.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. WHO Report on Cancer: Setting Priorities, Investing Wisely and Providing Care for All; World Health Organization: Geneva, Switzerland, 2020; ISBN 9789240001299. [Google Scholar]
- Abdel-Qadir, H.; Austin, P.C.; Lee, D.S.; Amir, E.; Tu, J.V.; Thavendiranathan, P.; Fung, K.; Anderson, G.M. A Population-Based Study of Cardiovascular Mortality Following Early-Stage Breast Cancer. JAMA Cardiol. 2017, 2, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Sud, A.; Kinnersley, B.; Houlston, R.S. Genome-Wide Association Studies of Cancer: Current Insights and Future Perspectives. Nat. Rev. Cancer 2017, 17, 692–704. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Cancer Collaboration Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2016: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2018, 4, 1553–1568. [CrossRef]
- Cibula, D.; Pötter, R.; Planchamp, F.; Avall-Lundqvist, E.; Fischerova, D.; Haie-Meder, C.; Köhler, C.; Landoni, F.; Lax, S.; Lindegaard, J.C.; et al. The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology Guidelines for the Management of Patients with Cervical Cancer. Virchows Arch. 2018, 472, 919–936. [Google Scholar] [CrossRef]
- Tu, H.; Wen, C.P.; Tsai, S.P.; Chow, W.-H.; Wen, C.; Ye, Y.; Zhao, H.; Tsai, M.K.; Huang, M.; Dinney, C.P.; et al. Cancer Risk Associated with Chronic Diseases and Disease Markers: Prospective Cohort Study. BMJ 2018, 360, k134. [Google Scholar] [CrossRef]
- Palesh, O.; Scheiber, C.; Kesler, S.; Mustian, K.; Koopman, C.; Schapira, L. Management of Side Effects during and Post-Treatment in Breast Cancer Survivors. Breast J. 2018, 24, 167–175. [Google Scholar] [CrossRef]
- Zaorsky, N.G.; Churilla, T.M.; Egleston, B.L.; Fisher, S.G.; Ridge, J.A.; Horwitz, E.M.; Meyer, J.E. Causes of Death among Cancer Patients. Ann. Oncol. 2017, 28, 400–407. [Google Scholar] [CrossRef]
- Yarchoan, R.; Uldrick, T.S. HIV-Associated Cancers and Related Diseases. N. Engl. J. Med. 2018, 378, 1029–1041. [Google Scholar] [CrossRef]
- Tocut, M.; Brenner, R.; Zandman-Goddard, G. Autoimmune Phenomena and Disease in Cancer Patients Treated with Immune Checkpoint Inhibitors. Autoimmun. Rev. 2018, 17, 610–616. [Google Scholar] [CrossRef]
- Delaunay, M.; Cadranel, J.; Lusque, A.; Meyer, N.; Gounant, V.; Moro-Sibilot, D.; Michot, J.-M.; Raimbourg, J.; Girard, N.; Guisier, F.; et al. Immune-Checkpoint Inhibitors Associated with Interstitial Lung Disease in Cancer Patients. Eur. Respir. J. 2017, 50, 1700050. [Google Scholar] [CrossRef]
- Curigliano, G.; Lenihan, D.; Fradley, M.; Ganatra, S.; Barac, A.; Blaes, A.; Herrmann, J.; Porter, C.; Lyon, A.R.; Lancellotti, P.; et al. Management of Cardiac Disease in Cancer Patients throughout Oncological Treatment: ESMO Consensus Recommendations. Ann. Oncol. 2020, 31, 171–190. [Google Scholar] [CrossRef] [PubMed]
- Pearman, T.P.; Beaumont, J.L.; Mroczek, D.; O’Connor, M.; Cella, D. Validity and Usefulness of a Single-Item Measure of Patient-Reported Bother from Side Effects of Cancer Therapy. Cancer 2018, 124, 991–997. [Google Scholar] [CrossRef]
- Pearce, A.; Haas, M.; Viney, R.; Pearson, S.-A.; Haywood, P.; Brown, C.; Ward, R. Incidence and Severity of Self-Reported Chemotherapy Side Effects in Routine Care: A Prospective Cohort Study. PLoS ONE 2017, 12, e0184360. [Google Scholar] [CrossRef]
- Demaria, M.; O’Leary, M.N.; Chang, J.; Shao, L.; Liu, S.; Alimirah, F.; Koenig, K.; Le, C.; Mitin, N.; Deal, A.M.; et al. Cellular Senescence Promotes Adverse Effects of Chemotherapy and Cancer Relapse. Cancer Discov. 2017, 7, 165–176. [Google Scholar] [CrossRef]
- Ariza-Garcia, A.; Lozano-Lozano, M.; Galiano-Castillo, N.; Postigo-Martin, P.; Arroyo-Morales, M.; Cantarero-Villanueva, I. A Web-Based Exercise System (e-CuidateChemo) to Counter the Side Effects of Chemotherapy in Patients with Breast Cancer: Randomized Controlled Trial. J. Med. Internet Res. 2019, 21, e14418. [Google Scholar] [CrossRef]
- Carlson, L.E.; Subnis, U.B.; Piedalue, K.-A.L.; Vallerand, J.; Speca, M.; Lupichuk, S.; Tang, P.; Faris, P.; Wolever, R.Q. The ONE-MIND Study: Rationale and Protocol for Assessing the Effects of ONlinE MINDfulness-Based Cancer Recovery for the Prevention of Fatigue and Other Common Side Effects during Chemotherapy. Eur. J. Cancer Care 2019, 28, e13074. [Google Scholar] [CrossRef]
- Gegechkori, N.; Haines, L.; Lin, J.J. Long-Term and Latent Side Effects of Specific Cancer Types. Med. Clin. N. Am. 2017, 101, 1053–1073. [Google Scholar] [CrossRef] [PubMed]
- McGowan, J.V.; Chung, R.; Maulik, A.; Piotrowska, I.; Walker, J.M.; Yellon, D.M. Anthracycline Chemotherapy and Cardiotoxicity. Cardiovasc. Drugs Ther. 2017, 31, 63–75. [Google Scholar] [CrossRef]
- Mostafavi, E.; Soltantabar, P.; Webster, T.J. Nanotechnology and picotechnology. In Biomaterials in Translational Medicine; Elsevier: Amsterdam, The Netherlands, 2019; pp. 191–212. ISBN 9780128134771. [Google Scholar]
- Chen, S.; Li, R.; Li, X.; Xie, J. Electrospinning: An Enabling Nanotechnology Platform for Drug Delivery and Regenerative Medicine. Adv. Drug Deliv. Rev. 2018, 132, 188–213. [Google Scholar] [CrossRef] [PubMed]
- Abadeer, N.S.; Murphy, C.J. Recent Progress in Cancer Thermal Therapy Using Gold Nanoparticles. J. Phys. Chem. C Nanomater. Interfaces 2016, 120, 4691–4716. [Google Scholar] [CrossRef]
- Song, W.; Anselmo, A.C.; Huang, L. Nanotechnology Intervention of the Microbiome for Cancer Therapy. Nat. Nanotechnol. 2019, 14, 1093–1103. [Google Scholar] [CrossRef] [PubMed]
