Music Therapy Self-Care Group for Parents of Preterm Infants in the Neonatal Intensive Care Unit: A Clinical Pilot Intervention
Abstract
1. Introduction
Family-Centered Care and Family-Centered Music Therapy in the NICU
2. Materials and Methods
2.1. Context and Setting
2.2. Music Therapy Self-Care Group: Procedure and Interventions
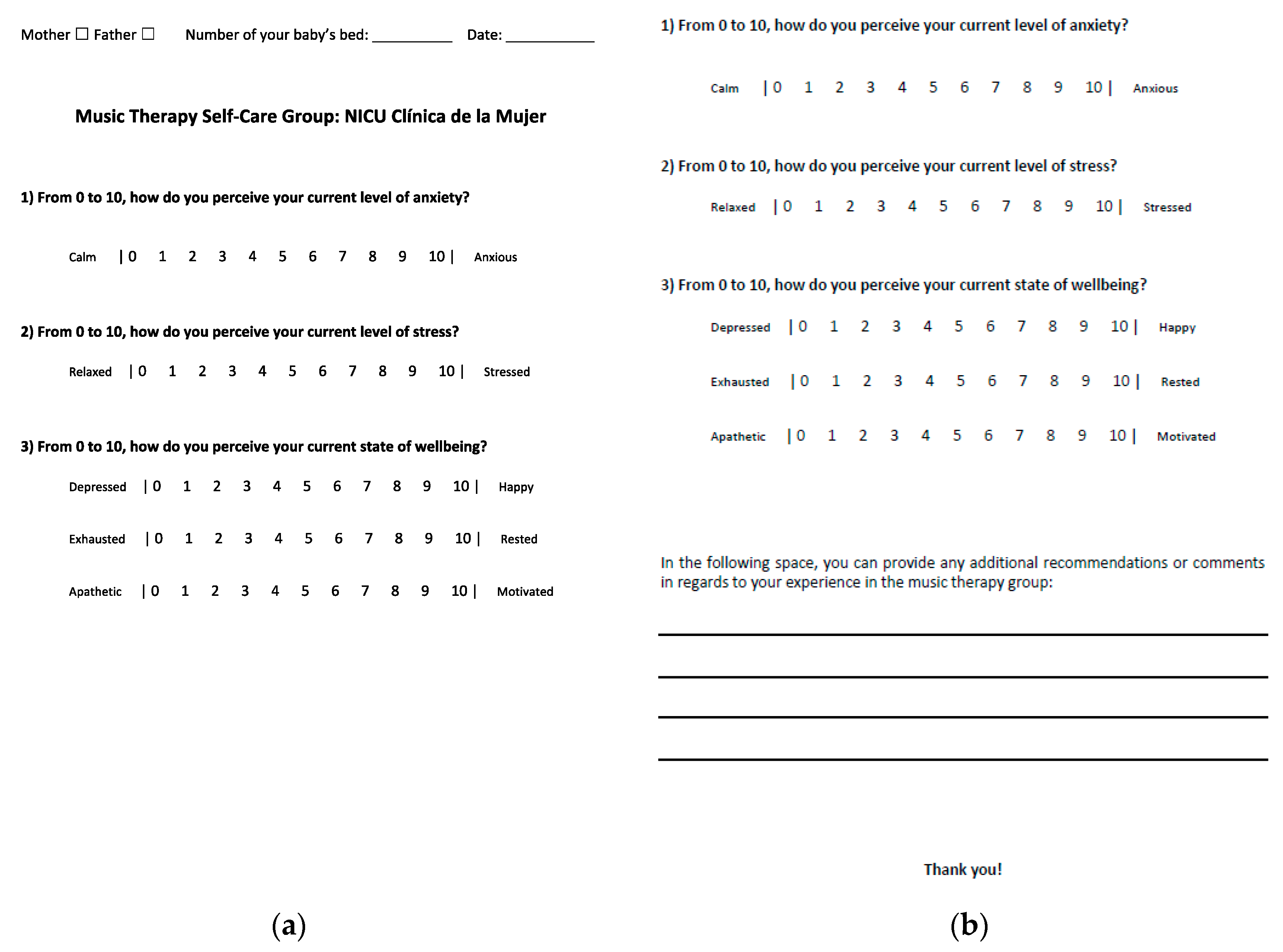
2.3. Evaluation and Measurements
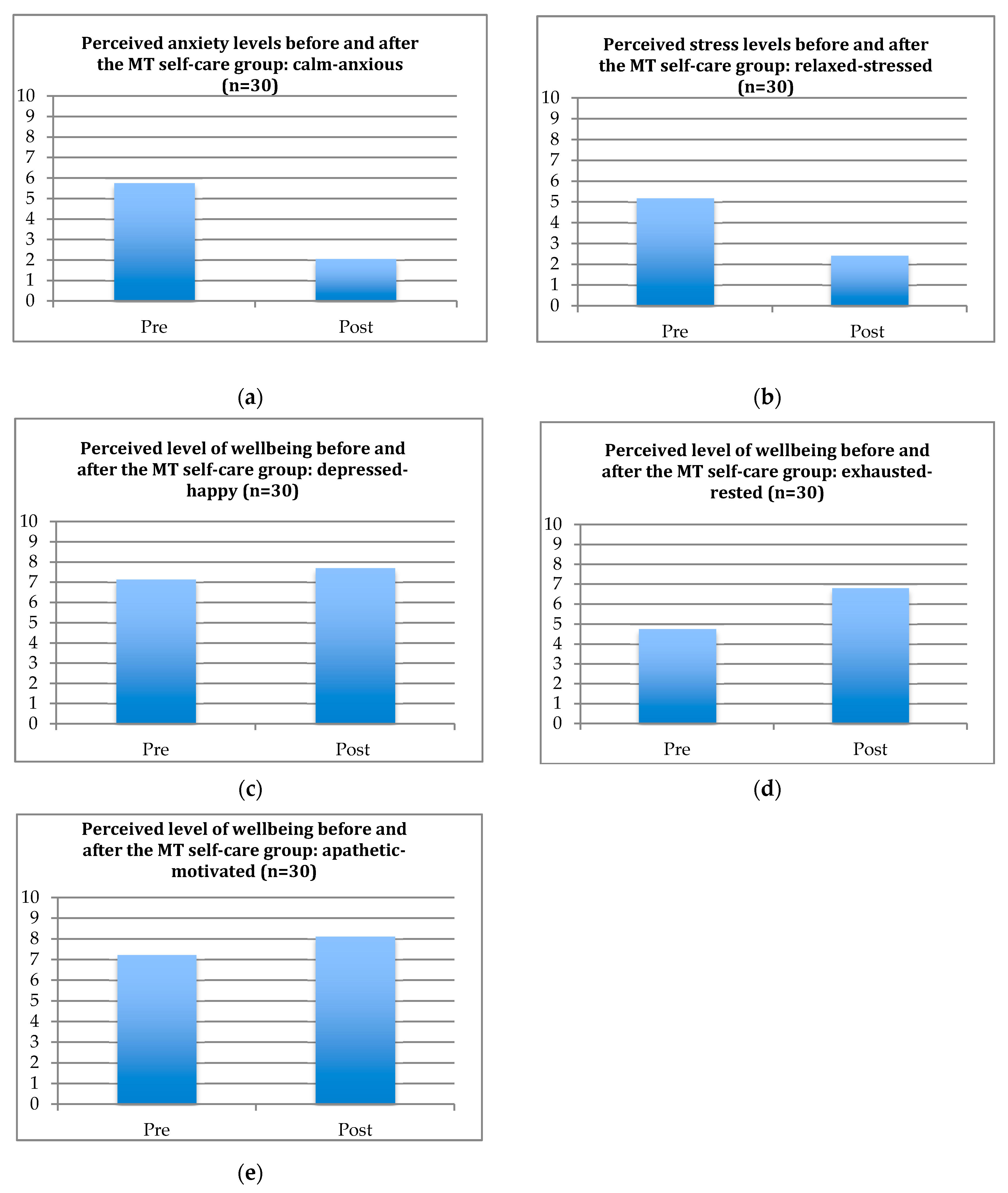
3. Results
4. Limitations
- The sessions take place in the breast milk extraction room between scheduled milk extraction time slots. Due to its size, it is currently the only available space in the NICU appropriate for group interventions. However, since breast milk extraction usually takes place continuously throughout the day, this caused difficulties with respect to the time restriction for the group on one of the days (Wednesday afternoon).