- Riaz, M.K.; Riaz, M.A.; Zhang, X.; Lin, C.; Wong, K.H.; Chen, X.; Zhang, G.; Lu, A.; Yang, Z. Surface Functionalization and Targeting Strategies of Liposomes in Solid Tumor Therapy: A Review. Int. J. Mol. Sci. 2018, 19, 195. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Deng, X.; Ding, J.; Zhou, W.; Zheng, X.; Tang, G. Mechanisms of Drug Release in pH-Sensitive Micelles for Tumour Targeted Drug Delivery System: A Review. Int. J. Pharm. 2018, 535, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Tao, W.; Ji, X.; Xu, X.; Islam, M.A.; Li, Z.; Chen, S.; Saw, P.E.; Zhang, H.; Bharwani, Z.; Guo, Z.; et al. Antimonene Quantum Dots: Synthesis and Application as near-Infrared Photothermal Agents for Effective Cancer Therapy. Angew. Chem. Weinh. Bergstr. Ger. 2017, 129, 12058–12062. [Google Scholar] [CrossRef]
- Palmerston Mendes, L.; Pan, J.; Torchilin, V.P. Dendrimers as Nanocarriers for Nucleic Acid and Drug Delivery in Cancer Therapy. Molecules 2017, 22, 1401. [Google Scholar] [CrossRef]
- Jia, Q.; Ge, J.; Liu, W.; Zheng, X.; Wang, M.; Zhang, H.; Wang, P. Biocompatible Iron Phthalocyanine-Albumin Assemblies as Photoacoustic and Thermal Theranostics in Living Mice. ACS Appl. Mater. Interfaces 2017, 9, 21124–21132. [Google Scholar] [CrossRef]
- Wang, P.; Zhang, L.; Zheng, W.; Cong, L.; Guo, Z.; Xie, Y.; Wang, L.; Tang, R.; Feng, Q.; Hamada, Y.; et al. Thermo-Triggered Release of CRISPR-Cas9 System by Lipid-Encapsulated Gold Nanoparticles for Tumor Therapy. Angew. Chem. Int. Ed. Engl. 2018, 57, 1491–1496. [Google Scholar] [CrossRef]
- Daraee, H.; Eatemadi, A.; Abbasi, E.; Fekri Aval, S.; Kouhi, M.; Akbarzadeh, A. Application of Gold Nanoparticles in Biomedical and Drug Delivery. Artif. Cells Nanomed. Biotechnol. 2016, 44, 410–422. [Google Scholar] [CrossRef]
- Cai, Y.; Liang, P.; Tang, Q.; Yang, X.; Si, W.; Huang, W.; Zhang, Q.; Dong, X. Diketopyrrolopyrrole-Triphenylamine Organic Nanoparticles as Multifunctional Reagents for Photoacoustic Imaging-Guided Photodynamic/Photothermal Synergistic Tumor Therapy. ACS Nano 2017, 11, 1054–1063. [Google Scholar] [CrossRef]
- Aghebati-Maleki, A.; Dolati, S.; Ahmadi, M.; Baghbanzhadeh, A.; Asadi, M.; Fotouhi, A.; Yousefi, M.; Aghebati-Maleki, L. Nanoparticles and Cancer Therapy: Perspectives for Application of Nanoparticles in the Treatment of Cancers. J. Cell. Physiol. 2020, 235, 1962–1972. [Google Scholar] [CrossRef]
- Xuan, M.; Shao, J.; Zhao, J.; Li, Q.; Dai, L.; Li, J. Magnetic Mesoporous Silica Nanoparticles Cloaked by Red Blood Cell Membranes: Applications in Cancer Therapy. Angew. Chem. Int. Ed. Engl. 2018, 57, 6049–6053. [Google Scholar] [CrossRef] [PubMed]
- Mishra, H.; Mishra, P.K.; Ekielski, A.; Jaggi, M.; Iqbal, Z.; Talegaonkar, S. Melanoma Treatment: From Conventional to Nanotechnology. J. Cancer Res. Clin. Oncol. 2018, 144, 2283–2302. [Google Scholar] [CrossRef] [PubMed]
- Candido, N.M.; de Melo, M.T.; Franchi, L.P.; Primo, F.L.; Tedesco, A.C.; Rahal, P.; Calmon, M.F. Combining Photodynamic Therapy and Chemotherapy: Improving Breast Cancer Treatment with Nanotechnology. J. Biomed. Nanotechnol. 2018, 14, 994–1008. [Google Scholar] [CrossRef] [PubMed]
- Janicka, M.; Gubernator, J. Use of Nanotechnology for Improved Pharmacokinetics and Activity of Immunogenic Cell Death Inducers Used in Cancer Chemotherapy. Expert Opin. Drug Deliv. 2017, 14, 1059–1075. [Google Scholar] [CrossRef]
- Zhao, C.-Y.; Cheng, R.; Yang, Z.; Tian, Z.-M. Nanotechnology for Cancer Therapy Based on Chemotherapy. Molecules 2018, 23, 826. [Google Scholar] [CrossRef]
- Falagan-Lotsch, P.; Grzincic, E.M.; Murphy, C.J. New Advances in Nanotechnology-Based Diagnosis and Therapeutics for Breast Cancer: An Assessment of Active-Targeting Inorganic Nanoplatforms. Bioconjug. Chem. 2017, 28, 135–152. [Google Scholar] [CrossRef]
- Matos, A.I.; Carreira, B.; Peres, C.; Moura, L.I.F.; Conniot, J.; Fourniols, T.; Scomparin, A.; Martínez-Barriocanal, Á.; Arango, D.; Conde, J.P.; et al. Nanotechnology Is an Important Strategy for Combinational Innovative Chemo-Immunotherapies against Colorectal Cancer. J. Control. Release 2019, 307, 108–138. [Google Scholar] [CrossRef]
- Pillai, G. Nanotechnology toward treating cancer. In Applications of Targeted Nano Drugs and Delivery Systems; Elsevier: Amsterdam, The Netherlands, 2019; pp. 221–256. ISBN 9780128140291. [Google Scholar]
- Sielaff, C.M.; Mousa, S.A. Status and Future Directions in the Management of Pancreatic Cancer: Potential Impact of Nanotechnology. J. Cancer Res. Clin. Oncol. 2018, 144, 1205–1217. [Google Scholar] [CrossRef]
- Song, G.; Cheng, L.; Chao, Y.; Yang, K.; Liu, Z. Emerging Nanotechnology and Advanced Materials for Cancer Radiation Therapy. Adv. Mater. 2017, 29, 1604894. [Google Scholar] [CrossRef]
- Deng, H.; Zhang, Z. The Application of Nanotechnology in Immune Checkpoint Blockade for Cancer Treatment. J. Control. Release 2018, 290, 28–45. [Google Scholar] [CrossRef]
- Cryer, A.M.; Thorley, A.J. Nanotechnology in the Diagnosis and Treatment of Lung Cancer. Pharmacol. Ther. 2019, 198, 189–205. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Yang, M.; Pang, B.; Vara, M.; Xia, Y. Gold Nanomaterials at Work in Biomedicine. Chem. Rev. 2015, 115, 10410–10488. [Google Scholar] [CrossRef] [PubMed]
- Dreaden, E.C.; Alkilany, A.M.; Huang, X.; Murphy, C.J.; El-Sayed, M.A. The Golden Age: Gold Nanoparticles for Biomedicine. Chem. Soc. Rev. 2012, 41, 2740–2779. [Google Scholar] [CrossRef] [PubMed]
- Beik, J.; Khateri, M.; Khosravi, Z.; Kamrava, S.K.; Kooranifar, S.; Ghaznavi, H.; Shakeri-Zadeh, A. Gold Nanoparticles in Combinatorial Cancer Therapy Strategies. Coord. Chem. Rev. 2019, 387, 299–324. [Google Scholar] [CrossRef]
- Maeda, H.; Wu, J.; Sawa, T.; Matsumura, Y.; Hori, K. Tumor Vascular Permeability and the EPR Effect in Macromolecular Therapeutics: A Review. J. Control. Release 2000, 65, 271–284. [Google Scholar] [CrossRef]
- Singh, P.; Pandit, S.; Mokkapati, V.R.S.S.; Garg, A.; Ravikumar, V.; Mijakovic, I. Gold Nanoparticles in Diagnostics and Therapeutics for Human Cancer. Int. J. Mol. Sci. 2018, 19, 1979. [Google Scholar] [CrossRef]
- Wei, Y.; Quan, L.; Zhou, C.; Zhan, Q. Factors Relating to the Biodistribution & Clearance of Nanoparticles & Their Effects on in Vivo Application. Nanomedicine 2018, 13, 1495–1512. [Google Scholar] [CrossRef]
- Angelov, B.; Angelova, A.; Filippov, S.K.; Drechsler, M.; Štěpánek, P.; Lesieur, S. Multicompartment Lipid Cubic Nanoparticles with High Protein Upload: Millisecond Dynamics of Formation. ACS Nano 2014, 8, 5216–5226. [Google Scholar] [CrossRef]
- Dou, Y.; Yang, X. Novel High-Sensitive Fluorescent Detection of Deoxyribonuclease I Based on DNA-Templated Gold/silver Nanoclusters. Anal. Chim. Acta 2013, 784, 53–58. [Google Scholar] [CrossRef]
- Weadick, D.S.; Liu, J. Phosphorothioate DNA Stabilized Fluorescent Gold and Silver Nanoclusters. Nanomaterials 2015, 5, 804–813. [Google Scholar] [CrossRef]
- Lee, Y.J.; Ahn, E.-Y.; Park, Y. Shape-Dependent Cytotoxicity and Cellular Uptake of Gold Nanoparticles Synthesized Using Green Tea Extract. Nanoscale Res. Lett. 2019, 14, 129. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Liao, J.; Shao, X.; Li, Q.; Lin, Y. The Effect of Shape on Cellular Uptake of Gold Nanoparticles in the Forms of Stars, Rods, and Triangles. Sci. Rep. 2017, 7, 3827. [Google Scholar] [CrossRef] [PubMed]
- Scarabelli, L.; Coronado-Puchau, M.; Giner-Casares, J.J.; Langer, J.; Liz-Marzán, L.M. Monodisperse Gold Nanotriangles: Size Control, Large-Scale Self-Assembly, and Performance in Surface-Enhanced Raman Scattering. ACS Nano 2014, 8, 5833–5842. [Google Scholar] [CrossRef] [PubMed]
- Sironi, L.; Freddi, S.; Caccia, M.; Pozzi, P.; Rossetti, L.; Pallavicini, P.; Donà, A.; Cabrini, E.; Gualtieri, M.; Rivolta, I.; et al. Gold Branched Nanoparticles for Cellular Treatments. J. Phys. Chem. C Nanomater. Interfaces 2012, 116, 18407–18418. [Google Scholar] [CrossRef]
- Steckiewicz, K.P.; Barcinska, E.; Malankowska, A.; Zauszkiewicz-Pawlak, A.; Nowaczyk, G.; Zaleska-Medynska, A.; Inkielewicz-Stepniak, I. Impact of Gold Nanoparticles Shape on Their Cytotoxicity against Human Osteoblast and Osteosarcoma in in Vitro Model. Evaluation of the Safety of Use and Anti-Cancer Potential. J. Mater. Sci. Mater. Med. 2019, 30, 22. [Google Scholar] [CrossRef] [PubMed]
- Suchomel, P.; Kvitek, L.; Prucek, R.; Panacek, A.; Halder, A.; Vajda, S.; Zboril, R. Simple Size-Controlled Synthesis of Au Nanoparticles and Their Size-Dependent Catalytic Activity. Sci. Rep. 2018, 8, 4589. [Google Scholar] [CrossRef]
- Xu, M.; Soliman, M.G.; Sun, X.; Pelaz, B.; Feliu, N.; Parak, W.J.; Liu, S. How Entanglement of Different Physicochemical Properties Complicates the Prediction of in Vitro and in Vivo Interactions of Gold Nanoparticles. ACS Nano 2018, 12, 10104–10113. [Google Scholar] [CrossRef]
- Tenzer, S.; Docter, D.; Rosfa, S.; Wlodarski, A.; Kuharev, J.; Rekik, A.; Knauer, S.K.; Bantz, C.; Nawroth, T.; Bier, C.; et al. Nanoparticle Size Is a Critical Physicochemical Determinant of the Human Blood Plasma Corona: A Comprehensive Quantitative Proteomic Analysis. ACS Nano 2011, 5, 7155–7167. [Google Scholar] [CrossRef]
- Walkey, C.D.; Olsen, J.B.; Song, F.; Liu, R.; Guo, H.; Olsen, D.W.H.; Cohen, Y.; Emili, A.; Chan, W.C.W. Protein Corona Fingerprinting Predicts the Cellular Interaction of Gold and Silver Nanoparticles. ACS Nano 2014, 8, 2439–2455. [Google Scholar] [CrossRef]
- Rozengurt, E.; Heppel, L.A. A Specific Effect of External ATP on the Permeability of Transformed 3T3 Cells. Biochem. Biophys. Res. Commun. 1975, 67, 1581–1588. [Google Scholar] [CrossRef]
- Liu, H.; Pierre-Pierre, N.; Huo, Q. Dynamic Light Scattering for Gold Nanorod Size Characterization and Study of Nanorod–protein Interactions. Gold Bull. 2012, 45, 187–195. [Google Scholar] [CrossRef]
- Duncan, B.; Kim, C.; Rotello, V.M. Gold Nanoparticle Platforms as Drug and Biomacromolecule Delivery Systems. J. Control. Release 2010, 148, 122–127. [Google Scholar] [CrossRef]
- Love, J.C.; Estroff, L.A.; Kriebel, J.K.; Nuzzo, R.G.; Whitesides, G.M. Self-Assembled Monolayers of Thiolates on Metals as a Form of Nanotechnology. Chem. Rev. 2005, 105, 1103–1169. [Google Scholar] [CrossRef]
- Hostetler, M.J.; Wingate, J.E.; Zhong, C.-J.; Harris, J.E.; Vachet, R.W.; Clark, M.R.; Londono, J.D.; Green, S.J.; Stokes, J.J.; Wignall, G.D.; et al. Alkanethiolate Gold Cluster Molecules with Core Diameters from 1.5 to 5.2 Nm: Core and Monolayer Properties as a Function of Core Size. Langmuir 1998, 14, 17–30. [Google Scholar] [CrossRef]
- Rana, S.; Bajaj, A.; Mout, R.; Rotello, V.M. Monolayer Coated Gold Nanoparticles for Delivery Applications. Adv. Drug Deliv. Rev. 2012, 64, 200–216. [Google Scholar] [CrossRef]
- Perrault, S.D.; Walkey, C.; Jennings, T.; Fischer, H.C.; Chan, W.C.W. Mediating Tumor Targeting Efficiency of Nanoparticles through Design. Nano Lett. 2009, 9, 1909–1915. [Google Scholar] [CrossRef] [PubMed]
- Maeda, H.; Nakamura, H.; Fang, J. The EPR Effect for Macromolecular Drug Delivery to Solid Tumors: Improvement of Tumor Uptake, Lowering of Systemic Toxicity, and Distinct Tumor Imaging in Vivo. Adv. Drug Deliv. Rev. 2013, 65, 71–79. [Google Scholar] [CrossRef]
- Park, J.; Choi, Y.; Chang, H.; Um, W.; Ryu, J.H.; Kwon, I.C. Alliance with EPR Effect: Combined Strategies to Improve the EPR Effect in the Tumor Microenvironment. Theranostics 2019, 9, 8073–8090. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Ortiz, M.; Zapata-Urzúa, C.; Acosta, G.A.; Álvarez-Lueje, A.; Albericio, F.; Kogan, M.J. Gold Nanoparticles as an Efficient Drug Delivery System for GLP-1 Peptides. Colloids Surf. B Biointerfaces 2017, 158, 25–32. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Yang, D.; Qin, M.; Zhang, Y.; He, B.; Dai, W.; Wang, X.; Zhang, Q.; Zhang, H.; Yin, C. Increased Cellular Uptake of Peptide-Modified PEGylated Gold Nanoparticles. Biochem. Biophys. Res. Commun. 2017, 494, 339–345. [Google Scholar] [CrossRef]
- Halamoda-Kenzaoui, B.; Ceridono, M.; Urbán, P.; Bogni, A.; Ponti, J.; Gioria, S.; Kinsner-Ovaskainen, A. The Agglomeration State of Nanoparticles Can Influence the Mechanism of Their Cellular Internalisation. J. Nanobiotechnol. 2017, 15, 48. [Google Scholar] [CrossRef]