- The clinical pilot program aims to address the needs of both mothers and fathers. Bearing in mind the cultural norms, perceptions on gender roles, and employment obligations in Colombian society, there were not as many fathers present as mothers throughout the pilot program. Nonetheless, participating fathers regularly express having a positive experience with the group and encouraged that it be formalized in NICU care.
- Since mothers do not always schedule the same time slot for breast milk extraction and kangaroo care with their babies, participation in the group session was inconsistent. Some mothers joined the group several times, but others participated just once. To better assess the outcomes, it is suggested that the participants have a consistent and scheduled attendance for the music therapy self-care group.
- The music therapy team designed the NRS which was used to evaluate the clinical pilot intervention based on the experiences in clinical practice; it is not a standardized assessment tool and has not been validated. Nevertheless, it seems to be an intuitive and easily applicable tool to quickly assess some of the most important domains of parental wellbeing and the parents reported no difficulties in understanding the NRS.
5. Discussion and Conclusions
“A state of wellbeing is easily achieved with music therapy. Being in the NICU is stressful, but it becomes tolerable with this type of support.”(A participating mother)
“It is a great space because it allows us to rest and disconnect from the situation we are going through.”(A participating father)
“It is a relaxing activity. It should be done more frequently. It allows us to alleviate the stress from this situation.”(A participating mother)
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Aagard, H.; Hall, E.O.C. Mothers’ experiences of having a preterm infant in the neonatal care unit: A meta-synthesis. J. Pediatr. Nurs. 2008, 23, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Carson, C.; Redshaw, M.; Gray, R.; Quigley, M.A. Risk of psychological distress in parents of preterm children in the first year: Evidence from the UK Millennium Cohort Study. BMJ Open 2015, 5, e007942. [Google Scholar] [CrossRef] [PubMed]
- Davis, L.; Edwards, H.; Mohay, H.; Wollin, J. The impact of very premature birth on the psychological health of mothers. Early Hum. Dev. 2003, 73, 61–70. [Google Scholar] [CrossRef]
- Meijssen, D.E.; Wolf, M.J.; Koldewijn, K.; van Wassenaer, A.G.; Kok, J.H.; Van Baar, A.L. Parenting stress in mothers after very preterm birth and the effect of the Infant Behavioural Assessment and Intervention Program. Child. Care Health Dev. 2011, 37, 195. [Google Scholar] [CrossRef] [PubMed]
- Singer, L.T.; Salvator, A.; Guo, S.; Collin, M.; Lilien, L.; Baley, J. Maternal Psychological Distress and Parenting Stress After the Birth of a Very Low-Birth-Weight Infant. JAMA 1999, 281, 799–805. [Google Scholar] [CrossRef] [PubMed]
- Miles, M.S.; Funk, S.G.; Kasper, M.A. The neonatal intensive care unit environment: Sources of stress for parents. AACN Clin. Issues Crit. Care Nurs. 1991, 2, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Stefana, A.; Padovani, E.M.; Biban, P.; Lavelli, M. Experiences with their preterm babies admitted to neonatal intensive care unit: A multi-method study. J. Adv. Nurs. 2018, 74, 1090–1098. [Google Scholar] [CrossRef]
- Kersting, A.; Dorsch, M.; Wesselmann, U.; Lüdorff, K.; Witthaut, J.; Ohrmann, P.; Arolt, V. Maternal posttraumatic stress response after the birth of a very low-birth-weight infant. J. Psychosom. Res. 2004, 57, 473–476. [Google Scholar] [CrossRef]
- Jotzo, M.; Poets, C.F. Helping Parents Cope with the Trauma of Premature Birth: An Evaluation of a Trauma-Preventive Psychological Intervention. Pediatrics 2005, 115, 915–919. [Google Scholar] [CrossRef]