- Odhner, J.H.; Moore Tibbetts, K.; Tangeysh, B.; Wayland, B.B.; Levis, R.J. Mechanism of Improved Au Nanoparticle Size Distributions Using Simultaneous Spatial and Temporal Focusing for Femtosecond Laser Irradiation of Aqueous KAuCl4. J. Phys. Chem. C Nanomater. Interfaces 2014, 118, 23986–23995. [Google Scholar] [CrossRef]
- Zhang, S.; Gao, H.; Bao, G. Physical Principles of Nanoparticle Cellular Endocytosis. ACS Nano 2015, 9, 8655–8671. [Google Scholar] [CrossRef]
- Nakase, I.; Niwa, M.; Takeuchi, T.; Sonomura, K.; Kawabata, N.; Koike, Y.; Takehashi, M.; Tanaka, S.; Ueda, K.; Simpson, J.C.; et al. Cellular Uptake of Arginine-Rich Peptides: Roles for Macropinocytosis and Actin Rearrangement. Mol. Ther. 2004, 10, 1011–1022. [Google Scholar] [CrossRef]
- Kapur, A.; Medina, S.H.; Wang, W.; Palui, G.; Schneider, J.P.; Mattoussi, H. Intracellular Delivery of Gold Nanocolloids Promoted by a Chemically Conjugated Anticancer Peptide. ACS Omega 2018, 3, 12754–12762. [Google Scholar] [CrossRef]
- Gaspar, D.; Veiga, A.S.; Sinthuvanich, C.; Schneider, J.P.; Castanho, M.A.R.B. Anticancer Peptide SVS-1: Efficacy Precedes Membrane Neutralization. Biochemistry 2012, 51, 6263–6265. [Google Scholar] [CrossRef][Green Version]
- Sinthuvanich, C.; Veiga, A.S.; Gupta, K.; Gaspar, D.; Blumenthal, R.; Schneider, J.P. Anticancer β-Hairpin Peptides: Membrane-Induced Folding Triggers Activity. J. Am. Chem. Soc. 2012, 134, 6210–6217. [Google Scholar] [CrossRef] [PubMed]
- Giljohann, D.A.; Seferos, D.S.; Daniel, W.L.; Massich, M.D.; Patel, P.C.; Mirkin, C.A. Gold Nanoparticles for Biology and Medicine. Angew. Chem. Int. Ed. Engl. 2010, 49, 3280–3294. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.C.; Giljohann, D.A.; Daniel, W.L.; Zheng, D.; Prigodich, A.E.; Mirkin, C.A. Scavenger Receptors Mediate Cellular Uptake of Polyvalent Oligonucleotide-Functionalized Gold Nanoparticles. Bioconjug. Chem. 2010, 21, 2250–2256. [Google Scholar] [CrossRef] [PubMed]
- McIntosh, C.M.; Esposito, E.A., 3rd; Boal, A.K.; Simard, J.M.; Martin, C.T.; Rotello, V.M. Inhibition of DNA Transcription Using Cationic Mixed Monolayer Protected Gold Clusters. J. Am. Chem. Soc. 2001, 123, 7626–7629. [Google Scholar] [CrossRef]
- Sandhu, K.K.; McIntosh, C.M.; Simard, J.M.; Smith, S.W.; Rotello, V.M. Gold Nanoparticle-Mediated Transfection of Mammalian Cells. Bioconjug. Chem. 2002, 13, 3–6. [Google Scholar] [CrossRef]
- Ding, Y.; Jiang, Z.; Saha, K.; Kim, C.S.; Kim, S.T.; Landis, R.F.; Rotello, V.M. Gold Nanoparticles for Nucleic Acid Delivery. Mol. Ther. 2014, 22, 1075–1083. [Google Scholar] [CrossRef]
- Kunoh, T.; Takeda, M.; Matsumoto, S.; Suzuki, I.; Takano, M.; Kunoh, H.; Takada, J. Green Synthesis of Gold Nanoparticles Coupled with Nucleic Acid Oxidation. ACS Sustain. Chem. Eng. 2018, 6, 364–373. [Google Scholar] [CrossRef]
- Labala, S.; Mandapalli, P.K.; Kurumaddali, A.; Venuganti, V.V.K. Layer-by-Layer Polymer Coated Gold Nanoparticles for Topical Delivery of Imatinib Mesylate to Treat Melanoma. Mol. Pharm. 2015, 12, 878–888. [Google Scholar] [CrossRef] [PubMed]
- Labala, S.; Jose, A.; Chawla, S.R.; Khan, M.S.; Bhatnagar, S.; Kulkarni, O.P.; Venuganti, V.V.K. Effective Melanoma Cancer Suppression by Iontophoretic Co-Delivery of STAT3 siRNA and Imatinib Using Gold Nanoparticles. Int. J. Pharm. 2017, 525, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Kwong, L.N.; Davies, M.A. Targeted Therapy for Melanoma: Rational Combinatorial Approaches. Oncogene 2014, 33, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Deng, R.; Ji, B.; Yu, H.; Bao, W.; Yang, Z.; Yu, Y.; Cui, Y.; Du, Y.; Song, M.; Liu, S.; et al. Multifunctional Gold Nanoparticles Overcome MicroRNA Regulatory Network Mediated-Multidrug Resistant Leukemia. Sci. Rep. 2019, 9, 5348. [Google Scholar] [CrossRef]
- Lynn, R.C.; Poussin, M.; Kalota, A.; Feng, Y.; Low, P.S.; Dimitrov, D.S.; Powell, D.J., Jr. Targeting of Folate Receptor β on Acute Myeloid Leukemia Blasts with Chimeric Antigen Receptor-Expressing T Cells. Blood 2015, 125, 3466–3476. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Zhao, Z.; Liu, T.; Li, X.; Hu, X.; Wei, X.; Zhang, X.; Tan, W. Smart Human-Serum-Albumin-As O Nanodrug with Self-Amplified Folate Receptor-Targeting Ability for Chronic Myeloid Leukemia Treatment. Angew. Chem. Int. Ed. Engl. 2017, 56, 10845–10849. [Google Scholar] [CrossRef]
- Shang, Y.; Zhang, Z.; Liu, Z.; Feng, B.; Ren, G.; Li, K.; Zhou, L.; Sun, Y.; Li, M.; Zhou, J.; et al. miR-508-5p Regulates Multidrug Resistance of Gastric Cancer by Targeting ABCB1 and ZNRD1. Oncogene 2014, 33, 3267–3276. [Google Scholar] [CrossRef]
- Zhao, X.; Yang, L.; Hu, J.; Ruan, J. miR-138 Might Reverse Multidrug Resistance of Leukemia Cells. Leuk. Res. 2010, 34, 1078–1082. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Choi, K.-J.; Moon, S.U.; Kim, S. Theragnosis-Based Combined Cancer Therapy Using Doxorubicin-Conjugated microRNA-221 Molecular Beacon. Biomaterials 2016, 74, 109–118. [Google Scholar] [CrossRef]
- Shiao, Y.-S.; Chiu, H.-H.; Wu, P.-H.; Huang, Y.-F. Aptamer-Functionalized Gold Nanoparticles as Photoresponsive Nanoplatform for Co-Drug Delivery. ACS Appl. Mater. Interfaces 2014, 6, 21832–21841. [Google Scholar] [CrossRef]
- Xiang, D.; Shigdar, S.; Qiao, G.; Wang, T.; Kouzani, A.Z.; Zhou, S.-F.; Kong, L.; Li, Y.; Pu, C.; Duan, W. Nucleic Acid Aptamer-Guided Cancer Therapeutics and Diagnostics: The next Generation of Cancer Medicine. Theranostics 2015, 5, 23–42. [Google Scholar] [CrossRef]
- Saravanakumar, K.; Sathiyaseelan, A.; Mariadoss, A.V.A.; Hu, X.; Venkatachalam, K.; Wang, M.-H. Nucleolin Targeted Delivery of Aptamer Tagged Trichoderma Derived Crude Protein Coated Gold Nanoparticles for Improved Cytotoxicity in Cancer Cells. Process. Biochem. 2021, 102, 325–332. [Google Scholar] [CrossRef]