- Hagan, R.; Evans, S.F.; Pope, S. Preventing postnatal depression in mothers of very preterm infants: A randomised controlled trial. BJOG Int. J. Obstetr. Gynaecol. 2004, 111, 641–647. [Google Scholar] [CrossRef]
- Muller-Nix, C.; Forcada-Guex, M.; Pierrehumbert, B.; Jaunin, L.; Borghini, A.; Ansermet, F. Prematurity, maternal stress and mother-child interactions. Early Hum. Dev. 2004, 79, 145–158. [Google Scholar] [CrossRef] [PubMed]
- Whitfield, M.F. Psychosocial effects of intensive care on infants and families after discharge. Semin. Neonatol. 2003, 8, 185–193. [Google Scholar] [CrossRef]
- Mondanaro, J.F.; Ettenberger, M.; Park, L. Mars Rising: Music Therapy and the Increasing Presence of Fathers in the NICU. Music Med. 2016, 8, 96–107. [Google Scholar]
- Arockiasamy, V.; Holsti, L.; Albersheim, S. Fathers’ experiences in the neonatal intensive care unit: A search for control. Pediatrics 2008, 121, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Garten, L.; Nazary, L.; Metze, B.; Bührer, C. Pilot study of experiences and needs of 111 fathers of very low birth weight infants in a neonatal intensive care unit. J. Perinatol. 2013, 33, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Hugill, K.; Letherby, G.; Reid, T.; Lavender, T. Experiences of fathers shortly after the birth of their preterm infants. J. Obstetr. Gynecol. Neonatal Nurs. 2013, 42, 655–663. [Google Scholar] [CrossRef]
- Sloan, K.; Rowe, J.; Jones, L. Stress and coping in fathers following the birth of a preterm infant. J. Neonatal Nurs. 2008, 14, 108–115. [Google Scholar] [CrossRef]
- Ahn, Y.-M.; Kim, N.-H. Parental Perception of Neonates, Parental Stress and Education for NICU Parents. Asian Nurs. Res. 2007, 1, 199–210. [Google Scholar] [CrossRef]
- Fabiyi, C.; Rankin, K.; Norr, K.; Shapiro, N.; White-Traut, R. Anxiety among Black and Latina Mothers of Premature Infants at Social-Environmental Risk. Newborn Infant Nurs. Rev. 2012, 12, 132–140. [Google Scholar] [CrossRef]
- Turan, T.; Başbakkal, Z.; Ozbek, S. Effect of nursing interventions on stressors of parents of premature infants in neonatal intensive care unit. J. Clin. Nurs. 2008, 17, 2856–2866. [Google Scholar] [CrossRef]
- Committee on Hospital Care; American Academy of Pediatrics. Family-centered care and the pediatrician’s role. Pediatrics 2003, 112 Pt 1, 691–697. [Google Scholar] [CrossRef]
- Kuo, D.Z.; Houtrow, A.J.; Arango, P.; Kuhlthau, K.A.; Simmons, J.M.; Neff, J.M. Family-centered care: Current applications and future directions in pediatric health care. Matern. Child. Health J. 2012, 16, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Gooding, J.S.; Cooper, L.G.; Blaine, A.I.; Franck, L.S.; Howse, J.L.; Berns, S.D. Family support and family-centered care in the neonatal intensive care unit: Origins, advances, impact. Semin. Perinatol. 2011, 35, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Cooper, L.G.; Gooding, J.S.; Gallagher, J.; Sternesky, L.; Ledsky, R.; Berns, S.D. Impact of a family-centered care initiative on NICU care, staff and families. J. Perinatol. 2007, 27 (Suppl. 2), 32–37. [Google Scholar] [CrossRef] [PubMed]
- Van Riper, M. Family-provider relationships and well-being in families with preterm infants in the NICU. Heart Lung J. Crit. Care 2001, 30, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Meyer, E.C.; Coll, C.T.; Lester, B.M.; Boukydis, C.F.; McDonough, S.M.; Oh, W. Family-based intervention improves maternal psychological well-being and feeding interaction of preterm infants. Pediatrics 1994, 93, 241–246. [Google Scholar]
- Haslbeck, F.B. Music therapy for premature infants and their parents: An integrative review. Nord. J. Music Ther. 2012, 21, 203–226. [Google Scholar] [CrossRef]
- Standley, J. Music therapy research in the NICU: An updated meta-analysis. Neonatal Netw. 2012, 31, 311–316. [Google Scholar] [CrossRef]
- Bieleninik, Ł.; Ghetti, C.; Gold, C. Music Therapy for Preterm Infants and Their Parents: A Meta-analysis. Pediatrics 2016, 138. [Google Scholar] [CrossRef]