- Shaabani, E.; Sharifiaghdam, M.; de Keersmaecker, H.; de Rycke, R.; de Smedt, S.; Faridi-Majidi, R.; Braeckmans, K.; Fraire, J.C. Layer by Layer Assembled Chitosan-Coated Gold Nanoparticles for Enhanced siRNA Delivery and Silencing. Int. J. Mol. Sci. 2021, 22, 831. [Google Scholar] [CrossRef] [PubMed]
- Sreelakshmi, C.; Goel, N.; Datta, K.K.R.; Addlagatta, A.; Ummanni, R.; Reddy, B.V.S. Green Synthesis of Curcumin Capped Gold Nanoparticles and Evaluation of Their Cytotoxicity. Nanosci. Nanotechnol. Lett. 2013, 5, 1258–1265. [Google Scholar] [CrossRef]
- Bertolino, V.; Cavallaro, G.; Lazzara, G.; Merli, M.; Milioto, S.; Parisi, F.; Sciascia, L. Effect of the Biopolymer Charge and the Nanoclay Morphology on Nanocomposite Materials. Ind. Eng. Chem. Res. 2016, 55, 7373–7380. [Google Scholar] [CrossRef]
- Bertolino, V.; Cavallaro, G.; Lazzara, G.; Milioto, S.; Parisi, F. Biopolymer-Targeted Adsorption onto Halloysite Nanotubes in Aqueous Media. Langmuir 2017, 33, 3317–3323. [Google Scholar] [CrossRef]
- Deljoo, S.; Rabiee, N.; Rabiee, M. Curcumin-Hybrid Nanoparticles in Drug Delivery System (Review). Asian J. Nanosci. Mater. 2019, 2, 66–91. [Google Scholar] [CrossRef]
- Wang, F.; Wang, Y.-C.; Dou, S.; Xiong, M.-H.; Sun, T.-M.; Wang, J. Doxorubicin-Tethered Responsive Gold Nanoparticles Facilitate Intracellular Drug Delivery for Overcoming Multidrug Resistance in Cancer Cells. ACS Nano 2011, 5, 3679–3692. [Google Scholar] [CrossRef]
- Ruan, S.; Hu, C.; Tang, X.; Cun, X.; Xiao, W.; Shi, K.; He, Q.; Gao, H. Increased Gold Nanoparticle Retention in Brain Tumors by in Situ Enzyme-Induced Aggregation. ACS Nano 2016, 10, 10086–10098. [Google Scholar] [CrossRef]
- Mats, L.; Logue, F.; Oleschuk, R.D. “Particle-Free” Magnetic Actuation of Droplets on Superhydrophobic Surfaces Using Dissolved Paramagnetic Salts. Anal. Chem. 2016, 88, 9486–9494. [Google Scholar] [CrossRef]
- Suarasan, S.; Focsan, M.; Potara, M.; Soritau, O.; Florea, A.; Maniu, D.; Astilean, S. Doxorubicin-Incorporated Nanotherapeutic Delivery System Based on Gelatin-Coated Gold Nanoparticles: Formulation, Drug Release, and Multimodal Imaging of Cellular Internalization. ACS Appl. Mater. Interfaces 2016, 8, 22900–22913. [Google Scholar] [CrossRef]
- Ou, Y.-C.; Webb, J.A.; Faley, S.; Shae, D.; Talbert, E.M.; Lin, S.; Cutright, C.C.; Wilson, J.T.; Bellan, L.M.; Bardhan, R. Gold Nanoantenna-Mediated Photothermal Drug Delivery from Thermosensitive Liposomes in Breast Cancer. ACS Omega 2016, 1, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Wang, G.; Alves, C.S.; Tomás, H.; Xiong, Z.; Shen, M.; Rodrigues, J.; Shi, X. Multifunctional Dendrimer-Entrapped Gold Nanoparticles Conjugated with Doxorubicin for pH-Responsive Drug Delivery and Targeted Computed Tomography Imaging. Langmuir 2018, 34, 12428–12435. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.-Q.; Liu, L.-N.; Du, Y.-Z.; Yuan, H. Synthesis and Antitumor Activity of Doxorubicin Conjugated Stearic Acid-G-Chitosan Oligosaccharide Polymeric Micelles. Biomaterials 2009, 30, 6955–6963. [Google Scholar] [CrossRef]
- Shen, W.C.; Ryser, H.J. Cis-Aconityl Spacer between Daunomycin and Macromolecular Carriers: A Model of pH-Sensitive Linkage Releasing Drug from a Lysosomotropic Conjugate. Biochem. Biophys. Res. Commun. 1981, 102, 1048–1054. [Google Scholar] [CrossRef]
- Liu, H.; Wang, H.; Xu, Y.; Shen, M.; Zhao, J.; Zhang, G.; Shi, X. Synthesis of PEGylated Low Generation Dendrimer-Entrapped Gold Nanoparticles for CT Imaging Applications. Nanoscale 2014, 6, 4521–4526. [Google Scholar] [CrossRef] [PubMed]
- Peng, C.; Zheng, L.; Chen, Q.; Shen, M.; Guo, R.; Wang, H.; Cao, X.; Zhang, G.; Shi, X. PEGylated Dendrimer-Entrapped Gold Nanoparticles for in Vivo Blood Pool and Tumor Imaging by Computed Tomography. Biomaterials 2012, 33, 1107–1119. [Google Scholar] [CrossRef]
- Khutale, G.V.; Casey, A. Synthesis and Characterization of a Multifunctional Gold-Doxorubicin Nanoparticle System for pH Triggered Intracellular Anticancer Drug Release. Eur. J. Pharm. Biopharm. 2017, 119, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Mallick, A.; More, P.; Ghosh, S.; Chippalkatti, R.; Chopade, B.A.; Lahiri, M.; Basu, S. Dual Drug Conjugated Nanoparticle for Simultaneous Targeting of Mitochondria and Nucleus in Cancer Cells. ACS Appl. Mater. Interfaces 2015, 7, 7584–7598. [Google Scholar] [CrossRef] [PubMed]
- Venkatesan, R.; Pichaimani, A.; Hari, K.; Balasubramanian, P.K.; Kulandaivel, J.; Premkumar, K. Doxorubicin Conjugated Gold Nanorods: A Sustained Drug Delivery Carrier for Improved Anticancer Therapy. J. Mater. Chem. B Mater. Biol. Med. 2013, 1, 1010–1018. [Google Scholar] [CrossRef] [PubMed]
- Rabiee, N.; Ahmadi, S.; Arab, Z.; Bagherzadeh, M.; Safarkhani, M.; Nasseri, B.; Rabiee, M.; Tahriri, M.; Webster, T.J.; Tayebi, L. Aptamer Hybrid Nanocomplexes as Targeting Components for Antibiotic/Gene Delivery Systems and Diagnostics: A Review. Int. J. Nanomed. 2020, 15, 4237–4256. [Google Scholar] [CrossRef]
- Ahmadi Nasab, N.; Hassani Kumleh, H.; Beygzadeh, M.; Teimourian, S.; Kazemzad, M. Delivery of Curcumin by a pH-Responsive Chitosan Mesoporous Silica Nanoparticles for Cancer Treatment. Artif. Cells Nanomed. Biotechnol. 2018, 46, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Fan, Z.; Li, Y.; Zhang, Y.; Yu, F.; Su, G.; Xie, L.; Hou, Z. Design of pH-Sensitive Methotrexate Prodrug-Targeted Curcumin Nanoparticles for Efficient Dual-Drug Delivery and Combination Cancer Therapy. Int. J. Nanomed. 2018, 13, 1381–1398. [Google Scholar] [CrossRef]
- Yan, J.; Wang, Y.; Zhang, X.; Liu, S.; Tian, C.; Wang, H. Targeted Nanomedicine for Prostate Cancer Therapy: Docetaxel and Curcumin Co-Encapsulated Lipid-Polymer Hybrid Nanoparticles for the Enhanced Anti-Tumor Activity in Vitro and in Vivo. Drug Deliv. 2016, 23, 1757–1762. [Google Scholar] [CrossRef]
- Rao, K.M.; Kumar, A.; Suneetha, M.; Han, S.S. pH and near-Infrared Active; Chitosan-Coated Halloysite Nanotubes Loaded with Curcumin-Au Hybrid Nanoparticles for Cancer Drug Delivery. Int. J. Biol. Macromol. 2018, 112, 119–125. [Google Scholar] [CrossRef]