- Ettenberger, M.; Cárdenas, C.R.; Parker, M.; Odell-Miller, H. Family-centred music therapy with preterm infants and their parents in the Neonatal Intensive Care Unit (NICU) in Colombia—A mixed-methods study. Nord. J. Music Ther. 2017, 26, 207–234. [Google Scholar] [CrossRef]
- Loewy, J.; Stewart, K.; Dassler, A.-M.; Telsey, A.; Homel, P. The Effects of Music Therapy on Vital Signs, Feeding, and Sleep in Premature Infants. Pediatrics 2013, 131, 902–918. [Google Scholar] [CrossRef] [PubMed]
- Loewy, J. NICU music therapy: Song of kin as critical lullaby in research and practice. Ann. N. Y. Acad. Sci. 2015, 1337, 178–185. [Google Scholar] [CrossRef] [PubMed]
- Ettenberger, M.; Odell-Miller, H.; Cárdenas, C.; Serrano, S.; Parker, M.; Camargo Llanos, S. Music Therapy With Premature Infants and Their Caregivers in Colombia—A Mixed Methods Pilot Study Including a Randomized Trial. Voices World Forum Music Ther. 2014, 14. [Google Scholar] [CrossRef]
- Teckenberg-Jansson, P.; Huotilainen, M.; Pölkki, T.; Lipsanen, J.; Järvenpää, A.-L. Rapid effects of neonatal music therapy combined with kangaroo care on prematurely-born infants. Nord. J. Music Ther. 2011, 20, 22–42. [Google Scholar] [CrossRef]
- Standley, J.M. The effect of music-reinforced nonnutritive sucking on feeding rate of premature infants. J. Pediatr. Nurs. 2003, 18, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Vianna, M.; Barbosa, A.P.; Carvalhaes, A.S.; Cunha, A. Music therapy may increase breastfeeding rates among mothers of premature newborns: A randomized controlled trial. Jornal de Pediatria 2011, 87, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Olischar, M.; Shoemark, H.; Holton, T.; Weninger, M.; Hunt, R.W. The influence of music on a EEG activity in neurologically healthy newborns ≥32 weeks’ gestational age. Acta Paediatr. 2011, 100, 670–675. [Google Scholar] [CrossRef]
- Cevasco, A.M. The effects of mothers’ singing on full-term and preterm infants and maternal emotional responses. J. Music Ther. 2008, 45, 273–306. [Google Scholar] [CrossRef]
- Walworth, D. Effects of Developmental Music Groups for Parents and Premature or Typical Infants Under Two Years on Parental Responsiveness and Infant Social Development. J. Music Ther. 2009, 46, 32–52. [Google Scholar] [CrossRef]
- Haslbeck, F.B. The interactive potential of creative music therapy with premature infants and their parents: A qualitative analysis. Nord. J. Music Ther. 2014, 23, 36–70. [Google Scholar] [CrossRef]
- McLean, E. Fostering intimacy through musical beginnings: Exploring the application of communicative musicality through the musical experience of parents in a neonatal intensive care unit. Voices World Forum Music Ther. 2016, 16. Available online: https://voices.no/index.php/voices/article/view/874/721 (accessed on 30 November 2018). [CrossRef]
- Palazzi, A.; Meschini, R.; Piccinini, C.A. Music therapy intervention for the mother-preterm infant dyad: Evidence from a case study in a Brazilian NICU. Voices World Forum Music Ther. 2017, 17. Available online: https://voices.no/index.php/voices/article/view/916 (accessed on 30 November 2018). [CrossRef]
- Shoemark, H.; Dearn, T. Keeping Parents at the Centre of Family Centred Music Therapy with Hospitalized Infants. Aust. J. Music Ther. 2008, 19, 3–24. [Google Scholar]
- Hutchinson, S.W.; Spillett, M.A.; Cronin, M. Parents’ Experiences during their Infant’s Transition from Neonatal Intensive Care Unit to Home: A Qualitative Study. Qual. Rep. 2012, 17, 1–20. [Google Scholar]
- McLean, E.; McFerran Skewes, K.; Thompson, G.A. Parents’ musical engagement with their baby in the neonatal unit to support emerging parental identity: A grounded theory study. J. Neonatal Nurs. 2018. [Google Scholar] [CrossRef]
- Haslbeck, F. Three little wonders. Music Therapy with families in neonatal care. In Music Therapy with Families; Lindhal, S., Ed.; Jessica Kingsley Publishers: London, UK, 2016; pp. 19–44. [Google Scholar]