- Yang, Q.; Peng, J.; Xiao, Y.; Li, W.; Tan, L.; Xu, X.; Qian, Z. Porous Au@Pt Nanoparticles: Therapeutic Platform for Tumor Chemo-Photothermal Co-Therapy and Alleviating Doxorubicin-Induced Oxidative Damage. ACS Appl. Mater. Interfaces 2018, 10, 150–164. [Google Scholar] [CrossRef]
- Norouzi, H.; Khoshgard, K.; Akbarzadeh, F. In Vitro Outlook of Gold Nanoparticles in Photo-Thermal Therapy: A Literature Review. Lasers Med. Sci. 2018, 33, 917–926. [Google Scholar] [CrossRef]
- Zhang, D.; Wu, T.; Qin, X.; Qiao, Q.; Shang, L.; Song, Q.; Yang, C.; Zhang, Z. Intracellularly Generated Immunological Gold Nanoparticles for Combinatorial Photothermal Therapy and Immunotherapy against Tumor. Nano Lett. 2019, 19, 6635–6646. [Google Scholar] [CrossRef]
- Riley, R.S.; Day, E.S. Gold Nanoparticle-Mediated Photothermal Therapy: Applications and Opportunities for Multimodal Cancer Treatment. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2017, 9. [Google Scholar] [CrossRef]
- Cheng, X.; Sun, R.; Yin, L.; Chai, Z.; Shi, H.; Gao, M. Light-Triggered Assembly of Gold Nanoparticles for Photothermal Therapy and Photoacoustic Imaging of Tumors In Vivo. Adv. Mater. 2017, 29. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.R.K.; Wu, Y.; El-Sayed, M.A. Gold-Nanoparticle-Assisted Plasmonic Photothermal Therapy Advances toward Clinical Application. J. Phys. Chem. C Nanomater. Interfaces 2019, 123, 15375–15393. [Google Scholar] [CrossRef]
- Liu, Y.; Crawford, B.M.; Vo-Dinh, T. Gold Nanoparticles-Mediated Photothermal Therapy and Immunotherapy. Immunotherapy 2018, 10, 1175–1188. [Google Scholar] [CrossRef]
- Yang, W.; Liang, H.; Ma, S.; Wang, D.; Huang, J. Gold Nanoparticle Based Photothermal Therapy: Development and Application for Effective Cancer Treatment. Sustain. Mater. Technol. 2019, 22, e00109. [Google Scholar] [CrossRef]
- Sun, M.; Peng, D.; Hao, H.; Hu, J.; Wang, D.; Wang, K.; Liu, J.; Guo, X.; Wei, Y.; Gao, W. Thermally Triggered in Situ Assembly of Gold Nanoparticles for Cancer Multimodal Imaging and Photothermal Therapy. ACS Appl. Mater. Interfaces 2017, 9, 10453–10460. [Google Scholar] [CrossRef]
- Kim, H.S.; Lee, D.Y. Photothermal Therapy with Gold Nanoparticles as an Anticancer Medication. J. Pharm. Investig. 2017, 47, 19–26. [Google Scholar] [CrossRef]
- Beik, J.; Asadi, M.; Khoei, S.; Laurent, S.; Abed, Z.; Mirrahimi, M.; Farashahi, A.; Hashemian, R.; Ghaznavi, H.; Shakeri-Zadeh, A. Simulation-Guided Photothermal Therapy Using MRI-Traceable Iron Oxide-Gold Nanoparticle. J. Photochem. Photobiol. B 2019, 199, 111599. [Google Scholar] [CrossRef] [PubMed]
- Neshastehriz, A.; Tabei, M.; Maleki, S.; Eynali, S.; Shakeri-Zadeh, A. Photothermal Therapy Using Folate Conjugated Gold Nanoparticles Enhances the Effects of 6MV X-Ray on Mouth Epidermal Carcinoma Cells. J. Photochem. Photobiol. B 2017, 172, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Du, B.; Huang, Y.; Yu, M.; Zheng, J. Cancer Photothermal Therapy with ICG-Conjugated Gold Nanoclusters. Bioconjug. Chem. 2020, 31, 1522–1528. [Google Scholar] [CrossRef]
- Kim, H.S.; Lee, D.Y. Near-Infrared-Responsive Cancer Photothermal and Photodynamic Therapy Using Gold Nanoparticles. Polymers 2018, 10, 961. [Google Scholar] [CrossRef]
- Sun, Z.; Zhang, Y.; Yu, H.; Yan, C.; Liu, Y.; Hong, S.; Tao, H.; Robertson, A.W.; Wang, Z.; Pádua, A.A.H. New Solvent-Stabilized Few-Layer Black Phosphorus for Antibacterial Applications. Nanoscale 2018, 10, 12543–12553. [Google Scholar] [CrossRef]
- Wang, X.; Shao, J.; Abd El Raouf, M.; Xie, H.; Huang, H.; Wang, H.; Chu, P.K.; Yu, X.-F.; Yang, Y.; AbdEl-Aal, A.M.; et al. Near-Infrared Light-Triggered Drug Delivery System Based on Black Phosphorus for in Vivo Bone Regeneration. Biomaterials 2018, 179, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Liu, Z.; Li, Y.; Hou, Y.; Fei, X.; Su, C.; Wang, S.; Zhuang, Z.; Guo, Z. Facile Synthesis of Black Phosphorus-Au Nanocomposites for Enhanced Photothermal Cancer Therapy and Surface-Enhanced Raman Scattering Analysis. Biomater. Sci. 2017, 5, 2048–2055. [Google Scholar] [CrossRef] [PubMed]
- Moradi, S.; Mokhtari-Dizaji, M.; Ghassemi, F.; Sheibani, S.; Amoli, F.A. The Effect of Ultrasound Hyperthermia with Gold Nanoparticles on Retinoblastoma Y79 Cells. Gold Bull. 2020, 53, 111–120. [Google Scholar] [CrossRef]
- Katifelis, H.; Mukha, I.; Lyberopoulou, A.; Vityuk, N.; Grammatikaki, M.; Pylypchuk, I.; Lazaris, F.; Storozhuk, L.; Kouloulias, V.; Gazouli, M. In Vitro Effect of Hyperthermic Ag and Au Fe3O4 Nanoparticles in Cancer Cells. Beilstein Arch. 2019, 2019, 101. [Google Scholar]
- Shanei, A.; Sazgarnia, A. An Overview of Therapeutic Applications of Ultrasound Based on Synergetic Effects with Gold Nanoparticles and Laser Excitation. Iran. J. Basic Med. Sci. 2019, 22, 848–855. [Google Scholar] [CrossRef]
- Canavese, G.; Ancona, A.; Racca, L.; Canta, M.; Dumontel, B.; Barbaresco, F.; Limongi, T.; Cauda, V. Nanoparticle-Assisted Ultrasound: A Special Focus on Sonodynamic Therapy against Cancer. Chem. Eng. J. 2018, 340, 155–172. [Google Scholar] [CrossRef]
- Beik, J.; Khademi, S.; Attaran, N.; Sarkar, S.; Shakeri-Zadeh, A.; Ghaznavi, H.; Ghadiri, H. A Nanotechnology-Based Strategy to Increase the Efficiency of Cancer Diagnosis and Therapy: Folate-Conjugated Gold Nanoparticles. Curr. Med. Chem. 2017, 24, 4399–4416. [Google Scholar] [CrossRef]
- Izadifar, Z.; Izadifar, Z.; Chapman, D.; Babyn, P. An Introduction to High Intensity Focused Ultrasound: Systematic Review on Principles, Devices, and Clinical Applications. J. Clin. Med. Res. 2020, 9, 460. [Google Scholar] [CrossRef]
- Kennedy, J.E. High-Intensity Focused Ultrasound in the Treatment of Solid Tumours. Nat. Rev. Cancer 2005, 5, 321–327. [Google Scholar] [CrossRef]
- Yu, T.; Wang, Z.; Jiang, S. Potentiation of Cytotoxicity of Adriamycin on Human Ovarian Carcinoma Cell Line 3AO by Low-Level Ultrasound. Ultrasonics 2001, 39, 307–309. [Google Scholar] [CrossRef]
- Yu, T.; Wang, Z.; Mason, T.J. A Review of Research into the Uses of Low Level Ultrasound in Cancer Therapy. Ultrason. Sonochem. 2004, 11, 95–103. [Google Scholar] [CrossRef]
- Marmottant, P.; Hilgenfeldt, S. Controlled Vesicle Deformation and Lysis by Single Oscillating Bubbles. Nature 2003, 423, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Tang, H.; Wang, C.C.J.; Blankschtein, D.; Langer, R. An Investigation of the Role of Cavitation in Low-Frequency Ultrasound-Mediated Transdermal Drug Transport. Pharm. Res. 2002, 19, 1160–1169. [Google Scholar] [CrossRef] [PubMed]
- Barnett, S.B.; ter Haar, G.R.; Ziskin, M.C.; Nyborg, W.L.; Maeda, K.; Bang, J. Current Status of Research on Biophysical Effects of Ultrasound. Ultrasound Med. Biol. 1994, 20, 205–218. [Google Scholar] [CrossRef]
- Barnett, S.B. Conclusions and Recommendations on Thermal and Non-Thermal Mechanisms for Biological Effects of Ultrasound; CSIRO Research Publications Repository: Melbourne, Australia, 1996. [Google Scholar]
- Tuziuti, T.; Yasui, K.; Sivakumar, M.; Iida, Y.; Miyoshi, N. Correlation between Acoustic Cavitation Noise and Yield Enhancement of Sonochemical Reaction by Particle Addition. J. Phys. Chem. A 2005, 109, 4869–4872. [Google Scholar] [CrossRef]
- Farny, C.H.; Wu, T.; Holt, R.G.; Murray, T.W.; Roy, R.A. Nucleating Cavitation from Laser-Illuminated Nano-Particles. Acoust. Res. Lett. Online 2005, 6, 138–143. [Google Scholar] [CrossRef]
- Victor, E.G.; Silveira, P.C.L.; Possato, J.C.; da Rosa, G.L.; Munari, U.B.; de Souza, C.T.; Pinho, R.A.; da Silva, L.; Streck, E.L.; Paula, M.M.S. Pulsed ultrasound Associated with Gold Nanoparticle Gel Reduces Oxidative Stress Parameters and Expression of pro-Inflammatory Molecules in an Animal Model of Muscle Injury. J. Nanobiotechnol. 2012, 10, 11. [Google Scholar] [CrossRef]
- Serrano, A.L.; Baeza-Raja, B.; Perdiguero, E.; Jardí, M.; Muñoz-Cánoves, P. Interleukin-6 Is an Essential Regulator of Satellite Cell-Mediated Skeletal Muscle Hypertrophy. Cell Metab. 2008, 7, 33–44. [Google Scholar] [CrossRef]
- Li, Y.-P. TNF-Alpha Is a Mitogen in Skeletal Muscle. Am. J. Physiol. Cell Physiol. 2003, 285, C370–C376. [Google Scholar] [CrossRef]
- Tsai, C.-Y.; Shiau, A.-L.; Chen, S.-Y.; Chen, Y.-H.; Cheng, P.-C.; Chang, M.-Y.; Chen, D.-H.; Chou, C.-H.; Wang, C.-R.; Wu, C.-L. Amelioration of Collagen-Induced Arthritis in Rats by Nanogold. Arthritis Rheum. 2007, 56, 544–554. [Google Scholar] [CrossRef]
- Beik, J.; Abed, Z.; Shakeri-Zadeh, A.; Nourbakhsh, M.; Shiran, M.B. Evaluation of the Sonosensitizing Properties of Nano-Graphene Oxide in Comparison with Iron Oxide and Gold Nanoparticles. Phys. E Low Dimens. Syst. Nanostruct. 2016, 81, 308–314. [Google Scholar] [CrossRef]
- Aminabad, N.S.; Farshbaf, M.; Akbarzadeh, A. Recent Advances of Gold Nanoparticles in Biomedical Applications: State of the Art. Cell Biochem. Biophys. 2019, 77, 123–137. [Google Scholar] [CrossRef] [PubMed]
- Mieszawska, A.J.; Mulder, W.J.M.; Fayad, Z.A.; Cormode, D.P. Multifunctional Gold Nanoparticles for Diagnosis and Therapy of Disease. Mol. Pharm. 2013, 10, 831–847. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, M.; Ferreira Carlos, F.; Pedrosa, P.; Lopez, A.; Baptista, P.V. Gold Nanoparticles for Diagnostics: Advances towards Points of Care. Diagnostics 2016, 6, 43. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.W.; So, P.T.C.; Dasari, R.R.; Lim, D.-K. High Resolution Live Cell Raman Imaging Using Subcellular Organelle-Targeting SERS-Sensitive Gold Nanoparticles with Highly Narrow Intra-Nanogap. Nano Lett. 2015, 15, 1766–1772. [Google Scholar] [CrossRef]
- Kumar, S.; Kumar, S.; Tiwari, S.; Augustine, S.; Srivastava, S.; Yadav, B.K.; Malhotra, B.D. Highly Sensitive Protein Functionalized Nanostructured Hafnium Oxide Based Biosensing Platform for Non-Invasive Oral Cancer Detection. Sens. Actuators B Chem. 2016, 235, 1–10. [Google Scholar] [CrossRef]
- Fleischmann, M.; Hendra, P.J.; McQuillan, A.J. Raman Spectra of Pyridine Adsorbed at a Silver Electrode. Chem. Phys. Lett. 1974, 26, 163–166. [Google Scholar] [CrossRef]
- Feng, S.; Chen, R.; Lin, J.; Pan, J.; Wu, Y.; Li, Y.; Chen, J.; Zeng, H. Gastric Cancer Detection Based on Blood Plasma Surface-Enhanced Raman Spectroscopy Excited by Polarized Laser Light. Biosens. Bioelectron. 2011, 26, 3167–3174. [Google Scholar] [CrossRef] [PubMed]
- Yan, B.; Li, B.; Wen, Z.; Luo, X.; Xue, L.; Li, L. Label-Free Blood Serum Detection by Using Surface-Enhanced Raman Spectroscopy and Support Vector Machine for the Preoperative Diagnosis of Parotid Gland Tumors. BMC Cancer 2015, 15, 650. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Yan, B.; Xue, L.; Li, Y.; Luo, X.; Ji, P. Surface-Enhanced Raman Spectroscopy of Blood Serum Based on Gold Nanoparticles for the Diagnosis of the Oral Squamous Cell Carcinoma. Lipids Health Dis. 2017, 16, 73. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Qu, Q.; Zhao, Y.; Luo, Z.; Zhao, Y.; Ng, K.W.; Zhao, Y. Graphene Oxide Wrapped Gold Nanoparticles for Intracellular Raman Imaging and Drug Delivery. J. Mater. Chem. B Mater. Biol. Med. 2013, 1, 6495–6500. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Chen, X. Gold Nanoparticles for Photoacoustic Imaging. Nanomedicine 2015, 10, 299–320. [Google Scholar] [CrossRef]
- Song, J.; Kim, J.; Hwang, S.; Jeon, M.; Jeong, S.; Kim, C.; Kim, S. “Smart” Gold Nanoparticles for Photoacoustic Imaging: An Imaging Contrast Agent Responsive to the Cancer Microenvironment and Signal Amplification via pH-Induced Aggregation. Chem. Commun. 2016, 52, 8287–8290. [Google Scholar] [CrossRef]