- Ettenberger, M. Music therapy in the neonatal intensive care unit: Putting the families at the centre of care. Br. J. Music Ther. 2017, 31, 12–17. [Google Scholar] [CrossRef]
- Carter, J.D.; Mulder, R.T.; Darlow, B.A. Parental stress in the NICU: The influence of personality, psychological, pregnancy and family factors. Person. Ment. Health 2007, 1, 40–50. [Google Scholar] [CrossRef]
- Pal, S.; Alpay, L.; Steenbrugge, G.; Detmar, S. An Exploration of Parents’ Experiences and Empowerment in the Care for Preterm Born Children. J. Child. Fam. Stud. 2014, 23, 1081–1089. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Alpert-Gillis, L.; Feinstein, N.F.; Crean, H.F.; Johnson, J.; Fairbanks, E.; Small, L.; Rubenstein, J.; Slota, M.; Corbo-Richert, B. Creating opportunities for parent empowerment: Program effects on the mental health/coping outcomes of critically ill young children and their mothers. Pediatrics 2004, 113, e597–e607. [Google Scholar] [CrossRef]
- Ettenberger. Family-Centred Music Therapy in the Neonatal Intensive Care Unit (NICU): Key concepts, research and examples of clinical practice. In Music Therapy for Premature and Newborn Infants, 2nd ed.; Nöcker-Ribaupierre, M., Ed.; Barcelona Publishers: Gilsum, NH, USA, 2018; in press. [Google Scholar]
- Longo, Y.; Coyne, I.; Joseph, S. The Scales of general well-being. Person. Individ. Differ. 2017, 109, 148–159. [Google Scholar] [CrossRef]
- Keith, D.R.; Weaver, B.S.; Vogel, R.L. The effect of music-based listening interventions on the volume, fat content, and caloric content of breast milk-produced by mothers of premature and critically ill infants. Adv. Neonatal Care 2012, 12, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Ak, J.; Lakshmanagowda, P.B.; G C M, P.; Goturu, J. Impact of music therapy on breast milk secretion in mothers of premature newborns. J. Clin. Diagn. Res. JCDR 2015, 9, 04–06. [Google Scholar] [CrossRef] [PubMed]
- Lai, H.-L.; Chen, C.-J.; Peng, T.-C.; Chang, F.-M.; Hsieh, M.-L.; Huang, H.Y.; Chang, S.-H. Randomized controlled trial of music during kangaroo care on maternal state anxiety and preterm infants’ responses. Int. J. Nurs. Stud. 2006, 43, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Schlez, A.; Litmanovitz, I.; Bauer, S.; Dolfin, T.; Regev, R.; Arnon, S. Combining Kangaroo Care and Live Harp Music Therapy in the Neonatal Intensive Care Unit Setting. Isr. Med. Assoc. J. 2011, 13, 354–358. [Google Scholar] [PubMed]
| Total Number of Sessions | Total Number of Participants | Total Number of Mothers | Total Number of Fathers |
|---|---|---|---|
| 30 | 122 | 106 | 16 |
| Intervention | Anxiety Levels | Stress Levels | Mood | Restfulness | Motivation |
|---|---|---|---|---|---|
| Pre-intervention | 5.8 | 5.2 | 7.1 | 4.8 | 7.2 |
| Post-intervention | 2.1 | 2.4 | 7.7 | 6.8 | 8.1 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roa, E.; Ettenberger, M. Music Therapy Self-Care Group for Parents of Preterm Infants in the Neonatal Intensive Care Unit: A Clinical Pilot Intervention. Medicines 2018, 5, 134. https://doi.org/10.3390/medicines5040134
Roa E, Ettenberger M. Music Therapy Self-Care Group for Parents of Preterm Infants in the Neonatal Intensive Care Unit: A Clinical Pilot Intervention. Medicines. 2018; 5(4):134. https://doi.org/10.3390/medicines5040134
Chicago/Turabian StyleRoa, Esteban, and Mark Ettenberger. 2018. "Music Therapy Self-Care Group for Parents of Preterm Infants in the Neonatal Intensive Care Unit: A Clinical Pilot Intervention" Medicines 5, no. 4: 134. https://doi.org/10.3390/medicines5040134
APA StyleRoa, E., & Ettenberger, M. (2018). Music Therapy Self-Care Group for Parents of Preterm Infants in the Neonatal Intensive Care Unit: A Clinical Pilot Intervention. Medicines, 5(4), 134. https://doi.org/10.3390/medicines5040134