- Sun, I.-C.; Dumani, D.; Emelianov, S.Y. Ultrasound-Guided Photoacoustic Imaging of Lymph Nodes with Biocompatible Gold Nanoparticles as a Novel Contrast Agent (Conference Presentation). In Proceedings of the Colloidal Nanoparticles for Biomedical Applications XII, San Francisco, CA, USA, 28 January–2 February 2017; Liang, X.-J., Parak, W.J., Osiński, M., Eds.; SPIE: Bellingham, WA, USA, 2017. [Google Scholar]
- Jin, H.-Y.; Li, D.-W.; Zhang, N.; Gu, Z.; Long, Y.-T. Analyzing Carbohydrate-Protein Interaction Based on Single Plasmonic Nanoparticle by Conventional Dark Field Microscopy. ACS Appl. Mater. Interfaces 2015, 7, 12249–12253. [Google Scholar] [CrossRef] [PubMed]
- Qian, W.; Huang, X.; Kang, B.; El-Sayed, M.A. Dark-Field Light Scattering Imaging of Living Cancer Cell Component from Birth through Division Using Bioconjugated Gold Nanoprobes. J. Biomed. Opt. 2010, 15, 046025. [Google Scholar] [CrossRef]
- Ma, J.; Liu, Y.; Gao, P.F.; Zou, H.Y.; Huang, C.Z. Precision Improvement in Dark-Field Microscopy Imaging by Using Gold Nanoparticles as an Internal Reference: A Combined Theoretical and Experimental Study. Nanoscale 2016, 8, 8729–8736. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; He, Y.; Liu, H.; Luo, Y.; Shen, M.; Xia, J.; Shi, X. Targeted CT Imaging of Human Hepatocellular Carcinoma Using Low-Generation Dendrimer-Entrapped Gold Nanoparticles Modified with Lactobionic Acid. J. Mater. Chem. B Mater. Biol. Med. 2015, 3, 286–295. [Google Scholar] [CrossRef]
- Meir, R.; Shamalov, K.; Betzer, O.; Motiei, M.; Horovitz-Fried, M.; Yehuda, R.; Popovtzer, A.; Popovtzer, R.; Cohen, C.J. Nanomedicine for Cancer Immunotherapy: Tracking Cancer-Specific T-Cells in Vivo with Gold Nanoparticles and CT Imaging. ACS Nano 2015, 9, 6363–6372. [Google Scholar] [CrossRef]
- Kim, J.; Lee, N.; Hyeon, T. Recent Development of Nanoparticles for Molecular Imaging. Philos. Trans. A Math. Phys. Eng. Sci. 2017, 375. [Google Scholar] [CrossRef]
- Na, H.B.; Song, I.C.; Hyeon, T. Inorganic Nanoparticles for MRI Contrast Agents. Adv. Mater. 2009, 21, 2133–2148. [Google Scholar] [CrossRef]
- Huang, J.-Y.; Lin, H.-T.; Chen, T.-H.; Chen, C.-A.; Chang, H.-T.; Chen, C.-F. Signal Amplified Gold Nanoparticles for Cancer Diagnosis on Paper-Based Analytical Devices. ACS Sens. 2018, 3, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Chen, Y.; Jiang, Y.; Ju, H. Polyadenine-Modulated DNA Conformation Monitored by Surface-Enhanced Raman Scattering (SERS) on Multibranched Gold Nanoparticles and Its Sensing Application. Chemistry 2017, 23, 9332–9337. [Google Scholar] [CrossRef] [PubMed]
- Cheung-Lau, J.C.; Liu, D.; Pulsipher, K.W.; Liu, W.; Dmochowski, I.J. Engineering a Well-Ordered, Functional Protein-Gold Nanoparticle Assembly. J. Inorg. Biochem. 2014, 130, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.K.; Vaze, A.; Shen, M.; Rusling, J.F. High-Throughput Electrochemical Microfluidic Immunoarray for Multiplexed Detection of Cancer Biomarker Proteins. ACS Sens. 2016, 1, 1036–1043. [Google Scholar] [CrossRef]
- Saeed, A.A.; Sánchez, J.L.A.; O’Sullivan, C.K.; Abbas, M.N. DNA Biosensors Based on Gold Nanoparticles-Modified Graphene Oxide for the Detection of Breast Cancer Biomarkers for Eary Diagnosis. Bioelectrochemistry 2017, 118, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Saha, K.; Agasti, S.S.; Kim, C.; Li, X.; Rotello, V.M. Gold Nanoparticles in Chemical and Biological Sensing. Chem. Rev. 2012, 112, 2739–2779. [Google Scholar] [CrossRef]
- Zeng, S.; Yong, K.-T.; Roy, I.; Dinh, X.-Q.; Yu, X.; Luan, F. A Review on Functionalized Gold Nanoparticles for Biosensing Applications. Plasmonics 2011, 6, 491–506. [Google Scholar] [CrossRef]
- Pingarrón, J.M.; Yáñez-Sedeño, P.; González-Cortés, A. Gold Nanoparticle-Based Electrochemical Biosensors. Electrochim. Acta 2008, 53, 5848–5866. [Google Scholar] [CrossRef]
- Meola, A.; Rao, J.; Chaudhary, N.; Sharma, M.; Chang, S.D. Gold Nanoparticles for Brain Tumor Imaging: A Systematic Review. Front. Neurol. 2018, 9, 328. [Google Scholar] [CrossRef] [PubMed]
- Bahadar, H.; Maqbool, F.; Niaz, K.; Abdollahi, M. Toxicity of Nanoparticles and an Overview of Current Experimental Models. Iran. Biomed. J. 2016, 20, 1–11. [Google Scholar] [CrossRef]
- Kim, D.-Y.; Kim, M.; Shinde, S.; Sung, J.-S.; Ghodake, G. Cytotoxicity and Antibacterial Assessment of Gallic Acid Capped Gold Nanoparticles. Colloids Surf. B Biointerfaces 2017, 149, 162–167. [Google Scholar] [CrossRef]
- Bhamidipati, M.; Fabris, L. Multiparametric Assessment of Gold Nanoparticle Cytotoxicity in Cancerous and Healthy Cells: The Role of Size, Shape, and Surface Chemistry. Bioconjug. Chem. 2017, 28, 449–460. [Google Scholar] [CrossRef] [PubMed]
- Albanese, A.; Walkey, C.D.; Olsen, J.B.; Guo, H.; Emili, A.; Chan, W.C.W. Secreted Biomolecules Alter the Biological Identity and Cellular Interactions of Nanoparticles. ACS Nano 2014, 8, 5515–5526. [Google Scholar] [CrossRef] [PubMed]
- Grainger, D.W.; Castner, D.G. Nanobiomaterials and Nanoanalysis: Opportunities for Improving the Science to Benefit Biomedical Technologies. Adv. Mater. 2008, 20, 867–877. [Google Scholar] [CrossRef]
- Walkey, C.D.; Olsen, J.B.; Guo, H.; Emili, A.; Chan, W.C.W. Nanoparticle Size and Surface Chemistry Determine Serum Protein Adsorption and Macrophage Uptake. J. Am. Chem. Soc. 2012, 134, 2139–2147. [Google Scholar] [CrossRef]
- Bailly, A.-L.; Correard, F.; Popov, A.; Tselikov, G.; Chaspoul, F.; Appay, R.; Al-Kattan, A.; Kabashin, A.V.; Braguer, D.; Esteve, M.-A. In Vivo Evaluation of Safety, Biodistribution and Pharmacokinetics of Laser-Synthesized Gold Nanoparticles. Sci. Rep. 2019, 9, 12890. [Google Scholar] [CrossRef]
- Wilhelm, S.; Tavares, A.J.; Dai, Q.; Ohta, S.; Audet, J.; Dvorak, H.F.; Chan, W.C.W. Analysis of Nanoparticle Delivery to Tumours. Nat. Rev. Mater. 2016, 1, 16014. [Google Scholar] [CrossRef]
- Dai, Q.; Bertleff-Zieschang, N.; Braunger, J.A.; Björnmalm, M.; Cortez-Jugo, C.; Caruso, F. Particle Targeting in Complex Biological Media. Adv. Healthc. Mater. 2018, 7, 1700575. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).